Abstract
The nano-sized iron oxide (Fe2O3-NPs) is one of the most used engineered nanomaterials worldwide. This study investigated the efficacy of natural polyphenol resveratrol (RSV) (20 mg/kg b.wt, orally once daily) to alleviate the impaired sperm quality and testicular injury resulting from Fe2O3-NPs exposure (3.5 or 7 mg/kg b.wt, intraperitoneally once a week) for eight weeks. Spermiograms, sexual hormonal levels, oxidative stress indicators, and lipid peroxidation biomarker were assessed. Moreover, the steroidogenesis-related genes mRNA expressions were evaluated. The results showed that RSV substantially rescued Fe2O3-NPs-mediated sperm defects. Additionally, the Fe2O3-NPs-induced depressing effects on sperm motility and viability were markedly counteracted by RSV. Moreover, RSV significantly restored Fe2O3-NPs-induced depletion of testosterone, follicle-stimulated hormone, luteinizing hormone, and testicular antioxidant enzymes but reduced malondialdehyde content. Furthermore, the Fe2O3-NPs-induced downregulation of steroidogenesis-related genes (3 β-HSD, 17 β-HSD, and Nr5A1) was significantly counteracted in the testicular tissue of RSV-treated rats. These findings concluded that RSV could limit the Fe2O3-NPs-induced reduced sperm quality and testicular injury most likely via their antioxidant activity and steroidogenesis-related gene expression modulation.
Keywords: iron oxide nanoparticles, resveratrol, male sex hormones, oxidative stress, steroidogenesis-related genes
1. Introduction
Incorporating engineered nanomaterials into nanotechnology applications has reached far across various fields, contributing to substantial nanoparticle (NPs) emissions in the surrounding environment [1,2]. The nanosized iron oxide (Fe2O3-NPs) is classified as one of Europe’s most used engineered nanomaterials for coating products, masts, fillers, plasters, non-metal surface treatment products, clay modeling products, and metal surface therapy products [3]. Fe2O3-NPs is also significant for its extensive uses, such as magnetic resonance imaging (MRI) [4], inducing magnetic hyperthermia for cancer treatment [5], carriers for targeted drug delivery [6], and tissue repair via soldering or welding [7].
Despite the broad applications of Fe2O3-NPs, some in vitro and in vivo studies have reported its toxic effects, including cytotoxicity [8], genotoxicity [9], hepatotoxicity [10], neurotoxicity [11], and pulmonary toxicity [12]. Oxidative stress has been implicated as a central mechanism for Fe2O3-NPs-induced injuries [13]. Moreover, the contribution of the iron ions released from Fe2O3-NPs in Fenton’s reaction resulting in oxidative damage has been confirmed [14,15,16].
Some recent studies showed that Fe2O3-NPs are harmful to sperm and testicular tissue. For instance, Sundarraj et al. [15] verified the testicular toxicity in mice following Fe2O3-NPs (25 and 50 mg/kg) intraperitoneal administration for four weeks. Furthermore, Sundarraj et al. [17] revealed that the oral dosing of 25 and 50 mg/kg b.wt Fe2O3-NPs in mice for 30 consecutive days adversely affected the prostate gland and seminal vesicle Additionally, the intraperitoneal dosing of Fe2O3-NPs (300 mg/kg b.wt) for four days induced a substantial decrease in sperm characteristics, including motility, spermatogonia, primary sperm cells, spermatids, Leydig cells, Sertoli, total tubular length, and the volumes of interstitial testicular tissue [18]. However, the underlying mechanisms of Fe2O3-NPs-induced testicular toxicity still need further investigation.
In this period, an increasing interest is directed to using natural supplements as therapeutic or protective interventions for male fertility disorders [19,20,21,22,23]. Resveratrol (RSV) is a natural phytoalexin antioxidant found in numerous plants, including grapes, blueberries, and peanuts [24,25]. RSV has attracted more attention due to its various biological activities, including antioxidative, anti-inflammatory, cytoprotective, and antiaging effects [26,27,28,29,30]. The RSV antioxidant effect is considered the fundamental mechanism of its health benefits [31]. Moreover, RSV showed potent therapeutic roles against various diseases, including respiratory viral infections [32], Alzheimer’s disease [33], diabetes mellitus [34], and renal diseases [35]. Recent in vivo and in vitro studies have shown that RSV protects sperm cells against lipid peroxidation and augments sperm viability and mitochondrial membrane potential [36,37,38]. Yet, to our knowledge, its ameliorative potentials against Fe2O3-NPs-induced testicular damage have not been investigated.
Hence, we hypothesized that RSV could offer protection against Fe2O3-NPs-induced reduced sperm quality and testicular injury in rats. To test this hypothesis, semen assessment, male sex hormones, testicular antioxidants enzymes, and lipid peroxidation indicators were assessed. Additionally, the expression of genes associated with steroidogenesis was studied in order to determine the probable mechanisms behind it.
2. Materials and Methods
2.1. Chemicals
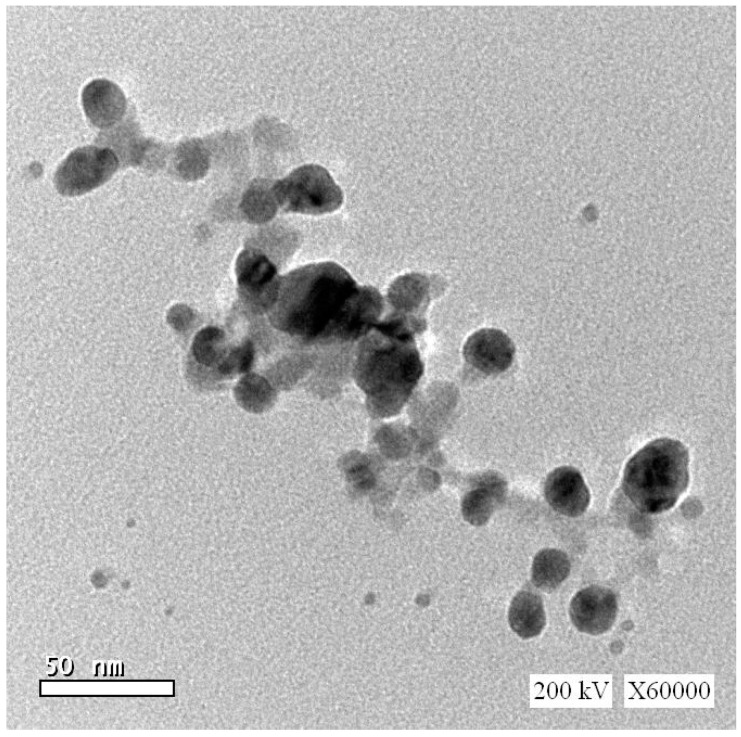
Fe2O3 nanopowder (Fe2O3-NPs, CAS registry number 1309-37-1, catalog number 544884, 99.5% purity, 0.05–0.24 m2/kg surface area, <50 nm diameter), RSV (CAS registry number 501-36-0, purity ≥ 99%), epinephrine, reduced glutathione, NADPH, and 5,5 dithiobis 2-nitrobenzoic acid (DTNB) were attained from Sigma-Aldrich (St. Louis, MO, USA). The Fe2O3-NPs transmission electron microscopy diffraction pattern is shown in Figure 1. All other reagents were obtained from the El-Nasr Company (Cairo, Egypt).
Figure 1.
Transmission electron microscopy diffraction patterns for iron oxide nanoparticles.
2.2. Animals and Experimental Design
Adult male Wistar albino rats (9 weeks old, 0.15–0.16 kg) were kindly obtained from the Animal House at the Faculty of Veterinary Medicine, Zagazig University, Sharkia, Egypt. They were maintained under standard laboratory conditions with free access and water in standard cages with 12 h/12 h dark-light cycles. The experiments were carried out in line with the Ethics Committee of the Faculty of Veterinary Medicine, Zagazig University. After two weeks of acclimation, fifty-four rats were arbitrarily allotted into six groups (9 rats/group). The control group rats received normal saline. The RSV-treated group of rats were orally given 20 mg RSV/kg b.wt once daily. The low and high Fe2O3-NPs-exposed groups of rats were, respectively, given intraperitoneal (IP) injections of 3.5 and 7 mg/kg b.wt Fe2O3-NPs dissolved in physiological saline, once a week. The RSV+low Fe2O3-NPs-exposed group of rats were concurrently treated with RSV and a low dose of Fe2O3-NPs at the abovementioned route and dose. The RSV+high Fe2O3-NPs group of rats were treated with RSV and a high dose of Fe2O3-NPs at the aforementioned dose and route. The experiment extended for eight weeks to cover the duration of spermatogenesis in rats, ranging from 56–60 days [39]. The protocol was permitted by the Institutional Animal Care and Use Committee of Zagazig University (IACUC), Egypt, with approval number (ZU-IACUC/2/F/44/2021). All efforts were made to handle the rats humanely and abide by ethical rules.
2.3. The Dose and Route Selection of RSV and Fe2O3-NPs
The selected RSV oral dose (20 mg RSV/kg b.wt ) has been reported to counteract the testicular toxicity of several environmental contaminants like cadmium [40] and cypermethrin [41]. Additionally, the oral dose of 20 mg RSV/kg b.wt enhanced the rats’ spermatogenesis after 2, 5-hexanedione exposure [42] and is safe in rats [43].
The IP route was selected as a route of administration based on the toxicokinetic studies that confirmed the invasion of Fe2O3-NPs in different body organs and testis following the intraperitoneal administration [44]. Moreover, comparable toxicological outcomes have been gained through other routes of administration of Fe2O3-NPs. For instance, Fe2O3-NPs have been shown to cross the blood–brain barrier, inducing neurotoxic impacts after oral [45], inhalation [46], and intraperitoneal [47] administration. Additionally, Fe2O3-NPs displayed a lack of genotoxicity following oral [9], IP [48], and intravenous routes [49]. In addition, the IP injection is a common route for administering Fe2O3-NPs into the body during biomedical applications [50]. Regarding Fe2O3-NPs doses selection, Prodan et al. [51] found that the IP injection of Fe2O3-NPs up to 3.7 mL/kg (equivalent to nearly 3.5 mg/kg b.wt) in Brown Norway rats did not induce significant changes in the liver, spleen, or lungs morphology. Nevertheless, the effects of the earlier dose on the testes have not been investigated. Hence, herein, the dose of 3.5 mg/kg b.wt was tested as a low dose and its double (7 mg/kg b.wt) as the high dose.
