Abstract
Experiences from clinical practice suggest that hypochlorous acid (HOCl) used as adjuvant treatment can shorten the time to clinical resolution of blepharitis, particularly in relation to the ophthalmic complications that often occur with a blepharitis diagnosis. In addition, in clinical practice, HOCl adjuvant treatment also resulted in a viable option for the management of ophthalmic disorders other than blepharitis. This case series presents and discusses real-life experiences with using an HOCl ophthalmic spray to manage eye infections, further characterizing the use of HOCl for ophthalmic applications.
Keywords: blepharitis, case series, herpes zoster, HOCl, hypochlorous acid, inflammation, ocular infections
Introduction
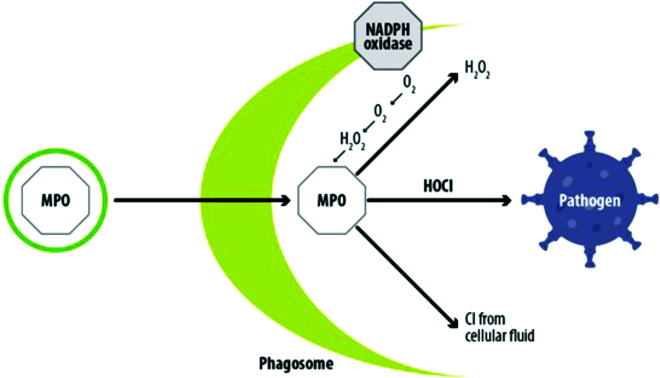
Hypochlorous acid (HOCl), a major inorganic bactericidal compound of innate immunity, is naturally produced as part of the cytotoxic myeloperoxidase system in neutrophils (Figure 1).1 In vitro, when used against various microorganisms, HOCl causes oxidation of nucleotides, inactivation of cell enzymes, disruption of cell membranes and rapid cell lysis.2 Consequently, solutions containing HOCl are highly active against all bacterial, viral and fungal human pathogens. Based on in vitro studies, the antimicrobial activity of 0.01% HOCl appears to be superior to other commonly used skin antiseptics but without cytotoxicity. Moreover, HOCl was well tolerated after continuous use and was not toxic to the human ocular surface.3–8 Consequently, these characteristics make HOCl an ideal adjuvant treatment for managing eye infections.9,10
Figure 1.
Hypochlorous acid (HOCl) production during the oxidative burst process. Neutrophils convert O2 to hydrogen peroxide (H2O2) using a mitochondrial membrane-bound enzyme (NADPH oxidase). The reaction between H2O2 and Cl− to generate HOCl is then catalysed by myeloperoxidase (MPO).
Notably, the presence of various organic compounds and inorganic ions result in rapid consumption of HOCl by oxidation reactions.11 Therefore, a major advance has been the development of a patented technology (Microcyn® technology) in which a single, free, chlorine stream is generated without a by-product of sodium hydroxide (NaOH).12 The stable HOCl formulation obtained with this technology showed a broad-spectrum antimicrobial activity and anti-inflammatory and immunomodulatory properties based on multiple laboratory analyses.13 Through the use of this technology, the development of highly stable (up to 2 years or more) and safe HOCl solutions was achieved and used for the development of commercial pharmaceutical formulations. In clinical practice, thanks to this innovative technology, an electrolyzed ophthalmic spray based on pure, stable, pH-neutral HOCl (Ocudox™, marketed in Italy by Alfa Intes; hereafter termed HOCl ophthalmic spray) can be used as an antiseptic with high disinfecting power. The HOCl ophthalmic spray is a medical device based on a 0.01% HOCl solution, the lowest pure HOCl concentration approved for the ocular surface.14 Use of the HOCl ophthalmic spray is indicated as an adjuvant in treating blepharitis and for cleansing the periocular area in the days before or after ocular surgery.15,16 Blepharitis is a common chronic ocular surface disease that involves 37–47% of patients referring to ophthalmologists and optometrists, causing significant discomfort and symptoms that include redness, itching, burning, foreign body sensations and blurred vision.17,18 Although bacteria may or may not initiate blepharitis, the oily and inflamed eyelid margins of patients with blepharitis are frequently colonized by bacteria. The main treatments for blepharitis are topical and/or systemic antibiotic therapies for bacterial aetiologies combined with topical steroids.17 However, many individuals with blepharitis require long-term therapy as blepharitis is chronic, and relief of symptoms may be temporary.
