Abstract
Since 1995, when we reported the case of a patient with glomerulonephritis with IgA deposition that occurred after a methicillin-resistant Staphylococcus aureus (MRSA) infection, many reports of MRSA infection-associated glomerulonephritis have accumulated. This disease is being systematized as Staphylococcus infection-associated glomerulonephritis (SAGN) in light of the apparent cause of infection, and as immunoglobulin A-dominant deposition infection-related glomerulonephritis (IgA-IRGN) in light of its histopathology. This glomerulonephritis usually presents as rapidly progressive glomerulonephritis or acute kidney injury with various degrees of proteinuria and microscopic hematuria along with an ongoing infection. Its renal pathology has shown several types of mesangial and/or endocapillary proliferative glomerulonephritis with various degrees of crescent formation and tubulointerstitial nephritis. IgA, IgG, and C3 staining in the mesangium and along the glomerular capillary walls have been observed on immunofluorescence examinations. A marked activation of T cells, an increase in specific variable regions of the T-cell receptor β-chain-positive cells, hypercytokinemia, and increased polyclonal immune complexes have also been observed in this glomerulonephritis. In the development of this disease, staphylococcal enterotoxin may be involved as a superantigen, but further investigations are needed to clarify the mechanisms underlying this disease. Here, we review 336 cases of IgA-IRGN and 218 cases of SAGN.
Keywords: Staphylococcus aureus, rapidly progressive glomerulonephritis, IgA-dominant glomerulonephritis, Staphylococcus infection-associated glomerulonephritis, bacterial superantigen, T-cell receptor, cytokine, polyclonal activation
1. Introduction
Staphylococci have been identified as causal agents in the genesis of glomerulonephritis. Most reports linking Staphylococci in infection-related glomerulonephritis (IRGN) have emphasized two clinical forms: Staphylococcus epidermidis (S. epidermidis) bacteremia with an infected ventriculojugular shunt [1], and Staphylococcus aureus (S. aureus) bacteremia with endocarditis [2]. These types of glomerulonephritis are caused by the deposition of immune complexes composed of immunoglobulin (Ig)G antibodies and bacterial antigens in the glomeruli. In contrast to those types of glomerulonephritis, in 1995 we reported the case of a patient with glomerulonephritis which had IgA deposition that occurred after a methicillin-resistant S. aureus (MRSA) infection [3]. Since then, many reports of MRSA infection-associated glomerulonephritis have accumulated. Most of the initial reports of MRSA infection-associated glomerulonephritis were from Japan; more recently, however, cases in the U.S. and in Europe have been described [4].
The same clinical features as MRSA infection-associated glomerulonephritis were observed in some cases with a methicillin-sensitive S. aureus or S. epidermidis infection. These types of glomerulonephritis are thus called Staphylococcus infection-associated glomerulonephritis (SAGN) [5,6]. The most common pattern observed in SAGN has consisted of mild-to-moderate IgA and moderate-to-strong complement factor 3 (C3) staining on immunofluorescence observation, with weak or no IgA in 25% of the cases. SAGN is thus not always IgA-dominant [6].
In all of the cases of MRSA infection-associated glomerulonephritis identified by our research group, the deposition of IgA has been remarkable; this feature differs from those of typical postinfection nephritis, which is characterized by glomerular deposition of either C3 and IgG, or of C3 only. Since our 1995 report [3], many descriptions of the same histological features as this glomerulonephritis have accumulated, and the features have been observed in cases with and without staphylococcal infection [7]. These types of glomerulonephritis are thus called IgA-dominant deposition infection-related glomerulonephritis (IgA-IRGN) [7,8].
In this review, we delineate the characteristics of SAGN and IgA-IRGN, and we describe the pathogenesis of SAGN with IgA-dominant deposition.
2. Review Methods
2.1. Literature Search
We searched the available literature in the following electronic databases: PubMed/MEDLINE, EMBASE, and Web of Science: Science Citation Index Expanded. The key words that were used included “Staphylococcus” and “infection” or “IgA-dominant” and “glomerulonephritis”.
Two hundred fifty-four reports were detected, and we collected the 206 reports that were published between our 1995 report [3] and 31 December 2021. Among the 206 reports, 20 reports that were in a language other than English, as well as a single study on birds (a hyacinth macaw), were excluded. Twenty-one other reports were excluded because of the publication type (e.g., review). Among the remaining 164 reports, 39 were excluded because the subjects had different diseases: nonrenal diseases (n = 13), hyper-IgE syndrome (n = 1), end-stage kidney disease (n = 6), urinary tract infection without glomerulonephritis (n = 2), AA amyloidosis (n = 1), lupus nephritis (n = 2), antineutrophil cytoplasmic antibody (ANCA)-associated vasculitis (n = 12), and antiglomerular basement disease (n = 2). One report of drug (rifampicin)-induced glomerulonephritis and five reports of noninfectious kidney diseases were excluded. Five nonclinical studies and two studies with a pool analysis of the literature [5,7] were excluded. Five reports of Staphylococcus aureus infection-related glomerulonephritis with IgA-dominant deposition [9,10,11,12,13] among our 12 reports of infection-related glomerulonephritis will be presented here together. Two pre-2000 cohort studies that were neither IgA-IRGN nor SAGN were also excluded. A final total consisting of 62 case reports (Table S1) [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75], 36 cohort studies [76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111], and our combined reports (Table S2) of IgA-IRGN or SAGN was obtained and qualified.
2.2. Categorize of Selected Cases
In the 36 cohort studies [76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105,106,107,108,109,110,111], the subjects had been identified with the use of varying definitions (Table S2). We categorized these studies as follows: IgA-IRGN or not, and SAGN or not. We analyzed the 62 case reports [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75] of patients with Staphylococcus infection-associated glomerulonephritis with dominant IgA deposition as both IgA-IRGN and SAGN, and we also categorized these reports as IgA-IRGN or not and SAGN or not. We integrated and analyzed our own papers [3,9,10,11,12,13] as both IgA-IRGN and SAGN. Thus, 336 cases of IgA-IRGN and 218 cases of SAGN were analyzed.
3. Clinical Features
3.1. Epidemiology and Characteristics
The incidences of both IgA-IRGN and SAGN are difficult to determine, as there has been no large study of the incidence or prevalence of those diseases in a general population. Table 1 summarizes the characteristics of the reviewed patients with IgA-IRGN and SAGN. According to the studies which included patients who had undergone a renal biopsy, of those patients, the frequency of IgA-IRGN was 0.40%, and the frequency of SAGN was 0.45%. In patients with IgA deposition confirmed by a renal biopsy, 4.31% of the patients were diagnosed with IgA-IRGN and 1.66% were diagnosed with SAGN. Among the patients diagnosed with IRGN, 10.18% of the cases were IgA-IRGN and 11.90% were SAGN.
Table 1.
Characteristics of the reported patients with IgA-IRGN or SAGN.
| IgA-IRGN n = 336 |
SAGN n = 218 |
|||
|---|---|---|---|---|
| Incidence: | ||||
| In patients with biopsy | 0.40% | 117/29,562 | 0.45% | 96/21,257 |
| In patients with IgA deposition | 4.31% | 40/927 | 1.66% | 12/722 |
| In patients with IRGN | 10.18% | 34/334 | 11.90% | 5/42 |
| Mean age, years | 54.7 | 3–90 | 57.4 | 6–90 |
| Male gender | 74.8% | 237/317 | 78.4% | 171/218 |
| Underlying disease: | ||||
| Diabetes | 42.1% | 118/280 | 33.1% | 52/157 |
| Cancer | 6.2% | 12/194 | 16.4% | 11/67 |
IRGN—infection-related glomerulonephritis; SAGN—Staphylococcus infection-associated glomerulonephritis.
Although a predominant age of patients with either IgA-IRGN or SAGN has not been established, the mean age of the reported IgA-IRGN patients was 54.7 years (range 3–90 years) and that of the SAGN patients was 57.4 (range 6–90 years). IgA-IRGN and SAGN have both been more common in men; 74.5% of the IgA-IRGN patients and 78.4% of the SAGN patients have been male.
Although all of the patients in the first reported study of IgA-IRGN had diabetes mellitus as an underlying disease [108], our review indicates that 42.1% of IgA-IRGN patients and 33.1% of SAGN patients have diabetes mellitus. Other than diabetes, malignant tumors have been one of the causes of infection, but malignant tumors were associated with only 6.2% of the IgA-IRGN cases and 16.4% of the SAGN cases.
3.2. Epidemiology and Characteristics
All causative bacteria in the SAGN cases were a staphylococcal strain, and Staphylococcus aureus was most frequently detected at 81.7%. In the patients with IgA-IRGN, a staphylococcal strain was most frequently detected (58.4%), but other bacteria or viruses were detected in 26.5% of those patients.
The infectious features of the patients with IgA-IRGN or SAGN are listed in Table 2. Regarding the infection sites, various types of infection have been described: skin infections, cellulitis or superficial abscesses, endocarditis, osteomyelitis or joint infection, upper respiratory infection or pneumonia, deep visceral abscesses, and others.
Table 2.
Infectious features of the reported patients with IgA-IRGN or SAGN.
| IgA-IRGN n = 336 |
SAGN n = 218 |
|||
|---|---|---|---|---|
| Causative bacteria | ||||
| Staphylococcal strain: | 58.4% | 185/317 | 100.0% | 218/218 |
| S. aureus | 54.9% | 174/305 | 81.7% | 178/218 |
| S. epidermidis | 1.7% | 5/298 | 6.9% | 15/218 |
| Other Staphylococcus | 1.7% | 5/298 | 11.5% | 25/218 |
| Streptococcus strain | 5.5% | 17/310 | 0.5% | 1/211 |
| Other bacteria | 21.0% | 65/310 | 3.3% | 7/211 |
| Unknown/not detected | 23.6% | 73/310 | 0% | 0/211 |
| Infection site: | ||||
| Cellulitis/skin infection | 25.1% | 68/271 | 23.6% | 45/191 |
| Endocarditis | 4.1% | 11/271 | 12.6% | 24/191 |
| Osteomyelitis/joint infection | 11.4% | 31/271 | 17.3% | 33/191 |
| Respiratory infection | 18.8% | 51/271 | 12.0% | 23/191 |
| Visceral abscess | 9.2% | 25/271 | 15.7% | 30/191 |
| Others | 22.9% | 62/271 | 19.4% | 37/191 |
| Unknown | 17.0% | 46/271 | 0% | 0/271 |
The IgA-IRGN and SAGN patients’ infections were typically still ongoing when the patients were encountered; however, the length of time from the infection to the onset of the disease varied, with a mean of 24.9 days (range 0–140 days) in the patients with IgA-IRGN and 28.2 days (range 2–140 days) in the patients with SAGN.
