Abstract
PURPOSE:
The study aimed to establish the outcome of multifocal contact lenses (MFCL) (Multistage + 1.50D and Proclear + 3.00D) on myopia progression and axial length elongation over an 18-month period.
METHODS:
Thirty myopic schoolchildren (5 males and 25 females) aged between 13 and 15 years were randomly assigned to wear either single vision contact lens (SVCL), Multistage MFCL + 1.50D, or Proclear +3.00D MFCL for 1½ years using a double-masked design. Cycloplegic refraction, corneal curvature, and axial length were measured.
RESULTS:
Myopia progression was controlled by 38.6% and 66.6% in children wearing Multistage + 1.50D and Proclear +3.00D MFCL, respectively, in comparison to children wearing SVCL over an 18-month period. In terms of axial elongation, this study found a 31.1% and 63.2% control in axial elongation over 18 months of treatment in comparison to the SVCL group. No statistical significant difference in corneal curvature was found between initial and last visits for all the three groups (SVCL, P = 0.90; Multistage + 1.50 MFCL, P = 0.78, and Proclear + 3.00 MFCL, P = 0.05).
CONCLUSION:
Proclear +3.00D MFCL was revealed to cause slow development of myopia and axial elongation among myopic schoolchildren. MFCL with higher add powers could be more effective on myopia progression in comparison with moderate add powers.
Keywords: Axial length, contact lens, eyeglasses, myopia, schoolchildren
INTRODUCTION
Nowadays, myopia is viewed as a major public health problem due to the potentially blinding complications associated with its progression. The occurrence of myopia among Asian countries has increased in recent decades, especially among the Chinese ethnic community.[1] The comprehensive etiology of myopia and identifying methods to stop further affliction have been the focus of the growing literature on myopia. Curative management proposed to feasibly slow the progression of myopia in children included outdoor play,[2] under correction of myopia,[3,4] multifocal/bifocal spectacles,[5,6] multifocal contact lenses (MFCL),[7,8] pharmacological interventions,[9,10] or orthokeratology contact lenses.[11]
In cases where myopia is remedied using traditional contact lenses or glasses, the image formed at the central retina is in focus; on the other hand, the images at the peripheral retina is out of focus, leading to comparative peripheral hyperopic defocus. This peripheral hyperopic defocus is considered the cause for the progression of myopia, according to previous animal studies.[12,13] Consequently, current researches on the treatment of myopic progression have aimed at eliminating this peripheral relative hyperopic defocus produced using soft multifocal or orthokeratology contact lenses. However, some studies proved that peripheral hyperopia was not significantly related to the progression and presence of myopia in children.[14,15]
Because of these studies, there is a growing attention in recommending soft MFCL to slow the progression of myopia. Most of the previous studies on controlling progression of myopia[16,17] had used a +2.00D addition for the bifocal or MFCL. However, the highest addition power (+2.50D add) in MFCL to control myopia in children was used by Lam et al. with defocus Incorporated soft contact lens (DISC).[7] A cross-sectional study conducted by Lopes-Ferreira et al. has shown that using commercial dominant design MFCL can stimulate myopic defocus in the peripheral retina with +3.00D and +4.00D addition power.[18]
In view of these previous research findings, we were interested to explore whether a lower or a higher add was better in controlling the progression of myopia. The primary aim of this study was to evaluate the effectiveness of MFCL in halting progression of myopia in children aged between 13 and 15 years in Kuala Lumpur and to compare the progression of myopia and axial elongation of schoolchildren prescribed with two commercially available distance – center soft MFCL (Multistage +1.50D and Proclear +3.00D MFCL) to a classic single-vision contact lens (SVCL) serving as the control group.
METHODS
Study population
An experimental longitudinal prospective randomized double-masked study was done at the Universiti Kebangsaan Malaysia Optometry Clinic and Vision Science Lab to identify the effect of two different MFCL on myopia progression. Thirty-seven Malaysian schoolchildren suffering from myopia aged between 13 and 15 years were requested to participate with the permission of their respective parents or guardians (31 females and 6 males). Children who have best-corrected visual acuity of 6/9 or better in both right and left eyes, spherical equivalent (SE) refractive error range of −2.00 to −6.00 D, astigmatism of ≤−1.00 D, been myopic for more than 6 months, and were willing to wear soft contact lenses for at least 8 h/day for a period of 18 months, were included in this study. On the other hand, children with any myopia-related ocular condition, abnormal binocular condition, associated systemic conditions, the past or recent history of soft contact lenses, bifocal/progressive spectacle wear, or orthokeratology contact lens wear were disqualified. There were seven dropouts during the follow-up of this study (three participants reported difficulties with contact lens wear, two participants moved out of Kuala Lumpur city, and two participants stopped coming to their follow-up appointments and did not answer the calls) as shown in Figure 1. Thirty participants (5 males, 25 females) successfully completed the study.