In November 2021, a group of Italian ophthalmologists participated in an online advisory board. They discussed the potential of HOCl for treating eye infections. Some experiences from clinical practice emerged during the discussion and suggested that adjuvant treatment with the HOCl ophthalmic spray resulted in a shortening of the time to clinical resolution of blepharitis, particularly in relation to the ophthalmic complications that often come with blepharitis diagnosis, according to the literature.17 In addition, in clinical practice, adjuvant treatment with the HOCl ophthalmic spray resulted in a viable option for managing ophthalmic disorders other than blepharitis. In the following paragraphs, some real-life experiences with the use of the HOCl ophthalmic spray are presented and discussed to further characterize the use of HOCl for ophthalmic applications.
Patients and methods
In the clinical experience of authors, clinical cases related to patients with ocular infections, in which the adjuvant treatment with the HOCl ophthalmic spray was prescribed in addition to the traditional therapies, were retrospectively reviewed and described. Inclusion criteria were age ≥18 years and an indication to treatment with the HOCl ophthalmic spray based on the physician’s routine clinical practice. Ocular complications are reported on a patient-by-patient basis. Due to the retrospective description of this case series, treatment regimens and patient education were not standardized. The study was conducted in accordance with the ethical principles of the revised version of the Declaration of Helsinki (52nd WMA General Assembly, Edinburgh, Scotland, October 2000). All patients had provided written informed consent to the treatment and publication of clinical data and any accompanying image. The HOCl ophthalmic spray was administered according to doses and modalities defined in the Summary of Product Characteristics.
Ethics approval
The retrospective review of patient data did not require ethical approval in accordance with local/national guidelines.
Consent for publication
Participants signed an informed consent form for publication of the details of the medical case and any accompanying images.
Case series
Adjuvant treatment with HOCl ophthalmic spray for the management of blepharitis complications
A total of 10 clinical cases related to patients with blepharitis and concomitant ophthalmic complications were selected. All patients were treated with the HOCl ophthalmic spray between November 2021 and January 2022. The characteristics of patients are summarized in Table 1.
Table 1.
Patient characteristics.
| Patient characteristics | n (%) |
|---|---|
|
| |
| Men | 6 (60) |
|
| |
| Age (years), mean (SD) | 59 (15) |
|
| |
| Systemic diseases: | |
| • Diabetes | • 3 (30) |
| • Hypertension | • 5 (50) |
| • Heart or lung disease | • 1 (10) |
| • Atopic dermatitis | • 1 (10) |
| • Immune system disorders | • 0 (0) |
| • None | • 2 (20) |
|
| |
| Ophthalmic disordersa: | |
| • Meibomitis/MGD | • 2 (20) |
| • Glaucoma | • 1 (10) |
| • Seasonal allergic conjunctivitis | • 1 (10) |
| • Chalazion | • 2 (20) |
| • Rosacea | • 1 (10) |
| • Blepharoconjunctivitis | • 2 (20) |
| • Ectropion | • 1 (10) |
Other than blepharitis.
MGD, Meibomian gland dysfunction; SD, standard deviation.
