Abstract
Introduction: There are studies that evaluate the association between chronic obstructive pulmonary disease (COPD) and heart failure (HF) but there is little evidence regarding the prognosis of this comorbidity in older patients admitted for acute HF. In addition, little attention has been given to the extracardiac and extrapulmonary symptoms presented by patients with HF and COPD in more advanced stages. The aim of this study was to evaluate the prognostic impact of COPD on mortality in elderly patients with acute and advanced HF and the clinical manifestations and management from a palliative point of view. Methods: The EPICTER study (“Epidemiological survey of advanced heart failure”) is a cross-sectional, multicenter project that consecutively collected patients admitted for HF in 74 Spanish hospitals. Demographic, clinical, treatment, organ-dependent terminal criteria (NYHA III-IV, LVEF <20%, intractable angina, HF despite optimal treatment), and general terminal criteria (estimated survival <6 months, patient/family acceptance of palliative approach, and one of the following: evidence of HF progression, multiple Emergency Room visits or admissions in the last six months, 10% weight loss in the last six months, and functional impairment) were collected. Terminal HF was considered if the patient met at least one organ-dependent criterion and all the general criteria. Both groups (HF with COPD and without COPD) were compared. A Kaplan–Meier survival analysis was performed to evaluate the presence of COPD on the vital prognosis of patients with HF. Results: A total of 3100 patients were included of which 812 had COPD. In the COPD group, dyspnea and anxiety were more frequently observed (86.2% vs. 75.3%, p = 0.001 and 35.4% vs. 31.2%, p = 0.043, respectively). In patients with a history of COPD, presentation of HF was in the form of acute pulmonary edema (21% vs. 14.4% in patients without COPD, p = 0.0001). Patients with COPD more frequently suffered from advanced HF (28.9% vs. 19.4%; p < 0.001). Consultation with the hospital palliative care service during admission was more frequent when patients with HF presented with associated COPD (94% vs. 6.8%; p = 0.036). In-hospital and six-month follow-up mortality was 36.5% in patients with COPD vs. 30.7% in patients without COPD, p = 0.005. The mean number of hospital admissions during follow-up was higher in patients with HF and COPD than in those with isolated HF (0.63 ± 0.98 vs. 0.51 ± 0.84; p < 0.002). Survival analysis showed that patients with a history of COPD had fewer survival days during follow-up than those without COPD (log Rank chi-squared 4.895 and p = 0.027). Conclusions: patients with HF and COPD had more severe symptoms (dyspnea and anxiety) and also a worse prognosis than patients without COPD. However, the prognosis of patients admitted to our setting is poor and many patients with HF and COPD may not receive the assessment and palliative care support they need. Palliative care is necessary in chronic non-oncologic diseases, especially in multipathologic and symptom-intensive patients. This is a clinical care aspect to be improved and evaluated in future research studies.
Keywords: hronic obstructive pulmonary disease, advance heart failure, palliative care
1. Introduction
The incidence and prevalence of heart failure (HF) and chronic obstructive pulmonary disease (COPD) is continuously increasing. HF prevalence has been reported to be higher in patients with COPD compared to the general population (10–30% versus 1–2%) [1,2]. HF is a common condition in patients hospitalized for exacerbation of COPD: in these patients, 20% have been described to have pre-existing HF while 40% have new HF [3]. Patients presenting both comorbid conditions (HF and COPD) are likely to be smokers and older with an important burden of comorbid conditions compared to patients with HF without COPD [1,3,4].
Clinically, the association of these two conditions is particularly challenging as they can present with similar clinical manifestations, which can significantly delay the diagnosis of HF [5,6]. In addition, HF remains underdiagnosed and undertreated in patients with COPD, with a one year mortality rate reaching 50% [3,7]. Thus, COPD is associated with increased cardiovascular morbidity and mortality independent of the left ventricular ejection fraction (LVEF) [8].
HF with preserved or reduced LVEF should not be treated differently if COPD coexists (1) and HF guidelines should be followed. However, beta-blockers are underprescribed in these patients due to concerns regarding their side effects on pulmonary function [1,9]. In a large retrospective analysis from an HF registry, beta-blocker selectivity was not associated with a difference in outcomes for patients with HF with COPD as compared with those with HF without COPD [10]. In addition, benefits from beta-blockers outweigh potential risks even in patients with severe COPD [1,10]. Regarding the impact of treatment with sacubitril/valsartan on pulmonary function, no data are available.
There are studies that evaluate the association between COPD and HF but there is little evidence regarding the prognosis of this comorbidity in older patients admitted for acute HF. In addition, little attention has been given to the extracardiac and extrapulmonary symptoms presented by patients with HF and COPD in more advanced stages.
