Abstract
Arsenic is widely present in nature and is a common environmental poison that seriously damages human health. Chronic exposure to arsenic is a major environmental poisoning factor that promotes cell proliferation and leads to malignant transformation. However, its molecular mechanism remains unclear. In this study, we found that arsenite can promote the transformation of immortalized human keratinocyte cells (HaCaT) from the G0/G1 phase to S phase and demonstrated malignant phenotypes. This phenomenon is accompanied by obviously elevated levels of NRF2, NQO1, Cyclin E, and Cyclin-dependent kinase 2 (CDK2). Silencing the NRF2 expression with small interfering RNA (siRNA) in arsenite-transformed (T-HaCaT) cells was shown to reverse the malignant phenotype. Furthermore, the siRNA silencing of NQO1 significantly decreased the levels of the cyclin E-CDK2 complex, inhibiting the G0/G1 to S phase cell cycle progression and transformation to the T-HaCaT phenotypes. Thus, we hypothesized that the NRF2/NQO1 pathway played a key role in the arsenite-induced malignancy of HaCaT cells. By increasing the expression of Cyclin E-CDK2, the NRF2/NQO1 pathway can affect cell cycle progression and cell proliferation. A new common health effect mechanism of arsenic carcinogenesis has been identified; thus, it would contribute to the development of novel treatments to prevent and treat skin cancer caused by arsenic.
Keywords: arsenite pollution, health effect, squamous cell carcinoma, NRF2/NQO1 pathway, cell proliferation, malignant transformation
1. Introduction
As the twentieth element of the Earth’s crust, arsenic is most commonly found in the form of sulfides in nature. Arsenic is released into the environment from natural sources as a result of natural phenomena, such as dust storms, volcanic eruptions, geothermal/hydrothermal activity, and forest fires [1]. Arsenic can interact with oxygen and other molecules of nature to form different compounds. Therefore, it is extremely commonplace in the daily life of humans [2]. Arsenic is widely used in the manufacture of industrial and agricultural products such as semiconductors, glassware, alloys, wood preservatives, and pesticides and in medical treatments for diseases such as syphilis, rickets, amoebic dysentery, and leukemia [3,4]. These human activities also have the potential to cause severe arsenic pollution in the environment. Arsenic contamination of drinking water and soil has become an international and regional problem over the past two decades. A survey of arsenic concentrations in groundwater in eastern Wisconsin, United States, found naturally occurring arsenic concentrations in groundwater of more than 12,000 μg/L, which is much higher than the U.S. Environmental Protection Agency (EPA) and WHO standard/baseline concentrations for arsenic in drinking water [5]. In other countries and regions, such as Argentina, Bangladesh, Chile, China, Mexico, India, Thailand, and Taiwan, the health effects of arsenic contamination in groundwater have become one of the major public health problems [3,6].
Arsenic is a common environmental toxin with toxic and teratogenic effects in many metazoans [7,8,9]. As water is the primary polluting medium for arsenic, aquatic organisms bear the brunt of arsenic [10,11,12]. In addition, humans have the highest risk of arsenic contamination due to the food chain. It is estimated that nearly hundreds of millions of people are exposed to the threat of arsenic compounds in drinking water and food worldwide [13,14,15]. The main source of human arsenic intake comes from water and food, with an average daily intake of approximately 50 μg [3]. The human arsenic intake from air, water, and soil is usually much smaller. However, these environmental media also deserve particular attention in areas contaminated with arsenic. In certain workplaces where arsenic compounds are produced and used, workers may be exposed to greater concentrations of arsenic than in the natural environment [16,17,18]. Thus, arsenic exposure is considered the leading cause of global health problems today. In the Indian subcontinent, for instance, exposure to arsenic and having related diseases have reached alarming levels, where nearly 359 million people may be at risk [19]. Long-term exposure to arsenic can lead to a number of adverse health effects, including hyperkeratosis, jaundice, and vascular diseases [20]. However, the carcinogenic role of arsenic has brought more significant concerns in recent years, as arsenic-related cancers can be diagnosed in the skin, lungs, liver, and other malignant tumors [21,22,23,24]. Arsenic is now classified as a Group A carcinogen by the EPA and a Group I carcinogen by the International Agency for Research on Cancer (IARC). Among the cancers caused by arsenic, skin cancer was the first one that has been confirmed. As early as the late 1880s, White et al. reported one case of skin cancer caused by psoriasis treated with potassium arsenite [25]. Currently, skin cancer is commonly referred to as skin melanoma (MC) and non-melanoma skin cancer (NMSC), the latter being composed of basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) [26]. Numerous epidemiological studies have shown that apart from ultraviolet (UV) radiation, arsenic is the most significant chemical damage factor related to SCC and BCC [27,28,29,30]. Unfortunately, the mechanics of arsenic-induced skin cancer are unclear, making treatment and control extremely difficult.
In most cases, the final outcome of cellular differentiation is antiproliferative and constitutes a barrier to the continued proliferation required for tumorigenesis. Therefore, the hallmarks and characteristics of cancer currently include the acquired capabilities for sustaining proliferative signaling, evading growth suppressors, resisting cell death, and enabling replicative immortality [31]. As the mechanisms of cell proliferation, malignant transformation, and carcinogenesis are complex, the Nrf2/NQO1 pathway is considered one of them. Nuclear erythroid factor 2 p45 (NRF2) is of primary importance in the alteration of cell homeostasis to respond in an adaptive manner to xenobiotic and oxidative stress [32]. The accumulation of studies has shown that NRF2 plays a significant role in cell proliferation, except for the regulation of intracellular redox homeostasis [33,34]. NRF2 has long been considered a cancer inhibitor, providing the rationale for cancer prevention strategies using NRF2 activators [35]. However, increased NRF2 activity has recently been observed in a wide range of cancers [36]. This deregulated Nrf2 condition provides several growth advantages to cancer cells [35]. Therefore, NRF2 has attracted great interest for its use in cancer therapy and diagnosis. NAD(P)H: quinine oxidoreductase 1 (NQO1) is one of the target genes regulated by the transcription factor NRF2 [37,38]. The function of NQO1 is widely regarded as a “cytoprotective agent” that protects cells from oxidative damage by inducing responses to various noxious stimuli [39,40]. As with NRF2, the accumulation of studies confirmed the high expression of the NQO1 gene in solid tumor tissue in recent years [41,42,43]. The upregulation of NQO1 may contribute to the growth of cancer cells, especially in oxidative stress environments [44,45,46]. Furthermore, the negative expression of NRF2 and NQO1 provides a better prognosis for patients with non-small cell lung cancer (NSCLC) [47]. In fact, we have reported that the long-term exposure to arsenite induced NRF2 accumulation and enhanced proliferation in human bronchial epithelial cells (HBE) [48] and immortalized human keratinocyte cells (HaCaT) [44], and we have found that the upregulation of NRF2/NQO1 caused the proliferation and transformation of arsenite-induced HBE cells by increasing cyclin E-CDK2 and then affecting the cell cycle [48]. It is suggested that a novel mechanistic pathway for arsenite carcinogenesis, the NRF2/NQO1 pathway, is involved in the dislocation of cell cycle progression in arsenite-induced malignancies. Nevertheless, this mechanism has not been confirmed in the study of arsenic-induced skin cancer.
In this study, we aimed to elucidate the mechanism of the NRF2/NQO1 pathway in mediating arsenite-induced malignant phenomena in HaCaT cells. To achieve our study objective, we analyzed the mechanism of dynamic changes in cell proliferation, NRF2, NQO1, cell cycle-related proteins, and cyclin-dependent kinases with arsenic-induced neoplastic transformation in HaCaT cells. In addition, we examined the actions of NRF2/NQO1 in arsenite-transformed HaCaT cells (T-HaCaT). We hope this study will lead to a greater understanding of arsenite skin toxicity, which may provide more possibilities for clinical applications for SCC.
2. Materials and Methods
2.1. Cell Culture and Exposure to Arsenic
HaCaT cells were developed by Boukamp et al. as a line of spontaneously immortalized human epithelial cells. They are immortal, nontumorigenic, and retain most of the characteristics of normal human keratinocytes (NHKs). HaCaT cells offer a suitable and stable model for keratinization studies. Moreover, this line could be reproducibly transfected with the activated human Ha-ras oncogene. Selected clones gave rise to highly differentiated benign epidermal cysts and/or squamous cell carcinomas in nude mice [49]. Thus, the HaCaT cell line is ideal for SCC studies. In this study, HaCaT cells were generously supplied by Prof M.Y (Dalian Medical University, Dalian, China). The cells were incubated at 37 °C in a humidified 5% atmosphere in Dulbecco’s modified Eagle’s medium (DMEM; Life Technologies/Gibco, Grand Island, NY, USA) with 10% fetal bovine serum (FBS; Hyclone, Thermo Scientific, Waltham, MA, USA), 100 U penicillin/mL, and 100 µg of streptomycin/mL. To create cellular patterns for the chronic arsenic exposure model with final concentrations of DMEM with 0.0 (control) or 1.0 µM sodium arsenite (NaAsO2; Merck Drugs & Biotechnology, Darmstadt, Germany, purity 99.0%), HaCaT cells were cultured for 35 passages (approximately 18 weeks). The experimental control cells were HaCaT cells exposed to 0.0 μM NaAsO2 for passage 0, while the transient matched control cells were exposed to 0.0 μM NaAsO2 at other times. T-HaCaT cells were defined as 35-passage HaCaT cells exposed to arsenite based on our previous study [44]. Analytical and quality-assured reagents were used in all experiments.