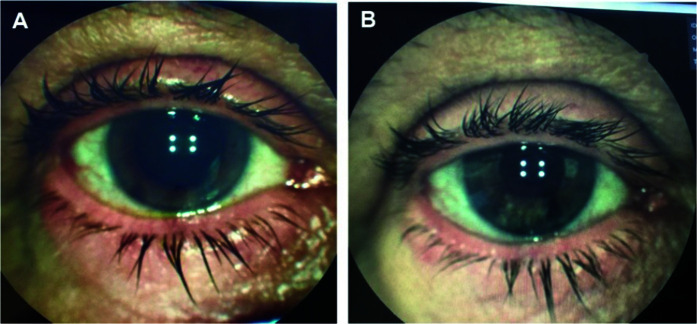
In all patients, the resolution of blepharitis was observed following adjuvant treatment with the HOCl ophthalmic spray. The mean treatment time was 20 days (standard deviation (SD) 10 days); patients received a mean of two applications (SD 1) per day of the HOCl ophthalmic spray. In all patients included, the use of antibiotics (eight were topical antibiotics, two were systemic antibiotics) combined with adjuvant treatment with the HOCl ophthalmic spray allowed a rapid improvement of the concomitant conditions associated with blepharitis. In particular, a 78-year-old patient treated with low-dose oral tetracycline for more than 1 month to treat blepharitis associated with meibomian gland dysfunction resolved his condition 7 days after the addition of the HOCl ophthalmic spray treatment, which allowed the patient to undergo cataract surgery (Figure 2).
Figure 2.
Patient with chronic blepharitis complicated by dysfunction of the meibomian glands. (A) Eyelid erythema, conjunctival hyperaemia and signs of dysfunction of the meibomian glands. (B) Reduction of erythema and dysfunction of the meibomian glands after 7 days of treatment with the HOCl ophthalmic spray in addition to oral tetracycline.
A similar result was obtained in another patient suffering from chronic blepharitis complicated by conjunctival hyperaemia and meibomitis. This patient underwent a combined corticosteroid and antibiotic topical therapy for 14 days with the adjunction of the HOCl ophthalmic spray twice a day. After 7 days of treatment, the patient reported symptom relief, and the conjunctival hyperaemia and meibomitis appeared to improve significantly (Figure 3).
Figure 3.
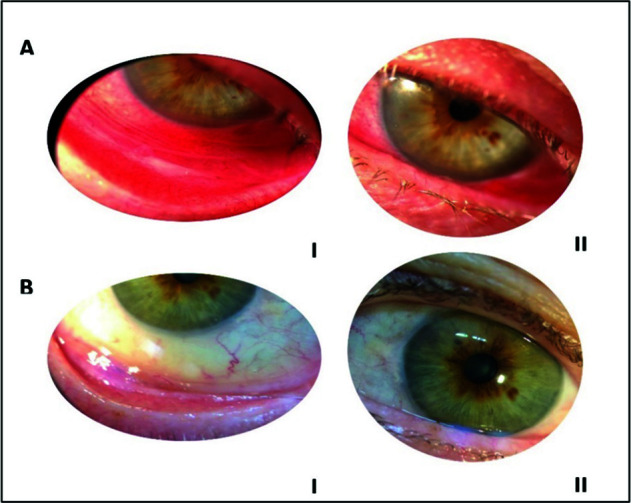
Patient with chronic blepharitis complicated by conjunctival hyperaemia and dysfunction of the meibomian glands. (A) (I and II) Eyelid erythema, conjunctival hyperaemia and signs of dysfunction of the meibomian glands. (B) (I and II) Reduction of erythema and dysfunction of the meibomian glands after 7 days of treatment with the HOCl ophthalmic spray in addition to combined corticosteroid and antibiotic topical therapy.
A 55-year-old patient suffering from chronic rosacea-associated blepharitis in treatment with oral tetracycline was reported to have suspended tetracycline treatment due to intolerance problems. The patient continued treatment with the HOCl ophthalmic spray, which led to the clinical resolution of rosacea-associated blepharitis within 15 days. In this case, the HOCl ophthalmic spray proved viable without following an oral antibiotic therapy (Figure 4).
Figure 4.
