Abstract
Dysregulation of neutrophil extracellular trap (NET) formation has been shown to mediate disease pathology in multiple viral infections, including SARS-CoV-2. At the beginning of COVID-19 pandemic, Thierry and Roch wrote a perspective on the mechanisms by which severe SARS-CoV-2 infection may lead to uncontrolled NET formation that leads to acute respiratory distress syndrome (ARDS), systemic vascular permeability, and end organ damage. In this commentary, the progress that has been made in regards to the ideas postulated by the perspective will be discussed, with a focus on the therapeutics that target NET formation.
Keywords: COVID-19, NETosis, neutrophils, SARS-CoV-2
In a seminal 2004 paper, it was reported that neutrophils undergo a form of cell death distinct from apoptosis or necrosis termed neutrophil extracellular trap (NET) formation or NETosis [1]. NETosis is triggered by multiple mechanisms, including pattern recognition receptor (PRR) activation, cytokines (especially IL-8 and Il-1β), FcR engagement, and activated platelets. This leads to the activation of protein arginine deiminase (PAD4), which converts peptidyl-arginine to peptidyl-citrulline in histones [2]. This results in the destabilization of chromatin followed by the release of chromatin fibers and various granule and cytoplasmic proteins, including elastase, myeloperoxidase, and various cathepsins, among many others. The network of proteins and DNA trap pathogens, limit their dissemination into tissues, and facilitate their killing. Despite their important role in antimicrobial activities, dysregulated NET formation and degradation is increasingly recognized to mediate disease pathology in both infections and inflammatory conditions [3]. In support of this concept, NETs have been shown to control infection in some viral infections such as Chikungunya and poxvirus [4,5] but can exacerbate other viral infections such as dengue virus, rhinovirus, and influenza A [6–9]. In addition, increased levels of NET markers such as myeloperoxidase-DNA (MPO-DNA) are associated with worsened outcomes and multiple organ dysfunction in influenza infection [10].
In June 2020, Thierry and Roch wrote a perspective on the mechanisms by which severe SARS-CoV-2 infection may lead to uncontrolled NET formation that causes severe pathophysiological consequences. They pointed out the similar features between uncontrolled NETosis and COVID-19, including acute respiratory distress syndrome (ARDS), coagulation abnormalities, endothelial and epithelial cytotoxicity, and systemic vascular permeability, all leading to end organ damage and sepsis which complicate many cases of COVID-19 and lead to mortality [11]. Increased levels of NETs were previously linked to ARDS in both transfusion- and infection-associated acute lung injury [12,13]. The authors noted that elevated markers of NET formation had very recently been identified in COVID-19 patients, including myeloperoxidase-DNA and citrullinated histone H3 [14]; thus, they suggested that targeting NETosis might be a viable therapeutic option. Since the publication of the manuscript, a large volume of data have been generated in support of the concepts postulated by the authors. I will briefly discuss some of the data that has been generated in regards to NET formation in COVID-19, potential COVID-19 therapeutics that target NETosis, and highlight some still unanswered questions in regard to uncontrolled NETosis in SARS-CoV-2 infection.
