Abstract
In the last decades, personalized medicine has been increasing its presence in different fields of medicine, including ophthalmology. A new factor that can help us direct medicine towards the challenge of personalized treatments is the microbiome. The gut microbiome plays an important role in controlling immune response, and dysbiosis has been associated with immune-mediated diseases such as non-infectious uveitis (NIU). In this review, we gather the published evidence, both in the pre-clinical and clinical studies, that support the possible role of intestinal dysbiosis in the pathogenesis of NIU, as well as the modulation of the gut microbiota as a new possible therapeutic target. We describe the different mechanisms that have been proposed to involve dysbiosis in the causality of NIU, as well as the potential pharmacological tools that could be used to modify the microbiome (dietary supplementation, antibiotics, fecal microbiota transplantation, immunomodulators, or biologic drugs) and, consequently, in the control of the NIU. Furthermore, there is increasing scientific evidence suggesting that the treatment with anti-TNF not only restores the composition of the gut microbiota but also that the study of the composition of the gut microbiome will help predict the response of each patient to anti-TNF treatment.
Keywords: non-infectious uveitis (NIU), immune-mediated disease, gut microbiota, intestinal microbiome, ocular microbiome, microbiota modulation
1. Introduction
Uveitis encompasses a heterogeneous group of intraocular inflammatory diseases consisting of inflammation of the uveal tract. This can affect adjacent structures such as the retina or optic nerve. They are classified according to their etiology into infectious and non-infectious, with the latter being related, in most cases, to immune-mediated diseases. The origin of this inflammation can be attributed to an endogenous mechanism, either as part of a systemic disease (sarcoidosis, Ankylosing spondylitis (AS), Behçet Disease (BD), multiple sclerosis (MS), Vogt-Koyanagi-Harada syndrome (VKH), etc.) or in isolated ocular (such as Birdshot disease) [1]. The exact pathogenic mechanism of immune-mediated uveitis is not yet known; although an imbalance has been observed between autoreactive effector T cells (Th1 and Th17) involved in effector and pathogenic functions and regulatory T cells (Treg), involved in immunomodulatory functions (tolerance) [2,3]. Pro-inflammatory cytokines play a fundamental role in all these pathophysiological mechanisms. Elevated levels of interleukin-6 (IL-6), IL-17, IL-23, or tumor necrosis factor-alpha (TNF α) have been detected at higher concentrations in the blood and/or ocular fluids of patients with uveitis of various etiologies; and most therapeutic targets in recent decades have involved these cytokine pathways [4]. Chronic or recurrent inflammation and tissue damage may result from an exaggerated host immune response, and the microbiome may be a significant source of antigens and antigen-specific T cells.
The intestinal microbiota is the most abundant in humans and is composed of approximately 1014 microorganisms whose genomes constitute 100 times the size of the human genome [5]. The most frequent phyla, both in adult humans and in mice, are Firmicutes and Bacteroidetes, followed by Actinobacteria and Proteobacteria, while the least represented are the Fusobacteria and Verrucomicrobia [6]. Its composition is established at birth by maternal transmission and constantly changes to maintain homeostatic balance with the host’s immune system [7]. It is possible that diet is the environmental factor with the greatest influence [8], although it is also affected by chronic stress, circadian rhythm, exposure to medications, toxins, colonization by other external microorganisms, and different diseases [9,10]. The intestinal microbiota plays an important role in many physiological functions, and its function as a regulator of the immune system, modulating innate and adaptive responses have gained importance in recent years [11]. The alteration of the intestinal microbiota compared to what we consider a healthy and diverse microbiota is known as dysbiosis [12]. This may alter the homeostatic immune state and induce diseases [9].
Chronic or recurrent uveitis can be caused by local reactivations of persistent microbial agents or inadequately cleared antigens, which may intermittently break the proportion of T cells. Experimental data have demonstrated the crucial role of the gut microbiome in controlling both the innate and adaptive immune response, linking dysbiosis to immune-mediated diseases [13]. Some bacterial strains such as segmented filamentous bacteria promote the differentiation of Th17 in the gut. They have been associated with immune-mediated diseases such as non-infectious uveitis (NIU). On the contrary, other bacterial species such as some types of Clostridia and the species Bacteroides Fragilis are usually part of the commensal microbiota, promote the differentiation of Treg, and contribute to immune homeostasis [4]. Most current theories about the relationship between the microbiota and the immune system in the pathogenesis of the NIU are extraocular in nature, although recent studies suggest the presence of a previously unrecognized intraocular microbiome, which opens a new research path [14]. In recent years, based on experimental studies with animal and clinical models, a relationship between the intestinal microbiota and uveitis has become gradually established [1]. This relationship may predispose or even be the origin of uveitogenic or adjuvant pathogens [15]. In addition, the fact that all immunosuppressive drugs have been shown to have intrinsic antimicrobial activity, together with the effect of immunosuppression on the intestinal microbiota, and inflammatory diseases, supports this relationship between the intestinal microbiota and the NIU [16]. The identification of the causal or protective species would allow us to initiate new lines of research focused on the modification of the microbiota as a therapeutic possibility in immune-mediated uveitis.
This review gathers published evidence on the association between microbiota and uveitis, both in the pre-clinical and clinical fields. In the publications, the different mechanisms by which intestinal dysbiosis could participate in the pathogenesis of the NIU are described, as well as the potential treatments aimed at modulating the intestinal microbiota that could be used and/or interfere positively or negatively in its treatment.
2. Mechanisms of Microbial Pathogenesis and Uveitis
Growing clinical and pre-clinical evidence points to the microbiome and dysbiosis in the immune response and susceptibility to systemic diseases, including both those of gastrointestinal origin such as Inflammatory bowel disease (IBD), and those of another origin [17]. It has also been implicated in the neurodevelopment and function of the central nervous system (CNS), through a bidirectional connection known as the “gut-brain axis” whose communication is regulated by the microbiota [18]; thus associating it with mental health (anxiety, depression), neurological diseases (Alzheimer’s disease, Parkinson’s disease…) and aging [18,19,20]. More and more studies are now focusing their attention towards understanding the relationship between the microbiota and immune-mediated diseases that occur with uveitis, such as Behçet’s disease (BD) [21,22], AS [23], or Vogt-Koyanagi-Harada syndrome [24]. The decrease in the diversity of the microbiome has been linked in the literature to multiple diseases, such as IBD and AS, which are present from pediatric stages of life, suggesting that this dysbiosis may be associated with a genetic predisposition and is not only an effect, but also contributes to the pathogenesis of the disease [23,25].
NIUs target the neuroretina, considered a part of the CNS. In addition to NIUs, multiple eye conditions have recently been linked to intestinal dysbiosis, such as diabetic retinopathy (DR), age-related macular degeneration (AMD), and glaucoma [26,27,28,29]. Many studies have shown the potential role of micronutrient supplementation in slowing down AMD progression, as well as animal models proved systemic inflammation induced by diet and dysbiosis, contributing to AMD development [28]. This suggests the existence of a “gut-retinal axis”, yet to know if as a part of the “gut-brain axis” or as an independent bidirectional communication [1].
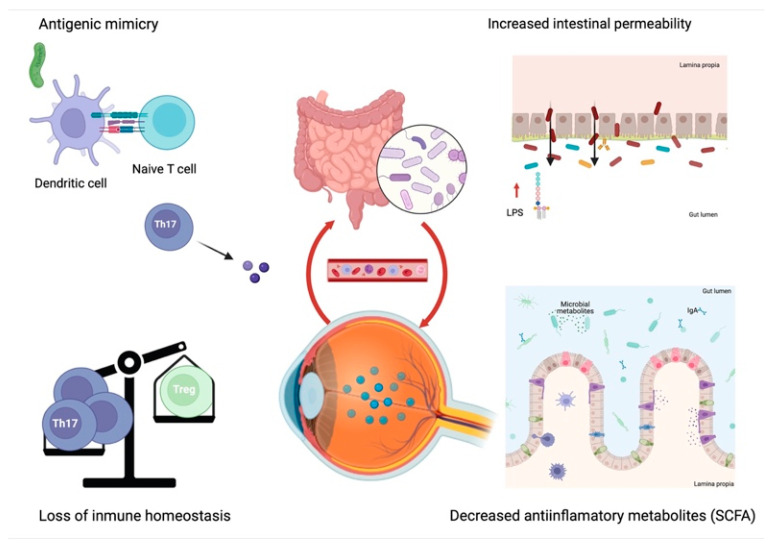
Interest in the study of the role of the microbiota in the development of NIU has been increasing in recent years, with several recent publications appearing that support its causality [15]. Dysbiosis participates in the pathogenesis of uveitis through four non-mutually exclusive mechanisms [30]: antigenic or molecular mimicry, the destruction of the intestinal barrier due to increased intestinal permeability, the loss of immune intestinal homeostasis, and the reduction of the production of beneficial anti-inflammatory metabolites (Figure 1).