Figure 1.
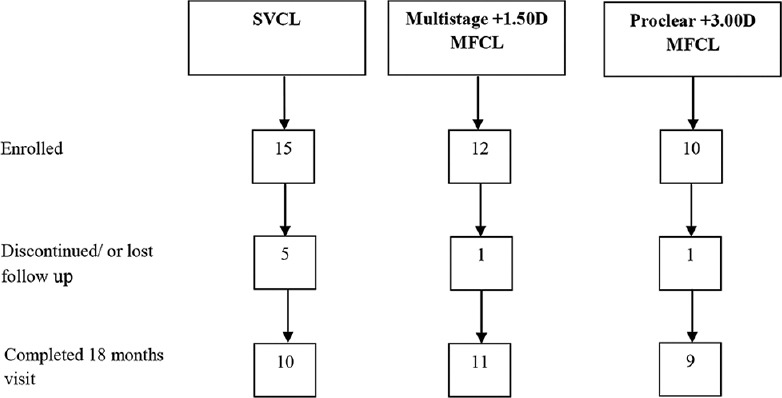
Flowchart of the participants
Study design
There were three groups of participants. The participants were randomly distributed by an unmasked optometrist (MO) into two treatment groups and one control group using a random sampling method. In Group 1, participants were fitted with Multistage +1.50D addition MFCL (SEED, Japan), in Group 2 participants were fitted with Proclear + 3.00D addition MFCL with the distance center (D-design) (CooperVision, NY, USA), and in Group 3 participants were fitted with (2-week Pure- SEED) SVCL in both eyes. The different contact lens designs used in the study are listed [Supplementary Table 1]. The lenses were worn every day with replacement every month for the Proclear MFCL and every two weeks for the Multistage MFCL as well as the SVCL. The participants were recommended to use the contact lenses for at least 8 h every day and were requested to wear their spectacles for the rest of the day. The lenses were cleaned, disinfected, and stored using Forest Leaf solution (SEED, Japan).
Supplementary Table 1.
Material and design specifications for the contact lenses used in the study
| Single vision CL | Multistage MFCL | Proclear MFCL | |
|---|---|---|---|
| Brand | 2 weeks pure | 2 weeks multistage | CooperVision |
| Material | Zwitterionic material SIB | Group IV - Ionic high water content | Omfilcon A |
| Modality | 2 weeks | 2 weeks | 1 month |
| Power (s) | Single vision | Type (B) add+1.50D | Type (D) Add +3.00 D |
| Base curve | 8.6 mm | 8.6 mm | 8.7 mm |
| Diameter | 14.2 mm | 14.2 mm | 14.4 mm |
| a. Spherical distance zone diameter | 2.5 ɸ mm | 2.3 ɸ mm | |
| b. Aspheric multifocal zone (width/Dia) | 0.5mm/2.5 ɸ to 3.5ɸ mm | 1.35 mm/2.3 ɸ to 5.0 ɸ mm | |
| c. Spherical near zone (width/Dia) | 2.25mm/3.5ɸ to 8.0ɸ mm | 1.75mm/5.0 ɸ to 8.5 ɸ mm | |
| Water content (%) | 58 | 58 | 62 |
MFCL=Multifocal contact lenses, CL=Contact lenses
Examination
A proficient and qualified optometrist conducted a comprehensive ocular examination, comprising fundus examination and anterior segment evaluation, among selected samples. LogMAR chart at 6 m using a mirror was used to measure the distance visual acuity. Eligible candidates underwent a series of measurements including corneal curvature, objective cycloplegic refraction using Grand-Seiko open field auto refractometer as well as subjective refraction, and axial length of both eyes by a MO at each follow-up visit. Corneal curvature was measured using a manual Bausch and Lomb keratometer as part of the initial and 18-month visits. The cycloplegic refraction was achieved after 30 min of instillation of a second drop of 1.0% cyclopentolate, separated by 5 min apart to assess the central refractive error. An ultrasound A-scan (Tomey AL-2000) was used to measure axial length (using a handheld probe) at 6, 12, and 18 months of treatment. The average of five measurements was taken. Accommodative response, lag of accommodation, and phoria at near and distance were evaluated at baseline.
Data analysis
The outcomes of the study were: (1) changes in SE refractive error, (2) changes in axial length, and (3) changes in corneal curvature from the baseline. Mean and standard deviation (SD), median, and range were computed to describe the continuous variable, while for categorical variables, we used counts and percentages. IBM SPSS software version 20 (SPSS Inc., Chicago, IL, USA) for windows was used for data analysis. The data from the right and left eyes revealed no statistically significant difference. Therefore, the data from both eyes of each individual participant were averaged in subsequent analyses. Myopia progression over 18 months was calculated as the difference in SE refraction between each visit. Analysis of variance (ANOVA) with Welch test and post hoc Games-Howell were performed to examine the treatment effects between SVCL, Multistage +1.50D, and Proclear +3.00D MFCL in outcome measures at 6, 12, and 18 months of treatment. Repeated measure ANOVA was performed to establish the progression of myopia and axial elongation over an 18-month duration for each contact lens group. Pearson’s correlation analysis was used to assess any association between SE and axial length for each group separately at baseline and at follow-up visits. In all analyses, the differences were defined as significant when the P < 0.05.
