Abstract
Background:
Diabetes technologies, such as insulin pumps and continuous glucose monitors (CGM), have been associated with improved glycemic control and increased quality of life for young people with type 1 diabetes (T1D); however, few young people use these devices, especially those from minority ethnic groups. Current literature predominantly focuses on white patients with private insurance and does not report experiences of diverse pediatric patients with limited resources.
Methods:
To explore potential differences between Latinx and non-Latinx patients, English- and Spanish-speaking young people with T1D (n = 173, ages 11-25 years) were surveyed to assess attitudes about and barriers to diabetes technologies using the Technology Use Attitudes and Barriers to Device Use questionnaires.
Results:
Both English- and Spanish-speaking participants who identified as Latinx were more likely to have public insurance (P = .0001). English-speaking Latinx participants reported higher Hemoglobin A1c values (P = .003), less CGM use (P = .002), and more negative attitudes about technology (generally, P = .003; and diabetes-specific, P < .001) than either non-Latinx or Spanish-speaking Latinx participants. Barriers were encountered with equivalent frequency across groups.
Conclusions:
Latinx English-speaking participants had less positive attitudes toward general and diabetes technology than Latinx Spanish-speaking and non-Latinx English-speaking peers, and differences in CGM use were associated with socioeconomic status. Additional work is needed to design and deliver diabetes interventions that are of interest to and supportive of patients from diverse ethnic and language backgrounds.
Keywords: barriers, diabetes technology, disparities, Latinx, pediatrics
Introduction
Type 1 diabetes (T1D) affects approximately 200,000 youth in the United States (US), with the incidence rising annually. 1 Diabetes control is especially important, as poor glycemic management leads to complications in multiple organ systems, and chronic hyperglycemia can result in cognitive dysfunction. 2 Diabetes technology, such as insulin pumps and continuous glucose monitors (CGM), has been associated with reductions in hypoglycemia and improved glycemic control, quality of life, and treatment satisfaction.3,4 In children and adolescents, CGM use alone or combined with pump use greater than 6 days per week leads to improved glycemic control.5,6 However, data show that only 60% of children aged 2 to 17 years use a pump and only 6% use CGM. 7 The use of such technological devices is lower in minority groups. 8 A cross-sectional study among young people with T1D, ages 2 to 26 years, showed that 71% of white patients used pumps and 76% used CGM, while only 16.6% Latinx patients used pumps and 10.8% used CGM. 9
Given the continued disparities in diabetes technologies in minority groups, it is important to assess and address potential barriers to such technology in racially, ethnically diverse, and low socioeconomic status (SES) groups. A large study of mostly white adults found that younger age,
shorter time with diabetes, higher hemoglobin A1c (HbA1c), more diabetes distress, and negative attitudes about technologies were barriers to diabetes device use. 10 Additionally, adolescent patients have reported similar barriers, including fear of change, trusting technology, expectation management, hassles and burdens of devices, diabetes distress, and discomfort with technology. 11
This study assesses adolescent and young adult patient attitudes toward and barriers to diabetes-specific technology in a predominantly minority, low SES population; and investigates whether these differ from non-minority youth.
Methods
Participants
A convenience sample of youth with T1D, ages 11 to 25 years, receiving care at Children’s Hospital Los Angeles (CHLA) and their family were approached either in-person or via telephone to participate in the study. Patients who had developmental or behavioral disabilities or had literacy or cognitive limitations were excluded. Families who had upcoming clinic visits were screened manually for inclusion and exclusion criteria prior to being approached. Both Latinx and non-Latinx English-speaking patients were approached first and recruited between January 2018 and September 2018; Spanish-speaking patients were recruited between August 2019 and March 2020.
After providing informed consent, participants and their families completed questionnaires in either English or Spanish, depending on their indicated language preference at the time of enrollment. Questionnaires were completed in clinic on paper or a tablet computer, or off-site using a personal electronic device (eg, phone, tablet, laptop, or desktop computer), and took approximately 1 hour to complete. Participants received a $10 gift card and parking validation as compensation for their time. The study protocol was approved by the CHLA Institutional Review Board (IRB #CHLA-17-00159).
Demographic and Clinical Data
Participants (≥18 years) and/or their family member (if participant <18 years) self-reported demographic data, including race, ethnicity, age, gender, and insurance. Diabetes history, including diabetes device usage (CGM or insulin pump) was also self-reported, and cross-checked with electronic medical record (EMR) data. HbA1c values (point-of-care testing in clinic or laboratory testing) during the 3 months before study enrollment were collected from the EMR and averaged.
Study Questionnaires
This study used 2 questionnaires developed at the Stanford University School of Medicine—the Barriers to Diabetes Device Use and the Technology Attitude questionnaires. 10
The Barriers to Diabetes Device Use assesses potential barriers derived from academic literature and market research. 10 Participants identified whether they have encountered any and up to 19 modifiable and non-modifiable barriers.
The Technology Attitude questionnaires about technology in general and diabetes-specific technology employs 6 and 5 questions, respectively. 10 Each item was scored on a 5-point Likert scale to indicate agreement with the statement. Higher scores indicate more positive attitudes toward technology.
Both questionnaires were translated from English to Spanish for this study by an approved certified translation service.