Figure 1.
Mechanisms by which dysbiosis can participate in the pathogenesis of uveitis. Created with BioRender.com.
2.1. Antigenic or Molecular Mimicry
Antigenic mimicry is an important autoimmunity mechanism in which autoreactive T cells are generated by cross-reactivity of microbial peptides with autoantigens [31]. The pathogenesis of diseases associated with human leukocyte antigen-B27 (HLA-B27), including uveitis, has thus been related to a wide variety of peptides derived from microorganisms that show a high affinity for this molecule [32], including the species Chlamydia trachomatis and Campylobacter jejuni and the genera Klebsiella, Salmonella, Yersinia and Shigella [33,34]. Experimental studies in mice with spontaneous experimental autoimmune uveitis (EAU) have demonstrated this pathogenic mechanism [35]. Elimination of the microbial community by administration of broad-spectrum oral antibiotics attenuates the severity of uveitis and reduces intestinal Th17 activation, while the transfer of T cells from a transgenic mouse grown with microbiota induces uveitis in wildtype mice [35].
2.2. Increased Intestinal Permeability
Inflammation of the mucosa caused by intestinal dysbiosis destroys the intestinal barrier, causing an increase in permeability and favors the translocation of microbiota or its products to the blood, lymphatic, submucosal, and lamina propria circulations. These products, such as lipopolysaccharides (LPS) and β-glucan, would reach different tissues through the vascular system, directly causing inflammation in target organs, and reaching the uvea and synovial tissue [32,36,37]. Experimental studies in mice with EAU demonstrated the relationship between the increase in intestinal permeability with uveitis. Janowitz et al. [38] studied intestinal changes in mice with EAU by immunization with inter-photoreceptor retinoid-binding protein (IRBP)161–180 peptide plus killed Mycobacterium tuberculosis (MTB) antigen as an adjuvant, whereas mice immunized with MTB alone or in combination with an irrelevant IRBP peptide that did not develop ocular inflammation were used as controls. An increased intestinal permeability was observed in IRBP-immunized mice through assessment of ZO-1 expression and a FITC-dextran assay. Both IRBP and MTB mice exhibited increased permeability compared to non-immunized mice, an increase that was more evident in IRBP-immunized mice. In contrast, only IRBP-immunized mice had increased permeability in the FITC-dextran assay that paralleled the course of uveitis. In addition, the increase in intestinal permeability coincided with changes in intestinal microbiota. Linear discriminant analysis of Effect Size (LEfSe) revealed an increased abundance in Clostridium and S24-7 bacteria, but depletion in Verrucomicrobia, Akkermansia, Dorea, and other bacteria in uveitic mice compared to MTB control mice. Interestingly, these differences were more marked at the peak of uveitis, with increased Prevotella, Lactobacilli, Anaeroplasma, Parabacteroides, and Clostridium species in IRB-immunized mice, while Ruminococcus, Bacteroidia, S24-7, Proteobacteria, and Desulfovibrio were more abundant in MTB control mice. Furthermore, the degree of intestinal inflammation correlated with the severity of uveitis [38]. Therefore, intestinal permeability alteration may start at the onset of uveitis and becomes more intense with the progression of ocular inflammation accompanied by preceding dysbiosis to the outbreak of ocular inflammation [38].
2.3. Loss of Intestinal Immune Homeostasis
As previously described, T cells play an important role in the pathogenesis of autoimmunity. In conditions of dysbiosis there is a loss of intestinal homeostasis, which breaks the balance between Th17 and Treg, and leads to immune activation by increasing Th17 (and IL-17) and decreasing Treg (and IL-10); thus, causing inflammation [39,40]. This theory has been supported by studies in mice with induced EAU, showing that the administration of broad-spectrum oral antibiotics modifies the composition of the microbiota by reducing Firmicutes and Bacteroidetes phyla and Alphaproteobacteria class, and increasing Gammaproteobacteria class, and reducing the severity of uveitis by increasing the proportion of Treg in various lymphoid tissues and the eye [41]. In addition, the existence of migration of immune cells from the intestine to the eye has been proposed, since T cells of intestinal origin have been detected in the eye in mouse models with EAU [42].
2.4. Reduction of Anti-Inflammatory Microbial Metabolites
It is estimated that gut microbes produce thousands of metabolites that can regulate immune responses. The most common metabolites are short-chain fatty acids (SCFAs): butyrate, propionate, and acetate. These are metabolites obtained by the colonic microbiota through the fermentation of dietary fiber. These beneficial and protective metabolites have previously been studied in other inflammatory autoimmune diseases, such as HLA-B27-associated spondyloarthropathy [43]. This theory has also been demonstrated in experimental studies with mice with EAU in which the severity of uveitis decreased with exogenous supplementation of SCFAs [42,44]. These can reduce inflammation by inducing and increasing Treg cells in the intestinal lamina propria and lymph nodes, as well as suppressing effector T cells and decreasing their transport between the intestine and spleen [42].
3. Microbial Dysbiosis and Uveitis
Recent advances have made it possible to sequence the microbiome present in the human cornea and conjunctiva [45]. These have a different composition and a lower density of microorganisms than in the intestinal microbiome, but also with potential inflammatory regulation functions. An association between the ocular surface microbiome and the tear proteome has also been demonstrated [46]. The composition of the flora of the ocular surface differs according to the collection and research methods used, both due to the differences between the microbiome and the microbiota, and because of the difficulties of metagenomic sequencing (small sample size, contamination due to difficulty of the technique, etc.). In addition, the microbiome of the normal ocular surface varies with age, sex, environment, and diet, and can be altered by the use of therapies on the ocular surface (such as topical drugs or excessive use of contact lenses) [47], by chronic diseases such as diabetes or BD [48], and by systemic treatments such as the use of oral antibiotics [49]. Despite the difficulty in establishing a reference state, the literature agrees that the predominant genera on the healthy ocular surface are Corynebacterium, Propionibacterium, and Staphylococcus [50]. The mucosa of the ocular surface, being in direct contact with the environment, serves as a defense against the colonization of potentially pathogenic microbial species. The ocular microbiome influences ocular homeostasis, and it has been shown that the alteration of normal commensal flora induced by pathological states or antibiotics can cause an imbalance in favor of pathogenic species, increasing the risk of infections or ocular neoplasms [51].
The inside of the eye contains multiple immune system cells and inflammatory mediators, but the immune privilege of the eyeball prevents intraocular inflammation through mechanisms of immune ignorance and immune tolerance [52]. Despite the sterility “per se” of the interior of the anterior chamber, recent studies suggest the presence of a still unknown microbiome [14] that could modulate intraocular inflammatory responses. Nonetheless, this is for now still controversial. The aqueous humor microbiome has not been examined in patients with recurrent acute anterior uveitis (AAU). The study of the presence of microorganisms in aqueous humor during acute attacks of AAU could reveal important information related to the immunological and microbial mechanisms underlying this inflammatory disease [33].
Changes in the composition of the microbiota of the ocular surface have been found in pathologies such as blepharitis, trachoma, and dry eye [47]. In more detail, patients with blepharitis exhibited an increased abundance in Staphylococcus, Streptophyta, Corynebacterium, Enhydrobacter, and a decrease of Propionibacterium; patients with trachoma presented lower bacterial diversity and increased Corynebacterium and Streptococcus, while patients with dry eye syndrome had increased Staphylococcus aureus, Corynebacterium, Propionibacterium, Rhodococcus and Klebsiella oxytoca, the two latter considered as potential pathogens [47]. Furthermore, a relationship between ocular and non-ocular microbiome in retinal diseases, such as AMD, DR, or glaucoma, as well as uveitis has been suggested. Neither uveitis nor the rest of the subsequent diseases of the eye have been related to the ocular microbiome to date; due to the lack of studies [53]. However, there are several studies that show the relationship between the intestinal microbiota and NIUs both clinically and pre-clinically:
3.1. Pre-Clinical Studies
The involvement of the microbiota in the development of uveitis is based, fundamentally, on the EAU model induced by active immunization with external retinal antigen “inter-photoreceptor retinoid-binding protein” (IRBP) [41,54] and the spontaneous EAU model of a transgenic mouse that expresses the self-reactive T cell receptor (TCR) of [35,55]. Pre-clinical studies in which the causality of uveitis is related to the microbiota, as well as different therapeutic strategies for its modulation, are described in Table 1.