3.3. Clinical Renal Features
Patients with IgA-IRGN or SAGN usually present with rapidly progressive glomerulonephritis (RPGN) or acute kidney injury (AKI)—79.1% in IgA-IRGN and 75.0% in SAGN (Table 3). Various degrees of proteinuria and microscopic hematuria were present in most cases, and nephrotic-range proteinuria was often present in 59.1% of the IgA-IRGN patients and 52.4% of the SAGN patients. Several patients with IgA-IRGN (40.7%) or SAGN (29.5%) had a purpuric lower extremity rash that was similar to IgA vasculitis (Henoch–Schönlein purpura); a skin biopsy revealed leukocytoclastic vasculitis.
Table 3.
Clinical features and laboratory data of the reported patients with IgA-IRGN or SAGN.
| IgA-IRGN n = 336 |
SAGN n = 218 |
|||
|---|---|---|---|---|
| Clinical features: | ||||
| AKI or RPGN | 79.1% | 178/225 | 75.0% | 78/104 |
| Nephrotic syndrome | 59.1% | 101/171 | 52.4% | 75/143 |
| Proteinuria | 98.9% | 183/185 | 98.4% | 183/186 |
| Hematuria | 95.0% | 226/238 | 91.4% | 106/116 |
| Purpura | 40.7% | 46/113 | 29.5% | 49/166 |
| Laboratory data: | ||||
| Excretion of urinary protein, g/day | 4.79 (n = 272) | 0–19.06 | 4.68 (n = 125) | 0–16.0 |
| Serum creatinine level, mg/dL | 3.54 (n = 312) | 0.38–21.94 | 3.61 (n = 138) | 0.38–10.4 |
| Serum IgA level, mg/dL | 642.5 (n = 98) | 97–1850 | 685.4 (n = 77) | 97–1850 |
| Elevated serum IgA level | 76.0% | 73/96 | 78.0% | 46/59 |
| Decreased serum C3 level | 33.3% | 74/222 | 34.3% | 60/175 |
| Decreased serum C4 level | 11.0% | 18/163 | 15.5% | 26/168 |
| Positive test for ANCA | 5.1% | 5/99 | 11.4% | 12/105 |
AKI—acute kidney injury; ANCA—antineutrophil cytoplasmic antibody; RPGN—rapidly progressive glomerulonephritis.
3.4. Laboratory Findings
As an infectious disease, SAGN has shown elevations in the white blood cell counts, erythrocyte sedimentation rates, and serum C-reactive protein levels (Table 3). Various degrees of proteinuria and hematuria and decreased renal function (elevated levels of serum creatinine, etc.) were also observed in SAGN—as seen in RPGN and acute kidney injury (AKI). The mean level of serum creatinine in the reports of IgA-IRGN was 3.54 mg/dL (range 0.38–21.94) and that in SAGN was 3.61 mg/dL (range 0.38–10.4). The mean excretion of urinary protein was 4.79 g/day (range 0–19.06) in IgA-IRGN and 4.68 g/day (range 0–16.0) in SAGN.
A polyclonal elevation of serum IgA was often observed in patients with IgA-IRGN (76.0%) or SAGN (78.0%); the mean serum IgA level was 642.5 mg/dL (range 97–1850) mg/dL in IgA-IRGN, and that in SAGN was 685.4 mg/dL (range 97–1850 mg/dL). The serum complement levels observed in IgA-IRGN or SAGN have varied. Decreased serum C3 levels were observed in 33.3% of patients with IgA-IRGN and in 34.3% of patients with SAGN. Although rheumatoid factor, autoantibodies (i.e., antiglomerular basement membrane antibody, anti-DNA antibody, and antinuclear antibody), and cryoglobulin were not usually detected in the IgA-IRGN or SAGN cases, antineutrophil cytoplasmic antibody (ANCA) was detected in 5.1% of patients with IgA-IRGN and in 11.4% of patients with SAGN, especially in patients with bacterial endocarditis [8,12].
4. Histological Findings
4.1. Light Microscopy Findings
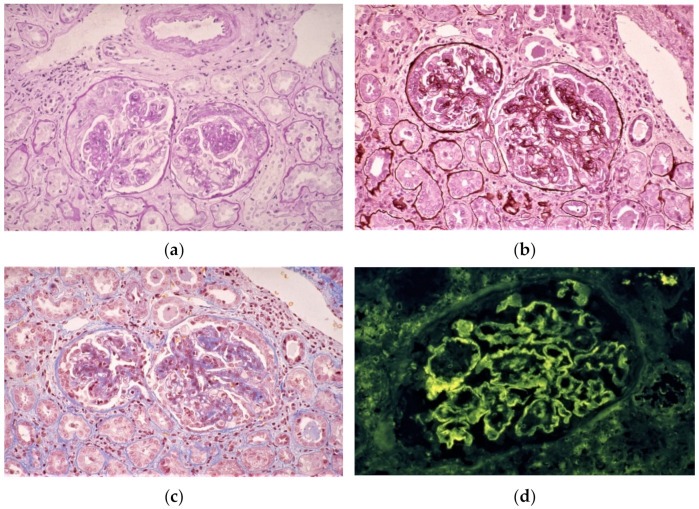
Light microscopy examinations have revealed a variety of types of mesangial and/or endocapillary proliferative glomerulonephritis with various degrees of crescent formation and tubulointerstitial nephritis in SAGN (Figure 1a–c). Endocapillary proliferation was more dominant in patients with IgA-IRGN (71.7%) compared to those with SAGN (58.6%), but the rates of mesangial hypercellularity/proliferation were very similar (73.9% in IgA-IRGN; 64.1% in SAGN). Necrotizing and crescentic glomerulonephritis was present in ~10% of cases of IRGN (9.1% in IgA-IRGN; 10.7% in SAGN), and crescent formation was demonstrated in ~50% of both types of IRGN (56.1% in IgA-IRGN; 47.6% in SAGN).
Figure 1.
Histological findings of SAGN with IgA-dominant deposition. Light microscopy images of renal biopsy samples stained with periodic acid Schiff (a), periodic acid methenamine silver (b), and Masson’s Trichrome (c); 400× magnification. The images (a–c) show mesangial and endocapillary proliferative glomerulonephritis with crescent formation and tubulointerstitial nephritis. (d–f) Immunofluorescence images of renal biopsy samples stained with anti-IgG (d), anti-IgA (e), and anti-C3 (f) antibodies, showing IgG, IgA, and C3 deposition in the mesangium and along the glomerular capillary walls. Electron microscopy images of renal biopsy samples (g,h) show electron-dense deposits in the mesangial and subendothelial areas.
4.2. Immunofluorescence Findings
Immunofluorescence has revealed IgA, IgG, and C3 in immune complex deposits, typically in the mesangium and along the glomerular capillary walls (Figure 1d–f). Positive IgA staining was observed in 100% of the reported patients with IgA-IRGN, but only in 85.1% of patients with SAGN. IgG staining was positive in 44.4% of patients with IgA-IRGN and in 51.3% of patients with SAGN. Positive C3 staining was documented in 97% of patients with IgA-IRGN and in 90.4% of patients with SAGN. C3 staining was typically concurrent with IgA staining, and it was sometimes stronger than the staining for IgA.
4.3. Electron Microscopy Findings
Electron microscopy examinations have frequently revealed electron-dense deposits (EDDs) in the mesangial area, but subendothelial and small subepithelial deposits can also occur (Figure 1g–h). As shown by the data in Table 4, EDDs are observed in the mesangial area in 78.2% of the IgA-IRGN cases and in 85.3% of the SAGN cases. Subendothelial and subepithelial deposits can also occur. In the reported patients with IgA-IRGN, the frequency of subendothelial EDDs was 43.1% and that of subepithelial EDDs was 54.3%. In contrast, 47.1% of the patients with SAGN exhibited subendothelial EDDs, and 40.5% of them had subepithelial EDDs. Unlike the observations of poststreptococcal acute glomerulonephritis (PSAGN), large subepithelial deposits (humps) were fewer but were identified in 37.5% of patients with IgA-IRGN and 31.7% of patients with SAGN.
Table 4.
Histological findings of the reported patients with IgA-IRGN or SAGN.
| IgA-IRGN n = 336 |
SAGN n = 218 |
|||
|---|---|---|---|---|
| Light microscopy: | ||||
| Mesangial hypercellularity | 73.9% | 209/283 | 64.1% | 66/103 |
| Endocapillary proliferation | 71.7% | 203/283 | 58.6% | 106/181 |
| Membranoproliferative GN | 5.9% | 16/270 | 7.8% | 8/103 |
| Necrotizing/crescentic GN | 9.1% | 21/231 | 10.7% | 11/103 |
| Presence of crescents | 56.1% | 143/255 | 47.6% | 78/164 |
| Immunofluorescence: | ||||
| Positive staining with IgG | 44.4% | 118/266 | 51.3% | 79/154 |
| Positive staining with IgA | 100.0% | 303/303 | 85.1% | 149/175 |
| Positive staining with C3 | 97.0% | 291/300 | 90.4% | 161/178 |
| Electron microscopy: | ||||
| Subepithelial EDD | 54.3% | 119/219 | 40.5% | 62/153 |
| Subendothelial EDD | 43.1% | 81/188 | 47.1% | 33/70 |
| Intramembranous EDD | 15.6% | 31/199 | 6.9% | 4/58 |
| Mesangial EDD | 78.2% | 147/188 | 85.3% | 64/75 |
| Humps | 37.5% | 90/240 | 31.7% | 46/145 |
EDD—electron dense deposit; GN—glomerulonephritis.
5. Pathogenesis
5.1. Bacterial Superantigens
Some of the enterotoxins (exotoxins) produced by several bacteria include antigens that have the ability to activate a huge number of T cells in a short amount of time; these antigens are called ‘superantigens’ [112]. In a specific antigen’s recognition, the specific antigen that has been processed by antigen-presenting cells (APCs) binds to the groove of the major histocompatibility complex (MHC) molecules, whereas a superantigen binds directly to the outer part of the MHC molecules without being processed [112]. In contrast, a T-cell receptor (TCR) is composed of variable (V), diversity (D), joining (J), and constant (C) domains, and the VDJ gene segment is referred to as the complementarity determining region 3 (CDR3), which recognizes specific antigens [113]. Upon the recognition of a superantigen by T cells, the T cells bind to this MHC molecule/superantigen complex with specific variable regions of the T-cell receptor β-chain (TCR-Vβ) element for each superantigen via an outer portion that differs from the complementarity-determining region (CDR) [112]. The TCR-Vβ repertoire includes ~26 types, and there are multiple TCR-Vβ regions that correspond to a single superantigen—even if the TCR-Vβ region is specific. Only ~0.0001% of the T cells are thus activated in an adaptive immune response, but superantigen exposure can activate up to 30% of the T cells [114].
