Abstract
This study investigated the association between micronutrient intake and breast cancer risk in South Korean adult women. This association was stratified according to body mass index (BMI) categories. Data from the Korean Genome and Epidemiology Study (KoGES) and the Health Examinee Study were analyzed. Altogether, 63,337 individuals (aged ≥40 years) completed the baseline and first follow-up surveys; 40,432 women without a history of cancer at baseline were included in this study. The association between micronutrient intake and breast cancer was determined by estimating the hazard ratio (HR) and 95% confidence interval (CI) using the Cox proportional hazard regression model. A stratified analysis by BMI (<25 kg/m2 and ≥25 kg/m2) was performed. The an analysis of 15 micronutrients and breast cancer risk revealed that none of the micronutrients were associated with breast cancer risk after adjusting for covariates. In obese women, the risk of breast cancer was significantly reduced in the group that consumed vitamin C more than the recommended level (HR = 0.54, 95% CI: 0.31–0.93) and vitamin B6 levels above the recommended level (HR = 0.48, 95% CI: 0.25–0.89). In obese women, exceeding the recommended daily intake levels of vitamin C and vitamin B6 was associated with a lower risk of breast cancer. However, other micronutrients were not associated with breast cancer risk in these women.
Keywords: breast cancer, body mass index, micronutrients, vitamin B6, vitamin C
1. Introduction
According to GLOBOCAN 2020, breast cancer is the most common cancer in women worldwide and ranks first in terms of cancer incidence and mortality in most countries (159 and 110 countries, respectively) [1]. According to the 2018 cancer registration statistics in South Korea, breast cancer is the most common cancer in women, with 23,647 (20.5%) cases, and the incidence rate has been continuously increasing [2]. Known risk factors for breast cancer are mainly reproductive factors, including the age at birth, the number of births, breastfeeding experience and duration, and the use of hormone replacement therapy after menopause [3]. The factors related to lifestyle, the level of physical activity, and alcohol consumption are well-known risk factors; however, diet findings have not been clearly understood [4,5]. In a meta-analysis, data from several studies showed that the intake of vitamins A and E reduced breast cancer risk, but no significant results were found in the cohort study [6]. The total retinol intake and breast cancer risk were not significant in the case-control study but were significant in the cohort study [6]. A study on the association between grain intake and breast cancer risk revealed heterogeneity [7]. A case-control study showed that grain intake reduced the risk of breast cancer; however, this finding was not significant in a cohort study [7].
The incidence of breast cancer in women is rapidly increasing in Asian countries, including in South Korea [8]. The rapid westernization of diet and lifestyle has been suggested to increase the incidence of breast cancer [1]. Westernized eating habits such as a high-fat diet [9,10], a high processed meat intake [11,12], a low fruit/vegetable intake [13,14], and soy products [15,16] have been associated with an increased breast cancer incidence in randomized controlled trials or meta-analyses of observational studies [17]. There is evidence of the protective effect of micronutrients on breast cancer progression through the alteration of signaling pathways related to apoptosis, the suppression of proliferation, and the invasion of breast cancer cells in in vitro models [18]. However, epidemiological studies have mostly focused on specific food items or macronutrients, and epidemiological studies on micronutrients and breast cancer are limited.
In South Korea, most studies on diet and cancer have focused on single nutrients or macronutrients, and most of the results were retrieved from small case-control studies, showing large variations in study results [19]. In addition, different associations between nutrition and breast cancer, such as the protective association of soy isoflavon in Asians, but no association in Western populations [15,16], were observed due to a large variation in the amount of intake between countries. Therefore, the association between micronutrients and breast cancer needs to be assessed in a large-scale prospective study, reflecting the dietary pattern of each country. Thus, we assessed the association between micronutrient intake and breast cancer risk in a large prospective cohort in South Korea from the Korean Genome and Epidemiology Study (KoGES) cohort study.
2. Materials and Methods
2.1. Study Design and Population
The KoGES is a cohort study administered by the Korea Agency for Disease Control and Prevention for the purpose of identifying the genetic and environmental etiology of common chronic diseases in the Korean population to establish a scientific basis for personalized prevention. The KoGES consists of six subcohorts: three population-based cohorts and three gene-environment model studies [20]. Of the six subcohorts, the data of the Health Examinee (HEXA) study, the largest subcohort, was applied in this study. The details of the KoGES and HEXA studies have been described previously [20].
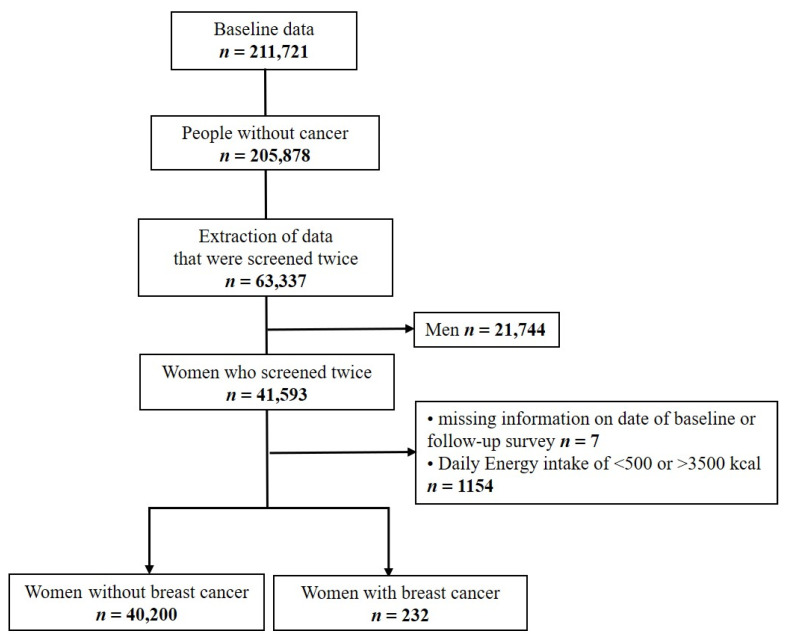
The baseline study population of the HEXA study included men and women aged ≥40 years who underwent a national health examination at 38 health examination centers from 2004 to 2013 [21]. Of the 211,721 participants who completed the baseline survey, those who reported a past history of cancer diagnosed by a doctor at the baseline survey (n = 5843) were excluded (Figure 1). A total of 63,337 individuals who completed the follow-up survey from 2012 to 2016 were considered for this study. Only women (n = 41,593) were included in the study. Women with missing information on the date of the baseline or follow-up survey and women with a daily energy intake of <500 kcal or >3500 kcal (n = 1161) were excluded, leaving 40,432 participants to be included in the analysis. This study was approved by the institutional review board of the Hanyang University College of Medicine, Republic of Korea (approval no. HYUIRB-202106-003-1).
