Abstract
Background:
A 2017 umbrella review defined the technology-enabled self-management (TES) feedback loop associated with a significant reduction in A1C. The purpose of this 2021 review was to develop a taxonomy of intervention attributes in technology-enabled interventions; review recent, high-quality systematic reviews and meta-analyses to determine if the TES framework was described and if elements contribute to improved diabetes outcomes; and to identify gaps in the literature.
Methods:
We identified key technology attributes needed to describe the active ingredients of TES interventions. We searched multiple databases for English language reviews published between April 2017 and April 2020, focused on PwD (population) receiving diabetes care and education (intervention) using technology-enabled self-management (comparator) in a randomized controlled trial, that impact glycemic, behavioral/psychosocial, and other diabetes self-management outcomes. AMSTAR-2 guidelines were used to assess 50 studies for methodological quality including risk of bias.
Results:
The TES Taxonomy was developed to standardize the description of technology-enabled interventions; and ensure research uses the taxonomy for replication and evaluation. Of the 26 included reviews, most evaluated smartphones, mobile applications, texting, internet, and telehealth. Twenty-one meta-analyses with the TES feedback loop significantly lowered A1C.
Conclusions:
Technology-enabled diabetes self-management interventions continue to be associated with improved clinical outcomes. The ongoing rapid adoption and engagement of technology makes it important to focus on uniform measures for behavioral/psychosocial outcomes to highlight healthy coping. Using the TES Taxonomy as a standard approach to describe technology-enabled interventions will support understanding of the impact technology has on diabetes outcomes.
Keywords: A1C, diabetes care and education, diabetes self-management education and support, taxonomy, technology-enabled self-management, umbrella review
Introduction
Multiple umbrella reviews identify significant improvement in clinical outcomes, including hemoglobin A1C (A1C) when technology is part of the model of care.1-4 These technologies include diabetes devices (eg, connected pens, glucose monitors and continuous glucose monitors), mobile devices (eg, mobile applications, wearables, fitness trackers) and technology-enabled communications (eg, text messaging, 2-way chat). In a 2017 review of high-quality systematic reviews, a framework evolved identifying 4 key elements of technology-enabled interventions associated with significant change in A1C. 1 The technology-enabled self-management (TES) feedback loop includes communication between the care team and people with diabetes (PwD); transmission and analysis of patient generated health data (PGHD); general or tailored education based on ADCES7 Self-Care Behaviors™, 5 informed by PGHD; and individualized PGHD feedback delivered in real-time or asynchronously by technology or care team. 1
As technology has evolved, digital/virtual programs focused on chronic condition management and supported by employers or health systems emerged (eg, Onduo, Livongo®, BlueStar®) that implement the TES feedback loop elements to provide care, education, and support. Additionally, the Association of Diabetes Care & Education Specialists (ADCES) has continued to define the role of the diabetes care and education specialist in the integration and implementation of technology-enabled self-management solutions. 6 While achieving target A1C is an essential piece of the puzzle, it is important to understand the type of technology, design of the interventions, user experience, and workflow, which influence glycemic, other physiological, and behavioral/psychosocial diabetes self-management outcomes.7,8 Recent systematic reviews have evaluated the impact of technology in diabetes care and education. While numerous authors cite the 2017 review, most focus on the association of technology with lowering A1C. Since 2017, the National Standards for Diabetes Self-Management Education and Support 9 and the American Diabetes Association (ADA) 10 Standards of Care (SOC) have recognized the TES framework for effective technology-enabled interventions. However, it is unclear if the TES framework is being used as a guide to develop and evaluate technology-enabled interventions.
The purpose of this umbrella review was to (1) develop a taxonomy to describe intervention attributes in technology-enabled interventions; (2) review recent, high-quality systematic reviews and meta-analyses to determine if the elements of the TES framework were described and whether the elements continue to contribute to improved diabetes outcomes; and (3) to identify gaps in the literature regarding technology-enabled diabetes self-management.
Methods
Phase 1 Taxonomy Development
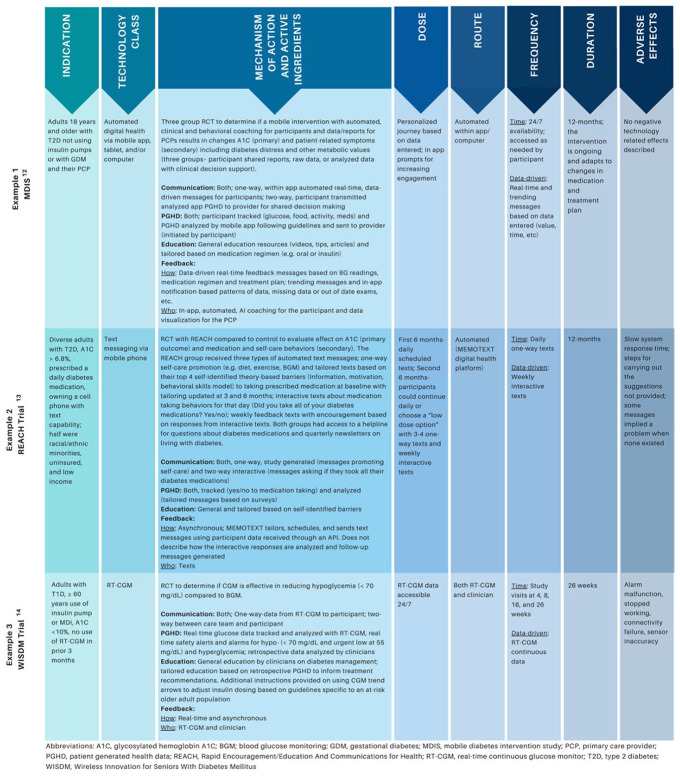
We reviewed the TES framework from the 2017 review 1 and identified additional key technology attributes needed to describe the active ingredients of technology-enabled interventions that lower A1C levels. As an exemplar, we applied the medication full prescribing information (FPI) 11 to define the detailed attributes of technology-enabled interventions, including indications, class, mechanism of action, active ingredients, dose, route, frequency, duration, and adverse effects.
The attribute definitions were evaluated for appropriateness and completeness in a 2-step process by applying the definitions to 3 representative technology studies.12-14 First, 2 authors applied the definitions to each study, then a third author reviewed for discordance. The definitions were then revised and applied to the same studies in a second review. Figure 1 shows the application of the definitions to the studies.
Figure 1.
Taxonomy definitions applied to exemplar studies.
Phase 2 Umbrella Review
We identified parameters a priori and searched for English language reviews published between April 2017 and April 2020, focused on PwD (population) receiving diabetes care and education (intervention) and using technology enabled self-management in randomized controlled trials (comparator) that impact, glycemic, other physiological, and behavioral/psychosocial outcomes. A medical librarian searched multiple databases using subject headings and text words related to technology, diabetes mellitus, self-management, self-care or patient education, and systematic reviews or meta-analysis following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) recommendations. 15 See Figure 2 for the PRISMA diagram.
Figure 2.
PRISMA flow diagram 2009.
Sources, Searching, and Review
Cumulative Index to Nursing and Allied Health Literature (CINAHL), Cochrane Database of Systematic Reviews, Cochrane Register of Controlled Trials, MEDLINE Complete, APA PsycInfo, and Web of Science were searched in April 2020 and repeated in June 2020 to retrieve current literature. (See Supplemental Appendix A). After identifying duplicates, reviewers screened abstracts from 723 articles specific to technology-enabled diabetes self-management or education interventions. Two independent reviewers screened each abstract (DI, ML, JB, JD, VC). A third reviewer (DG or MP) resolved disagreements. A total of 111 full text articles (US and international) met inclusion criteria. Reviews were included if 2 authors reviewed for inclusion criteria and identified 2 or more databases for their search strategy. Reviews were excluded if they did not measure outcomes, if studies were protocols of reviews or incomplete, if technology was not the focus of the study, or if studies were included in the 2017 review. Studies of school site/classroom interventions, diabetes devices only, or solely feasibility, costs, and mortality were excluded. Full text review was completed on 111 studies. Each study was reviewed by 2 independent reviewers (DG, DI, JB, JD, ML, MP, VC) and conflicts were discussed to consensus. Fifty studies were retained.