2.2. Proliferation of Cells Assay
To determine whether exposure to 0.0 or 1.0 μM NaAsO2 at various passages (0, 1, 7, 14, 21, 28, and 35 passages) of HaCaT cells would induce transformation, cellular proliferation changes were measured. As instructed by the manufacturer, the cell proliferation assay was measured by a 3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl-2-H tetrazolium bromide (MTT) kit. In brief, before 10 μL of MTT labeling reagent was added, 50,000 cells/mL were washed with phosphate-buffered saline (PBS), seeded onto 96-well plates, and incubated at 37 °C with 5% CO2 for 24 h. Afterward, 100 μL of solubilization solution was added 4 h later. Finally, a microplate scanner was used to measure blue formazan from viable cells at 570 nm in accordance with the manufacturer’s protocol. The experiment was repeated three times.
2.3. Flow Cytometry Analysis of the Cell Cycle
The cell cycle was detected by the cell cycle test kit. As per the manufacturer’s instructions, synchronizing the cells before exposure required 48 h of culture in DMEM with 0.5% FBS. After continuous exposure to arsenite over a period of time, HaCaT cells were harvested at different passages, collected with 0.25% trypsin without EDTA, and washed twice with 4 °C pre-cooled PBS. The cells were left at −20 °C overnight with the addition of 1 mL of 70% pre-cooled ethanol. After two rounds of washing in cold PBS, the cells were stained for 30 min with 20 μg/mL of PI (Beyotime Institute of Biotechnology, Haimen, China) and 200 μg/mL of ribonuclease A (RNaseA, Beyotime Institute of Biotechnology, Haimen, China) diluted in PBS. Following the above processing, the data were analyzed using cell cycle analysis software based on flow cytometry (Beckman Coulter FC500, Brea, CA, USA) for detection. The experiment was repeated three times.
2.4. Western Blots
The experimental process was as follows: After three washes with ice-cold PBS and centrifugation at 16,000× g for 10 min at 4 °C, whole cell extracts were obtained using a cell lysis buffer for Western blot and Immunol precipitation (IP) (Beyotime Institute of Biotechnology, Haimen, China) with 1.0% phenylmethanesulfonyl fluoride (PMSF; Beyotime Institute of Biotechnology, Haimen, China), and the protein fractions were quantified using a BCA Protein Assay Kit (Beyotime). Protein lysates were subjected to sodium polyacrylamide dodecyl sulphate gel electrophoresis (SDS-PAGE) and transferred to polyvinylidene difluoride membranes (Millipore, Bedford, MA, USA) in equal amounts. The membranes were blocked with 5% skim milk (Yili Industrial Group Limited by Share Ltd., Hohhot, China) for 1 h and then incubated with the appropriate primary antibodies overnight at 4 °C. The following primary antibodies were used in this research: NRF2 (sc-13032) (dilution 1:500), NQO1 (sc-32793) (dilution 1:500), and CDK2 (sc-6248) (dilution 1:500) were purchased from Santa Cruz Biotech (Santa Cruz, CA, USA); Cyclin E (WL01072) (WB 1:750) and Cyclin D1 (WL01435a) (WB 1:750) were acquired from Wanlei Organic Company (Shenyang, China); Cycline A (RLT1167) (dilution 1:500) was acquired from Suzhou Ruiying Organic Company. The loading control was GAPDH (Beyotime Institute of Biotechnology, Haimen, China) (dilution 1:1000) or β-actin (sc-47778) (dilution 1:500) (Santa Cruz, CA, USA). Following three washes in TBST (Tween 20 Tris-buffered saline) saline solution, membranes were incubated with secondary antibodies conjugated with equine radish peroxidase (Beyotime). An improved chemiluminescence kit (Millipore, Bedford, MA, USA) and G: BOX Chemi XRQ (Syngene, Cambridge, UK) were used for the detection of immunoreactive proteins. To correct for changes in protein load between the different test groups, densitometry was used to quantify the plots and standardize them with GAPDH or β-actin. The results obtained relate to three autonomous experiments.
2.5. SiRNA Interference Assays
According to the manufacturer’s protocol, NRF2 siRNA transfection and NQO1 siRNA transfection were performed on the 35 passages (T-HaCaT) cells exposed to 1.0 μM arsenite to silence the NRF2 and NQO1 genes to further understand the roles of NRF2/NQO1 in our research. First, 2 × 105 cells were seeded in 2 mL of antibiotic-free DMEM containing FBS and then added to each well of a 6-well plate 24 h before transfection. Next, the biphasic siRNA solution (solution A) and diluted transfection reagent (solution B) (sc-29528, Santa Cruz Biotechnology) were mixed with siRNA transfection medium (sc-36868, Santa Cruz Biotechnology) prior to siRNA in preparing a mix of transfection reagents. The above mixtures were incubated at room temperature for 15–45 min and then added to the cells and stirred evenly. The cells were incubated in a 37 °C 5% CO2 incubator for 5–7 h, and then 1 mL of DMEM containing 20% fetal bovine serum and 2% antibiotics was added without removing the transfection mixture. After incubation for 18–24 h, the cells were collected for analysis. Control siRNA, NRF2 siRNA, and NQO1 siRNA were purchased from Santa Cruz Biotechnology (Santa Cruz, CA, USA). HaCaT cells (passage 35), not exposed to arsenite, served as a negative control.
2.6. Wound-Healing (Cell Migration) Assay
The wound-healing assay is a method for studying the role of various experimental conditions in cellular migration and proliferation. It is simple and cost-effective and is one of the earliest methods to be used for targeted in vitro cell migration studies. To determine cell migration, wound healing experiments were conducted. The objective of the wound-healing test was to analyze the impact of NRF2 and NQO1 inhibition on cell migration. In short, HaCaT and T-HaCaT cells with or without NRF2 siRNA and NQO1 siRNA transfection were seeded in 6 cm dishes to form confluent monolayers. The cell monolayer was wounded using a 200 μL pipette tip and washed twice with PBS. Then, the wound width (0 h and the subsequent 24 h incubation period were photographed immediately after scratching. The tests were conducted in three petri dishes in triplicate, and the results are expressed as the relative scratch width based on the distance migrated relative to the original scratched distance. Cell migration rate = (the width of the wound at 0 h-the width of the wound at 48 h)/the width of the wound at 48 h.
2.7. Anchor-Independent Growth Experiment
Normal cell proliferation requires the costimulation of growth factor signaling and cell adhesion, but an important feature of phenotypically transformed cells is anchor-independent growth. To determine the growth of cells independent of the anchor, a soft agar cloning assay was used. Sweet AGAR plates were prepared with 0.70% agarose underlay in DMEM supplemented with 10% FBS in a 35 mm (diameter) container. To observe the growth capacity of colonies on soft AGAR, cells were cultivated in three copies at a density of 5 × 103 in 2 mL of 0.35% agarose overlaid with 0.70% agarose in the same medium. Cells were incubated at 37 °C in a humidified atmosphere at 5% with a routing replenished of medium every three days. After 3 weeks, colonies of more than 30 cells were examined under a microscope and photographed under a dissective microscope.
2.8. Statistical Analysis
Data analysis was performed using SPSS software (version 20.0, SPSS Inc., Chicago, IL, USA). All experimental data were tested for homoscedasticity, and differences between groups were assessed using one-way analysis of variance (ANOVA). Pairwise comparisons of sample means with uniform variance were performed by ANOVA using the SNK test and Tamhane’s T2 test for nonuniform variance. The test results were statistically significant at p < 0.05. Data from the triplicate experiments reported as the mean ± standard deviation (SD) were analyzed.