Figure 1.
Flow chart for the participant selection protocol.
2.2. Assessment of Nutrient Intake
Dietary evaluation in the KoGES was based on the results of a standardized semi-quantitative food frequency questionnaire (FFQ). A total of 103 items were included in the FFQ, and micronutrient intake was estimated based on the FFQ. The detailed process for the development and validation of the FFQ is described elsewhere [22]. The estimated micronutrient intake in the HEXA study was divided according to the 2020 Dietary Reference Intakes for Koreans (KDRIs) established by the Ministry of Health and Welfare in Korea [23]. The KDRIs provide the recommended daily nutritional intake for 15 micronutrients (calcium, phosphorus, iron, potassium, vitamin A, sodium, vitamin B1, vitamin B2, niacin, vitamin C, zinc, vitamin B6, folate, vitamin E, and cholesterol) and four main nutrients (energy, proteins, fats, and carbohydrates) according to age group. Participants were divided into two groups: women who consumed more than the recommended daily nutritional intake and those who consumed up to the recommended daily nutritional intake. Cut-off values differ by age group (30–49 years, 50–64 years, 65–74 years, and ≥75 years) and by nutrients. For example, women aged 30–49 years consuming >700 mg of calcium fall into the recommended excess group (>recommended intake). Details on the recommended nutrient intake standards are presented in Table A1.
2.3. Breast Cancer Incidence
The incidence of breast cancer was defined as that among those who reported cancer-free at baseline survey and those who answered that they had been diagnosed with breast cancer by a doctor after the baseline survey at the follow-up survey. A total of 232 women reported that they had been diagnosed with breast cancer by a physician after the baseline survey.
2.4. Covariates
Participants’ information was retrieved from the data surveyed by well-trained staff using standardized questionnaires. Basic survey data included sociodemographic factors, medical history, family medical history, smoking, drinking, level of physical activity, and female reproductive history [20]. The covariates considered in this study were age (40–49, 50–59, 60–69, and ≥70 years), body mass index (BMI; <25 kg/m2, ≥25 kg/m2, or missing), history of benign breast tumors (no, yes, or missing), age at menarche (<15 years, ≥15 years, or missing), menopausal status and age (no, <52 years, ≥52 years, or missing), breastfeeding (no, yes, or missing), smoking (never, former, current, or missing), drinking (no, yes, or missing), physical activity (no, <150 min/week, ≥150 min/week, or missing), and family history of breast cancer (no, yes, or missing). BMI was calculated by dividing weight by the square of height in meters and was classified as ≥25 kg/m2 or <25 kg/m2.
2.5. Statistical Analysis
The distribution of risk factors for breast cancer and micronutrient intake at baseline was compared between women who developed breast cancer and those who did not develop. Nutritional intake was presented as the mean and proportion of women who consumed more or less than the daily recommended intake. We investigated the association between micronutrient intake (more than the recommended level vs. less than the recommended level) and breast cancer risk by estimating hazard ratio (HR) and 95% confidence interval (CI) using the Cox proportional hazards regression model adjusted for the above-mentioned covariates. The follow-up period was calculated as the number of years between the baseline survey and the year of cancer diagnosis or the year of the follow-up survey. In addition, the association between micronutrient intake and breast cancer risk was estimated in obese (BMI ≥25 kg/m2) and non-obese women (BMI <25 kg/m2). All statistical analyses were performed using the SAS statistical software (version 9.4; SAS Institute, Cary, NC, USA).
3. Results
Of the 40,432 cancer-free women who completed both the baseline and follow-up surveys, 232 were diagnosed with breast cancer. The mean follow-up period was 4.9 years (median: 4.0 years). Table 1 presents the participants’ characteristics. In the baseline survey, 35.0% of the women who did not develop breast cancer were in their forties, whereas 44.8% of women who developed breast cancer were in their forties, showing a younger age at baseline of women who developed breast cancer (p = 0.012). The proportion of premenopausal women, women without breastfeeding experience, and women with physical activity for ≥150 min/week were higher in women who developed breast cancer than those in women without breast cancer (p < 0.05).
Table 1.
General characteristics of participants according to breast cancer.
| Characteristic | Total | % | Breast Cancer | p-Value * | |||
|---|---|---|---|---|---|---|---|
| No (n = 40,200) |
% | Yes (n = 232) |
% | ||||
| Age (years) | |||||||
| 40–49 | 14,187 | 35.1 | 14,083 | 35.0 | 104 | 44.8 | 0.012 |
| 50–59 | 17,471 | 43.2 | 17,392 | 43.3 | 79 | 34.1 | |
| 60–69 | 8409 | 20.8 | 8362 | 20.8 | 47 | 20.3 | |
| ≥70 | 365 | 0.9 | 363 | 0.9 | 2 | 0.8 | |
| Body mass index (kg/m2) | |||||||
| <25 | 29,103 | 72.0 | 28,939 | 72.0 | 164 | 70.7 | 0.855 |
| ≥25 | 11,310 | 27.9 | 11,242 | 27.9 | 68 | 29.3 | |
| Missing | 19 | 0.1 | 19 | 0.1 | 0 | 0 | |
| Diagnosis of benign breast cancer | |||||||
| No | 28,924 | 71.5 | 28,772 | 71.6 | 152 | 65.5 | 0.061 |
| Yes | 2183 | 5.4 | 2164 | 5.4 | 19 | 8.2 | |
| Missing | 9325 | 23.1 | 9264 | 23.0 | 61 | 26.3 | |
| Age at menarche (years) | |||||||
| <15 | 15,082 | 37.3 | 14,981 | 37.3 | 101 | 43.6 | 0.140 |
| ≥15 | 24,468 | 60.5 | 24,341 | 60.6 | 127 | 54.7 | |
| Missing | 882 | 2.2 | 878 | 2.1 | 4 | 1.7 | |
| Menopausal status and age (years) | |||||||
| No | 14,831 | 36.7 | 14,736 | 36.7 | 95 | 41.0 | <0.001 |
| <52 | 15,287 | 37.8 | 15,224 | 37.9 | 63 | 27.2 | |
| ≥52 | 8182 | 20.2 | 8130 | 20.2 | 52 | 22.4 | |
| Missing | 2132 | 5.2 | 2110 | 5.2 | 22 | 9.4 | |
| Breastfeeding | |||||||
| No | 4980 | 12.3 | 4935 | 12.3 | 45 | 19.4 | <0.001 |
| Yes | 33,497 | 82.9 | 33,326 | 82.9 | 171 | 73.7 | |
| Missing | 1955 | 4.8 | 1939 | 4.8 | 16 | 6.9 | |
| Smoking | |||||||
| No | 39,078 | 96.7 | 38,856 | 96.7 | 222 | 95.7 | 0.106 |
| Former | 461 | 1.1 | 455 | 1.1 | 6 | 2.5 | |
| Current | 704 | 1.7 | 702 | 1.8 | 2 | 0.9 | |
| Missing | 189 | 0.5 | 187 | 0.4 | 2 | 0.9 | |
| Drinking | |||||||
| No | 27,635 | 68.4 | 27,473 | 68.3 | 162 | 69.8 | 0.888 |
| Yes | 12,607 | 31.1 | 12,538 | 31.2 | 69 | 29.8 | |
| Missing | 190 | 0.5 | 189 | 0.5 | 1 | 0.4 | |
| Physical activity (min/week) | |||||||
| No | 18,723 | 46.3 | 18,634 | 46.4 | 89 | 38.4 | 0.002 |
| <150 | 4932 | 12.2 | 4910 | 12.2 | 22 | 9.5 | |
| ≥150 | 15,458 | 38.2 | 15,352 | 38.2 | 106 | 45.7 | |
| Missing | 1319 | 3.3 | 1304 | 3.2 | 15 | 6.4 | |
| Family history of breast cancer | |||||||
| No | 6734 | 16.7 | 6701 | 16.7 | 33 | 14.2 | 0.375 |
| Yes | 553 | 1.4 | 548 | 1.4 | 5 | 2.2 | |
| Missing | 33,145 | 81.9 | 32,951 | 81.9 | 194 | 83.6 | |
* p-values for categorical variables were calculated using the chi-square test.