Analysis Plan
Prior to study recruitment, a power calculation was performed to ensure that the study could observe differences in CGM and Insulin Pump use reported in previous research (eg, larger than 50% disparity between white and Latinx adult patients). 9 Assuming a type I error rate of 5% and type II error rate of 20% (ie, 80% power), only 14 patients per group were required to observe a significant difference of this magnitude. Thus, a recruitment goal of twice this amount was set (at least n = 28 per group), allowing for the observation of significant differences as small as 35% between any 2 groups.
Participants were arranged into 3 groups based on ethnicity and primary language spoken at home by their parents—Latinx Spanish speakers, Latinx English speakers, and non-Latinx English speakers. Demographic and clinical data, self-reported exposure to diabetes devices, barriers to technology, and attitudes toward general and diabetes technology were collected and stored using REDCap. 12 These data were summarized by group using descriptive statistics; continuous variables were summarized as mean and standard deviation and categorical variables as number and percentage. Total scores of attitudes about technology in general and diabetes-specific technology were calculated as summary variables. One-way analysis of variance (ANOVA) with Scheffé post-hoc testing was used to assess mean differences in continuous demographic variables; Pearson Chi-squared or Fisher’s Exact tests were used to examine differences in all categorical variables, where appropriate. Patient data were excluded from analysis if responses to either the Barriers to Diabetes Device Use or the Technology Attitude questionnaires were incomplete. Two patients were unsure about previous CGM use, but their responses were otherwise complete and included in analyses.
To consider the independent effects of language and ethnicity on all outcomes of interest while accounting for covariates, multivariable logistic regression models were used to evaluate measures of diabetes device exposure (CGM or pump use, currently or ever). Multivariable linear regression models were used to evaluate attitudes toward technology (summed total scores from 3 Likert-scale items on 2 subscales) while accounting for covariates; standardized beta coefficients with bootstrapped standard error terms are reported for these analyses. Sub-analyses were conducted as needed using models appropriate for a given outcome variable (ie, logistic regression for CGM use, linear regression for HbA1c). A Type I error (ie, alpha) level of <0.05 was used to determine statistical significance of any test. All analyses were performed using Stata/SE 14.2 (StataCorp, LLC, College Station, Texas).
Results
Recruitment
Of the 129 Spanish-speaking eligible participants, 49 potential participants were approached equaling 38% of the eligible population. The reasons for not approaching the other 62% included missing the potential participants in clinic, provider recommending not approaching the potential participants, and potential participants rescheduling or no-showing for clinic appointments. Of the 49 potential participants approached, 33 were enrolled and 16 declined (67% recruitment rate). Of the 33 enrolled, 30 completed the assessments and were included in the final analysis.
Of the 561 English-speaking eligible participants, 191 patients were approached equaling 34% of the eligible population. The reasons for not approaching the other 66% included missing the patient in clinic, provider recommending not approaching the potential participants, patients rescheduling or no-showing for clinic appointments, and potential participants transitioning out of the clinic. Of the 191 potential participants approached, 150 were enrolled and 41 declined (79% recruitment rate). Of the 150 enrolled, 143 completed the assessments and were included in the final analysis.
Of note, English-speaking families completed questionnaires electronically either in clinic or at their preferred location, whereas the majority of Spanish-speaking Latinx families completed their questionnaires on paper in clinic.
Demographic and Clinical Characteristics
Demographic and clinical characteristics are shown in Table 1. Several notable differences in participant characteristics were observed. Significantly more Latinx participants (both English and Spanish-speaking) were publicly insured, compared to non-Latinx English-speaking participants (P < .0001). Latinx Spanish-speaking participants were significantly younger than participants from other groups (P < .001), and Latinx English-speaking participants reported higher HbA1c levels (P = .003).
Table 1.
Demographic Characteristics.
| Variable n (%) | Category/unit | English-Speaking, Non-Latinx (n = 75) | English-Speaking Latinx (n = 68) | Spanish-Speaking Latinx (n = 29) | P-Value |
|---|---|---|---|---|---|
| Race | African-American or Black | 4 (5.33) | 1 (1.47) | 0 | .004 |
| Asian-American or Pacific Islander | 5 (6.67) | 0 | 0 | ||
| White | 30 (40.00) | 16 (23.53) | 6 (20.69) | ||
| Other/Declined | 36 (48.00) | 51 (75.00) | 23 (79.31) | ||
| Sex | Male | 42 (56.00) | 42 (61.76) | 14 (46.67) | .35 |
| Female | 32 (42.67) | 25 (36.76) | 14 (46.67) | ||
| Other/Declined | 1 (1.33) | 1 (1.47) | 2 (6.67) | ||
| Age (in years) | Mean (SD) | 16.80 (3.36) | 17.62 (2.78) | 14.21 (1.91) | <.0001 |
| Health insurance | Private | 45 (60.00) | 9 (13.24) | 3 (10.00) | <.0001 |
| Public | 30 (40.00) | 59 (86.76) | 27 (90.00) | ||
| HbA1c | Mean (SD) | 8.63 (1.88) | 9.69 (2.22) | 8.49 (1.94) | .003 |
In a sub-analysis of HbA1c data using multiple linear regression to account for age differences, Latinx English-speaking participants reported higher HbA1c levels than non-Latinx English-speaking or Latinx Spanish-speaking participants (P = .002); age at enrollment was not significantly associated with differences in HbA1c after accounting for study group (P = .42).