2.4. Blood and Tissue Sampling
All rats were fasted overnight, weighed, and blood samples were collected in non-heparinized tubes at the end of the trial using a retro-orbital plexus site. The serum samples were separated by centrifugation at 1075× g for 10 min and stored at −20 °C for further hormonal analysis. After rats were anesthetized by an intramuscular injection of xylazine (5 mg/kg b.wt) and ketamine hydrochloride (50 mg/kg b.wt); euthanized by cervical dislocation; and the testes were harvested, cleaned of surrounding tissues, and weighed with an electronic analytical balance. The gonadosomatic index was calculated according to the following equation: (The average of the right and left testicle weights (g)/the final body weight (g)) × 100 [52]. One side of rat testes was necropsied then directly transmitted in liquid nitrogen to be kept at −80 °C for gene expression. One gram of other-sided ones was homogenized using a tissue homogenizer (Potter–Elvehjem, Thomas Scientific, Swedesboro, NJ, USA) in chilled potassium chloride followed by centrifugation at 3000 rpm for 10 min at 4 °C to collect supernatant that was used to assess the antioxidant status of testicular tissue.
2.5. Semen Analysis
The epididymal content of each rat in different experimental groups was obtained by directly cutting the caudal epididymis and smoothly pressing it in a clean petri dish containing 2 mL of pre-warmed physiological saline solution and incubating it at for 30 min 37 °C for liquefaction. The sperm progressive motility was evaluated according to Slott et al. [53] method. One drop of the aforementioned prepared solution was placed on a pre-warmed slide with 80-µm-deep chambers. Then, a high-power light microscope was used to measure the motile spermatozoa percentage in numerous microscopic fields at 400× magnification. Using a hemocytometer, total sperm count was determined in semen diluted with physiological saline at 1:4 with 5 drops of formalin (40%) solution. The total sperm count was calculated as the sum of counted spermatozoa in five secondary square × dilution rate × 2500 and expressed as the total number of spermatozoa/mL [54]. Sperm viability and abnormalities were determined according to the protocol of Filler [55]. A drop of the epididymal content of each rat was mixed with the same amount of eosin–nigrosin stain and spread on grease-free clean slides for the microscopical examination of anomalies in the tail, neck/middle part, and head.
2.6. Hormonal Assay
Following the guidelines of manufacturer’s protocols, testosterone (TES), follicle-stimulating hormone (FSH), and luteinizing hormone (LH) were assessed via rat-specific enzyme-linked immunosorbent assay (ELISA) kits no. MBS282195, MBS2502190, and MBS764675, respectively (MyBioSource, San Diego, CA, USA), following the manufacturer’s instructions.
2.7. Testicular Oxidative/Antioxidant Status
In testes homogenate, the superoxide dismutase (SOD), catalase (CAT), glutathione peroxidase (GPx), reduced glutathione (GSH), and malondialdehyde (MDA) levels were determined using kits reagents of Bio-diagnostic Co., Giza, Egypt (Catalogue no. SD 25 21, CA 25 17, GP 2524, GR 25 11, and MD 25 29, respectively) following the methods applied by Nishikimi et al. [56], Aebi [57], Paglia and Valentine [58], Beutler [59], and Ohkawa et al. [60], respectively.
2.8. Extraction of Total RNA and Real Time-PCR
The total RNA of the testes samples was isolated by Rneasy mini kit (Qiagen) in line with the manufacturer’s protocol guidelines and as previously described [61]. The high quality of RNA samples was tested by 1% gel electrophoresis, and the purity of RNA samples was determined by obtaining the optical density at 260 and 280 nm. Then, 2 µg of total RNA was used to produce cDNA using the RevertAid H minus Reverse Transcriptase kit (Catalog number: EP0451, Thermo Scientific, Waltham, MA, USA). Real-time quantitative PCR was performed by StepOnePlus system (Applied Biosystem, Foster City, CA, USA), where 25 µL PCR reaction mixture was prepared using cDNA (150 ng), forward primer (1 µm), reverse primer (1 µm), Maxima SYBR Green (Catalog number: K0221, Thermo Scientific, Waltham, MA, USA) (12.5 µL), and Rnase free water (Catalog number: 129112, Qiagen Inc., Valencia, CA, USA) (till 25 µL). Rotor-Gene Q2 plex (Qiagen Inc., Valencia, CA, USA) was used to amplify the reaction. The primer sequence used for 3 beta-hydroxysteroid dehydrogenases (3β-HSD), 17-beta hydroxysteroid dehydrogenase (17β-HSD), and nuclear Receptor Subfamily 5 Group A Member 1 (Nr5A1), the PCR amplification condition, and product length are presented in Table 1. Β-actin was used as a housekeeping gene. The 2−ΔΔCt method was employed to compute each transcript’s relative quantity in 3 replicates. The period threshold values for the objective genes have been determined concerning the level of β-actin mRNA [62].
Table 1.
Primer sequences, accession number, and product size for the quantitative RT-PCR for the analyzed genes in the testicular tissue.
| Gene | Primer Sequences | Reaction Conditions | Accession No. | PCR Product Size | |
|---|---|---|---|---|---|
| 3β-HSD | F | 5′–GCATTAACCCCACTCCCACT–3′ | 95 °C, 10 min/60 °C, 30 s/72 °C, 5 min (35 cycles) | NM 017265 | 146 bp |
| R | 5′–GGACCCTGACCTCCTTCAGA–3′ | ||||
| 17β-HSD | F | 5′–GTGTGCACATTTTCCAAGGC–3′ | 95 °C, 10 min/60 °C, 30 s/72 °C, 5 min (35 cycles) | NM 054007 | 144 bp |
| R | 5′–TTTAACAAACTCATCGGCGG–3′ | ||||
| Nr5A1 | F | 5′–CGCCAGGAGTTTGTCTGTCT–3′ | 95 °C, 10 min/60 °C, 30 s/72 °C, 5 min (35 cycles) | NM 001191099 | 185 bp |
| R | 5′–ACCTCCACCAGGCACAATAG–3′ | ||||
| β-actin | F | 5′–CCTGCTTGCTGATCCACA–3′ | 95 °C, 10 min/60 °C, 30 s/72 °C, 5 min (35 cycles) | V01217 | 97 bp |
| R | 5′–CTGACCGAGCGTGGCTAC–3′ |
F indicates forward primer; R indicates reverse primer; 3β-HSD: 3 beta-Hydroxysteroid dehydrogenase; 17β-HSD: 17-beta hydroxysteroid dehydrogenase; Nr5A1: Nuclear Receptor Subfamily 5 Group A Member 1.
2.9. Statistical Analysis
Data were checked for the normality and homogeneity of variances using the Kolmogorov–Smirnov test and Levene’s test, respectively. Where normality assumptions were met, data were subjected to one-way analysis of variance (ANOVA) to statistically determine the variation between groups followed by Tukey’s multiple range post hoc test for pairwise comparisons. The data have been shown as means ±SD for each group. Mean differences were taken into account at p < 0.05. Moreover, the Graphpad computer program was used for regression analysis and data collection (ISI Software, Philadelphia, PA, USA).
3. Results
3.1. Effect of RSV and/or Fe2O3-NPs on the Bodyweight Change and Gonadosomatic Index
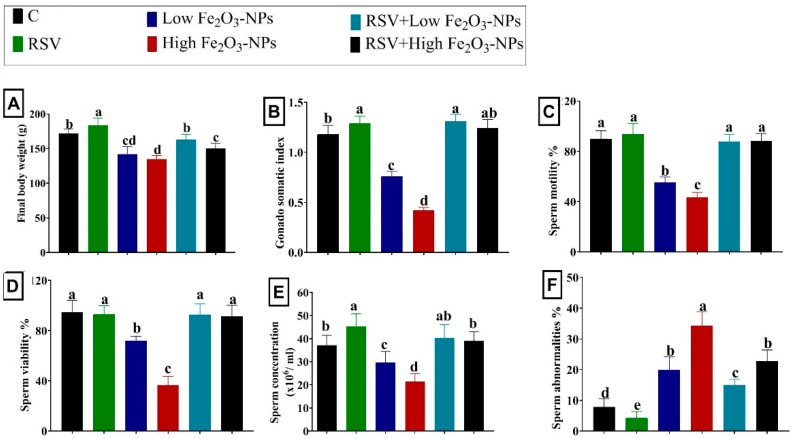
Figure 2A,B showed the final body weight and gonadosomatic index variations in rats who received RSV and/or low or high doses of Fe2O3-NPs for eight weeks. Initially, the RSV-treated rats increased (p < 0.001) in final body weight and gonadosomatic index compared to the control group. Low or high doses of Fe2O3-NPs administered to rats reduced (p < 0.001) final body weight and gonadosomatic index relative to the control group. In contrast, the RSV treatment restored (p < 0.001) the Fe2O3-NPs-induced reduction in final body weight and gonadosomatic index until they became non-significant relative to the control group.
Figure 2.
Effect of resveratrol (RSV; 20 mg/kg b.wt) and/or iron oxide nanoparticles (Fe2O3-NPs 3.5 or 7 mg/kg b.wt) administration for eight weeks on the final body weight (A); gonadosomatic index (B); sperm motility (C); viability (D); concentration (E); and abnormalities (F) of male rats. Data expressed as mean ± SD, n = 9 for each group. Different letters (a, b, c, and d) on columns indicate statistically significant differences at p < 0.05 between the different experimental groups.