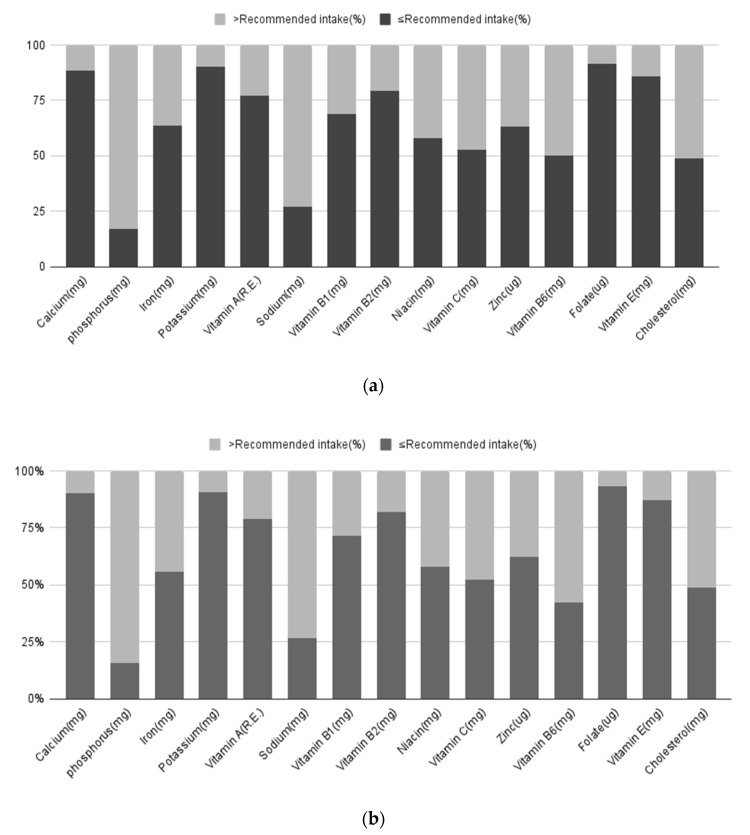
Table 2 compares the mean micronutrient intake and the proportion of women who consumed more or less than the daily recommended intake in those who did and did not develop breast cancer. The recommended micronutrient intakes and the distribution of breast cancer incidences are shown in Figure 2. A higher proportion of women who consumed less than the recommended amount of iron was observed in women who developed breast cancer (63.8%) than in those without breast cancer (56.0%) (p = 0.017). However, the average intake between the two groups was not significantly different.
Table 2.
Comparison of nutrient intake recommendations for patients with breast cancer.
| Nutrient | Breast Cancer | p-Value * | |||
|---|---|---|---|---|---|
| No (n = 40,200) | Yes (n = 232) | ||||
| N | % | N | % | ||
| Calcium (mg) | |||||
| Mean ± SD | 453.46 ± 250.64 | 481.60 ± 311.53 | 0.171 | ||
| ≤Recommended intake ** | 36,307 | 90.3 | 205 | 88.4 | 0.316 |
| >Recommended intake ** | 3893 | 9.7 | 27 | 11.6 | |
| Phosphorus (mg) | |||||
| Mean ± SD | 870.53 ± 319.01 | 886.96 ± 360.40 | 0.489 | ||
| ≤Recommended intake ** | 6450 | 16.0 | 40 | 17.2 | 0.621 |
| >Recommended intake ** | 33,750 | 84.0 | 192 | 82.8 | |
| Iron (mg) | |||||
| Mean ± SD | 9.83 ± 4.49 | 10.11 ± 5.03 | 0.402 | ||
| ≤Recommended intake ** | 22,514 | 56.0 | 148 | 63.8 | 0.017 |
| >Recommended intake ** | 17,686 | 44.0 | 84 | 36.2 | |
| Potassium(mg) | |||||
| Mean ± SD | 2229.23 ± 990.89 | 2277.75 ± 1077.79 | 0.457 | ||
| ≤Recommended intake ** | 36,382 | 90.5 | 209 | 90.1 | 0.829 |
| >Recommended intake ** | 3818 | 9.5 | 23 | 9.9 | |
| Vitamin A (R.E.) | |||||
| Mean ± SD | 468.86 ± 321.25 | 490.82 ± 361.00 | 0.356 | ||
| ≤Recommended intake ** | 31,664 | 78.8 | 179 | 77.2 | 0.550 |
| >Recommended intake ** | 8536 | 21.2 | 53 | 22.8 | |
| Sodium (mg) | |||||
| Mean ± SD | 2370.63 ± 1319.25 | 2391.46 ± 1387.47 | 0.811 | ||
| ≤Recommended intake ** | 10,764 | 26.8 | 63 | 27.2 | 0.897 |
| >Recommended intake ** | 29,436 | 73.2 | 169 | 72.8 | |
| Vitamin B1 (mg) | |||||
| Mean ± SD | 0.96 ± 0.37 | 0.96 ± 0.39 | 0.795 | ||
| ≤Recommended intake ** | 28,657 | 71.3 | 160 | 69.0 | 0.436 |
| >Recommended intake ** | 11,543 | 28.7 | 72 | 31.0 | |
| Vitamin B2 (mg) | |||||
| Mean ± SD | 0.89 ± 0.41 | 0.92 ± 0.45 | 0.305 | ||
| ≤Recommended intake ** | 32,964 | 82.0 | 184 | 79.3 | 0.288 |
| >Recommended intake ** | 7236 | 18.0 | 48 | 20.7 | |
| Niacin (mg) | |||||
| Mean ± SD | 13.84 ± 5.28 | 13.98 ± 5.66 | 0.692 | ||
| ≤Recommended intake ** | 23,292 | 57.9 | 135 | 58.1 | 0.939 |
| >Recommended intake ** | 16,908 | 42.1 | 97 | 41.9 | |
| Vitamin C (mg) | |||||
| Mean ± SD | 110.51 ± 68.07 | 114.28 ± 76.84 | 0.456 | ||
| ≤Recommended intake ** | 21,115 | 52.5 | 122 | 52.6 | 0.985 |
| >Recommended intake ** | 19,085 | 47.5 | 110 | 47.4 | |
| Zinc (µg) | |||||
| Mean ± SD | 7.65 ± 3.05 | 7.78 ± 3.20 | 0.488 | ||
| ≤Recommended intake ** | 25,007 | 62.2 | 147 | 63.4 | 0.717 |
| >Recommended intake ** | 15,193 | 37.8 | 85 | 36.6 | |
| Vitamin B6 (mg) | |||||
| Mean ± SD | 1.55 ± 0.62 | 1.56 ± 0.64 | 0.746 | ||
| ≤Recommended intake ** | 18,816 | 46.8 | 116 | 50.0 | 0.331 |
| >Recommended intake ** | 21,384 | 53.2 | 116 | 50.0 | |
| Folate (µg) | |||||
| Mean ± SD | 216.96 ± 114.93 | 220.17 ± 116.86 | 0.672 | ||
| ≤Recommended intake ** | 37,554 | 93.4 | 212 | 91.4 | 0.212 |
| >Recommended intake ** | 2646 | 6.6 | 20 | 8.6 | |
| Vitamin E (mg) | |||||
| Mean ± SD | 7.94 ± 3.92 | 8.34 ± 4.14 | 0.121 | ||
| ≤Recommended intake ** | 35,078 | 87.3 | 199 | 85.8 | 0.500 |
| >Recommended intake ** | 5122 | 12.7 | 33 | 14.2 | |
| Cholesterol (mg) | |||||
| Mean ± SD | 161.10 ± 110.61 | 166.87 ± 134.66 | 0.515 | ||