3. Results
3.1. Malignant Phenotypes Were Induced in HaCaT Cells with Continuous Arsenic Exposure
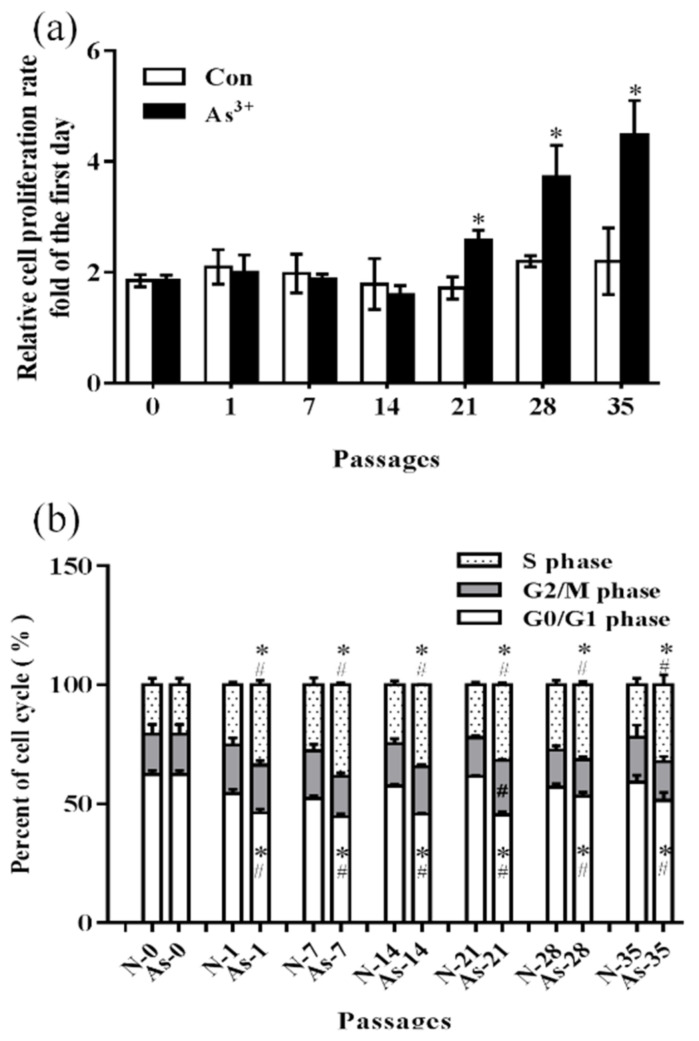
To drive cells toward a malignant phenotype, normal HaCaT cells were exposed to 0.0 or 1.0 μM NaAsO2 for 18 weeks (35 passes). As a result, the proliferation rate in the treatment group (1.0 μM NaAsO2) was significantly higher at passages 21, 28, and 35 than that in the passage-matched control group (0.0 μM NaAsO2) and showed a trend of increasing passage by passage (p < 0.05) (Figure 1a). Furthermore, the ratio of G1 phase cells was significantly decreased, and the ratio of the S phase was significantly increased in the treatment group from passage 1 to 35 (p < 0.05) (Figure 1b), which indicated that arsenite can promote the transformation of HaCaT cells from the G0/G1 phase to S phase. The data demonstrated malignant phenotypes (T-HaCaT) in cells processed by NaAsO2.
Figure 1.
Changes in cell proliferation and cell cycle in HaCaT cells exposed to 1.0 μM arsenite or without arsenite exposure for different passages. (a) Change in the cell proliferation rate in HaCaT cells. (b) Change in the cell cycle in HaCaT cells. Error bars are the mean ± SD (n = 3). * Compared with the passage-matched control group, p < 0.05; # Compared with the experimental control group, p < 0.05.
3.2. Decreased Cell Cycle-Related Proteins and NRF2 and NQO1 in HaCaT Cells Exposed to Arsenite
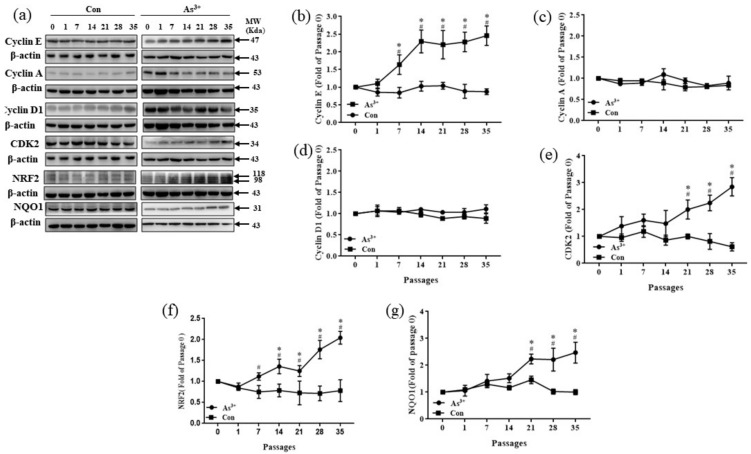
Cyclin proteins, including A, B, D, E, G, and H, collaborate with their cyclin-dependent kinases. They act as the nucleus of the cell cycle process [50]. Cyclin and cyclin kinases were measured in HaCaT cells as indicators to assess changes in the cell cycle in arsenite-induced malignant transformation in this study. Compared with the passage-matched control groups, Cyclin E was significantly increased after passage 7 and showed an upward trend after continuous exposure to 1.0 μM NaAsO2 (p < 0.05) (Figure 2b–d). Moreover, the protein expression of cyclin-dependent kinase CDK2 showed a significant increase after 21 passages in HaCaT cells and increased with each passage; however, similar changes were not observed in the control groups (p < 0.05) (Figure 2e). No significant differences were observed between the other cyclin and the cyclin-dependent kinases with the control groups. These results suggest that arsenite-exposed cell proliferation promotes the progression of the cell cycle from the G0/G1 phase to S phase through an increase in cyclin E-CDK2, thereby causing the malignant transformation of HaCaT. Changes in NRF2 and NQO1 were also measured. During the 1.0 μM NaAsO2-induced malignant transformation in HaCaT cells, the elevated expression levels of NRF2 and NQO1 increased. As shown in Figure 2f,g, compared to the control groups, the protein level of NRF2 expression increased significantly after seven passages and displayed an upward trend. As a target of NRF2, the protein expression of NQO1 was upregulated after passage 21 (p < 0.05). These results indicate that the protein level of NRF2 and its target gene NQO1 were increased by arsenite exposure.
Figure 2.
Relative protein expression and quantification of changes in NRF2, NQO1, and cell cycle-related proteins in HaCaT cells exposed to 1.0 μM arsenite or without arsenite exposure for different passages. (a) Protein bands. (b) Relative protein levels of Cyclin E. (c) Relative protein levels of Cyclin A. (d) Relative protein levels of Cyclin D1. (e) Relative protein levels of CDK2. (f) Relative protein levels of NRF2. (g) Relative protein levels of NQO1. Error bars are the mean ± SD (n = 3). * Compared with the passage-matched control group, p < 0.05; # Compared with the experimental control group, p < 0.05.
3.3. NRF2-Mediated Cellular Proliferation in Arsenite-Exposed HaCaT Cells
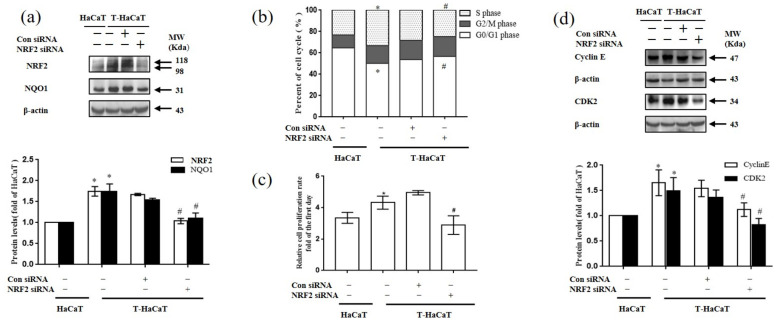
Considering that the levels of NRF2 and NQO1 proteins in T-HaCaT cells were higher than those in the control, to understand more about the role in the arsenite-induced malignant transformation of HaCaT cells, NRF2 was silenced by NRF2 siRNA in arsenite-transformed T-HaCaT cells. After T-HaCaT cells were transfected with NRF2 siRNA, the protein levels of NRF2 and NQO1 were significantly decreased in T-HaCaT cells compared with the con-siRNA transfected group (T-HaCaT (−)) (p < 0.05, Figure 3a). In addition, compared to the T-HaCaT (−) cells, the G0/G1 phase of the cells increased, whereas the S phase decreased after the T-HaCaT cells were transformed by NRF2 siRNA (Figure 3b). It is suggested that silencing NRF2 resulted in cell cycle stoppage. Levels of cyclic E-CDK2 proteins were reduced in transfected T-HaCaT cells compared to T-HaCaT (−) cells (p < 0.05, Figure 3d). Meanwhile, NRF2 silencing blocked the proliferation of T-HaCaT cells (p < 0.05, Figure 3c).
Figure 3.
Effects of NRF2 on arsenite-induced malignant transformation of HaCaT cells. (a) Protein bands and relative protein levels of NRF2 and NQO1 in HaCaT cells and T-HaCaT cells with or without NRF2 siRNA transfection. (b) Changes in the cell cycle. (c) Change in the cell proliferation rate. (d) Protein bands and relative protein levels of the cell-cycle-related proteins Cyclin E and CDK2. Error bars are the mean ± SD (n = 3). * Compared with HaCaT cells, p < 0.05; # Compared with control siRNA cells, p < 0.05.
More importantly, silencing NRF2 activity inhibited HaCaT cell migration, as detected by the wound-healing assay (p < 0.05, Figure 4a), and the anchorage-independent growth capacity was suppressed, as detected by colony formation in soft agar (p < 0.05, Figure 4b), which suggests that the malignant phenotype in HaCaT cells was relieved. These results demonstrated that NRF2 deficiency blocked the proliferation of T-HaCaT cells by blocking the change in the cell cycle, which suggested that NRF2 is a key factor in mediating cellular proliferation in arsenite-exposed HaCaT cells.
