Abstract
Salmonella is a Gram-negative bacterium known to be the major cause of gastrointestinal diseases and systemic infections. During infection of murine B cells, Salmonella activates the PI3K/Akt pathway through its effector, SopB. This signaling pathway induces the downregulation of NLRC4 transcription, resulting in reduced secretion of IL-1β. Thus, Salmonella-infected B cells do not progress to pyroptosis; consequently, the bacteria can survive inside these cells. However, the mechanism by which Salmonella evades the control of B cells has not yet been elucidated. In this study, we found that SopB activates mTORC1, which is necessary for bacterial survival, since B cells cultured with the mTORC1 inhibitor rapamycin and B cells lacking raptor can control Salmonella infection. A similar result was observed in B cells when they were infected with the Salmonella SopB mutant (Δsopb). Salmonella also promoted the phosphorylation of the ULK1 complex at serine 757 (Ser757) by mTORC1, resulting in decreased levels of LC3-II in infected B cells. In this study, we did not observe these results when B cells were infected with Δsopb Salmonella. Our results demonstrated that Salmonella survival within B cells depends on the inhibition of autophagy by mTORC1 activation.
Keywords: Salmonella, B cells, autophagy, SopB, mTORC1, ULK1
1. Introduction
Salmonella enterica serovar Typhimurium (Salmonella) is a Gram-negative bacterium that causes gastrointestinal illness in humans, whereas in mice it causes a systemic infection similar to typhoid fever [1]. Worldwide, it is estimated that between 11 and 20 million new infections occur annually [2]. In addition, approximately 2–5% of people who become ill with typhoid fever become carriers of Salmonella [3]. In the gallbladder of these individuals, Salmonella forms biofilms that have been associated with the formation of gallstones and bladder stones, allowing Salmonella to evade both the immune system and the effect of drugs [4,5]. Once ingested, the bacteria cross the epithelial barrier of the small intestine, where they infect macrophages. These infected cells die by pyroptosis as a consequence of inflammasome activation, which permits Salmonella to spread to other anatomical sites and infect other cells [1,6]. Among the cells that may be infected are B cells, which have been reported to allow Salmonella survival for at least 60 days [7,8,9].
During the process of B-cell infection, Salmonella translocates a series of effector proteins through its Type III secretion system (T3SS). Among these effector proteins is SopB. Together with SopE and SopE2, SopB is involved in the activation of Cdc42 and Rac, permitting the entry of Salmonella into nonphagocytic cells [10,11]. In addition, SopB induces the accumulation of PIP3 in the cell membrane via its inositide phosphatase function, leading to the activation of PI3K [12]. During B-cell infection, SopB promotes Akt activation mediated by PI3K and thus the activation of the PI3K/Akt pathway, which allows phosphorylation and retention of YAP in the cytoplasm of B cells, preventing its dimerization with p73 in the nucleus; hence, NLRC4 gene expression does not occur [13,14]. Consequently, Salmonella represses inflammasome activation and IL-1β production. Contrary to what is observed in macrophages, B cells are not killed by pyroptosis; thus, Salmonella is able to survive within these cells. Pharmacological inhibitors for PI3K (wortmannin), AKT (AKTVII), or PDK1 (GSK 23334470) restore IL-1β production and bacterial control in B cells. Likewise, B lymphocytes from rictor gene conditional knockout mice also produce IL-1β and efficiently control Salmonella infection [14]. However, the mechanism that prevents this cell lineage from controlling Salmonella infection has not been described.
One of the main mechanisms for eliminating intracellular pathogens is autophagy [15,16]. This mechanism is characterized by the formation of double-membrane vacuoles, called autophagosomes. The onset of autophagosome formation is dependent on the ULK1 complex, which consists of UKL1, FIP200, and ATG101 proteins [17]. During autophagosome maturation, LC3-I binds to the autophagosome membrane to form LC3-II, allowing the recruitment of cargo into the phagosomes, which subsequently fuse with lysosomes, where enzymes degrade the content [18]. mTORC1 and AMPK are central regulators of the ULK1 complex. AMPK allows the activation of ULK1, whereas mTORC1 activation inhibits ULK1 by phosphorylating its serine 757 (Ser757) [17,19,20]. Although autophagy is a mechanism that effectively eliminates intracellular pathogens, several bacteria have adapted various mechanisms that allow them to evade it [16,21,22,23].
Since the PI3K/Akt pathway activates mTORC1 and this pathway is active during B-cell Salmonella infection, we considered whether Salmonella survival within B cells is autophagy inhibition-dependent through the activation of the PI3K/Akt/mTORC1 pathway through SopB.
2. Materials and Methods
2.1. Salmonella Strains
Salmonella enterica serovar Typhimurium 14028 (Salmonella) was obtained from ATCC, which was used to generate a strain lacking SopB (Salmonella Δsopb), using the lamda red system, as previously described. Salmonella and Salmonella Δsopb were transformed with the plasmid pEM180 [24], which codes for a green fluorescent protein (GFP).
Salmonella Δsopb was reconstituted with pSopBWT, a plasmid that expresses SopB under its promoter [25], or pSopBC460S, a plasmid that codifies for an inactive catalytic form of SopB [26]. Both the GFP and plasmid-reconstituted Salmonella strains were grown in LB medium supplemented with ampicillin (100 μg/mL).