Table 1.
Pre-clinical studies with experimental autoimmune uveitis (EAU).
| Authors | Study Type | Modulation–Intervention | Findings | |
|---|---|---|---|---|
|
Horai et al., 2015 [35] |
Experimental Spontaneous EAU |
Decreased bacterial load of the microbiota |
|
|
| Zárate-Baldés et al., 2017 [55] | Experimental Spontaneous EAU |
|
|
|
| Nakamura et al., 2016 [41] | Experimental Induced EAU |
|
|
|
| Heissigerova et al., 2016 [54] | Experimental Induced EAU |
|
|
|
| Dusek et al., 2020 [56] | Experimental Induced EAU | Supplementation with probiotics |
|
|
| Kim et al., 2017 [57] | Experimental Induced EAU |
|
|
|
| Chen et al., 2017 [44] | Experimental EAU | Supplementation with prebiotics |
|
|
| Nakamura et al., 2017 [42] | Experimental Induced EAU |
|
|
|
IRBP: inter-photoreceptor retinoid-binding protein. EcN: Escherichia coli Nissle 1917. EcO: Escherichia coli O83:K24:H31.
The absence of microbiota in “germ-free” mice or the decrease in bacterial load prior to disease induction by administration of oral antibiotics has been shown to significantly attenuate the susceptibility of developing EAU induced by IRBP [54].
In germ-free mice, lower retinal infiltration of T cells, lower levels of IFN-γ- and IL-17-producing T cells, and higher levels of regulatory T cells were found in the drainage lymph nodes of the eye [54]. This suggests that the microbiota regulates the inflammatory response by the adaptive pathway during autoantigen recognition. Nevertheless, this was not demonstrated in mice treated with antibiotics, suggesting that the reduction of the microbiota was incomplete in this group.
Nakamura et al. also observed a decrease in the severity of induced EAU following administration of broad-spectrum oral antibiotics, especially with vancomycin and metronidazole, but not with other antibiotics, which not only modified the composition of the microbiota but also produced an increase in the proportion of Treg in the intestinal lamina propria at the first week, and subsequently in extraintestinal lymphoid tissues and the eye [41].
On the other hand, Horai et al. tried to explain with a spontaneous EAU model [35] how immunologically privileged organs such as the eye are targets of autoimmunity, after a possible peripheral activation of autoreactive T cells that identify commensal microbiota. They found a decrease in disease severity in “germ-free” mice and when administering broad-spectrum oral antibiotics in combination, they observed an associated decrease in IRBP-specific T cells in the lamina propria of the intestine [55].
Experimental models also demonstrated that exogenous supplementation of SCFAs decreased the severity of uveitis [42,44]. Supplementation with sodium butyrate (NaB) attenuated the severity of EAU in mice, modified the balance of T cells, and switched from pathogenic Th17 to Treg [44]. These authors suggest that NaB reverses the differentiation from Th17 to Treg as previously demonstrated in vitro and in vivo [58], attenuating the severity of EAU via the Nrf2/HO-1 pathway.
Finally, experimental studies with transgenic rats for the HLA B27 gene have suggested the function of this in modulating the microbiome. The expression of HLA B27 was related to differences in the composition of the intestinal microbiome, with an increase in the relative abundance of Prevotella spp. and a decrease in Rikenellaceae, compared to wild rats, as well as an increase in Bacteroides vulgatus [59].
3.2. Clinical Studies
Clinical studies confirm some of the conclusions derived from pre-clinical studies. They have found a decrease in the abundance and diversity of bacterial [60] and fungal [61] microbiota in patients with undifferentiated and immune-mediated uveitis. There is also a decrease in anti-inflammatory or anti-pathogenic bacterial and fungal species, as well as an increase in pro-inflammatory and opportunistic species [60,61]. The clinical studies in which the causality of the NIU is related to the microbiota, as well as different therapeutic strategies for its modulation, are described in Table 2.
Table 2.
Clinical studies in which the causality of NIU has been related to the microbiota, and different therapeutic strategies for its modulation.
| Authors | Disease | n Patients and n Control | Findings |
|---|---|---|---|
| Kalyana et al., 2018 [60] | NIU | 13 NIU vs. 13 healthy |
|
| Jayasudha et al., 2019 [61] | 14 NIU vs. 24 healthy |
|
|
| Huang et al., 2018 [62] | AAU | 38 AAU vs. 40 healthy |
|
| Consolandi et al., 2015 [63] | BD | 22 BD vs. 16 healthy |
|
| Yasar et al., 2020 [21] | 27 BD vs. 10 healthy 3 clinical forms of BD |
|
|
| Shimizu et al., 2016 [64] | 12 BD vs. 12 healthy |
|
|
| Ye et al., 2018 [22] | 32 BD vs. 74 healthy |
|
|
| Ye et al., 2020 [65] | VKH | 82 VKH vs. 63 healthy |
|
EAU: Experimental autoimmune uveitis. NIU: Non-infectious uveitis. VKH: Vogt-Koyanagi-Harada syndrome. AAU: Acute anterior uveitis. BD: Behçet disease. FMT: Faecal microbiota transplantation. CsA: Cyclosporine A.
Despite finding no differences in the gut microbiome of patients with AAU compared to healthy subjects, Huang et al. found a different metabolic phenotype in AAU patients with increased expression of seven fecal metabolites (Table 2) by using gas chromatographic mass spectrometry-based metabolomics [62]. Clinical studies in patients with BD have shown an alteration in the composition of their microbiota [21,64], as well as significant differences in the composition of the gut microbiome between patients with BD without uveitis and those who develop uveitis (Table 2) [21]. This suggests an association of intestinal dysbiosis with the pathophysiology of this disease. Several authors have reported a decrease in butyrate-producing bacteria [22,63] and, consequently, a decrease in butyrate (anti-inflammatory), which could justify an increase in the inflammatory state. It has also been proposed that the gut microbiota can be modified by dietary patterns in these patients [66]. In patients with active VKH, a decrease in butyrate, lactate, and methane-producing bacteria was also seen, associated with an increase in Gram-negative bacteria, such as Paraprevotella spp. In addition, these differences decreased after immunosuppressive treatment, with an identifiable prognostic response to treatment markers [65].
The intestine has also been related to the pathogenesis of spondylarthritis: an alteration in the composition of the microbiota of patients with AS with respect to healthy controls, correlated with the state of their disease has been described [67]. An association has also been found between their intestinal inflammatory status and microbiota profile, with greater microbial richness in inflamed compared to non-inflamed tissues and higher in chronically than in acutely inflamed samples. Also, the composition of the bacterial community in inflamed samples differed from that of non-inflamed samples in AS patients, with no differences between chronic and acute inflammatory status. Unfortunately, information on the specific bacteria is not available from this study [66]. An increase in the bacterial genus Dialister has also been reported, which is positively correlated with inflammatory activity, suggesting that this bacterial species may serve as a marker of activity in AS [68].
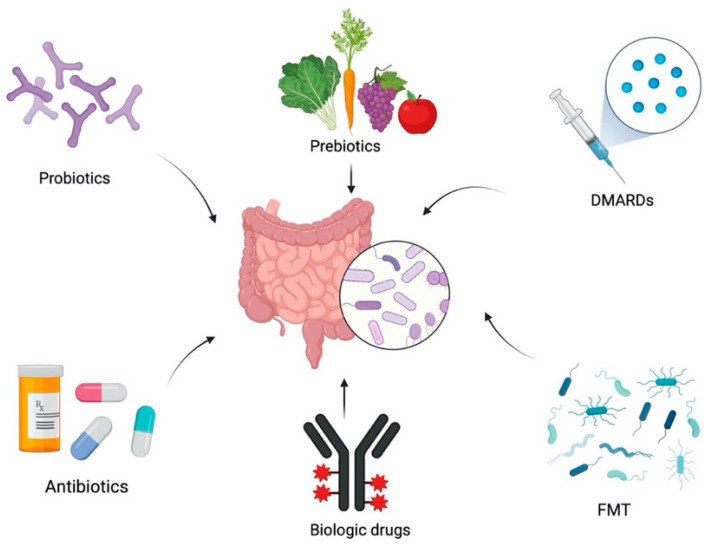
4. Therapeutic Approaches Aimed at Modifying the Intestinal Microbiota
Experimental models, as well as results in clinical studies, lead to the conclusion that the gut microbiota can modulate the responses and behavior of uveitogenic T cells at various levels, providing adaptive and innate stimuli, as well as possible regulatory effects. This connection not only allows us to advance in the knowledge of the pathogenesis of the disease, but also opens the way to possible new therapeutic targets focused on the modification of the microbiome. The pharmacological tools currently used to modify the microbiome (Figure 2), and that have shown their potential usefulness in the treatment of uveitis, are described below, either in EAU experimental models or in clinical studies, which are described in Table 1 and Table 2.