Patient with chronic rosacea-associated blepharitis. (A) Hyperaemic eyelid rim and eyelid skin. (B) Reduction of the hyperaemia of the eyelid rim and of the eyelid skin after 15 days of treatment with the sole HOCl ophthalmic spray.
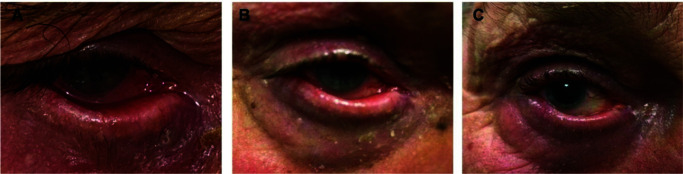
A 78-year-old patient presented with inflamed eyelids with marked hyperaemia associated with ulceration and crustaceous conglutination of the eyelashes, epiphora and ectropion (Figure 5A). Other associated symptoms were burning, warmth and tearing. A diagnosis of severe blepharitis associated with catarrhal conjunctivitis was made, and the patient was prescribed a topical antibiotic and corticosteroid therapy with the adjunction of the HOCl ophthalmic spray three times a day. After 2 weeks, the patient showed a moderate improvement in symptoms and signs (Figure 5B). At the last visit, conducted after 40 days of the combined treatment, epithelial suffering, eyelid inflammation and catarrhal conjunctivitis were resolved, ulcerations were absent, and subjective symptoms were drastically improved, with a decreased sensation of a foreign object associated with a reduction in burning and tearing (Figure 5C).
Figure 5.
Patient with severe blepharitis associated with catarrhal conjunctivitis and ectropion. (A) Inflamed eyelids with marked hyperaemia, ulceration and crustaceous conglutination of the eyelashes, epiphora and ectropion. (B) Moderate improvement in symptoms and signs after 2 weeks of topic antibiotic and corticosteroid treatment associated with HOCl ophthalmic spray administration. (C) Great reduction of epithelial suffering and eyelid inflammation after 40 days of combined treatment.
All considered patients reported an improvement in subjective symptomatology in the first days of using the HOCl ophthalmic spray. The main sensations reported were decreased foreign body sensation and reduced burning and tearing. The use of the HOCl ophthalmic spray has been well tolerated by all patients. No adverse events were reported following treatment, and treatment compliance was high.
HOCl ophthalmic spray in combination with antiviral therapy for the management of herpes zoster infection
Two clinical cases of patients affected by herpes zoster and treated with the ophthalmic spray were reported. Both were men with no other concomitant ophthalmic disorders.
The first was a 67-year-old patient who attended with oedema and erythema across the right half-face; the eyelid of the right eye was completely closed because of palpebral oedema (Figure 6A). A clinical diagnosis of hypertensive herpes uveitis caused by herpes zoster was made. The patient was prescribed systemic antiviral therapy for 1 week, but he suspended the therapy after 3 days with no signs of clinical improvement. On the second visit, the patient presented scabs and pustules hitting the whole right side of the face, accompanied by a red, swollen and painful right eye (Figure 6B). The patient was then prescribed a topical antiviral (ophthalmic ointment) in addition to the systemic antiviral, along with topical dexamethasone, tropicamide and dorzolamide for the treatment of uveitis. The use of the HOCl ophthalmic spray twice a day was also recommended. The patient was examined after 3 days. In this short amount of time, the scabs and pustules on the face were completely resolved. The hypertensive herpetic uveitis was in resolution (Figure 6C); the patient was instructed to continue antiviral therapy. HOCl ophthalmic spray solution was well tolerated and no adverse events were reported.
Figure 6.