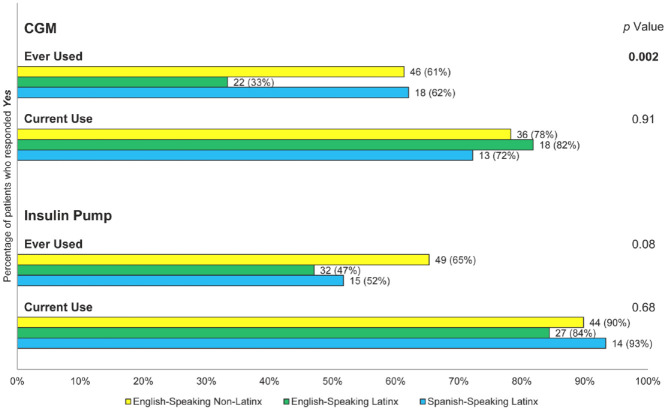
CGM and Pump Use
Figure 1 shows the frequencies and percentages of CGM and insulin pump use by study group. Overall, Latinx English-speakers reported lower lifetime rates (“ever use”) of CGM (33%; p = 0.002) compared to other groups (61% of non-Latinx English-speaking, 62% of Latinx Spanish-speaking); however, among those participants reporting any CGM use before the study, current CGM use was reported at similar rates across patient groups (76-82%; P = .91). All groups reported similar insulin pump use before the study (65% of non-Latinx English-speaking, 47% of Latinx English-speaking, 52% of Latinx Spanish-speaking; P = .08), and like CGM use, current insulin pump use among those reporting any previous exposure was comparable across groups (84-93%; P = .68).
Figure 1.
CGM and insulin pump use.
Current use percentages are calculated based on the number of patients who report any CGM or Insulin Pump use ever.
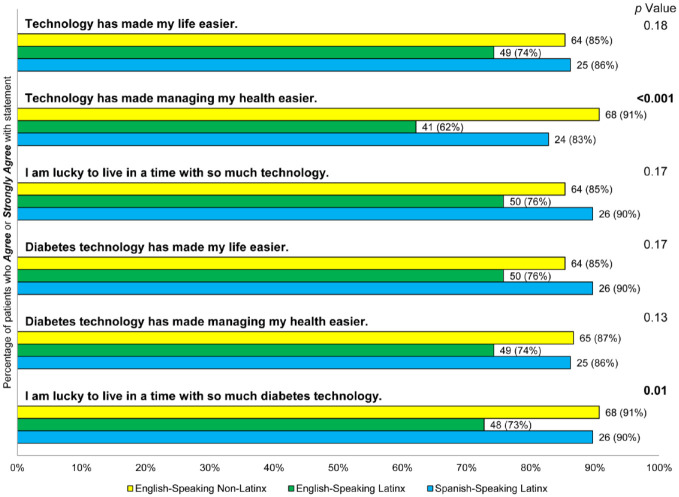
Attitudes about Technology
Participants’ attitudes about technology in general, and diabetes-specific technology, were assessed in multiple linear regression models controlling for age, sex, HbA1c, and insurance (Figure 2). HbA1c values were strongly associated with negative attitudes about technology (β = 0.26, P = 0.001), where those participants with higher values tended to disagree more strongly with the idea that technology is beneficial, regardless of ethnicity or spoken language. Also, Latinx English-speaking participants disagreed more strongly with the idea that technology is beneficial (β = 0.28, P = 0.004), while Latinx Spanish-speaking participants’ attitudes did not significantly differ from those of non-Latinx English speakers (P = 0.12; see Table 2). These same associations held when participants considered the diabetes-specific technology, where Latinx English-speaking participants viewed technology as less beneficial (β = 0.24, P < 0.001), and HbA1c values were strongly and positively related to negative attitudes about technology (β = 0.28, P = 0.001).
Figure 2.
Attitudes about technology by study group.
Table 2.
Predictors of Negative Attitudes about Technology.
| Attitude/variables | Standardized beta (β) | Bootstrapped standard error | P-Value |
|---|---|---|---|
| Negative attitudes about technology in general (total score) | |||
| Age | −0.04 | 0.18 | .62 |
| Female sex | 0.11 | 0.40 | .19 |
| Public insurance | −0.15 | 0.49 | .13 |
| A1c | 0.26 | 0.17 | .001 |
| Latinx ethnicity | |||
| English-speaking | 0.28 | 0.45 | .004 |
| Spanish-speaking | 0.13 | 0.52 | .12 |
| Negative attitudes about diabetes-specific technology (total score) | |||
| Age | −0.12 | 0.17 | .08 |
| Female sex | 0.04 | 0.44 | .69 |
| Public insurance | −0.02 | 0.44 | .79 |
| A1c | 0.28 | 0.20 | .001 |
| Latinx ethnicity | |||
| English-speaking | 0.24 | 0.48 | .02 |
| Spanish-speaking | 0.05 | 0.56 | .53 |
In sub-analyses of attitudes toward technology by age group, similar associations between HbA1c and negative attitudes were observed, especially in the case of diabetes-specific technology (P-values <.01). As with technology adoption, differences between study groups were far more pronounced in young adult participants (P-values <.02) than in adolescents. In adolescent participants, the Latinx English-speaking group reported more negative attitudes about technology than either Latinx Spanish speakers or non-Latinx English speakers, but this effect was not significant after adjusting for covariates (P = .22).