2.2. Mice
C57BL/6 mice were obtained from the CINVESTAV Experimental Animal Production Unit; cd19+/creraptorfl/fl mice were generated by performing several crosses between B6.Cg-Rptortm1.1Dmsa/J (Jackson Laboratory 013188) and B6.129P2(C)-Cd19tm1(cre)Cgn/J (Jackson Laboratory 006785) mice. The genotype of these animals was corroborated according to the Jackson Laboratory’s instructions. Mice were handled according to NOM-062-ZOO-1999 and CINVESTAV guidelines. This project was approved by CINVESTAV’s Animal Care and Use Committee under protocol 0078-14.
2.3. Primary B-Cell Culture
Primary B cells from 6-to-8-week-old C57BL/6 mouse spleens were purified through negative selection, according to the manufacturer’s protocol (Miltenyi Biotec 130.090.862). The percentage of purity was evaluated through flow cytometry. A purity of about 98% was obtained (Figure S1A). Primary B cells were grown in RPMI medium supplemented with 10% heat-inactivated fetal bovine serum (RPMI 10% FBS) at 37 °C in 5% CO2.
2.4. Infection of B Cells with Salmonella
Salmonella strains were grown in LB medium supplemented with their corresponding antibiotics at 37 °C, with agitation for 18 h. Then, a dilution of 1:30 was performed in fresh LB medium, which was then incubated at 37 °C until a density of 0.6 was obtained at 600 nm. Subsequently, bacteria were centrifuged and then resuspended in RPMI 10% FBS. B cells were placed in contact with Salmonella at a MOI of 50 for 10 min at 37 °C; after incubation, the cells were centrifuged and the supernatant was discarded. The pellet alone was incubated for 20 min at 37 °C in 5% CO2. After this, cells were washed twice with PBS-gentamycin (80 μg/mL) and cultivated in RPMI 10% FBS supplemented with gentamycin (80 μg/mL) at 37 °C in 5% CO2. The percentage of infected B cells oscillated between 12% and 20% (Figure S1B). At 1, 3, and 24 h post-infection, cells were harvested through centrifugation, and the formed pellet was lysed using PBS 1% Triton X-100. Dilutions of lysates were plated in LB agar to measure CFUs. For pharmacological inhibitors essays, these were added 1 h before the infection and were maintained during the infection process. Pharmacological inhibitors were used at the following concentrations: wortmannin (Sigma, St. Louis, MO, USA, W1628), 0.05, 0.2, and 1.0 μM; AZD8186 (Selleck, S7694), 500 nM; and rapamycin (Sigma, St. Louis, MO, USA, R0395), 160 nM.
Salmonella-infected primary B cells were cultured for 24 h in RPMI medium supplemented with 10% FBS. Peptide D11 (Novus, NBP2-49888) and a control scramble peptide, L11 (Novus, NBP2-49887), were added after 21.5 h post-infection at a concentration of 20 μM, followed by the growth of the cultured cells at 24 h post-infection. Formation of CFUs was evaluated 24 h post-infection through plating on LB agar.
2.5. Viability Assays on Salmonella and B Cells
Cytotoxicity was assessed using a lactate dehydrogenase (LDH) release assay (Promega, G1780). The percentage of LDH released was calculated using the following formula: percentage of release = (experimental LDH release—spontaneous LDH release)/(maximal LDH release—spontaneous LDH release) × 100%. To evaluate the effect of the inhibitors in Salmonella, a kinetic assay was conducted. Inhibitor concentrations were maintained, as previously shown. Assays were performed over the 8 h; for each hour, the optic density was evaluated. At the end of the lapse time, CFU formation was evaluated through plating on LB agar.
2.6. Western Blot Analysis
Total infected B-cell protein was obtained through lysis with RIPA buffer. Samples in acrylamide gel were resolved at 12% or 15% via SDS-PAGE. Subsequently, proteins were transferred to a PVDF membrane and then blocked using 1% BSA solution for 1 h. Antibodies were diluted in block solution: pS6 ser 235/236 (Cell, Danvers, MA, USA D57.2.2E), 1:1000; S6 (Cell signaling, 5G10), 1:1000; pULK1 ser 757 (Cell signaling, D7O6U), 1:1000; ULK (Cell signaling, D8H5), 1:1000; LC3 (Cell signaling, #2775), 1:1000; β actin (Cell signaling, D6A8), 1:2000. The membranes, together with the primary antibodies, were incubated for 1 h at room temperature. After incubation, the membranes were washed five times with TBST. Then, antirabbit HRP at 1:3000 dilution (Cell signaling, #7074) was added. Five washes with TBST were performed to eliminate antibody excess. Images were obtained in ChemiDoc (BioRad, Hercules, CA, USA) and analyzed by Image Lab (BioRad, Hercules, CA, USA, version 6.1).
2.7. Statistical Analysis
Statistical analysis was performed through one- and two-way ANOVA and Bartlett’s post-analysis test, using GraphPad Prism software. The Student’s t-test was used for the bars, which represent standard deviations (SDs). Values of p < 0.05 were considered statistically significant. At least 2 independent experiments of n = 3 were conducted for each of the experimental processes.