Ethical approval
All candidates and their custodians were given detailed information regarding the process of the study and probable complications or side effects associated with the test, after which written consents were taken from legal guardians. This study was approved by the Ethics Committee of Universiti Kebangsaan Malaysia (UKM 1.5.3.5/244/NN-144-2013) and followed the principles of the Declaration of Helsinki for exploiting human participants.
RESULTS
A total of thirty participants were randomly assigned to wear SVCL (n = 10), Multistage + 1.50D MFCL (n = 11), or Proclear + 3.00D MFCL (n = 9) for 1½ years using a double-masked design. The mean age of participants was 14.2 ± 0.71 years and ranged between 13 and 15 years old at the baseline visit. Visual acuity of all children was 6/6 with correction in either eye. The mean SE refractive error of the enrolled sample was − 3.96 ± 1.17D (range: −2.18 to − 6.03D) at baseline.
Demographic and biometric data
The demographic and biometric data at the baseline of participants for all groups are illustrated in Table 1. At baseline, unpaired t-test analysis revealed that MFCL group was not significantly different in comparison to the SVCL group regarding the comparative number of boys and girls, the SE refractive error, axial length, age, and the prevalence of parental myopia. However, the Multistage +1.50D MFCL group had slightly more girls and less myopic parents than the control group.
Table 1.
Demographic and biometric data at baseline of children in single-vision contact lens, multistage +1.50 D, and proclear +3.00 D multifocal contact lenses groups
| SVCL (n=10) | Multistage (n=11) | P a | Proclear (n=9) | P b | |
|---|---|---|---|---|---|
| Age (years) | 14.22±0.68 | 14.16±0.64 | 0.864 | 14.23±0.77 | 0.970 |
| Female, n (%) | 8 (80) | 10 (91) | 7 (78) | ||
| SE (D) | −3.82±1.25 D | −4.38±0.98 D | 0.299 | −3.59±1.14 D | 0.686 |
| AL (mm) | 24.41±0.66 mm | 24.37±0.94 mm | 0.926 | 24.56±0.70 mm | 0.651 |
| Parental myopia (%) | |||||
| None | 30 | 41 | 27 | ||
| ≥1 parent | 70 | 59 | 73 |
aP value represents unpaired t-test between SVCL and multistage groups, bP value represents unpaired t-test between SVCL, and proclear groups. SE=Spherical equivalent; SVCL=Single-vision contact lens; AL=Axial length
Spherical equivalent, axial length, and corneal curvature variability at 6, 12, and 18 months
The participants at baseline had SE range of −2.59–−6.03D for SVCL group, −2.81–−5.77D for Multistage +1.50D MFCL group, and −2.18–−5.89D for Proclear +3.00D MFCL group. The progressive changes in mean refractive error, axial elongation, and corneal curvature over the study periods are shown in Table 2. One-way ANOVA showed no significant difference in SE at baseline among the three groups (P = 0.32). Repeated measure ANOVA was applied to determine the treatment effect on refractive error over the 18-month study duration for all the groups. The results for SVCL indicated a significant change during treatment (F [1.839, 16.548] = 25.578, P < 0.001). Bonferroni post hoc analysis exhibited a significant difference between the baseline visit and all the follow-up visits (6 months, P = 0.008; 12 months, P = 0.007; and 18 months, P < 0.001). Moreover, Multistage +1.50D add power MFCL showed similar results (F [1.718, 17.178] = 17.369, P < 0.001). Findings of the study also showed a significant difference between the baseline visit and all the follow-up visits (6 months, 12 months, and 18 months, P < 0.001). This indicated a significant change in refractive error in every visit for the study duration for the SVCL and Multistage MFCL groups. However, the Proclear +3.00D add power MFCL had no significant changes during the 6-month (P = 0.93) and the 12-month (P = 0.21) visits. The significant changes occurred at 18 months of treatment (P = 0.01), (F [2.063, 16.503] = 4.157, P = 0.03).
Table 2.