The aim of this study was to evaluate the prognostic association of COPD on mortality in elderly patients with acute HF and to evaluate the clinical manifestations and management from a palliative point of view.
2. Material and Methods
2.1. Study Population
The EPICTER study (“Epidemiological survey of advanced heart failure”) is a cross-sectional and prospective, multicenter project that consecutively collected data on patients admitted for HF in 74 Spanish public or private hospitals, regardless of hospital size. Patients were recruited in two periods (summer and winter). To avoid bias, hospitals began collecting data on the same day (1 June and 30 November 2016) in which all patients admitted to Cardiology or Internal Medicine departments, Intensive Care Units, or any other service were included. Researchers at each center checked patients who met the inclusion criteria daily and each hospital continued to recruit patients on subsequent days until the required number was reached. The minimum number of patients to be included for each hospital was pre-determined according to the number of hospital beds. Inclusion criteria were (1) age older than 18 years, (2) admission to the hospital room before 8:00 o’clock on the day of data collection, (3) HF as the main cause of admission: acute HF, acute pulmonary edema, acute coronary syndrome Killip III-IV, or cardiogenic shock. Exclusion criteria were (1) patients attended in the Emergency Department, but not yet admitted, and (2) patients who did not sign the informed consent. All patients received the usual treatments and medical care and were classified into two groups according to whether or not they had no COPD.
2.2. Study Variables
Demographic, clinical, treatment, organ-dependent terminal criteria (NYHA III-IV, LVEF < 20%, intractable angina, HF despite optimal treatment), and general terminal criteria (estimated survival <6 months, patient/family acceptance of palliative approach, and one of these: evidence of HF progression, multiple ER visits or admissions in the last 6 months, 10% weight loss in the last 6 months, functional impairment) were collected. Terminal HF was considered if the patient met at least one organ-dependent criterion and all the general criteria. Vital status of patients at 6 months follow-up was verified by the researchers of each hospital. For this purpose, local health databases were used or relatives were contacted (Supplementary File S1).
2.3. Statistical Analysis
Continuous variables were expressed as mean (standard deviation) or median (with 25th to 75th interquartile range), and categorical variables as frequencies and percentages. Continuous variables were compared using Student’s t-test or non-parametric Kruskal–Wallis test. Categorical variables were compared using the Chi-square test.
Both groups (HF with and without COPD) were compared. A Kaplan–Meier survival analysis was performed to evaluate the impact of the presence of COPD on the vital prognosis of patients with HF. A p-value of less than 0.05 was considered statistically significant. All analyses were performed with the Statistical Package for the Social Sciences (SPSS) program (version 26.0, SPSS Inc., Chicago, IL, USA).
2.4. Ethical Aspects
The study was carried out in accordance with the Declaration of Helsinki. Ethical approval (Ethics Committee of the Hospital Virgen Macarena, Internal code 0942-N-15; 24 November 2015) was obtained before recruitment. All patients signed the informed consent at inclusion.
2.5. Results
A total of 3100 patients were included of which 812 had COPD. The mean age in the COPD group was 79.29 ± 10.2 years with a predominance of male sex (63%). Mean LVEF was 53.28% ± 15.78 and mean NT-proBNP was 8936.2 pg/mL ± 1047.51. Of the patients, 21.4% were in NYHA functional class III-IV. Patients with COPD had a more advanced NYHA functional class than patients without COPD. No significant statistical differences were observed between groups in relation to LVEF and NT-proBNP levels (Table 1).
Table 1.
Clinical characteristics of patients with HF with/without history of COPD.