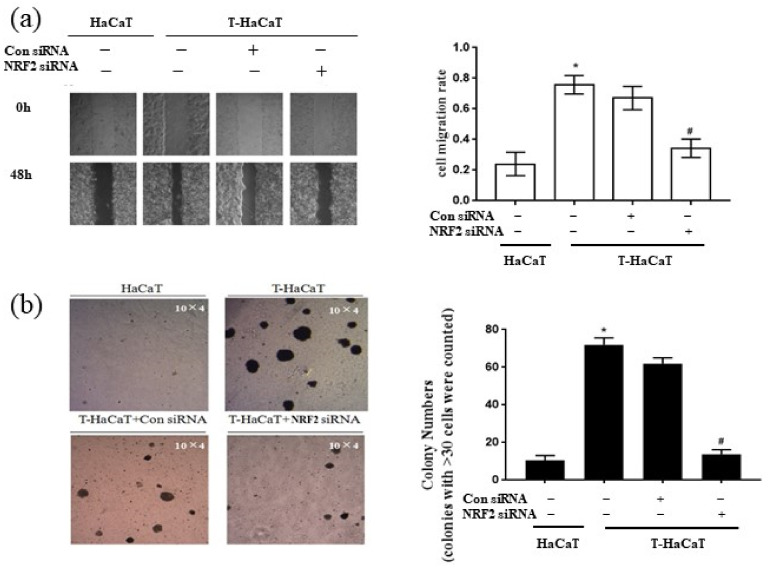
Figure 4.
The cell migration rate and the colony number in T-HaCaT cells after transfection NRF2. (a) Wound-healing assay (Scheme 10 × 4) and the rate of migration. (b) Colony formation assay and colony numbers. Error bars are the mean ± SD (n = 3). * Compared with HaCaT cells, p < 0.05; # Compared with control siRNA cells, p < 0.05.
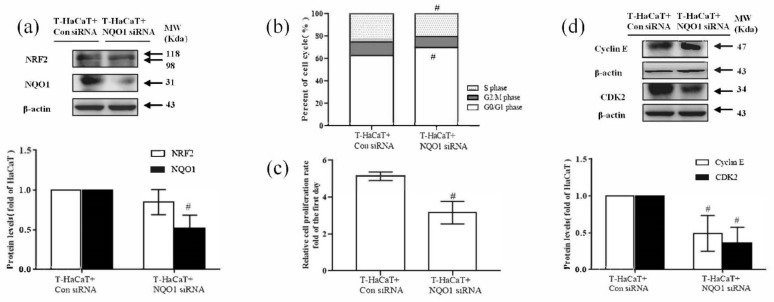
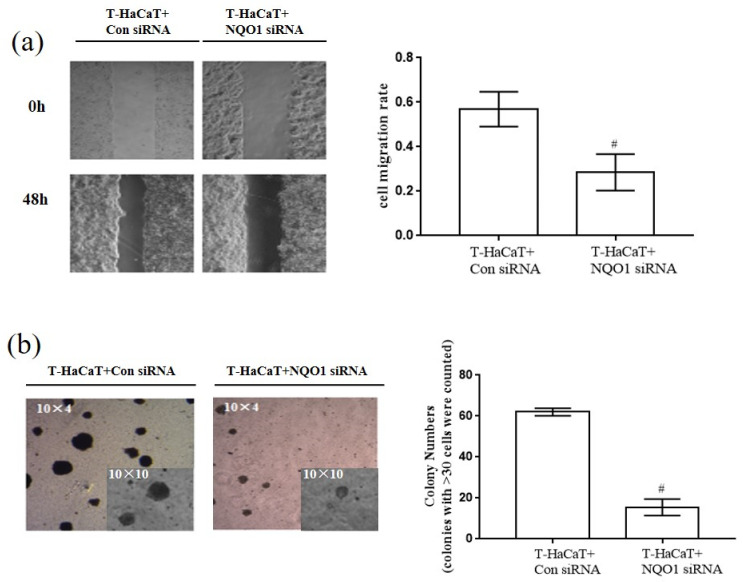
3.4. NQO1-Mediated Cellular Proliferation in Arsenite-Exposed HaCaT Cells
To learn more about the role of NQO1 in the arsenide-induced malignant transformation of HaCaT cells, NQO1 was silenced by NQO1 siRNA in arsenite-transformed T-HaCaT cells. After NQO1 siRNA transfection of T-HaCaT cells, the NQO1 protein level was significantly decreased in T-HaCaT cells, while the NRF2 protein level was not changed (p < 0.05, Figure 5a). The proportion of G0/G1 phase cells was significantly increased and S phase cells were decreased significantly after silencing NQO1 (p < 0.05, Figure 5b), and the expression of the cell cycle-related proteins cyclin E and CDK2 was reduced after transfection (p < 0.05, Figure 5d). Furthermore, the proliferation of T-HaCaT cells was blocked (p < 0.05, Figure 5c), HaCaT cell migration was suppressed (p < 0.05, Figure 6a), and the anchorage-independent growth capacity of T-HaCaT cells was decreased (p < 0.05, Figure 6b) after blocking NQO1 expression with siRNA, which suggested that the malignant phenotype in HaCaT cells was relieved. These results demonstrated that NQO1 deficiency blocked the proliferation of T-HaCaT cells by blocking the change in the cell cycle, which suggested that, in addition to NRF2, NQO1 is also a key factor in cell proliferation in HaCaT cells exposed to arsenite.
Figure 5.
Effect of NQO1 on arsenite-induced malignant transformation of HaCaT cells. (a) Protein bands and relative protein levels of NRF2 and NQO1 in HaCaT cells and T-HaCaT cells with or without NQO1. (b) Changes in the cell cycle. (c) Change in the cell proliferation rate. (d) Protein bands and relative protein levels of cell cycle related protein Cyclin E and CDK2. Error bars are the mean ± SD (n = 3). # Compared with control siRNA cells, p < 0.05.
Figure 6.
The cell migration rate and the colony number in T-HaCaT cells after transfection with NQO1 siRNA. (a) Wound-healing assay (magnification factor: 10 × 4) and the rate of migration. (b) Colony formation assay and colony numbers. Error bars are the mean ± SD (n = 3). # Compared with control siRNA cells, p < 0.05.
4. Discussion
Long-term exposure to inorganic arsenic can lead to the occurrence of multisystem and multiorgan cancers [51,52]. Many studies have demonstrated the malignant transformation of normal cells after arsenite exposure and revealed the mechanism of arsenic-induced cancer [53,54,55]. For animal models of arsenic-induced skin cancer, which have not been constructed [56], HaCaT cells are widely used as an in vitro model to study the mechanism of arsenic-mediated skin cancer, especially in SCC [57,58,59]. Numerous studies have shown that exposure to a variety of exogenous chemicals may lead to the malignant transformation of HaCaT cells [60,61,62]. We found in an earlier study that HaCaT cells in soft agar exhibited high proliferation rates, increased MMP-9 secretion, and multicolony characteristics after being treated with 1.0 M sodium arsenite for more than 35 passages [44]. In the present study, we again verified that 1.0 µM sodium arsenite exposure can lead to a malignant phenotype in HaCaT cells by affecting the cell cycle of HaCaT cells (from the first passage) and increasing their proliferation rate from passage to passage (from passage 7) because sustaining proliferative signaling, evading growth suppressors, and replicative immortality are the hallmarks of cancer [31].
Furthermore, we explored the potential molecular mechanisms for promoting cellular proliferation for the carcinogenesis of arsenite. Many previous reports have suggested that the activation of NRF2 in tumor cells could affect proliferation [63,64] and accelerate the development of the disease [65,66,67,68], whose target gene NQO1 also plays an important role in cellular proliferation and is overexpressed in many cancer tissues [41,69,70]. Indeed, our past studies have found that high levels of NRF2 may induce arsenite-induced tumors [44,46]; in this study, we observed that either high levels of NRF2 (after seven passages) or NQO1 (after 21 passages) were caused by arsenite. Notably, the in vitro UV irradiation of melanocytes has been demonstrated to induce the activation of NRF2 and its target genes, including NQO1 [71]. Consistent with our results, NQO1 promotes an aggressive phenotype in hepatocellular carcinoma by amplifying ERK-NRF2 signaling [72]; immunohistochemical analysis showed that the protein levels of NRF2 and NQO1 were higher in carcinoma tissues than in benign follicular adenomas and hyperplastic nodules [73]. Overall, the NRF2/NQO1 pathway is important in response to environmental toxins and may be a tumor suppressor [74]. In addition, the results of the study also indicated that arsenite can regulate the protein expression levels of cyclin E and CDK2, which are also associated with cell proliferation and malignant transformation. This finding explains the cell cycle progression from the G0/G1 to S phase observed in this study. Cyclin E is an essential component of the nuclear cell cycle machinery. In mammalian cells, two types of cyclin E activate CDK2 and initiate cell cycle progression by phosphorylating various cellular proteins [75]. Cyclin E appears at the end of the G1 phase, which can facilitate and shorten the transition from the G/S phase [76]. Cyclin E binds to CDK2 at the end of stage G1, activates CDK2 activity, and promotes the expression of genes related to DNA replication, thereby initiating cellular DNA replication [77]. Lee et al. found that the fargesin-induced colony growth inhibition of colon cancer cells was mediated by suppression of the cyclin-dependent kinase 2 (CDK2)/cyclin E signaling axis by the upregulation of p21WAF1/Cip1, resulting in G1-phase cell cycle accumulation in a dose-dependent manner [78]. Liang et al. demonstrated that the administration of cyclin E siRNA could inhibit breast tumor growth in nude mice [79]. Therefore, we proposed that arsenite can induce the malignant transformation of HaCaT cells, affect cell cycle progression, and promote cell proliferation. The phase shift of the cell cycle can be adjusted by the G0/G1 and S phase structural ratio by increasing the expression of Cyclin E-CDK2.