Screening for Methodological Quality
Four reviewers in teams of 2 (DG and DI; JB and JD) assessed the 50 studies for methodological quality, including risk of bias, following
the AMSTAR-2 quality assessment guidelines. 16 This 16-question guideline was designed to identify critical flaws pertaining to study design and allow researchers to assign overall confidence. The research team identified 9 critical questions (# 1,2,3,4,5,6,8,9,16). Studies with one or more critical flaws were excluded. Studies with non-critical flaws but no critical flaws were included in the review and final analysis. Twenty-six reviews were retained. (See Supplemental Appendix A for critical questions and critical flaws)
Data Extraction and Analysis
Eight reviewers in teams of 2 (JB and JY; JD and AH; DG and DI; VC and ML) independently entered data into a data extraction table then met to confirm assessments. Tables included the following information: research question and components of PICO (population, intervention, comparator group, outcome); description of included studies (number, year, location, duration, participant characteristics, types of clinicians involved in interventions, technology and devices used); outcomes (technology usability, behavioral/psychosocial, ADCES7 Self-Care Behaviors™, physiological and glycemic including A1C); and TES features. Supplemental data were used where available to gather complete information.
Results
Phase 1
Building upon the 2017 TES feedback loop 1 and definitions applied in this review, we developed a preliminary taxonomy to be used when describing technology-enabled interventions. Similar to other taxonomies, 17 the Taxonomy of Technology-Enabled Self-Management Interventions (TES Taxonomy) was developed for 2 purposes: (1) to standardize the description of technology-enabled self-management interventions and (2) to ensure that future research uses the taxonomy to encourage replication, comparison, and evaluation. 18 Table 1 describes the attributes and the definitions of the TES Taxonomy.
Table 1.
Taxonomy of Technology-Enabled Self-Management Interventions (TES Taxonomy).
| Taxonomy attributes | Definition |
|---|---|
| Indication | Identifies who the intervention is for and who it is not for |
| Technology class | Describes the main technology device class (eg, BGM, CGM, mobile apps, text messaging, insulin pump, pen devices, online peer support) |
| Mechanism of action and active ingredients | Provides a description of the intervention including individual components and desired outcomes, and defines the features of the TES Feedback loop: |
| Communication: One-way, 2-way, both | |
| PGHD: Data tracked, analyzed or both | |
| Education: General or tailored based on PGHD | |
| Feedback: | |
| How: Real-time, asynchronous, or both | |
| Who: Human (care team, interventionist) or technology (AI) | |
| Dose | Describes how much of the intervention is delivered (eg, just in time, accessible 24/7, anytime anywhere, front loaded with taper) |
| Route | How the intervention is delivered (eg, automated, human-augmented, or both) and who or what delivers it |
| Frequency | Describes how often and when the intervention is delivered |
| Time-based: Daily, weekly, as needed, etc. | |
| Data-driven | |
| Duration | Describes how long the intervention is delivered. (eg, 12-weeks, 6-months, maintenance, intermittent) |
| Adverse effects | Describes any untoward effects identified from the study (eg, device malfunction vs user device issues, technical connectivity issue or Internet access) |
Abbreviations: AI, artificial intelligence; BGM, blood glucose monitoring; CGM, continuous glucose monitoring; PGHD, patient generated health data; TES, technology-enabled self-management.
Phase 2
Study Characteristics
Twenty-six reviews, published between 2017 and 2020, conducted in multiple countries, were included in this umbrella review,19-44 See Table 2. The number of studies in the selected reviews ranged from 7 to 111, and the number of participants ranged from 30 to 23,648. Participants included children through older adults with mean age range from 8-80 years. Three (11.5%) reviews did not report age ranges26,34,42, 2 (9.5%) reported only “adults.”27,29 Four (15.4%) included studies with only T1D,22,37,42,44 14 (53.8%) included studies with only T2D,19,20,23,24,27-29,31-33,38,39,42,44 and 12 (46.2%) reviews included both T1D and T2D.21,24-26,29,34-36,39,41-43 Studies utilized a variety of clinicians; 3 (11.5%) studies did not report type of clinician20,23,37, 5 (19.2%) studies stated only “healthcare professionals.”19,32,39,41,42
Table 2.
Study Characteristics (n = 26).
| Authors | Articles (n) | Subjects (n) | Mean age or range (years) | Country/continent, language | Clinician |
|---|---|---|---|---|---|
| Aminuddin et al 19 | 26 | 2645 | 47.5-65.8 | Bangladesh, China, Democratic Republic of Congo,
Finland, India, Iran, Japan, Mexico, Norway,
Philippines, South Korea, Thailand,
US English |
HCPs |
| Cai et al 20 | 14 | 2129 | 51.1-66.1 | Canada, China, Finland, India, Japan, Korea, Mexico,
Norway, Spain, US English |
Not reported |
| Faruque et al 21 | 111 | 23648 | 24-75 | Australia, Canada, Korea, US English |
CDE/BCADM/Educator, MD/DO, Peer/CHW, Pharmacist,
Psychologist/behaviorist, RDN/Dietitian/Nutritionist,
RN Others: Allied health, Care manager, Diabetes team, Exercise Physiologist, Exercise trainer, Non-specialized support, Researcher |
| Feigerlová et al 22 | 8 | 757 | 15-38.4 | Australia, Italy, Spain, US No language restrictions |
CDE/BCADM/Educator, MD/DO Other: Nurse care manager |
| Haider et al 23 | 11 | 1710 | 47-59 | China, Hungary, India, US, New Zealand, Iran,
Bangladesh, UAE, Philippines English |
Not reported |
| Heitkemper et al 24 | 13 | 3257 | 50.5-70.9 | US or not reported Cantonese, English, Spanish | CDE/BCADM/Educator, Peer/CHW,
RDN/Dietitian/Nutritionist, RN Others: Clinician, Research coordinator |
| Hu et al 25 | 14 | 1324 | 25-68 | Canada, China, Greece, India, Israel, Italy, Korea,
Poland Saudi Arabia, Spain, US English |
CDE/BCADM/Educator, MD/DO, RN Others: CDS systems, Diabetes teams, Research teams (Caregivers, Nursing specialists, Researchers) |
| Huang et al 26 | 13 | 1164 | Not reported | Asia, Australia English |
RN |
| Kirk et al 27 | 35 | 4528 | Adults | Australia, Belgium, Brazil, Canada, Denmark, Finland, France, Germany, India Netherlands, South Korea, UK, US English |
MD/DO, RN Others: Healthcare team, Researcher |
| Kongstad et al 28 | 27 | 4215 | 51.7-62 | Country/continent not reported Danish, English, Norwegian, Swedish |