Figure 2.
Therapeutic approaches that modify the intestinal microbiota. Created with BioRender.com. FMT: Faecal microbiota transplantation. DMARDs: Disease-modifying anti-rheumatic drugs.
4.1. Probiotics
Probiotics introduce functional microbial components that are beneficial to the correct functioning of the gut and could be treatment options due to provoking an attenuation of the immune response. Bifidobacterium preserves intestinal barrier functions and produces SCFAs, and there is growing evidence demonstrating the beneficial effects of their supplementation on health, from protection against infection to different positive extra and intra-intestinal effects [69]. Their use in autoimmune diseases has been suggested since oral administration of probiotics in experimental murine models has been shown to have immunoregulatory functions [70]. Treatment with probiotics such as Lactobacillus spp. and Bifidobacterium bifidum produce induction of Treg in the intestinal mucosa and a decrease in inflammatory activity [70].
Supplementation with IRT-5 probiotics (Lactobacillus casei, Lactobacillus acidophilus, Lactobacillus reuteri, Bifidobacterium bifidum, and Streptococcus thermophilus) following removal of the microbiota with antibiotics reduced the severity of induced EAU in mice [57]. Likewise, treatment with the live probiotic Escherichia coli Nissle 1917 (EcN) prior to the induction of EAU in mice also protected against the development of uveitis and produced reinforcement of the integrity of the intestinal mucosa towards an anti-inflammatory state [56].
4.2. Prebiotics
Every day more articles show the impact of diet on health, possibly by modulating the microbiome and its metabolites. Prebiotics stimulate the proliferation of beneficial microorganisms and are present in foods of plant origin rich in fiber. Diets rich in unrefined cereals, fruits, vegetables, and legumes improve the profile of the intestinal microbiota since they are high in fiber, whose fermentation gives rise to the aforementioned SCFAs and other beneficial microbial metabolites with the ability to restore immune homeostasis [71,72,73]. Exogenous supplements of propionate [42,43] and butyrate [44] have been shown to modulate the immune system by attenuating the severity of EAU in animal models, as previously mentioned, turning them into potential treatment strategies.
Studies in patients with BD show a reduction in butyrate production that is linked to an increase in inflammatory status [22,63]. In this pathology, the change in the microbiota associated with three different diets is being analyzed, and one of them is supplemented with butyrate [66].
4.3. Antibiotic Therapy
Through the use of antibiotics, the microbiome can also be modulated. Experimental models in mice with EAU—both induced and spontaneous—have shown that oral administration of antibiotics attenuates ocular inflammation by modifying the composition of their gut microbiota. Different antibiotics have been used in isolation and combination in these studies: metronidazole and ciprofloxacin [54], ampicillin, metronidazole, neomycin, and vancomycin [35,41,55].
Trying to find the causative bacteria of the disease, Zárate-Baldés et al. perform their study with ampicillin, metronidazole, neomycin, and vancomycin individually, thus limiting the spectrum of microorganisms. Despite slight modifications in the development of the disease, none of them in isolation reduced the severity of uveitis as drastically as when they were used in combination. This could indicate that the bacterial origin of antigenic cross-reactivity is not limited to a single type of microorganism, but that several species of the microbiota contribute to uveitis [55].
Despite their obvious usefulness, broad-spectrum antibiotics also lead to an increase in resistant bacterial strains, which is a serious public health problem [41]. This makes this option not quite as interesting as it might at first seem and leads to the search for drugs with a narrower spectrum that eliminates targeted communities of bacteria, such as highly specific immunoglobulins. This approach has been suggested by Okai and colleagues as a potential treatment for IBD [74,75] using immunoglobulin A (IgA), an efficient modulator of the intestinal microbiota. These authors selected IgA monoclonal antibodies (clone W27) from the small intestine of healthy mice (which in vitro selectively bind to potentially pathogenic commensal bacteria such as Escherichia coli, but not to supposedly beneficial ones such as Lactobacillus casei); and found that its oral administration effectively prevented the development of the disease in experimental models of mice with colitis [75].
4.4. Faecal Microbiota Transplantation (FMT)
Another way to modulate the microbiota is the use of FMT, a procedure in which fecal matter from a healthy donor is transferred to a sick recipient. Its use is being investigated in a wide variety of diseases, and it has been approved for the treatment of recurrent colitis by Clostridium difficile, for which it has demonstrated its effectiveness [76]. FMT from patients with BD [22] or VKH [65] to EAU mouse models exacerbated the activity of their uveitis, with increased production of IL-17 and IFN-γ. However, due to its great interindividual variability, among other reasons, there is still not enough clinical evidence for its use in other diseases such as IBD, AS, and uveitis [77].
4.5. Immunomodulatory Drugs
The use of immunomodulatory drugs belonging to the group of “Disease-modifying anti-rheumatic drugs” (DMARDs) suppresses the growth of different bacteria, fungi, and viruses, and it is postulated that they could improve the severity of uveitis by acting through the intestinal microbiota [16,78]. Sulfasalazine, like other immunomodulators, has antibiotic functions and reduces vascular permeability, and improves both joint disease in patients with AS [79] and uveitis associated with HLA B27. On the other hand, dysbiosis of patients with active VKH decreased after immunosuppressive treatment with CsA, which also resolved intraocular inflammation, suggesting the effect of immunosuppressants on the microbiota [65].
Recently, an immunomodulatory effect of methotrexate and mycophenolate mofetil potentially linked to changes in the intestinal bacterial composition [80], which is specific and distinct for each drug, used in the EAU murine model has been suggested. Specifically, methotrexate at low maintained doses was able to decrease the adaptive, effector, and regulatory cellular response, both in the eye and in other tissues. This immunomodulatory effect correlated with specific changes in the composition of the gut microbiome. In contrast, mycophenolate induced an increase in highly suppressive Treg lymphocytes, showing a less suppressive effect on effector T populations in the eye and other tissues. This immunomodulatory effect was also proportional to differences in intestinal microbial composition after treatment [80].
4.6. Biological Drugs
Biological drugs have the ability to modify the natural course of numerous inflammatory diseases. A better understanding of the role of cytokines has led to the publication of studies supporting the use of anti-cytokine drugs (anti-TNF and anti-IL-6) in NIUs [33]. Adalimumab (ADA, anti-TNF drug) has been successfully used in the management of uveitis in patients with AS [81] and VISUAL I, II, and III clinical trials [82,83,84] have demonstrated efficacy and safety in non-anterior non-infectious, corticosteroid-refractory uveitis or in which corticosteroids cannot be used at acceptable doses. It is the only biological drug approved for this indication in the US and Europe [82,85]. In addition, Infliximab (IFX, anti-TNF drug) is approved in Japan for BD-associated uveitis, where it has demonstrated good tolerance and efficacy [86]. Nonetheless, this is not the case in other countries, where it must be used off-label.
Previous studies have suggested that treatment with anti-TNF restores the composition of the gut microbiota in intestinal [87] and extraintestinal [23] autoimmune pathologies. These are described in Table 3. Furthermore, there is increasing scientific evidence suggesting that the gut microbiome could be an indicator of clinical response to anti-TNF treatment and could play an important role in the efficacy of the drug [88]. Ribaldone et al. [87] evaluated in patients with Crohn’s disease (CD) the modification of the microbiota at baseline and six months of ADA treatment and found a decrease of Proteobacteria, which abundance is associated with dysbiosis and a diseased state, and an increase of Lachnospiraceae, composed mainly of anti-inflammatory butyrogenic species, in responder patients. This is in line with the idea that anti-TNF therapy restores the intestinal “eubiosis”, i.e., the balance of the intestinal microbial ecosystem. Similarly, Zhou et al. [89] also observed a restoration of the gut microbiota diversity in patients with CD that responded to IFX. In these patients, the abundance of Clostridiales increased to the levels detected in healthy individuals, but not in non-responder patients. In addition, predictive patterns of good response to IFX treatment have been identified [89]. Restoration of the gut microbiota has been also reported in patients with AS treated with ADA [23]. In this study, the differences in the intestinal microbiota of patients with AS were restored after 6 months of treatment with ADA, reaching a state similar to healthy controls by restoring the normal proportion of Bacteroidetes and Firmicutes, without finding differences between responders and non-responders [23]. If this association between the gut microbiome and clinical response to anti-TNF is confirmed, it could be used as an indicator of response to treatment before the start of therapy, increasing the accuracy of its indication. However, there are no published studies in patients with uveitis to date regarding the effect of anti-TNF therapy on microbiome status.