Superantigens stimulate resting T cells to proliferate, causing a massive activation of T cells and a subsequent release of T-cell-derived lymphokines (e.g., interleukin [IL]-1, -2, or -6) and cytokines (e.g., tumor necrosis factor-alpha [TNF-α] or interferon-gamma [INF-γ]) [115]. There have been reports of a role of staphylococcal enterotoxin in the pathogenesis of toxic shock syndrome [115] and other autoimmune diseases, including rheumatoid arthritis, Kawasaki disease, Sjögren syndrome, and multiple sclerosis [115]. In these diseases, an increase in the usages of some specific TCR-Vβ regions is thought to be a marker of superantigen-related disease [115]. Twenty-six different staphylococcal derivatives have been established as superantigens: toxic shock syndrome toxin-1 (TSST-1), 11 staphylococcal enterotoxins (SE), and 14 staphylococcal enterotoxin-like proteins [116,117].
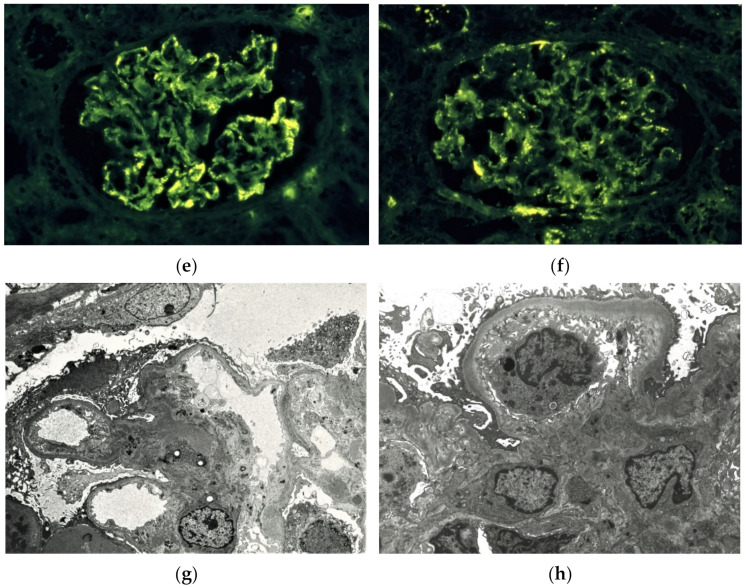
In the culture supernatants of blood, urine, sputum, and various fluid samples obtained from our patients with SAGN with dominant IgA deposition, staphylococcal enterotoxin C (SEC) was most frequently detected (in 20 of 23 patients). SEA was detected in eight patients, SEB in three, SED in one, and TSST-1 in 13 patients [3,9,10,11,12,13]. SEC and TSST-1 were also detected in SAGN patients with dominant IgA deposition in case reports other than ours [47,58,71]. In analyses of 17 types of TCR-Vβ regions of peripheral blood mononuclear cells (PBMCs) that were obtained from SAGN patients with dominant IgA deposition (Figure 2), the percentages of Vβ8- and Vβ12.1-positive cells were also significantly higher than those observed in healthy controls [3,9,10,11,12,13].
Figure 2.
TCR-Vβ usages in SAGN with IgA-dominant deposition. Peripheral blood mononuclear cells (PBMCs) obtained from patients with SAGN, S. aureus-infected patients without glomerulonephritis, and healthy controls stained with fluorescence-labeled monoclonal antibodies against 17 types of TCR-Vβ (6 of 17 types of TCR-Vβ were reported [3,9,10,11,12,13], and the other 11 types are unpublished data); Vβ5.1 (Vβ5c), Vβ5.2+5.3 (Vβ5a), Vβ 5.3 (Vβ5b), Vβ6.7 (Vβ6a), Vβ8 subfamily (Vβ8a) and Vβ12.1 (Vβ12a), Vβ2, Vβ3 (Vβ3a), Vβ11, Vβ13 (Vβ13a), Vβ13.6, Vβ14, Vβ16, Vβ17, Vβ20, Vβ21.3, and Vβ22. The stained PBMCs were then analyzed using flow cytometry. The percentages of 17 TCR-Vβ-positive cells among circulating CD3-positive cells are shown. Black closed circles: the mean percentages of cells in patients with SAGN. Gray closed circles: the mean percentages of cells in S. aureus-infected patients without glomerulonephritis. Open circles: the mean percentages of cells in healthy controls. Bars: the standard deviation of positive cells. The percentages of Vβ8- and Vβ12.1-positive cells in the SAGN patients were significantly increased compared to those in the controls, and the percentages of Vβ8-positive cells in the patients with SAGN were significantly higher compared to those in patients without glomerulonephritis (* p < 0.05; ** p < 0.005).
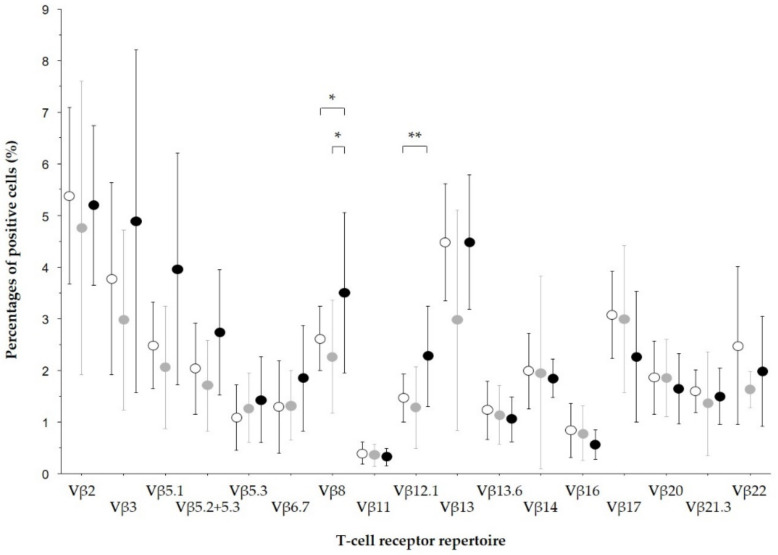
Specific TCR-Vβ usage was also detected in SAGN cases in a report other than ours [47]. The results of a serum cytokine analysis (Figure 3) demonstrated significantly higher serum levels of IL-2, IL-6, IL-8, IL-10, and TNF-α in SAGN patients with dominant IgA deposition compared to those of healthy controls [9,10,11,12,13]. Cytokinemia was also detected in SAGN cases in case reports other than ours [58]. By enzyme-linked immunosorbent assays using anti-C3d antibodies and either antihuman IgG or IgA antibodies, the amounts of both the circulating immune complexes containing IgG and those containing IgA were significantly increased in our patients of SAGN with dominant IgA deposition compared to those in the healthy controls [3].
Figure 3.
Serum cytokine levels in SAGN with IgA-dominant deposition. Sera were obtained from patients with SAGN S. aureus-infected patients without glomerulonephritis and healthy controls, and the following 10 cytokines were measured by enzyme-linked immunosorbent assays: IL-1α, -1β, IL-2, IL-4, IL-6, IL-8, IL-10, TNF-α, TNF-β, and INF-γ [9,10,11,12,13]. The serum levels of eight cytokines are shown. Black closed bars: the mean levels of cytokines in patients with SAGN. Gray closed bars: the mean levels of cytokines in S. aureus-infected patients without glomerulonephritis. Open bars: the mean levels of cytokines in healthy controls. Bars: the standard deviation. Serum levels of IL-2, IL-6, IL-8, IL-10, and TNF-α in the patients with SAGN were significantly higher compared to those in the controls, and serum levels of IL-8 and TNF-α in the patients with SAGN were significantly higher compared to those in patients without glomerulonephritis (* p < 0.05; ** p < 0.01; *** p < 0.001). Serum IL-4 and TNF-β were not detected in all three groups.
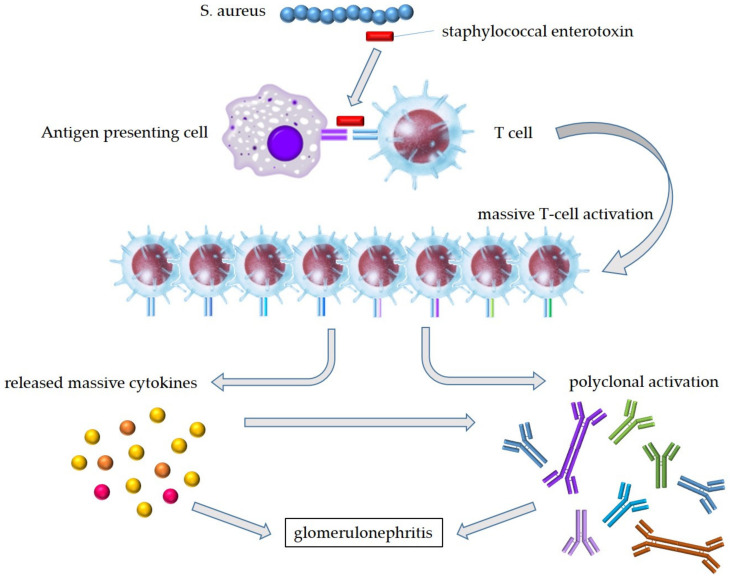
It has thus been speculated that staphylococcal enterotoxins activate T cells as a superantigen via specific TCR-Vβ regions, and the subsequent excessive release of cytokines activates not only T cells but also B cells; the polyclonal immunoglobulin production leads to the formation of immune complexes, resulting in the onset of SAGN with dominant IgA deposition (Figure 4). In contrast, the reported cases of IgA-IRGN developed due to infections that were caused by bacteria or viruses for which superantigens had not been confirmed, and it may thus not be possible to say that superantigens are involved in all IgA-IRGN cases. However, IgA-IRGN was recently confirmed in a patient with a severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection [17], and SARS-CoV-2 was recently reported to cause many of the biological and clinical consequences of a superantigen [118].
Figure 4.
Hypothesis of pathogenesis in SAGN with IgA-dominant deposition. Staphylococcal enterotoxins produced by S. aureus bind to specific TCR-Vβ on T cells and the outer part of the MHC molecules without being processed. Bacterial superantigens lead the MHC-unrestricted huge T-cell activation. The subsequent excessive release of cytokines activates not only T cells but also B cells; the polyclonal immunoglobulin production leads to the formation of immune complexes, resulting in the onset of SAGN. S. aureus—Staphylococcus aureus.
Specific TCR-Vβ usage in an IgA-IRGN patient with a Chlamydia pneumonia infection was also detected [62]. Therefore, in IgA-IRGN associated with bacteria and/or viruses that were not produced by a superantigen, the bacterium and/or virus may act as a superantigenic or superantigen-like pathogen, resulting in cytokinemia and the production of polyclonal immunoglobulin.