Coach, Peer/CHW, RDN/Dietitian/Nutritionist, RN |
| Kuo et al 29 | 16 | 30-786 | Adults | Australia, Canada, England, Germany, Netherlands, South
Korea, Thailand, US Chinese, English |
Coach, Peer/CHW, RN Not reported |
| Lee et al 30 | 41 | 2582 | Children and teens (mean 14, range: 10-17). Adults (mean 24, range: 24-43). | Asia, Europe, North America No language restrictions |
Case Manager, CDE/BCADM/Educator, Peer/CHW, MD/DO, Pharmacist, Psychologist/Behaviorist, RDN/Dietitian/Nutritionist, RN |
| Liu et al 31 | 24 | 2285 | 48.4-69.5 | Africa, Asia, Europe, North America English |
CDE/BCADM/Educator, Coach, MD/DO, Peer/CHW, RN |
| Michaud et al 32 | 17 | 2453 | 46.7-66.2 | Countries/continents not reported English |
HCPs Other: specialized team |
| Shen et al 33 | 35 | 6475 | 42.3-79.9 | Canada, China, Congo, England, Finland, Italy, Japan,
Korea, Norway, Poland, Spain, Turkey,
US *Language not reported |
CDE/BCADM/Educator, MD/DO, RN |
| So and Chung 34 | 7 | 853 | Not reported | Iran, South Korea, US English |
MD/DO, RN Other: Student |
| Tao et al 35 | 80 | 11820 | 8.5-70.8 | Asia, Europe, North America, Oceania English |
Coach, NP, Peer/CHW |
| Tchero et al 36 | 42 | 6170 | 13.3-71 | Australia, Canada, China, Georgia, Finland, France,
Greece, Israel, Italy, Japan, Korea, Poland, South
Korea, Spain, UK, US English |
CDE/BCADM/Educator Coach, NP, Pharmacist, RN |
| Wang et al 37 | 8 | 602 | 12.9-38.4 | Australia, France, Germany, Italy, Scotland,
US English |
Not reported |
| Wei et al 38 | 18 | 3954 | 52-68 | Australia, Belgium, China, Germany, Iran, Jordan, Korea,
UK, US English |
Pharmacist, Psychologist/Behaviorist,
RDN/Dietitian/Nutritionist, RN Others: Clinicians, Paraprofessionals |
| Wu et al 39 | 13 | 974 | Not reported | Australia, Italy, Japan, Korea, Netherlands, Norway, UK,
US Chinese, English |
HCPs |
| Wu et al 40 | 17 | 2225 | 42.3-65.8 | Canada, Democratic Republic of the Congo, Finland,
Japan, Korea, Mexico, Norway, UK, US No language restrictions |
HCPs |
| Wu et al 41 | 19 | 6294 | 45.5-68.4 | US, Europe English |
HCPs, MD/DO, RN Others: Clinical health psychologists, Exercise experts |
| Wu et al 42 | 26 | 2526 | T1D: 34.9-39.7 T2D: 44.7-66.3 | Type 1: Australia, Europe Type 2: Asia, Australia, Europe, North America Pre-diabetes: US GDM: US No language restrictions |
HCPs |
| Yang et al 43 | 17 | 20-237 | 26.35-63.8 | Australia, Belgium, China, Denmark, Egypt, Greece, Iran,
Thailand, Turkey, UK, US English |
RN |
| Yoshida et al 44 | 32 | 3290 | 45-67 | China, Iran, India, Japan, South Korea,
US Europe English |
MD/DO, RN Others: Medical care providers; some non-medical |
Abbreviations: BC-ADM, board certified, advanced diabetes management; CDE, certified diabetes educator (now known as certified diabetes care and education specialists); CHW, community health worker; HCP, healthcare professional/provider; MD/DO, physician; NP, nurse practitioner; RDN, registered dietitian nutritionist; RN, registered nurse; T1D, type 1 diabetes; T2D, type 2 diabetes.
Technology and Outcomes
Studies (n = 26) reviewed multiple types of technology interventions and their impact on diabetes self-management outcomes (glycemic, other physiological and behavioral/psychosocial). Studies most frequently (n = 18, 69.2%) evaluated smartphone and mobile applications (smartphone/apps)19,20,22,25-27,29-31,33-37,39-42 followed by text messaging and secure messaging (texting/secure messaging [n = 14, 53.8%]),19,23-35 internet or website interventions (web/internet/websites/portals [n = 13, 50.0%]),22,24-33,35,43 and telehealth related patient-provider interactions (telehealth/video conferencing/telemedicine/provider chat [n = 12, 46.2%]).21,22,24,29-36,43 Technology interventions are displayed in Table 3.
Table 3.
Types of Technology Included in the Interventions and Outcomes Measured (n = 26).
| Authors | Type of technology |
Diabetes outcomes |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Glycemic a | Other physiological b | Behavorial and psychosocial c | |
| Aminuddin et al 19 | X | X | A1C d | BMI, BP | QoL, SE d | |||||||||
| Cai et al 20 | X | A1C | BMI, WC | |||||||||||
| Faruque et al 21 | X | X | X | A1C i , Hypo | BMI | D, DD, QoL | ||||||||
| Feigerlová et al 22 | X | X | X | A1C d | ||||||||||
| Haider et al 23 | X | X | A1C d | PS, QoL, SE, SM | ||||||||||
| Heitkemper et al 24 | X | X | X | X | X | X | A1C i | |||||||
| Hu et al 25 | X | X | X | X | X | X | A1C d , Hypo | BMI | ||||||
| Huang et al 26 | X | X | X | X | A1Cf,j, Gluc f , Hypo | PS, SM | ||||||||
| Kirk et al 27 | X | X | X | X | X | X | A1C, Gluc | BMI, BP, PA d , Weight | ||||||
| Kongstad et al 28 | X | X | X | X | PA d | |||||||||
| Kuo et al 29 | X | X | X | X | X | X | X | X | A1C d | BMI, PA d , Weight d | E d , QoL d , SE d | |||
| Lee et al 30 | X | X | X | X | X | A1C d , Gluc, Hypo | BMI, BP, HLD, Weight | QoL | ||||||
| Liu et al 31 | X | X | X | X | X | X | X | A1C d | BP d | QoL, SM | ||||
| Michaud et al 32 | X | X | X | X | X | X | A1C d | Weight | QoL | |||||
| Shen et al 33 | X | X | X | X | X | A1C d | ||||||||
| So and Chung 34 | X | X | X | X | A1C d , Gluc | SM | ||||||||
| Tao et al 35 | X | X | X | X | X | X | X | A1C d | DD, PS, SM | |||||
| Tchero et al 36 | X | X | X | A1Cd,g | ||||||||||
| Wang et al 37 | X | A1C e | ||||||||||||
| Wei et al 38 | X | A1C d | BP, HLD, Weight | SM | ||||||||||
| Wu et al 39 | X | X | A1C d | BP, HLD, Weight | QoL | |||||||||
| Wu et al 40 | X | A1C d , Gluc | ||||||||||||
| Wu et al 41 | X | A1C h | SM | |||||||||||
| Wu et al 42 | X | A1C g | ||||||||||||
| Yang et al 43 | X | X | X | X | A1C d , Gluc d | BMI, HLD | ||||||||
| Yoshida et al 44 | X | BP d , HLD, Weight | ||||||||||||
|
Type of Technology (listed in order
of most common)
1. Smartphones/Apps (applications) 2. Texting and SMS (short message service) 3. Web/Internet/Websites/Portals 4. Telehealth/Video Conferencing/Telemedicine/Provider Chat 5. Telephone 6. Remote Monitoring 7. Email Messaging 8. Personal Computer 9. Wearables 10. Digital Therapeutics 11. Health Information Technologies 12 | ||||||||||||||
A1C, hemoglobin A1C; Gluc, fasting blood glucose; Hypo, hypoglycemia.
BMI, body mass index; BP, blood pressure; HLD, hyperlipidemia; PA, physical activity; WC, waist circumference; Weight.
D, depression/depressive symptoms; DD, diabetes distress; E, empowerment; PS, patient satisfaction; QoL, quality of life; SE, self-efficacy; SM, self-management.
Statically significant outcome.
Significant with Apps only (not SMS).
Significant with SMS only (not Apps).
Significant mean difference larger in T2D.
Significant in just T2D.