Table 3.
Clinical studies in other autoimmune diseases (not uveitis).
| Authors | Disease | n Patients and n Control | Study Type | Findings |
|---|---|---|---|---|
| Tito et al., 2017 [68] | AS | 27 AS vs. 15 healthy |
Causality |
|
| Costello et al., 2015 [67] | 9 AS vs. 9 healthy |
|
||
| Chen et al., 2021 [23] | 30 AS vs. 24 healthy |
Modulation |
|
|
| Ribaldone et al., 2019 [87] | IBD | 20 CD pre- and post-ADA treatment |
|
|
| Zhou et al., 2018 [89] | 72 CD, 51 UC vs. 73 healthy 16 CD pre- and post-IFX |
|
AS: Ankylosing spondylitis. IBD: Inflammatory bowel disease. ADA Adalimumab. IFX Infliximab. CD Crohn’s Disease. UC Ulcerative colitis.
The above-mentioned studies have provided compelling evidence for the involvement of the microbiome in the pathogenesis and progression of NIU and have demonstrated the potentially beneficial effects of several treatment approaches that have an effect, directly or indirectly, on the microbiome, such as supplementation of probiotics or prebiotics, FMT, DMARDs and biological drugs. Probiotics and prebiotics, through direct modulation of the microbiome, have demonstrated an enhancement of the anti-inflammatory response of the intestinal immune system in animal models by increasing gut antimicrobial peptide expression [56] and decreasing the production of pro-inflammatory cytokines in the retinas [44] and cervical lymph nodes [57]. In addition, supplementation of prebiotics, mainly SCFAs, modifies the balance of T cells, switching from pathogenic Th17 to Treg [44] and decreasing induction of effector T cells [42]. In patients with BD, a reduced butyrate production by their microbiota has been linked to an increased inflammatory status [22,63], and a clinical trial is currently underway to determine whether butyrate supplementation could improve clinical manifestations of these patients by modulating their gut microbiota [63]. Unfortunately, literature on the effect of probiotic/prebiotic supplementation on the inflammatory level of patients with NIU is lacking, but evidence derived from animal models suggests that it may be a treatment option to attenuate the severity of uveitis [42,44,56,57]. FMT may also be considered a promising therapeutic approach in NIU. It has been demonstrated that FMT from patients with autoimmune diseases associated with uveitis, such as BD [22] and VKH [65], exacerbate the activity of the uveitis in EAU mice. Therefore, it is reasonable to hypothesize that FMT from healthy donors could directly improve the inflammatory status of NIU by introducing beneficial species into the microbiome. Regarding DMARDs, one study in VKH patients showed partial restoration of their microbiota to a state more similar to that of healthy controls after treatment and identified microbial markers predictive of treatment response [65]. Therefore, DMARDs treatment of NIU could also induce microbiota recovery, at least partially, thus decreasing disease severity. Finally, biologic drugs have proven their effect on microbiome modulation in immune-mediated diseases such as CD, IBD, and AS [23,87,89]. Recent evidence on ADA and IFX treatment of patients with these immune-mediated diseases shows a trend towards microbial restitution, which was more evident in those patients who responded to therapy [87,89], but with differentially altered bacteria in each study. A remarkable finding of these studies was the different microbial patterns observed in responders compared to non-responders to the biological therapy, which allowed the identification of microbial predictive markers of response to treatment. Although these results are promising in the area of personalized medicine, no such studies have been conducted on patients with NIU. If the association between the gut microbiome and clinical response to anti-TNF observed in other immune-mediated diseases is confirmed in NIU, the study of the gut microbiome would emerge as a useful tool for the implementation of personalized medicine in NIU.
5. Conclusions
We currently have growing scientific evidence supporting the causality between intestinal dysbiosis and disease induction by altering the host’s homeostatic immune status, with speculation of a possible association between an altered microbiome and the pathogenesis of intraocular inflammation. However, there are still some unknowns in the relationship between the microbiome and uveitis, as microbial mono-association studies that demonstrate causality of changes in the microbiome with the development or maintenance of uveitis are very rare. We review the most recent studies associating intestinal dysbiosis and uveitis, both in animal and human models. The ability to modulate the composition of the microbiota through dietary supplementation or the use of drugs such as antibiotics, immunomodulators, or biologics opens a new therapeutic line for this disease. In addition, although new studies are needed to confirm this, an association between the intestinal microbiota and the clinical response to anti-TNF seems likely, which would allow personalizing and monitoring of the treatment of these patients more accurately.
We believe that this review will be of great use to research groups working in this field since it compiles all the information published to date.
Acknowledgments
CMG and AFF acknowledge the support of Instituto de Salud Carlos III (ISCIII) by research grants (JR20/0026 and JR18/00014).
Author Contributions
Conceptualization, C.A.R.-F., M.B.I., M.G.-B., C.M.-G. and A.F.-F.; investigation, B.d.D., K.C.-P. and J.A.V.; writing—original draft preparation, C.A.R.-F. and M.B.I.; writing—review and editing, L.R.-M. and V.L.; supervision, M.P. and A.F.-F.; project administration, A.F.-F.; funding acquisition, M.P and A.F.-F. All authors have read and agreed to the published version of the manuscript.
Conflicts of Interest
The authors declare that there is no conflict of interest.
Funding Statement
This work was partially supported by ISCIII co-funded by FEDER (PI20/00719, PI20/00413) and by Xunta de Galicia IN607D 2021 and IN607A 2020/05.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Horai R., Caspi R.R. Microbiome and Autoimmune Uveitis. Front Immunol. 2019;10:232. doi: 10.3389/fimmu.2019.00232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mochizuki M., Sugita S., Kamoi K. Immunological homeostasis of the eye. Prog. Retin. Eye Res. 2013;33:10–27. doi: 10.1016/j.preteyeres.2012.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Levy-Clarke G., Jabs D.A., Read R.W., Rosenbaum J.T., Vitale A., Van Gelder R.N. Expert Panel Recommendations for the Use of Anti–Tumor Necrosis Factor Biologic Agents in Patients with Ocular Inflammatory Disorders. Ophthalmology. 2014;121:785–796.e3. doi: 10.1016/j.ophtha.2013.09.048. [DOI] [PubMed] [Google Scholar]
- 4.Lin P. The role of the intestinal microbiome in ocular inflammatory disease. Curr. Opin. Ophthalmol. 2018;29:261–266. doi: 10.1097/ICU.0000000000000465. [DOI] [PubMed] [Google Scholar]
- 5.Turnbaugh P.J., Ley R.E., Hamady M., Fraser-Liggett C.M., Knight R., Gordon J.I. The human microbiome project. Nature. 2007;449:804–810. doi: 10.1038/nature06244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eckburg P.B., Bik E.M., Bernstein C.N., Purdom E., Dethlefsen L., Sargent M., Gill S.R., Nelson K.E., Relman D.A. Diversity of the human intestinal microbial flora. Science. 2005;308:1635–1638. doi: 10.1126/science.1110591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang H.X., Wang Y.P. Gut Microbiota-brain Axis. Chin. Med. J. 2016;129:2373–2380. doi: 10.4103/0366-6999.190667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ley R.E., Bäckhed F., Turnbaugh P., Lozupone C.A., Knight R.D., Gordon J.I. Obesity alters gut microbial ecology. Proc. Natl. Acad. Sci. USA. 2005;102:11070–11075. doi: 10.1073/pnas.0504978102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gritz E.C., Bhandari V. The human neonatal gut microbiome: A brief review. Front. Pediatr. 2015;3:17. doi: 10.3389/fped.2015.00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Matenchuk B.A., Mandhane P.J., Kozyrskyj A.L. Sleep, circadian rhythm, and gut microbiota. Sleep Med. Rev. 2020;53:101340. doi: 10.1016/j.smrv.2020.101340. [DOI] [PubMed] [Google Scholar]
