Abstract
An iris cyst is a nonkeratinized squamous epithelial-lined space involving a layer of iris. The presentation of iris cyst can be variable-innocuous or presenting with secondary complications. The identification of whether the cyst is primary or secondary is important. The prognosis of primary iris cysts is good, as the majority does not require treatment and that of secondary iris cysts is much more capricious depending on their presentation. Their optimal management often poses a challenge for ophthalmologists. Here, we will present two cases of iris cysts with diverse presentation along with a review of the literature of this rare clinical entity.
Keywords: Implantation cysts, iris cyst, juvenile rheumatoid arthritis, primary iris stromal cyst, primary pigment epithelial iris cyst, ring cyst
INTRODUCTION
An iris cyst is a nonkeratinized squamous epithelial-lined space involving a layer of iris. A primary cyst has no recognizable etiology, congenital and occurs sporadically. A secondary cyst has a recognizable etiology-surgical or nonsurgical trauma/miotic drugs. The presentation of iris cyst can be variable-innocuous or presenting as secondary complications. The identification of whether the cyst is primary or secondary is important in deciding about the management. The prognosis of primary iris cysts is good, as the majority does not require treatment and that of secondary iris cysts is much more capricious. Proper history taking, examination on slit lamp and imaging modalities such as ultrasound biomicroscopy (UBM) or anterior segment optical coherence tomography (AS-OCT) are mandatory in detailed evaluation of iris cysts. The optimal management of secondary cysts often poses a challenge for ophthalmologists. Below are two case reports of iris cyst having diverse presentations.
UNUSUAL CASE OF RING IRIS CYST IN A CHILD WITH JUVENILE RHEUMATOID ARTHRITIS
A 7-year-old Indian girl, known case of oligoarticular juvenile rheumatoid arthritis, presented to us with painful diminution of vision in the left eye. Systemic history revealed waxing and waning pattern of knee joint swelling involving both sides for which she was on systemic immunosupressants. Visual acuity was 20/200 in the left eye and intraocular pressure was 32 mmHg. Slit-lamp examination showed anterior chamber reaction of 2 plus cells. Ring iris cyst was seen at the pupillary border [Figure 1]. UBM confirmed the diagnosis [Figure 2] and Nd: YAG laser iridotomy was performed to puncture the cyst. The right eye was within the normal limits, and it was confirmed on UBM. The anterior chamber in the left eye deepened after the laser [Figure 3]. UBM was repeated which showed the resolution of ring cyst [Figure 4], and the patient has been stable 5 years post-YAG laser.
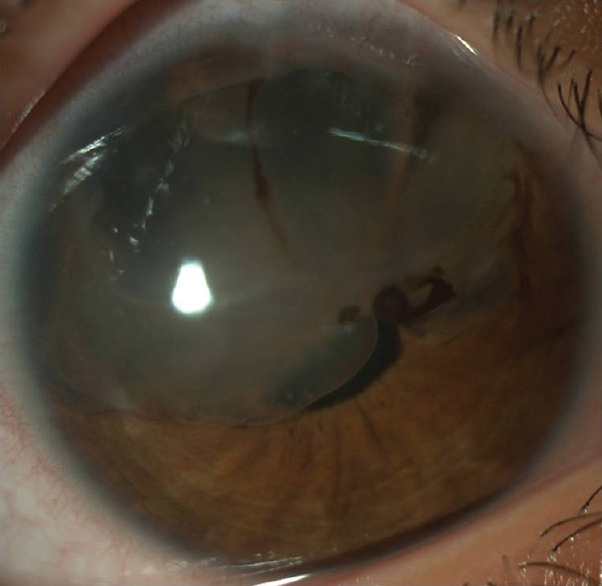
Figure 1.