It was recently demonstrated in an animal model that the specific TCR-Vβ usage in S. aureus infection was the result of using the specific VDJ gene segment [119]. That report suggested that the specific TCR-Vβ usage in an S. aureus infection may be recognized by the specific antigen originating from S. aureus, instead of from superantigens. In our studies, however, we observed specific TCR-Vβ usage in SAGN patients with dominant IgA deposition, unlike in patients with an S. aureus infection without glomerulonephritis [3,9,10,11,12,13]. In addition to the S. aureus infection that causes the specific TCR-Vβ usage, more specific TCR-Vβ usage was found in SAGN, suggesting that the onset of SAGN has factors other than the antigen associated with the infection. Further analyses of the uses of the specific VDJ gene segment in SAGN are needed.
It has also been demonstrated that several single-nucleotide polymorphisms (SNPs) on the human leukocyte antigen (HLA) class II region of chromosome six were enriched in the infection group of a genomewide association study of biological specimens from culture-confirmed cases and matched controls [120]. Furthermore, it was reported that some bacterial superantigens had a high affinity with specific HLA class II alleles [121]. We demonstrated a specific usage of TCR-Vβ in SAGN, but MHC molecules (HLA class II), which bind to superantigens on the opposite side of TCR-Vβ, have not been analyzed. It could thus be informative to examine MHC molecules in SAGN.
ANCA has been detected in several patients with IgA-IRGN and/or SAGN, and several research groups have reported expansions of various T cell subsets in patients with ANCA-associated vasculitis [122]. However, other studies (including ours) demonstrated that there was no difference in TCR-Vβ usage in peripheral blood and bronchoalveolar lavage in ANCA-associated vasculitis [123,124]. Expansions of peripheral blood T cell subsets expressing T-cell receptors with ANCA-associated vasculitis are thus a controversial topic. We speculate that ANCA-associated vasculitis may be different from SAGN with dominant IgA deposition, which is associated with circulating staphylococcal superantigens.
5.2. Neutrophil Extracellular Traps (NETs)
Regarding one of the pathogeneses of ANCA-associated vasculitis, neutrophil extracellular traps (NETs) have been described [125]. NETs are structures of chromatin fibers that are released by dying neutrophils, which trap and kill extracellular invading microbes [126]. However, this DNA web (which contains a number of antimicrobial peptides including myeloperoxidase and proteinase-3) can also stick to and damage the endothelium of small blood vessels, causing vasculitis [125,127]. NETs may be associated with pathology in several kidney diseases, such as AKI, lupus nephritis, and antiglomerular basement membrane disease [128], but the involvement of NETs in infection-related glomerulonephritis is not yet clear.
5.3. Dominant IgA Deposition
The mechanism by which IgA is deposited on the glomerulus, which is a characteristic of IgA-IRGN/SAGN, is not clear. IgA-IRGN/SAGN and IgA nephropathy are similar in that IgA is deposited on the glomerulus, but IgA deposition has not been observed on sclerotic glomeruli in SAGN (which is not similar to IgA nephropathy) [129]. In a proteome analysis of kidney biopsy tissues of SAGN patients reported in 2020, significantly higher levels of monocyte/macrophage proteins, a lower abundance of metabolic pathway proteins, and higher levels of extracellular matrix proteins in SAGN were demonstrated compared to the corresponding values in IgA nephropathy [130].
In patients with IgA nephropathy, galactose-deficient IgA1 (Gd-IgA1) depositions were observed in the glomeruli [131]. Gd-IgA1 depositions were also identified in the glomeruli of patients with IgA-IRGN associated with parvovirus B19 infection [24] and of patients with an infection of unknown origin [18]. However, in a cohort analysis of 12 patients with IgA-IRGN [80], the Gd-IgA1 staining showed very weakly positive or negative findings, unlike IgA nephropathy. It was thus speculated that IgA-IRGN and IgA nephropathy are similar regarding at least some points, such as the deposition of glomerular IgA, but these diseases appear to remain separate disease entities.
6. Treatments and Outcomes
6.1. Treatments
Because persistent infection is an important component in the onset and progression of both IgA-IRGN and SAGN, the treatments for these diseases are essentially treatments for the infecting bacterium or virus. In particular, staphylococcal infections in SAGN are often intractable and present difficulties in diagnosis, with drug-resistant bacteria, deep infection sites, and weakness of immunity. Achieving the appropriate diagnosis of the infectious disease is thus the initial requirement. The diagnoses of infections based on the results of laboratory tests and blood cultures (and the culturing of microbial isolates in particular) are essential to both the determination of the antimicrobial susceptibility and the identification of effective treatments to control the infection. Modalities including X-rays, CT scans, MRIs, transthoracic ultrasonography, and, if necessary, an esophageal echo examination, are thus helpful for identifying the site of infection.
In cases of S. aureus infections, resistance to methicillin is particularly relevant to the selection of antibiotics. For patients with a MRSA infection, polypeptide antibiotics (vancomycin, teicoplanin, etc.) and aminoglycoside antibiotics (arbekacin, etc.) are used at doses that are based on the patient’s renal function. It is necessary to adjust the dose(s) while monitoring the drug concentration(s) in order to prevent side effects. In cases with deep infection sites, a prolonged antibiotics course of up to six weeks might be required, and the removal of infected lesions by surgery or drainage may also be useful.
A well-controlled postinfection treatment with one or more corticosteroids and/or immunosuppressants can result in a rapid improvement of urinary parameters and the retention of renal function. In a cohort of elderly patients, renal lesions improved in only 14% of the patients treated with corticosteroids, and 18% of the patients died due to recurrent sepsis [98]. In another investigation of patients with endocarditis, the mortality of the patients treated with corticosteroids (23.5%) was higher than that of the patients treated with antibiotics alone (10%) [90]. In the 62 case reports of IgA-IRGN or SAGN that we reviewed [14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75], 34 of 66 patients were treated with corticosteroids. Among the 34 patients treated with corticosteroids, four patients (12%) died, ten patients (29%) developed end-stage kidney disease (ESKD), and 14 patients (41%) achieved remission. In contrast, among the 32 patients treated without corticosteroids, two patients (6%) died, four patients (13%) developed ESKD, and 14 patients (44%) achieved remission. It thus appears that corticosteroids and/or immunosuppressants usually exacerbate the infection and may cause its recurrence.
Alternative treatments for IgA-IRGN or SAGN have been reported; the efficacy of plasma exchange therapy for removing the immune complexes involved in the development of SAGN [71] and the utility of endotoxin adsorption therapy with polymyxin-immobilized fiber [109] have been described.
6.2. Outcomes
The prognoses of IgA-IRGN and SAGN have not yet been established, but the outcomes may be dependent on the eradication of the infection. Our review found that among patients with IgA-IRGN, 17.1% (34/199) died from the disease and 27.9% (50/179) suffered end-stage renal failure. Similarly, 17.6% of patients with SAGN (16/91) died and 31.0% (22/71) suffered end-stage renal failure. Diagnosis and treatment with the appropriate antibiotics are often delayed in cases with deep infection sites, which allows chronic damage to accrue. The risk factors for poor renal outcomes may be similar to those of infectious disease, i.e., advanced age, diabetes mellitus, cancer/malignant tumor, and deteriorated renal function before presentation.
7. Conclusions
IgA-IRGN and SAGN are considered to be similar diseases in that most cases of IgA-IRGN are due to infection with S. aureus, and most cases of SAGN exhibit IgA deposition in glomeruli. Although positive IgA and C3 staining on immunofluorescence is an essential finding in IgA-IRGN, weak or no IgA staining has been observed in 25% of SAGN cases. In contrast, S. aureus infection is an essential finding in SAGN, but IgA-IRGN can occur with infections other than S. aureus. In analyses of the pathogenic mechanism of both diseases, researchers should keep in mind the commonalities and differences between IgA-IRGN and SAGN.
Acknowledgments
We thank our colleagues for participating in this review: Hirayasu Kai, Joichi Usui, Kaori Mase, and Kunihiro Yamagata (Department of Nephrology, University of Tsukuba); Naoto Yamaguchi (Ibaraki Prefectural University of Health Sciences); Keigyo Yoh and Takashi Ishizu (Department of Nephrology, Ushiku Aiwa Hospital); and Yoshio Shimizu (Department of Nephrology, Juntendo University Shizuoka Hospital).
Supplementary Materials
The following supporting information can be downloaded at: www.mdpi.com/article/10.3390/ijms23137482/s1.
Author Contributions
All authors contributed to the writing of the initial draft of the paper; M.K. provided Figure 1; K.H. reanalyzed the flow cytometry data and drew Figure 2; A.K. reanalyzed the ELISA data and provided Figure 3. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not available.
Informed Consent Statement
Not available.