Neutrophilia is a hallmark of acute infection, but excessive neutrophil numbers in the bloodstream and an increased neutrophil-to-lymphocyte ratio were noted early in the pandemic in hospitalized COVID-19 patients [15,16]. Neutrophils are also elevated in the nasopharyngeal epithelium and in more distal parts of the lungs of COVID patients [17]. Further, post-mortem examination of COVID-19 patients revealed high levels of neutrophil extravasation in pulmonary capillaries, heart, and liver [18]. Additional studies also reported elevated circulating NET markers, including citrullinated histone H3, neutrophil elastase, MPO-DNA, and cell-free DNA in COVID-19 patients relative to healthy controls [19–21]. It was also reported that increased circulating NETosis markers were higher in hospitalized patients that needed mechanical ventilation versus those breathing room air [14]. Further, NET markers are predictive of disease severity and end organ damage in critically ill COVID-19 patients [22]. Increased NETs are also present in the lungs of deceased COVID patients [19,20]. These data lead to the question: why do neutrophils from COVID-19 patients have a higher capacity for NET formation? It is likely for multiple reasons. First, SARS-CoV-2 particles can directly trigger NETosis in a process that requires viral entry and replication [19]. The neutrophil compartment is dysregulated in COVID-19, as evidenced by an increased occurrence of neutrophil precursors in the blood and dysfunctional mature neutrophils [23]. In addition, the milieu of inflammatory mediators in the circulation may further increase NET formation. Serum from patients with COVID-19 can induce NET formation [20], and specifically IgG purified from COVID-19 plasma can induce NET formation by neutrophils from healthy patients in vitro [24]. In addition to IgG triggering NET formation, various autoantibodies, including anti-phospholipid, anti-nuclear, anti-cytokine, and anti-NET antibodies have been reported in COVID-19 patients [24–27]. It is likely that these autoantibodies can influence the progression of COVID-19 disease as well as the ability to clear NETs. For example, anti-NET antibodies from COVID-19 patients were recently shown to stabilize NETs and impair their clearance by DNase [28]. Finally, COVID-19 patients have increased platelet-neutrophil aggregates that also increase NET production and lead to occlusion of microvessels in the lungs and other tissues [29,30].
Several compounds that target NETs were proposed by Thierry and Roch to treat complications associated with COVID-19 infection. In addition, many other NETosis-related therapeutics have been suggested and tested in patients with COVID-19 in the time since the publication of the perspective. Some drugs are already available that target key proteins in NET formation or molecules released upon NETosis, such as gasdermin D, neutrophil elastase, and DNA. Gasdermin D is thought to form pores in the nuclear and plasma membrane that are important for NET formation [31,32]. Disulfiram is an FDA-approved gasdermin D inhibitor that is used to treat alcohol use disorder. It reduced NETs in a mouse model of acute lung injury as well as in SARS-CoV-2 infected golden hamsters [33]. One registered clinical trial tested disulfiram in mild-to-moderate symptomatic COVID-19, but the results are not yet available (NCT04485130). The neutrophil elastase inhibitor Sivelestat was shown to improve lung function in several animal models of lung injury and can mitigate acute lung injury associated with acute respiratory distress syndrome (ARDS) and sepsis [34]. Further, it is approved for use in Japan and South Korea to treat ARDS, but it did not improve survival after analyses of clinical trials. It has been frequently suggested as a potential COVID-19 therapeutic [35]; however, there are no ongoing clinical trials testing this therapeutic at the time of writing of this manuscript. Several other neutrophil elastase inhibitors are currently in development, including ionodelostat and alvelestat that may be tested in COVID-19 infection or other infections. DNase I is an attractive therapeutic option to degrade DNA and disrupt the chromatin structure of NETs. Recombinant DNase I (dornase alfa) is used in the treatment of cystic fibrosis, and has also been previously used in the management of ARDS [36]. Several studies have shown its effectiveness in the management in COVID-19-associated ARDS as well [37,38]. A very recently published study showed the efficacy of combined administration of DNAase plus the IL-6 receptor antagonist tocilizumab and a JAK-1/JAK-2 inhibitor baricitinib to prevent mortality in a group of patients with COVID-19 severe respiratory failure [39]. Theirry and Roch noted that DNase treatment may also need adjunctive therapies to remove toxic proteins such as naked histones. Indeed, elevated circulating histones are reported to associate with coagulopathy and mortality in COVID-19 [40].
Another potential avenue to impact NET formation is blockade of either PRR or cytokine/chemokine signaling pathways that trigger NETosis. This is especially attractive, as pathways involving Toll-like receptors (TLR) and C-type lectins also signal to produce inflammatory cytokines that can lead to a cytokine storm in viral infection. Thierry and Roch suggested that targeting the spleen tyrosine kinase (Syk)-coupled C-type lectins CLEC2 and CLEC5A may be useful as a COVID-19 therapeutic. Both of these lectins were recently shown to trigger NETosis in response to microbes [41]. CLEC5A is abundantly expressed on neutrophils and was previously shown to bind to the dengue virus virion and lead to dengue hemorrhagic fever and dengue shock syndrome [42]. CLEC5A forms a heterodimer with TLR2, with each binding to a distinct portion of the microbial surface. Blockade of a CLEC5A/TLR2 heterodimer leads to attenuation of NET formation in dengue virus infection [41]. CLEC2 is expressed on platelets and to a lesser extent on neutrophils. It has been shown to interact with DC-SIGN to mediate capture of HIV-1 by platelets [43], and was also recently shown to be a PRR for dengue virus [41]. The SARS-CoV-2 spike protein has 22 N-linked glycans [44], but it is unknown whether SARS-CoV-2 particles bind to (Syk)-coupled C-type lectins and trigger NETosis. The spike and nucleocapsid proteins were shown to trigger NET formation, but CLEC interactions were not directly tested [45].