- 11.Nell S., Suerbaum S., Josenhans C. The impact of the microbiota on the pathogenesis of IBD: Lessons from mouse infection models. Nat. Rev. Microbiol. 2010;8:564–577. doi: 10.1038/nrmicro2403. [DOI] [PubMed] [Google Scholar]
- 12.Kc D., Sumner R., Lippmann S. Gut microbiota and health. Postgrad. Med. 2020;132:274. doi: 10.1080/00325481.2019.1662711. [DOI] [PubMed] [Google Scholar]
- 13.Forrester J.V., Kuffova L., Dick A.D. Autoimmunity, Autoinflammation, and Infection in Uveitis. Am. J. Ophthalmol. 2018;189:77–85. doi: 10.1016/j.ajo.2018.02.019. [DOI] [PubMed] [Google Scholar]
- 14.Wen X., Hu X., Miao L., Ge X., Deng Y., Bible P.W., Wei L. Epigenetics, microbiota, and intraocular inflammation: New paradigms of immune regulation in the eye. Prog. Retin. Eye Res. 2018;64:84–95. doi: 10.1016/j.preteyeres.2018.01.001. [DOI] [PubMed] [Google Scholar]
- 15.Rosenbaum J.T., Lin P., Asquith M. Does the Microbiome Cause B27-related Acute Anterior Uveitis? Ocul. Immunol. Inflamm. 2016;24:440–444. doi: 10.3109/09273948.2016.1142574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones N.P. Immunosuppression in the Management of Presumed Non-infective Uveitis; Are We Sure What We are Treating? Notes on the Antimicrobial Properties of the Systemic Immunosuppressants. Ocul. Immunol. Inflamm. 2020;28:994–1003. doi: 10.1080/09273948.2019.1643030. [DOI] [PubMed] [Google Scholar]
- 17.Nishida A., Inoue R., Inatomi O., Bamba S., Naito Y., Andoh A. Gut microbiota in the pathogenesis of inflammatory bowel disease. Clin. J. Gastroenterol. 2018;11:1–10. doi: 10.1007/s12328-017-0813-5. [DOI] [PubMed] [Google Scholar]
- 18.Clapp M., Aurora N., Herrera L., Bhatia M., Wilen E., Wakefield S. Gut microbiota’s effect on mental health: The gut-brain axis. Clin. Pract. 2017;7:987. doi: 10.4081/cp.2017.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Angelucci F., Cechova K., Amlerova J., Hort J. Antibiotics, gut microbiota, and Alzheimer’s disease. J. Neuroinflamm. 2019;16:108. doi: 10.1186/s12974-019-1494-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim S., Jazwinski S.M. The Gut Microbiota and Healthy Aging: A Mini-Review. Gerontology. 2018;64:513–520. doi: 10.1159/000490615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yasar Bilge N.S., Pérez Brocal V., Kasifoglu T., Bilge U., Kasifoglu N., Moya A., Dinleyici E.C. Intestinal microbiota composition of patients with Behçet’s disease: Differences between eye, mucocutaneous and vascular involvement. The Rheuma-BIOTA study. Clin. Exp. Rheumatol. 2020;38((Suppl. 127)):60–68. [PubMed] [Google Scholar]
- 22.Ye Z., Zhang N., Wu C., Zhang X., Wang Q., Huang X., Du L., Cao Q., Tang J., Zhou C., et al. A metagenomic study of the gut microbiome in Behcet’s disease. Microbiome. 2018;6:135. doi: 10.1186/s40168-018-0520-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen Z., Zheng X., Wu X., Wu J., Li X., Wei Q., Zhang X., Fang L., Jin O., Gu J. Adalimumab Therapy Restores the Gut Microbiota in Patients With Ankylosing Spondylitis. Front Immunol. 2021;12:700570. doi: 10.3389/fimmu.2021.700570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li M., Yang L., Cao J., Liu T., Liu X. Enriched and Decreased Intestinal Microbes in Active VKH Patients. Investig. Ophthalmol. Vis. Sci. 2022;63:21. doi: 10.1167/iovs.63.2.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moustafa A., Li W., Anderson E.L., Wong E.H.M., Dulai P.S., Sandborn W.J., Biggs W., Yooseph S., Jones M.B., Venter C.J., et al. Genetic risk, dysbiosis, and treatment stratification using host genome and gut microbiome in inflammatory bowel disease. Clin. Transl. Gastroenterol. 2018;9:e132. doi: 10.1038/ctg.2017.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rowan S., Taylor A. The Role of Microbiota in Retinal Disease. Adv. Exp. Med. Biol. 2018;1074:429–435. doi: 10.1007/978-3-319-75402-4_53. [DOI] [PubMed] [Google Scholar]
- 27.Tanase D.M., Gosav E.M., Neculae E., Costea C.F., Ciocoiu M., Hurjui L.L., Tarniceriu C.C., Maranduca M.A., Lacatusu C.M., Floria M., et al. Role of Gut Microbiota on Onset and Progression of Microvascular Complications of Type 2 Diabetes (T2DM) Nutrients. 2020;12:3719. doi: 10.3390/nu12123719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rinninella E., Mele M.C., Merendino N., Cintoni M., Anselmi G., Caporossi A., Minnella A.M. The Role of Diet, Micronutrients and the Gut Microbiota in Age-Related Macular Degeneration: New Perspectives from the Gut−Retina Axis. Nutrients. 2018;10:1677. doi: 10.3390/nu10111677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Geyer O., Levo Y. Glaucoma is an autoimmune disease. Autoimmun. Rev. 2020;19:102535. doi: 10.1016/j.autrev.2020.102535. [DOI] [PubMed] [Google Scholar]
- 30.Fu X., Chen Y., Chen D. The Role of Gut Microbiome in Autoimmune Uveitis. [(accessed on 20 November 2021)];Ophthalmic. Res. 2021 64:168–177. doi: 10.1159/000510212. Available online: https://www.karger.com/Article/FullText/510212. [DOI] [PubMed] [Google Scholar]
- 31.Rojas M., Restrepo-Jiménez P., Monsalve D.M., Pacheco Y., Acosta-Ampudia Y., Ramírez-Santana C., Leung P.S.C., Ansari A.A., Gershwin M.E., Anaya J.M. Molecular mimicry and autoimmunity. J. Autoimmun. 2018;95:100–123. doi: 10.1016/j.jaut.2018.10.012. [DOI] [PubMed] [Google Scholar]
- 32.Rosenbaum J.T., Asquith M. The microbiome and HLA-B27-associated acute anterior uveitis. Nat. Rev. Rheumatol. 2018;14:704–713. doi: 10.1038/s41584-018-0097-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wakefield D., Clarke D., McCluskey P. Recent Developments in HLA B27 Anterior Uveitis. Front. Immunol. 2021;11:608134. doi: 10.3389/fimmu.2020.608134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scofield R.H., Warren W.L., Koelsch G., Harley J.B. A hypothesis for the HLA-B27 immune dysregulation in spondyloarthropathy: Contributions from enteric organisms, B27 structure, peptides bound by B27, and convergent evolution. Proc. Natl. Acad. Sci. USA. 1993;90:9330–9334. doi: 10.1073/pnas.90.20.9330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Horai R., Zárate-Bladés C., Dillenburg-Pilla P., Chen J., Kielczewski J.L., Silver P.B., Jittayasothorn Y., Chan C.-C., Yamane H., Honda K., et al. Microbiota-Dependent Activation of an Autoreactive T Cell Receptor Provokes Autoimmunity in an Immunologically Privileged Site. Immunity. 2015;43:343–353. doi: 10.1016/j.immuni.2015.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosenbaum J.T., Lin P., Asquith M. The microbiome, HLA, and the pathogenesis of uveitis. Jpn. J. Ophthalmol. 2016;60:1–6. doi: 10.1007/s10384-015-0416-y. [DOI] [PubMed] [Google Scholar]