Changes in spherical equivalent refraction (mean±SD), axial length, and corneal curvature over the course of 18 months for single-vision contact lens, multistage +1.50D, and proclear +3.00D multifocal contact lenses
| Refractive error (D) | Axial length (mm) | K-reading (mm) | |
|---|---|---|---|
| SVCL | |||
| Baseline | −3.82±1.25D | 24.41±0.66 | 7.761±0.28 |
| 6 months | −4.14±1.17D | 24.57±0.62 | - |
| 12 months | −4.26±1.09D | 24.62±0.57 | - |
| 18 months | −4.39±1.13D | 24.69±0.61 | 7.758±0.27 |
| Progression/18 months | −0.57±1.68D | 0.228±0.89 | -0.0027±0.39 |
| Multistage +1.50 | |||
| Baseline | −4.38±0.98D | 24.37±0.94 | 7.690±0.23 |
| 6 months | −4.65±0.97D | 24.47±0.95 | - |
| 12 months | −4.78±1.03D | 24.54±0.95 | - |
| 18 months | −4.73±1.05D | 24.53±0.95 | 7.686±0.22 |
| Progression/18 months | −0.35±1.44D | 0.157±1.34 | -0.003±0.32 |
| Proclear +3.00 | |||
| Baseline | −3.59±1.14D | 24.56±0.70 | 7.765±0.16 |
| 6 months | −3.68±1.14D | 24.63±0.76 | - |
| 12 months | −3.78±1.11D | 24.62±0.76 | - |
| 18 months | −3.78±1.14D | 24.64±0.74 | 7.786±0.16 |
| Progression/18 months | −0.19±1.61D | 0.084±1.02 | 0.021±0.22 |
D=Diopter; K-reading=Corneal curvature; SVCL=Single-vision contact lens
Axial length reduction was found in Multistage +1.50D MFCL and Proclear +3.00D MFCL, when compared to SVCL group (31% vs. 63%, respectively). Conversely, no significant difference was found among the three groups along the study period (P = 0.09) in terms of axial length elongation. Figure 2 illustrates the relative axial elongation over the three follow-up visits during the 18 months of the study. The annual rate of axial elongation was 0.187 ± 0.59 mm, 0.104 ± 0.89 mm, and 0.056 ± 0.68 mm for SVCL, Multistage +1.50D MFCL, and Proclear +3.00D MFCL wearers, respectively. No significant correlation between SE and axial length was found in single-vision lens wearers. However, significant strong negative correlation was found between SE and axial length in Multistage +1.5 MFCL wearers at baseline (r = −0.78, P = 0.005), after 6 months (r = −0.79, P = 0.003), after 12 months (r = −0.73, P = 0.01), and after 18 months (r = −0.73, P = 0.012). For Proclear +3.00 MFCL wearers, a significant strong negative correlation was also shown between SE and axial length of the eye at baseline (r = −0.87, P = 0.003), after 6 months (r = −0.81, P = 0.008), after 12 months (r = −0.83, P = 0.005), and after 18 months (r = −0.80, P = 0.009)
Figure 2.
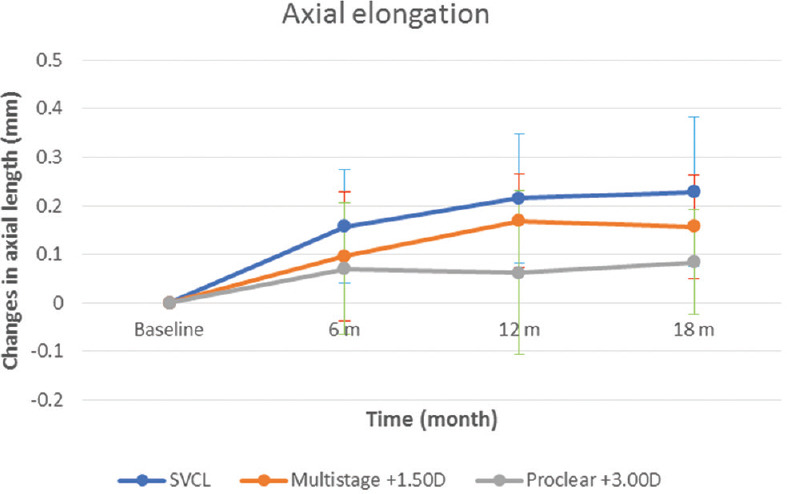
Relative axial elongation changes during 6-, 12-, and 18-month follow-up visits for myopic schoolchildren
Despite some observed flattening of the cornea in the SVCL and Multistage MFCL groups at 18 months, no statistically significant changes in the corneal curvature between the initial visit and the last visit after 18 months of wearing the contact lenses among the three groups (SVCL, P = 0.900), (Multistage +1.50D, P = 0.779), and (Proclear +3.00D, P = 0.051) were found. This indicates that wearing the contact lenses over 18 months had no impact on changing the corneal curvature and did not flattening the cornea.