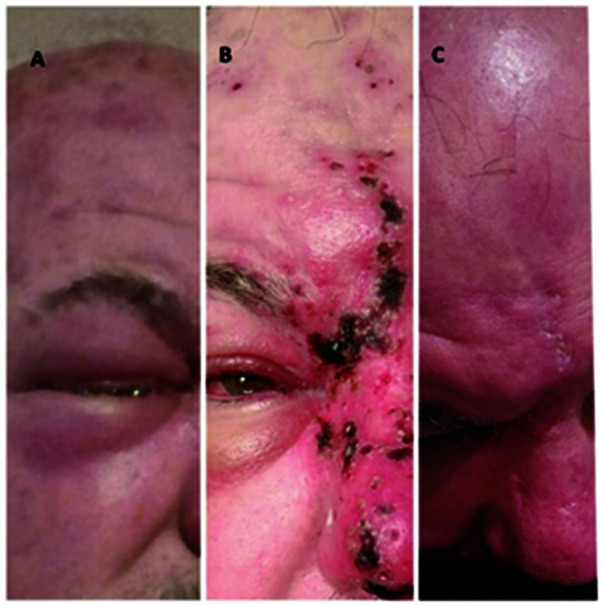
Patient with hypertensive herpes uveitis caused by herpes zoster. (A) Oedema and erythema across the right half-face, eyelid of the right eye completely closed. (B) Scabs and pustules on the whole right side of the face; red, swollen and painful right eye. Hutchinson’s sign due to nasociliary nerve involvement. (C) Absence of scabs and pustules on the face, hypertensive herpetic uveitis in resolution after 3 days of treatment with systemic antiviral, topical dexamethasone, tropicamide and dorzolamide, and HOCl ophthalmic spray administration.
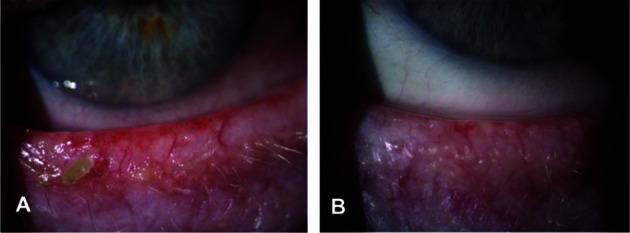
An 83-year-old patient suffering from diabetes and hypertension attended with a rash of the upper eyelid and the skin of the nose, forehead, and scalp in the left half-face, accompanied by pain in these areas. No concomitant eye diseases were found. Herpes zoster infection of the first left trigeminal branch was diagnosed. The patient was prescribed a systemic antiviral for 10 days and application of the HOCl ophthalmic spray on the face, eyelids and eye surface four times a day. In the subsequent control, performed after 3 days, a reduction of the vesicular eruption of the superior eyelid, a reduction of the superior palpebral oedema, and a reduction of the vesicular eruption along the course of the first left trigeminal branch (nose skin, forehead and left half-face) were reported. After 10 days of therapy, rare vesicles and some crusts were found along the course of the first left trigeminal branch and the systemic antiviral was suspended (Figure 7). The patient continued treatment with the HOCl ophthalmic spray for 1 month up to the resolution of the clinical picture. Treatment with the HOCl ophthalmic spray was well tolerated. The HOCl ophthalmic spray was applied with an open eye, and there were no corneal lesions or signs of toxicity to the eye surface. The patient also appreciated the ease of application of the HOCl ophthalmic spray on painful scabs.
Figure 7.
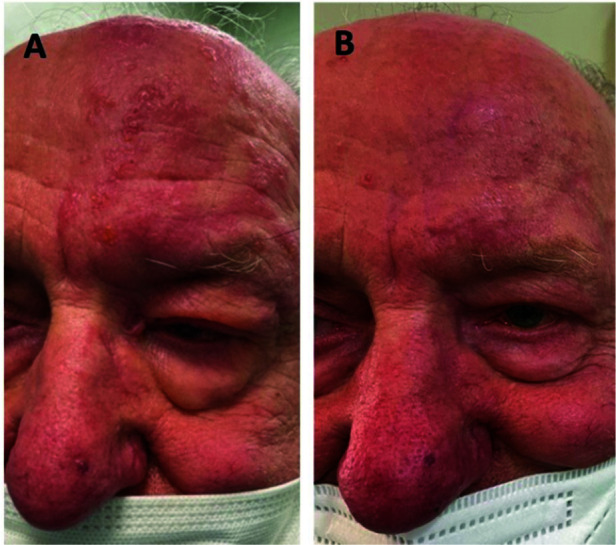
Patient with Herpes zoster infection of the first left trigeminal branch. (A) Erythematous and vesicular eruption on the skin of the left half face and along the course of the first trigeminal branch, also involving the upper eyelid of the left eye. (B) Reduction of the vesicular eruption along the course of the first trigeminal branch and on the left upper eyelid after 10 days of antiviral therapy and HOCl ophthalmic spray administration; a slight skin hyperaemia remains.