Barriers to Technology Adoption
Table 3 reports the percentage of participants in each study group that endorsed barriers to technology. Neither language nor ethnicity accounted for significant differences in exposure to a range of barriers to the utilization of diabetes technology. However, Latinx English-speaking participants reported feeling nervousness more frequently when dealing with technology, consistent with their attitudes about technology.
Table 3.
Barriers to Technology.
| Barriers n (%) of patients who have encountered barrier | English-Speaking, Non-Latinx (n = 75) | English-Speaking Latinx (n = 68) | Spanish-Speaking Latinx (n = 29) | P-Value |
|---|---|---|---|---|
| Cost of supplies | 4 (5.33) | 4 (5.88) | 0 | .57 |
| Cost of device | 4 (5.33) | 1 (1.47) | 0 | .39 |
| Insurance coverage | 8 (10.67) | 5 (7.35) | 0 | .18 |
| It is stressful wearing device all of the time | 14 (18.67) | 9 (13.24) | 4 (13.79) | .67 |
| I do not like having diabetes devices on my body | 13 (17.33) | 16 (23.53) | 4 (13.79) | .52 |
| I do not like how diabetes devices look on my body | 15 (20.00) | 9 (13.24) | 3 (10.34) | .45 |
| I get nervous that the device might not work | 6 (8.00) | 13 (19.12) | 3 (10.34) | .13 |
| I do not want to take more time from my day to take care of my diabetes | 5 (6.67) | 2 (2.94) | 2 (6.90) | .59 |
| I get nervous to depend on technology | 2 (2.67) | 7 (10.29) | 1 (3.45) | .15 |
| I worry about what other will think of me | 8 (10.67) | 5 (7.35) | 4 (13.79) | .59 |
| I do not like diabetes devices because people notice them & ask questions | 11 (14.67) | 9 (13.24) | 2 (6.90) | .66 |
| I am too busy to learn how to use a new technology or device | 1 (1.33) | 2 (2.94) | 0 | .77 |
| My diabetes care team has never talked with me about the tech options | 0 | 0 | 0 | — |
| I do not understand what to do with the info or features of the devices | 0 | 0 | 0 | — |
| I am not able to get my diabetes care team to write me a prescription | 1 (1.33) | 1 (1.47) | 0 | 1.00 |
| I do not get enough help from my family | 0 | 0 | 0 | — |
| I do not get enough help from my diabetes care team in using devices | 0 | 0 | 0 | — |
| I do not want to have more information about my diabetes | 1 (1.33) | 0 | 0 | 1.00 |
| My family does not think diabetes devices are important for taking care of my diabetes | 1 (1.33) | 0 | 1 (3.45) | .31 |
Impact of Attitudes and Barriers on Technology Adoption
Despite large percentages of Latinx English-speaking participants reporting less frequent CGM or pump use, these associations were not significant in multiple logistic regression models accounting for insurance, exposure to barriers, attitudes toward technology, age, sex, and HbA1c. Notably, participants with public insurance were less likely to report lifetime CGM use, compared to participants with private insurance (OR = 0.31, 95% CI = 0.13-0.72, P = .007; see Table 4). Attitudes toward technology (generally or diabetes-specific) and barriers to access were not associated with differences in current or lifetime CGM use.
Table 4.
Predictors of CGM and Pump Use.