| Variable | HF with COPD (n = 812) |
HF without COPD (n = 2288) |
p |
|---|---|---|---|
| Age (years) mean ± SD | 77.5 ± 10.1 | 79.4 ± 11.1 | 0.001 |
| Sex (male), N (%) | 575 (70.8%) | 955 (41.7%) | 0.001 |
| NYHA III-IV, N (%) | 233/802 (29.1%) | 486/2241 (21.7%) | 0.001 |
| LVEF, mean ± SD | 50.08 ± 16.5 | 51.26 ± 15.9 | 0.65 |
| NTpro-BNP pg/mL, mean | 7910.4 | 8550.2 | 0.4 |
| Comorbidities | |||
| Charlson comorbidity index mean ± SD | 4.49 ± 1.76 | 3.24 ± 1.8 | 0.0001 |
| Hypertension N (%) | 694/809 (85.8%) | 1936/2283 (84.8%) | 0.528 |
| Diabetes N (%) | 397/810 (49%) | 1010/2279 (44.3%) | 0.022 |
| Ischemic heart disease N (%) | 271/804 (33.7%) | 713/2257 (31.6%) | 0.271 |
| Atrial fibrillation N (%) | 470/809 (58.1%) | 1286/2281 (56.4%) | 0.409 |
| Valve disease N (%) | 176/377 (37.8%) | 1012/2194 (46.1%) | 0.001 |
| Chronic kidney disease N (%) | 410/807 (50.8%) | 1041/2270 (45.9%) | 0.017 |
| Cerebrovascular disease N (%) | 164/797 (20.6%) | 498/2269 (21.9%) | 0.453 |
| Anemia N (%) | 382/806 (47.4%) | 1118/2274 (48.7%) | 0.390 |
Legend: NYHA: New York Heart Association functional class, LVEF: left ventricular ejection fraction, COPD: chronic obstructive pulmonary disease. The diagnosis of acute HF was based on 2016 ESC clinical practice guidelines. COPD was considered if the patient presented the diagnosis of the disease according to their medical history. The diagnosis of anemia was established according to the definition of the World Health Organization (<13 g/L hemoglobin for men and <12 g/L hemoglobin for women). Chronic renal failure was defined as a persistent glomerular filtration rate below 60 mL/min/according to MDRD at least three months.
Patients with a history of COPD had a higher frequency of diabetes and chronic kidney disease at admission as well as a higher Charlson comorbidity index with statistically significant differences (4.49 ± 1.76 vs. 3.24 ± 1.8; p < 0.001) (Table 1).
In relation to the collected symptoms of advanced and terminal disease, in the COPD group, dyspnea and anxiety were more frequently observed (86.2% vs. 75.3%, p = 0.001 and 35.4% vs. 31.2%, p = 0.043, respectively). No significant statistical differences were observed between groups in relation to chest pain, nausea, insomnia, delirium, and generalized pain (Table 2). In patients with COPD, presentation in the form of acute pulmonary edema was more frequent than in patients without COPD (21% vs. 14%, p = 0.0001). Patients with COPD more frequently experience advanced HF (28.9% vs. 19.4%; p < 0.001).
Table 2.
Clinical manifestations of advanced disease evaluated among elderly acute HF patients with and without COPD.
| Variable | HF with COPD n = 528 |
HF without COPD n = 1480 |
p-Value |
|---|---|---|---|
| Dyspnea N (%) | 455/528 (86.2%) | 1114/1480 (75.3%) | 0.0001 |
| >10% Weight loss N (%) | 48/356 (13.5%) | 121/900 (11.9%) | 0.236 |
| Functional impairment N (%) | 146/379 (38.5%) | 390/715 (35.3%) | 0.265 |
| Anxiety N (%) | 187/528 (35.4%) | 462/1480 (31.2%) | 0.043 |
| Nausea N (%) | 52/528 (9.8%) | 176/1480 (11.9%) | 0.231 |
| Chest pain N (%) | 99/528 (18.8%) | 281/1478 (19%) | 0.948 |
| Generalized pain N (%) | 157/528 (29.7%) | 394/1477 (26.7%) | 0.098 |
| Delirium N (%) | 83/528 (15.7%) | 217/1480 (14.7%) | 0.570 |
| Insomnia N (%) | 197/528 (37.3%) | 507/1478 (35%) | 0.222 |
Table 3 shows the treatment received during admission in both groups of patients. Subjects with a history of COPD were more frequently treated with noninvasive mechanical ventilation (7.6 vs. 4.6; p = 0.004) and high flow oxygen (14% vs. 11.4%; p = 0.018). No statistically significant differences were found between groups in the administration of furosemide doses, use of amines, and oral and subcutaneous morphine. Consultation with the hospital palliative care service during admission was more frequent when patients with HF presented with associated COPD (49/520; 94% vs. 99/1450; 6.8%; p = 0.036).
Table 3.