Discussion
Blepharitis is a quite common ocular condition in older patients.17 This condition is often associated with concomitant ophthalmic complications, potentially exacerbating each other and making the treatment more challenging in terms of duration. Previous data report that eyelid complications may last for many months.19 The clinical cases presented in this paper suggest that adjuvant treatment with the HOCl ophthalmic spray was useful in reducing antibiotic and corticosteroids treatment times, also in the case of severe conditions. This adjuvant activity is sustained by the anti-inflammatory properties of the stable HOCl formulation used in the ophthalmic spray, which allows the reduction of infections along with an improvement of itch, pain, and scarring and counteracts harmful inflammatory responses.13 The ophthalmic spray is indicated for periocular use, but even in case of contact with the ocular surface, it was safe and highly tolerable, as previously observed.8,20 In addition, the possibility of prolonging treatment with the HOCl ophthalmic spray may be useful for preventing the risk of recurrence as in the case of patients suffering from chalazion. For instance, often, blepharitis that is not well treated can represent a source of contamination and risk of endophthalmitis following cataract surgery in elderly patients.21 Prophylaxis with the ophthalmic spray can represent an effective and safe solution for patient candidates for this surgery who suffer from recurrent/chronic blepharitis. Of note, in patients with blepharitis, it has been shown that 0.01% pure HOCl reduced the bacterial load without altering the diversity of bacterial species remaining on the skin under the lower eyelid.16 Eyelid cleaning with HOCl did not affect the biodiversity in the meibomian gland secretions of patients with internal hordeolum.22
Herpes zoster (shingles) is a self-limiting condition caused by the reactivation of the varicella-zoster virus (VZV). The risk of VZV increases with advancing age, from 0.86 per 1000 person-years in individuals aged <19 years to 12.78 per 1000 person-years amongst those aged >80 years.23 When VZV reactivation occurs in the cranial nerve (e.g. trigeminal nerve), herpes zoster ophthalmicus develops. Symptoms related to herpes zoster ophthalmicus tend to resolve over 10–15 days after antiviral therapy.24 Reported clinical experiences suggested an advantage in combining antiviral therapy with the HOCl ophthalmic spray in terms of symptom reduction and treatment times. Indeed, adjuvant HOCl treatment showed a reduced resolution time of infection compared to antiviral therapy alone and prevented bacterial overinfection of skin lesions. This feature characterizes the clinical picture of infection with herpes zoster.
The use of 0.01% HOCl presents some advantages over other antiseptic products to manage eye infections. HOCl 0.01% had an immediate microbicidal effect on all organisms evaluated compared with commonly used highly concentrated skin antiseptics (isopropyl alcohol 70%, povidone iodine 5%, chlorhexidine gluconate 4%).5,14 This feature allows its use even in particularly sensitive and inflamed areas. In addition, the HOCl ophthalmic spray formulation was easy and comfortable to handle, thus promoting continuity of treatment as suggested by the presented clinical cases and previous literature evidence.4
Conclusion
The literature evidence, along with real-life clinical experience, supports the use of HOCl as an adjuvant treatment for the management of eye infections and for cleansing the periocular area before and after ocular surgery. In particular, in clinical practice, adjuvant treatment with the HOCl ophthalmic spray shortened the time to clinical resolution of blepharitis and other ophthalmic disorders, resulting in an effective and safe option for the management of ophthalmic infections.