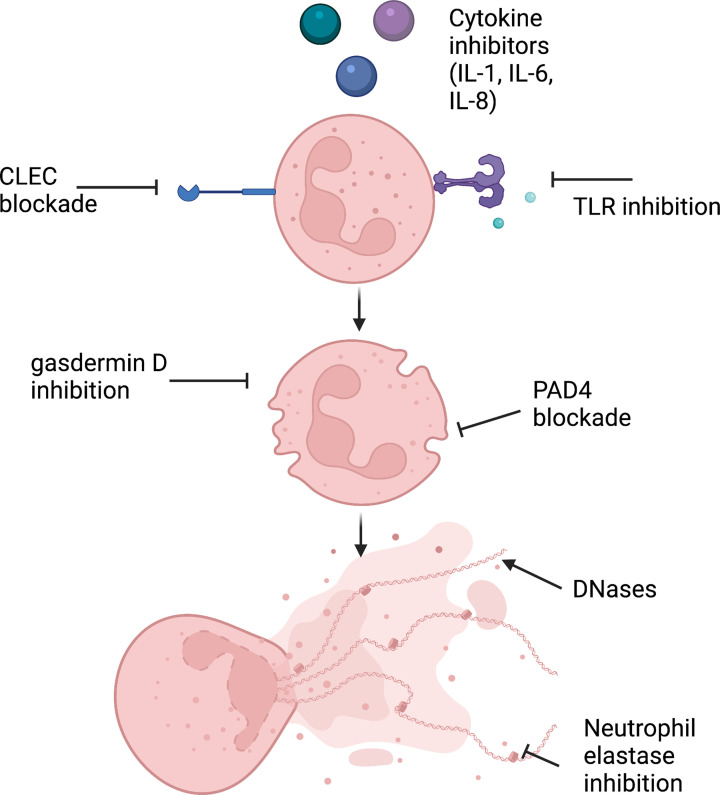
Several chemokine-targeting drugs that affect NET formation have been proposed as treatments for COVID-19 and are in various stages of testing. IL-8 can trigger NET formation by binding to CXCR2 on neutrophils; thus, an anti-IL-8 monoclonal antibody (Humax IL-8) was tested in a clinical trial (NCT04347226). However, the study was terminated early due to a lack of a significantly different outcome from standard of care for hospitalized COVID patients with severe respiratory disease. An additional phase 2 study of a noncompetitive allosteric inhibitor of CXCR1 and CXCR2 (Reparixin) showed a lower rate of clinical events in COVID patients [46]. A phase 3 trial is currently being conducted using Reparixin (NCT04878055). The IL-1 receptor antagonist anakinra is currently being tested as a treatment that for COVID-19 with an assessment of NETosis as an endpoint (NCT04594356). A summary of the therapies and pathways targeted in regards to NETosis are shown in Figure 1.
Figure 1. Summary of NETosis-related pathways that can be targeted in COVID-19 therapeutics.