Data Availability Statement
Not available.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This manuscript received no specific grants from any funding agency.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dobrin R.S., Day N.K., Quie P.G., Moore H.L., Vernier H.L., Michael A.F., Fish A.J. The role of complement, immunoglobulin and bacterial antigen in coagulase-negative staphylococcal shunt nephritis. Am. J. Med. 1975;59:660–673. doi: 10.1016/0002-9343(75)90227-2. [DOI] [PubMed] [Google Scholar]
- 2.Pertschuk L.P., Vuletin J.C., Sutton A.L., Velazquez L.A. Demonstration of antigen and immune complex in glomerulonephritis due to Staphylococcus aureus. Am. J. Clin. Pathol. 1976;66:1027. doi: 10.1093/ajcp/66.6.1027. [DOI] [PubMed] [Google Scholar]
- 3.Koyama A., Kobayashi M., Yamaguchi N., Yamagata K., Takano K., Nakajima M., Irie F., Goto M., Igarashi M., Iitsuka T., et al. Glomerulonephritis associated with MRSA infection: A possible role of bacterial superantigen. Kidney Int. 1995;47:207–216. doi: 10.1038/ki.1995.25. [DOI] [PubMed] [Google Scholar]
- 4.Denton M.D., Digumarthy S.R., Chua S., Colvin R.B. Case records of the Massachusetts General Hospital. Case 20-2006. An 84-year-old man with staphylococcal bacteremia and renal failure. N. Engl. J. Med. 2006;354:2803–2813. doi: 10.1056/NEJMcpc069012. [DOI] [PubMed] [Google Scholar]
- 5.Wang S.Y., Bu R., Zhang Q., Liang S., Wu J., Liu X.Z.S., Cai G.Y., Chen X.M. Clinical, Pathological, and Prognostic Characteristics of Glomerulonephritis Related to Staphylococcal Infection. Medicine. 2016;95:e3386. doi: 10.1097/MD.0000000000003386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Satoskar A.A., Parikh S.V., Nadasdy T. Epidemiology, pathogenesis, treatment and outcomes of infection-associated glomerulonephritis. Nat. Rev. Nephrol. 2020;16:32–50. doi: 10.1038/s41581-019-0178-8. [DOI] [PubMed] [Google Scholar]
- 7.Bu R., Li Q., Duan Z.Y., Wu J., Chen P., Chen X.M., Cai G.Y. Clinicopathologic features of IgA-dominant infection-associated glomerulonephritis: A pooled analysis of 78 cases. Am. J. Nephrol. 2015;41:98–106. doi: 10.1159/000377684. [DOI] [PubMed] [Google Scholar]
- 8.Nasr S.H., D’Agati V.D. IgA-dominant postinfectious glomerulonephritis: A new twist on an old disease. Nephron Clin. Pract. 2011;119:c18–c25. doi: 10.1159/000324180. [DOI] [PubMed] [Google Scholar]
- 9.Hirayama K., Kobayashi M., Muro K., Yoh K., Yamagata K., Koyama A. Specific T-cell receptor usage with cytokinemia in Henoch-Schonlein purpura nephritis associated with Staphylococcus aureus infection. J. Intern. Med. 2001;249:289–295. doi: 10.1046/j.1365-2796.2001.00815.x. [DOI] [PubMed] [Google Scholar]
- 10.Yoh K., Kobayashi M., Yamaguchi N., Hirayama K., Ishizu T., Kikuchi S., Iwabuchi S., Muro K., Nagase S., Aoyagi K., et al. Cytokines and T-cell responses in superantigen-related glomerulonephritis following methicillin-resistant Staphylococcus aureus infection. Nephrol. Dial. Transplant. 2000;15:1170–1174. doi: 10.1093/ndt/15.8.1170. [DOI] [PubMed] [Google Scholar]
- 11.Kobayashi M., Koyama A. Methicillin-resistant Staphylococcus aureus (MRSA) infection in glomerulonephritis—A novel hazard emerging on the horizon. Nephrol. Dial. Transplant. 1998;13:2999–3001. doi: 10.1093/ndt/13.12.2999. [DOI] [PubMed] [Google Scholar]
- 12.Hirayama K., Kobayashi M., Kondoh M., Muro K., Iwabuchi S., Yoh K., Ishizu T., Kikuchi S., Yamaguchi N., Nagase S., et al. Henoch-Schonlein purpura nephritis associated with methicillin-resistant Staphylococcus aureus infection. Nephrol. Dial. Transplant. 1998;13:2703–2704. doi: 10.1093/ndt/13.10.2703. [DOI] [PubMed] [Google Scholar]
- 13.Yoh K., Kobayashi M., Hirayama A., Hirayama K., Yamaguchi N., Nagase S., Koyama A. A case of superantigen-related glomerulonephritis after methicillin-resistant Staphylococcus aureus (MRSA) infection. Clin. Nephrol. 1997;48:311–316. [PubMed] [Google Scholar]
- 14.Garcia R.A., Gaznabi S., Musoke L., Osnard M., Balakumaran K., Armitage K.B., Al-Kindi S.G., Ginwalla M., Abu-Omar Y., Elamm C.A. LVAD vasculitis case series: Suggestion of a new ratal LVAD-related phenomenon. JACC Case Rep. 2021;3:1013–1017. doi: 10.1016/j.jaccas.2021.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nogueira R.F., Oliveira N., Sousa V., Alves R. Staphylococcus-induced glomerulonephritis: Potential role for corticosteroids. BMJ Case Rep. 2021;14:e237011. doi: 10.1136/bcr-2020-237011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sahoo R.R., Pradhan S., Goel A.P., Wakhlu A. Staphylococcus-associated acute glomerulonephritis in a patient with dermatomyositis. BMJ Case Rep. 2021;14:e236695. doi: 10.1136/bcr-2020-236695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pérez A., Torregrosa I., D’Marco L., Juan I., Terradez L., Solís M.Á., Moncho F., Carda-Batalla C., Forner M.J., Gorriz J.L. IgA-dominant infection-associated glomerulonephritis following SARS-CoV-2 infection. Viruses. 2021;13:587. doi: 10.3390/v13040587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Han W., Suzuki T., Watanabe S., Nakata M., Ichikawa D., Koike J., Oda T., Suzuki H., Suzuki Y., Shibagaki Y. Galactose-deficient IgA1 and nephritis-associated plasmin receptors as markers for IgA-dominant infection-related glomerulonephritis: A case report. Medicine. 2021;100:e24460. doi: 10.1097/MD.0000000000024460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hellwege R.S., Gawaz M. Right-sided infective endocarditis in association with a left-to-right shunt complicated by haemoptysis and acute renal failure: A case report. BMC Cardiovasc. Disord. 2020;20:494. doi: 10.1186/s12872-020-01772-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brunet A., Julien G., Cros A., Beaudoux O., Hittinger-Roux A., Bani-Sadr F., Servettaz A., N’Guyen Y. Vasculitides and glomerulonephritis associated with Staphylocococcus aureus infective endocarditis: Case reports and mini-review of the literature. Ann. Med. 2020;52:265–274. doi: 10.1080/07853890.2020.1778778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang Y., Wang H.B., Chu B., Zhao H.Z., Li H., Zhou H.M., Wang T. Disparate effects of methicillin-resistant Staphylococcus aureus infection on renal function in IgA-dominant infection-associated glomerulonephritis and menstrual toxic shock syndrome: A case report and literature review. J. Int. Med. Res. 2020;48:300060520933810. doi: 10.1177/0300060520933810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nguyen N., Chikkalingaiah K.M., Walker P.D., Wall B.M. Resolution of IgA and C3 immune deposits in Staphylococcus infection-associated glomerulonephritis in a kidney transplant recipient. Clin. Nephrol. 2020;94:97–102. doi: 10.5414/CN110059. [DOI] [PubMed] [Google Scholar]
- 23.Indhumathi E., Dhanapriya J., Dineshkumar T., Sakthirajan R., Gopalakrishnan N. Hansen’s disease with lepra reaction presenting with IgA dominant infection related glomerulonephritis. Indian J. Pathol. Microbiol. 2020;63:289–291. doi: 10.4103/IJPM.IJPM_654_17. [DOI] [PubMed] [Google Scholar]
- 24.Shirai Y., Miura K., Yabuuchi T., Nagasawa T., Ishizuka K., Takahashi K., Taneda S., Honda K., Yamaguchi Y., Suzuki H., et al. Rapid progression to end-stage renal disease in a child with IgA-dominant infection-related glomerulonephritis associated with parvovirus B19. CEN Case Rep. 2020;9:423–430. doi: 10.1007/s13730-020-00501-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Klimko A., Toma G.A., Ion L., Mehedinti A.M., Andreiana I. A Case Report of Generalized Pustular Psoriasis Associated With IgA Nephropathy. Cureus. 2020;12:e10090. doi: 10.7759/cureus.10090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Völker L.A., Burkert K., Scholten N., Grundmann F., Kurschat C., Benzing T., Hampl J., Becker J.U., Müller R.U. A case report of recurrent membranoproliferative glomerulonephritis after kidney transplantation due to ventriculoatrial shunt infection. BMC Nephrol. 2019;20:296. doi: 10.1186/s12882-019-1472-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Carbayo J., Rodriguez-Benitez P., Diaz-Crespo F., Muñoz de Morales A.M. IgA dominant postinfectious glomerulonephritis secondary to cutaneous infection by methicillin-resistant Staphylococcus aureus. Nefrologia. 2019;39:447–449. doi: 10.1016/j.nefroe.2018.10.015. [DOI] [PubMed] [Google Scholar]
- 28.Alqahtani H., Alqahtani F.Y., Aleanizy F.S., Baloch S., Tabb D. IgA Nephropathy Flare-Up Mimicking Staphylococcus Post-Infection Glomerulonephritis in Patient with Staphylococcus Aureus Infection Treated with Cefazolin: A Case Report and Brief Review of the Literature. Am. J. Case Rep. 2019;20:508–510. doi: 10.12659/AJCR.914935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Parente Y.D.M., Castro A.L., Araújo F.B., Teixeira A.C., Lima Í.C., Daher E.F. Acute renal failure by rapidly progressive glomerulonephritis with IgA deposition in a patient concomitantly diagnosed with multibacillary Hansen’s disease: A case report. J. Bras. Nefrol. 2019;41:152–156. doi: 10.1590/2175-8239-jbn-2018-0056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molina-Andújar A., Montagud-Marrahí E., Cucchiari D., Ventura-Aguiar P., De Sousa-Amorim E., Revuelta I., Cofan F., Solé M., García-Herrera A., Diekmann F., et al. Postinfectious acute glomerulonephritis in renal transplantation: An emergent aetiology of renal allograft loss. Case Rep. Transplant. 2019;2019:7438254. doi: 10.1155/2019/7438254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Orozco Guillén A.O., Velazquez Silva R.I., Moguel González B., Guell Y.A., Garciadiego Fossas P., Custodio Gómez I.G., Miranda Araujo O., Soto Abraham V., Piccoli G.B., Madero M. Acute IgA-dominant glomerulonephritis associated with syphilis infection in a pregnant teenager: A new disease association. J. Clin. Med. 2019;8:114. doi: 10.3390/jcm8010114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.De Sá D.C., Rodrigues L., Santos L., Romãozinho C., Macário F., Marinho C., Pratas J., Alves R., Figueiredo A. Staphylococcus Infection–Associated Glomerulonephritis in a Kidney Transplant Patient: Case Report. Transplant. Proc. 2018;50:853–856. doi: 10.1016/j.transproceed.2018.02.005. [DOI] [PubMed] [Google Scholar]