Myopia progression at 6, 12, and 18 months
Myopia progression was controlled in children wearing Multistage +1.50D and Proclear +3.00D MFCL, in comparison to children wearing SVCL over an 18-month period (38.6% vs. 66.6%, respectively). Figure 3 illustrates the progression of myopia over the three follow-up visits during the 18-month study period. The mean ± SD of SE progression of myopia over 1½ years was − 0.57 ± 1.68 D for SVCL wearers, −0.35 ± 1.44 D for Multistage +1.50D MFCL wearers, and − 0.19 ± 1.61D for the Proclear +3.00 MFCL wearers.
Figure 3.
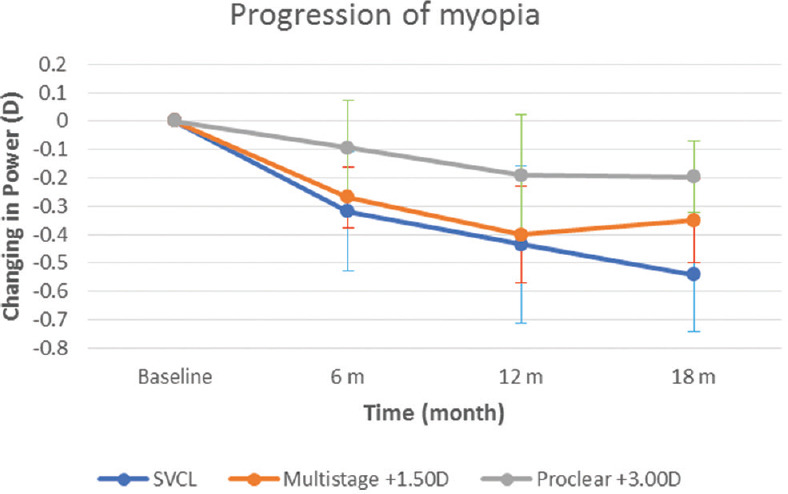
Relative myopia progression changes during 6-, 12-, and 18-month follow-up visits for myopic schoolchildren
In comparison to the SVCL group, there was no significant difference in myopia progression in the first 6 months as well as in the 12 months for the multistage +1.50D MFCL group and Proclear +3.00D MFCL group (F [2,4.29] = 15.480, P = 0.06) and (F [2,2.649] = 17.425, P = 0.09), respectively. However, there was a significant difference in myopic progression as compared to the control group (F [2,10.077] = 17.702, P < 0.001) during the 18-month visit. Notably, there was a statistically significant difference found between SVCL group and Proclear +3.00D MFL (P < 0.001), while multistage +1.50D MFCL did not show a significant statistical difference (P = 0.06). Paired t-test between multistage +1.50D and Proclear +3.00D MFCL showed statistically significant difference at 6, 12, and 18 months (P = 0.02, P = 0.05, and P = 0.41, respectively). Table 3 demonstrates the values of mean and SD at baseline for accommodative response, lag of accommodation, and phoria deviation at near and distance. Proclear MFCL of +3.00D add showed near normal lag of accommodation compared to multistage +1.5 MFCL but no significant difference in the lag of accommodation between the different addition powers of MFCL (P > 0.05). The Bonferroni post hoc tests revealed no significant difference in phoria between full correction of SVCL and all the addition power of contact lenses used in this study (P > 0.05) at distance and near phoria.
Table 3.
Accommodative response, lag of accommodation, and phoria deviation for baseline (without lens), multistage +1.5D, and proclear +3.0D multifocal contact lenses
| Contact lens | Accommodative response | Lag of accommodation | Phoria at near | Phoria at distance |
|---|---|---|---|---|
| Baseline | 0.23 D±0.28 | 2.27 D±0.28 | 0.30±2.35 (eso) | −0.15±1.35 (exo) |
| Multistage +1.5D | 1.33 D±0.61 | 1.17 D±0.61 | 0.63±3.73 (eso) | −0.11±1.57 (exo) |
| Proclear +3.0D | 1.40 D±0.83 | 1.10 D±0.83 | −0.31±2.49 (exo) | 0.31±1.46 (eso) |
D=Diopter; Eso=esophoria; Exo=Exophoria
DISCUSSION
Previous studies reported that correcting central refractive error with SVCL increased the absolute hyperopic defocus in myopic eyes worsening the unwanted blur at the peripheral retina.[19] This peripheral hyperopia may be a possible cause of myopia progression. After 18 months of follow-up, the outcomes of this study showed a greater progression of myopia, change in refractive error, and axial length in the SVCL wearer group in comparison to the treatment groups with negligible affection on the corneal curvature. The findings of this study showed that the highest reduction of myopia progression and axial elongation was with the Proclear +3.00D MFCL group.