3.2. Effect of RSV and/or Fe2O3-NPs on Spermiogram
As displayed in Figure 2B,C, the sperm motility percent, sperm concentration, and live sperm percentage were reduced (p < 0.001) in the low (38.37%, 20.17%, and 23.99%, respectively) and high (51.41%, 42.54%, and 61.49%, respectively) Fe2O3-NPs-exposed groups relative to the control group. The percent of sperm abnormalities, including detached and bifurcated sperm heads and short, coiled, and bent sperm tails, was increased (p < 0.001) by about twofold and threefold in the low and high Fe2O3-NPs-exposed groups, respectively, compared to the control group. In contrast, the sperm count, motility, and living sperm percentages were substantially restored by RSV oral dosing, but the sperm abnormality percentage decreased compared with Fe2O3-NPs-exposed rats. It is of note that all the spermiogram elements, except the sperm abnormalities, improved (p < 0.001) in the RSV+ Fe2O3-NPs-treated groups efficiently until they became not considerably different from those in the control group.
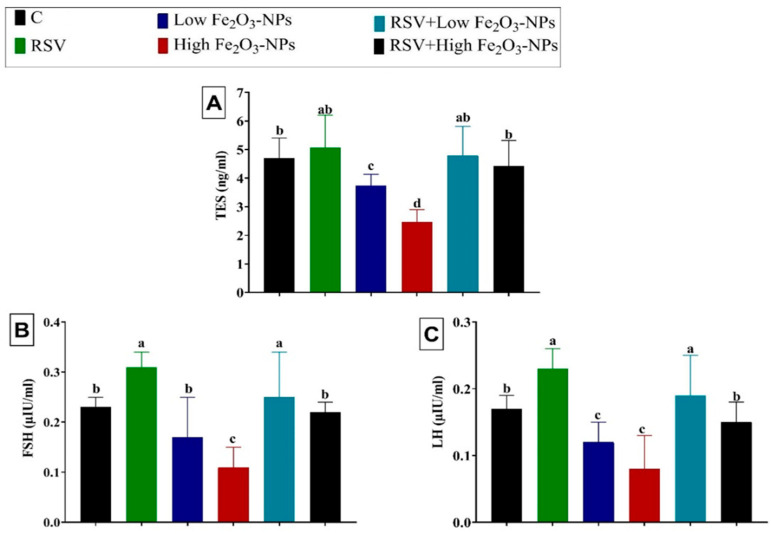
3.3. Effect of RSV and/or Fe2O3-NPs on Male Sex Hormones
As demonstrated in Figure 3, the TES, FSH, and LH levels declined (p < 0.001) in the low (6.50%, 26.09%, and 29.41%, respectively) and high (38.25%, 52.17%, and 52.94%, respectively) Fe2O3-NPs-exposed groups compared to the control group. However, RSV oral dosing reestablished (p < 0.001) the Fe2O3-NPs-induced depletion in sexual hormone levels until it became not substantially different from the control group.
Figure 3.
The effect of resveratrol (RSV; 20 mg/kg b.wt) and/or iron oxide nanoparticles (Fe2O3-NPs 3.5 or 7 mg/kg bwt) administration for eight weeks on the serum levels of male sexual hormones, including testosterone (TES) (A), follicle-stimulating hormone (FSH) (B), and luteinizing hormone (LH) (C) in male rats. Data expressed as mean ± SD, n = 9 for each group. Different letters (a, b, c, and d) on columns indicate statistically significant differences at p < 0.05 between the different experimental groups.
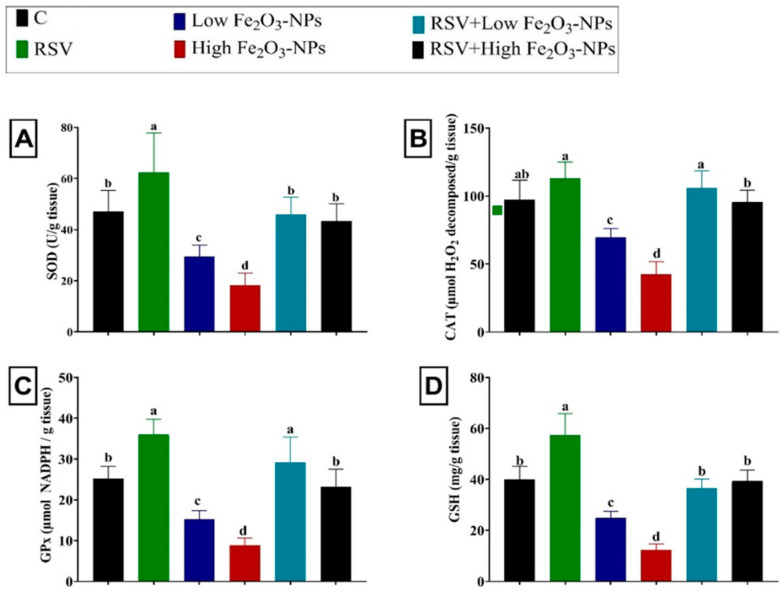
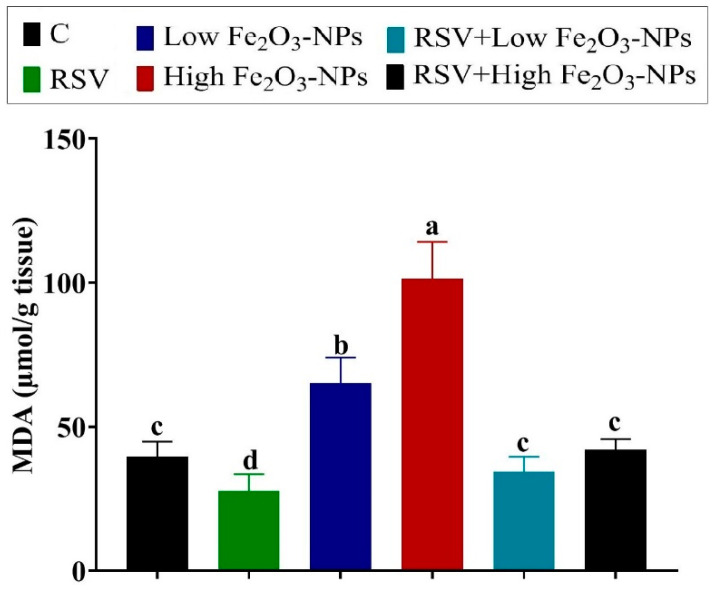
3.4. Effect of RSV and/or Fe2O3-NPs on Testicular Antioxidants and Lipid Peroxidation Level
The noticeable depletion of the enzymatic antioxidants SOD (p = 0.012), CAT (p < 0.001), and GPx (p < 0.001) was recorded in the low (37.50%, 28.46%, and 39.37%, respectively) and high (61.31%, 56.30%, and 65.05%, respectively) Fe2O3-NPs-exposed groups relative to the control group (Figure 4). Furthermore, the non-enzymatic antioxidant content, GSH, was exhausted (p < 0.001) in the low and high Fe2O3-NPs-exposed groups (37.78% and 69.03%, respectively) relative to the control group. Nevertheless, compared to the control group, the level of lipid peroxidative marker (MDA) was increased (p < 0.001) by 64.61% and twofold in the low and high Fe2O3-NPs-exposed groups, respectively (Figure 5). However, in the testicular tissue of RSV+Fe2O3-NPs-treated rats, the CAT, SOD, GPx, and GSH levels were (p < 0.001) reestablished and MDA elevation was suppressed (p < 0.001) until it became not significantly different from the control group.
Figure 4.
Effect of resveratrol (RSV; 20 mg/kg b.wt) and/or iron oxide nanoparticles (Fe2O3-NPs 3.5 or 7 mg/kg b.wt) administration for eight weeks on superoxide dismutase (SOD) (A) catalase (CAT) (B), glutathione peroxidase (GPx) (C), and reduced glutathione (GSH) (D) levels in the testicular tissues of male rats. Data expressed as mean ± SD, n = 9 for each group. Different letters (a, b, c, and d) on columns indicate statistically significant differences at p < 0.05 between the different experimental groups.
Figure 5.
Effect of resveratrol (RSV; 20 mg/kg b.wt) and/or iron oxide nanoparticles (Fe2O3-NPs 3.5 or 7 mg/kg b.wt) administration for eight weeks on malondialdehyde (MDA) levels in the testicular tissues of male rats. Data expressed as mean ± SD, n = 9 for each group. Different letters (a, b, c, and d) on columns indicate statistically significant differences at p < 0.05 between the different experimental groups.
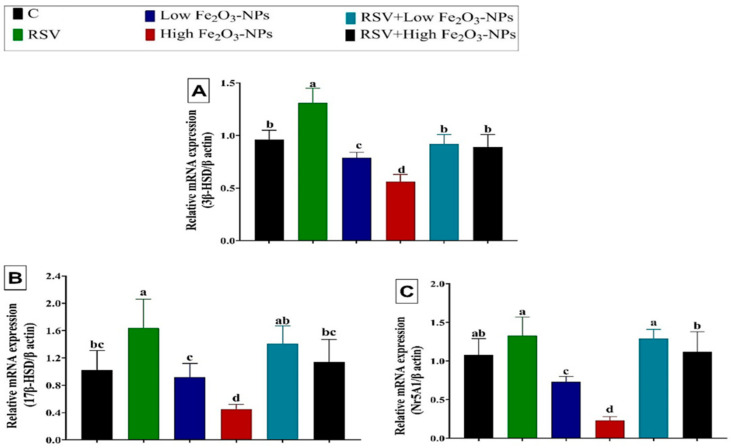
3.5. Effect of RSV and/or Fe2O3-NPs on Gene Expression in Testicular Tissue
As displayed in Figure 6, steroidogenesis-related genes, including 3β-HSD, 17β-HSD, and Nr5A1, were downregulated (p < 0.001) in the testicular tissue of low (0.79 ± 0.03, 0.92 ± 0.08, and 0.73± 0.04, respectively) and high (0.56 ± 0.04, 0.45 ± 0.03, and 0.23 ± 0.03, respectively) Fe2O3-NPs-exposed rats relative to the control group (0.96 ± 0.05, 1.02 ± 0.12, and 1.08 ± 0.12, respectively). The RSV dosing to the low or high Fe2O3-NPs-exposed rats counteracted (p < 0.001) the downregulation of analyzed steroidogenesis-related genes until they became not significantly changed from the control group.