- 33.Shimamura Y., Maeda T., Gocho Y., Ogawa Y., Takizawa H. IgA-dominant infection-related glomerulonephritis. Nefrologia. 2018;38:669–670. doi: 10.1016/j.nefro.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 34.Basic-Jukic N., Coric M., Kastelan Z. IgA-dominant extracapillary proliferative glomerulonephritis following Escherichia coli sepsis in a renal transplant recipient. Transpl. Infect. Dis. 2018;20:e12927. doi: 10.1111/tid.12927. [DOI] [PubMed] [Google Scholar]
- 35.Mahmood T., Puckrin R., Sugar L., Naimark D. Staphylococcus-Associated Glomerulonephritis Mimicking Henoch-Schonlein Purpura and Cryoglobulinemic Vasculitis in a Patient With an Epidural Abscess: A Case Report and Brief Review of the Literature. Can. J. Kidney Health Dis. 2018;5:2054358118776325. doi: 10.1177/2054358118776325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Liang J.H., Fang Y.W., Yang A.H., Tsai M.H. Devastating renal outcome caused by skin infection with methicillin-resistant Staphylococcus aureus: A case report. Medicine. 2016;95:e4023. doi: 10.1097/MD.0000000000004023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Okada M., Sato M., Ogura M., Kamei K., Matsuoka K., Ito S. Central venous catheter infection-related glomerulonephritis under long-term parenteral nutrition: A report of two cases. BMC Res. Notes. 2016;9:196. doi: 10.1186/s13104-016-1997-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Srinivasaraghavan R., Krishnamurthy S., Dubey A.K., Parameswaran S., Biswal N., Srinivas B.H. IgA Dominant Post-infectious Glomerulonephritis in a 12-year-old Child. Indian J. Pediatr. 2016;83:470–472. doi: 10.1007/s12098-015-1879-z. [DOI] [PubMed] [Google Scholar]
- 39.Nayer A., Davda G., Pai R., Ortega L.M. IgA-dominant post-infectious glomerulonephritis; making another case in support of renal biopsy in type 2 diabetic nephropathy. J. Ren. Inj. Prev. 2016;5:45–47. doi: 10.15171/jrip.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Caetano J., Pereira F., Oliveira S., Delgado Alves J. IgA-dominant postinfectious glomerulonephritis induced by methicillin-sensitive Staphylococcus aureus. BMJ Case Rep. 2015;2015:bcr2014208513. doi: 10.1136/bcr-2014-208513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hayashi S., Mori A., Kawamura T., Ito S., Shibuya T., Fushimi N. Glomerulonephritis Caused by CV Catheter-related Blood Stream Infection. Intern. Med. 2015;54:2219–2223. doi: 10.2169/internalmedicine.54.4607. [DOI] [PubMed] [Google Scholar]
- 42.Rus R.R., Toplak N., Vizjak A., Mraz J., Ferluga D. IgA-dominant acute poststreptococcal glomerulonephritis with concomitant rheumatic fever successfully treated with steroids: A case report. Croat. Med. J. 2015;56:567–572. doi: 10.3325/cmj.2015.56.567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Saad M., Daoud M., Nasr P., Syed R., El-Sayegh S. IgA-dominant post-infectious glomerulonephritis presenting as a fatal pulmonary-renal syndrome. Int. J. Nephrol. Renovasc. Dis. 2015;8:77–81. doi: 10.2147/IJNRD.S84061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kikuchi H., Aoyagi M., Nagahama K., Yamamura C., Arai Y., Hirasawa S., Aki S., Inaba N., Tanaka H., Tamura T. IgA-dominant postinfectious glomerulonephritis associated with Escherichia coli infection caused by cholangitis. Intern. Med. 2014;53:2619–2624. doi: 10.2169/internalmedicine.53.2742. [DOI] [PubMed] [Google Scholar]
- 45.Mandai S., Aoyagi M., Nagahama K., Arai Y., Hirasawa S., Aki S., Inaba N., Tanaka H., Tsuura Y., Tamura T., et al. Post-Staphylococcal infection Henoch–Schonlein purpura nephritis: A case report and review of the literature. Ren. Fail. 2013;35:869–874. doi: 10.3109/0886022X.2013.794703. [DOI] [PubMed] [Google Scholar]
- 46.Erqou S., Kamat N., Moschos S., Im A., Bastacky S. A 61 year diabetic man with methicillin-sensitive Staphylococcus aureus septic arthritis and acute renal failure: A case of IgA-dominant postinfectious glomerulonephritis. Nephrology. 2012;17:780–781. doi: 10.1111/j.1440-1797.2012.01602.x. [DOI] [PubMed] [Google Scholar]
- 47.Kimata T., Tsuji S., Yoshimura K., Tsukaguchi H., Kaneko K. Methicillin-resistant Staphylococcus aureus-related glomerulonephritis in a child. Pediatr. Nephrol. 2012;27:2149–2152. doi: 10.1007/s00467-012-2229-2. [DOI] [PubMed] [Google Scholar]
- 48.Chen Y.-R., Wen Y.-K. Favorable Outcome of Crescentic IgA Nephropathy Associated with Methicillin-Resistant Staphylococcus aureus Infection. Ren. Fail. 2011;33:96–100. doi: 10.3109/0886022X.2010.541576. [DOI] [PubMed] [Google Scholar]
- 49.Wehbe E., Salem C., Simon J.F., Navaneethan S.D., Pohl M. IgA-dominant Staphylococcus infection-associated glomerulonephritis: Case reports and review of the literature. NDT Plus. 2011;4:181–185. doi: 10.1093/ndtplus/sfr017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kapadia A.S., Panda M., Fogo A.B. Postinfectious glomerulonephritis: Is there a role for steroids? Indian J. Nephrol. 2011;21:116–119. doi: 10.4103/0971-4065.82141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Upadhaya B.K., Sharma A., Khaira A., Dinda A.K., Agarwal S.K., Tiwari S.C. Transient IgA nephropathy with acute kidney injury in a patient with dengue fever. Saudi J. Kidney Dis. Transplant. 2010;21:521–525. [PubMed] [Google Scholar]
- 52.Riley A.M., Wall B.M., Cooke C.R. Favorable Outcome After Aggressive Treatment of Infection in a Diabetic Patient With MRSA-Related IgA Nephropathy. Am. J. Med. Sci. 2009;337:221–223. doi: 10.1097/MAJ.0b013e318184a4a1. [DOI] [PubMed] [Google Scholar]
- 53.Okuyama S., Wakui H., Maki N., Kuroki J., Nishinari T., Asakura K., Komatsuda A., Sawada K. Successful treatment of post-MRSA infection glomerulonephritis with steroid therapy. Clin. Nephrol. 2008;70:344–347. doi: 10.5414/CNP70344. [DOI] [PubMed] [Google Scholar]
- 54.Kusaba T., Nakayama M., Kato H., Uchiyama H., Sato K., Kajita Y. Crescentic glomerulonephritis associated with totally implantable central venous catheter-related Staphylococcus epidermidis infection. Clin. Nephrol. 2008;70:54–58. doi: 10.5414/CNP70054. [DOI] [PubMed] [Google Scholar]
- 55.Ho C.-I., Wen Y.-K., Chen M.-L. Glomerulonephritis with Acute Renal Failure Related to Osteomyelitis. J. Chin. Med. Assoc. 2008;71:315–317. doi: 10.1016/S1726-4901(08)70129-1. [DOI] [PubMed] [Google Scholar]
- 56.Kimmel M., Kuhlmann U., Alscher D.M. Pacemaker infection with propionibacterium and a nephritic sediment. Clin. Nephrol. 2008;69:127–129. doi: 10.5414/CNP69127. [DOI] [PubMed] [Google Scholar]
- 57.Hashimoto M., Nogaki F., Oida E., Tanaka M., Ito-Ihara T., Nomura K., Liu N., Muso E., Fukatsu A., Kita T., et al. Glomerulonephritis induced by methicillin-resistant Staphylococcus aureus infection that progressed during puerperal period. Clin. Exp. Nephrol. 2007;11:92–96. doi: 10.1007/s10157-006-0444-5. [DOI] [PubMed] [Google Scholar]
- 58.Hoshino C., Satoh N., Sugawara S., Kuriyama C., Kikuchi A., Ohta M. Community-Acquired Staphylococcus aureus Pneumonia Accompanied by Rapidly Progressive Glomerulonephritis and Hemophagocytic Syndrome. Intern. Med. 2007;46:1047–1053. doi: 10.2169/internalmedicine.46.6378. [DOI] [PubMed] [Google Scholar]
- 59.Long J.A., Cook W.J. IgA Deposits and Acute Glomerulonephritis in a Patient With Staphylococcal Infection. Am. J. Kidney Dis. 2006;48:851–855. doi: 10.1053/j.ajkd.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 60.Kitamura T., Nakase H., Iizuka H. Henoch-Schonlein purpura after postoperative Staphylococcus aureus infection with hepatic IgA nephropathy. J. Nephrol. 2006;19:687–690. [PubMed] [Google Scholar]
- 61.Ohara S., Kawasaki Y., Takano K., Isome M., Nozawa R., Suzuki H., Hosoya M. Glomerulonephritis associated with chronic infection from long-term central venous catheterization. Pediatr. Nephrol. 2006;21:427–429. doi: 10.1007/s00467-005-2124-1. [DOI] [PubMed] [Google Scholar]
- 62.Iyoda M., Hato T., Matsumoto K., Ito J., Ajiro Y., Kuroki A., Shibata T., Kitazawa K., Sugisaki T. Rapidly progressive glomerulonephritis in a patient with Chlamydia pneumoniae infection: A possibility of superantigenic mechanism of its pathogenesis. Clin. Nephrol. 2006;65:48–52. doi: 10.5414/CNP65048. [DOI] [PubMed] [Google Scholar]
- 63.Manzoor K., Khan S., Ahmed E., Akhter F., Mubarak M., Naqvi S.A.A., Rizvi A.H. Crescentic glomerulonephritis associated with bacterial endocarditis—Antibiotics alone may be sufficient. A case report. J. Pak. Med. Assoc. 2005;55:352–354. [PubMed] [Google Scholar]
- 64.Cheema S.R., Arif F., Charney D., Meisels I.S. IgA-dominant glomerulonephritis associated with hepatitis A. Clin. Nephrol. 2004;62:138–143. doi: 10.5414/CNP62138. [DOI] [PubMed] [Google Scholar]