| Usage/variable | Odds ratio | 95% CI | P-Value |
|---|---|---|---|
| Ever used CGM | |||
| Age | 0.91 | (0.63-1.30) | .59 |
| Female sex | 1.11 | (0.55-2.22) | .77 |
| Public insurance | 0.31 | (0.13-0.72) | .007 |
| A1c | 1.21 | (0.83-1.77) | .32 |
| Attitudes toward technology | 0.96 | (0.88-1.04) | .32 |
| Psychosocial barriers | 0.83 | (0.67-1.02) | .07 |
| Latinx ethnicity | |||
| English-speaking | 0.54 | (0.22-1.08) | .14 |
| Spanish-speaking | 1.54 | (0.58-4.75) | .43 |
| Current CGM use | |||
| Age | 0.87 | (0.61-1.23) | .42 |
| Female sex | 1.13 | (0.57-2.23) | .73 |
| Public insurance | 0.58 | (0.25-1.30) | .19 |
| A1c | 1.14 | (0.79-1.66) | .49 |
| Attitudes toward technology | 1.00 | (0.92-1.08) | .97 |
| Psychosocial barriers | 0.91 | (0.74-1.12) | .37 |
| Latinx ethnicity | |||
| English-speaking | 0.51 | (0.22-1.18) | .12 |
| Spanish-speaking | 0.93 | (0.33-2.63) | .89 |
| Ever used insulin pump | |||
| Age | 1.39 | (0.90-2.13) | .13 |
| Female sex | 3.26 | (1.46-7.24) | .004 |
| Public insurance | 0.86 | (0.33-2.24) | .76 |
| A1c | 0.65 | (0.44-0.98) | .04 |
| Attitudes toward technology | 0.80 | (0.72-0.89) | <.0001 |
| Psychosocial barriers | 0.73 | (0.58-0.93) | .01 |
| Latinx ethnicity | |||
| English-speaking | 0.78 | (0.31-1.95) | .59 |
| Spanish-speaking | 0.66 | (0.20-2.17) | .49 |
| Current insulin pump use | |||
| Age | 1.16 | (0.76-1.76) | .50 |
| Female sex | 2.65 | (1.19-5.89) | .02 |
| Public insurance | 0.84 | (0.32-2.22) | .73 |
| A1c | 0.57 | (0.37-0.88) | .01 |
| Attitudes toward technology | 0.79 | (0.70-0.88) | <.0001 |
| Psychosocial barriers | 0.62 | (0.47-0.81) | .001 |
| Latinx ethnicity | |||
| English-speaking | 0.90 | (0.34-2.35) | .83 |
| Spanish-speaking | 0.66 | (0.20-2.20) | .49 |
Pump use was not significantly associated with ethnicity or spoken language in logistic regression models. However, both attitudes toward technology (total score; current: OR = 0.79, 95% CI = 0.70-0.88, P < .0001; lifetime: OR = 0.80, 95% CI = 0.72-0.89, P < .0001) and number of barriers encountered (current: OR = 0.62, 95% CI = 0.58-0.93, P = .001; lifetime: OR = 0.73, 95% CI = 0.58-0.93, P = .01) were significantly associated with reduced odds of current or lifetime use of insulin pumps. In addition, pump use was significantly associated with HbA1c, where each 2% increase in HbA1c was associated with nearly 50% reduced odds of current (OR = 0.57, 95% CI = 0.37-0.88, P = .01) or lifetime pump use (OR = 0.65, 95% CI = 0.44-0.98, P = .04).
Technology adoption by age group
To examine whether predictors of CGM and insulin pump use varied by age, participants were subdivided into 2 groups—adolescents (ages 11-17) and young adults (YA; ages 18-25)—and their responses were examined post-hoc in multiple logistic regression models. Ethnic identity and SES only predicted ever use of CGM in YA (SES: OR = 0.15, 95% CI = 0.05-0.53, P = .003) but no other variations in use. Attitudes and barriers did not impact CGM use.
Similarly, associations between HbA1c and insulin pump usage (ever or current) were only significant in the YA (ever: OR = 0.42, 95% CI = 0.25-0.71, P = .001; current: OR = 0.38, 95% CI = 0.22-0.68, P = .001), and not in the adolescent group (P-values >0.13). For YA, each 2% increase in HbA1c was associated with approximately 60% reduced odds of using a pump. As with CGM use, adolescents showed an age effect for pump use, where older adolescents reported greater odds of pump use ever (OR = 2.78, 95% CI = 1.15-6.69, P = .02) or current (OR = 2.42, 95% CI = 1.02-5.73, P = .04). Similar effects for attitudes and barriers were observed.
Discussion
CHLA serves a unique pediatric population that is ideal for studying attitudes and access to diabetes-specific technology. Eighty-five percent of patients identify with racial and ethnic minority groups, and 72% are publicly insured. To our knowledge, this is one of the first studies to investigate attitudes about diabetes-specific technology and barriers to its use in a diverse group of youth with a focus on the Latinx community. Similar to previously published reports as well as national data, we found that our Latinx participants had public insurance more frequently. Latinx English-speaking participants also had less positive attitudes toward general and diabetes-specific technology compared to both Latinx Spanish speakers and non-Latinx English speakers. These variations in attitudes and adoption among Latinx youth highlight the importance of culturally sensitive interventions that consider individual patient needs, rather than perpetuate broad assumptions based on ethnic identity.
Socioeconomic disparities consistently affect the Latinx community and explain much of the reported differences in CGM use. U.S. Census data show that approximately 6.1 million of under-resourced, marginalized children in the United States are Latinx 13 and only 46.4% of Latinx have private insurance, compared to 67.1% of the white population. 14 Our Latinx English- and Spanish-speaking participants rely significantly more on public insurance to a similar degree. For minorities, low levels of SES also reduce their odds of using the Internet for health information. 15 According to the Pew Research Center, Latinx adults are less likely to own a computer (57% vs 82%) or have access to high-speed internet at home (61% vs 79%) compared to whites. The increased availability and use of smartphones (79% vs 82%) is bridging these digital gaps, 16 but broadband internet access via smartphone devices may limit access to some advanced telehealth services and features. 17 Regardless of cultural background, holding negative views about diabetes technology was strongly associated with reduced odds of current or lifetime insulin pump use. Due to the fact our Latinx English-speaking participants (but not Spanish speakers) reported negative views more frequently, suggests a deeper issue than access alone in influencing both their technology uptake and subsequent health outcomes.