In addition, the upstream–downstream relationship between NRF2/NQO1 and cyclin E-CDK2 in promoting cell proliferation and subsequent malignant transformation caused by arsenite drew our attention. To clarify this problem, we silenced the 35 passages of T-HaCaT cells by transfection with NRF2 siRNA and NQO1 siRNA, a kind of double-stranded RNA with a length of 20 to 25 nucleotides, by interfering with the post transcriptional degradation of mRNA expressing specific genes with complementary nucleotide sequences, thus preventing translation. We found that in addition to downregulating NQO1 expression, the silencing of NRF2 by siRNA interference reduced the cell proliferation rate and cell cycle-related proteins Cyclin E and CDK2 and ultimately decreased the migration rate and colony-forming capacity of T-HaCaT cells. This result corresponds to Homma et al. [66]. They found that the knockout of NRF2 in A549 and NCI-H292 cells caused cell cycle arrest in the G1 phase. Furthermore, other in vitro experiments showed that a lack of NRF2 prevented cell cycle progression and slowed cell proliferation [80,81]. Moreover, there are few reports of the relationship between NQO1 and cyclin E-CDK2. We further observed the same situation as NRF2 and NQO1 silencing resulted in decreased cyclin E and CDK2 protein levels, arrested cell cycle progression from the G0/G1 to S phase, and restricted cell proliferation and malignant phenotypes in arsenite-transformed cells, which were characterized by reduced colonization and limited migration. This result is consistent with our previous report on HBC cells [48]. From this, we conclude that a new common pathway of arsenic carcinogenesis has been identified.
NRF2 and NQO1 are generally recognized to play important roles in cancer prevention and treatment [82,83,84,85], so they can be targeted for skin cancer. Researchers searched for molecules able to intentionally activate NRF2 because it has been shown to be a way to prevent skin cancer [86,87,88]. As the activation of NRF2 in cancer is two-sided [36,89], its functions are more far-reaching than originally envisioned, which presents new challenges and opportunities for targeting NRF2 and NQO1 in skin cancer prevention and treatment [90].
Unfortunately, we do not yet know the mechanism by which the NRF2/NQO1 pathway regulates cyclin E-CDK2; in addition, we performed all the experiments on a single cell line, and we have not yet validated our results based on animal models by using cell-derived xenografts, which are our research plans for the future. It must be acknowledged that the mechanism of SCC is complex and must therefore be taken into account holistically in the interpretation of the mechanism and future treatment. Moreover, a genomic approach is necessary for determining DNA mutations caused by arsenite treatment in future studies, which is important to understand whether arsenite is a carcinogenicity promoter or initiator.
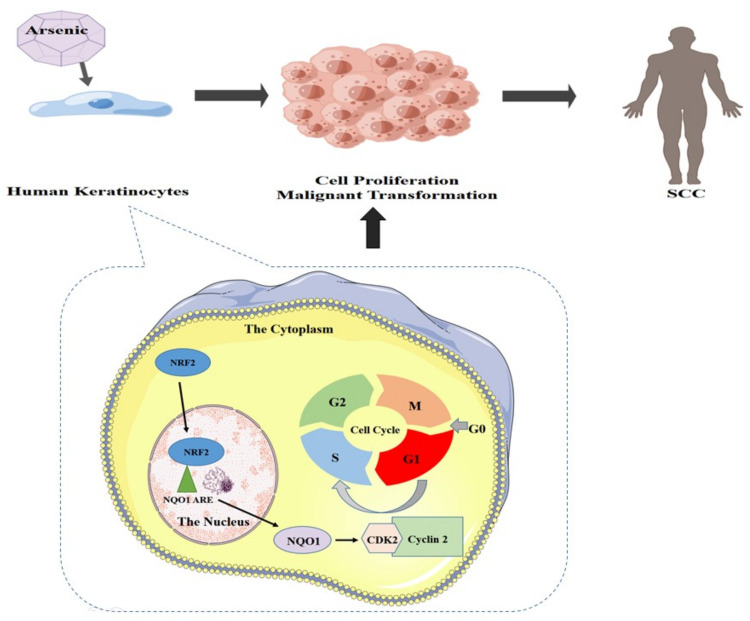
5. Conclusions
In conclusion, we demonstrated that NRF2/NQO1 plays an important role in the arsenite-induced malignant transformation of cells. Increased regulation of NRF2/NQO1 increases cyclin E-cdk2 expression and promotes arsenite-induced disruption of the HaCaT cell cycle from the G0/G1 to S phase, which leads to cell proliferation and malignancy. In summary, NRF2 has been shown to regulate NQO1, and both contribute to the transformation of arsenite-induced cell malignancy (Figure 7). Our research provides important information about the molecular mechanisms of arsenic-induced SCC. We found that using siRNA to silence NRF2 and NQO1 led to a significant decrease in protein expression in genes downstream of NRF2 (NQO1) and Cyclin E-CDK2. Therefore, these results suggest that the silencing of NRF2 and NQO1 inhibits the growth of HaCaT cells and that arsenite-induced malignant phenotypes are alleviated. In summary, the findings from this study can assist in further understanding the health effect mechanism of arsenic pollution and facilitate future developments of new arsenic and other similar environmental factors (e.g., UV radiation)-induced SCC treatment and prevention.
Figure 7.
Proposed model by which NRF2 regulates NQO1 to promote proliferation in arsenite-induced malignant transformation.
Acknowledgments
We would like to thank Yangming Gao from Dalian Medical University for his generously supplied HaCaT cells in this study.
Abbreviations
| ANOVA | analysis of variance |
| ARE | antioxidant response element |
| CDK2 | Cyclin-dependent kinase 2 |
| DMEM | Dulbecco’s modified Eagle’s medium |
| FBS | Fetal bovine serum |
| HaCaT | immortalized human keratinocyte cells |
| Keap1 | Kelch-like ECH-associated protein 1 |
| NaAsO2 | sodium arsenite |
| NRF2 | nuclear factor-erythroid-2 p45-related factor 2 |
| NQO-1 | NAD(P) H: Quinine oxidoreductase 1 |
| NADPH | nicotinamide adenine dinucleotide phosphate |
| PBS | phosphate-buffered saline |
| PI | Propidium iodide |
| ROS | reactive oxygen species |
| T-HaCaT | arsenite-transformed HaCaT cells |
| HBE | human bronchial epithelial |
| MC | skin melanoma |
| NMSC | non-melanoma skin cancer |
| BCC | basal cell carcinoma |
| SCC | squamous cell carcinoma |
| UV | ultraviolet radiation |
| siRNA | small interfering RNA |
Author Contributions
Conceptualization, Y.A.; methodology, Y.M.; software, H.X.; validation, R.Y. and Q.Y.; formal analysis, K.K.; investigation, H.D.; resources, H.Z.; data curation, X.W. and C.L.; writing—original draft preparation, Q.Y.; writing—review and editing, T.J.; visualization, Q.Y.; supervision, J.Z.; project administration, Y.A.; funding acquisition, T.J. and Y.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported in part by the National Natural Science Foundation of China (NSFC) (No. 81872646; 81811540034; 81573173); a project funded by the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD); the open project of key laboratory of environmental pollution and disease surveillance, Ministry of Education (qian jiao he KY NO. [2018]483); and the Guizhou province science and technology planning project, Science and Technology Department of Guizhou Province (qian jiao he support NO. [2020]4Y235).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Garelick H., Jones H., Dybowska A., Valsami-Jones E. Arsenic pollution sources. Rev. Environ. Contam. Toxicol. 2008;197:17–60. doi: 10.1007/978-0-387-79284-2_2. [DOI] [PubMed] [Google Scholar]
- 2.Hong Y.S., Song K.H., Chung J.Y. Health effects of chronic arsenic exposure. J. Prev. Med. Public Health. 2014;47:245–252. doi: 10.3961/jpmph.14.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tchounwou P.B., Wilson B., Ishaque A. Important considerations in the development of public health advisories for arsenic and arsenic-containing compounds in drinking water. Rev. Environ. Health. 1999;14:211–229. doi: 10.1515/REVEH.1999.14.4.211. [DOI] [PubMed] [Google Scholar]
- 4.Rousselot P., Labaume S., Marolleau J.P., Larghero J., Noguera M.H., Brouet J.C., Fermand J.P. Arsenic trioxide and melarsoprol induce apoptosis in plasma cell lines and in plasma cells from myeloma patients. Cancer Res. 1999;59:1041–1048. [PubMed] [Google Scholar]
- 5.Missimer T.M., Teaf C.M., Beeson W.T., Maliva R.G., Woolschlager J., Covert D.J. Natural Background and Anthropogenic Arsenic Enrichment in Florida Soils, Surface Water, and Groundwater: A Review with a Discussion on Public Health Risk. Int. J. Environ. Res. Public Health. 2018;15:2278. doi: 10.3390/ijerph15102278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oremland R.S., Stolz J.F. The ecology of arsenic. Science. 2003;300:939–944. doi: 10.1126/science.1081903. [DOI] [PubMed] [Google Scholar]