Treatment received during admission in groups of heart failure patients with and without COPD.
| Variable | HF with COPD (n = 812) |
HF without COPD (n = 2288) |
p |
|---|---|---|---|
| Non-invasive mechanical ventilation n (%) | 62 (7.6%) | 105 (4.6%) | 0.004 |
| High Flow oxygen n (%) | 74/529 (14%) | 229/2014 (11.4%) | 0.018 |
| Nitroglicerine iv | 69/805(86%) | 237/2281(20.4%) | 0.222 |
| Hypertonic saline + furosemide n (%) | 15/536 (2.8%) | 34/1495 (2.3%) | 0.297 |
| Furosemide perfusion n (%) | 138/812 (17%) | 364/2288 (15.9%) | 0.770 |
| Use of amines n (%) | 50/812 (6.2%) | 110/2288 (4.8%) | 0.326 |
| Levosimendan n (%) | 11/812 (1.4%) | 23/2288 (1%) | |
| Dialysis n (%) | 6/536 (1.1%) | 17/1493 (1.1%) | 1.000 |
| Oral morphine n (%) | 151/536 (28.2%) | 379/1497 (25.3%) | 0.109 |
| Subcutaneous morphine n (%) | 74/472 (15.7%) | 223/1304 (17.1%) | 0.263 |
| Benzodiazepines n (%) | 185/535 (34.6%) | 496/1496 (33.2%) | 0.292 |
In-hospital and 6-month follow-up mortality was 36.5% (270/740) in patients with COPD vs. 30.7% (639/2080) without COPD (p = 0.005). The mean number of hospital admissions during follow-up was higher in patients with HF and COPD than in those with isolated HF (0.63 ± 0.98 vs. 0.51 ± 0.84; p < 0.002).
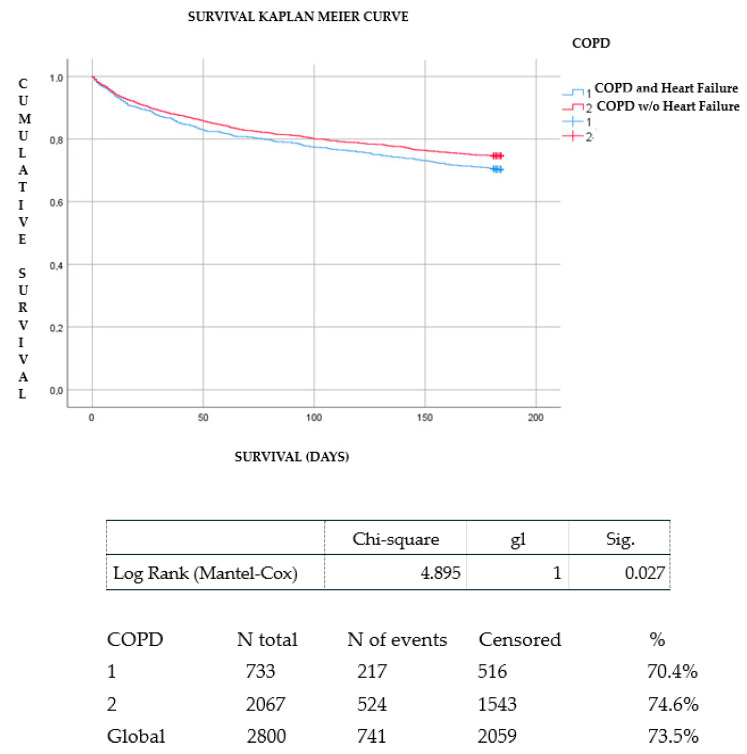
Survival analysis showed that patients with a history of COPD had fewer survival days during follow-up than those without COPD (log Rank chi-squared 4.895 and p = 0.027). (Figure 1). The causes among patients with acute HF with and without COPD are shown in Supplementary Table S1.
Figure 1.
Kaplan–Meier survival curve between HF patients with and without COPD.
3. Discussion
The results of our research demonstrate that six month mortality after hospital admission in elderly acute HF patients was higher in those subjects with a medical antecedent of COPD. This entity confers an even greater risk of dying following hospitalization for acute HF as reported in previous studies [9]. Measures of the severity of COPD (FEV1 and GOLD [Global Initiative for Chronic Obstructive Lung Disease] stage) have been shown to be independent predictors of mortality and event-free survival, respectively, in patients with COPD and concomitant HF [11]. In addition, the impact of COPD on mortality in acute HF seems to be more important over the long term [9]. In the OPTIMIZE-HF registry of patients hospitalized with acute HF there were no differences in in-hospital or 60-day mortality rates between patients with and without COPD [12]. However, in our study, we observed a high mortality rate of more than 30% at six months of follow-up, which was even higher for patients with COPD. The differences in the short-term prognosis observed in the different published studies show that our sample of patients included in the EPICTER registry with HF and COPD were in a more advanced and terminal phase of the disease [12].
The presence of COPD was more frequent in the men in our sample. This finding may be due to a higher frequency of smoking in elderly patients admitted for HF in our environment [13].