Created on Biorender.com
Many unresolved questions remain in regard to NETosis in SARS-CoV-2 infection. Are patients that had severe COVID-19 symptoms and high levels of NETs more likely to develop autoimmune diseases such as systemic lupus erythematosus, multiple sclerosis, and rheumatoid arthritis in the future? Viral infections including herpesviruses, hepatitis B and C viruses, and enteroviruses are associated with the development of autoimmunity, although the virally induced mechanisms that lead to a breakdown of self-tolerance are far from completely understood [47]. It is possible that unchecked NETosis in viral infection could impact the development of autoimmune tendencies. The link between dysregulated NETosis and autoimmune diseases such as SLE, antineutrophil cytoplasmic antibody vasculitis, and rheumatoid arthritis has been reported in both animal models and clinical studies [48]. In one recent systematic review, new-onset autoimmune disease after COVID-19 infection was analyzed. The most common diseases reported were vasculitis and arthritis, although there was a wide spectrum of autoimmune diseases reported [49]. Another important question is whether people who experienced mild-to-moderate symptoms when infected with SARS-CoV-2 also had dysregulated NETosis (albeit to a lesser extent) that also results in the development of autoantibodies. While detailed analyses of the persistence of NETosis markers in COVID patients has not been reported, one study showed that citrullinated histone H3, cell-free DNA and neutrophil elastase were at the same levels as healthy controls four months postinfection [21]. Many patients who have recovered from COVID-19 report persistent symptoms and sequelae long after the primary infection, commonly referred to as ‘long COVID’ [50]. It will be important to study these patients and examine for the presence of residual NETs and autoantibodies that could be responsible for symptoms.
Abbreviations
- ARDS
acute respiratory distress syndrome
- MPO
myeloperoxidase
- NET
neutrophil extracellular trap
- PAD4
protein arginine deiminase
- PRR
pattern recognition receptor
- TLR
Toll-like receptors
Data Availability
Data sharing is not applicable to this manuscript.
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
NIH NHLBI R00HL146888 (to E.B.T.) and NIH NIGMS P20GM104357 to the UMMC Department of Physiology and Biophysics.
CRediT Author Contribution
Erin B. Taylor: Conceptualization, Writing—original draft, Writing—review & editing.
References
- 1.Brinkmann V.et al. (2004) Neutrophil extracellular traps kill bacteria. Science 303, 1532–1535 10.1126/science.1092385 [DOI] [PubMed] [Google Scholar]
- 2.Li P.et al. (2010) PAD4 is essential for antibacterial innate immunity mediated by neutrophil extracellular traps. J. Exp. Med. 207, 1853–1862 10.1084/jem.20100239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Papayannopoulos V. (2018) Neutrophil extracellular traps in immunity and disease. Nat. Rev. Immunol. 18, 134–147 10.1038/nri.2017.105 [DOI] [PubMed] [Google Scholar]
- 4.Jenne C.N.et al. (2013) Neutrophils recruited to sites of infection protect from virus challenge by releasing neutrophil extracellular traps. Cell Host Microbe 13, 169–180 10.1016/j.chom.2013.01.005 [DOI] [PubMed] [Google Scholar]
- 5.Hiroki C.H.et al. (2019) Neutrophil extracellular traps effectively control acute chikungunya virus infection. Front. Immunol. 10, 3108 10.3389/fimmu.2019.03108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Funchal G.A.et al. (2015) Respiratory syncytial virus fusion protein promotes TLR-4-dependent neutrophil extracellular trap formation by human neutrophils. PLoS ONE 10, e0124082 10.1371/journal.pone.0124082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Narasaraju T.et al. (2011) Excessive neutrophils and neutrophil extracellular traps contribute to acute lung injury of influenza pneumonitis. Am. J. Pathol. 179, 199–210 10.1016/j.ajpath.2011.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Toussaint M.et al. (2017) Host DNA released by NETosis promotes rhinovirus-induced type-2 allergic asthma exacerbation. Nat. Med. 23, 681–691 10.1038/nm.4332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cortjens B.et al. (2016) Neutrophil extracellular traps cause airway obstruction during respiratory syncytial virus disease. J. Pathol. 238, 401–411 10.1002/path.4660 [DOI] [PubMed] [Google Scholar]