- 65.Handa T., Ono T., Watanabe H., Takeda T., Muso E., Kita T. Glomerulonephritis induced by methicillin-sensitive Staphylococcus aureus infection. Clin. Exp. Nephrol. 2003;7:247–249. doi: 10.1007/s10157-003-0240-4. [DOI] [PubMed] [Google Scholar]
- 66.Arrizabalaga P., Saurina A., Solé M., Bladé J. Henoch-Schonlein IgA glomerulonephritis complicating myeloma kidneys: Case report. Ann. Hematol. 2003;82:526–528. doi: 10.1007/s00277-003-0698-x. [DOI] [PubMed] [Google Scholar]
- 67.Pola E., Logroscino G., De Santis V., Canducci F., Delcogliano A., Gasbarrini A. Onset of Berger disease after Staphylococcus aureus infection: Septic arthritis after anterior cruciate ligament reconstruction. Arthroscopy. 2003;19:E29. doi: 10.1053/jars.2003.50118. [DOI] [PubMed] [Google Scholar]
- 68.Peel R., Sellars L., Long E.D., Bhandari S. A man with backache and renal failure. Am. J. Kidney Dis. 2003;41:e1.1–e1.3.. doi: 10.1053/ajkd.2003.50019. [DOI] [PubMed] [Google Scholar]
- 69.Kubota M., Sakata Y., Saeki N., Yamaura A., Ogawa M. A case of shunt nephritis diagnosed 17 years after ventriculoatrial shunt implantation. Clin. Neurol. Neurosurg. 2001;103:245–246. doi: 10.1016/S0303-8467(01)00155-X. [DOI] [PubMed] [Google Scholar]
- 70.Balogun R.A., Palmisano J., Kaplan A.A., Khurshid H., Yamase H., Adams N.D. Shunt nephritis from Propionibacterium acnes in a solitary kidney. Am. J. Kidney Dis. 2001;38:e18.1–e18.7. doi: 10.1053/ajkd.2001.27726. [DOI] [PubMed] [Google Scholar]
- 71.Yamashita Y., Tanase T., Terada Y., Tamura H., Akiba T., Inoue H., Ida T., Sasaki S., Marumo F., Nakamoto Y. Glomerulonephritis after methicillin-resistant Staphylococcus aureus infection resulting in end-stage renal failure. Intern. Med. 2001;40:424–427. doi: 10.2169/internalmedicine.40.424. [DOI] [PubMed] [Google Scholar]
- 72.Barnadas M.A., Gelpí C., Rocamora V., Baró E., Ballarín J., Nadal C., Bielsa A., Aróstegui J., Alomar A. Bullous pemphigoid associated with acute glomerulonephritis. Br. J. Dermatol. 1998;138:867–871. doi: 10.1046/j.1365-2133.1998.02227.x. [DOI] [PubMed] [Google Scholar]
- 73.Griffin M.D., Björnsson J., Erickson S.B. Diffuse proliferative glomerulonephritis and acute renal failure associated with acute staphylococcal osteomyelitis. J. Am. Soc. Nephrol. 1997;8:1633–1639. doi: 10.1681/ASN.V8101633. [DOI] [PubMed] [Google Scholar]
- 74.Kitazawa M., Tomosugi N., Ishii T., Hotta F., Nishizawa M., Itou T., Nakano S., Kigoshi T., Ishikawa I., Uchida K. Rapidly progressive glomerulonephritis concomitant with diabetic nephropathy. Intern. Med. 1997;36:906–911. doi: 10.2169/internalmedicine.36.906. [DOI] [PubMed] [Google Scholar]
- 75.Pulik M., Lionnet F., Genet P., Petitdidier C., Vacher B. Immune-complex glomerulonephritis associated with Staphylococcus aureus infection of a totally implantable venous device. Support Care Cancer. 1995;3:324–326. doi: 10.1007/BF00335312. [DOI] [PubMed] [Google Scholar]
- 76.Ramineni S., Bandi V.K. Clinicopathological profile and outcomes of infection-related glomerulonephritis in adults. Clin. Nephrol. 2021;95:93–98. doi: 10.5414/CN110246. [DOI] [PubMed] [Google Scholar]
- 77.Ai S., Ma G., Liu J., Bai X., Hu R., Fan X., Miao Q., Qin Y., Li X. Infective endocarditis-associated purpura and glomerulonephritis mimicking IgA vasculitis: A diagnostic pitfall. Am. J. Med. 2021;134:1539–1545. doi: 10.1016/j.amjmed.2021.06.033. [DOI] [PubMed] [Google Scholar]
- 78.Grosser D.S., Persad P., Talento R.V., Shoemaker L.R., Hunley T.E., Hidalgo G., Subtirelu M.M., Coventry S., Baliga R., Fogo A.B. IgA-dominant infection-associated glomerulonephritis in the pediatric population. Pediatr. Nephrol. 2021;37:593–600. doi: 10.1007/s00467-021-05245-y. [DOI] [PubMed] [Google Scholar]
- 79.Huang Z., Chen B., Zhou Y., Liang Y., Qiu W., Lv Y., Ding X., Zhang J., Chen C. Clinicopathological and prognostic study of IgA-dominant postinfectious glomerulonephritis. BMC Nephrol. 2021;22:248. doi: 10.1186/s12882-021-02462-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhang M., Zhou W., Liu S., Zhang L., Ni Z., Hao C. KM55 Monoclonal antibody staining in IgA-dominant infection-related glomerulonephritis. Nephron. 2021;145:225–237. doi: 10.1159/000513269. [DOI] [PubMed] [Google Scholar]
- 81.Miquelestorena-Standley E., Jaulerry C., Machet M.-C., Rabot N., Barbet C., Hummel A., Karras A., Garrouste C., Crepin T., Ducloux D., et al. Clinicopathologic features of infection-related glomerulonephritis with IgA deposits: A French Nationwide study. Diagn. Pathol. 2020;15:62. doi: 10.1186/s13000-020-00980-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kitamura M., Obata Y., Ota Y., Muta K., Yamashita H., Harada T., Mukae H., Nishino T. Significance of subepithelial deposits in patients diagnosed with IgA nephropathy. PLoS ONE. 2019;14:e0211812. doi: 10.1371/journal.pone.0211812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sakthirajan R., Dhanapriya J., Nagarajan M., Dineshkumar T., Balasubramaniyan T., Gopalakrishnan N. Crescentic infection related glomerulonephritis in adult and its outcome. Saudi J. Kidney Dis. Transplant. 2018;29:623–629. doi: 10.4103/1319-2442.235169. [DOI] [PubMed] [Google Scholar]
- 84.Handa T., Kakita H., Tateishi Y., Endo T., Suzuki H., Katayama T., Tsukamoto T., Muso E. The features in IgA-dominant infection-related glomerulonephritis distinct from IgA nephropathy: A single-center study. Clin. Exp. Nephrol. 2018;22:1116–1127. doi: 10.1007/s10157-018-1564-4. [DOI] [PubMed] [Google Scholar]
- 85.Khalighi M.A., Al-Rabadi L., Chalasani M., Smith M., Kakani S., Revelo M.P., Meehan S.M. Staphylococcal infection-related glomerulonephritis with cryoglobulinemic features. Kidney Int. Rep. 2018;3:1128–1134. doi: 10.1016/j.ekir.2018.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Hemminger J., Arole V., Ayoub I., Brodsky S.V., Nadasdy T., Satoskar A.A. Acute glomerulonephritis with large confluent IgA-dominant deposits associated with liver cirrhosis. PLoS ONE. 2018;13:e0193274. doi: 10.1371/journal.pone.0193274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ramanathan G., Abeyaratne A., Sundaram M., Fernandes D.K., Pawar B., Perry G.J., Sajiv C., Majoni S.W. Analysis of clinical presentation, pathological spectra, treatment and outcomes of biopsy-proven acute postinfectious glomerulonephritis in adult indigenous people of the Northern Territory of Australia. Nephrology. 2017;22:403–411. doi: 10.1111/nep.12797. [DOI] [PubMed] [Google Scholar]
- 88.Satoskar A.A., Suleiman S., Ayoub I., Hemminger J., Parikh S., Brodsky S.V., Bott C., Calomeni E., Nadasdy G.M., Rovin B., et al. Staphylococcus infection-associated GN–spectrum of IgA staining and prevalence of ANCA in a single-center cohort. Clin. J. Am. Soc. Nephrol. 2017;12:39–49. doi: 10.2215/CJN.05070516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Dhanapriya J., Balasubramaniyan T., Maharajan S.P., Dineshkumar T., Sakthirajan R., Gopalakrishnan N., Nagarajan M. IgA-dominant infection-related glomerulonephritis in India: A single-center experience. Indian J. Nephrol. 2017;27:435–439. doi: 10.4103/ijn.IJN_337_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Boils C.L., Nasr S.H., Walker P.D., Couser W.G., Larsen C.P. Update on endocarditis-associated glomerulonephritis. Kidney Int. 2015;87:1241–1249. doi: 10.1038/ki.2014.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Murakami C.A., Attia D., Carter-Monroe N., Lucas G.M., Estrella M.M., Fine D.M., Atta M.G. The Clinical Characteristics and Pathological Patterns of Postinfectious Glomerulonephritis in HIV-Infected Patients. PLoS ONE. 2014;9:e108398. doi: 10.1371/journal.pone.0108398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Hamouda M., Mrabet I., Dhia N.B., Aloui S., Letaif A., Frih M.A., Skhiri H., Elmay M. Acute post-infectious glomerulonephritis in adults: A single center report. Saudi J. Kidney Dis. Transplant. 2014;25:567–571. doi: 10.4103/1319-2442.132185. [DOI] [PubMed] [Google Scholar]
- 93.Cossey L.N., Messias N., Messias E., Walker P.D., Silva F.G. Defining the spectrum of immunoglobulin A–dominant/codominant glomerular deposition in diabetic nephropathy. Hum. Pathol. 2014;45:2294–2301. doi: 10.1016/j.humpath.2014.07.015. [DOI] [PubMed] [Google Scholar]
- 94.Satoskar A.A., Molenda M., Scipio P., Shim R., Zirwas M., Variath R.S., Brodsky S.V., Nadasdy G.M., Hebert L., Rovin B., et al. Henoch-Schonlein purpura-like presentation in IgA-dominant Staphylococcus infection–associated glomerulonephritis—A diagnostic pitfall. Clin. Nephrol. 2013;79:302–312. doi: 10.5414/CN107756. [DOI] [PubMed] [Google Scholar]
- 95.Koo T.Y., Kim G.H., Park M.H. Clinicopathologic features of IgA-dominant postinfectious glomerulonephritis. Korean J. Pathol. 2012;46:105–114. doi: 10.4132/KoreanJPathol.2012.46.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Worawichawong S., Girard L., Trpkov K., Gough J.C., Gregson D.B., Benediktsson H. Immunoglobulin A–dominant postinfectious glomerulonephritis: Frequent occurrence in nondiabetic patients with Staphylococcus aureus infection. Hum. Pathol. 2011;42:279–284. doi: 10.1016/j.humpath.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 97.Wen Y.K., Chen M.L. IgA-dominant postinfectious glomerulonephritis: Not peculiar to staphylococcal infection and diabetic patients. Ren. Fail. 2011;33:480–485. doi: 10.3109/0886022X.2011.573895. [DOI] [PubMed] [Google Scholar]