Acknowledgements
Editorial and graphical assistance were provided by Simonetta Papa, PhD, Massimiliano Pianta and Aashni Shah (Polistudium SRL, Milan, Italy). This assistance was supported by Alfa Intes.
Footnotes
Contributions: All authors contributed to the definition and contextualization of paper contents, critically edited the manuscript, and approved its final version for submission. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosure and potential conflicts of interest: None of the authors declared conflict of interests. The International Committee of Medical Journal Editors (ICMJE) Potential Conflicts of Interests form for the authors is available for download at: https://www.drugsincontext.com/wp-content/uploads/2022/05/dic.2022-3-10-COI.pdf
Funding declaration: This project was conducted with the non-conditioning assistance of Alfa Intes.
Correct attribution: Copyright © 2022 Bertone C, Mollicone A, Russo S, Sasso P, Fasciani R, Riccardi C, Lizzano M, the ALI working group. https://doi.org/10.7573/dic.2022-3-10. Published by Drugs in Context under Creative Commons License Deed CC BY NC ND 4.0.
Article URL: https://www.drugsincontext.com/the-role-of-hypochlorous-acid-in-the-management-of-eye-infections-a-case-series
Provenance: Submitted; externally peer reviewed.
Drugs in Context is published by BioExcel Publishing Ltd. Registered office: Plaza Building, Lee High Road, London, England, SE13 5PT.
BioExcel Publishing Limited is registered in England Number 10038393. VAT GB 252 7720 07.
For all manuscript and submissions enquiries, contact the Editorial office editorial@drugsincontext.com
For all permissions, rights and reprints, contact David Hughes david.hughes@bioexcelpublishing.com
References
- 1.Wang L, Bassiri M, Najafi R, et al. Hypochlorous acid as a potential wound care agent: part I. Stabilized hypochlorous acid: a component of the inorganic armamentarium of innate immunity. J Burns Wounds. 2007;6:e5. [PMC free article] [PubMed] [Google Scholar]
- 2.Sakarya S, Gunay N, Karakulak M, et al. Hypochlorous acid: an ideal wound care agent with powerful microbicidal, antibiofilm, and wound healing potency. Wounds. 2014;26(12):342–350. [PubMed] [Google Scholar]
- 3.Li Z, Wang H, Liang M, et al. Hypochlorous acid can be the novel option for the meibomian gland dysfunction dry eye through ultrasonic atomization. Dis Markers. 2022;2022:8631038. doi: 10.1155/2022/8631038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fam A, Finger PT, Tomar AS, Garg G, Chin KJ. Hypochlorous acid antiseptic washout improves patient comfort after intravitreal injection: a patient reported outcomes study. Indian J Ophthalmol. 2020;68(11):2439–2444. doi: 10.4103/ijo.IJO_2001_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Anagnostopoulos AG, Rong A, Miller D, et al. 0.01% hypochlorous acid as an alternative skin antiseptic: an in vitro comparison. Dermatol Surg. 2018;44(12):1489–1493. doi: 10.1097/DSS.0000000000001594. [DOI] [PubMed] [Google Scholar]
- 6.Klocek MS, Mammen A, Dhaliwal D, Kowalski RP. Time-kill comparison of povidone iodine to hypochlorous acid against endophthalmitis isolates of Staphylococci. Invest Ophthalmol Vis Sci. 2016;57(12):5861. [Google Scholar]
- 7.Armstrong DG, Bohn G, Glat P, et al. Expert recommendations for the use of hypochlorous solution: science and clinical application. Ostomy Wound Manage. 2015;61(5):S2–S19. [PubMed] [Google Scholar]