Greatest reduction at first follow-up timepoint.
Greater significance in T1D.
The studies explored diabetes self-management (glycemic, other physiological and behavioral/psychological) related outcomes (Table 3). For glycemic outcomes, most (n = 24, 92.3%)19-27,29-43 studies included A1C as an outcome. The most common technology interventions and glycemic outcomes were smartphone, mobile applications, and A1C (n = 18, 69.2%),19,20,22,25-27,29-31,33-37,39-42 with most (n = 13/18, 72.2%) having statistically significant findings.19,22,25,29-31,33-37,39,40,42 Over half of the studies assessed non-glycemic physiological outcomes (other physiological outcomes) (n = 14, 53.8%).19,21,25,27-32,35,38,40,43,44 The most common other physiological outcome measured was BMI (n = 8, 33.3%),19-21,25,27,29,30,43 which was assessed in relation to smartphone and mobile application interventions (n = 6/8, 75.0%).19,20,25,27,29,30 No studies assessing BMI reported statistical significance. Thirteen studies (50.0%) assessed behavioral/psychosocial outcomes.19,21,23,26,29-32,34,35,38,40,41 The most common behavioral/psychosocial outcome measure, quality of life (n = 8, 30.8%)19,21,23,29-32,40 was linked to texting/SMS interventions (n = 6/8, 75.0%).19,29-32,40 However, only one study found a significant outcome between quality of life and texting/SMS interventions. 29 Another common outcome measured was general self-management behaviors (n = 7, 26.9%)23,26,31,34,35,38,41 using smartphone and mobile applications (n = 5/7, 71.4%).26,31,34,35,41 However, none of these outcomes were significant.
Interventions incorporating multiple modalities (eg, texting or telehealth in combination with web-based tools) more frequently had significant outcomes compared to single interventions. There is also strong evidence supporting A1C reduction with a variety of technologies (Table 3). Three studies identified that technology-enabled interventions were more effective in people with T2D,36,39,40 one study determined interventions were more effective in T1D; 26 however, no pattern emerged to identify technologies with the greatest reduction in A1C for specific populations. Two studies reported greater short-term A1C reductions at the first follow-up timepoint.21,24
Table 4 identifies the ADCES7 self-care behaviors™ 5 addressed by the studies included in the reviews. Healthy eating was the most common self-care behavior addressed in the studies and being active ranked second highest. Only eight (38%) studies included problem–solving,19,22,24,26,27,30,42,43 which ranked second lowest, and 5 (23.8%) studies focused on healthy coping.19,24,29,30,34
Table 4.
ADCES7 Self-Care Behaviors™ Addressed by Technology (n = 26).
| Authors | Healthy eating | Being active | Monitoring | Taking medications | Reducing risk | Problem solving | Healthy coping |
|---|---|---|---|---|---|---|---|
| Aminuddin et al 19 | X | X | X | X | X | X | X |
| Cai et al 20 | X | X | X | X | |||
| Faruque et al 21 | X | X | X | ||||
| Feigerlová et al 22 | X | X | |||||
| Haider et al 23 | X | X | X | ||||
| Heitkemper et al 24 | X | X | X | X | X | X | X |
| Hu et al 25 | X | X | X | X | |||
| Huang et al 26 | X | X | X | X | X | ||
| Kirk et al 27 | X | X | X | ||||
| Kongstad et al 28 | X | ||||||
| Kuo et al 29 | X | X | X | ||||
| Lee et al 30 | X | X | X | X | X | X | |
| Liu et al 31 | X | ||||||
| Michaud et al 32 | X | X | X | X | |||
| Shen et al 33 | X | X | X | X | X | ||
| So and Chung 34 | X | X | X | X | |||
| Tao et al 35 | X | X | X | ||||
| Tchero et al 36 | X | X | |||||
| Wang et al 37 | X | ||||||
| Wei et al 38 | X | X | X | X | |||
| Wu et al 39 | X | X | X | ||||
| Wu et al 40 | X | X | X | X | |||
| Wu et al 41 | X | X | X | ||||
| Wu et al 42 | X | X | |||||
| Yang et al 43 | X | X | X | X | X | ||
| Yoshida et al 44 | X | X | |||||
| Total | 19 | 18 | 16 | 16 | 9 | 8 | 5 |
Intervention Features
In this review we evaluated the 4 essential intervention features of the TES feedback loop: communication, patient generated health data (PGHD) analysis, education, and feedback. We used the TES feature definitions from Greenwood et al, 1 and expanded the definition of feedback into 2 sub-categories. To compare the results of this study with the 2017 research, the 21 studies that included a meta-analysis with significant mean difference in A1C between the intervention and control groups are displayed in Table 5. In the table, the authors are ordered by the mean difference in A1C from greatest to least.
Table 5.
Technology-Enabled Self-Management (TES) Feedback Loop Intervention Features of Studies With Meta-Analysis and Significant A1C Mean Difference Between Intervention and Control Group (n = 21).
| Authors a | Communication one-way, 2-way, or both | Patient generated health data tracked, analyzed or both | Education content general, tailored or both | Feedback How: Realtime, asynchronous or both |
Feedback- Who: Individual/team, automated or both |
A1C significant mean difference (%) |
|---|---|---|---|---|---|---|
| Yang et al 43 | Both | Both | Both | Both | Both | −0.68 |
| Wu et al 39 | Both | Both | Both | AS | Both | −0.67 (T2D) |
| −0.37 (T1D) | ||||||
| Huang et al 26 | Both | Tracked | Both | AS | I/T | −0.62 (SMS) |
| −0.99 (T1D) | ||||||
| −0.65 (T2D) | ||||||
| Faruque et al 21 | Two | Both | Both | AS | I/T | −0.57 (3 m) |
| −0.28 (4-12 m) | ||||||
| −0.26 (>12 m) | ||||||
| Aminuddin et al 19 | Both | Both | Both | Both | I/T | −0.55 |
| Wu et al 40 | Both | Both | Both | Both | Both | −0.51 |
| Heitkemper et al 24 | Both | Tracked | Both | Both | I/T | −0.36 (6 m) |
| −0.27 (12 m) | ||||||
| Shen et al 33 | Both | Both | Both | Both | Both | −0.48 |
| Tchero et al 36 | Both | Both | Both | Both | Both | −0.48 (T2D) |
| −0.26 (T1D) | ||||||
| Kuo et al 29 | Both | Tracked | Both | Both | I/T | −0.43 |
| Liu et al 31 | Both | Both | Both | AS | Both | −0.42 |
| Tao et al 35 | Both | Both | Both | RT | Both | −0.31 |
| Michaud et al 32 | Both | Both | Both | Both | Both | −0.30 |
| Haider et al 23 | One-way | Both | Both | AS | Both | −0.38 |
| Kirk et al 27 | Both | Tracked | Both | Both | Both | −0.38 |
| Hu et al 25 | Both | Both | Both | Both | Both | −0.28 |
| Wang et al 37 | Both | None | None | Both | Automated b | −0.25 (apps) |
| Wu et al 42 | Both | Both | Both | Both | Both | −0.25 (T2D) |
| Wu et al 41 | Both | Both | Both | Both | I/T | −0.22 |
| Lee et al 30 | Both | Both | Both | Both | Both | −0.18 |
| Wei et al 38 | Two | Tracked | General | RT | I/T | −0.12 |
Abbreviations: Apps, applications; AS, asynchronous; I/T, individual/team; m, months; RT, real-time; SMS, short message service; T1D, type 1 diabetes; T2D, type 2 diabetes.
Authors ordered from greatest A1C decrease.
Some not defined.