- 98.Nasr S.H., Fidler M.E., Valeri A.M., Cornell L.D., Sethi S., Zoller A., Stokes M.B., Markowitz G.S., D’Agati V.D. Postinfectious Glomerulonephritis in the Elderly. J. Am. Soc. Nephrol. 2011;22:187–195. doi: 10.1681/ASN.2010060611. [DOI] [PubMed] [Google Scholar]
- 99.Wen Y.K. Clinicopathological study of infection-associated glomerulonephritis in adults. Int. Urol. Nephrol. 2010;42:477–485. doi: 10.1007/s11255-009-9628-8. [DOI] [PubMed] [Google Scholar]
- 100.Wen Y.K., Chen M.L. The significance of atypical morphology in the changes of spectrum of postinfectious glomerulonephritis. Clin. Nephrol. 2010;73:173–179. doi: 10.5414/CNP73173. [DOI] [PubMed] [Google Scholar]
- 101.Wen Y.K., Chen M.L. Discrimination between postinfectious IgA-dominant glomerulonephritis and idiopathic IgA nephropathy. Ren. Fail. 2010;32:572–577. doi: 10.3109/08860221003753331. [DOI] [PubMed] [Google Scholar]
- 102.Hsieh Y.P., Wen Y.K., Chen M.L. Comparison of Typical Endocapillary and Atypical Mesangial Proliferation in Postinfectious Glomerulonephritis. Ren. Fail. 2010;32:55–61. doi: 10.3109/08860220903367494. [DOI] [PubMed] [Google Scholar]
- 103.Wen Y.K. The Spectrum of Adult Postinfectious Glomerulonephritis in the New Millennium. Ren. Fail. 2009;31:676–682. doi: 10.3109/08860220903118616. [DOI] [PubMed] [Google Scholar]
- 104.Haas M., Racusen L.C., Bagnasco S.M. IgA-dominant postinfectious glomerulonephritis: A report of 13 cases with common ultrastructural features. Hum. Pathol. 2008;39:1309–1316. doi: 10.1016/j.humpath.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 105.Zeledon J.I., McKelvey R.L., Servilla K.S., Hofinger D., Konstantinov K.N., Kellie S., Sun Y., Massie L.W., Hartshorne M.F., Tzamaloukas A.H. Glomerulonephritis causing acute renal failure during the course of bacterial infections. Histological varieties, potential pathogenetic pathways and treatment. Int. Urol. Nephrol. 2008;40:461–470. doi: 10.1007/s11255-007-9323-6. [DOI] [PubMed] [Google Scholar]
- 106.Nasr S.H., Markowitz G.S., Stokes M.B., Said S.M., Valeri A.M., D’Agati V.D. Acute postinfectious glomerulonephritis in the modern era: Experience with 86 adults and review of the literature. Medicine. 2008;87:21–32. doi: 10.1097/md.0b013e318161b0fc. [DOI] [PubMed] [Google Scholar]
- 107.Satoskar A.A., Nadasdy G., Plaza J.A., Sedmak D., Shidham G., Hebert L., Nadasdy T. Staphylococcus Infection-Associated Glomerulonephritis Mimicking IgA Nephropathy. Clin. J. Am. Soc. Nephrol. 2006;1:1179–1186. doi: 10.2215/CJN.01030306. [DOI] [PubMed] [Google Scholar]
- 108.Nasr S.H., Markowitz G.S., Whelan J.D., Albanese J.J., Rosen R.M., Fein D.A., Kim S.S., D’Agati V.D. IgA-dominant acute poststaphylococcal glomerulonephritis complicating diabetic nephropathy. Hum. Pathol. 2003;34:1235–1241. doi: 10.1016/S0046-8177(03)00424-6. [DOI] [PubMed] [Google Scholar]
- 109.Nakamura T., Ushiyama C., Suzuki Y., Osada S., Inoue T., Shoji H., Hara M., Shimada N., Koide H. Hemoperfusion with polymyxin B-immobilized fiber in septic patients with methicillin-resistant Staphylococcus aureus-associated glomerulonephritis. Nephron Clin. Pract. 2003;94:c33–c39. doi: 10.1159/000071279. [DOI] [PubMed] [Google Scholar]
- 110.Nagaba Y., Hiki Y., Aoyama T., Sano T., Matsuo T., Shimizu T., Tateno S., Sakamoto H., Kamata K., Shigematsu H., et al. Effective antibiotic treatment of methicillin-resistant Staphylococcus aureus-associated glomerulonephritis. Nephron. 2002;92:297–303. doi: 10.1159/000063309. [DOI] [PubMed] [Google Scholar]
- 111.Majumdar A., Chowdhary S., Ferreira M.A.S., Hammond L.A., Howie A.J., Lipkin G.W., Littler W.A. Renal pathological findings in infective endocarditis. Nephrol. Dial. Transplant. 2000;15:1782–1787. doi: 10.1093/ndt/15.11.1782. [DOI] [PubMed] [Google Scholar]
- 112.Deacy A.M., Gan S.K.E., Derrick J.P. Superantigen Recognition and Interactions: Functions, Mechanisms and Applications. Front. Immunol. 2021;12:731845. doi: 10.3389/fimmu.2021.731845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Murphy K., Weaver C. T-Cell Receptor Gene Rearrangement. In: Murphy K., Weaver C., editors. Janeway’s Immunobiology. 9th ed. Garland Science; New York, NY, USA: 2017. pp. 187–191. [Google Scholar]
- 114.Tuffs S.W., Haeryfar S.M.M., McCormick J.K. Manipulation of innate and adaptive immunity by Staphylococcal superantigens. Pathogens. 2018;7:53. doi: 10.3390/pathogens7020053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Sfriso P., Ghirardello A., Botsios C., Tonon M., Zen M., Basso N., Bassetto F., Doria A. Infections and autoimmunity: The multifaceted relationship. J. Leukoc. Biol. 2020;87:385–395. doi: 10.1189/jlb.0709517. [DOI] [PubMed] [Google Scholar]
- 116.Seo K.S., Park J.Y., Terman D.S., Bohach G.A. A quantitative real time PCR method to analyze T cell receptor Vbeta subgroup expansion by staphylococcal superantigens. J. Transl. Med. 2010;8:2. doi: 10.1186/1479-5876-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Abdurrahman G., Schmiedeke F., Bachert C., Broker B.M., Holtfreter S. Allergy—A new role for T cell superantigens of Staphylococcus aureus? Toxins. 2020;12:176. doi: 10.3390/toxins12030176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Hamdy A., Leonardi A. Superantigens and SARS-CoV-2. Pathogens. 2022;11:390. doi: 10.3390/pathogens11040390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Liu J., Liu Z., Zhu Y., Dong B., Cai Z., Liang Q., Wang K. T Cell Receptor Immune Repertoires Are Promptly Reconstituted After Methicillin-Resistant Staphylococcus aureus Infection. Front. Microbiol. 2019;10:2012. doi: 10.3389/fmicb.2019.02012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.DeLorenze G.N., Nelson C.L., Scott W.K., Allen A.S., Ray G.T., Tsai A.L., Quesenberry C.P., Jr., Fowler V.G., Jr. Polymorphisms in HLA class II genes are associated with susceptibility to Staphylococcus aureus infection in a white population. J. Infect. Dis. 2016;213:816–823. doi: 10.1093/infdis/jiv483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Dan J.M., Havenar-Daughton C., Kendric K., Al-Kolla R., Kaushik K., Rosales S.L., Anderson E.L., LaRock C.N., Vija-yanand P., Seumois G., et al. Recurrent group A Streptococcus tonsillitis is an immunosusceptibility disease involving antibody deficiency and aberrant TFH cells. Sci. Transl. Med. 2019;11:eaau3776. doi: 10.1126/scitranslmed.aau3776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Csernok E., Lamprecht P., Gross W.L. Clinical and immunological features of drug-induced and infection-induced proteinase 3-antineutrophil cytoplasmic antibodies and myeloperoxidase-antineutrophil cytoplasmic antibodies and vasculitis. Curr. Opin. Rheumatol. 2010;22:43–48. doi: 10.1097/BOR.0b013e3283323538. [DOI] [PubMed] [Google Scholar]
- 123.Schnabel A., Renz H., Petermann R., Csernok E., Gross W.L. T Cell Receptor Vβ Repertoire in Bronchoalveolar Lavage in Wegener’s Granulomatosis and Sarcoidosis. Int. Arch. Allergy Immunol. 1999;119:223–230. doi: 10.1159/000024198. [DOI] [PubMed] [Google Scholar]
- 124.Hirayama K., Ishizu T., Shimohata H., Miyamoto Y., Kakita T., Nagai M., Ogawa Y., Fujita S., Hirayama A., Yamagata K., et al. Analysis of T-cell receptor usage in myeloperoxidase-antineutrophil cytoplasmic antibody-associated renal vasculitis. Clin. Exp. Nephrol. 2010;14:36–42. doi: 10.1007/s10157-009-0230-2. [DOI] [PubMed] [Google Scholar]
- 125.Kessenbrock K., Krumbholz M., Schönermarck U., Back W., Gross W.L., Werb Z., Gröne H.J., Brinkmann V., Jenne D.E. Netting neutrophils in autoimmune small-vessel vasculitis. Nat. Med. 2009;15:623–625. doi: 10.1038/nm.1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Brinkmann V., Reichard U., Goosmann C., Fauler B., Uhlemann Y., Weiss D.S., Weinrauch Y., Zychlinsky A. Neutrophil extracellular traps kill bacteria. Science. 2004;303:1532–1535. doi: 10.1126/science.1092385. [DOI] [PubMed] [Google Scholar]
- 127.Schreiber A., Rousselle A., Becker J.U., von Mässenhausen A., Linkermann A., Kettritz R. Necroptosis controls NET generation and mediates complement activation, endothelial damage, and autoimmune vasculitis. Proc. Natl. Acad. Sci. USA. 2017;114:E9618–E9625. doi: 10.1073/pnas.1708247114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Huang S.U.S., O’Sullivan K.M. The Expanding Role of Extracellular Traps in Inflammation and Autoimmunity: The New Players in Casting Dark Webs. Int. J. Mol. Sci. 2022;23:3793. doi: 10.3390/ijms23073793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Brodsky S.V., Nadasdy T., Cassol C., Satoskar A. IgA Staining Patterns Differentiate Between IgA Nephropathy and IgA-Dominant Infection-Associated Glomerulonephritis. Kidney Int. Rep. 2020;5:909–911. doi: 10.1016/j.ekir.2020.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Satoskar A.A., Shapiro J.P., Jones M., Bott C., Parikh S.V., Brodsky S.V., Yu L., Nagaraja H.N., Wilkey D.W., Merchant M.L., et al. Differentiating Staphylococcus infection-associated glomerulonephritis and primary IgA nephropathy: A mass spectrometry-based exploratory study. Sci. Rep. 2020;10:17179. doi: 10.1038/s41598-020-73847-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Suzuki H., Yasutake J., Makita Y., Tanbo Y., Yamasaki K., Sofue T., Kano T., Suzuki Y. IgA nephropathy and IgA vasculitis with nephritis have a shared feature involving galactose-deficient IgA1-oriented pathogenesis. Kidney Int. 2018;93:700–705. doi: 10.1016/j.kint.2017.10.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not available.