Figure 6.
Effect of resveratrol (RSV; 20 mg/kg b.wt) and/or iron oxide nanoparticles (Fe2O3-NPs 3.5 or 7 mg/kg b.wt) administration for eight weeks on mRNA expression of (A) 3 beta-Hydroxysteroid dehydrogenase (3β-HSD), (B) 17-beta hydroxysteroid dehydrogenase (17β-HSD), and (C) Nuclear Receptor Subfamily 5 Group A Member 1 (Nr5A1) in the testicular tissues of male rats. Data expressed as mean ± SD, n = 9 for each group. Different letters (a, b, c, and d) on columns indicate statistically significant differences at p < 0.05 between the different experimental groups.
4. Discussion
Initially, in the current study, Fe2O3-NPs-exposed rats showed a significant decrease in final body weight and gonadosomtic index compared to the control group. In this context, Sundarraj et al. [17] reported that Fe2O3-NPs oral exposure (25 and 50 mg/kg) caused a significant decrease in food consumption, water intake, body weight gain, and organosomatic index. A similar reduction in body weight was recorded following exposure to other NPs, including silver NPs [63] and titanium dioxide NPs [64]. It is of note that in the current study, the gonadotropins level (LH and FSH) was significantly reduced despite this earlier reported inverse relationship between LH and FSH and body mass index changes [65]. Hence, despite the weight reduction, the recorded reduction of gonadotropins levels denotes that the Fe2O3-NPs exposure effect on the male sexual hormones and gonadosomatic index is a specific action rather than a non-specific stress effect. Fe2O3-NPs mediated testis weight decreases seemed to inhibit spermatogenesis after the germ cells’ death [66]. On the other hand, RSV oral dosing normalized reduced weight of the testes in Fe2O3-NPs-exposed rats possibly by cell stimulation and spermatogenesis due to RSV-mediated oxidative stress relief [67].
One key reason for the increase in male infertility is deteriorating semen quality [68]. Herein, the marked decline in sperm count, motility, and viability with a significant increase in morphological aberrations in the low or high Fe2O3-NPs-exposed rats reflected a pronounced deterioration of sperm quality. In this regard, Sundarraj et al. [17] reported that the fructose levels of the seminal vesicle decreased from Fe2O3-NPs. The decrease in the fructose amount in the seminal vesicle impedes energy in sperm [69] and contributes to seminal vesicle hypofunction that leads to infertility [70]. On the other hand, RSV treatment significantly improved the sperm quality in the low or high Fe2O3-NPs-exposed rats, denoting further improved fertility. Comparably, previous animal studies have shown that RSV successfully enhances the structure and quality of sperm as well as drugs/chemicals-induced testicular structural change, possibly due to its antioxidant properties [71,72,73,74].
The process of sperm production is known to be controlled by the three leading male fertility hormones: TES, FSH, and LH [75]. Our data revealed that Fe2O3-NPs exposure markedly decreased the male sexual hormones, including TES, FSH, and LH levels in the male rats. The former reductions could be linked to the earlier reported Fe2O3-NPs endocrine-disrupting activity that might have interrupted the hypothalamic-hypophyseal–testicular axis [15]. In addition, the Fe2O3-NPs-induced oxidative stress and lipid peroxidation could share in the reduction of male sexual hormones [76,77]. Similarly, other metal oxide NPs have been reported to reduce the three key male hormones levels and impair male fertility. For instance, the oral dosing of manganese oxides NP (100–400 mg/kg b.wt for 14 days) significantly reduced TES, FSH, and LH levels [78]. Interestingly, the re-establishment of the TES, FSH, and LH concentrations following RSV treatment displayed their protective effect against male sex hormones deficits mediated by Fe2O3-NPs exposure in the experimental animals. In this regard, Juan et al. [79] reported that RSV supplementation of normal rats led to increased hypothalamic–pituitary–gonadal axis function. Moreover, due to its structural similarity with estrogen, RSV is an estrogen agonist [80], which could promote the FSH and TES levels [79].
Diverse in vitro and in vivo studies have shown that multiple mechanisms could be involved in Fe2O3-NPs negative impacts, but the Fe2O3-NPs-mediated oxidative stress and lipid peroxidation is considered the dominant mechanism [8,81]. In the current investigation, the Fe2O3-NPs-exposed rats exhibited a marked reduction in enzymatic (CAT, GPx, and SOD) and non-enzymatic (GSH) antioxidants simultaneously with a sharp rise in the lipid peroxidation marker, MDA. SOD, CAT, GPx, and GSH are vital antioxidant molecules that guard against lipid peroxidation via ROS elimination. SOD catalyzes the dismutation of superoxide anion (O2•) radical to hydrogen peroxide (H2O2), whereas CAT degrades H2O2 into an oxygen molecule and a water molecule [82]. The H2O2 is also a substrate for GPx, which uses H2O2 to oxidize GSH [83]. The significant changes in this antioxidant system in the testes of rats exposed to Fe2O3-NPs concomitant with increased MDA levels allow us to conclude that the testicular antioxidant defenses did not protected the tissue from the action of Fe2O3-NPs-induced lipid peroxidation. Similarly, Sundarraj et al. [17] confirmed the reduction of GSH content in the male accessory organs on exposure to Fe2O3-NPs. Fe2O3-NPs in the cells remain in endosomes or lysosomes and become free iron, which raises the total iron pool within the cells [84]. Several previous studies have confirmed that iron, when present in excess within cells, interrupts redox homeostasis and catalyzes the ROS propagation, creating an oxidative environment [85,86]. By comparison, oral RSV dosing substantially restored the depleted antioxidant enzymes and suppressed the high MDA content of Fe2O3-NPs-exposed rats in their testicular tissue. RSV has been reported to cross the blood–testes barrier and give the testis its defensive effects [87]. The RSV-induced inhibition of oxidants in testicular tissue is probably linked to its capacity to trap superoxide anion, hydroxyl radicals, hydrogen peroxide, and up-control the production of endogenous antioxidants [88]. The RSV’s antioxidant activity is determined by the arrangement of functional groups on the nuclear structure. As a result, the configuration, substitution, and the total number of hydroxyl groups all significantly impact several antioxidant mechanisms, including radical scavenging and metal ion chelation. Previous research has shown that the hydroxyl group in the 4′ position is not the only determinant of antioxidant activity, but that the 3- and 5-OH groups also play a role [89,90]. The antioxidant effect of RSV on hydroxyl (•OH) and hydroperoxyl (•OOH) radicals were studied, and it was discovered that RSV could act as an efficient •OOH, and possibly •OOR, radical scavenger [91]. Additionally, the RSV antioxidant properties in vivo are more likely to be attributable to its effect as a gene regulator [92]. For instance, RSV inhibits NADPH oxidase-mediated release of ROS through downregulating the oxidase expression. Additionally, RSV reduces mitochondrial superoxide generation by motivating mitochondria biogenesis [93]. Furthermore, RSV increased the expression of various antioxidant enzymes in different cell types [94].
Testicular steroidogenesis is a regulated multistep process controlled by multiple genes [95,96]. TES is produced chiefly in Leydig cells through a series of enzymatic reactions. First, the steroidogenic acute regulatory (StAR) protein transfers cholesterol to the mitochondria [97]. Then, the mitochondrial cytochrome P450scc converts cholesterol into pregnenolone. Consequently, other enzymes (3β-HSD, P450c17, and 17β-HSD) transform the pregnenolone into TES [98]. In addition, several transcription factors play essential roles in regulating steroidogenic genes. For instance, Nr5A1 is a transcription factor that regulates the expression of steroidogenic genes like 3β-HSD in Leydig cells. Hence, some authors explored the influence of metal oxide NPs on the expression of genes related to steroidogenesis [99]. For instance, Hussein et al. [100] reported that the intragastric administration of zinc oxide NPs (100 and 400 mg/kg b.wt) for 12 weeks significantly downregulated the expression of 17β-HSD, 3β-HSD, and Nr5A1 and simultaneously reduced the TES level. Additionally, 3β-HSD downregulation concomitantly with reduced TES level have been recorded with exposure to cerium oxide NPs (orally, 10–40 mg/kg b.wt, 32 days) in mice [98] and Fe3O4 (orally, 5 mg/kg b.wt, 79 days) in rats [101]. Consequently, in the current study, we assessed the expression of two steroidogenic genes, 3β-HSD, and 17β-HSD and the important regulating factor Nr5A1. The results revealed that the testicular 3β-HSD, 17β-HSD, and Nr5A1 mRNA expressions were downregulated in the Fe2O3-NPs-exposed rats demonstrating reduced testicular steroidogenesis. Thus, we hypothesize that suppression of the rate-limiting step of steroidogenesis and decreased transcript levels of genes encoding for 3β-HSD, and 17β-HSD, which catalyze the downstream reactions in steroidogenesis, are responsible for the decreased TES levels and the subsequent LH and FSH reduction in the present study. The decline of the three male sex hormone levels was reflected in the decrease in sperm count and motility in Fe2O3-NPs-exposed rats. Comparably, the downregulation of steroidogenesis-related genes was the machinery mechanism of the testicular damage induced by several metal NPs [98,101].
Accumulative evidence has shown that testicular steroidogenesis dysfunction and spermatogenesis triggered by chemical-induced oxidative stress were related to impaired male fertility [102]. Additionally, many studies suggested that testicular steroidogenesis is interrupted in the oxidative stress conditions via the inhibition of the major transcription factors that regulate the expression of steroidogenic enzyme genes [103,104,105,106,107]. Moreover, a strong correlation has been reported between steroidogenesis disruption and lipid peroxidation [108,109]. Hence, the Fe2O3-NPs-induced oxidative stress and lipid peroxidative damage in the testicular tissues could effectively impair the steroidogenesis process. However, further studies are highly recommended on the underlying mechanisms of Fe2O3-NPs-induced testicular damage, focusing on the protein expressions of the tested genes and other genes involved in the steroidogenesis process.