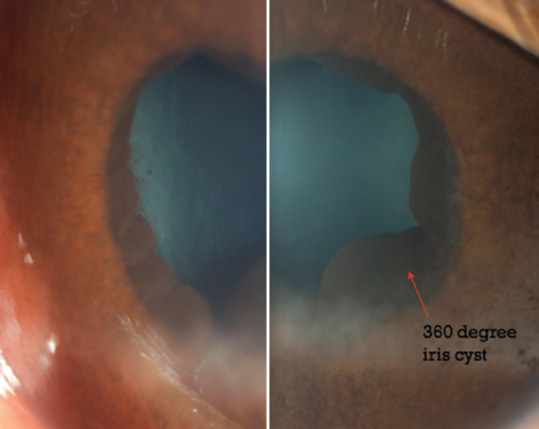
Slit-lamp photograph (25X magnification) of the left eye showing 360 degrees iris ring cyst enchroaching the pupillary border
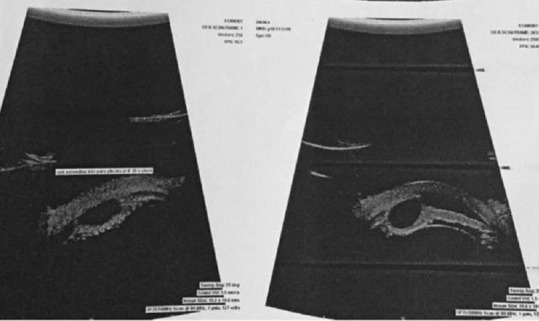
Figure 2.
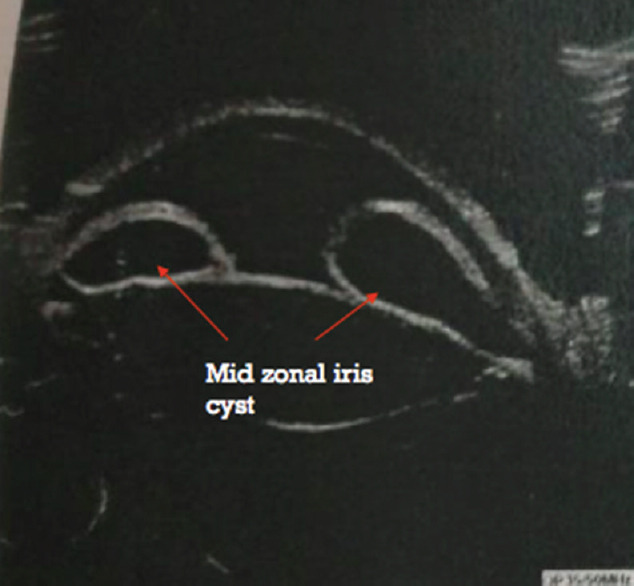
Ultrasound biomicroscopy image of the left eye at the presentation showing mid-zonal iris ring cyst
Figure 3.
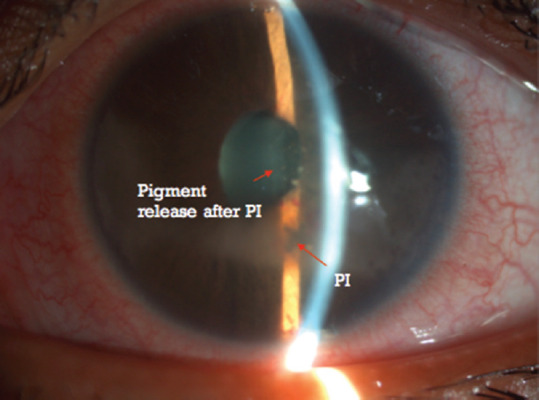
Slit-lamp photograph of the left eye showing resolved iris ring cyst and deepening of the anterior chamber after a successful paracentral Nd: YAG laser with subsequent pigment release
Figure 4.