- 7.Hull E.A., Barajas M., Burkart K.A., Fung S.R., Jackson B.P., Barrett P.M., Neumann R.B., Olden J.D., Gawel J.E. Human health risk from consumption of aquatic species in arsenic-contaminated shallow urban lakes. Sci. Total Environ. 2021;770:145318. doi: 10.1016/j.scitotenv.2021.145318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xue L., Zhao Z., Zhang Y., Liao J., Wu M., Wang M., Sun J., Gong H., Guo M., Li S., et al. Dietary exposure to arsenic and human health risks in western Tibet. Sci. Total Environ. 2020;731:138840. doi: 10.1016/j.scitotenv.2020.138840. [DOI] [PubMed] [Google Scholar]
- 9.Monteiro D.O.E., Caixeta E.S., Santos V., Pereira B.B. Arsenic exposure from groundwater: Environmental contamination, human health effects, and sustainable solutions. J. Toxicol. Environ. Health B Crit. Rev. 2021;24:119–135. doi: 10.1080/10937404.2021.1898504. [DOI] [PubMed] [Google Scholar]
- 10.Byeon E., Kang H.M., Yoon C., Lee J.S. Toxicity mechanisms of arsenic compounds in aquatic organisms. Aquat Toxicol. 2021;237:105901. doi: 10.1016/j.aquatox.2021.105901. [DOI] [PubMed] [Google Scholar]
- 11.Rahman M.A., Hasegawa H., Lim R.P. Bioaccumulation, biotransformation and trophic transfer of arsenic in the aquatic food chain. Environ. Res. 2012;116:118–135. doi: 10.1016/j.envres.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 12.Wei Z., Zhiqiang G., Dongdong S., Sen D., Li Z. Arsenic speciation in wild marine organisms and a health risk assessment in a subtropical bay of China. Sci. Total Environ. 2018;626:621–629. doi: 10.1016/j.scitotenv.2018.01.108. [DOI] [PubMed] [Google Scholar]
- 13.Vahter M., Skroder H., Rahman S.M., Levi M., Derakhshani H.J., Kippler M. Prenatal and childhood arsenic exposure through drinking water and food and cognitive abilities at 10 years of age: A prospective cohort study. Environ. Int. 2020;139:105723. doi: 10.1016/j.envint.2020.105723. [DOI] [PubMed] [Google Scholar]
- 14.Mondal D., Rahman M.M., Suman S., Sharma P., Siddique A.B., Rahman M.A., Bari A., Kumar R., Bose N., Singh S.K., et al. Arsenic exposure from food exceeds that from drinking water in endemic area of Bihar, India. Sci. Total Environ. 2021;754:142082. doi: 10.1016/j.scitotenv.2020.142082. [DOI] [PubMed] [Google Scholar]
- 15.Joardar M., Das A., Chowdhury N.R., Mridha D., De A., Majumdar K.K., Roychowdhury T. Health effect and risk assessment of the populations exposed to different arsenic levels in drinking water and foodstuffs from four villages in arsenic endemic Gaighata block, West Bengal, India. Environ. Geochem. Health. 2021;43:3027–3053. doi: 10.1007/s10653-021-00823-3. [DOI] [PubMed] [Google Scholar]
- 16.Baker B.A., Cassano V.A., Murray C. Arsenic Exposure, Assessment, Toxicity, Diagnosis, and Management: Guidance for Occupational and Environmental Physicians. J. Occup. Environ. Med. 2018;60:e634–e639. doi: 10.1097/JOM.0000000000001485. [DOI] [PubMed] [Google Scholar]
- 17.Chou C.H., De Rosa C.T. Case studies—Arsenic. Int. J. Hyg. Environ. Health. 2003;206:381–386. doi: 10.1078/1438-4639-00234. [DOI] [PubMed] [Google Scholar]
- 18.Jarup L. Hazards of heavy metal contamination. Br. Med. Bull. 2003;68:167–182. doi: 10.1093/bmb/ldg032. [DOI] [PubMed] [Google Scholar]
- 19.Chakraborti D., Rahman M.M., Chatterjee A., Das D., Das B., Nayak B., Pal A., Chowdhury U.K., Ahmed S., Biswas B.K., et al. Fate of over 480 million inhabitants living in arsenic and fluoride endemic Indian districts: Magnitude, health, socio-economic effects and mitigation approaches. J Trace Elem Med Biol. 2016;38:33–45. doi: 10.1016/j.jtemb.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 20.Tchounwou P.B., Yedjou C.G., Udensi U.K., Pacurari M., Stevens J.J., Patlolla A.K., Noubissi F., Kumar S. State of the science review of the health effects of inorganic arsenic: Perspectives for future research. Environ. Toxicol. 2019;34:188–202. doi: 10.1002/tox.22673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pye-Smith R.J. Arsenic Cancer, with Description of a Case. Proc. R. Soc. Med. 1913;6:229–236. doi: 10.1177/0035915713006002111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bungeler W. Arsenic cancer. Munch. Med. Wochenschr. 1958;100:1117–1118. [PubMed] [Google Scholar]
- 23.Wei S., Zhang H., Tao S. A review of arsenic exposure and lung cancer. Toxicol. Res. 2019;8:319–327. doi: 10.1039/C8TX00298C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mayer J.E., Goldman R.H. Arsenic and skin cancer in the USA: The current evidence regarding arsenic-contaminated drinking water. Int. J. Dermatol. 2016;55:e585–e591. doi: 10.1111/ijd.13318. [DOI] [PubMed] [Google Scholar]
- 25.Jackson R., Grainge J.W. Arsenic and cancer. Can. Med. Assoc. J. 1975;113:396–401. [PMC free article] [PubMed] [Google Scholar]
- 26.Hamilton A. Industrial Toxicology. 2nd ed. P. B. Hoeber; New York, NY, USA: 1949. [Google Scholar]
- 27.Gordon R. Skin cancer: An overview of epidemiology and risk factors. Semin. Oncol. Nurs. 2013;29:160–169. doi: 10.1016/j.soncn.2013.06.002. [DOI] [PubMed] [Google Scholar]
- 28.Rosales-Castillo J.A., Acosta-Saavedra L.C., Torres R., Ochoa-Fierro J., Borja-Aburto V.H., Lopez-Carrillo L., Garcia-Vargas G.G., Gurrola G.B., Cebrian M.E., Calderon-Aranda E.S. Arsenic exposure and human papillomavirus response in non-melanoma skin cancer Mexican patients: A pilot study. Int. Arch. Occup. Environ. Health. 2004;77:418–423. doi: 10.1007/s00420-004-0527-0. [DOI] [PubMed] [Google Scholar]
- 29.Surdu S. Non-melanoma skin cancer: Occupational risk from UV light and arsenic exposure. Rev. Environ. Health. 2014;29:255–264. doi: 10.1515/reveh-2014-0040. [DOI] [PubMed] [Google Scholar]
- 30.Surdu S., Fitzgerald E.F., Bloom M.S., Boscoe F.P., Carpenter D.O., Haase R.F., Gurzau E., Rudnai P., Koppova K., Vahter M., et al. Polymorphisms in DNA repair genes XRCC1 and XRCC3, occupational exposure to arsenic and sunlight, and the risk of non-melanoma skin cancer in a European case-control study. Environ. Res. 2014;134:382–389. doi: 10.1016/j.envres.2014.08.020. [DOI] [PubMed] [Google Scholar]
- 31.Kim T.H., Seo J.W., Hong Y.S., Song K.H. Case-control study of chronic low-level exposure of inorganic arsenic species and non-melanoma skin cancer. J. Dermatol. 2017;44:1374–1379. doi: 10.1111/1346-8138.13993. [DOI] [PubMed] [Google Scholar]
- 32.Hanahan D. Hallmarks of Cancer: New Dimensions. Cancer Discov. 2022;12:31–46. doi: 10.1158/2159-8290.CD-21-1059. [DOI] [PubMed] [Google Scholar]
- 33.Wu S., Lu H., Bai Y. Nrf2 in cancers: A double-edged sword. Cancer Med. 2019;8:2252–2267. doi: 10.1002/cam4.2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fan Z., Wirth A.K., Chen D., Wruck C.J., Rauh M., Buchfelder M., Savaskan N. Nrf2-Keap1 pathway promotes cell proliferation and diminishes ferroptosis. Oncogenesis. 2017;6:e371. doi: 10.1038/oncsis.2017.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Murakami S., Motohashi H. Roles of Nrf2 in cell proliferation and differentiation. Free Radic. Biol. Med. 2015;88:168–178. doi: 10.1016/j.freeradbiomed.2015.06.030. [DOI] [PubMed] [Google Scholar]