| ≤Recommended intake ** | 19,583 | 48.7 | 113 | 48.7 | 0.998 |
| >Recommended intake ** | 20,617 | 51.3 | 119 | 51.3 | |
* p-values for continuous and categorical variables were calculated using the t-test and chi-square test, respectively. ** The recommended nutrient intake standards were presented in Table A1.
Figure 2.
Recommended intake levels of nutrients for breast cancer (%). (a) Normal people; (b) People with breast cancer.
Among the micronutrients, iron intake above the recommended daily intake was associated with a reduced risk of breast cancer in the univariate analysis (cHR = 0.72; 95% CI: 0.55–0.95, Table 3); however, no statistical significance was observed after adjusting for covariates. No other micronutrient showed a statistically significant association.
Table 3.
HR (95% CI) of breast cancer risk for recommended nutrient intake.
| Nutrient | Breast Cancer | ||
|---|---|---|---|
| No. of Events/ Person Year |
cHR (95% CI) | aHR * (95% CI) | |
| Calcium (mg) | |||
| ≤Recommended intake ** | 205/177,782 | 1 | 1 |
| >Recommended intake ** | 27/20,390 | 1.17 (0.78–1.75) | 1.12 (0.72–1.76) |
| Phosphorus (mg) | |||
| ≤Recommended intake ** | 40/31,774 | 1 | 1 |
| >Recommended intake ** | 192/166,398 | 0.92 (0.65–1.29) | 0.88 (0.59–1.32) |
| Iron (mg) | |||
| ≤Recommended intake ** | 148/111,063 | 1 | 1 |
| >Recommended intake ** | 84/87,109 | 0.72 (0.55–0.95) | 0.74 (0.52–1.06) |
| Potassium (mg) | |||
| ≤Recommended intake ** | 209/177,987 | 1 | 1 |
| >Recommended intake ** | 23/20,185 | 0.99 (0.65–1.53) | 0.96 (0.59–1.57) |
| Vitamin A (R.E.) | |||
| ≤Recommended intake ** | 179/155,182 | 1 | 1 |
| >Recommended intake ** | 53/42,990 | 1.08 (0.79–1.47) | 1.12 (0.80–1.56) |
| Sodium (mg) | |||
| ≤Recommended intake ** | 63/52,688 | 1 | 1 |
| >Recommended intake ** | 169/145,484 | 0.98 (0.73–1.30) | 0.98 (0.72–1.34) |
| Vitamin B1 (mg) | |||
| ≤Recommended intake ** | 160/140,297 | 1 | 1 |
| >Recommended intake ** | 72/57,875 | 1.10 (0.83–1.45) | 1.14 (0.78–1.66) |
| Vitamin B2 (mg) | |||
| ≤Recommended intake ** | 184/160,930 | 1 | 1 |
| >Recommended intake ** | 48/37,242 | 1.15 (0.83–1.58) | 1.17 (0.80–1.73) |
| Niacin (mg) | |||
| ≤Recommended intake ** | 135/114,543 | 1 | 1 |
| >Recommended intake ** | 97/83,629 | 0.99 (0.76–1.28) | 0.95 (0.67–1.33) |
| Vitamin C (mg) | |||
| ≤Recommended intake ** | 122/102,230 | ||
| >Recommended intake ** | 110/95,942 | 0.97 (0.75–1.26) | 0.95 (0.71–1.26) |
| Zinc (µg) | |||
| ≤Recommended intake ** | 147/122,609 | 1 | 1 |
| >Recommended intake ** | 85/75,563 | 0.94 (0.72–1.23) | 0.89 (0.61–1.28) |
| Vitamin B6 (mg) | |||
| ≤Recommended intake ** | 116/91,707 | 1 | 1 |
| >Recommended intake ** | 116/106,465 | 0.87 (0.67–1.12) | 0.78 (0.56–1.09) |
| Folate (µg) | |||
| ≤Recommended intake ** | 212/184,209 | 1 | 1 |
| >Recommended intake ** | 20/13,963 | 1.27 (0.81–2.01) | 1.32 (0.80–2.19) |
| Vitamin E (mg) | |||
| ≤Recommended intake ** | 199/171,659 | 1 | 1 |
| >Recommended intake ** | 33/26,513 | 1.09 (0.76–1.58) | 1.07 (0.69–1.66) |
| Cholesterol (mg) | |||
| ≤Recommended intake ** | 113/99,875 | 1 | 1 |
| >Recommended intake ** | 119/98,297 | 1.03 (0.79–1.33) | 1.11 (0.83–1.49) |
* Adjusted for energy, age (40–49, 50–59, 60–69, and ≥70 years), body mass index (<25 kg/m2 or ≥25 kg/m2), diagnosis of benign breast cancer (no or yes), age at menarche (<15 or ≥15 years), menopausal status and age (no, <52 years, or ≥52 years), breastfeeding (no or yes), smoking (never, former, or current), drinking (no or yes), physical activity (no, <150 min/week, or ≥150 min/week), and family history of breast cancer (no or yes); aHR, adjusted hazard ratio; CI, confidence interval. ** The recommended nutrient intake standards were presented in Table A1.