The presence of COPD was also accompanied by a greater number of comorbidities associated with HF such as diabetes and the presence of previous chronic kidney disease. These findings may be because COPD is also associated with an increased risk of diabetes, among which the use of steroids to control flare-ups may contribute to worsened glycemic control in this type of patient. It is well known that diabetes, previous smoking, and advanced age contribute to the development of chronic kidney disease [1,2,3].
Patients with HF and COPD in the EPICTER study presented more symptoms of advanced HF reporting more dyspnea, anxiety, and need for more use of high oxygen mask supply and noninvasive mechanical ventilation than patients with isolated HF. These findings may be explained by the presence of both conditions in the same patients which imparts a negative impact upon them.
It is very common that HF produces disorders in pulmonary ventilation and perfusion that aggravate COPD and, conversely, that COPD itself, through hypoxemia and/or hypercapnia, increases the risk of cardiac arrhythmias and worsens pulmonary congestion. These findings could explain why COPD patients presented more frequently in acute pulmonary edema as the HF presentation in this study. The findings of our investigation show that the palliative care team evaluated patients with HF and COPD more frequently. There was no difference in the palliative treatment received. Interestingly, although HF is generally considered as a serious condition and equivalent to malignant disease in terms of symptom burden and mortality, only a few patients receive specialist palliative care [14,15,16]. However, evidence indicates that a palliative approach in HF significantly improves patient outcomes, including symptom control and mental health, decreased hospital admissions and mortality, and reduced healthcare costs [17,18].
Interestingly, there were no differences in the use of levosimendan in both groups. Levosimendan augments the calcium sensitivity of the troponin complex subsequently improving cardiac muscle contractility [19,20]. Besides, it has also been shown to improve contractility of the diaphragm [19]. In advanced HF patients, levosimendan has showed positive effects in reducing mortality and three months hospitalization [21,22]. Regarding quality of life and symptoms improvement levosimendan showed contrasting effect among the studies on advanced HF patients [21,23].
The study has some limitations. First, we must consider that the COPD variable was established as an antecedent in the EPICTER study data collection. In this regard, we do not know if the diagnosis of COPD was based on spirometric criteria or on concomitant treatment received for COPD. Second, in-hospital mortality was not differentiated from that of patients surviving admission. Since this was an acute HF registry, only drugs for the control and treatment of acute HF were collected. We do not have specific treatments for chronic HF or COPD. We did not evaluate data regarding congestion such as the presence of pleural effusion as it has related to more cardio-respiratory complications with higher mortality [22]. Finally, not all centers had the same access to specialized palliative care. These aspects are important when interpreting our results. A strength of the study is that the large cohort is prospective and unselected, so it is representative of the real world.
4. Conclusions
Patients with HF and COPD had more severe symptoms (dyspnea and anxiety) and also a worse prognosis than patients without COPD. However, the prognosis of patients admitted to our setting is poor and many patients with HF and COPD may not receive the assessment and palliative care support they need. Palliative care is necessary in chronic non-oncologic diseases, especially in multipathologic and symptom-intensive patients. This is a clinical care aspect to be improved and evaluated in future research studies.