3. Results
3.1. mTORC1 Activation by SopB Allows Salmonella Survival in B cells
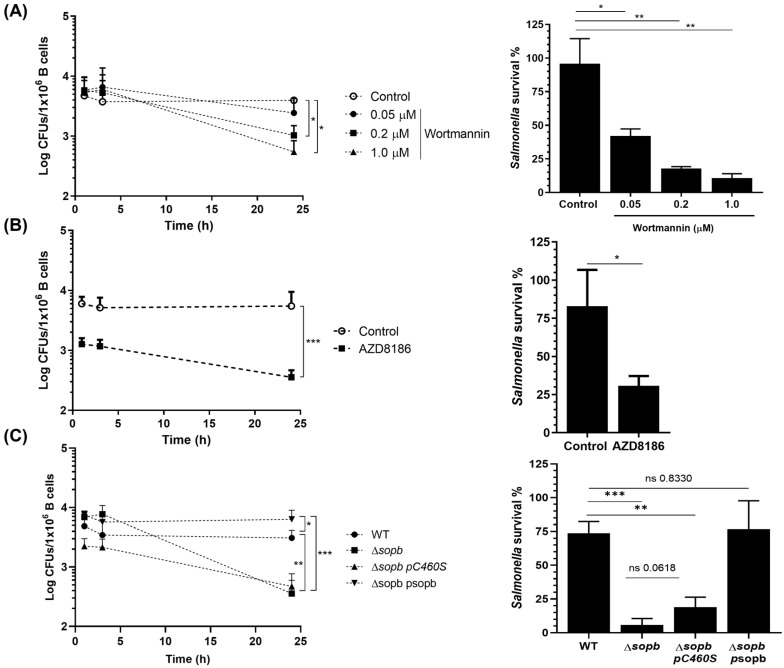
Salmonella activates the PI3K/Akt pathway during infection, and this activation allows Salmonella to inhibit pyroptosis in B cells, impeding the elimination of the bacteria. In these Salmonella-infected B cells, NLRP4 transcription and IL-1β production are inhibited. The pharmacological inhibition of PI3K or Akt, as well as the deletion of the rictor gene in B cells, is capable of rescuing the transcription of NLRP4 and IL-1β production, reflecting the control of Salmonella infection. These results suggest the possible activation of mTORC1 in Salmonella-infected B cells, blocking autophagy and avoiding the elimination of the bacteria [14,27,28]. Therefore, we considered whether, in addition to allowing the survival of B cells, PI3K/Akt activation participated in the inhibition of Salmonella infection control. For this purpose, we treated primary B cells with different concentrations of the PI3K class I inhibitor wortmannin during infection. The results showed that the control of Salmonella was proportional to PI3K inhibition by wortmannin (Figure 1A). We observed a similar result with AZD8186 (PI3K inhibitor), where B cells treated with this molecule substantially reduced their bacterial load (Figure 1B). None of the pharmacological inhibitors were toxic to B cells (Figure S2A) or Salmonella (Figure S2B) at the concentrations used. To corroborate the results obtained with the pharmacological inhibitors, we infected B cells with a Salmonella lacking the sopb gene (Salmonella Δsopb) or with another strain complemented with a form of SopB lacking its inositide phosphatase function (Salmonella Δsopb pC460S); both strains were incapable of activating the PI3K/Akt pathway. B cells infected with these mutant strains were able to control intracellular infections of Salmonella compared with B cells infected with Salmonella WT or with Salmonella Δsopb complemented with sopb WT (Salmonella Δsopb + psopb) (Figure 1C). Overall, these results showed that PI3K activation is essential for Salmonella survival in B cells.
Figure 1.
Class-I PI3K is needed for Salmonella survival in B cells. B cells were purified from the spleens of C57BL/6 mice and infected at a MOI of 50 with Salmonella. Subsequently, the cells were lysed and plated on LB Agar at the indicated times. (A) CFUs were recovered from infected B cells and treated 1 h before and during infection with the indicated concentrations of wortmannin or (B) treated with the PI3K class I inhibitor AZD8186 (500 nM). (C) B cells were infected at a MOI of 50 with Salmonella WT, Salmonella ∆sopb, Salmonella ∆sopb pC460S (phosphatase-inactive domain), or Salmonella ∆sopb psopb (WT SopB). Percentage of Salmonella survival in (A–C) was calculated by dividing CFUs recovered at 24 h between CFUs recovered at 1 h. Results are expressed as means ± SDs. n = 3. A two-way ANOVA test was used for multiple comparisons, and an unpaired Student’s t-test was used for bars. * p < 0.05, ** p < 0.01, and *** p < 0.001.