Aiming to include myopic children with potential for myopia progression, the study revealed that the SE inclusion required for recruitment into this study ranged between −2.00D and −6.00D, which was slightly higher than the SE in previous studies ranging between −0.75D and −4.50D at the baseline visit.[16,20] Moreover, the age group in this research was slightly older than previous studies (13 to 15 years).[17,21] Since the participants who participated in this research were slightly older compared to similar previous studies, the progression rate of myopia was found to be slower (SE progression of myopia over 1½ years was −0.57 ± 1.68 D for SVCL wearers and −0.19 ± 1.61D for the MFCL wearers) in comparison to the rate of progression in another study with younger children (myopic advancement at the end of the 2nd year for the SVCL wearers was −1.03 ± 0.06 D and −0.51 ± 0.06 for the MFCL wearers).[17]
The reason for conducting this current study over 1½ years was that several previous myopia control studies, including spectacles multifocal[22] and atropine intervention,[10] reported that myopia control treatment was limited to the 1st year of treatment, and after the 1st year both treatment and control participants progressed at similar rates. This research showed a statistically significant change of myopia progression between SVCL wearers and multistage MFCL (−0.13 ± 0.10D vs. +0.05 ± 0.15D, P = 0.023), but no significant change between Proclear and SVCL wearers (−0.13 ± 0.10D vs. −0.006 ± 0.15D, P = 0.073) for the following 6-month period after 1st year of treatment. Therefore, more studies are needed to determine the efficacy of contact lenses in halting myopia progression over several years.
The findings of our current study indicated no statistically significant changes in the corneal curvature between the initial visit and the last visit after 18 months of wearing the contact lenses among the three groups (SVCL, P = 0.90), (multistage +1.50D, P = 0.78), and (Proclear +3.00D, P = 0.05). This result indicated that wearing the contact lenses over 18 months had no impact on changing the corneal curvature and did not flatten the cornea. Moreover, the contact lens material, diameter, and base curve, which could normally affect the corneal curvature, were similar between the three different investigated lenses. We can deduce that the control of myopia progression in both treatment groups was purely due to the slowdown of the axial elongation.
Multistage +1.50D and Proclear +3.00D soft MFCL with center distance design controlled the progression of myopia by 38.6% and 66.6%, respectively, in comparison to the SVCL lens control group. It was important for this decrease in myopic progression to be linked with a nearly similar reduction in the rate of axial elongation. However, in terms of axial elongation, no significant differences were revealed among the groups over the 18-month period. The results of this study were comparable to the findings of several previous studies. Anstice and Philips found a 37% decrease in myopic progression and a 49% reduction in axial length elongation over a period of 10 months.[20] The researchers used Dual-focus soft contact lenses (add power +2.00D) on 11- to 14-year-old children with them wearing the treatment lens in one eye and SVCL in the another eye for 10 months, then the lenses were swapped for another 10 months. Although there were significant differences in mean progression of myopia between the three groups in our research, the results showed no statistically significant difference among the groups in the axial elongation. Moreover, a strong negative correlation was shown in the MFCL wearers in our study between SE and axial length at baseline, and this correlation was maintained along the study period at 6, 12, and 18 months. No change in the degree of correlation was noted along the study periods meaning axial elongation matched the myopia progression in our study. With regard to myopia progression, our study is in accordance with Walline et al., whose participants, 27 children aged between 8 and 11 years old, used Proclear +2.00D MFCL.[21] The authors found that Proclear MFCL slowed the progression of myopia by 50%, while axial length was controlled by only 29.3% over 2 years of treatment. In the Walline et al. study, the reasons for myopia progression not matching the axial elongation might have been due to the 5-year variance in data gathering between the control group (September 2003–October 2004) and the treatment group (June 2007–May 2009). Furthermore, the data were retrospectively matched for age and gender with a previous SVCL study. In our study, the lack of significant axial length reduction could be due to the high SD in axial length results among the three groups. Our small sample size may also account for this lack of significance. In addition, immersion A-scans are known to be superior and more accurate than the ultrasound application technique,[23] which are very sensitive to fear, tension, and abnormal breathing.
Most of the previous studies used +2.00D addition, and the range of myopia control ranged between 33% and 50%. The highest addition power of +2.50D add in MFCL to control myopia in children was used by Lam et al., with DISC.[7] Although the addition used was very close to the Proclear MFCL addition used in this research (Proclear +3.00D MFCL), the control of myopia progression was 25%, and axial elongation was 31% in comparison to SVCL group over 2 years of the study. This differs from our finding where using Proclear +3.00D MFCL exhibited up to 66% myopia control. On the other hand, in their study, participants who wore contact lenses an average of 5 h/day were found to have a greater reduction in myopia progression by 50% in comparison to the control group.[7] Possibly, by increasing the addition power and lens wear duration in distance center MFCL, one could achieve a greater reduction of myopia progression. Another study suggested prescribing the addition power of multifocal/bifocal soft contact lenses based on neutralizing the associated esophoria in children, resulting in better control of myopia progression (up to 70%) compared to the single-vision group.[8] In our study, the results also showed that a +3.00D add for the Proclear MFCL was the optimal choice as it could halt the progression of myopia while maintaining near normal lag of accommodation (1.10 ± 0.83D) and exophoria (−0.31 ± 2.49PD).