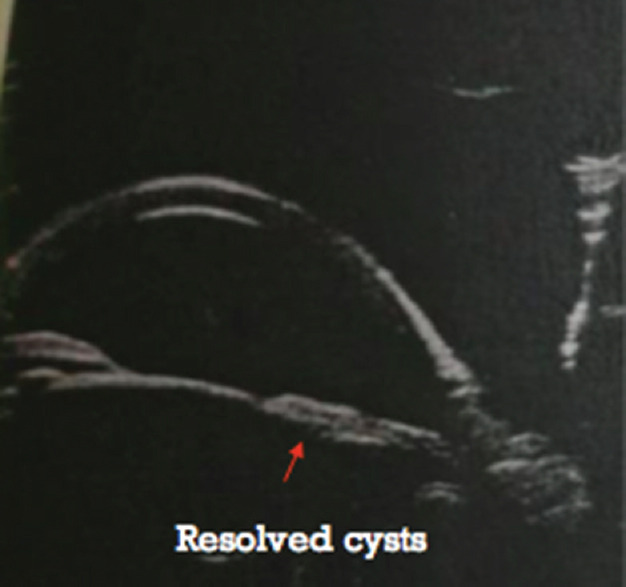
Ultrasound biomicroscopy image of the left eye postlaser showing resolved iris cysts
IMPLANTATION CYST-POST TRAUMATIC IN A 6-YEAR-OLD CHILD
A 6-year-old girl, who underwent a limbal perforation repair posttrauma with a cutter, noticed a whitish, progressive, painless membrane like structure in the right eye after 3–4 months of surgery with associated blurring of vision. Best-corrected visual acuity was 20/200 and 20/30 in the right and left eyes, respectively. The right eye showed a clear fluid filled, irregular, isolated, loculated, translucent iris cyst like structure present from 9 to 2 o’clock position covering the pupillary axis attached to the corneal endothelium which was nonmobile, no variable pigmentation/abnormal vasculature with dense iris pigments inside it [Figure 5]. A provisional diagnosis of implantation cyst postlimbal repair postpenetrating injury in the right eye was made, and the findings were confirmed on UBM [Figure 6]. Cyst aspiration-excision with sectoral iridectomy was done and histopathology of the cyst wall showed a squamous epithelium lined iris cyst with no atypia/dysplasia and no goblet cells [Figure 7]. UBM confirmed the resolution of the cyst with a best-corrected visual acuity of 20/40 in the right eye. The child has been stable for 3 years [Figure 8].
Figure 5.
Slit-lamp photograph (25X magnification) of the right eye showing clear fluid filled, irregular, isolated, loculated, translucent iris cyst present from 9 to 2 o’clock position covering the pupillary axis attached to the corneal endothelium with no variable pigmentation/abnormal vasculature with dense iris pigments inside it
Figure 6.
Ultrasound biomicroscopy image of the right eye showing clear iris cyst temporally with extension into pars plicata region from 8 to 10 o’clock position
Figure 7.
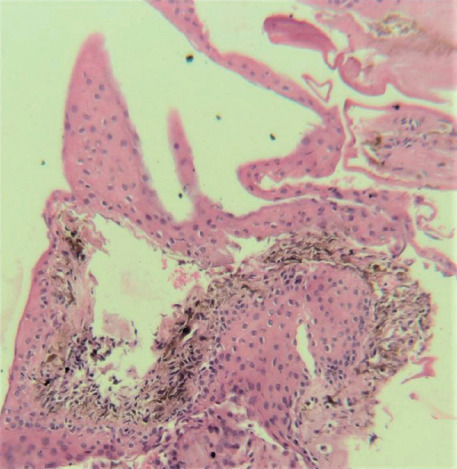
Histopathology image (10X magnification) showing iris cyst lined with normal squamous epithelium with no dysplasia or atypia with interspersed melanocytes. Goblet cells or malignant cells were not seen
Figure 8.
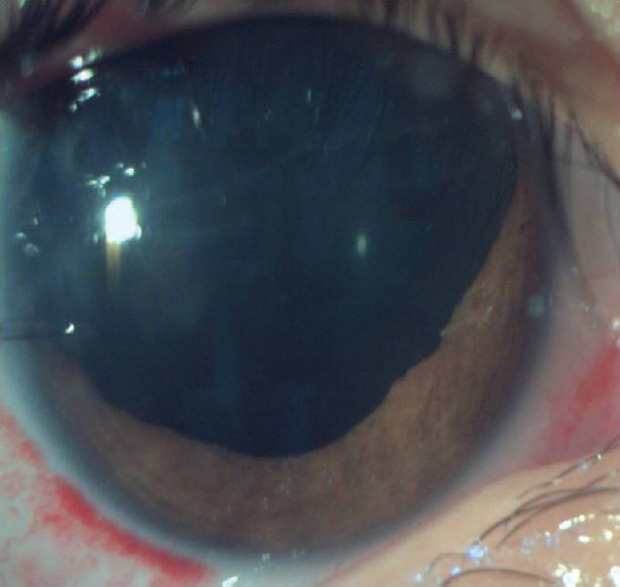
Slit-lamp photograph (10X magnification) of the right eye immediately postcyst aspiration-evacuation and sector iridectomy
REVIEW OF LITERATURE AND DISCUSSION
An iris cyst is a nonkeratinized squamous epithelial-lined space that involves a layer of the iris.[1]
Classification of iris cysts
The classification of iris cyst is given below[2,3]
-
Primary cysts
Iris pigment epithelium cysts
Iris stromal cysts
-
Secondary cysts
-
Epithelial downgrowth
- Postsurgical
- Posttraumatic
-
Cysts secondary to intraocular tumors
-
Iris melanomaMedulloepithelioma
-
- Postinflammation
-
Medication-induced
-
Miotics (phospholine iodide)Prostaglandin analogs.