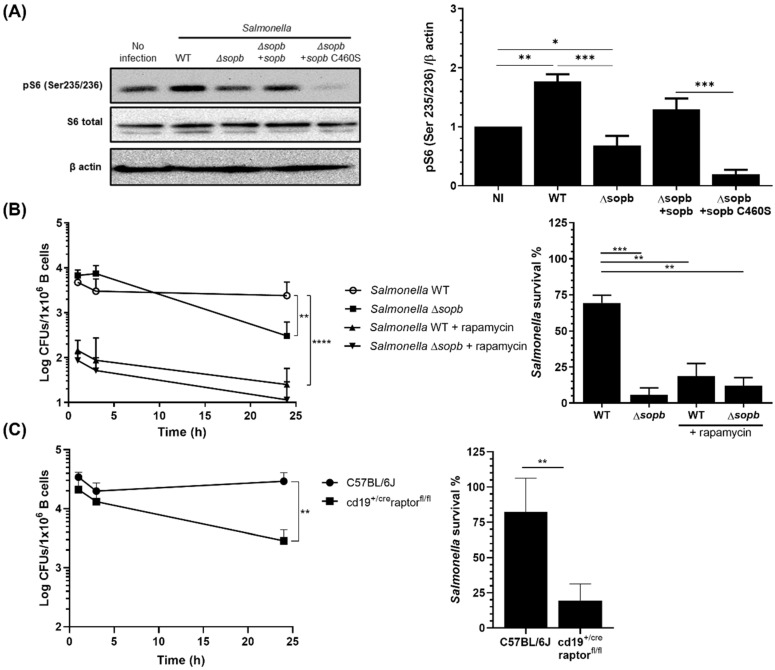
Since Salmonella induces the activation of the PI3K-Akt pathway in order to survive inside B cells, we evaluated whether Salmonella infection promotes the mTORC1 activation mediated by this pathway. For this purpose, we infected primary B cells for three hours with our different Salmonella strains; subsequently, we determined mTORC1 activation by measuring S6 protein phosphorylation. We observed an increase in pS6 in Salmonella WT-infected B cells compared with uninfected B cells. This increase did not occur in Salmonella Δsopb-infected B cells (Figure 2A). By infecting B lymphocytes with Salmonella Δsopb strains reconstituted with plasmids, as previously described, we determined that mTORC1 activation is mediated primarily by the inositide phosphatase function of SopB (Figure 2A). Once we determined that Salmonella activates mTORC1, we assessed whether this process is essential for Salmonella survival within B cells. For this purpose, we treated B lymphocytes with rapamycin (160 nM), an inhibitor of mTORC1. The rapamycin-treated B cells showed efficient control of Salmonella infection compared with the untreated B cells. Salmonella survival was affected in the presence of rapamycin in WT bacteria, as well as in the mutant (Δsopb) (Figure 2B). This was reflected in the formation of CFUs and in the percentage of survival. In addition to the decrease we observed in the bacterial load at 24 h in rapamycin-treated B lymphocytes, we observed a substantial decrease in the numbers of Salmonella at 1 h post-infection (Figure 2B). The bacterial effector was therefore necessary for the maintenance of the bacteria in B cells. To corroborate the results obtained with rapamycin, we infected splenic B cells lacking mTORC1 (cd19+/creraptorfl/fl) with Salmonella. The kinetics showed the effective control of Salmonella infection by B cells lacking mTORC1 compared with B cells from C57BL/6J mice (Figure 2C). These results are consistent with those obtained using rapamycin treatment. To reinforce the results obtained in vitro, as described above, cd19+/creraptorfl/fl mice were infected via orogastric inoculation with Salmonella WT GFP+. Preliminary results showed that cd19+/creraptorfl/fl mice had a lower bacterial load in the spleen and liver compared with WT mice. Additionally, when measuring the percentage of infection in mouse spleen B lymphocytes, a decrease in the percentage of CD19+ GFP+ cells was observed in cd19+/creraptorfl/fl mouse cells compared to what was seen in WT mouse cells (data not shown). Taking together, these results showed that Salmonella, through SopB, activates the mTORC1 complex, and that this activation allows Salmonella to survive intracellularly in B cells.
Figure 2.
SopB activates mTORC1 to promote the survival of Salmonella in B cells. (A) mTORC1 activation was measured by pS6 (S235/S236) levels in B cells infected at a MOI of 50 with different strains of Salmonella. Total levels of 6S are shown. Data were normalized based on loading control and non-infected B cells. (B) CFUs recovered from B cells treated or not with the mTOC1 inhibitor rapamycin (160 nM) and infected at a MOI of 50 with S. Typhimurium WT or ∆sopb. (C) CFUs recovered from C57BL/6J or cd19+/creraptorfl/fl (mTORC1 KO) mouse B cells infected with Salmonella WT for 24 h. The percentage of Salmonella survival in (B) and (C) was calculated by dividing CFUs recovered at 24 h between CFUs recovered at 1 h. Results are expressed as means ± SDs. n = 3. A two-way ANOVA test was used for multiple comparisons and an unpaired Student’s t-test was used for bars. * p < 0.05, ** p < 0.01, *** p < 0.001 and **** p < 0.0001.
3.2. SopB-Mediated Activation of mTORC1 Inhibits Autophagy in B Cells
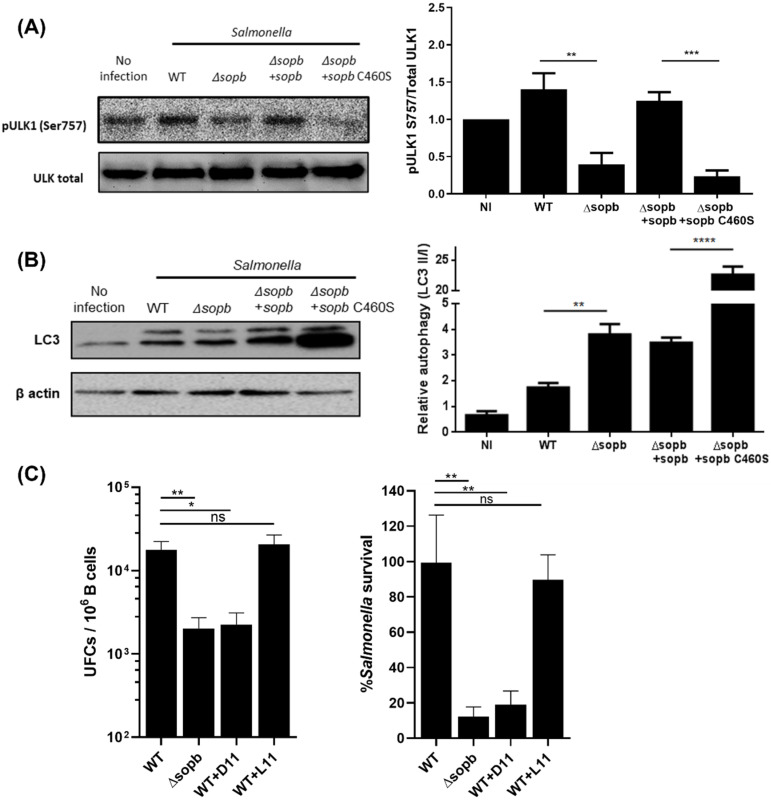
The PI3K/Akt/mTORC1 pathway is one of the central negative regulators of autophagy. Due to the fact that Salmonella activates and uses this pathway to survive in B cells, we evaluated whether Salmonella inhibits autophagy to promote its survival in B cells. For this purpose, we analyzed the phosphorylation of ULK1 Ser757; this phosphorylation is provided by mTORC1 and prevents autophagy initiation. Salmonella WT infection increased the levels of pULK1 Ser757 in B lymphocytes compared with uninfected cells. In contrast, Salmonella Δsopb infection did not induce this increase in pULK1 Ser757 (Figure 3A). Using reconstitution assays with psopb and psopb C460S plasmids, we determined that the inositide phosphatase function is responsible for the increase in pULK1 