- 10.Zhu L.et al. (2018) High level of neutrophil extracellular traps correlates with poor prognosis of severe influenza A infection. J. Infect. Dis. 217, 428–437 10.1093/infdis/jix475 [DOI] [PubMed] [Google Scholar]
- 11.Thierry A.R. and Roch B. (2020) SARS-CoV2 may evade innate immune response, causing uncontrolled neutrophil extracellular traps formation and multi-organ failure. Clin. Sci. (Lond.) 134, 1295–1300 10.1042/CS20200531 [DOI] [PubMed] [Google Scholar]
- 12.Caudrillier A.et al. (2012) Platelets induce neutrophil extracellular traps in transfusion-related acute lung injury. J. Clin. Invest. 122, 2661–2671 10.1172/JCI61303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lefrancais E.et al. (2018) Maladaptive role of neutrophil extracellular traps in pathogen-induced lung injury. JCI Insight 3,e98178 10.1172/jci.insight.98178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zuo Y.et al. (2020) Neutrophil extracellular traps in COVID-19. JCI Insight 5, e138999 10.1172/jci.insight.138999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang D.et al. (2020) Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 323, 1061–1069 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu J.et al. (2020) Neutrophil-to-lymphocyte ratio predicts critical illness patients with 2019 coronavirus disease in the early stage. J. Transl. Med. 18, 206 10.1186/s12967-020-02374-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reusch N.et al. (2021) Neutrophils in COVID-19. Front. Immunol. 12, 652470 10.3389/fimmu.2021.652470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bian X.W. and Team C.-P. (2020) Autopsy of COVID-19 patients in China. Natl. Sci. Rev. 7, 1414–1418 10.1093/nsr/nwaa123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Veras F.P.et al. (2020) SARS-CoV-2-triggered neutrophil extracellular traps mediate COVID-19 pathology. J. Exp. Med. 217, e20201129 10.1084/jem.20201129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Middleton E.A.et al. (2020) Neutrophil extracellular traps contribute to immunothrombosis in COVID-19 acute respiratory distress syndrome. Blood 136, 1169–1179 10.1182/blood.2020007008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ng H.et al. (2021) Circulating markers of neutrophil extracellular traps are of prognostic value in patients with COVID-19. Arterioscler. Thromb. Vasc. Biol. 41, 988–994 10.1161/ATVBAHA.120.315267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huckriede J.et al. (2021) Evolution of NETosis markers and DAMPs have prognostic value in critically ill COVID-19 patients. Sci. Rep. 11, 15701 10.1038/s41598-021-95209-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schulte-Schrepping J.et al. (2020) Severe COVID-19 is marked by a dysregulated myeloid cell compartment. Cell 182, 1419–1440 10.1016/j.cell.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zuo Y.et al. (2020) Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19. Sci. Transl. Med. 12, eabd3876 10.1126/scitranslmed.abd3876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borghi M.O.et al. (2020) Anti-phospholipid antibodies in COVID-19 are different from those detectable in the anti-phospholipid syndrome. Front. Immunol. 11, 584241 10.3389/fimmu.2020.584241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Vlachoyiannopoulos P.G.et al. (2020) Autoantibodies related to systemic autoimmune rheumatic diseases in severely ill patients with COVID-19. Ann. Rheum. Dis. 79, 1661–1663 10.1136/annrheumdis-2020-218009 [DOI] [PubMed] [Google Scholar]
- 27.Wang E.Y.et al. (2021) Diverse functional autoantibodies in patients with COVID-19. Nature 595, 283–288 10.1038/s41586-021-03631-y [DOI] [PubMed] [Google Scholar]
- 28.Zuo Y.et al. (2021) Autoantibodies stabilize neutrophil extracellular traps in COVID-19. JCI Insight 6, e150111 10.1172/jci.insight.150111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Manne B.K.et al. (2020) Platelet gene expression and function in patients with COVID-19. Blood 136, 1317–1329 10.1182/blood.2020007214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leppkes M.et al. (2020) Vascular occlusion by neutrophil extracellular traps in COVID-19. EBioMedicine 58, 102925 10.1016/j.ebiom.2020.102925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chen K.W.et al. (2018) Noncanonical inflammasome signaling elicits gasdermin D-dependent neutrophil extracellular traps. Sci. Immunol. 3, eaar6676 10.1126/sciimmunol.aar6676 [DOI] [PubMed] [Google Scholar]