-
-
Primary iris cysts are congenital, with no recognizable etiology and occur sporadically, which may not be detected until late first or second decade of life. Although rare, familial cases do occur which have an autosomal-dominant hereditary pattern with variable penetrance, and there usually is bilateral involvement with multiple cysts. No systemic abnormalities are associated with primary cysts.[3] Iris pigment epithelial cysts occur more commonly in adults while iris stromal cysts occur more in children most commonly in the 1st year of life. Based on their location, cysts have been classified previously as central at the pupillary margin, midzonal between the pupillary margin and the iris root, peripheral at the iridociliary sulcus, and dislodged to the anterior chamber or to the vitreous cavity.[1] Primary cyst most commonly arises from posterior pigment epithelial cells and is located in the peripheral iris.[4]
Iris pigment epithelial cysts are thought to be remnants of the marginal sinus of the iris that have not been obliterated. These are developmental anomalies resulting from the cystic expansion of the potential space between the pigment epithelial layers of the posterior iris. They can occur along the posterior surface of the iris, anywhere from the pupillary margin to the anterior ciliary body. The iris stromal cysts are thought to be formed by entrapped surface ectoderm tissue likely during the formation of the lens vesicle (4th week of embryogenesis) as suggested by the presence of goblet cells, positive reaction to epithelial cytokeratin markers and a negative staining for Sl00 proteins on immunocytological studies.[5,6,7,8]
There is no sex prelidiction for primary cysts. Iris pigment epithelial cysts have a brown/black, velvety appearance and typically do not transilluminate. Iris stromal cysts appear as clear masses on the anterior surface of the iris and do transilluminate.[9] Central and peripheral pigment epithelial cysts were found most commonly in young patients (20–30 years of age), whereas midzonal and dislodged cysts were seen in older patients (40–50 years of age).[3] Acquired cysts are usually unilateral, solitary, thick-walled, brilliantly transilluminant, filled with hypoechoic material corresponding to fluid and degenerated epithelial cells, mostly located in the iris stroma protruding into the anterior chamber, gradually expanding over time and with a possibility of erosion through the iris or invading the posterior chamber usually in continuity with the wound and with the signs of previous trauma/surgical intervention.
A complete ring cyst of the iris epithelium, as in our case 1 is extremely rare with only three previous case reports[10,11,12] just like ours and is formed when an abnormal membranous sac arises from the posterior aspect of the iris. Two cases had similar presentation like ours with acute congestive angle closure glaucoma and third case was postintracapsular cataract extraction surgery. The cyst cavity contains clear serous fluid in a single confluent space extending for 360° around the pupil.[13] The main differential diagnosis for a complete iris ring cyst includes iris ring melanoma and multifocal abutting cysts of the iris pigment epithelium simulating a confluent ring cyst.[10] This identity although very rare should be kept in mind when unilateral acute angle closure glaucoma is present without pupillary block, especially in children or young adults. A careful slit-lamp examination and gonioscopy with UBM becomes necessary in these cases to reach a correct diagnosis and determine the localization and extension of the cyst which in turn will help in appropriate and timely management of these cases. These cases should also be followed up regularly to rule out any recurrence of the cyst. The ring cyst in our case 1 can be primary or secondary due to inflammation (juvenile rheumatoid arthritis), although we cannot be certain of the etiology of the same. The presence of active cells can point toward a postinflammatory secondary cyst, but the cells can also be seen in a patient with acute congestive glaucoma or can be an incidental finding.
The pathogenesis of iris cyst postinstillation of prostaglandin analogs is uncertain; however, the increased uveoscleral outflow may contribute to cyst formation by changing the fluid dynamics through the interepithelial space of the posterior iris. These drugs could also have acted directly on the cyst-lining epithelial cells and thereby increased intracavitary fluid secretion. An alternative mechanism could be inflammation due to subclinical uveitis commonly associated with these drugs.[14] These secondary cysts are reversible on stopping the offending drugs; however, they have a tendency of recurrence once the drug is reinstilled.[14,15]
Depending on the size, location, and compression of adjacent structures, the following complications may occur secondary to iris cysts:[4]
Secondary angle-closure glaucoma
Plateau iris syndrome
Secondary pigment dispersion syndrome
Corneal edema
Focal cataract
Lens subluxation
Iritis.