The first major strength of our current research is the fact that it was a double-masked, prospective, randomized controlled clinical trial. Second, the same two researchers examined both groups of children to reduce the possibility of interexaminer discrepancies. Another important strength is the relatively long follow-up period. The reason for conducting this current study over 1½ years was that several previous myopia control studies, including spectacles multifocal,[22] and atropine intervention,[10] reported that myopia control treatment was limited to the 1st year of treatment, and after the first year, both control and treatment participants progressed at the same rates. This research showed a statistically significant change of myopia progression between SVCL wearers and multistage MFCL (−0.13 ± 0.10D vs. +0.05 ± 0.15D, P = 0.02), but no significant difference between Proclear and SVCL wearers for the following 6-month period after 1st year of treatment, which signifies the importance of longer follow-up periods.
There were several limitations in this study. First, the inclusion power of SE was limited to range from −2.00D to −6.00D, which decreased the chance of recruiting sufficient numbers of participants in Kuala Lumpur. Second, the dropout rate was high in this longitudinal study (19%). The main reason for dropout in this study was the hassle of wearing and cleaning the contact lenses among these children. The sample size was another limitation in this study. The recruitment was insufficient due to the difficulty in convincing parents, difficulties in transportation, language barrier, and misbeliefs about the dangers of wearing contact lenses. In addition, we were not able to obtain data on vision with the +3.00 D add, which is very important, as many clinicians may believe that the vision with a +3.00 D add may not be sufficient. Finally, myopia progression typically arrests at the age of 16,[24] making our selection of age range suboptimal. Since the study period is not in full years, seasonal differences in progression might play a role. Even in places close to the equator, there is a marked seasonal difference in the progression of myopia, which might limit the interpretation of our study.
CONCLUSION
There appear to be advantages with the use of daily soft MFCL over 8 h/day to reduce myopic progression up to 66% and axial elongation up to 63% among myopic schoolchildren. Based on the observations of this study, it can be suggested that prescribing MFCL with higher add powers might be a superior option compared to SVCL in halting the progression of myopia in children. The treatment effect of MFCL might be of clinical significance; however, further studies are needed with larger samples to identify the safest modality of treatment, providing a clinically significant management of myopic advancement in children.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The researchers would like to acknowledge SEED Co., Japan, for providing the contact lenses and solutions used in this study.
Many thanks to all the staff in the Optometry and Vision Science Program, School of Health Science, UKM, for the valuable guidance and assistance.
Thanks to all the children who participated, cooperated, and complied to wearing their contact lenses during this study, with special thanks to their families for taking part in this research.
REFERENCES
- 1.Lu B, Congdon N, Liu X, Choi K, Lam DS, Zhang M, et al. Associations between near work, outdoor activity, and myopia among adolescent students in rural china: The xichang pediatric refractive error study report no 2. Arch Ophthalmol. 2009;127:769–75. doi: 10.1001/archophthalmol.2009.105. [DOI] [PubMed] [Google Scholar]
- 2.Wu PC, Chen CT, Lin KK, Sun CC, Kuo CN, Huang HM, et al. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology. 2018;125:1239–50. doi: 10.1016/j.ophtha.2017.12.011. [DOI] [PubMed] [Google Scholar]
- 3.Chung K, Mohidin N, O’Leary DJ. Undercorrection of myopia enhances rather than inhibits myopia progression. Vision Res. 2002;42:2555–9. doi: 10.1016/s0042-6989(02)00258-4. [DOI] [PubMed] [Google Scholar]
- 4.Adler D, Millodot M. The possible effect of undercorrection on myopic progression in children. Clin Exp Optom. 2006;89:315–21. doi: 10.1111/j.1444-0938.2006.00055.x. [DOI] [PubMed] [Google Scholar]
- 5.Edwards MH, Li RW, Lam CS, Lew JK, Yu BS. The Hong Kong progressive lens myopia control study: Study design and main findings. Invest Ophthalmol Vis Sci. 2002;43:2852–8. [PubMed] [Google Scholar]