Acknowledgments
EPICTER Study Group: Patricia Vázquez-Rodríguez, Teresa Choucino-Fernández, Ana B. Porto-Pérez, Patricia Piñeiro-Parga, Manuel L. López-Reboiro, Cristina Pedrosa-Fraga, Roi Suárez-Gil, Juan J. González-Soler, Pablo López-aMato, Ana Latorre-Díez, Adriana Gómez-Gigirey, Lucía Ferreira-González, Mercedes Sánchez-Cembellin, María Gallego-Villalobos, Jessica P. Rugeles-Niño, Elisa E. Rodríguez-Avila, Alvaro González-Franco, Carla de la Guerra-Acebal, Angel Sebastián-Leza, Juan Monte-Armenteros, Gorka Frutos-Muñoyerro, Carolina Clemente-Sarasa, Jesús Díez-Manglano, Claudia Josa-Laorden, Isabel Torres-Courchoud, Noelia Gómez-Aguirre, Rosa Jordana-Camajuncosa, Luis E. Cajamarca-Calva, Isabel Torrente-Jiménez, Ana Serrado-Iglesias, Luis M. Ceresuela, Rosario Salas-Campos, Jordi Delás-Amat, Francesc Formiga, Ariadna Brasé-Arnau, Irene Petit-Salas, Verónica Romaní-Costa, Antonia Expósito-López, Carlos E. Sabbagh-Fajardo, Jesús Recio-Iglesias, Carmen Alemán-Llansó, Josep M. Suriñach-Caralt, Joan Carles Trullás-Vila, Arola Armengou-Arxe, Sara García-Torras, José Luis Morales-Rull, Cristina Solé-Felip, Ana Lacal-Martínez, Cristina Sánchez-Sánchez, Miguel Otero-Soler, Alberto Muela-Molinero, Margarita Carrera-Izquierdo, Patricio Arribas-Arribas, Luis Inglada-Galiana, Ángela Ruiz de Temiño de la Peña, Álvaro Silva-Vázquez, Lucía Fuentes-Pardo, María García-García, Esther Piniella-Ruiz, Bethania Pérez-Alves, Sonia Gonzalo-Pascua, Jorge Marrero-Francés, Manuel Méndez-Bailón, Francico J. Martín-Sánchez, Marta Varas-Mayoral, María Asenjo-Martínez, Miguel Yebra-Yebra, Beatriz Sánchez-Sauce, Benjamín Herreros-Ruiz, Angustias Quesada-Simón, Ivo Vives-Beltrán, Jorge Álvarez-Troncoso, Luis A. Martínez-Marín, Paloma Gil Martínez, Estrella Díaz de Mayorga, Miguel A. Moreno-Palanco, Llanos Soler-Rangel, Javier Abellán-Martínez, Ana M. Colás-Herrera, Genoveva T. López-Castellanos, Raúl Ruíz-Ortega, Evelyn Ruiz-Barraza, María L. Martín-Jiménez, Esther Montero-Hernández, José C. Arévalo-Lorido, Juana Carretero-Gómez, Patricia Calderón-Jiménez, Almudena Herrero-Domingo, Sheyla Martín-Barba, Julio C. Blázquez-Encinar, Carlos Jiménez-Guardiola, Jóse M. Cepeda-Rodrigo, Dolores Quiles-García, Sara Carrascosa-García, Pau Llacer-Iborra, María C. Moreno-García, Luis F. Díez-García, Purificación Sánchez-López, María J. Martínez-Soriano, Eva Menor, Manuel Montero-Pérez-Barquero, Manuel P. Anguita-Sánchez, María Sánchez-Moruno, María Fuentes-Espínola, José L. Zambrana-García, Esther Guisado-Espartero, Inmaculada Mejías-Real, José N. Alcalá-Pedrajas, Inmaculada Páez-Rubio, Francisco J. Carrasco-Sánchez, Catalina Díaz-Pérez, Marcos Guzmán-García, Sara Domingo-Roa, Begoña Cortés-Rodríguez, Carmen García-Redecillas, Rosario Martín-Navarro, Raúl Quirós-López, Patricia Macías-Ávila, Isabel Antequera-Martín-Portugués, María Blanco-Soto, José L. Arias-Jiménez, Oscar Aramburu-Bodas, Prado Salamanca-Bautista, Miriam Romero-Correa, José A. García-García, Francisco J. Flores-Álvarez, Reyes Aparicio-Santos, M. Dolores Nieto-Martín, Rocío García-Serrano, Carlos Jiménez-de-Juan, Jara Ternero-Vega, María Villalonga-Comas, Manuel Díaz-Cañestro, Javier Asensio-Rodríguez, Alicia Conde-Martel, Aída Gil-Díaz, Iván Marrero-Medina, Alicia Puente-Fernández, Diego Gudiño-Aguirre, Melitón F. Dávila-Ramos, Eduardo Calderón.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jcm11133709/s1, Supplementary File S1. End stage disease criteria. Table S1. Causes of death in patients with HF with and without COPD in the EPICTER registry. Table S2. Logistic regression analysis of mortality evaluating the COPD variable.