The following may be considered in the differential diagnosis of iris cysts:[4]
-
Solid
-
Melanocytic
- Nevus
- Melanocytoma
- Melanocytosis
- Lisch nodules
- Iris/ciliary body melanoma
-
-
Epithelial
- Iris pigment epithelium adenoma
- Medulloepithelioma.
It is very important to rule out iris melanoma when evaluating an iris cyst. Iris melanomas appear as a brown lesion arising from the stroma. Unlike primary cysts, they can be variably colored, maintain stable contour even after dilation. The presence of sentinel vessels and intrinsic vessels within the lesion is strongly suggestive of a solid tumor rather than a benign cyst.[16]
The diagnosis of iris cysts is based on thorough slit-lamp examination and UBM or AS-OCT imaging. UBM remains the gold-standard imaging due to ability to better characterize the interior of the cystic structures and to visualize well the structures behind the iris/posterior extent of the cyst.[17] Iris cysts appear round or ovoid with a thin, hyperechoic wall (due to the epithelial cell lining) and a hypoechoic interior (due to its fluid contents) with no solid component on imaging.[18] Whereas, an iris melanoma appears as a solid irregular iris mass with variable internal reflectivity, distortion of surrounding structures and irregularity or convex bowing of posterior iris plane. UBM shows multiple discrete cysts if there are multifocal abutting iris epithelial cysts extending 360° around the pupil.[11]
MANAGEMENT AND NATURAL HISTORY
Most cases of primary epithelial cysts have a benign clinical course, and the occurrence of associated complications is extremely rare. The need for the treatment is exceptional
Iris stromal cysts usually have a benign course when occurring in adulthood. In children, these cysts usually have a tendency to enlarge and block the visual axis, with the subsequent risk for amblyopia necessitating treatment as early as possible
Secondary acquired cysts posttrauma or due to epithelial downgrowth frequently enlarge in size, especially in the pediatric population owing to higher proliferating capability of the implanted epithelial sheet, causing complications necessitating management in the majority of such cases
Iris cysts that are stable and not causing symptoms or secondary complications require no treatment but should be followed regularly
Iris cysts that involve the visual axis, particularly in children at risk for amblyopia, necessitate intervention[13]
Treating iris cysts is by using a step-wise approach, starting with less-invasive treatment before proceeding to surgical excision whenever possible[19]
Iris cysts secondary to miotics (such as-phospholine iodide) are treated with phenylephrine 2.5%. Cysts also resolve with discontinuation of phospholine iodide
Argon laser photocoagulation-photocoagulation of the cyst epithelium may be able to halt production of cystic fluid contents. This may be performed to shrink the cysts, although recurrence is common. Its utility is limited in cases of large cysts and when visualization is difficult.[20,21] Associated with inflammation due to the release of the contents of the cyst and recurrence
Nd: YAG-photodisruption (laser cystostomy) of the cyst wall may allow perforation of the cyst and release of contents into the anterior chamber[22] associated with recurrences and inflammation
Cyst aspiration with injection of sclerosing agent: Aspiration of the cyst contents with subsequent injection of absolute alcohol to induce sclerosis has demonstrated good success. It is a minimally invasive method and alcohol is infused until the cyst wall turns gray, after which the alcohol is removed.[23] While recurrence is not common, this procedure can be repeated if it does occur. Other sclerosants which can be used include trichloroacetic acid, 5-Fluorouracil, and Mitomycin C.[24] The mechanism of sclerosant-induced cyst collapse is related to chemical toxic effects on the epithelial cyst lining. This procedure should be performed using exquisite care, with constant monitoring of the needle tip to avoid sclerosant leakage into the anterior chamber