Communication was defined as a one-way or 2-way exchange of information between the participant and care team. Twenty reviews described studies with 2-way communication, with one study including only one-directional texts. 23 while 18 (85.7%)19,20,22,24-37,39-44 of the studies included both one-way and 2-way communication. PGHD was defined as either tracked or tracked and analyzed (both). Fifteen (71.4%) of the reviews19,21,23,25,30-33,35,36,39-43 described PGHD as both and 5 (23.8%) reviews24,26,27,29,38 described as tracked only. One did not clarify how PGHD were used, but detailed that interventions included either texts or a diabetes management app. 37 Education content was defined as either general self-management education or tailored based on self-care behaviors and PGHD, with 19 of the reviews identifying both types of education (90.4%).19,21,23-27,29-33,35,36,39-43 General education was described in one 38 (4.7%) and not described in one 37 (4.7%). In this review, we expanded feedback into 2 sub-categories: how the feedback was provided, either real time or asynchronously, and who provided the feedback, an individual/diabetes team member or via an automated response. In this review, feedback to participants was reported as asynchronous by 5 (23.8%) reviews,21,23,26,31,39 both asynchronous and real-time by 1419,24,25,27,29,30,32,33,36,37,40-43 (66.6%) and only real-time by 235,38 (9.5%) reviews. The feedback was reported as delivered by an individual/diabetes care team in 7 (33%) reviews.19,21,24,26,29,38,41 One (4.7%) described only automated feedback 37 and 13 (61.9%) reviews23,25,27,30-33,35,36,39,40,42,43 described both individual/team and automated feedback.
Gaps for Technology-Enabled Self-Management
A key finding is that the systematic reviews and meta-analyses lacked overall intervention descriptions making it difficult to identify the mechanism of action of the intervention and which features impacted health outcomes. Supplemental Appendix B applies the TES Taxonomy to the 21 meta-analyses in Table 5. Five additional gaps were identified (Table 6). There was lack of evaluation of the impact of continuous glucose monitoring (CGM) or mobile health interventions, and minimal focus on healthy coping or evaluation of pyschosocial impact. In addition there was limited description of theoretical frameworks used to develop interventions. Finally, studies need to report on ethnicity/race and health disparities.45-50
Table 6.
Research Gaps Identified and Future Opportunities.
| Gaps | Our findings | Opportunities for future research |
|---|---|---|
| 1. Lack of CGM/mobile health research integrated into self-management interventions | While CGM and mobile health research exists, studies specific to CGM/mobile health and its integration with behavior change are lacking | Future research is needed to understand how patient- generated BGM/CGM and mobile health data are being used to impact self-management, tailor education, and engage in real-time 2-way communication with the care team. |
| 2. Lack of interventions focused on healthy coping | Healthy coping is central to all other diabetes self-care behaviors. 5 Yet, there was an overall lack of interventions that described healthy coping and therefore it is unknown if healthy coping was delivered, and if so to what extent. | There is a myriad of opportunities to support healthy coping using technology approaches. Online peer support has been found to support healthy coping 45 and can be delivered by community health workers. 46 Exploration of technology-delivered healthy coping is needed. |
| 3. Minimal data on psychosocial impact | While psychosocial outcomes were examined (ie, quality of life, diabetes distress, depressive symptoms), validated tools were not always used in the systematic reviews studied. | Using validated tools while not overwhelming participants with survey questions can be challenging. We recommend researchers follow guidelines recommended by the ADA position statement on psychosocial care. 47 |
| 4. Lack of theoretical frameworks | Systematic reviews are not describing guiding theoretical frameworks when designing interventions to impact behavior change. | Future research needs to report on all theoretical frameworks and identify when they are lacking. |
| 5. Health inequity and health disparities | The primary systematic reviews did not report ethnicity/race/disability data, and therefore we are unable to report on those data. However, we know diabetes disparities exist. Often individuals with disabilities are excluded from research. 48 Further, technology disparities exist.49,50 | Future research should seek to identify how diabetes technologies work in a variety of populations, including those from different race and ethnic categories, but also those who may have disabilities that may or may not be related to diabetes (ie, blind or low vision, deaf or hard of hearing). |
Abbreviations: BGM, blood glucose monitoring; CGM, continuous glucose monitoring.
Discussion
The intent of this umbrella review was to develop a taxonomy to describe intervention attributes in technology-enabled interventions and review high-quality systematic reviews and meta-analyses, published since the original 2017 review, to determine if the elements of the TES framework are being described in the interventions, and if the elements continue to result in achieving diabetes outcomes. Additionally, this umbrella review identified significant gaps in the literature regarding technology-enabled diabetes self-management. Our findings confirm technology-enabled self-management interventions with a TES feedback loop continue to be associated with a reduction in A1C.
The Taxonomy of Technology-Enabled Self-Management Interventions (TES Taxonomy)
Given the evolving models of care and the rapid influx of technology-enabled interventions, more emphasis needs to be placed on clear description of the design and process of implementing interventions. The lack of description of intervention components and how the TES features are operationalized makes it difficult to pinpoint types or features of technology-enabled interventions that impact glycemic, other physiological and behavioral/psychosocial diabetes self-management outcomes. Research, including systematic reviews, should fully describe intervention details, including participant characteristics; who the interventionist(s) were; what type of technology was used, including details on automation or tailored delivery; how often participants interacted with technology and/or the interventionist, including the duration of the intervention; while following a systematic process. A 2019 paper referenced key characteristics of digital interventions that need to be identified prior to recommending the intervention, specifically the “mechanism of action” that will impact outcomes. 51 Incorporating the TES Taxonomy can support recommendations of technology-enabled interventions by clinicians. Recent research describes similar challenges with digital health interventions, indicating a lack of consistency in reporting original research, which makes conducting systematic reviews more challenging.8,52 This lack of overall description could happen for several reasons, including publication word limitations or proprietary concerns. Scientists should be clear when reporting methodology so appropriate conclusions can be drawn.
Update to the 2017 Review
In this update, mobile and smartphone interventions were successful in lowering A1C with 2 studies reporting greater change in A1C in T2D compared to T1D.36,42 Similar to our original review, there was heterogeneity in the interventions, technologies, and methodologies. In addition to A1C being the most common clinical outcome reported, there is a lack of assessment and evaluation of psychosocial and self-management outcomes. When assessed, self-report and inadequately validated instruments were used, limiting the ability to draw comparisons and statistical conclusions.
Most reviews were meta-analyses focusing on A1C outcomes, not narratively summarizing interventions in detail. Compared to 2017, this update found that more reviews described “both” basic and advanced TES framework features, possibly reflecting the evolving technology available for interventions. Several studies in our update identified that interventions combining multiple technologies lowered A1C significantly which corresponds to the ADA 2021 SOC recommendation: “systems that combine technology and online coaching can be beneficial in treating prediabetes and diabetes for some individuals.” 10
Different from the 2017 review, we extracted the clinician’s specialty (eg, RN, MD, coach) to understand their role in implementing the technology intervention. However, clinicians were not always reported, and it was not clear which clinicians were conducting the intervention tasks. Overall, intervention details were minimal, making it challenging to understand the active ingredient of the technology. When we applied the TES Taxonomy to the 21 meta-analyses (Supplemental Appendix B), we were able to define a more complete picture of the interventions that significantly lowered A1C; however, there were missing data for several attributes. If original studies and reviews incorporated a taxonomy to describe interventions, data synthesis would be streamlined, and more clarity would exist.
Research Gaps Identified and Future Opportunities
Based on gaps identified, opportunities for future research are suggested (Table 6). Despite the rise in adoption of CGM and integrated apps, and a focus on time-in-range as a metric of diabetes management, current reviews do not include these elements. Mobile health and digital health interventions may be evaluated more often as real-world evidence and not in randomized controlled trials, thus not included in systematic review data.