- 36.Geismann C., Arlt A., Sebens S., Schafer H. Cytoprotection “gone astray”: Nrf2 and its role in cancer. OncoTargets Ther. 2014;7:1497–1518. doi: 10.2147/OTT.S36624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Montserrat R.D.L.V., Eli C., Donna D.Z. NRF2 and the Hallmarks of Cancer. Cancer Cell. 2018;34:21–43. doi: 10.1016/j.ccell.2018.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chorley B.N., Campbell M.R., Wang X., Karaca M., Sambandan D., Bangura F., Xue P., Pi J., Kleeberger S.R., Bell D.A. Identification of novel NRF2-regulated genes by ChIP-Seq: Influence on retinoid X receptor alpha. Nucleic Acids Res. 2012;40:7416–7429. doi: 10.1093/nar/gks409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Malhotra D., Portales-Casamar E., Singh A., Srivastava S., Arenillas D., Happel C., Shyr C., Wakabayashi N., Kensler T.W., Wasserman W.W., et al. Global mapping of binding sites for Nrf2 identifies novel targets in cell survival response through ChIP-Seq profiling and network analysis. Nucleic Acids Res. 2010;38:5718–5734. doi: 10.1093/nar/gkq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dinkova-Kostova A.T., Talalay P. NAD(P)H:quinone acceptor oxidoreductase 1 (NQO1), a multifunctional antioxidant enzyme and exceptionally versatile cytoprotector. Arch. Biochem. Biophys. 2010;501:116–123. doi: 10.1016/j.abb.2010.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ross D., Kepa J.K., Winski S.L., Beall H.D., Anwar A., Siegel D. NAD(P)H:quinone oxidoreductase 1 (NQO1): Chemoprotection, bioactivation, gene regulation and genetic polymorphisms. Chem. Biol. Interact. 2000;129:77–97. doi: 10.1016/S0009-2797(00)00199-X. [DOI] [PubMed] [Google Scholar]
- 42.Yang Y., Zhu G., Dong B., Piao J., Chen L., Lin Z. The NQO1/PKLR axis promotes lymph node metastasis and breast cancer progression by modulating glycolytic reprogramming. Cancer Lett. 2019;453:170–183. doi: 10.1016/j.canlet.2019.03.054. [DOI] [PubMed] [Google Scholar]
- 43.Butsri S., Kukongviriyapan V., Senggunprai L., Kongpetch S., Zeekpudsa P., Prawan A. Downregulation of NAD(P)H:quinone oxidoreductase 1 inhibits proliferation, cell cycle and migration of cholangiocarcinoma cells. Oncol. Lett. 2017;13:4540–4548. doi: 10.3892/ol.2017.5951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cheng Y., Li J., Martinka M., Li G. The expression of NAD(P)H:quinone oxidoreductase 1 is increased along with NF-kappaB p105/p50 in human cutaneous melanomas. Oncol. Rep. 2010;23:973–979. doi: 10.3892/or_00000722. [DOI] [PubMed] [Google Scholar]
- 45.Wang D., Ma Y., Yang X., Xu X., Zhao Y., Zhu Z., Wang X., Deng H., Li C., Gao F., et al. Hypermethylation of the Keap1 gene inactivates its function, promotes Nrf2 nuclear accumulation, and is involved in arsenite-induced human keratinocyte transformation. Free Radic. Biol. Med. 2015;89:209–219. doi: 10.1016/j.freeradbiomed.2015.07.153. [DOI] [PubMed] [Google Scholar]
- 46.Luo S., Lei K., Xiang D., Ye K. NQO1 Is Regulated by PTEN in Glioblastoma, Mediating Cell Proliferation and Oxidative Stress. Oxid. Med. Cell. Longev. 2018;2018:9146528. doi: 10.1155/2018/9146528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yang X., Wang D., Ma Y., Xu X., Zhu Z., Wang X., Deng H., Li C., Chen M., Tong J., et al. Continuous activation of Nrf2 and its target antioxidant enzymes leads to arsenite-induced malignant transformation of human bronchial epithelial cells. Toxicol. Appl. Pharmacol. 2015;289:231–239. doi: 10.1016/j.taap.2015.09.020. [DOI] [PubMed] [Google Scholar]
- 48.Tong Y.H., Zhang B., Yan Y.Y., Fan Y., Yu J.W., Kong S.S., Zhang D., Fang L., Su D., Lin N.M. Dual-negative expression of Nrf2 and NQO1 predicts superior outcomes in patients with non-small cell lung cancer. Oncotarget. 2017;8:45750–45758. doi: 10.18632/oncotarget.17403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kong Q., Deng H., Li C., Wang X., Shimoda Y., Tao S., Kato K., Zhang J., Yamanaka K., An Y. Sustained high expression of NRF2 and its target genes induces dysregulation of cellular proliferation and apoptosis is associated with arsenite-induced malignant transformation of human bronchial epithelial cells. Sci. Total Environ. 2021;756:143840. doi: 10.1016/j.scitotenv.2020.143840. [DOI] [PubMed] [Google Scholar]
- 50.Boukamp P., Petrussevska R.T., Breitkreutz D., Hornung J., Markham A., Fusenig N.E. Normal keratinization in a spontaneously immortalized aneuploid human keratinocyte cell line. J. Cell Biol. 1988;106:761–771. doi: 10.1083/jcb.106.3.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schafer K.A. The Cell Cycle: A Review. Vet. Pathol. 1998;35:461–478. doi: 10.1177/030098589803500601. [DOI] [PubMed] [Google Scholar]
- 52.Yu S., Liao W.T., Lee C.H., Chai C.Y., Yu C.L., Yu H.S. Immunological dysfunction in chronic arsenic exposure: From subclinical condition to skin cancer. J. Dermatol. 2018;45:1271–1277. doi: 10.1111/1346-8138.14620. [DOI] [PubMed] [Google Scholar]
- 53.Wang Z., Zhao Y., Smith E., Goodall G.J., Drew P.A., Brabletz T., Yang C. Reversal and prevention of arsenic-induced human bronchial epithelial cell malignant transformation by microRNA-200b. Toxicol. Sci. 2011;121:110–122. doi: 10.1093/toxsci/kfr029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ge Y., Zhu J., Wang X., Zheng N., Tu C., Qu J., Ren X. Mapping dynamic histone modification patterns during arsenic-induced malignant transformation of human bladder cells. Toxicol. Appl. Pharmacol. 2018;355:164–173. doi: 10.1016/j.taap.2018.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Benbrahim-Tallaa L., Waterland R.A., Styblo M., Achanzar W.E., Webber M.M., Waalkes M.P. Molecular events associated with arsenic-induced malignant transformation of human prostatic epithelial cells: Aberrant genomic DNA methylation and K-ras oncogene activation. Toxicol. Appl. Pharmacol. 2005;206:288–298. doi: 10.1016/j.taap.2004.11.017. [DOI] [PubMed] [Google Scholar]
- 56.Hunt K.M., Srivastava R.K., Elmets C.A., Athar M. The mechanistic basis of arsenicosis: Pathogenesis of skin cancer. Cancer Lett. 2014;354:211–219. doi: 10.1016/j.canlet.2014.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rusanov A.L., Romashin D.D., Zgoda V.G., Butkova T.V., Luzgina N.G. Protein dataset of immortalized keratinocyte HaCaT cells and normal human keratinocytes. Data Brief. 2021;35:106871. doi: 10.1016/j.dib.2021.106871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Valerio H.P., Ravagnani F.G., Ronsein G.E., Di Mascio P. A single dose of Ultraviolet-A induces proteome remodeling and senescence in primary human keratinocytes. Sci. Rep. 2021;11:23355. doi: 10.1038/s41598-021-02658-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lee R.H., Oh J.D., Hwang J.S., Lee H.K., Shin D. Antitumorigenic effect of insect-derived peptide poecilocorisin-1 in human skin cancer cells through regulation of Sp1 transcription factor. Sci. Rep. 2021;11:18445. doi: 10.1038/s41598-021-97581-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bicheng F., Pradeep D., Fengjie L., Laura G., Martina B., Alfonso M., Deniz T. Pyrenosetin D, a New Pentacyclic Decalinoyltetramic Acid Derivative from the Algicolous Fungus Pyrenochaetopsis sp. FVE-087. Mar. Drugs. 2020;18:281. doi: 10.3390/md18060281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Makoto S., Kazunori H., Masafumi Y., Mohammad D.A., Said H.F., Nobuyuki H., Lisa K., Kiyoshi Y., Masashi K. Lithium promotes malignant transformation of nontumorigenic cells in vitro. Sci. Total Environ. 2020;744:140830. doi: 10.1016/j.scitotenv.2020.140830. [DOI] [PubMed] [Google Scholar]