Studies examining acculturation, the process by which an immigrant group adopts the cultures of a host population, 18 found that less acculturated Latinx youth with T1D had stronger family support and oversight for their diabetes as well as improved glycemic control, compared to Latinx youth in more acculturated families. 19 Additionally, studies indicate that the patient-provider relationship needs to feel personal for members of the Latinx community, with authentic relationships and trust. 20 Trust influences health-related factors, including quality of the patient-provider interaction and patient healthcare utilization,21,22 and is associated with cultural or race concordance or a perceived personal similarity to one’s provider. 23 For patients with diabetes, trust has been shown to increase self-efficacy and treatment adherence.24,25
Spoken language may also present a barrier, as limited English proficiency (LEP) is generally associated with poorer health. 26 In previous studies, language concordance, when a patient has a physician who is highly proficient in their preferred language, has resulted in better glycemic control for patients with type 2 diabetes.27,28 At CHLA, 21.4% of our providers who care for patients with T1D, including diabetes educators, registered nurses, and social workers, identify as Latinx, and 42.9% of our providers endorse the ability to speak with patients in Spanish. While our robust percentages at CHLA may support families with LEP in adopting diabetes-specific technology more frequently and exhibiting greater glycemic control, we found that any benefits of language or cultural concordance was limited to our Latinx Spanish-speaking participants. Latinx English-speaking participants report the highest HbA1c levels of all participants in this current study, as well as greater negative attitudes about diabetes-specific technology associated with lower insulin pump adoption rates, even after accounting for age and insurance status.
Latinx English-speaking patients may be more acculturated than their parents, and thus have more familial conflict and decreased communication, creating a family “acculturation gap” that impacts their care and functioning. 29 Latinx parents of adolescents with T1D have previously described integrating T1D management as a united family and expressed gratitude for access to insulin pumps and CGMs.19 Although their adolescents emphasized the importance of family, they were less convinced their heritage influenced their diabetes care and prioritize being a “normal adolescent” and acculturated. 30 In our study, it is possible that Latinx participants with parents with LEP reside in a less acculturated community offering more familial support and thus higher adoption of diabetes-specific technology. Pediatric practices structured around cultural competency are scarce, but have shown to improve communication, outcomes, and satisfaction.31,32
This study observed differences by age group in terms of attitudes about technology and its adoption, where Latinx English-speaking YA reported views more negative than their younger adolescent counterparts. Since adolescents are typically receiving direct care assistance from their parents or caregivers, while YA are more likely responsible for their own care, adolescents may be buffered from any socioeconomic or cultural influences that are contributing to more negative attitudes about technology. Notably, some Latinx English-speaking adolescent participants shared many of the same negative views about diabetes-specific technology held by their older peers, but not enough to reach statistical significance. Additional research is needed on the care transition process from adolescence to adulthood for Latinx patients, with specific attention to the role acculturation may play in shaping views and behaviors.
Our cohort did not associate either ethnicity or language with differences in barriers to adoption of diabetes-specific technology. When compared to current, mostly adult literature, some similarities and differences are observed. The physicality of devices poses a barrier for many adults 10 as well as pediatric populations. Insurance and cost of supplies, 10 however, appear to be more of a hurdle for adults whereas very few participants in our cohort endorsed them as barriers. This may largely be due to coverage from California Children’s Services (CCS). In the State of California, Medicaid recipients with certain chronic diseases, such as T1D, are eligible for this ancillary insurance coverage. 33 Specifically, when certain criteria are met, CCS covers diabetes supplies, including pumps and CGM. This may lessen the hurdle for many pediatric patients in California to use diabetes devices, specifically for those with historically disadvantaged backgrounds. Prahalad et al 34 found young people with CCS coverage for CGM can successfully use and continue CGM technology. An additional study by Addala et al 35 found that CGM initiation for young people with CCS resulted in improvement in glycemic control; and if coverage for CGM was lost, glycemic control worsened.
More research into how cultural background shapes medical decisions is needed, as it may be the key to better understanding differences in technology attitudes and other aspects of medical care. In the current study, identifying as “Other” was the most common response when racial identity was queried, even among non-Latinx English-speaking patients. Instead of presuming that a patient has certain experiences because of their appearance, spoken language, or identity, care providers should learn about how each of their patients experiences diabetes personally, as a range of factors may impact their perceptions and willingness to change, if necessary. Based on the current study, actual use of diabetes-specific technologies, may be influenced by many factors, including degree of acculturation, patient-provider trust, insurance and other care access problems, or physician preference; ethnicity or general exposure to technology have less impact on attitudes and behavior in patients with T1D.
Strengths and Limitations
This study sheds light on disparities in care between pediatric Latinx and non-Latinx groups with T1D; however, several methodological limitations must be addressed. The study is cross-sectional and explores only one point in time. Cross-sectional data may be biased by immediate feelings or recent experiences at the time of the study, and precludes inference of causal effects (eg, between attitudes or psychosocial barriers and technology adoption). Also, a convenience sample was used, possibly resulting in a sample that is not a true representative of the population. Specifically, the Latinx Spanish-speaking participants did not include patients over the age of 17, so attitudes and behaviors reported for this subgroup do not include young adults, who may encounter greater socioeconomic or cultural barriers. Additionally, the questionnaires used to assess barriers and attitudes toward technology were validated in adults and adapted in this study for pediatrics and Spanish-speakers and their family members. Pediatric-specific focus groups were not used to develop or modify these questionnaires. Furthermore, Spanish-speaking participant recruitment was completed after English-speaking participant recruitment, opening the possibility of time impacting outcomes. Lastly, although an approved service was used, the Spanish questionnaires were not fully validated with translation into Spanish and back to English.