In a separate analysis by obesity status (BMI ≥25 kg/m2 or <25 kg/m2), iron intake more than the daily recommended level was associated with a reduced risk of breast cancer with a cHR of 0.69 (95% CI: 0.50–0.96) in a univariate analysis with a normal weight. In addition, the intake of vitamin C and vitamin B6 above the daily recommended value was associated with a reduced risk in obese women with aHR of 0.53 (95% CI: 0.30–0.92) and 0.45 (95% CI: 0.24–0.86), but a significant association was not observed in women with normal weight (Table 4). None of the other micronutrients exhibited a significant association in both women with a normal weight and obese women.
Table 4.
Adjusted HR (95% CI) of breast cancer risk for recommended nutrient intake according to BMI.
| Nutrient | BMI < 25 kg/m2 | BMI ≥ 25 kg/m2 | ||
|---|---|---|---|---|
| cHR (95% CI) | aHR * (95% CI) | cHR (95% CI) | aHR * (95% CI) | |
| >Recommended Intake (Reference: ≤Recommended Intake) ** | ||||
| Calcium (mg) | 1.00 (0.61–1.66) | 0.93 (0.53–1.62) | 1.64 (0.84–3.22) | 1.60 (0.74–3.47) |
| Phosphorus (mg) | 0.83 (0.56–1.23) | 0.74 (0.46–1.18) | 1.21 (0.60–2.45) | 1.34 (0.60–2.97) |
| Iron (mg) | 0.69 (0.50–0.96) | 0.68 (0.44–1.04) | 0.78 (0.48–1.27) | 0.90 (0.48–1.70) |
| Potassium (mg) | 0.98 (0.58–1.64) | 0.94 (0.53–1.69) | 1.03 (0.47–2.26) | 0.93 (0.38–2.31) |
| Vitamin A (R.E.) | 1.05 (0.73–1.52) | 1.09 (0.72–1.63) | 1.13 (0.66–1.96) | 1.17 (0.63–2.14) |
| Sodium (mg) | 1.01 (0.71–1.42) | 1.01 (0.70–1.47) | 0.90 (0.52–1.54) | 0.89 (0.50–1.58) |
| Vitamin B1 (mg) | 1.15 (0.83–1.59) | 1.23 (0.79–1.92) | 0.99 (0.59–1.67) | 0.97 (0.48–1.96) |
| Vitamin B2 (mg) | 1.15 (0.79–1.67) | 1.18 (0.74–1.88) | 1.14 (0.63–2.05) | 1.13 (0.55–2.35) |
| Niacin (mg) | 1.04 (0.76–1.42) | 1.02 (0.68–1.54) | 0.87 (0.53–1.41) | 0.80 (0.42–1.52) |
| Vitamin C (mg) | 1.18 (0.87–1.61) | 1.19 (0.85–1.67) | 0.60 (0.36–0.99) | 0.53 (0.30–0.92) |
| Zinc (µg) | 0.97 (0.71–1.34) | 0.93 (0.60–1.43) | 0.88 (0.53–1.44) | 0.79 (0.40–1.56) |
| Vitamin B6 (mg) | 1.01 (0.74–1.37) | 0.98 (0.66–1.45) | 0.61 (0.37–0.98) | 0.45 (0.24–0.86) |
| Folate (µg) | 1.25 (0.73–2.17) | 1.29 (0.71–2.36) | 1.31 (0.57–3.03) | 1.25 (0.49–3.19) |
| Vitamin E (mg) | 1.11 (0.72–1.72) | 1.08 (0.64–1.82) | 1.05 (0.52–2.11) | 0.98 (0.42–2.30) |
| Cholesterol (mg) | 0.96 (0.71–1.31) | 1.04 (0.73–1.47) | 1.19 (0.73–1.92) | 1.31 (0.76–2.26) |
* Adjusted for energy, age (40–49, 50–59, 60–69, or ≥70 years), diagnosis of benign breast cancer (no or yes), age at menarche (<15 or ≥15 years), menopausal status and age (no, <52 years, or ≥52 years), breastfeeding (no or yes), smoking (never, former, or current), drinking (no or yes), physical activity (no, <150 min/week, or ≥150 min/week), and family history of breast cancer (no or yes); aHR, adjusted hazard ratio; CI, confidence interval. ** The recommended nutrient intake standards were presented in Table A1.
4. Discussion
This study evaluated micronutrients in a large prospective cohort study in Korea and identified that the intake of vitamin C and vitamin B6 above the daily recommendation level was associated with a reduced risk of breast cancer in obese women. To the best of our knowledge, this is the first prospective study to investigate the association between micronutrients and breast cancer in Korea.
Vitamin C has antioxidant activity and is found in vegetables and fruits. Its ability to reduce free radicals and oxidative damage to DNA are suggested mechanisms for reducing cancer risk [24,25]. Despite the protective association between vitamin C and several types of cancer from meta-analyses, including colorectal adenoma [26], gastric cancer [27,28], esophageal cancer [29], endometrial cancer [30], lung cancer [31], and breast cancer [6,32], several aspects should be considered.
First, the association between vitamin C and breast cancer was affected by the study design. A meta-analysis of case-control studies showed a protective effect of high-dose vitamin C on breast cancer risk; cohort studies did not show significant associations. In addition, the heterogeneity of the included studies was high [6,32]. Similarly, significant differences in the plasma levels of vitamin C between breast cancer cases and controls were observed only in case-control studies, but not in cohort-based studies [33]. Patients with breast cancer changed their dietary habits soon after the diagnosis by eating more fruits and vegetables, taking dietary supplements, and eating less meat and fat intake [34]. Therefore, the protective effect of vitamin C may be overestimated in case-control studies. A previous meta-analysis performed a subgroup analysis by menopausal status, vitamin C source, geographical location, and study design [6,32,33]. In this study, we did not find a different result according to menopausal status (Table A2), but when stratified by obesity status, a protective association was evident in obese women. Obesity is associated with higher estrogen levels in postmenopausal women due to the aromatase change of testosterone to estrogen in adipose tissue, as well as chronic inflammation status with increased oxidative stress permanently [35,36]. Thus, the antioxidant effect of vitamin C may be more prominent in women with obesity.