Coping is the cornerstone for diabetes self-management; 5 however, healthy coping was not evaluated in these studies. In this update, 15% (n = 4) included healthy coping, compared to 24% (n = 6) in the previous review. Although healthy coping was not evaluated, behavioral/psychosocial outcomes were measured and found to often influence healthy coping outcomes. Technology has primarily focused on tracking metabolic measures and not on psychosocial needs. However, technology interventions can leverage the real-time capability of smartphones to capture mood assessment, social determinants of health data, and other information to provide inputs for automated or human coaching.
Technology intervention development and research should be guided by theoretical frameworks, yet they were rarely described. Frameworks typically address behavioral or therapeutic approaches, and they can also guide technology implementation. While the TES framework describes the necessary intervention features to achieve diabetes outcomes, it does not describe the process of implementing technology into a clinic, health system, or community setting. The ADA SOC 2021 indicate that “diabetes technology, when coupled with education and follow-up, can improve the lives and health of PwD; however, the complexity and rapid change of the diabetes technology landscape can also be a barrier to patient and provider implementation.” 10 People with diabetes need HCPs who are knowledgeable about diabetes technologies, especially as diabetes technology use is shifting from specialty to primary care.
Two recent publications provide guidance regarding technology optimization and integration.53,54 The Identify, Configure, Collaborate (ICC) Framework describes a 3-step, simplified, systematic approach to optimize technology-enabled diabetes care and education. This framework can streamline the process of technology implementation and use of PGHD. Additionally, the DATAA Model, presents a simple approach for HCPs and PwD to collaborate and evaluate ambulatory glucose profile data. 54 These publications can support researchers and clinicians in systematically describing their processes to facilitate evaluation and understanding of what works.
Health disparities exist with diabetes technology. Recent data from the T1D Exchange demonstrated that while use of technology has increased over the past 10 years, individuals with low socio-economic status (SES) and non-white racial/ethnic groups have lower technology use and higher A1C levels. 50 Smartphones can increase access to diabetes technologies, and yet diverse populations continue to be underrepresented.49,50 Research has shown that implicit provider bias limits the prescription of technology in lower SES and non-white populations. 49 Lack of trust in research teams, difficulty recruiting, and overt exclusion from studies is problematic. Future studies, when possible, could consider subgroup analysis of underrepresented groups.
Designing technology interventions to address disparities, disabilities, and non-English speaking individuals (inclusive design) could increase inclusion and equity. Developing options for one population (eg, flashing light alerts for Deaf populations) may provide derivative benefits for other populations.48-50 Diabetes technologies should be accessible, affordable, and available to all populations.
Conclusion
Technology-enabled diabetes self-management interventions continue to be associated with improved clinical outcomes. The rapid adoption and engagement with technology requires a focus on uniform measures for psychosocial outcomes, including healthy coping. Using the TES Taxonomy as a standard approach to describe technology-enabled interventions will support further understanding of the impact that technology has on diabetes outcomes and provide a systematic framework for ADCES to frame strategic conversations for technology and practice.
Supplemental Material
Supplemental material, sj-pdf-1-dst-10.1177_19322968211036430 for A New Taxonomy for Technology-Enabled Diabetes Self-Management Interventions: Results of an Umbrella Review by Deborah A. Greenwood, Michelle L. Litchman, Diana Isaacs, Julia E. Blanchette, Jane K. Dickinson, Allyson Hughes, Vanessa D. Colicchio, Jiancheng Ye, Kirsten Yehl, Andrew Todd and Malinda M. Peeples in Journal of Diabetes Science and Technology
Supplemental material, sj-pdf-2-dst-10.1177_19322968211036430 for A New Taxonomy for Technology-Enabled Diabetes Self-Management Interventions: Results of an Umbrella Review by Deborah A. Greenwood, Michelle L. Litchman, Diana Isaacs, Julia E. Blanchette, Jane K. Dickinson, Allyson Hughes, Vanessa D. Colicchio, Jiancheng Ye, Kirsten Yehl, Andrew Todd and Malinda M. Peeples in Journal of Diabetes Science and Technology
Acknowledgments
The authors would like to acknowledge the Association of Diabetes Care & Education Specialists for their support in completing this publication.
Footnotes
Abbreviations: A1c, hemoglobin A1c; AI, artificial intelligence; API, application programing interface; AS, asynchronous; BGM, blood glucose monitoring; BMI, body mass index; BP, blood pressure; CGM, continuous glucose monitoring; GCM, gestational diabetes; D, depression/depressive symptoms; DD, diabetes distress; E, empowerment; Gluc, fasting blood glucose; HCP, healthcare professional; HLD, hyperlipidemia; Hypo, hypoglycemia; I/T, individual/team; M, months; MDI, multiple daily injections; MDIS, mobile diabetes intervention study; PA, physical activity; PGHD, patient generated health data; PS, patient satisfaction; QoL, quality of life; REACH, rapid education/encouragement and communications for health; RCT, randomized clinical trial; RT, real time; SE, self-efficacy; SM, self-management; TES, technology-enabled self-management; T1D, type 1 diabetes; T2D, type 2 diabetes; WC, waist circumference
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Deborah Greenwood is an employee of Dexcom Corporation and faculty for Lifescan Diabetes Institute, consultant for Lifescan, and Silverfern; Digital health advisory board, Novo Nordisk.
Michelle L. Litchman was the PI of an investigator-initiated trial funded by Abbott Diabetes Care unrelated to this study.
Julia E. Blanchette is a consultant for WellDoc, Inc; a consultant/independent contractor for Insulet Corporation and Tandem Diabetes; Advisory Board for Cardinal Health and Provention Bio; Research Support from the Association of Diabetes Care and Education Specialists and the Certification Board for Diabetes Care and Education unrelated to this study.
Jane K. Dickinson has no relevant disclosures.
Allyson S. Hughes has no relevant disclosures.
Jiancheng Ye has no relevant disclosures.
Kirsten Yehl is on staff at the Association of Diabetes Care & Education Specialists.
Andrew Todd has no relevant disclosures
Malinda Peeples is an employee of Welldoc, Inc.
Diana Isaacs serves on the speaker’s bureau for Dexcom, Abbott, Medtronic, Novo Nordisk and a consultant for Lifescan. She has served on Advisory Boards for Medtronic, Lilly, and Prevention Bio.