On the contrary, a considerable recovery was distinguished in the steroidogenic-related gene expression following the RSV oral dosing. The potent antioxidant activity and anti-lipid peroxidative action of RSV could be the initial mechanism through which the other beneficial effects, including the correction of the transcription of steroidogenic-related genes, have been attained. In accordance with our results, Banerjee et al. [110] reported that RSV (oral doses of 50 mg/kg b.wt daily for 60 days) effectively mitigated oxidative stress in Leydig cells and increased the transcriptional level of CYP11A1, 17β-HSD, 3β-HSD, and StAR and thus protected steroidogenesis from Benzo(a)pyrene’s negative impact in rats.
Despite the evident protective role of RSV against the Fe2O3-NPs-induced impairment in sperm quality, male hormone balance, and the regulation of some steroidogenic-related genes, the present study has some limitations. First, several probable underlying mechanisms have not been covered, such as the regulation of the apoptotic events, the DNA damage repair, and the inflammatory events. Second, we did not experimentally examine the molecular effects of Fe2O3-NPs and RSV on the specific testicular cell types. Third, the expressions of other genes incorporated into the pathway regulation of testicular steroidogenesis have not been explored. Therefore, the current study findings need to be deepened by future mechanistic studies to cover the gap in knowledge regarding the other probable underlying mechanisms of both RSV and Fe2O3-NPs on male fertility.
5. Conclusions
The findings of the current study provide novel clues for the possible involvement of the downregulation of steroidogenesis-related genes (3β-HSD, 17β-HSD, and Nr5A1) in the induction of testicular damage in Fe2O3-NPs-exposed rats. Our results suggested that the RSV administration could be beneficial in the defense against Fe2O3-NPs-induced impaired sperm quality and testicular damage via amplifying the antioxidant capacity and the subsequent appropriate steroidogenesis-related gene regulation. Thus, RSV could be suggested as a natural dietary supplement in persons frequently exposed to Fe2O3-NPs. Further studies are highly recommended on the other probable mechanisms implicated in the protective role of RSV against chemical-induced testicular injury, such as anti-apoptotic and anti-inflammatory effects, as well as the repair of DNA damage.
Author Contributions
M.M.A., conceptualization, methodology, resources, investigation, data curation, writing—review and editing; M.M.A.H., conceptualization, methodology, resources, investigation, visualization, writing—review and editing; T.S., conceptualization, resources, software, formal analysis, visualization, writing—review and editing, funding acquisition; Y.M.A.-E., conceptualization, software, formal analysis, investigation, data curation, visualization, writing—original draft. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The protocol was permitted by the Institutional Animal Care and Use Committee of Zagazig University (IACUC), Egypt, with approval number ZU-IACUC/2/F/44/2021. All efforts were made to handle the rats humanely and achieve ethical rules.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data is contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This study was supported by Taif University Researchers Supporting Project (TURSP-2020/152), Taif University, Taif, Saudi Arabia.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Pyrgiotakis G., Vedantam P., Cirenza C., McDevitt J., Eleftheriadou M., Leonard S.S., Demokritou P. Optimization of a nanotechnology based antimicrobial platform for food safety applications using Engineered Water Nanostructures (EWNS) Sci. Rep. 2016;6:21073. doi: 10.1038/srep21073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abd-Elhakim Y.M., Hashem M.M., Abo-EL-Sooud K., Hassan B.A., Elbohi K.M., Al-Sagheer A.A. Effects of Co-Exposure of Nanoparticles and Metals on Different Organisms: A Review. Toxics. 2021;9:284. doi: 10.3390/toxics9110284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.ECHA European Union Observatory for Nanomaterial: Catalogue of Cosmetic Ingredients. 2019. [(accessed on 12 April 2022)]. Available online: https://euon.echa.europa.eu/catalogue-ofcosmetic-ingredients.
- 4.Häfeli U.O., Riffle J.S., Harris-Shekhawat L., Carmichael-Baranauskas A., Mark F., Dailey J.P., Bardenstein D. Cell uptake and in vitro toxicity of magnetic nanoparticles suitable for drug delivery. Mol. Pharm. 2009;6:1417–1428. doi: 10.1021/mp900083m. [DOI] [PubMed] [Google Scholar]
- 5.Gonzales-Weimuller M., Zeisberger M., Krishnan K.M. Size-dependant heating rates of iron oxide nanoparticles for magnetic fluid hyperthermia. J. Magn. Magn. Mater. 2009;321:1947–1950. doi: 10.1016/j.jmmm.2008.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xie J., Huang J., Li X., Sun S., Chen X. Iron oxide nanoparticle platform for biomedical applications. Curr. Med. Chem. 2009;16:1278–1294. doi: 10.2174/092986709787846604. [DOI] [PubMed] [Google Scholar]
- 7.Lobel B., Eyal O., Kariv N., Katzir A. Temperature controlled CO2 laser welding of soft tissues: Urinary bladder welding in different animal models (rats, rabbits, and cats) Lasers Surg. Med. Off. J. Am. Soc. Laser Med. Surg. 2000;26:4–12. doi: 10.1002/(SICI)1096-9101(2000)26:1<4::AID-LSM3>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 8.Naqvi S., Samim M., Abdin M., Ahmed F.J., Maitra A., Prashant C., Dinda A.K. Concentration-dependent toxicity of iron oxide nanoparticles mediated by increased oxidative stress. Int. J. Nanomed. 2010;5:983. doi: 10.2147/IJN.S13244. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 9.Singh S.P., Rahman M.F., Murty U.S.N., Mahboob M., Grover P. Comparative study of genotoxicity and tissue distribution of nano and micron sized iron oxide in rats after acute oral treatment. Toxicol. Appl. Pharmacol. 2013;266:56–66. doi: 10.1016/j.taap.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 10.Sadeghi L., Espanani H. Toxic effects of the Fe2O3 nanoparticles on the liver and lung tissue. Bratisl. Lek. Listy. 2015;116:373–378. doi: 10.4149/BLL_2015_071. [DOI] [PubMed] [Google Scholar]
- 11.Askri D., Ouni S., Galai S., Chovelon B., Arnaud J., Lehmann S.G., Sakly M., Seve M., Amara S. Sub-acute intravenous exposure to Fe2O3 nanoparticles does not alter cognitive performances and catecholamine levels, but slightly disrupts plasma iron level and brain iron content in rats. J. Trace Elem. Med. Biol. 2018;50:73–79. doi: 10.1016/j.jtemb.2018.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Hadrup N., Saber A.T., Kyjovska Z.O., Jacobsen N.R., Vippola M., Sarlin E., Ding Y., Schmid O., Wallin H., Jensen K.A. Pulmonary toxicity of Fe2O3, ZnFe2O4, NiFe2O4 and NiZnFe4O8 nanomaterials: Inflammation and DNA strand breaks. Environ. Toxicol. Pharmacol. 2020;74:103303. doi: 10.1016/j.etap.2019.103303. [DOI] [PubMed] [Google Scholar]
- 13.Gaharwar U.S., Meena R., Rajamani P. Iron oxide nanoparticles induced cytotoxicity, oxidative stress and DNA damage in lymphocytes. J. Appl. Toxicol. 2017;37:1232–1244. doi: 10.1002/jat.3485. [DOI] [PubMed] [Google Scholar]
- 14.Yarjanli Z., Ghaedi K., Esmaeili A., Rahgozar S., Zarrabi A. Iron oxide nanoparticles may damage to the neural tissue through iron accumulation, oxidative stress, and protein aggregation. BMC Neurosci. 2017;18:51. doi: 10.1186/s12868-017-0369-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sundarraj K., Manickam V., Raghunath A., Periyasamy M., Viswanathan M.P., Perumal E. Repeated exposure to iron oxide nanoparticles causes testicular toxicity in mice. Environ. Toxicol. 2017;32:594–608. doi: 10.1002/tox.22262. [DOI] [PubMed] [Google Scholar]
- 16.Dora M.F., Taha N.M., Lebda M.A., Hashem A.E., Elfeky M.S., El-Sayed Y.S., Jaouni S.A., El-Far A.H. Quercetin Attenuates Brain Oxidative Alterations Induced by Iron Oxide Nanoparticles in Rats. Int. J. Mol. Sci. 2021;22:3829. doi: 10.3390/ijms22083829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sundarraj K., Raghunath A., Panneerselvam L., Perumal E. Iron oxide nanoparticles modulate heat shock proteins and organ specific markers expression in mice male accessory organs. Toxicol. Appl. Pharmacol. 2017;317:12–24. doi: 10.1016/j.taap.2017.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Mirzaei Varzeghani S., Parivar K., Abdollahifar M.-A., Karamian A. Effects of Iron Oxide Nanoparticles on Mouse Sperm Parameters and Testicular Tissue. Iran. J. Toxicol. 2018;12:39–44. doi: 10.32598/IJT.12.6.490.1. [DOI] [Google Scholar]