Second, dietary vitamin C was associated with a decreased risk of breast cancer, but supplementation did not show this association [6,32]. However, studies have shown inconsistent results regarding fruit and vegetable intake and breast cancer. A previous study showed that fruit intake was not associated with breast cancer, but a higher vegetable intake had a protective effect against breast cancer [14]. Otherwise, a meta-analysis of prospective studies showed an association between a high intake of fruit or fruit and vegetables combined with breast cancer but not with that of vegetables [13]. A recent large prospective study also showed a reduced association with an increased fruit intake [37]. Although fruits and vegetables are major sources of vitamin C, vitamin C is not prevalent in all vegetables and fruits [38]. Thus, the effect of vitamin C on breast cancer needs to be interpreted in combination with its source. In this study, vitamin C level was measured using the FFQ of 103 food items, and dietary supplements were not included in the food items. There is a moderate relationship between plasma vitamin C and estimated vitamin C from FFQ, and this relationship is stronger in non-smokers and obese people [39,40]. In this study, approximately 97% of women were non-smokers; thus, the association would reflect dietary vitamin C intake, with a better relationship with vitamin C.
Vitamin B6 is a B vitamin found in various sources, such as meat, fish, dairy, and root vegetables. Vitamin B6 is a one-carbon metabolism-related vitamin that affects carcinogenesis and development through its effect on DNA replication, repair, gene expression, DNA synthesis, and methylation, upholding DNA integrity, and regulating gene expression [41,42]. Vitamin B6 intake and serum pyridoxal 5-phosphate, an active form of vitamin B6, have been suggested to have protective effects against gastrointestinal cancers [43] including colorectal [44] and pancreatic cancers [45]. However, the association between vitamin B6 intake, serum pyridoxal 5-phosphate, and breast cancer showed inconsistent findings, even in a meta-analysis. A meta-analysis including prospective and case-control studies showed no association between dietary intake of vitamin B6 and breast cancer risk, but a protective association between serum pyridoxal 5-phosphate, an active form of vitamin B6, and breast cancer in postmenopausal women with a dose–response relationship [46]. Another meta-analysis showed a protective association between dietary intake of vitamin B6 and breast cancer but no association between pyridoxal 5-phosphate and breast cancer [43]. A recent meta-analysis of prospective studies identified a slightly reduced risk of breast cancer by 6% (pooled OR = 0.94) associated with a high intake of vitamin B6 [47]. However, in the subgroup analysis according to intake assessment, study design, menopausal status, and hormone receptor status, no significant association was observed [47]. Among the biomarkers of vitamin B6, pyridoxal 5-phosphate showed a strong correlation with vitamin B6 intake, and the correlation was affected by personal and lifestyle factors, including sex and menopausal status [48]. This might explain the inconsistencies between the studies. In this study, a protective association of high vitamin B6 intake was observed only in obese women [49]. Studies have suggested that vitamin B6 is also involved in insulin resistance by controlling the expression of adipogenesis-related genes [50]. Thus, the protective effect may be more prominent in women with obesity.
Previous studies on diet and cancer risk in Korea were mostly case-control studies [19]. To the best of our knowledge, this is the largest prospective study to show the association between micronutrients and breast cancer risk in Korean women. The main limitation of this study is that micronutrient intake was estimated based on a single assessment of the FFQ. Thus, measurement errors would be present due to the limited inclusion of food items and an inaccurate recall of their food intake over a long period [20]. Despite these limitations, the FFQ is the most common and practical dietary assessment tool used in prospective studies [20] and the FFQ applied in the KoGES has been well validated [51]. Second, cancer development was assessed using a follow-up questionnaire. Despite possible information bias, a previous study showed that self-reported cancer history in the HEXA study had a high accuracy, especially for breast cancer [52]. Third, the proportion of women who participated in the follow-up survey was low; thus, the selection bias was due to systemic differences between women who did or did not participate in the follow-up. However, when we compared the baseline characteristics between the two groups, no differences were identified. Fourth, we did not consider the subtypes of breast cancer based on hormone receptor status because of the unavailability of information. Fifth, there was only one follow-up survey, and the average follow-up period of 4.9 years may be too short to examine the effect of dietary intake on breast cancer incidence. In addition, possible confounding factors that were not measured or were measured suboptimally cannot be excluded. Therefore, it is necessary to study many patients with breast cancer with further follow-up.
In this study, only two micronutrients showed a reduced association with breast cancer risk. Recent studies have identified that only a few nutrients or food items are associated with breast cancer [37,53]. According to the report of the World Cancer Research Fund, all diet and nutrition, except for alcohol, have limited evidence on breast cancer risk [54]. These findings would support the suggestion that diet in mid-life or recent years might contribute minimally to breast cancer development [55]. However, micronutrients with a significantly reduced breast cancer risk in obese women in this study (vitamins C and B6) were intensively investigated in the Western population, which was consistent with findings in the Korean population despite variations in eating habits. Further studies related to nutritional status throughout the life course or critical period, such as during childhood or early adulthood, are warranted.
Appendix A
Table A1.
Dietary reference intake levels for females in South Korean in 2020 according to age group.
| Nutrient | Age Group (y) | |||
|---|---|---|---|---|
| 30–49 | 50–64 | 65–74 | ≥75 | |
| Calcium (mg) | 700 | 800 | 800 | 800 |
| Phosphorus (mg) | 580 | 580 | 580 | 580 |
| Iron (mg) | 14 | 8 | 8 | 7 |
| Potassium (mg) | 3500 | 3500 | 3500 | 3500 |
| Vitamin A (R.E.) | 650 | 600 | 600 | 550 |
| Sodium (mg) | 1500 | 1500 | 1500 | 1500 |
| Vitamin B1 (mg) | 1.1 | 1.1 | 1 | 0.8 |
| Vitamin B2 (mg) | 1.2 | 1.2 | 1.1 | 1 |
| Niacin (mg) | 14 | 14 | 13 | 12 |
| Vitamin C (mg) | 100 | 100 | 100 | 100 |
| Zinc (µg) | 8 | 8 | 7 | 7 |
| Vitamin B6 (mg) | 1.4 | 1.4 | 1.4 | 1.4 |
| Folate (µg) | 400 | 400 | 400 | 400 |
| Fiber (g) | 20 | 20 | 20 | 20 |
| Vitamin E (mg) | 12 | 12 | 12 | 12 |
| Cholesterol (mg) | 180 | 120 | 50 | 20 |
Table A2.