Ser757. We measured the LC3-II/LC3-I levels to corroborate the decrease in autophagy during Salmonella infection. The LC3-II/LC3-I levels showed a pattern similar to that of pULK1 Ser757; the autophagy levels decreased in B cells infected with Salmonella WT in contrast with the levels we observed in B cells infected with Salmonella Δsopb. Likewise, SopB, through its inositide phosphatase function, was mainly responsible for the observed effect (Figure 3B). The obtained results indicated that Salmonella inhibits autophagy in B cells. To determine whether this mechanism is essential for Salmonella survival, we treated infected B cells with D11, an autophagy-inducer peptide. Whereas untreated B cells were unable to control Salmonella infection, B cells treated with D11 efficiently controlled Salmonella WT, in a manner similar to that which we observed in B cells infected with Salmonella Δsopb. As expected, we observed a recuperation of the percentage of surviving bacteria when treated with L11, a scramble peptide for D11, up to the percentage observed in the survival of Salmonella WT (Figure 3C). This result demonstrated that B cells, through autophagy, control Salmonella infection; however, the bacteria are capable of surviving within B cells that inhibit autophagy.
Figure 3.
SopB-mediated activation of mTORC1 inhibits autophagy. Detection of pULK1 (S757) (A) or LC3-I/LC3-II (B) in B cells infected with indicated Salmonella strains for 3 h. (C) CFUs recovered from B cells infected with Salmonella strains for 24 h and treated for 1.5 h with autophagy-inducer peptide D11(20 μM) or scramble peptide L11 (20 μM). The percentage of Salmonella survival in (C) was calculated by considering Salmonella WT as 100% of survival. Results are expressed as means ± SDs. n = 3. An unpaired Student’s t-test was used for the bars. * p < 0.05, ** p < 0.01, *** p < 0.001, and **** p < 0.0001.
4. Discussion
The interplay between Salmonella and autophagy has been addressed mainly in HeLa cells and macrophages [28,29,30,31,32]. However, the mechanism Salmonella uses during infection of target B cells and the mechanisms that allow the survival of this bacterium in B cells have not been addressed in depth.
Here, we have shown, for the first time, that the Salmonella effector protein SopB activates mTORC1 and inhibits autophagy by phosphorylating ULK1 at its Ser757. The activation of this pathway facilitates Salmonella survival in B cells. The inhibition of autophagy in Salmonella-infected B cells contrasts with the findings reported for epithelial cells, where Salmonella proliferation is controlled by autophagy [33]. In HeLa cells, Salmonella is labeled by NDP52 and recruited to autophagosomes by galectin 8 (GAL8). Similarly, in macrophages, compartments containing Salmonella are labeled by LC3. In both cases, these labels favor bacteria control by autophagy [34,35]. The accumulation of LC3-II levels, as shown in Figure 3A, resembles what is observed in cells treated with chloroquine (CQ) and bafilomycin A (BafA). These molecules impair the function of lysosomes [33,34]. SopB might also block lysosome function; nevertheless, Salmonella-infected B cells are capable of completing the autophagy process when treated with autophagy inductor D11, thus controlling infection. The pULK1 levels were not statistically different in Salmonella WT-infected B cells compared with those observed in Salmonella-complemented strain-infected lymphocytes (Figure 3B). These results contrast with our observation that levels of the LC3-II/LC3-I ratio differ between the two groups of cells infected either with the Salmonella ΔSopB complemented strain or Salmonella WT. Other bacterial effectors likely participate in infected B cells along the autophagy pathway.
The activation of the PI3K/Akt/mTORC1 pathway by Salmonella was previously reported in macrophages. However, the bacterial effector responsible for such effects was not reported [29]. The hypothesis that SopB in B cells is responsible for the activation of the PI3K/Akt/mTORC1 pathway is supported both by previous reports [13,14] and by the actual results obtained in SopB-complemented assays, in which the SopB inositide phosphatase function was found to be responsible for the activation of this signaling pathway (Figure 2 and Figure 3). This can occur in infected B cells as well as in neighboring B cells, as previously described for the downregulation of NLRC4 levels [13] and the accumulation of PIP3 in the cytoplasmic membrane [14], which is observed in infected and noninfected B cells.