- 32.Sollberger G.et al. (2018) Gasdermin D plays a vital role in the generation of neutrophil extracellular traps. Sci. Immunol. 3, eaar6689 10.1126/sciimmunol.aar6689 [DOI] [PubMed] [Google Scholar]
- 33.Adrover J.M.et al. (2022) Disulfiram inhibits neutrophil extracellular trap formation and protects rodents from acute lung injury and SARS-CoV-2 infection. JCI Insight 7, e157342 10.1172/jci.insight.157342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tagami T.et al. (2014) Effect of a selective neutrophil elastase inhibitor on mortality and ventilator-free days in patients with increased extravascular lung water: a post hoc analysis of the PiCCO Pulmonary Edema Study. J. Intensive Care 2, 67 10.1186/s40560-014-0067-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sahebnasagh A.et al. (2020) Neutrophil elastase inhibitor (sivelestat) may be a promising therapeutic option for management of acute lung injury/acute respiratory distress syndrome or disseminated intravascular coagulation in COVID-19. J. Clin. Pharm. Ther. 45, 1515–1519 10.1111/jcpt.13251 [DOI] [PubMed] [Google Scholar]
- 36.Morris C. and Mullan B. (2004) Use of dornase alfa in the management of ARDS. Anaesthesia 59, 1249 10.1111/j.1365-2044.2004.04018.x [DOI] [PubMed] [Google Scholar]
- 37.Toma A.et al. (2021) The use of dornase alfa in the management of COVID-19-associated adult respiratory distress syndrome. Crit. Care Res. Pract. 2021, 8881115 10.1155/2021/8881115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Holliday Z.M.et al. (2021) Non-randomized trial of dornase alfa for acute respiratory distress syndrome secondary to Covid-19. Front. Immunol. 12, 714833 10.3389/fimmu.2021.714833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gavriilidis E.et al. (2022) Combined administration of inhaled DNase, baricitinib and tocilizumab as rescue treatment in COVID-19 patients with severe respiratory failure. Clin. Immunol. 238, 109016 10.1016/j.clim.2022.109016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Shaw R.J.et al. (2021) Circulating histones play a central role in COVID-19-associated coagulopathy and mortality. Haematologica 106, 2493–2498 10.3324/haematol.2021.278492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sung P.S., Huang T.F. and Hsieh S.L. (2019) Extracellular vesicles from CLEC2-activated platelets enhance dengue virus-induced lethality via CLEC5A/TLR2. Nat. Commun. 10, 2402 10.1038/s41467-019-10360-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen S.T.et al. (2008) CLEC5A is critical for dengue-virus-induced lethal disease. Nature 453, 672–676 10.1038/nature07013 [DOI] [PubMed] [Google Scholar]
- 43.Chaipan C.et al. (2006) DC-SIGN and CLEC-2 mediate human immunodeficiency virus type 1 capture by platelets. J. Virol. 80, 8951–8960 10.1128/JVI.00136-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Watanabe Y.et al. (2020) Site-specific glycan analysis of the SARS-CoV-2 spike. Science 369, 330–333 10.1126/science.abb9983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Youn Y.J.et al. (2021) Nucleocapsid and spike proteins of SARS-CoV-2 drive neutrophil extracellular trap formation. Immune. Netw. 21, e16 10.4110/in.2021.21.e16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Landoni G.et al. (2022) A multicenter phase 2 randomized controlled study on the efficacy and safety of reparixin in the treatment of hospitalized patients with COVID-19 pneumonia. Infect. Dis. Ther., 10.1007/s40121-022-00644-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Smatti M.K.et al. (2019) Viruses and autoimmunity: a review on the potential interaction and molecular mechanisms. Viruses 11, 762 10.3390/v11080762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gupta S. and Kaplan M.J. (2016) The role of neutrophils and NETosis in autoimmune and renal diseases. Nat. Rev. Nephrol. 12, 402–413 10.1038/nrneph.2016.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gracia-Ramos A.E., Martin-Nares E. and Hernandez-Molina G. (2021) New Onset of Autoimmune Diseases Following COVID-19 Diagnosis. Cells 10, 3592 10.3390/cells10123592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sudre C.H.et al. (2021) Attributes and predictors of long COVID. Nat. Med. 27, 626–631 10.1038/s41591-021-01292-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this manuscript.