- 6.Cheng D, Woo GC, Drobe B, Schmid KL. Effect of bifocal and prismatic bifocal spectacles on myopia progression in children: Three-year results of a randomized clinical trial. JAMA Ophthalmol. 2014;132:258–64. doi: 10.1001/jamaophthalmol.2013.7623. [DOI] [PubMed] [Google Scholar]
- 7.Lam CS, Tang WC, Tse DY, Tang YY, To CH. Defocus incorporated soft contact (DISC) lens slows myopia progression in Hong Kong Chinese schoolchildren: A 2-year randomised clinical trial. Br J Ophthalmol. 2014;98:40–5. doi: 10.1136/bjophthalmol-2013-303914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aller TA, Liu M, Wildsoet CF. Myopia control with bifocal contact lenses: A Randomized clinical trial. Optom Vis Sci. 2016;93:344–52. doi: 10.1097/OPX.0000000000000808. [DOI] [PubMed] [Google Scholar]
- 9.Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A, et al. Atropine for the treatment of childhood myopia: Safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the treatment of myopia 2) Ophthalmology. 2012;119:347–54. doi: 10.1016/j.ophtha.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 10.Chua WH, Balakrishnan V, Chan YH, Tong L, Ling Y, Quah BL, et al. Atropine for the treatment of childhood myopia. Ophthalmology. 2006;113:2285–91. doi: 10.1016/j.ophtha.2006.05.062. [DOI] [PubMed] [Google Scholar]
- 11.Lipson MJ, Brooks MM, Koffler BH. The role of orthokeratology in myopia control: A Review. Eye Contact Lens. 2018;44:224–30. doi: 10.1097/ICL.0000000000000520. [DOI] [PubMed] [Google Scholar]
- 12.Smith EL, 3rd, Ramamirtham R, Qiao-Grider Y, Hung LF, Huang J, Kee CS, et al. Effects of foveal ablation on emmetropization and form-deprivation myopia. Invest Ophthalmol Vis Sci. 2007;48:3914–22. doi: 10.1167/iovs.06-1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smith EL., 3rd Prentice award lecture 2010: A case for peripheral optical treatment strategies for myopia. Optom Vis Sci. 2011;88:1029–44. doi: 10.1097/OPX.0b013e3182279cfa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atchison DA, Li SM, Li H, Li SY, Liu LR, Kang MT, et al. Relative peripheral hyperopia does not predict development and progression of myopia in children. Invest Ophthalmol Vis Sci. 2015;56:6162–6170. doi: 10.1167/iovs.15-17200. [DOI] [PubMed] [Google Scholar]
- 15.Mutti DO, Sinnott LT, Mitchell GL, Jones-Jordan LA, Moeschberger ML, Cotter SA, et al. Relative peripheral refractive error and the risk of onset and progression of myopia in children. Invest Ophthalmol Vis Sci. 2011;52:199–205. doi: 10.1167/iovs.09-4826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sankaridurg P, Holden B, Smith E, 3rd, Naduvilath T, Chen X, de la Jara PL, et al. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: One-year results. Invest Ophthalmol Vis Sci. 2011;52:9362–7. doi: 10.1167/iovs.11-7260. [DOI] [PubMed] [Google Scholar]
- 17.Walline JJ, Greiner KL, McVey ME, Jones-Jordan LA. Multifocal contact lens myopia control. Optom Vis Sci. 2013;90:1207–14. doi: 10.1097/OPX.0000000000000036. [DOI] [PubMed] [Google Scholar]
- 18.Lopes-Ferreira D, Ribeiro C, Neves H, Faria-Ribeiro M, Queirós A, Villa-Collar C, et al. Peripheral refraction with dominant design multifocal contact lenses in young myopes. J Optom. 2013;6:85–94. [Google Scholar]
- 19.Kang P, Fan Y, Oh K, Trac K, Zhang F, Swarbrick H, et al. Effect of single vision soft contact lenses on peripheral refraction. Optom Vis Sci. 2012;89:1014–21. doi: 10.1097/OPX.0b013e31825da339. [DOI] [PubMed] [Google Scholar]
- 20.Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118:1152–61. doi: 10.1016/j.ophtha.2010.10.035. [DOI] [PubMed] [Google Scholar]
- 21.Walline JJ, Jones LA, Mutti DO, Zadnik K. A randomized trial of the effects of rigid contact lenses on myopia progression. Arch Ophthalmol. 2004;122:1760–6. doi: 10.1001/archopht.122.12.1760. [DOI] [PubMed] [Google Scholar]
- 22.Gwiazda J, Hyman L, Hussein M, Everett D, Norton TT, Kurtz D, et al. A randomized clinical trial of progressive addition lenses versus single vision lenses on the progression of myopia in children. Invest Ophthalmol Vis Sci. 2003;44:1492–500. doi: 10.1167/iovs.02-0816. [DOI] [PubMed] [Google Scholar]
- 23.Ademola-Popoola DS, Nzeh DA, Saka SE, Olokoba LB, Obajolowo TS. Comparison of ocular biometry measurements by applanation and immersion A-scan techniques. J Curr Opthalmol. 2015;27:110–4. doi: 10.1016/j.joco.2015.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.COMET Group. Myopia stabilization and associated factors among participants in the correction of myopia evaluation trial (COMET) Invest Ophthalmol Vis Sci. 2013;54:7871–84. doi: 10.1167/iovs.13-12403. [DOI] [PMC free article] [PubMed] [Google Scholar]