Vanessa D. Colicchio is a full-time PhD candidate at the University of Utah College of Nursing and has no relevant disclosures.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Association of Diabetes Care & Education Specialists
ORCID iDs: Deborah A. Greenwood  https://orcid.org/0000-0002-7603-4624
https://orcid.org/0000-0002-7603-4624
Michelle L. Litchman  https://orcid.org/0000-0002-8928-5748
https://orcid.org/0000-0002-8928-5748
Julia E. Blanchette  https://orcid.org/0000-0002-6714-4792
https://orcid.org/0000-0002-6714-4792
Jane K. Dickinson  https://orcid.org/0000-0003-0732-8116
https://orcid.org/0000-0003-0732-8116
Allyson Hughes  https://orcid.org/0000-0003-1054-7096
https://orcid.org/0000-0003-1054-7096
Vanessa D. Colicchio  https://orcid.org/0000-0002-4656-2047
https://orcid.org/0000-0002-4656-2047
Jiancheng Ye  https://orcid.org/0000-0003-4143-8423
https://orcid.org/0000-0003-4143-8423
Kirsten Yehl  https://orcid.org/0000-0002-5763-4464
https://orcid.org/0000-0002-5763-4464
Andrew Todd  https://orcid.org/0000-0002-4989-7280
https://orcid.org/0000-0002-4989-7280
Malinda M. Peeples  https://orcid.org/0000-0003-4097-1584
https://orcid.org/0000-0003-4097-1584
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Greenwood DA, Gee PM, Fatkin KJ, Peeples M. A systematic review of reviews evaluating technology-enabled diabetes self-management education and support. J Diabetes Sci Technol. 2017;11(5):1015-1027. doi: 10.1177/1932296817713506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Whittemore R, Siverly L, Wischik DL, Whitehouse CR. An umbrella review of text message programs for adults with type 2 diabetes. Diabetes Educ. 2020;46(6):514-526. doi: 10.1177/0145721720965464 [DOI] [PubMed] [Google Scholar]
- 3. Timpel P, Oswald S, Schwarz PEH, Harst L. Mapping the evidence on the effectiveness of telemedicine interventions in diabetes, dyslipidemia, and hypertension: an umbrella review of systematic reviews and meta-analyses. J Med Internet Res. 2020;22(3):e16791. doi: 10.2196/16791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Levine BJ, Close KL, Gabbay RA., Reviewing U.S. connected diabetes care: the newest member of the team. Diabetes Technol Ther. 2020;22:1-9. doi: 10.1089/dia.2019.0273 [DOI] [PubMed] [Google Scholar]
- 5. Association of Diabetes Care and Education Specialists, Association of Diabetes Care, Association of Diabetes Care, Kolb L. An effective model of diabetes care and education: the ADCES7 self-care behaviors™. Sci Diabetes Self Manag Care. 2021;47(1):30-53. doi: 10.1177/0145721720978154 [DOI] [PubMed] [Google Scholar]
- 6. Scalzo P. From the Association of Diabetes Care & Education Specialists: the role of the diabetes care and education specialist as a champion of technology integration. Sci Diabetes Self Manag Care. 2021;47(2):120-123. doi: 10.1177/0145721721995478 [DOI] [PubMed] [Google Scholar]
- 7. Ross J, Stevenson F, Dack C, et al. Developing an implementation strategy for a digital health intervention: an example in routine healthcare. BMC Health Serv Res. 2018;18(1):794. doi: 10.1186/s12913-018-3615-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang Y, Fadhil A, Lange J-P, Reiterer H. Integrating taxonomies into theory-based digital health interventions for behavior change: a holistic framework. JMIR Res Protoc. 2019;8(1):e8055. doi: 10.2196/resprot.8055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Beck J, Greenwood DA, Blanton L, et al. 2017 National standards for diabetes self-management education and support. Diabetes Educ. 2017;43(5):449-464. doi: 10.1177/0145721717722968 [DOI] [PubMed] [Google Scholar]
- 10. American Diabetes Association. 7. Diabetes technology: standards of medical care in diabetes-2021. Diabetes Care. 2021;44(suppl 1):S85-S99. doi: 10.2337/dc21-S007 [DOI] [PubMed] [Google Scholar]
- 11. Nathan J, Vider E. The package insert. US Pharm. 2015;40(5):8-10. [Google Scholar]
- 12. Quinn CC, Butler EC, Swasey KK, et al. Mobile diabetes intervention study of patient engagement and impact on blood glucose: mixed methods analysis. JMIR Mhealth Uhealth. 2018;6(2):e31. doi: 10.2196/mhealth.9265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nelson LA, Greevy RA, Spieker A, et al. Effects of a tailored text messaging intervention among diverse adults with type 2 diabetes: evidence from the 15-month REACH randomized controlled trial. Diabetes Care. 2021;44(1):26-34. doi: 10.2337/dc20-0961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pratley RE, Kanapka LG, Rickels MR, et al. Effect of continuous glucose monitoring on hypoglycemia in older adults with type 1 Diabetes: a randomized clinical trial. JAMA. 2020;323(23):2397. doi: 10.1001/jama.2020.6928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shea BJ, Reeves BC, Wells G, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017. Published online September 21, 2017. doi: 10.1136/bmj.j4008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Schardt C, Adams MB, Owens T, Keitz S, Fontelo P. Utilization of the PICO framework to improve searching PubMed for clinical questions. BMC Med Inform Decis Mak. 2007;7(1):16. doi: 10.1186/1472-6947-7-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. FARSEEING project. Taxonomy of technologies. 2014; Accessed April 1, 2021. http://farseeingresearch.eu/wp-content/uploads/2014/07/FARSEEING-Taxonomy-of-Technologies-V4.pdf
- 19. Aminuddin HB, Jiao N, Jiang Y, Hong J, Wang W. Effectiveness of smartphone-based self-management interventions on self-efficacy, self-care activities, health-related quality of life and clinical outcomes in patients with type 2 diabetes: a systematic review and meta-analysis. Int J Nurs Stud. 2021;116:103286. doi: 10.1016/j.ijnurstu.2019.02.003 [DOI] [PubMed] [Google Scholar]
- 20. Cai X, Qiu S, Luo D, Wang L, Lu Y, Li M. Mobile application interventions and weight loss in type 2 diabetes: a meta-analysis. Obesity. 2020;28(3):502-509. doi: 10.1002/oby.22715 [DOI] [PubMed] [Google Scholar]
- 21. Faruque LI, Wiebe N, Ehteshami-Afshar A, et al. Effect of telemedicine on glycated hemoglobin in diabetes: a systematic review and meta-analysis of randomized trials. Can Med Assoc J. 2017;189(9):E341-E364. doi: 10.1503/cmaj.150885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Feigerlová E, Oussalah A, Zuily S, et al. E-health education interventions on HbA1c in patients with type 1 diabetes on intensive insulin therapy: a systematic review and meta-analysis of randomized controlled trials. Diabetes Metab Res Rev. 2020;36(6):e3313. doi: 10.1002/dmrr.3313 [DOI] [PubMed] [Google Scholar]
- 23. Haider R, Sudini L, Chow CK, Cheung NW. Mobile phone text messaging in improving glycaemic control for patients with type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Res Clin Pract. 2019;150:27-37. doi: 10.1016/j.diabres.2019.02.022 [DOI] [PubMed] [Google Scholar]
- 24. Heitkemper EM, Mamykina L, Travers J, Smaldone A. Do health information technology self-management interventions improve glycemic control in medically underserved adults with diabetes? A systematic review and meta-analysis. J Am Med Inform Assoc. 2017;24(5):1024-1035. doi: 10.1093/jamia/ocx025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hu Y, Wen X, Wang F, et al. Effect of telemedicine intervention on hypoglycaemia in diabetes patients: a systematic review and meta-analysis of randomised controlled trials. J Telemed Telecare. 2019;25(7):402-413. doi: 10.1177/1357633X18776823 [DOI] [PubMed] [Google Scholar]
- 26. Huang L, Yan Z, Huang H. The effect of short message service intervention on glycemic control in diabetes: a systematic review and meta-analysis. Postgrad Med. 2019;131(8):566-571. doi: 10.1080/00325481.2019.1668723 [DOI] [PubMed] [Google Scholar]
- 27. Kirk MA, Amiri M, Pirbaglou M, Ritvo P. Wearable technology and physical activity behavior change in adults with chronic cardiometabolic disease: a systematic review and meta-analysis. Am J Health Promot. 2019;33(5):778-791. doi: 10.1177/0890117118816278 [DOI] [PubMed] [Google Scholar]