Conclusions
In conclusion, Latinx English-speaking participants who responded to our questionnaires expressed less positive attitudes toward general and diabetes-specific technology in contrast with both their Latinx Spanish-speaking and non-Latinx English-speaking peers. Differences in CGM use were associated with socioeconomic status, as patients on public insurance used these devices less frequently. Insulin pump use was related to differences in HbA1c, where higher HbA1c was associated with less frequent use. Neither ethnicity nor language was associated with differences in self-reported barriers to use of diabetes-specific technology. Given increased risk for poor glycemic control and diabetes complications for Latinx young people, further investigation into technology, language, and cultural barriers is needed. Increasing device uptake, as well as cultural competency and concordance, are important for improving diabetes care in the Latinx community.
Acknowledgments
The authors would like to thank all young people and families who participated in this study.
Footnotes
Abbreviations: CGM, continuous glucose monitor; CHLA, Children’s Hospital Los Angeles; LEP, limited English proficiency; SES, socioeconomic status; T1D, type 1 diabetes.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was partially funded by The Leona M. and Harry B. Helmsley Charitable Trust and The Gustavus and Louise Pfeiffer Research Foundation.
ORCID iDs: David Tsai  https://orcid.org/0000-0002-9431-4857
https://orcid.org/0000-0002-9431-4857
Mark W. Reid  https://orcid.org/0000-0002-1942-225X
https://orcid.org/0000-0002-1942-225X
Jennifer K. Raymond  https://orcid.org/0000-0003-1866-4932
https://orcid.org/0000-0003-1866-4932
References
- 1. Mobasseri M, Shirmohammadi M, Amiri T, Vahed N, Hosseini Fard H, Ghojazadeh M. Prevalence and incidence of type 1 diabetes in the world: a systematic review and meta-analysis. Health Promot Perspect. 2020;10(2):98-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. DiMeglio LA, Evans-Molina C, Oram RA. Type 1 diabetes. Lancet. 2018;391(10138):2449-2462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tamborlane WV, Beck RW, Bode BW, et al. ; Juvenile Diabetes Research Foundation Continuous Glucose Monitoring Study Group. Continuous glucose monitoring and intensive treatment of type 1 diabetes. N Engl J Med. 2008;359:1464-1476. [DOI] [PubMed] [Google Scholar]
- 4. Phillip M, Battelino T, Rodriguez H, Danne T, Kaufman F. Use of insulin pump therapy in the pediatric age-group: consensus statement from the European Society for Paediatric Endocrinology, the Lawson Wilkins Pediatric Endocrine Society, and the International Society for Pediatric and Adolescent Diabetes. Diabetes Care. 2007;30:1653-1662. [DOI] [PubMed] [Google Scholar]
- 5. Chase HP, Beck RW, Xing D, et al. Continuous glucose monitoring in youth with type 1 diabetes: 12-month follow-up of the Juvenile Diabetes Research Foundation continuous glucose monitoring randomized trial. Diabetes Technol Ther. 2010;12(7):507-515. [DOI] [PubMed] [Google Scholar]
- 6. Bergenstal RM, Tamborlane WV, Ahmann A, et al. Sensor Augmented Pump Therapy for A1C Reduction (STAR 3) Study: results from the 6-month continuation phase. Diabetes Care. 2011;34(11):2403-2405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Miller KM, Foster NC, Beck RW, et al. Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry. Diabetes Care. 2015;38(6):971-978. [DOI] [PubMed] [Google Scholar]
- 8. Willi SM, Miller KM, DiMeglio LA, et al. Racial-ethnic disparities in management and outcomes among children with type 1 diabetes. Pediatrics. 2015;135(3):424-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sheikh K, Bartz SK, Lyons SK, DeSalvo DJ. Diabetes device use and glycemic control among youth with type 1 diabetes: a single-center, cross-sectional study. J Diabetes Res. 2018;2018:5162162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Tanenbaum ML, Hanes SJ, Miller KM, Naranjo D, Bensen R, Hood KK. Diabetes device use in adults with type 1 diabetes: barriers to uptake and potential intervention targets. Diabetes Care. 2017;40(2):181-187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Vaala SE, Hood KK, Laffel L, Kumah-Crystal YA, Lybarger CK, Mulvaney SA. Use of commonly available technologies for diabetes information and self-management among adolescents with type 1 diabetes and their parents: a web-based survey study. Interact J Med Res. 2015;4(4):e24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Harris PA, Taylor R, Minor BL, et al. ; REDCap Consortium. The REDCap consortium: building an international community of software partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Pew Research Center: Latinx Trends. Childhood Poverty among Latinxs Sets Record, Leads Records. Pew Research Center; 2015. [Google Scholar]
- 14. CDC. Health of Mexican American Population. Summary Health Statistics Tables for the U.S. Population. National Health Interview Survey; 2018. [Google Scholar]