Adjusted HR (95% CI) of breast cancer risk for the recommended nutrient intake level according to menopausal age.
| Nutrient | No | <52 | ≥52 |
|---|---|---|---|
| aHR * (95% CI) | aHR * (95% CI) | aHR * (95% CI) | |
| >Recommended Intake (Reference: ≤Recommended Intake) ** | |||
| Calcium (mg) | 1.08 (0.54–2.16) | 0.61 (0.22–1.65) | 2.12 (0.85–5.29) |
| Phosphorus (mg) | 1.28 (0.64–2.55) | 0.98 (0.44–2.22) | 0.61 (0.28–1.33) |
| Iron (mg) | 0.73 (0.37–1.44) | 0.57 (0.30–1.10) | 0.87 (0.44–1.72) |
| Potassium (mg) | 0.62 (0.25–1.51) | 0.55 (0.20–1.53) | 2.17 (0.88–5.36) |
| Vitamin A (R.E.) | 1.42 (0.84–2.41) | 0.60 (0.29–1.22) | 1.21 (0.61–2.42) |
| Sodium (mg) | 0.77 (0.48–1.24) | 1.34 (0.70–2.57) | 0.89 (0.47–1.68) |
| Vitamin B1 (mg) | 1.02 (0.57–1.81) | 0.87 (0.42–1.80) | 2.31 (1.05–5.08) |
| Vitamin B2 (mg) | 1.05 (0.56–1.95) | 0.85 (0.39–1.83) | 2.60 (1.21–5.59) |
| Niacin (mg) | 1.12 (0.66–1.91) | 0.78 (0.40–1.51) | 1.14 (0.55–2.38) |
| Vitamin C (mg) | 0.91 (0.58–1.42) | 1.35 (0.78–2.33) | 0.83 (0.45–1.54) |
| Zinc (µg) | 0.88 (0.50–1.57) | 0.89 (0.45–1.77) | 0.83 (0.38–1.81) |
| Vitamin B6 (mg) | 1.12 (0.67–1.89) | 0.60 (0.31–1.13) | 0.84 (0.42–1.70) |
| Folate (µg) | 1.13 (0.46–2.75) | 1.19 (0.47–3.03) | 1.22 (0.39–3.79) |
| Vitamin E (mg) | 1.27 (0.65–2.46) | 0.76 (0.31–1.86) | 1.06 (0.39–2.87) |
| Cholesterol (mg) | 1.17 (0.74–1.86) | 1.06 (0.60–1.87) | 1.23 (0.67–2.26) |
* Adjusted for energy, age (40–49, 50–59, 60–69, and ≥70 years), body mass index (<25 kg/m2 or ≥25 kg/m2), diagnosis of benign breast cancer (no or yes), age at menarche (<15 or ≥15 years), breastfeeding (no or yes), smoking (never, former, or current), drinking (no and yes), physical activity (no, <150 min/week or ≥150 min/week), and family history of breast cancer (no or yes); aHR, adjusted hazard ratio; CI, confidence interval. ** The recommended nutrient intake standards were presented in Table A1.
Table A3.
Summary of previous studies on the association between nutrients and breast cancer risk by obesity status.
| (a). Calcium—1/2pt | ||
| Study type | Title | Findings |
| Cohort study | Calcium intake is not related to breast cancer risk among Singapore Chinese women [56]. |
|
| Case-control study | Dairy Products, Calcium Intake, and Breast Cancer Risk: A Case-Control Study in China [57]. |
|
| Meta-analysis | Meta-analysis of vitamin D, calcium, and the prevention of breast cancer [58]. |
|
| Case-control study | Raw and Cooked Vegetables, Fruits, Selected Micronutrients, and Breast Cancer Risk: A Case–Control Study in Germany [59]. |
|
| (b). Phosphorus | ||
| Study type | Title | Findings |
| Cohort study | Imbalanced Nutrient Intake in Cancer Survivors from the Examination from the Nationwide Health Examination Center-Based Cohort [60]. |
|
| Case-control study | The Intake of some Nutrients is Associated with the Risk of Breast Cancer: Results from Jordanian Case-Control Study [61]. |
|
| (c). Iron | ||
| Study type | Title | Findings |
| Cohort study | Dietary Iron and Heme Iron Intake and Risk of Breast Cancer: A Prospective Cohort Study [62]. |
|
| Case-control study | A case-control study on heme/non-heme iron and breast cancer risk breast cancer risk [63]. |
|
| Case-control study | Raw and Cooked Vegetables, Fruits, Selected Micronutrients, and Breast Cancer Risk: A Case–Control Study in Germany [59]. |
|
| Meta-analysis | Iron intake, body iron status, and risk of breast cancer: a systematic review and meta-analysis [64]. |
|
| (d). Vitamin A | ||
| Study type | Title | Findings |
| Cohort study | A Prospective Study of the Intake of Vitamins C, E, and A and the Risk of Breast Cancer [65]. |
|
| Case-control study | Intake of Carrots, Spinach, and Supplements Containing Vitamin A in Relation to Risk of Breast Cancer [66]. |
|
| Meta-analysis | Vitamin A and Breast Cancer Survival: A Systematic Review and Meta-analysis [67]. |
|
| (e). Vitamin B1 | ||
| Study type | Title | Findings |
| Cohort study | B-Vitamin Intake from Diet and Supplements and Breast Cancer Risk in Middle-Aged Women: Results from the Prospective NutriNet-Santé Cohort [68]. |
|
| Case-control study | Nutrient Patterns and Risk of Breast Cancer among Iranian Women: a Case- Control Study [69]. |
|
| Cohort study | B-Vitamin Intake, One-Carbon Metabolism, and Survival in a Population-Based Study of Women with Breast Cancer [68]. |
|
| (f). Vitamin B2 | ||
| Study type | Title | Findings |
| Cohort study | Dietary B-Vitamin Intake and Risk of Breast, Endometrial, Ovarian and Colorectal Cancer among Canadians [70]. |
|
| Case-control study | Nutrient Patterns and Risk of Breast Cancer among Iranian Women: a Case–Control Study [69]. |
|
| Meta-analysis | Dietary vitamin B2 intake and breast cancer risk: a systematic review and meta-analysis [71]. |
|
| (g). Vitamin C | ||
| Study type | Title | Findings |
| Cohort study | Vitamin C intake from diary recordings and risk of breast cancer in the UK Dietary Cohort Consortium [72]. |
|
| Case-control study | Raw and Cooked Vegetables, Fruits, Selected Micronutrients, and Breast Cancer Risk: A Case–Control Study in Germany [59]. |
|
| Cohort study | Dietary fiber, vitamins A, C, and E, and risk of breast cancer: a cohort study [73]. |
|
| (h). Zinc | ||
| Study type | Title | Findings |
| Prospective nested case-control study | Serum zinc and dietary intake of zinc in relation to risk of different breast cancer subgroups and serum levels as a marker of intake: a prospective nested case-control study [74]. |
|
| Case-control study | Raw and Cooked Vegetables, Fruits, Selected Micronutrients, and Breast Cancer Risk: A Case–Control Study in Germany [59]. |
|
| Meta-analysis | A meta-analysis of zinc levels in breast cancer [75]. |
|
| (i). Vitamin B6 | ||
| Study type | Title | Findings |