- 19.Abd-Elhakim Y.M., Ghoneim M.H., Ebraheim L.L., Imam T.S. Taurine and hesperidin rescues carbon tetrachloride-triggered testicular and kidney damage in rat via modulating oxidative stress and inflammation. Life Sci. 2020;254:117782. doi: 10.1016/j.lfs.2020.117782. [DOI] [PubMed] [Google Scholar]
- 20.Abd El-Hakim Y.M., Mohamed W.A., El-Metwally A.E. Spirulina platensis attenuates furan reprotoxicity by regulating oxidative stress, inflammation, and apoptosis in testis of rats. Ecotoxicol. Environ. Saf. 2018;161:25–33. doi: 10.1016/j.ecoenv.2018.05.073. [DOI] [PubMed] [Google Scholar]
- 21.Behairy A., El-Sharkawy N.I., Saber T.M., Soliman M.M., Metwally M.M.M., Abd El-Rahman G.I., Abd-Elhakim Y.M., El Deib M.M. The Modulatory Role of Vitamin C in Boldenone Undecylenate Induced Testicular Oxidative Damage and Androgen Receptor Dysregulation in Adult Male Rats. Antioxidants. 2020;9:1053. doi: 10.3390/antiox9111053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sahoo D.K., Roy A., Chainy G.B. Protective effects of vitamin E and curcumin on L-thyroxine-induced rat testicular oxidative stress. Chem. Biol. Interact. 2008;176:121–128. doi: 10.1016/j.cbi.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 23.Elewa Y.H.A., Mohamed A.A.-R., Galal A.A.A., El-naseery N.I., Ichii O., Kon Y. Food Yellow4 reprotoxicity in relation to localization of DMC1 and apoptosis in rat testes: Roles of royal jelly and cod liver oil. Ecotoxicol. Environ. Saf. 2019;169:696–706. doi: 10.1016/j.ecoenv.2018.11.082. [DOI] [PubMed] [Google Scholar]
- 24.Salehi B., Mishra A.P., Nigam M., Sener B., Kilic M., Sharifi-Rad M., Fokou P.V.T., Martins N., Sharifi-Rad J. Resveratrol: A Double-Edged Sword in Health Benefits. Biomedicines. 2018;6:91. doi: 10.3390/biomedicines6030091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oh W.Y., Shahidi F. Antioxidant activity of resveratrol ester derivatives in food and biological model systems. Food Chem. 2018;261:267–273. doi: 10.1016/j.foodchem.2018.03.085. [DOI] [PubMed] [Google Scholar]
- 26.Nie Z., Zhang L., Chen W., Zhang Y., Hua R., Wang W., Zhang T., Wu H. The protective effects of pretreatment with resveratrol in cyclophosphamide-induced rat ovarian granulosa cell injury: In vitro study. Reprod. Toxicol. 2020;95:66–74. doi: 10.1016/j.reprotox.2020.05.005. [DOI] [PubMed] [Google Scholar]
- 27.Lee I.T., Lin C.-F., Huang Y.-L., Chong K.-Y., Hsieh M.-F., Huang T.-H., Cheng C.-Y. Protective mechanisms of resveratrol derivatives against TNF-α-induced inflammatory responses in rat mesangial cells. Cytokine. 2019;113:380–392. doi: 10.1016/j.cyto.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 28.Pannu N., Bhatnagar A. Resveratrol: From enhanced biosynthesis and bioavailability to multitargeting chronic diseases. Biomed. Pharmacother. 2019;109:2237–2251. doi: 10.1016/j.biopha.2018.11.075. [DOI] [PubMed] [Google Scholar]
- 29.Carrizzo A., Forte M., Damato A., Trimarco V., Salzano F., Bartolo M., Maciag A., Puca A.A., Vecchione C. Antioxidant effects of resveratrol in cardiovascular, cerebral and metabolic diseases. Food Chem. Toxicol. 2013;61:215–226. doi: 10.1016/j.fct.2013.07.021. [DOI] [PubMed] [Google Scholar]
- 30.AlBasher G., Abdel-Daim M.M., Almeer R., Ibrahim K.A., Hamza R.Z., Bungau S., Aleya L. Synergistic antioxidant effects of resveratrol and curcumin against fipronil-triggered oxidative damage in male albino rats. Environ. Sci. Pollut. Res. 2020;27:6505–6514. doi: 10.1007/s11356-019-07344-8. [DOI] [PubMed] [Google Scholar]
- 31.Xia N., Daiber A., Förstermann U., Li H. Antioxidant effects of resveratrol in the cardiovascular system. Br. J. Pharmacol. 2017;174:1633–1646. doi: 10.1111/bph.13492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Filardo S., Di Pietro M., Mastromarino P., Sessa R. Therapeutic potential of resveratrol against emerging respiratory viral infections. Pharmacol. Ther. 2020;214:107613. doi: 10.1016/j.pharmthera.2020.107613. [DOI] [PubMed] [Google Scholar]
- 33.Rahman M.H., Akter R., Bhattacharya T., Abdel-Daim M.M., Alkahtani S., Arafah M.W., Al-Johani N.S., Alhoshani N.M., Alkeraishan N., Alhenaky A., et al. Resveratrol and Neuroprotection: Impact and Its Therapeutic Potential in Alzheimer’s Disease. Front. Pharmacol. 2020;11:2272. doi: 10.3389/fphar.2020.619024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Rai R.C., Bagul P.K., Banerjee S.K. NLRP3 inflammasome drives inflammation in high fructose fed diabetic rat liver: Effect of resveratrol and metformin. Life Sci. 2020;253:117727. doi: 10.1016/j.lfs.2020.117727. [DOI] [PubMed] [Google Scholar]
- 35.Buys-Gonçalves G.F., Sampaio F.J.B., Silva M.E.M., Pereira-Sampaio M.A., De Souza D.B. Histomorphometric evaluation of the rat kidney submitted to warm ischemia and the protective effect of resveratrol. Am. J. Surg. 2020;220:1119–1123. doi: 10.1016/j.amjsurg.2020.02.025. [DOI] [PubMed] [Google Scholar]
- 36.Mojica-Villegas M.A., Izquierdo-Vega J.A., Chamorro-Cevallos G., Sánchez-Gutiérrez M. Protective effect of resveratrol on biomarkers of oxidative stress induced by iron/ascorbate in mouse spermatozoa. Nutrients. 2014;6:489–503. doi: 10.3390/nu6020489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bucak M., Ataman M., Başpınar N., Uysal O., Taşpınar M., Bilgili A., Öztürk C., Güngör Ş., Inanc M., Akal E. Lycopene and resveratrol improve post-thaw bull sperm parameters: Sperm motility, mitochondrial activity and DNA integrity. Andrologia. 2015;47:545–552. doi: 10.1111/and.12301. [DOI] [PubMed] [Google Scholar]
- 38.Collodel G., Federico M., Geminiani M., Martini S., Bonechi C., Rossi C., Figura N., Moretti E. Effect of trans-resveratrol on induced oxidative stress in human sperm and in rat germinal cells. Reprod. Toxicol. 2011;31:239–246. doi: 10.1016/j.reprotox.2010.11.010. [DOI] [PubMed] [Google Scholar]
- 39.Adler I.-D. Comparison of the duration of spermatogenesis between male rodents and humans. Mutat. Res. /Fundam. Mol. Mech. Mutagenesis. 1996;352:169–172. doi: 10.1016/0027-5107(95)00223-5. [DOI] [PubMed] [Google Scholar]
- 40.Eleawa S.M., Alkhateeb M.A., Alhashem F.H., Bin-Jaliah I., Sakr H.F., Elrefaey H.M., Elkarib A.O., Alessa R.M., Haidara M.A., Shatoor A.S., et al. Resveratrol reverses cadmium chloride-induced testicular damage and subfertility by downregulating p53 and Bax and upregulating gonadotropins and Bcl-2 gene expression. J. Reprod. Dev. 2014;60:115–127. doi: 10.1262/jrd.2013-097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Sharma P., Huq A.U., Singh R. Cypermethrin-induced reproductive toxicity in the rat is prevented by resveratrol. J. Hum. Reprod. Sci. 2014;7:99. doi: 10.4103/0974-1208.138867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jiang Y.-g., Tao P., Yong L., Li M.-c., Lin Y.-h. Resveratrol reestablishes spermatogenesis after testicular injury in rats caused by 2, 5-hexanedione. Chin. Med. J. 2008;121:1204–1209. doi: 10.1097/00029330-200807010-00010. [DOI] [PubMed] [Google Scholar]
- 43.Juan M.E., Vinardell M.P., Planas J.M. The daily oral administration of high doses of trans-resveratrol to rats for 28 days is not harmful. J. Nutr. 2002;132:257–260. doi: 10.1093/jn/132.2.257. [DOI] [PubMed] [Google Scholar]
- 44.Kim J.S., Yoon T.-J., Yu K.N., Kim B.G., Park S.J., Kim H.W., Lee K.H., Park S.B., Lee J.-K., Cho M.H. Toxicity and tissue distribution of magnetic nanoparticles in mice. Toxicol. Sci. 2006;89:338–347. doi: 10.1093/toxsci/kfj027. [DOI] [PubMed] [Google Scholar]
- 45.Kumari M., Rajak S., Singh S.P., Kumari S.I., Kumar P.U., Murty U.S.N., Mahboob M., Grover P., Rahman M.F. Repeated Oral Dose Toxicity of Iron Oxide Nanoparticles: Biochemical and Histopathological Alterations in Different Tissues of Rats. J. Nanosci. Nanotechnol. 2012;12:2149–2159. doi: 10.1166/jnn.2012.5796. [DOI] [PubMed] [Google Scholar]
- 46.Askri D., Cunin V., Ouni S., Béal D., Rachidi W., Sakly M., Amara S., Lehmann S.G., Sève M. Effects of Iron Oxide Nanoparticles (γ-Fe2O3) on Liver, Lung and Brain Proteomes following Sub-Acute Intranasal Exposure: A New Toxicological Assessment in Rat Model Using iTRAQ-Based Quantitative Proteomics. Int. J. Mol. Sci. 2019;20:5186. doi: 10.3390/ijms20205186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dhakshinamoorthy V., Manickam V., Perumal E. Neurobehavioural Toxicity of Iron Oxide Nanoparticles in Mice. Neurotox. Res. 2017;32:187–203. doi: 10.1007/s12640-017-9721-1. [DOI] [PubMed] [Google Scholar]