- 15. Yoon H, Jang Y, Vaughan PW, Garcia M. Older adults’ internet use for health information: digital divide by race/ethnicity and socioeconomic status. J Appl Gerontol. 2020;39(1):105-110. [DOI] [PubMed] [Google Scholar]
- 16. St George SM, Delamater AM, Pulgaron ER, Daigre A, Sanchez J. Access to and interest in using smartphone technology for the management of type 1 diabetes in ethnic minority adolescents and their parents. Diabetes Technol Ther. 2016;18(2):104-109. [DOI] [PubMed] [Google Scholar]
- 17. Perrin A, Turner E. Smartphones Help Blacks, Hispanics Bridge Some – but Not All – Digital Gaps with Whites. Pew Research Center. Updated August 20, 2019. Accessed August 31, 2017. https://www.pewresearch.org/fact-tank/2019/08/20/smartphones-help-blacks-hispanics-bridge-some-but-not-all-digital-gaps-with-whites/ [Google Scholar]
- 18. Berry JW. Immigraton, acculturation, and adaptation. Appl Pyschol. 1997;46:5-34. [Google Scholar]
- 19. Hsin O, La Greca AM, Valenzuela J, Moine CT, Delamater A. Adherence and glycemic control among Latinx youth with type 1 diabetes: role of family involvement and acculturation. J Pediatr Psychol. 2010;35:156-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Julliard K, Vivar J, Delgado C, Cruz E, Kabak J, Sabers H. What Latina patients don’t tell their doctors: a qualitative study. Ann Fam Med. 2008;6(6):543-549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Moskowitz D, Lyles CR, Karter AJ, Adler N, Moffet HH, Schillinger D. Patient reported interpersonal processes of care and perceived social position: the Diabetes Study of Northern California (DISTANCE). Patient Educ Couns. 2013;90(3):392-398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. LaVeist TA, Isaac LA, Williams KP. Mistrust of health care organizations is associated with underutilization of health services. Health Serv Res. 2009;44(6):2093-2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Street RL, Jr, O’Malley KJ, Cooper LA, Haidet P. Understanding concordance in patient-physician relationships: personal and ethnic dimensions of shared identity. Ann Fam Med. 2008;6(3):198-205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lee YY, Lin JL. The effects of trust in physician on self-efficacy, adherence and diabetes outcomes. Soc Sci Med (1982). 2009;68:1060-1068. [DOI] [PubMed] [Google Scholar]
- 25. Fernandez A, Seligman H, Quan J, Stern RJ, Jacobs EA. Associations between aspects of culturally competent care and clinical outcomes among patients with diabetes. Med Care. 2012;50(9 Suppl 2):S74-S79. [DOI] [PubMed] [Google Scholar]
- 26. Sentell T, Braun K. Low health literacy, limited English proficiency, and health status in Asians, Latinos, and other racial/ethnic groups in California. J Health Commun. 2012;17(Suppl 3):82-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Fernandez A, Schillinger D, Warton EM, et al. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE). J Gen Intern Med. 2011;26(2):170-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Parker MM, Fernández A, Moffet HH, Grant RW, Torreblanca A, Karter AJ. Association of patient-physician language concordance and glycemic control for limited-English proficiency Latinos with type 2 diabetes. JAMA Intern Med. 2017;177(3):380-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Telzer EH. Expanding the acculturation gap-distress model: an integrative review of research. Human Dev. 2010;53:313-340. [Google Scholar]
- 30. Gandhi K, Baranowski T, Anderson B, et al. Psychosocial aspects of type 1 diabetes in Latino- and Asian-American youth. Pediatr Res. 2016;80:347-355. [DOI] [PubMed] [Google Scholar]
- 31. Pascual AB, Pyle L, Nieto J, Klingensmith GJ, Gonzalez AG. Novel, culturally sensitive, shared medical appointment model for Latinx pediatric type 1 diabetes patients. Pediatr Diabetes. 2019;20(4):468-473. [DOI] [PubMed] [Google Scholar]
- 32. Jaramillo J, Snyder E, Dunlap JL, Wright R, Mendoza F, Bruzoni M. The Latinx Clinic for Pediatric Surgery: a model to improve parent-provider communication for Latinx pediatric surgery patients. J Pediatr Surg. 2016;51(4):670-674. [DOI] [PubMed] [Google Scholar]
- 33. California Children’s Services Program Overview. CA Department of Health Care Services. 2020. Accessed June 16, 2020. https://www.dhcs.ca.gov/services/ccs/Pages/ProgramOverview.aspx [Google Scholar]
- 34. Prahalad P, Addala A, Buckingham BA, Wilson DM, Maahs DM. Sustained continuous glucose monitor use in low-income youth with type 1 diabetes following insurance coverage supports expansion of continuous glucose monitor coverage for all. Diabetes Technol Ther. 2018;20:632-634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Addala A, Maahs DM, Scheinker D, Chertow S, Leverenz B, Prahalad P. Uninterrupted continuous glucose monitoring access is associated with a decrease in HbA1c in youth with type 1 diabetes and public insurance. Pediatr Diabetes. 2020;21(7):1301-1309. [DOI] [PMC free article] [PubMed] [Google Scholar]