Author Contributions
Conceptualization, M.M.-B., N.L.-V., M.R.-C., C.J.-L., L.I.-G., E.M.-C., N.G.-A., C.C.-S., R.S.-C., C.G.-R., M.A.-M., J.C.T., B.C.-R., C.d.l.G.-A., A.S.I., R.A.-S., F.F., E.A., O.A.-B., P.S.-B.; methodology, M.R.-C., C.J.-L., L.I.-G., E.M.-C., N.G.-A., C.C.-S., R.S.-C., C.G.-R., M.A.-M., J.C.T., B.C.-R., C.d.l.G.-A., A.S.I., R.A.-S., F.F., E.A., O.A.-B., P.S.-B.; software, M.M.-B.; validation, M.M.-B., N.L.-V., E.A., O.A.-B., P.S.-B.; formal analysis, M.M.-B., N.L.-V., O.A.-B., P.S.-B.; investigation, M.M.-B., N.L.-V., M.R.-C., C.J.-L., L.I.-G., E.M.-C., N.G.-A., C.C.-S., R.S.-C., C.G.-R., M.A.-M., J.C.T., B.C.-R., C.d.l.G.-A., A.S.I., R.A.-S., F.F., E.A., O.A.-B., P.S.-B.; resources, M.M.-B., N.L.-V., O.A.-B., P.S.-B.; data curation, M.M.-B., N.L.-V., O.A.-B., P.S.-B.; writing—original draft preparation, M.M.-B., E.A., N.L.-V., O.A.-B., P.S.-B.; writing—review and editing, M.M.-B., E.A., N.L.-V., O.A.-B., P.S.-B.; visualization, M.M.-B., N.L.-V.; supervision, M.M.-B., N.L.-V., O.A.-B., P.S.-B.; project administration, M.M.-B., O.A.-B., P.S.-B. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Ethical approval (Ethics Committee of the Hospital Virgen Macarena, Internal code 0942-N-15; 24 November 2015) was obtained before recruitment.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data is contained within the article.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Roversi S., Fabbri L.M., Sin D.D., Hawkins N.M., Agustí A. Chronic Obstructive Pulmonary Disease and Cardiac Diseases. An Urgent Need for Integrated Care. Am. J. Respir. Crit. Care Med. 2016;194:1319–1336. doi: 10.1164/rccm.201604-0690SO. [DOI] [PubMed] [Google Scholar]
- 2.Mullerova H., Agusti A., Erqou S., Mapel D.W. Cardiovascular comorbidity in COPD: Systematic literature review. Chest. 2013;144:1163–1178. doi: 10.1378/chest.12-2847. [DOI] [PubMed] [Google Scholar]
- 3.Hesse K., Bourke S., Steer J. Heart failure in patients with COPD exacerbations: Looking below the tip of the iceberg. Respir. Med. 2022;196:106800. doi: 10.1016/j.rmed.2022.106800. [DOI] [PubMed] [Google Scholar]
- 4.Simou A., Xanthopoulos A., Giamouzis G., Papagiannis D., Dimos A., Economou D., Skoularigis J., Triposkiadis F. Coexisting morbidity burden in elderly hospitalized patients with and without heart failure. Hell. J. Cardiol. 2022;65:53–55. doi: 10.1016/j.hjc.2022.02.002. [DOI] [PubMed] [Google Scholar]
- 5.Tinè M., Bazzan E., Semenzato U., Biondini D., Cocconcelli E., Balestro E., Casara A., Baraldo S., Turato G., Cosio M.G., et al. Heart failure is highly prevalent and difficult to diagnose in severe exacerbations of COPD presenting to the emergency department. J. Clin. Med. 2020;9:2644. doi: 10.3390/jcm9082644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loosen S.H., Roderburg C., Curth O., Gaensbacher J., Joerdens M., Luedde T., Konrad M., Kostev K., Luedde M. The spectrum of comorbidities at the initial diagnosis of heart failure a case control study. Sci. Rep. 2022;12:2670. doi: 10.1038/s41598-022-06618-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rushton C.A., Satchithananda D.K., Jones P.W., Kadam U.T. Noncardiovascular comorbidity, severity and prognosis in non-selected heart failure populations: A systematic review and meta-analysis. Int. J. Cardiol. 2015;196:98–106. doi: 10.1016/j.ijcard.2015.05.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoshihisa A., Takiguchi M., Shimizu T., Nakamura Y., Yamauchi H., Iwaya S., Owada T., Miyata M., Abe S., Sato T., et al. Cardiovascular function and prognosis of patients with heart failure coexistent with chronic obstructive pulmonary disease. J. Cardiol. 2014;64:256–264. doi: 10.1016/j.jjcc.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 9.Fisher K.A., Stefan M.S., Darling C., Lessard D., Goldberg R.J. Impact of COPD on the mortality and treatment of patients hospitalized with acute decompensated heart failure: The Worcester Heart Failure Study. Chest. 2015;147:637–645. doi: 10.1378/chest.14-0607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Creagh-Brown B. Benefits of b blockers in chronic obstructive pulmonary disease and heart failure. BMJ. 2014;348:g3316. doi: 10.1136/bmj.g3316. [DOI] [PubMed] [Google Scholar]