B cells substantially increased autophagy levels in response to Salmonella Δsopb or Salmonella Δsopb pC460S infection (Figure 3). These results were probably due to AMPK activation being promoted by the decrease in cytoplasmic amino acid concentration, in a manner similar to that which was observed in Salmonella-infected HeLa cells [35]. In Salmonella-infected B cells, autophagy was blocked due to the SopB-mediated activation of mTORC1, causing the infected cells to maintain levels similar to those of uninfected B cells (Figure 3). Since autophagy is an essential process for maintaining cell homeostasis, autophagy levels during infection that remain close to those observed for basal levels may favor the functional maintenance of B cells and prevent their death.
Although the data suggested that, in B cells, SopB is mainly responsible for blocking autophagy, in other cell lines, other bacterial effectors triggered this phenomenon, as is the case for the macrophage cell line J774A.1, in which the phosphothreonine lyase spvC is responsible for inhibiting autophagy [28]. This result suggested that Salmonella possess several mechanisms that allow modification to mammalian cell biology and adapt according to host cell lineage.
As one of the consequences of mTORC1 activation, we observed phosphorylation of ULK1 at Ser757 and thus blocking of autophagy (Figure 2 and Figure 3). However, due to the high number of signaling pathways impacted by mTORC1, we considered that SopB may be modifying other signaling pathways, as well as the metabolic state of B cells, thereby favoring the establishment of appropriate modifications in B cells, permitting them to become promising niches for Salmonella.
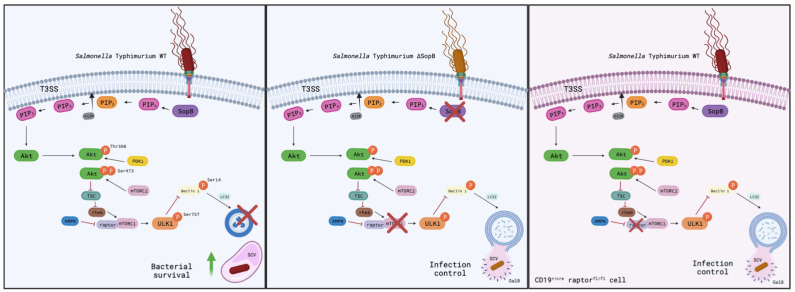
Our results suggested that B lymphocytes may be important niches in which Salmonella remains viable long enough to achieve a persistent infection and invade other types of tissues. Evaluating the function of Salmonella-infected B cells with the objective of better understanding the likely effect on antibody production would be interesting. Overall, our results demonstrated that Salmonella survival within B cells depends on the inhibition of autophagy by mTORC1 activation (Figure 4).
Figure 4.
Salmonella promotes its survival in B cells through SopB-mediated autophagy inhibition. During B cell infection, Salmonella translocate SopB, which mediates, through its inositide phosphatase domain, the induction of the activation of PI3K/Akt/mTORC1 pathway. As a result of mTORC1 activation, ULK1 is phosphorylated at its ser 757, inhibiting the autophagy process and allowing the survival of Salmonella in these cells (left). In the absence of SopB, Salmonella is unable to activate the PI3K/Akt/mTORC1 pathway, permitting increased levels of autophagy (including the fusion of the autophagosome with the Salmonella-containing vacuole “SCV” marked with galectin-8 for its recognition) and the control of the bacterium (center). This last phenomenon can be seen in cd19+/cre raptorfl/fl (mTORC1 KO) mice, where the absence of the protein raptor disables the formation of the mTORC1 complex, thus inhibiting the autophagy process.
Acknowledgments
We thank Olivia Steele-Mortimer, National Institute of Health, for the generous donation of pSopB and pSopB-C460S plasmids; Victor Manuel Garcia-Gomez and Felipe Cruz-Martinez at UPEAL-CINVESTAV for support with mouse breeding and supervision; and Benjamin Ortiz-Lopez for his support in the Western blotting.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/cells11132061/s1, Figure S1: Purified B lymphocytes by MACs and Salmonella infected purified B cells; Figure S2: Pharmacological inhibitors do not affect the viability of B cells or Salmonella; Figure S3: Characterization of cd19+/creraptorfl/fl mice.
Author Contributions
O.-N.V. and G.-G.A. conceived the original idea. L.-B.L., G.-E.C. and G.-T.A. carried out the experiments. E.-G.I. and M.-L.M. analyzed the data. All authors provided critical feedback and helped shape the research, analysis, and manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The experiments in the present study were conducted according to the guidelines of the Official Mexican Norm NOM-062-ZOO-1999. In addition, the project protocol was approved by the Committee for Laboratory Animal Care of the Center of Research and Advanced Studies (CICUAL-CINVESTAV) under approval number 0078-14.
Informed Consent Statement
Not applicable.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflict of interest.
Funding Statement
The present work was supported by the Consejo Nacional de Ciencia y Tecnología CF-2019-21082 to V.O., CVU 764829 to L.-B.L., and CVU 1078873 to G.-T.A.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Haraga A., Ohlson M.B., Miller S.I. Salmonellae interplay with host cells. Nat. Rev. Microbiol. 2008;6:53–66. doi: 10.1038/nrmicro1788. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Drug Resistant Nontyphoidal Salmonella. [(accessed on 8 December 2021)];2019 :2. Available online: www.wou.edu/las/natsci_math/biology/boomer/Bio440/emerging2002/Salmonella2.