- 8.Finger PT, Fam A, Tomar AS, Garg G, Chin KJ. COVID-19 prophylaxis in ophthalmology. Indian J Ophthalmol. 2020;68(10):2062–2063. doi: 10.4103/ijo.IJO_2459_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harsch AG, Stout N, Lighthizer N. Beat the blepharitis blues. Rev Cornea Contact Lens. 2016;153(7):12–15. [Google Scholar]
- 10.Kern JR, Fahmy AH. Dry eye patients report improvement in symptoms with hypochlorous acid use over 30 days. Invest Ophthalmol Vis Sci. 2019;60(9):6740. [Google Scholar]
- 11.Ishihara M, Murakami K, Fukuda K, et al. Stability of weakly acidic hypochlorous acid solution with microbicidal activity. Biocontrol Sci. 2017;22(4):223–227. doi: 10.4265/bio.22.223. [DOI] [PubMed] [Google Scholar]
- 12.Landa-Solis C, González-Espinosa D, Guzmán-Soriano B, et al. Microcyn: a novel super-oxidized water with neutral pH and disinfectant activity. J Hosp Infect. 2005;61(4):291–299. doi: 10.1016/j.jhin.2005.04.021. [DOI] [PubMed] [Google Scholar]
- 13.Del Rosso JQ, Bhatia N. Status report on topical hypochlorous acid: clinical relevance of specific formulations, potential modes of action, and study outcomes. J Clin Aesthet Dermatol. 2018;11(11):36–39. [PMC free article] [PubMed] [Google Scholar]
- 14.Tran AQ, Topilow N, Rong A, et al. Comparison of skin antiseptic agents and the role of 0.01% hypochlorous acid. Aesthet Surg J. 2021;41(10):1170–1175. doi: 10.1093/asj/sjaa322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ocudox™ Summary of Product Characteristics. https://www.alfaintes.it/it/prodotto/18 .
- 16.Stroman DW, Mintun K, Epstein AB, et al. Reduction in bacterial load using hypochlorous acid hygiene solution on ocular skin. Clin Ophthalmol. 2017;11:707–714. doi: 10.2147/OPTH.S132851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Onghanseng N, Ng SM, Halim MS, et al. Oral antibiotics for chronic blepharitis. Cochrane Database Syst Rev. 2021;6(6):CD013697. doi: 10.1002/14651858.CD013697.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Romanowski EG, Stella NA, Yates KA, et al. In vitro evaluation of a hypochlorous acid hygiene solution on established biofilms. Eye Contact Lens. 2018;44(Suppl 2):S187–S191. doi: 10.1097/ICL.0000000000000456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sklar BA, Gervasio KA, Leng S, et al. Management and outcomes of proteasome inhibitor associated chalazia and blepharitis: a case series. BMC Ophthalmol. 2019;19(1):110. doi: 10.1186/s12886-019-1118-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Romano GL, Lazzara F, Conti F, et al. Ocular safety profile of a new formulation based on hypochlorous acid in rabbit eye. ARVO poster. 2021. https://iovs.arvojournals.org/article.aspx?articleid=2774442 .
- 21.Schwartz SG, Flynn HW, Jr, Das T, et al. Ocular infection: endophthalmitis. Dev Ophthalmol. 2016;55:176–188. doi: 10.1159/000431195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang S, Wu BC, Cheng Z, et al. The microbiome of meibomian gland secretions from patients with internal hordeolum treated with hypochlorous acid eyelid wipes. Dis Markers. 2022;2022:7550090. doi: 10.1155/2022/7550090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bakacs T. Healing of severe herpes zoster ophthalmicus within a few days: an autobiographical case report. Cureus. 2021;13(12):e20303. doi: 10.7759/cureus.20303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lee CY, Tsai HC, Lee SS, Chen YS. Orbital apex syndrome: an unusual complication of herpes zoster ophthalmicus. BMC Infect Dis. 2015;15:33. doi: 10.1186/s12879-015-0760-z. [DOI] [PMC free article] [PubMed] [Google Scholar]