- 28. Kongstad MB, Valentiner LS, Ried-Larsen M, Walker KC, Juhl CB, Langberg H. Effectiveness of remote feedback on physical activity in persons with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. J Telemed Telecare. 2019;25(1):26-34. doi: 10.1177/1357633X17733772 [DOI] [PubMed] [Google Scholar]
- 29. Kuo C-C, Su YJ, Lin C-C. A systematic review and meta-analysis: effectiveness of internet empowerment-based self-management interventions on adults with metabolic diseases. J Adv Nurs. 2018;74(8):1787-1802. doi: 10.1111/jan.13574 [DOI] [PubMed] [Google Scholar]
- 30. Lee SWH, Ooi L, Lai YK. telemedicine for the management of glycemic control and clinical outcomes of type 1 diabetes mellitus: a systematic review and meta-analysis of randomized controlled studies. Front Pharmacol. 2017;8:330. doi: 10.3389/fphar.2017.00330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Liu K, Xie Z, Or CK. Effectiveness of mobile app-assisted self-care interventions for improving patient outcomes in type 2 diabetes and/or hypertension: systematic review and meta-analysis of randomized controlled trials. JMIR Mhealth Uhealth. 2020;8(8):e15779. doi: 10.2196/15779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Michaud TL, Ern J, Scoggins D, Su D. Assessing the impact of telemonitoring-facilitated lifestyle modifications on Diabetes outcomes: a systematic review and meta-analysis. Telemed E-Health. 2021;27(2):124-136. doi: 10.1089/tmj.2019.0319 [DOI] [PubMed] [Google Scholar]
- 33. Shen Y, Wang F, Zhang X, et al. Effectiveness of internet-based interventions on glycemic control in patients with type 2 diabetes: meta-analysis of randomized controlled trials. J Med Internet Res. 2018;20(5):e172. doi: 10.2196/jmir.9133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. So CF, Chung JW. Telehealth for diabetes self-management in primary healthcare: a systematic review and meta-analysis. J Telemed Telecare. 2018;24(5):356-364. doi: 10.1177/1357633X17700552 [DOI] [PubMed] [Google Scholar]
- 35. Tao D, Wang T, Wang T, Liu S, Qu X. Effects of consumer-oriented health information technologies in diabetes management over time: a systematic review and meta-analysis of randomized controlled trials. J Am Med Inform Assoc. 2017;24(5):1014-1023. doi: 10.1093/jamia/ocx014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Tchero H, Kangambega P, Briatte C, Brunet-Houdard S, Retali G-R, Rusch E. Clinical effectiveness of telemedicine in Diabetes Mellitus: a meta-analysis of 42 randomized controlled trials. Telemed E-Health. 2019;25(7):569-583. doi: 10.1089/tmj.2018.0128 [DOI] [PubMed] [Google Scholar]
- 37. Wang X, Shu W, Du J, et al. Mobile health in the management of type 1 diabetes: a systematic review and meta-analysis. BMC Endocr Disord. 2019;19(1):21. doi: 10.1186/s12902-019-0347-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wei J, Zheng H, Wang L, Wang Q, Wei F, Bai L. Effects of telephone call intervention on cardiovascular risk factors in T2DM: a meta-analysis. J Telemed Telecare. 2019;25(2):93-105. doi: 10.1177/1357633X17745456 [DOI] [PubMed] [Google Scholar]
- 39. Wu IXY, Kee JCY, Threapleton DE, et al. Effectiveness of smartphone technologies on glycaemic control in patients with type 2 diabetes: systematic review with meta-analysis of 17 trials. Obes Rev. 2018;19(6):825-838. doi: 10.1111/obr.12669 [DOI] [PubMed] [Google Scholar]
- 40. Wu C, Wu Z, Yang L, et al. Evaluation of the clinical outcomes of telehealth for managing diabetes: a PRISMA-compliant meta-analysis. Medicine. 2018;97(43):e12962. doi: 10.1097/MD.0000000000012962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wu X, Guo X, Zhang Z. The efficacy of mobile phone apps for lifestyle modification in diabetes: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2019;7(1):e12297. doi: 10.2196/12297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Wu Y, Yao X, Vespasiani G, et al. Mobile app-based interventions to support diabetes self-management: a systematic review of randomized controlled trials to identify functions associated with glycemic efficacy. JMIR Mhealth Uhealth. 2017;5(3):e35. doi: 10.2196/mhealth.6522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Yang S, Jiang Q, Li H. The role of telenursing in the management of diabetes: a systematic review and meta-analysis. Public Health Nurs. 2019; 36(4):575-586. doi: 10.1111/phn.12603 [DOI] [PubMed] [Google Scholar]
- 44. Yoshida Y, Boren SA, Soares J, et al. Effect of health information technologies on cardiovascular risk factors among patients with diabetes. Curr Diab Rep. 2019;19(6):28. doi: 10.1007/s11892-019-1152-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Litchman ML, Walker HR, Ng AH, et al. State of the science: a scoping review and gap analysis of diabetes online communities. J Diabetes Sci Technol. 2019;13(3):466-492. doi: 10.1177/1932296819831042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Litchman ML, Oser TK, Hodgson L, et al. In-person and technology-mediated peer support in diabetes care: a systematic review of reviews and gap analysis. Diabetes Educ. 2020;46(3):230-241. doi: 10.1177/0145721720913275 [DOI] [PubMed] [Google Scholar]
- 47. Young-Hyman D, de Groot M, Hill-Briggs F, Gonzalez JS, Hood K, Peyrot M. Psychosocial care for people with diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2016;39(12):2126-2140. doi: 10.2337/dc16-2053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Clarkson J. (200). Inclusive design design for the whole population. In: 15th International Conference on Design Theory and Methodology, 3, Vol. 3b. https://www.springer.com/gp/book/9781852337001 [Google Scholar]
- 49. Agarwal S, Schechter C, Gonzalez J, Long JA. Racial-ethnic disparities in diabetes technology use among young adults with type 1 diabetes. Diabetes Technol Ther. 2021;23(4):306-313. doi: 10.1089/dia.2020.0338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Miller KM, Beck RW, Foster NC, Maahs DM; for the T1D Exchange. HbA1c levels in type 1 diabetes from early childhood to older adults: a deeper dive into the influence of technology and socioeconomic status on HbA1c in the T1D exchange clinic registry findings. Diabetes Technol Ther. 2020;22(9):645-650. doi: 10.1089/dia.2019.0393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kaufman N. Digital therapeutics: leading the way to improved outcomes for people with diabetes. Diabetes Spectr. 2019;32(4):301-303. doi: 10.2337/ds19-0012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. O’Cathain A, Croot L, Sworn K, et al. Taxonomy of approaches to developing interventions to improve health: a systematic methods overview. Pilot Feasibility Stud. 2019;5(1):41. doi: 10.1186/s40814-019-0425-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Greenwood DA, Howell F, Scher L, et al. A framework for optimizing technology-enabled diabetes and cardiometabolic care and education: the role of the diabetes care and education specialist. Diabetes Educ. 2020;46(4):315-322. doi: 10.1177/0145721720935125 [DOI] [PubMed] [Google Scholar]
- 54. Isaacs D, Cox C, Schwab K, et al. Technology integration: the role of the diabetes care and education specialist in practice. Diabetes Educ. 2020;46(4):323-334. doi: 10.1177/0145721720935123 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-dst-10.1177_19322968211036430 for A New Taxonomy for Technology-Enabled Diabetes Self-Management Interventions: Results of an Umbrella Review by Deborah A. Greenwood, Michelle L. Litchman, Diana Isaacs, Julia E. Blanchette, Jane K. Dickinson, Allyson Hughes, Vanessa D. Colicchio, Jiancheng Ye, Kirsten Yehl, Andrew Todd and Malinda M. Peeples in Journal of Diabetes Science and Technology
Supplemental material, sj-pdf-2-dst-10.1177_19322968211036430 for A New Taxonomy for Technology-Enabled Diabetes Self-Management Interventions: Results of an Umbrella Review by Deborah A. Greenwood, Michelle L. Litchman, Diana Isaacs, Julia E. Blanchette, Jane K. Dickinson, Allyson Hughes, Vanessa D. Colicchio, Jiancheng Ye, Kirsten Yehl, Andrew Todd and Malinda M. Peeples in Journal of Diabetes Science and Technology