- 48.Wang Z.-Y., Song J., Zhang D.-S. Nanosized As2O3/Fe2O3 complexes combined with magnetic fluid hyperthermia selectively target liver cancer cells. World J. Gastroenterol. 2009;15:2995. doi: 10.3748/wjg.15.2995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sadeghiani N., Barbosa L., Silva L., Azevedo R., Morais P., Lacava Z. Genotoxicity and inflammatory investigation in mice treated with magnetite nanoparticles surface coated with polyaspartic acid. J. Magn. Magn. Mater. 2005;289:466–468. doi: 10.1016/j.jmmm.2004.11.131. [DOI] [Google Scholar]
- 50.Pham B.T., Colvin E.K., Pham N.T., Kim B.J., Fuller E.S., Moon E.A., Barbey R., Yuen S., Rickman B.H., Bryce N.S. Biodistribution and clearance of stable superparamagnetic maghemite iron oxide nanoparticles in mice following intraperitoneal administration. Int. J. Mol. Sci. 2018;19:205. doi: 10.3390/ijms19010205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Prodan A.M., Iconaru S.L., Ciobanu C.S., Chifiriuc M.C., Stoicea M., Predoi D. Iron Oxide Magnetic Nanoparticles: Characterization and Toxicity Evaluation by In Vitro and In Vivo Assays. J. Nanomater. 2013;2013:587021. doi: 10.1155/2013/587021. [DOI] [Google Scholar]
- 52.Adebayo A., Oke B., Akinloye A. Characterizing the gonadosomatic index and its relationship with age in greater cane rat (Thryonomys swinderianus, Temminck) J. Vet. Anat. 2009;2:53–59. doi: 10.21608/jva.2009.42311. [DOI] [Google Scholar]
- 53.Slott V.L., Suarez J.D., Perreault S.D. Rat sperm motility analysis: Methodologic considerations. Reprod. Toxicol. 1991;5:449–458. doi: 10.1016/0890-6238(91)90009-5. [DOI] [PubMed] [Google Scholar]
- 54.Mailankot M., Kunnath A.P., Jayalekshmi H., Koduru B., Valsalan R. Radio frequency electromagnetic radiation (RF-EMR) from GSM (0.9/1.8 GHz) mobile phones induces oxidative stress and reduces sperm motility in rats. Clinics. 2009;64:561–565. doi: 10.1590/S1807-59322009000600011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Filler R. Methods for evaluation of rat epididymal sperm morphology. In: Chapin R.E., Heildel J.J., editors. Methods in Toxicology: Male Reproductive Toxicology. Elsevier; Amsterdam, The Netherlands: 1993. pp. 334–343. [Google Scholar]
- 56.Nishikimi M., Rao N.A., Yagi K. The occurrence of superoxide anion in the reaction of reduced phenazine methosulfate and molecular oxygen. Biochem. Biophys. Res. Commun. 1972;46:849–854. doi: 10.1016/S0006-291X(72)80218-3. [DOI] [PubMed] [Google Scholar]
- 57.Aebi H. Methods in Enzymology. Volume 105. Elsevier; Amsterdam, The Netherlands: 1984. [13] Catalase in vitro; pp. 121–126. [DOI] [PubMed] [Google Scholar]
- 58.Paglia D.E., Valentine W.N. Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. J. Lab. Clin. Med. 1967;70:158–169. [PubMed] [Google Scholar]
- 59.Beutler E. Improved method for the determination of blood glutathione. J. Lab. Clin. Med. 1963;61:882–888. [PubMed] [Google Scholar]
- 60.Ohkawa H., Ohishi N., Yagi K. Assay for lipid peroxides in animal tissues by thiobarbituric acid reaction. Anal. Biochem. 1979;95:351–358. doi: 10.1016/0003-2697(79)90738-3. [DOI] [PubMed] [Google Scholar]
- 61.Ahmed M.M., Hussein M.M. Neurotoxic effects of silver nanoparticles and the protective role of rutin. Biomed. Pharmacother. 2017;90:731–739. doi: 10.1016/j.biopha.2017.04.026. [DOI] [PubMed] [Google Scholar]
- 62.Livak K.J., Schmittgen T.D. Analysis of relative gene expression data using real-time quantitative PCR and the 2− ΔΔCT method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 63.Shahare B., Yashpal M., Gajendra Toxic effects of repeated oral exposure of silver nanoparticles on small intestine mucosa of mice. Toxicol. Mech. Methods. 2013;23:161–167. doi: 10.3109/15376516.2013.764950. [DOI] [PubMed] [Google Scholar]
- 64.Xu J., Shi H., Ruth M., Yu H., Lazar L., Zou B., Yang C., Wu A., Zhao J. Acute toxicity of intravenously administered titanium dioxide nanoparticles in mice. PLoS ONE. 2013;8:e70618. doi: 10.1371/journal.pone.0070618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Birkebaek N.H., Lange A., Holland-Fischer P., Kristensen K., Rittig S., Vilstrup H., Handberg A., Gronbaek H. Effect of weight reduction on insulin sensitivity, sex hormone-binding globulin, sex hormones and gonadotrophins in obese children. Eur. J. Endocrinol. 2010;163:895–900. doi: 10.1530/EJE-10-0538. [DOI] [PubMed] [Google Scholar]
- 66.Kilarkaje N., Al-hussaini H., Al-Bader M. Diabetes-induced DNA damage and apoptosis are associated with poly (ADP ribose) polymerase 1 inhibition in the rat testis. Eur. J. Pharmacol. 2014;737:29–40. doi: 10.1016/j.ejphar.2014.05.005. [DOI] [PubMed] [Google Scholar]
- 67.Faid I., Al-Hussaini H., Kilarkaje N. Resveratrol alleviates diabetes-induced testicular dysfunction by inhibiting oxidative stress and c-Jun N-terminal kinase signaling in rats. Toxicol. Appl. Pharmacol. 2015;289:482–494. doi: 10.1016/j.taap.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 68.Kumar N., Singh A.K. Impact of environmental factors on human semen quality and male fertility: A narrative review. Environ. Sci. Eur. 2022;34:6. doi: 10.1186/s12302-021-00585-w. [DOI] [Google Scholar]
- 69.Sarkar M., Gangopadhyay P., Basak B., Chakrabarty K., Banerji J., Adhikary P., Chatterjee A. The reversible antifertility effect of Piper betle Linn. on Swiss albino male mice. Contraception. 2000;62:271–274. doi: 10.1016/S0010-7824(00)00177-3. [DOI] [PubMed] [Google Scholar]
- 70.Gonzales G., Kortebani G., Mazzolli A. Hyperviscosity and hypofunction of the seminal vesicles. Arch. Androl. 1993;30:63–68. doi: 10.3109/01485019308988370. [DOI] [PubMed] [Google Scholar]
- 71.Chirumbolo S. Resveratrol in spermatogenesis. Cell Biol. Int. 2015;39:775–776. doi: 10.1002/cbin.10451. [DOI] [PubMed] [Google Scholar]
- 72.Li E., Guo Y., Wang G., Chen F., Li Q. Effect of resveratrol on restoring spermatogenesis in experimental cryptorchid mice and analysis of related differentially expressed proteins. Cell Biol. Int. 2015;39:733–740. doi: 10.1002/cbin.10441. [DOI] [PubMed] [Google Scholar]
- 73.Banerjee B., Nandi P., Chakraborty S., Raha S., Sen P.C., Jana K. Resveratrol ameliorates benzo (a) pyrene-induced testicular dysfunction and apoptosis: Involvement of p38 MAPK/ATF2/iNOS signaling. J. Nutr. Biochem. 2016;34:17–29. doi: 10.1016/j.jnutbio.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 74.Türedi S., Yuluğ E., Alver A., Kutlu Ö., Kahraman C. Effects of resveratrol on doxorubicin induced testicular damage in rats. Exp. Toxicol. Pathol. 2015;67:229–235. doi: 10.1016/j.etp.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 75.Hassan M.A., El Bohy K.M., El Sharkawy N.I., Imam T.S., El-Metwally A.E., Hamed Arisha A., Mohammed H.A., Abd-Elhakim Y.M. Iprodione and chlorpyrifos induce testicular damage, oxidative stress, apoptosis and suppression of steroidogenic-and spermatogenic-related genes in immature male albino rats. Andrologia. 2021;53:e13978. doi: 10.1111/and.13978. [DOI] [PubMed] [Google Scholar]
- 76.Chainy G.B.N., Sahoo D.K. Hormones and oxidative stress: An overview. Free Radic. Res. 2020;54:1–26. doi: 10.1080/10715762.2019.1702656. [DOI] [PubMed] [Google Scholar]
- 77.Sahoo D.K., Jena S., Chainy G.B.N. Chapter 2.7—Thyroid Dysfunction and Testicular Redox Status: An Intriguing Association. In: Henkel R., Samanta L., Agarwal A., editors. Oxidants, Antioxidants and Impact of the Oxidative Status in Male Reproduction. Academic Press; Cambridge, MA, USA: 2019. pp. 149–170. [Google Scholar]
- 78.Negahdary M., Arefian Z., Dastjerdi H.A., Ajdary M. Toxic effects of Mn2O3 nanoparticles on rat testis and sex hormone. J. Nat. Sci. Biol. Med. 2015;6:335. doi: 10.4103/0976-9668.159998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Juan M.E., Gonzalez-Pons E., Munuera T., Ballester J., Rodríguez-Gil J.E., Planas J.M. trans-Resveratrol, a natural antioxidant from grapes, increases sperm output in healthy rats. J. Nutr. 2005;135:757–760. doi: 10.1093/jn/135.4.757. [DOI] [PubMed] [Google Scholar]
- 80.Abou-Zeid L.A., El-Mowafy A.M. Differential recognition of resveratrol isomers by the human estrogen receptor-α: Molecular dynamics evidence for stereoselective ligand binding. Chirality. 2004;16:190–195. doi: 10.1002/chir.20007. [DOI] [PubMed] [Google Scholar]