En bloc excision with or without light cryotherapy While this procedure has a good success rate, there is greater risk of causing collateral damage to ocular structures[20]
Secondary iris cysts due to epithelial downgrowth may require more aggressive surgical excision and devitalization of the epithelial tissues with vitrectomy, lensectomy, and cryodestruction of residual cells at the excision site. Viscoelastics can be used to separate the cyst from the corneal endothelium so that the cyst may be excised with minimal trauma to the endothelium and adjacent ocular structures. The challenge in the surgical management of an iris cyst is to identify the complete extent of the epithelial down growth, and to ensure the removal of the cyst in toto. If the cyst is ruptured, or part of the cyst wall or associated epithelial downgrowth is left behind, there is a high chance of recurrence and postoperative inflammatory reaction. On the other hand, aggressive surgical procedures aimed at complete eradication of the proliferative epithelial tissue are likely to produce significant collateral damage to the adjacent ocular structures, which in turn, would result in a poor functional outcome[25]
Lower recurrence rates have been observed in eyes where extended cyst excision with sectoral iridectomy was done for acquired implantation cysts. In cases where limited cyst resection is performed, it is possible that with just cyst aspiration and removal with underlying intact iris, some cells from the cyst wall may be retained on the iris predisposing to recurrence. In eyes where broad-based surgical iridectomy has been done, this problem of retained cells in the iris may not arise.[26]
CONCLUSION
The presentation of iris cyst can be variable-innocuous, compression of adjacent structures or presenting as secondary complications. The identification of whether the cyst is primary or secondary is important. The prognosis of primary iris cysts is good, as the majority do not require treatment. Recurrence after excision is more common in stromal cysts than pigment epithelial cysts. The prognosis of secondary iris cysts is much more variable. Their optimal management often poses a challenge for ophthalmologists and is a two-edged sword. The basic principle in the surgical management of secondary iris cysts is complete excision of the proliferative epithelial tissue which constitutes the cyst wall, and the associated epithelial downgrowth, while keeping the collateral tissue damage at a minimum level. Complete cyst excision with sector iridectomy is an effective treatment option for acquired cysts if other less invasive surgical approaches fail.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient (s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initial s will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Shields JA. Primary cysts of the iris. Trans Am Ophthalmol Soc. 1981;79:771–809. [PMC free article] [PubMed] [Google Scholar]
- 2.Shields JA, Kline MW, Augsburger JJ. Primary iris cysts: A review of the literature and report of 62 cases. Br J Ophthalmol. 1984;68:152–66. doi: 10.1136/bjo.68.3.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lois N, Shields CL, Shields JA, Mercado G. Primary cysts of the iris pigment epithelium. Clinical features and natural course in 234 patients. Ophthalmology. 1998;105:1879–85. doi: 10.1016/S0161-6420(98)91034-X. [DOI] [PubMed] [Google Scholar]
- 4.Shields CL, Kancherla S, Patel J, Vijayvargiya P, Suriano MM, Kolbus E, et al. Clinical survey of 3680 iris tumors based on patient age at presentation. Ophthalmology. 2012;119:407–14. doi: 10.1016/j.ophtha.2011.07.059. [DOI] [PubMed] [Google Scholar]
- 5.Grutzmacher RD, Lindquist TD, Chittum ME, Bunt-Milam AH, Kalina RE. Congenital iris cysts. Br J Ophthalmol. 1987;71:227–34. doi: 10.1136/bjo.71.3.227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Naumann G, Green WR. Spontaneous nonpigmented iris cysts. Arch Ophthalmol. 1967;78:496–500. doi: 10.1001/archopht.1967.00980030498016. [DOI] [PubMed] [Google Scholar]
- 7.Paridaens AD, Deuble K, McCartney AC. Spontaneous congenital non-pigmented epithelial cysts of the iris stroma. Br J Ophthalmol. 1992;76:39–42. doi: 10.1136/bjo.76.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lois N, Shields CL, Shields JA, Mercado G, De Potter P. Primary iris stromal cysts. A report of 17 cases. Ophthalmology. 1998;105:1317–22. doi: 10.1016/S0161-6420(98)97041-5. [DOI] [PubMed] [Google Scholar]