- 37.Ciccia F., Guggino G., Rizzo A., Alessandro R., Luchetti M.M., Milling S., Saieva L., Cypers H., Stampone T., Di Benedetto P., et al. Dysbiosis and zonulin upregulation alter gut epithelial and vascular barriers in patients with ankylosing spondylitis. Ann. Rheum. Dis. 2017;76:1123–1132. doi: 10.1136/annrheumdis-2016-210000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Janowitz C., Nakamura Y.K., Metea C., Gligor A., Yu W., Karstens L., Rosenbaum J.T., Asquith M., Lin P. Disruption of Intestinal Homeostasis and Intestinal Microbiota During Experimental Autoimmune Uveitis. Investig. Opthalmol. Vis. Sci. 2019;60:420. doi: 10.1167/iovs.18-24813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhuang Z., Wang Y., Zhu G., Gu Y., Mao L., Hong M., Li Y., Zheng M. Imbalance of Th17/Treg cells in pathogenesis of patients with human leukocyte antigen B27 associated acute anterior uveitis. Sci. Rep. 2017;7:40414. doi: 10.1038/srep40414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Asquith M.J., Stauffer P., Davin S., Mitchell C., Lin P., Rosenbaum J.T. Perturbed Mucosal Immunity and Dysbiosis Accompany Clinical Disease in a Rat Model of Spondyloarthritis. Arthritis Rheumatol. 2016;68:2151–2162. doi: 10.1002/art.39681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nakamura Y.K., Metea C., Karstens L., Asquith M., Gruner H., Moscibrocki C., Lee I., Brislawn C.J., Jansson J.K., Rosenbaum J.T., et al. Gut Microbial Alterations Associated With Protection From Autoimmune Uveitis. Investig. Ophthalmol. Vis. Sci. 2016;57:3747–3758. doi: 10.1167/iovs.16-19733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nakamura Y.K., Janowitz C., Metea C., Asquith M., Karstens L., Rosenbaum J.T., Lin P. Short chain fatty acids ameliorate immune-mediated uveitis partially by altering migration of lymphocytes from the intestine. Sci. Rep. 2017;7:11745. doi: 10.1038/s41598-017-12163-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Asquith M., Davin S., Stauffer P., Michell C., Janowitz C., Lin P., Ensign-Lewis J., Kinchen J.M., Koop D.R., Rosenbaum J.T. Intestinal Metabolites Are Profoundly Altered in the Context of HLA-B27 Expression and Functionally Modulate Disease in a Rat Model of Spondyloarthritis. Arthritis Rheumatol. 2017;69:1984–1995. doi: 10.1002/art.40183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen X., Su W., Wan T., Yu J., Zhu W., Tang F., Liu G., Olsen N., Liang D., Zheng S.G. Sodium butyrate regulates Th17/Treg cell balance to ameliorate uveitis via the Nrf2/HO-1 pathway. Biochem. Pharmacol. 2017;142:111–119. doi: 10.1016/j.bcp.2017.06.136. [DOI] [PubMed] [Google Scholar]
- 45.Matysiak A., Kabza M., Karolak J., Jaworska M., Rydzanicz M., Ploski R., Szaflik J., Gajecka M. Characterization of Ocular Surface Microbial Profiles Revealed Discrepancies between Conjunctival and Corneal Microbiota. Pathogens. 2021;10:405. doi: 10.3390/pathogens10040405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zysset-Burri D.C., Schlegel I., Lincke J.-B., Jaggi D., Keller I., Heller M., Lagache S.B., Wolf S., Zinkernagel M.S. Understanding the Interactions Between the Ocular Surface Microbiome and the Tear Proteome. Investig. Ophthalmol. Vis. Sci. 2021;62:8. doi: 10.1167/iovs.62.10.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gomes J.Á.P., Frizon L., Demeda V.F. Ocular Surface Microbiome in Health and Disease. Asia-Pac. J. Ophthalmol. 2020;9:505–511. doi: 10.1097/APO.0000000000000330. [DOI] [PubMed] [Google Scholar]
- 48.Gündüz A., Gündüz A., Cumurcu T., Seyrek A. Conjunctival flora in Behçet patients. Can. J. Ophthalmol. 2008;43:476–479. doi: 10.3129/i08-089. [DOI] [PubMed] [Google Scholar]
- 49.Aragona P., Baudouin C., del Castillo J.M.B., Messmer E., Barabino S., Merayo-Lloves J., Brignole-Baudouin F., Inferrera L., Rolando M., Mencucci R., et al. The ocular microbiome and microbiota and their effects on ocular surface pathophysiology and disorders. Surv. Ophthalmol. 2021;66:907–925. doi: 10.1016/j.survophthal.2021.03.010. [DOI] [PubMed] [Google Scholar]
- 50.Li J.J., Yi S., Wei L. Ocular Microbiota and Intraocular Inflammation. Front. Immunol. 2020;11:609765. doi: 10.3389/fimmu.2020.609765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Petrillo F., Pignataro D., Lavano M.A., Santella B., Folliero V., Zannella C., Astarita C., Gagliano C., Franci G., Avitabile T., et al. Current Evidence on the Ocular Surface Microbiota and Related Diseases. Microorganisms. 2020;8:1033. doi: 10.3390/microorganisms8071033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Streilein J.W. Ocular immune privilege: Therapeutic opportunities from an experiment of nature. Nat. Rev. Immunol. 2003;3:879–889. doi: 10.1038/nri1224. [DOI] [PubMed] [Google Scholar]
- 53.Ozkan J., Willcox M.D. The Ocular Microbiome: Molecular Characterisation of a Unique and Low Microbial Environment. Curr. Eye Res. 2019;44:685–694. doi: 10.1080/02713683.2019.1570526. [DOI] [PubMed] [Google Scholar]
- 54.Heissigerova J., Stangova P.S., Klimova A., Svozilkova P., Hrncir T., Stepankova R., Kverka M., Tlaskalova-Hogenova H., Forrester J.V. The Microbiota Determines Susceptibility to Experimental Autoimmune Uveoretinitis. J. Immunol. Res. 2016;2016:5065703. doi: 10.1155/2016/5065703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zárate-Bladés C.R., Horai R., Mattapallil M.J., Ajami N.J., Wong M., Petrosino J.F., Itoh K., Chan C.-C., Caspi R.R. Gut microbiota as a source of a surrogate antigen that triggers autoimmunity in an immune privileged site. Gut Microbes. 2017;8:59–66. doi: 10.1080/19490976.2016.1273996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dusek O., Fajstova A., Klimova A., Svozilkova P., Hrncir T., Kverka M., Coufal S., Slemin J., Tlaskalova-Hogenova H., Forrester J.V., et al. Severity of Experimental Autoimmune Uveitis Is Reduced by Pretreatment with Live Probiotic Escherichia coli Nissle 1917. Cells. 2020;10:23. doi: 10.3390/cells10010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim J., Choi S.H., Kim Y.J., Jeong H.J., Ryu J.S., Lee H.J., Kim T.W., Im S.-H., Oh J.Y., Kim M.K. Clinical Effect of IRT-5 Probiotics on Immune Modulation of Autoimmunity or Alloimmunity in the Eye. Nutrients. 2017;9:1166. doi: 10.3390/nu9111166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Furusawa Y., Obata Y., Fukuda S., Endo T.A., Nakato G., Takahashi D., Nakanishi Y., Uetake C., Kato K., Kato T., et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature. 2013;504:446–450. doi: 10.1038/nature12721. [DOI] [PubMed] [Google Scholar]
- 59.Lin P., Bach M., Asquith M., Lee A.Y., Akileswaran L., Stauffer P., Davin S., Pan Y., Cambronne E.D., Dorris M., et al. HLA-B27 and Human β2-Microglobulin Affect the Gut Microbiota of Transgenic Rats. PLoS ONE. 2014;9:e105684. doi: 10.1371/journal.pone.0105684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Chakravarthy S.K., Jayasudha R., Prashanthi G.S., Ali M.H., Sharma S., Tyagi M., Shivaji S. Dysbiosis in the Gut Bacterial Microbiome of Patients with Uveitis, an Inflammatory Disease of the Eye. Indian J. Microbiol. 2018;58:457–469. doi: 10.1007/s12088-018-0746-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jayasudha R., Chakravarthy S.K., Prashanthi G.S., Sharma S., Tyagi M., Shivaji S. Implicating Dysbiosis of the Gut Fungal Microbiome in Uveitis, an Inflammatory Disease of the Eye. Investig. Ophthalmol. Vis. Sci. 2019;60:1384–1393. doi: 10.1167/iovs.18-26426. [DOI] [PubMed] [Google Scholar]
- 62.Huang X., Ye Z., Cao Q., Su G., Wang Q., Deng J., Zhou C., Kijlstra A., Yang P. Gut Microbiota Composition and Fecal Metabolic Phenotype in Patients With Acute Anterior Uveitis. Investig. Ophthalmol. Vis. Sci. 2018;59:1523–1531. doi: 10.1167/iovs.17-22677. [DOI] [PubMed] [Google Scholar]