- 81.Mahmoudi M., Hofmann H., Rothen-Rutishauser B., Petri-Fink A. Assessing the in vitro and in vivo toxicity of superparamagnetic iron oxide nanoparticles. Chem. Rev. 2012;112:2323–2338. doi: 10.1021/cr2002596. [DOI] [PubMed] [Google Scholar]
- 82.Jurczuk M., Brzóska M.M., Moniuszko-Jakoniuk J., Gałażyn-Sidorczuk M., Kulikowska-Karpińska E. Antioxidant enzymes activity and lipid peroxidation in liver and kidney of rats exposed to cadmium and ethanol. Food Chem. Toxicol. 2004;42:429–438. doi: 10.1016/j.fct.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 83.Abarikwu S.O., Adesiyan A.C., Oyeloja T.O., Oyeyemi M.O., Farombi E.O. Changes in sperm characteristics and induction of oxidative stress in the testis and epididymis of experimental rats by a herbicide, atrazine. Arch. Environ. Contam. Toxicol. 2010;58:874–882. doi: 10.1007/s00244-009-9371-2. [DOI] [PubMed] [Google Scholar]
- 84.Mittra E.S., Goris M.L., Iagaru A.H., Kardan A., Burton L., Berganos R., Chang E., Liu S., Shen B., Chin F.T. Pilot pharmacokinetic and dosimetric studies of 18F-FPPRGD2: A PET radiopharmaceutical agent for imaging αvβ3 integrin levels. Radiology. 2011;260:182–191. doi: 10.1148/radiol.11101139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lee H.J., Choi J.S., Lee H.J., Kim W.-H., Park S.I., Song J. Effect of excess iron on oxidative stress and gluconeogenesis through hepcidin during mitochondrial dysfunction. J. Nutr. Biochem. 2015;26:1414–1423. doi: 10.1016/j.jnutbio.2015.07.008. [DOI] [PubMed] [Google Scholar]
- 86.Galaris D., Barbouti A., Pantopoulos K. Iron homeostasis and oxidative stress: An intimate relationship. Biochim. Biophys. Acta BBA Mol. Cell Res. 2019;1866:118535. doi: 10.1016/j.bbamcr.2019.118535. [DOI] [PubMed] [Google Scholar]
- 87.Aitken R.J., Roman S.D. Molecular Mechanisms in Spermatogenesis. Springer; Berlin/Heidelberg, Germany: 2009. Antioxidant systems and oxidative stress in the testes; pp. 154–171. [Google Scholar]
- 88.Li H., Xia N., Förstermann U. Cardiovascular effects and molecular targets of resveratrol. Nitric Oxide. 2012;26:102–110. doi: 10.1016/j.niox.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 89.Stivala L.A., Savio M., Carafoli F., Perucca P., Bianchi L., Maga G., Forti L., Pagnoni U.M., Albini A., Prosperi E. Specific structural determinants are responsible for the antioxidant activity and the cell cycle effects of resveratrol. J. Biol. Chem. 2001;276:22586–22594. doi: 10.1074/jbc.M101846200. [DOI] [PubMed] [Google Scholar]
- 90.Szekeres T., Fritzer-Szekeres M., Saiko P., Jäger W. Resveratrol and resveratrol analogues—Structure—Activity relationship. Pharm. Res. 2010;27:1042–1048. doi: 10.1007/s11095-010-0090-1. [DOI] [PubMed] [Google Scholar]
- 91.Iuga C., Alvarez-Idaboy J.R.l., Russo N. Antioxidant activity of trans-resveratrol toward hydroxyl and hydroperoxyl radicals: A quantum chemical and computation al kinetics study. J. Org. Chem. 2012;77:3868–3877. doi: 10.1021/jo3002134. [DOI] [PubMed] [Google Scholar]
- 92.Xia N., Forstermann U., Li H. Resveratrol as a gene regulator in the vasculature. Curr. Pharm. Biotechnol. 2014;15:401–408. doi: 10.2174/1389201015666140711114450. [DOI] [PubMed] [Google Scholar]
- 93.Jia Z., Zhu H., Misra B.R., Mahaney J.E., Li Y., Misra H.P. EPR studies on the superoxide-scavenging capacity of the nutraceutical resveratrol. Mol. Cell. Biochem. 2008;313:187–194. doi: 10.1007/s11010-008-9756-y. [DOI] [PubMed] [Google Scholar]
- 94.Ungvari Z., Labinskyy N., Mukhopadhyay P., Pinto J.T., Bagi Z., Ballabh P., Zhang C., Pacher P., Csiszar A. Resveratrol attenuates mitochondrial oxidative stress in coronary arterial endothelial cells. Am. J. Physiol.—Heart Circ. Physiol. 2009;297:H1876–H1881. doi: 10.1152/ajpheart.00375.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bremer A., Miller W. Cellular Endocrinology in Health and Disease. Elsevier; Amsterdam, The Netherlands: 2014. Chapter 13-Regulation of Steroidogenesis; pp. 207–227. [Google Scholar]
- 96.Abd-Elhakim Y.M., El Sharkawy N.I., El Bohy K.M., Hassan M.A., Gharib H.S., El-Metwally A.E., Arisha A.H., Imam T.S. Iprodione and/or chlorpyrifos exposure induced testicular toxicity in adult rats by suppression of steroidogenic genes and SIRT1/TERT/PGC-1α pathway. Environ. Sci. Pollut. Res. 2021;28:56491–56506. doi: 10.1007/s11356-021-14339-x. [DOI] [PubMed] [Google Scholar]
- 97.Abd El-Hakim Y.M., Abdel-Rahman Mohamed A., Khater S.I., Hamed Arisha A., Metwally M.M., Nassan M.A., Hassan M.E. Chitosan-stabilized selenium nanoparticles and metformin synergistically rescue testicular oxidative damage and steroidogenesis-related genes dysregulation in high-fat diet/streptozotocin-induced diabetic rats. Antioxidants. 2020;10:17. doi: 10.3390/antiox10010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Qin F., Shen T., Li J., Qian J., Zhang J., Zhou G., Tong J. SF-1 mediates reproductive toxicity induced by Cerium oxide nanoparticles in male mice. J. Nanobiotechnol. 2019;17:1–13. doi: 10.1186/s12951-019-0474-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Vassal M., Rebelo S., Pereira M.d.L. Metal Oxide Nanoparticles: Evidence of Adverse Effects on the Male Reproductive System. Int. J. Mol. Sci. 2021;22:8061. doi: 10.3390/ijms22158061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Hussein M.M., Ali H.A., Saadeldin I.M., Ahmed M.M. Querectin alleviates zinc oxide nanoreprotoxicity in male albino rats. J. Biochem. Mol. Toxicol. 2016;30:489–496. doi: 10.1002/jbt.21812. [DOI] [PubMed] [Google Scholar]
- 101.Ahmed I.Y., Mokhtar I.Y., Maher A.-N., Rakhad A., Jubran M.A. Changes in semen characteristics and sex hormones of rats treated with iron oxide nanoparticles, silver nanoparticles and their mixture. GSC Biol. Pharm. Sci. 2020;12:229–237. doi: 10.30574/gscbps.2020.12.2.0272. [DOI] [Google Scholar]
- 102.Premalatha R., Jubendradass R., Rani S.J.A., Srikumar K., Mathur P.P. A phytooxysterol, 28-homobrassinolide modulates rat testicular steroidogenesis in normal and diabetic rats. Reprod. Sci. 2013;20:589–596. doi: 10.1177/1933719112459241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Lee S.-Y., Gong E.-Y., Hong C.Y., Kim K.-H., Han J.-S., Ryu J.C., Chae H.Z., Yun C.-H., Lee K. ROS inhibit the expression of testicular steroidogenic enzyme genes via the suppression of Nur77 transactivation. Free Radic. Biol. Med. 2009;47:1591–1600. doi: 10.1016/j.freeradbiomed.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 104.Tsai S.C., Lu C.C., Lin C.S., Wang P.S. Antisteroidogenic actions of hydrogen peroxide on rat Leydig cells. J. Cell. Biochem. 2003;90:1276–1286. doi: 10.1002/jcb.10738. [DOI] [PubMed] [Google Scholar]
- 105.Stocco D.M., Wells J., Clark B.J. The effects of hydrogen peroxide on steroidogenesis in mouse Leydig tumor cells. Endocrinology. 1993;133:2827–2832. doi: 10.1210/endo.133.6.8243310. [DOI] [PubMed] [Google Scholar]
- 106.Turner T.T., Lysiak J.J. Oxidative stress: A common factor in testicular dysfunction. J. Androl. 2008;29:488–498. doi: 10.2164/jandrol.108.005132. [DOI] [PubMed] [Google Scholar]
- 107.Abidi P., Zhang H., Zaidi S.M., Shen W.-J., Leers-Sucheta S., Cortez Y., Han J., Azhar S. Oxidative stress-induced inhibition of adrenal steroidogenesis requires participation of p38 mitogen-activated protein kinase signaling pathway. J. Endocrinol. 2008;198:193–208. doi: 10.1677/JOE-07-0570. [DOI] [PubMed] [Google Scholar]
- 108.Peltola V., Huhtaniemi I., Metsa-Ketela T., Ahotupa M. Induction of lipid peroxidation during steroidogenesis in the rat testis. Endocrinology. 1996;137:105–112. doi: 10.1210/endo.137.1.8536600. [DOI] [PubMed] [Google Scholar]
- 109.Abarikwu S., Duru Q., Chinonso O., Njoku R.C. Antioxidant enzymes activity, lipid peroxidation, oxidative damage in the testis and epididymis, and steroidogenesis in rats after co-exposure to atrazine and ethanol. Andrologia. 2016;48:548–557. doi: 10.1111/and.12478. [DOI] [PubMed] [Google Scholar]
- 110.Banerjee B., Chakraborty S., Chakraborty P., Ghosh D., Jana K. Protective Effect of Resveratrol on Benzo(a)Pyrene Induced Dysfunctions of Steroidogenesis and Steroidogenic Acute Regulatory Gene Expression in Leydig Cells. Front. Endocrinol. 2019;10:272. doi: 10.3389/fendo.2019.00272. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is contained within the article.