- 9.Iris Abnormalities- Primary Iris Cysts: AAO Basic and Clinical Science: Section 6- Paediatric Ophthalmology and Strabismus- The Eye MD association. Elsivier. 2013 [Google Scholar]
- 10.Laham A, Corrêa ZM, Augsburger JJ, Heur M. Complete ring cyst of iris pigment epithelium documented by ultrasound biomicroscopy. Ophthalmic Surg Lasers Imaging. 2009;40:495–7. doi: 10.3928/15428877-20090901-10. [DOI] [PubMed] [Google Scholar]
- 11.Bron AJ, Wilson CB, Hill AR. Laser treatment of primary ring-shaped epithelial iris cyst. Br J Ophthalmol. 1984;68:859–65. doi: 10.1136/bjo.68.12.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turati M, Flores-Sánchez BC, Isida-Llerandi CG, Kahook M, Gil-Carrasco F. Iris ring cyst. Case report. Rev Mex Oftalmol. 2013;87:59–63. [Google Scholar]
- 13.Kozart DM. Echographic evaluation of primary cysts of the iris pigment epithelium. Am J Ophthalmol. 1996;121:100–1. doi: 10.1016/s0002-9394(14)70544-6. [DOI] [PubMed] [Google Scholar]
- 14.Krohn J, Hove VK. Recurrent iris pigment epithelial cyst induced by topical prostaglandin F2α analogues. Arch Ophthalmol. 2008;126:867–8. doi: 10.1001/archopht.126.6.867. [DOI] [PubMed] [Google Scholar]
- 15.Browning DJ, Perkins SL, Lark KK. Iris cyst secondary to latanoprost mimicking iris melanoma. Am J Ophthalmol. 2003;135:419–21. doi: 10.1016/s0002-9394(02)01953-0. [DOI] [PubMed] [Google Scholar]
- 16.Melanoma I. Amsterdam, Netherlands: Elsevier; 2013. AAO Basic and Clinical Science Course Section 4: Ophthalmic Pathology and Intraocular Tumors. [Google Scholar]
- 17.Hau SC, Papastefanou V, Shah S, Sagoo MS, Restori M, Cohen V. Evaluation of iris and iridociliary body lesions with anterior segment optical coherence tomography versus ultrasound B-scan. Br J Ophthalmol. 2015;99:81–6. doi: 10.1136/bjophthalmol-2014-305218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marigo FA, Esaki K, Finger PT, Ishikawa H, Greenfield DS, Liebmann JM, et al. Differential diagnosis of anterior segment cysts by ultrasound biomicroscopy. Ophthalmology. 1999;106:2131–5. doi: 10.1016/S0161-6420(99)90495-5. [DOI] [PubMed] [Google Scholar]
- 19.Georgalas I, Petrou P, Papaconstantinou D, Brouzas D, Koutsandrea C, Kanakis M. Iris cysts: A comprehensive review on diagnosis and treatment. Surv Ophthalmol. 2018;63:347–64. doi: 10.1016/j.survophthal.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 20.Haller JA, Stark WJ, Azab A, Thomsen RW, Gottsch JD. Surgical management of anterior chamber epithelial cysts. Am J Ophthalmol. 2003;135:309–13. doi: 10.1016/s0002-9394(02)01960-8. [DOI] [PubMed] [Google Scholar]
- 21.Leung EW, Mehta JR, Croasdale CR. Laser photocoagulation of primary central pigment epithelial iris cysts. Arch Ophthalmol. 2005;123:1276. doi: 10.1001/archopht.123.9.1276. [DOI] [PubMed] [Google Scholar]
- 22.Baranwal VK, Kumar S, Gaur S, Satyabala K, Dutta AK, Murthy PK. An uncommon case of primary iris cyst managed with Nd YAG laser. Med J Armed Forces India. 2015;71:S82–4. doi: 10.1016/j.mjafi.2013.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Behrouzi Z, Khodadoust A. Epithelial iris cyst treatment with intracystic ethanol irrigation. Ophthalmology. 2003;110:1601–5. doi: 10.1016/s0161-6420(03)00543-8. [DOI] [PubMed] [Google Scholar]
- 24.Shields CL, Arepalli S, Lally EB, Lally SE, Shields JA. Iris stromal cyst management with absolute alcohol-induced sclerosis in 16 patients. JAMA Ophthalmol. 2014;132:703–8. doi: 10.1001/jamaophthalmol.2014.160. [DOI] [PubMed] [Google Scholar]
- 25.Philip SS, John DR, Ninan F, John SS. Surgical management of post-traumatic iris cyst. Open Ophthalmol J. 2015;9:164–6. doi: 10.2174/1874364101509010164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shanbhag SS, Ramappa M, Chaurasia S, Murthy SI. Surgical management of acquired implantation iris cysts: Indications, surgical challenges and outcomes. Br J Ophthalmol. 2019;103:1179–83. doi: 10.1136/bjophthalmol-2018-312738. [DOI] [PubMed] [Google Scholar]