- 63.Consolandi C., Turroni S., Emmi G., Severgnini M., Fiori J., Peano C., Biagi E., Grassi A., Rampelli S., Silvestri E., et al. Behçet’s syndrome patients exhibit specific microbiome signature. Autoimmun. Rev. 2015;14:269–276. doi: 10.1016/j.autrev.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 64.Shimizu J., Kubota T., Takada E., Takai K., Fujiwara N., Arimitsu N., Ueda Y., Wakisaka S., Suzuki T., Suzuki N. Bifidobacteria Abundance-Featured Gut Microbiota Compositional Change in Patients with Behcet’s Disease. PLoS ONE. 2016;11:e0153746. doi: 10.1371/journal.pone.0153746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Ye Z., Wu C., Zhang N., Du L., Cao Q., Huang X., Tang J., Wang Q., Li F., Zhou C., et al. Altered gut microbiome composition in patients with Vogt-Koyanagi-Harada disease. Gut Microbes. 2020;11:539–555. doi: 10.1080/19490976.2019.1700754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Pagliai G., Dinu M., Fiorillo C., Becatti M., Turroni S., Emmi G., Sofi F. Modulation of gut microbiota through nutritional interventions in Behçet’s syndrome patients (the MAMBA study): Study protocol for a randomized controlled trial. Trials. 2020;21:511. doi: 10.1186/s13063-020-04444-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Costello M.E., Ciccia F., Willner D., Warrington N., Robinson P.C., Gardiner B., Marshall M., Kenna T.J., Triolo G., Brown M.A. Brief Report: Intestinal Dysbiosis in Ankylosing Spondylitis: Gut Microbiome and AS-Related Genes. Arthritis Rheumatol. 2015;67:686–691. doi: 10.1002/art.38967. [DOI] [PubMed] [Google Scholar]
- 68.Tito R.Y., Cypers H., Joossens M., Varkas G., Van Praet L., Glorieus E., Bosch F.V.D., De Vos M., Raes J., Elewaut D. Brief Report: Dialister as a Microbial Marker of Disease Activity in Spondyloarthritis. Arthritis Rheumatol. 2017;69:114–121. doi: 10.1002/art.39802. [DOI] [PubMed] [Google Scholar]
- 69.Arboleya S., Watkins C., Stanton C., Ross R.P. Gut Bifidobacteria Populations in Human Health and Aging. Front. Microbiol. 2016;7:1204. doi: 10.3389/fmicb.2016.01204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.De Oliveira G.L.V., Leite A.Z., Higuchi B.S., Gonzaga M.I., Mariano V.S. Intestinal dysbiosis and probiotic applications in autoimmune diseases. Immunology. 2017;152:1–12. doi: 10.1111/imm.12765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Holscher H.D. Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes. 2017;8:172–184. doi: 10.1080/19490976.2017.1290756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zmora N., Suez J., Elinav E. You are what you eat: Diet, health and the gut microbiota. Nat. Rev. Gastroenterol. Hepatol. 2019;16:35–56. doi: 10.1038/s41575-018-0061-2. [DOI] [PubMed] [Google Scholar]
- 73.De Filippis F., Pellegrini N., Vannini L., Jeffery I.B., La Storia A., Laghi L., Serrazanetti D.I., di Cagno R., Ferrocino I., Lazzi C., et al. High-level adherence to a Mediterranean diet beneficially impacts the gut microbiota and associated metabolome. Gut. 2016;65:1812–1821. doi: 10.1136/gutjnl-2015-309957. [DOI] [PubMed] [Google Scholar]
- 74.Okai S., Usui F., Ohta M., Mori H., Kurokawa K., Matsumoto S., Kato T., Miyauchi E., Ohno H., Shinkura R. Intestinal IgA as a modulator of the gut microbiota. Gut Microbes. 2017;8:486–492. doi: 10.1080/19490976.2017.1310357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Okai S., Usui F., Yokota S., Hori-I Y., Hasegawa M., Nakamura T., Kurosawa M., Okada S., Yamamoto K., Nishiyama E., et al. High-affinity monoclonal IgA regulates gut microbiota and prevents colitis in mice. Nat. Microbiol. 2016;1:16103. doi: 10.1038/nmicrobiol.2016.103. [DOI] [PubMed] [Google Scholar]
- 76.van Nood E., Vrieze A., Nieuwdorp M., Fuentes S., Zoetendal E.G., de Vos W.M., Visser C.E., Kuijper E.J., Bartelsman J.F.W.M., Tijssen J.G.P., et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N. Engl. J. Med. 2013;368:407–415. doi: 10.1056/NEJMoa1205037. [DOI] [PubMed] [Google Scholar]
- 77.Choi R.Y., Asquith M., Rosenbaum J.T. Fecal transplants in spondyloarthritis and uveitis: Ready for a clinical trial? Curr. Opin. Rheumatol. 2018;30:303–309. doi: 10.1097/BOR.0000000000000506. [DOI] [PubMed] [Google Scholar]
- 78.Rossi D.C., Ribi C., Guex-Crosier Y. Treatment of chronic non-infectious uveitis and scleritis. Swiss Med. Wkly. 2019;149:w20025. doi: 10.4414/smw.2019.20025. [DOI] [PubMed] [Google Scholar]
- 79.Sharma S.K., Kadiyala V., Naidu G., Dhir V. A randomized controlled trial to study the efficacy of sulfasalazine for axial disease in ankylosing spondylitis. Int. J. Rheum. Dis. 2018;21:308–314. doi: 10.1111/1756-185X.13124. [DOI] [PubMed] [Google Scholar]
- 80.Llorenç V., Nakamura Y., Metea C., Karstens L., Molins B., Lin P. Antimetabolite Drugs Exhibit Distinctive Immunomodulatory Mechanisms and Effects on the Intestinal Microbiota in Experimental Autoimmune Uveitis. Investig. Opthalmol. Vis. Sci. 2022;63:30. doi: 10.1167/iovs.63.3.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ward M.M., Deodhar A., Gensler L.S., Dubreuil M., Yu D., Khan M.A., Visser C.E., Kuijper E.J., Bartelsman J.F.W.M., Tijssen J.G.P., et al. 2019 Update of the American College of Rheumatology/Spondylitis Association of America/Spondyloarthritis Research and Treatment Network Recommendations for the Treatment of Ankylosing Spondylitis and Nonradiographic Axial Spondyloarthritis. Arthritis Rheumatol. 2019;71:1599–1613. doi: 10.1002/art.41042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Nguyen Q.D., Merrill P., Jaffe G.J., Dick A.D., Kurup S.K., Sheppard J., Schlaen A., Pavesio C., Cimino L., Van Calster J., et al. Adalimumab for prevention of uveitic flare in patients with inactive non-infectious uveitis controlled by corticosteroids (VISUAL II): A multicentre, double-masked, randomised, placebo-controlled phase 3 trial. Lancet. 2016;388:1183–1192. doi: 10.1016/S0140-6736(16)31339-3. [DOI] [PubMed] [Google Scholar]
- 83.Suhler E.B., Adán A., Brézin A.P., Fortin E., Goto H., Jaffe G.J. Safety and Efficacy of Adalimumab in Patients with Noninfectious Uveitis in an Ongoing Open-Label Study: VISUAL III. Ophthalmology. 2018;125:1075–1087. doi: 10.1016/j.ophtha.2017.12.039. [DOI] [PubMed] [Google Scholar]
- 84.Goto H., Zako M., Namba K., Hashida N., Kaburaki T., Miyazaki M., Sonoda K.-H., Abe T., Mizuki N., Kamoi K., et al. Adalimumab in Active and Inactive, Non-Infectious Uveitis: Global Results from the VISUAL I and VISUAL II Trials. Ocul. Immunol. Inflamm. 2019;27:40–50. doi: 10.1080/09273948.2018.1491605. [DOI] [PubMed] [Google Scholar]
- 85.You C., Sahawneh H., Ma L., Kubaisi B., Schmidt A., Foster S. A review and update on orphan drugs for the treatment of noninfectious uveitis. Clin. Ophthalmol. 2017;11:257–265. doi: 10.2147/OPTH.S121734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ohno S., Umebayashi I., Matsukawa M., Goto T., Yano T. Safety and efficacy of infliximab in the treatment of refractory uveoretinitis in Behçet’s disease: A large-scale, long-term postmarketing surveillance in Japan. Arthritis Res. Ther. 2019;21:2. doi: 10.1186/s13075-018-1793-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ribaldone D.G., Caviglia G.P., Abdulle A., Pellicano R., Ditto M.C., Morino M., Fusaro E., Saracco G.M., Bugianesi E., Astegiano M. Adalimumab Therapy Improves Intestinal Dysbiosis in Crohn’s Disease. J. Clin. Med. 2019;8:1646. doi: 10.3390/jcm8101646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Weersma R.K., Zhernakova A., Fu J. Interaction between drugs and the gut microbiome. Gut. 2020;69:1510–1519. doi: 10.1136/gutjnl-2019-320204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Zhou Y., Xu Z.Z., He Y., Yang Y., Liu L., Lin Q., Nie Y., Li M., Zhi F., Liu S., et al. Gut Microbiota Offers Universal Biomarkers across Ethnicity in Inflammatory Bowel Disease Diagnosis and Infliximab Response Prediction. [(accessed on 17 January 2022)];mSystems. 2018 3:e00188-17. doi: 10.1128/mSystems.00188-17. Available online: https://journals.asm.org/doi/10.1128/mSystems.00188-17. [DOI] [PMC free article] [PubMed] [Google Scholar]