- 62.Wright C., Iyer A.K.V., Wang L., Wu N., Yakisich J.S., Rojanasakul Y., Azad N. Effects of titanium dioxide nanoparticles on human keratinocytes. Drug Chem. Toxicol. 2017;40:90–100. doi: 10.1080/01480545.2016.1185111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang H.S., Zhang Z.G., Du G.Y., Sun H.L., Liu H.Y., Zhou Z., Gou X.M., Wu X.H., Yu X.Y., Huang Y.H. Nrf2 promotes breast cancer cell migration via up-regulation of G6PD/HIF-1alpha/Notch1 axis. J. Cell Mol. Med. 2019;23:3451–3463. doi: 10.1111/jcmm.14241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xu P., Jiang L., Yang Y., Wu M., Liu B., Shi Y., Shen Q., Jiang X., He Y., Cheng D., et al. PAQR4 promotes chemoresistance in non-small cell lung cancer through inhibiting Nrf2 protein degradation. Theranostics. 2020;10:3767–3778. doi: 10.7150/thno.43142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Mitsuishi Y., Taguchi K., Kawatani Y., Shibata T., Nukiwa T., Aburatani H., Yamamoto M., Motohashi H. Nrf2 redirects glucose and glutamine into anabolic pathways in metabolic reprogramming. Cancer Cell. 2012;22:66–79. doi: 10.1016/j.ccr.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 66.Homma S., Ishii Y., Morishima Y., Yamadori T., Matsuno Y., Haraguchi N., Kikuchi N., Satoh H., Sakamoto T., Hizawa N., et al. Nrf2 enhances cell proliferation and resistance to anticancer drugs in human lung cancer. Clin. Cancer Res. 2009;15:3423–3432. doi: 10.1158/1078-0432.CCR-08-2822. [DOI] [PubMed] [Google Scholar]
- 67.Jaramillo M.C., Zhang D.D. The emerging role of the Nrf2-Keap1 signaling pathway in cancer. Genes Dev. 2013;27:2179–2191. doi: 10.1101/gad.225680.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Yamadori T., Ishii Y., Homma S., Morishima Y., Kurishima K., Itoh K., Yamamoto M., Minami Y., Noguchi M., Hizawa N. Molecular mechanisms for the regulation of Nrf2-mediated cell proliferation in non-small-cell lung cancers. Oncogene. 2012;31:4768–4777. doi: 10.1038/onc.2011.628. [DOI] [PubMed] [Google Scholar]
- 69.Hosein A.N., Beg M.S. Pancreatic Cancer Metabolism: Molecular Mechanisms and Clinical Applications. Curr. Oncol. Rep. 2018;20:56. doi: 10.1007/s11912-018-0699-5. [DOI] [PubMed] [Google Scholar]
- 70.Marco G., Aijaz A.W., Gang L. The NAD(P)H:Quinone Oxidoreductase 1 induces cell cycle progression and proliferation of melanoma cells. Free Radical. Bio. Med. 2010;48:1601–1609. doi: 10.1016/j.freeradbiomed.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 71.Marrot L., Jones C., Perez P., Meunier J.R. The significance of Nrf2 pathway in (photo)-oxidative stress response in melanocytes and keratinocytes of the human epidermis. Pigment. Cell Melanoma Res. 2008;21:79–88. doi: 10.1111/j.1755-148X.2007.00424.x. [DOI] [PubMed] [Google Scholar]
- 72.Yang Y., Zheng J., Wang M., Zhang J., Tian T., Wang Z., Yuan S., Liu L., Zhu P., Gu F., et al. NQO1 promotes an aggressive phenotype in hepatocellular carcinoma via amplifying ERK-NRF2 signaling. Cancer Sci. 2021;112:641–654. doi: 10.1111/cas.14744. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 73.Cedric O.R., Panos G.Z., Dionysios V.C., Dionysios V.C., Massimo B., Gerasimos P.S. Keap1/Nrf2 Signaling: A New Player in Thyroid Pathophysiology and Thyroid Cancer. Front. Endocrinol. 2019;10:510. doi: 10.3389/fendo.2019.00510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Carpenter E.L., Becker A.L., Indra A.K. NRF2 and Key Transcriptional Targets in Melanoma Redox Manipulation. Cancers. 2022;14:1531. doi: 10.3390/cancers14061531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chu C., Geng Y., Zhou Y., Sicinski P. Cyclin E in normal physiology and disease states. Trends Cell Biol. 2021;31:732–746. doi: 10.1016/j.tcb.2021.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Siu K.T., Rosner M.R., Minella A.C. An integrated view of cyclin E function and regulation. Cell Cycle. 2012;11:57–64. doi: 10.4161/cc.11.1.18775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hwang H.C., Clurman B.E. Cyclin E in normal and neoplastic cell cycles. Oncogene. 2005;24:2776–2786. doi: 10.1038/sj.onc.1208613. [DOI] [PubMed] [Google Scholar]
- 78.Lee G., Lee C., An H., Kang H.C., Lee H.S., Lee J.Y., Oh S., Cho S., Kim D.J., Cho Y. Fargesin Inhibits EGF-Induced Cell Transformation and Colon Cancer Cell Growth by Suppression of CDK2/Cyclin E Signaling Pathway. Int. J. Mol. Sci. 2021;22:2073. doi: 10.3390/ijms22042073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Liang Y., Gao H., Lin S.Y., Goss J.A., Brunicardi F.C., Li K. siRNA-based targeting of cyclin E overexpression inhibits breast cancer cell growth and suppresses tumor development in breast cancer mouse model. PLoS ONE. 2010;5:e12860. doi: 10.1371/journal.pone.0012860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lastra D., Escoll M., Cuadrado A. Transcription Factor NRF2 Participates in Cell Cycle Progression at the Level of G1/S and Mitotic Checkpoints. Antioxidants. 2022;11:946. doi: 10.3390/antiox11050946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Reddy N.M., Kleeberger S.R., Bream J.H., Fallon P.G., Kensler T.W., Yamamoto M., Reddy S.P. Genetic disruption of the Nrf2 compromises cell-cycle progression by impairing GSH-induced redox signaling. Oncogene. 2008;27:5821–5832. doi: 10.1038/onc.2008.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Zhang K., Chen D., Ma K., Wu X., Hao H., Jiang S. NAD(P)H:Quinone Oxidoreductase 1 (NQO1) as a Therapeutic and Diagnostic Target in Cancer. J. Med. Chem. 2018;61:6983–7003. doi: 10.1021/acs.jmedchem.8b00124. [DOI] [PubMed] [Google Scholar]
- 83.Oh E.T., Park H.J. Implications of NQO1 in cancer therapy. BMB Rep. 2015;48:609–617. doi: 10.5483/BMBRep.2015.48.11.190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Russo M., Spagnuolo C., Russo G.L., Skalicka-Wozniak K., Daglia M., Sobarzo-Sanchez E., Nabavi S.F., Nabavi S.M. Nrf2 targeting by sulforaphane: A potential therapy for cancer treatment. Crit. Rev. Food Sci. Nutr. 2018;58:1391–1405. doi: 10.1080/10408398.2016.1259983. [DOI] [PubMed] [Google Scholar]
- 85.Hammad A., Namani A., Elshaer M., Wang X.J., Tang X. “NRF2 addiction” in lung cancer cells and its impact on cancer therapy. Cancer Lett. 2019;467:40–49. doi: 10.1016/j.canlet.2019.09.016. [DOI] [PubMed] [Google Scholar]
- 86.Yang Y., Yang I., Cao M., Su Z.Y., Wu R., Guo Y., Fang M., Kong A.N. Fucoxanthin Elicits Epigenetic Modifications, Nrf2 Activation and Blocking Transformation in Mouse Skin JB6 P+ Cells. AAPS J. 2018;20:32. doi: 10.1208/s12248-018-0197-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chun K.S., Kundu J., Kundu J.K., Surh Y.J. Targeting Nrf2-Keap1 signaling for chemoprevention of skin carcinogenesis with bioactive phytochemicals. Toxicol. Lett. 2014;229:73–84. doi: 10.1016/j.toxlet.2014.05.018. [DOI] [PubMed] [Google Scholar]
- 88.Yang H.L., Lee C.L., Korivi M., Liao J.W., Rajendran P., Wu J.J., Hseu Y.C. Zerumbone protects human skin keratinocytes against UVA-irradiated damages through Nrf2 induction. Biochem. Pharmacol. 2018;148:130–146. doi: 10.1016/j.bcp.2017.12.014. [DOI] [PubMed] [Google Scholar]
- 89.Sivinski J., Zhang D.D., Chapman E. Targeting NRF2 to treat cancer. Semin. Cancer Biol. 2021;76:61–73. doi: 10.1016/j.semcancer.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Yang Y., Yin R., Wu R., Ramirez C.N., Sargsyan D., Li S., Wang L., Cheng D., Wang C., Hudlikar R., et al. DNA methylome and transcriptome alterations and cancer prevention by triterpenoid ursolic acid in UVB-induced skin tumor in mice. Mol. Carcinog. 2019;58:1738–1753. doi: 10.1002/mc.23046. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.