- 11.Kwon B.-J., Kim D.-B., Jang S.-W., Yoo K.-D., Moon K.-W., Shim B.J., Ahn S.-H., Cho E.-J., Rho T.-H., Kim J.-H. Prognosis of heart failure patients with reduced and preserved ejection fraction and coexistent chronic obstructive pulmonary disease. Eur. J. Heart Fail. 2010;12:1339–1344. doi: 10.1093/eurjhf/hfq157. [DOI] [PubMed] [Google Scholar]
- 12.Mentz R.J., Fiuzat M., Wojdyla D.M., Chiswell K., Gheorghiade M., Fonarow G.C., O’Connor C.M. Clinical characteristics and outcomes of hospitalized heart failure patients with systolic dysfunction and chronic obstructive pulmonary disease: Findings from OPTIMIZE-HF. Eur. J. Heart Fail. 2012;14:395–403. doi: 10.1093/eurjhf/hfs009. [DOI] [PubMed] [Google Scholar]
- 13.Martınez-Selles M., Garcıa Robles J.A., Prieto L., Dominguez Munos M., Frades E., Dıaz-Castro O., Almendral J. Systolic dysfunction is a predictor of long term mortality in men but not in women with heart failure. Eur. Heart J. 2003;24:2046–2053. doi: 10.1016/j.ehj.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 14.Méndez-Bailón M., Lorenzo-Villalba N., Romero-Correa M., Guisado-Espartero E., González-Soler J., Rugeles-Niño J., Sebastián-Leza A., Ceresuela-Eito L., Romaní-Costa V., Quesada-Simón A., et al. Cancer Impacts Prognosis on Mortality in Patients with Acute Heart Failure: Analysis of the EPICTER Study. J. Clin. Med. 2022;11:571. doi: 10.3390/jcm11030571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patel R.B., Warraich H.J., Butler J., Vaduganathan M. Surprise, surprise: Improving the referral pathway to palliative care interventions in advanced heart failure. Eur. J. Heart Fail. 2019;21:235–237. doi: 10.1002/ejhf.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Díez-Manglano J., Sánchez Muñoz L.Á., García Fenoll R., Freire E., Isasi de Isasmendi Pérez S., Carneiro A.H., Torres Bonafonte O. Spanish and Portuguese Societies of Internal Medicine consensus guideline about best practice in end-of-life care. Rev. Clin. Esp. 2020;221:33–44. doi: 10.1016/j.rce.2020.04.014. [DOI] [PubMed] [Google Scholar]
- 17.Florea V.G., Henein M.Y., Rauchhaus M., Koloczek V., Sharma R., Doehner W., Poole-Wilson P.A., Coats A.J., Anker S.D. The cardiac component of cardiac cachexia. Am. Heart J. 2002;144:45–50. doi: 10.1067/mhj.2002.123314. [DOI] [PubMed] [Google Scholar]
- 18.Argilés J.M., Busquets S., López-Soriano F.J., Figueras M. Fisiopatología de la caquexia neoplásica Pathophysiology of neoplasic cachexia. Nutr. Hosp. 2006;21:4–9. [PubMed] [Google Scholar]
- 19.Roesthuis L., van der Hoeven H., Sinderby C., Frenzel T., Ottenheijm C., Brochard L., Doorduin J., Heunks L. Effects of levosimendan on respiratory muscle function in patients weaning from mechanical ventilation. Intensive Care Med. 2019;45:1372–1381. doi: 10.1007/s00134-019-05767-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Farmakis D., Alvarez J., Gal T.B., Brito D., Fedele F., Fonseca C., Gordon A.C., Gotsman I., Grossini E., Guarracino F., et al. Levosimendan beyond inotropy and acute heart failure: Evidence of pleiotropic effects on the heart and other organs: An expert panel position paper. Int. J. Cardiol. 2016;222:303–312. doi: 10.1016/j.ijcard.2016.07.202. [DOI] [PubMed] [Google Scholar]
- 21.Crespo-Leiro M.G., Metra M., Lund L.H., Milicic D., Costanzo M.R., Filippatos G., Gustafsson F., Tsui S., Barge-Caballero E., De Jonge N., et al. Advanced heart failure: A position statement of the Heart Failure Association of the European Society of Cardiology. Eur. J. Heart Fail. 2018;20:1505–1535. doi: 10.1002/ejhf.1236. [DOI] [PubMed] [Google Scholar]
- 22.Cereda A., Toselli M., Palmisano A., Leone R., Vignale D., Nicoletti V., Campo G., Monello A., Ippolito D., Giannini F., et al. Is pleural effusion in COVID-19 interstitial pneumonia related to in-hospital mortality? Ital. J. Med. 2021;15:56–58. doi: 10.4081/itjm.2021.1440. [DOI] [Google Scholar]
- 23.Ruocco G., Pastorini G., Feola M. Echocardiography and impedance cardiography as determinants of successful slow levosimendan infusion in advanced older heart failure patients. J. Geriatr. Cardiol. 2021;18:1058–1062. doi: 10.11909/j.issn.1671-5411.2021.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data is contained within the article.