- 3.Levine M.M., Black R., Lanata C. Precise Estimation of the Numbers of Chronic Carriers of Salmonella typhi in Santiago, Chile, an Endemic Area. J. Infect. Dis. 1982;146:724–726. doi: 10.1093/infdis/146.6.724. [DOI] [PubMed] [Google Scholar]
- 4.Hornick R.B., Greisman S.E., Woodward T.E., DuPont H.L., Dawkins A.T., Snyder M.J. Typhoid Fever: Pathogenesis and Immunologic Control. N. Engl. J. Med. 1970;283:686–691. doi: 10.1056/NEJM197009242831306. [DOI] [PubMed] [Google Scholar]
- 5.Dongol S., Thompson C.N., Clare S., Nga T.V.T., Duy P.T., Karkey A., Arjyal A., Koirala S., Khatri N.S., Maskey P., et al. The Microbiological and Clinical Characteristics of Invasive Salmonella in Gallbladders from Cholecystectomy Patients in Kathmandu, Nepal. PLoS ONE. 2012;7:e47342. doi: 10.1371/journal.pone.0047342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brigo N., Pfeifhofer-Obermair C., Tymoszuk P., Demetz E., Engl S., Barros-Pinkelnig M., Dichtl S., Fischer C., Valente De Souza L., Petzer V., et al. Cytokine-Mediated Regulation of ARG1 in Macrophages and Its Impact on the Control of Salmonella enterica Serovar Typhimurium Infection. Cells. 2021;10:1823. doi: 10.3390/cells10071823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosales-Reyes R., Alpuche-Aranda C., Ramírez-Aguilar M.D.L.L., Castro-Eguiluz A.D., Ortiz-Navarrete V. Survival of Salmonella enterica Serovar Typhimurium within Late Endosomal-Lysosomal Compartments of B Lymphocytes Is Associated with the Inability To Use the Vacuolar Alternative Major Histocompatibility Complex Class I Antigen-Processing Pathway. Infect. Immun. 2005;73:3937–3944. doi: 10.1128/IAI.73.7.3937-3944.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Castro-Eguiluz D., Pelayo R., Rosales-Garcia V., Rosales-Reyes R., Alpuche-Aranda C., Ortiz-Navarrete V. B cell precursors are targets for Salmonella infection. Microb. Pathog. 2009;47:52–56. doi: 10.1016/j.micpath.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Alvarez M.I., Glover L.C., Luo P., Wang L., Theusch E., Oehlers S.H., Walton E.M., Tram T.T.B., Kuang Y.-L., Rotter J.I., et al. Human genetic variation in VAC14 regulates Salmonella invasion and typhoid fever through modulation of cholesterol. Proc. Natl. Acad. Sci. USA. 2017;114:E7746–E7755. doi: 10.1073/pnas.1706070114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel J.C., Galán J.E. Differential activation and function of Rho GTPases during Salmonella–host cell interactions. J. Cell Biol. 2006;175:453–463. doi: 10.1083/jcb.200605144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burkinshaw B.J., Prehna G., Worrall L.J., Strynadka N.C. Structure of Salmonella Effector Protein SopB N-terminal Domain in Complex with Host Rho GTPase Cdc42. J. Biol. Chem. 2012;287:13348–13355. doi: 10.1074/jbc.M111.331330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Knodler L., Finlay B.B., Steele-Mortimer O. The Salmonella Effector Protein SopB Protects Epithelial Cells from Apoptosis by Sustained Activation of Akt. J. Biol. Chem. 2005;280:9058–9064. doi: 10.1074/jbc.M412588200. [DOI] [PubMed] [Google Scholar]
- 13.Perez-Lopez A., Rosales-Reyes R., Alpuche-Aranda C.M., Ortiz-Navarrete V. Salmonella Downregulates Nod-like Receptor Family CARD Domain Containing Protein 4 Expression To Promote Its Survival in B Cells by Preventing Inflammasome Activation and Cell Death. J. Immunol. 2013;190:1201–1209. doi: 10.4049/jimmunol.1200415. [DOI] [PubMed] [Google Scholar]
- 14.García-Gil A., Galán-Enríquez C.S., Pérez-López A., Nava P., Alpuche-Aranda C., Ortiz-Navarrete V. SopB activates the Akt-YAP pathway to promote Salmonella survival within B cells. Virulence. 2018;9:1390–1402. doi: 10.1080/21505594.2018.1509664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Castrejón-Jiménez N.S., Leyva-Paredes K., Hernández-González J.C., Luna-Herrera J., García-Pérez B.E. The role of autophagy in bacterial infections. Biosci. Trends. 2015;9:149–159. doi: 10.5582/bst.2015.01035. [DOI] [PubMed] [Google Scholar]
- 16.Ogawa M., Yoshimori T., Suzuki T., Sagara H., Mizushima N., Sasakawa C. Escape of Intracellular Shigella from Autophagy. Science. 2005;307:727–731. doi: 10.1126/science.1106036. [DOI] [PubMed] [Google Scholar]
- 17.Kim J., Kundu M., Viollet B., Guan K.-L. AMPK and mTOR regulate autophagy through direct phosphorylation of Ulk1. Nat. Cell Biol. 2011;13:132–141. doi: 10.1038/ncb2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Starokadomskyy P., Dmytruk K.V. A bird’s-eye view of autophagy. Autophagy. 2013;9:1121–1126. doi: 10.4161/auto.24544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meley D., Bauvy C., Houben-Weerts J.H., Dubbelhuis P.F., Helmond M.T., Codogno P., Meijer A.J. AMP-activated Protein Kinase and the Regulation of Autophagic Proteolysis. J. Biol. Chem. 2006;281:34870–34879. doi: 10.1074/jbc.M605488200. [DOI] [PubMed] [Google Scholar]
- 20.Zhu Y.P., Brown J.R., Sag D., Zhang L., Suttles J. Adenosine 5′-Monophosphate–Activated Protein Kinase Regulates IL-10–Mediated Anti-Inflammatory Signaling Pathways in Macrophages. J. Immunol. 2014;194:584–594. doi: 10.4049/jimmunol.1401024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Birmingham C.L., Canadien V., Kaniuk N.A., Steinberg B.E., Higgins D.E., Brumell J.H. Listeriolysin O allows Listeria monocytogenes replication in macrophage vacuoles. Nature. 2008;451:350–354. doi: 10.1038/nature06479. [DOI] [PubMed] [Google Scholar]
- 22.Huang D., Bao L. Mycobacterium tuberculosis EspB protein suppresses interferon-γ-induced autophagy in murine macrophages. J. Microbiol. Immunol. Infect. 2015;49:859–865. doi: 10.1016/j.jmii.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 23.Kayath C.A., Hussey S., El Hajjami N., Nagra K., Philpott D., Allaoui A. Escape of intracellular Shigella from autophagy requires binding to cholesterol through the type III effector, IcsB. Microbes Infect. 2010;12:956–966. doi: 10.1016/j.micinf.2010.06.006. [DOI] [PubMed] [Google Scholar]
- 24.Miao E., Brittnacher M., Haraga A., Jeng R.L., Welch M.D., Miller S.I. Salmonella effectors translocated across the vacuolar membrane interact with the actin cytoskeleton. Mol. Microbiol. 2003;48:401–415. doi: 10.1046/j.1365-2958.2003.t01-1-03456.x. [DOI] [PubMed] [Google Scholar]
- 25.Knodler L.A., Winfree S., Drecktrah D., Ireland R., Steele-Mortimer O. Ubiquitination of the bacterial inositol phosphatase, SopB, regulates its biological activity at the plasma membrane. Cell. Microbiol. 2009;11:1652–1670. doi: 10.1111/j.1462-5822.2009.01356.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Finn C.E., Chong A., Cooper K.G., Starr T., Steele-Mortimer O. A second wave of Salmonella T3SS1 activity prolongs the lifespan of infected epithelial cells. PLOS Pathog. 2017;13:e1006354. doi: 10.1371/journal.ppat.1006354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosales-Reyes R., Pérez-López A., Sánchez-Gómez C., Hernández-Mote R.R., Castro-Eguiluz D., Ortiz-Navarrete V., Alpuche-Aranda C.M. Salmonella infects B cells by macropinocytosis and formation of spacious phagosomes but does not induce pyroptosis in favor of its survival. Microb. Pathog. 2012;52:367–374. doi: 10.1016/j.micpath.2012.03.007. [DOI] [PubMed] [Google Scholar]
- 28.Zhou L., Li Y., Gao S., Yuan H., Zuo L., Wu C., Huang R., Wu S. Salmonella spvC Gene Inhibits Autophagy of Host Cells and Suppresses NLRP3 as Well as NLRC4. Front. Immunol. 2021;12 doi: 10.3389/fimmu.2021.639019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Owen K.A., Meyer C.B., Bouton A.H., Casanova J.E. Activation of Focal Adhesion Kinase by Salmonella Suppresses Autophagy via an Akt/mTOR Signaling Pathway and Promotes Bacterial Survival in Macrophages. PLOS Pathog. 2014;10:e1004159. doi: 10.1371/journal.ppat.1004159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Scheidel J., Amstein L., Ackermann J., Dikic I., Koch I. In Silico Knockout Studies of Xenophagic Capturing of Salmonella. PLOS Comput. Biol. 2016;12:e1005200. doi: 10.1371/journal.pcbi.1005200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kreibich S., Emmenlauer M., Fredlund J., Rämö P., Münz C., Dehio C., Enninga J., Hardt W.-D. Autophagy Proteins Promote Repair of Endosomal Membranes Damaged by the Salmonella Type Three Secretion System 1. Cell Host Microbe. 2015;18:527–537. doi: 10.1016/j.chom.2015.10.015. [DOI] [PubMed] [Google Scholar]
- 32.Cemma M., Kim P.K., Brumell J.H. The ubiquitin-binding adaptor proteins p62/SQSTM1 and NDP52 are recruited independently to bacteria-associated microdomains to target Salmonella to the autophagy pathway. Autophagy. 2011;7:341–345. doi: 10.4161/auto.7.3.14046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mauthe M., Orhon I., Rocchi C., Zhou X., Luhr M., Hijlkema K.-J., Coppes R.P., Engedal N., Mari M., Reggiori F. Chloroquine inhibits autophagic flux by decreasing autophagosome-lysosome fusion. Autophagy. 2018;14:1435–1455. doi: 10.1080/15548627.2018.1474314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fedele A.O., Proud C.G. Chloroquine and bafilomycin A mimic lysosomal storage disorders and impair mTORC1 signalling. Biosci. Rep. 2020;40:BSR20200905. doi: 10.1042/BSR20200905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tattoli I., Sorbara M.T., Vuckovic D., Ling A., Soares F., Carneiro L., Yang C., Emili A., Philpott D.J., Girardin S.E. Amino Acid Starvation Induced by Invasive Bacterial Pathogens Triggers an Innate Host Defense Program. Cell Host Microbe. 2012;11:563–575. doi: 10.1016/j.chom.2012.04.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.