| Nested case-control study | Plasma Folate, Vitamin B6, Vitamin B12, Homocysteine, and Risk of Breast Cancer [76]. |
|
| Nested case-control study | Association of vitamin B6, vitamin B12 and methionine with risk of breast cancer: a dose–response meta-analysis [46]. |
|
| Meta-analysis | Folate, Vitamin B6, and Vitamin B12 Intake and the Risk of Breast Cancer Among Mexican Women [77]. |
|
| (j). Folate | ||
| Study type | Title | Findings |
| Case-control study | Raw and Cooked Vegetables, Fruits, Selected Micronutrients, and Breast Cancer Risk: A Case–Control Study in Germany [59]. |
|
| Meta-analysis | Higher dietary folate intake reduces the breast cancer risk: a systematic review and meta-analysis [78]. |
|
| Meta-analysis | Folate, Vitamin B6, and Vitamin B12 Intake and the Risk of Breast Cancer Among Mexican Women [77]. |
|
| (k). Vitamin E | ||
| Study type | Title | Findings |
| Meta-analysis | Retinol, vitamins A, C, and E and breast cancer risk: a meta-analysis and meta-regression [6]. |
|
| Case-control study | Raw and Cooked Vegetables, Fruits, Selected Micronutrients, and Breast Cancer Risk: A Case–Control Study in Germany [59]. |
|
| (l). Cholesterol | ||
| Study type | Title | Findings |
| Cohort study | Dietary Factors and Female Breast Cancer Risk: A Prospective Cohort Study [79]. |
|
| Case-control study | Dietary cholesterol intake and cancer [80]. |
|
| Meta-analysis | Updating the role of obesity and cholesterol in breast cancer [81]. |
|
Author Contributions
Conceptualization, H.S. and A.J.; formal analysis, H.S., A.J. and B.P.; data curation, H.S., A.J. and B.P.; writing—original draft preparation, H.S., A.J., T.X.M.T., J.L., M.K. and B.P.; writing—review and editing, H.S., A.J., T.X.M.T., J.L., M.K. and B.P.; visualization, H.S. and A.J.; supervision, M.K. and B.P.; validation, M.K.; investigation, T.X.M.T.; methodology, T.X.M.T.; project administration, H.S. and A.J.; resources, J.L.; software, J.L; funding acquisition, B.P. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Hanyang University College of Medicine, Republic of Korea (approval no. HYUIRB-202106-003-1).
Informed Consent Statement
Not applicable.
Data Availability Statement
The data underlying the results of out study are not publicly available because of KoGES data policy. Data are available from the Division of Genetic Epidemiology and Health Index, Korea Center for Disease Control and Prevention, for researchers who meet the criteria for access to confidential data.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was supported by a National Research Foundation of Korea grant funded by the South Korean government (grant number 2021R1A2C1011958).
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sung H., Ferlay J., Siegel R.L., Laversanne M., Soerjomataram I., Jemal A., Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Hong S., Won Y.J., Lee J.J., Jung K.W., Kong H.J., Im J.S., Seo H.G. The Community of Population-Based Regional Cancer Registries Cancer Statistics in Korea: Incidence, Mortality, Survival, and Prevalence in 2018. Cancer Res. Treat. 2021;53:301–315. doi: 10.4143/crt.2021.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McPherson K., Steel C., Dixon J. Breast cancer—epidemiology, risk factors, and genetics. Bmj. 2000;321:624–628. doi: 10.1136/bmj.321.7261.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomson C.A. Diet and breast cancer: Understanding risks and benefits. Nutr. Clin. Pract. 2012;27:636–650. doi: 10.1177/0884533612454302. [DOI] [PubMed] [Google Scholar]
- 5.Velie E.M., Schairer C., Flood A., He J.-P., Khattree R., Schatzkin A. Empirically derived dietary patterns and risk of postmenopausal breast cancer in a large prospective cohort study. Am. J. Clin. Nutr. 2005;82:1308–1319. doi: 10.1093/ajcn/82.6.1308. [DOI] [PubMed] [Google Scholar]
- 6.Fulan H., Changxing J., Baina W.Y., Wencui Z., Chunqing L., Fan W., Dandan L., Dianjun S., Tong W., Da P., et al. Retinol, vitamins A, C, and E and breast cancer risk: A meta-analysis and meta-regression. Cancer Causes Control. 2011;22:1383–1396. doi: 10.1007/s10552-011-9811-y. [DOI] [PubMed] [Google Scholar]
- 7.Xiao Y., Ke Y., Wu S., Huang S., Li S., Lv Z., Yeoh E.-K., Lao X., Wong S., Kim J.H., et al. Association between whole grain intake and breast cancer risk: A systematic review and meta-analysis of observational studies. Nutr. J. 2018;17:87. doi: 10.1186/s12937-018-0394-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghoncheh M., Mahdavifar N., Darvishi E., Salehiniya H. Epidemiology, incidence and mortality of breast cancer in Asia. Asian Pac. J. Cancer Prev. 2016;17:47–52. doi: 10.7314/APJCP.2016.17.S3.47. [DOI] [PubMed] [Google Scholar]
- 9.Turner L.B. A meta-analysis of fat intake, reproduction, and breast cancer risk: An evolutionary perspective. Am. J. Hum. Biol. 2011;23:601–608. doi: 10.1002/ajhb.21176. [DOI] [PubMed] [Google Scholar]
- 10.Prentice R.L., Caan B., Chlebowski R.T., Patterson R., Kuller L.H., Ockene J.K., Margolis K.L., Limacher M.C., Manson J.E., Parker L.M., et al. Low-Fat dietary pattern and risk of invasive breast cancer: The women’s health initiative randomized controlled dietary modification trial. Jama. 2006;295:629–642. doi: 10.1001/jama.295.6.629. [DOI] [PubMed] [Google Scholar]
- 11.Anderson J.J., Darwis N.D., Mackay D.F., Celis-Morales C.A., Lyall D.M., Sattar N., Gill J.M., Pell J.P. Red and processed meat consumption and breast cancer: UK Biobank cohort study and meta-analysis. Eur. J. Cancer. 2017;90:73–82. doi: 10.1016/j.ejca.2017.11.022. [DOI] [PubMed] [Google Scholar]
- 12.Farvid M.S., Stern M.C., Norat T., Sasazuki S., Vineis P., Weijenberg M.P., Wolk A., Wu K., Stewart B.W., Cho E. Consumption of red and processed meat and breast cancer incidence: A systematic review and meta-analysis of prospective studies. Int. J. Cancer. 2018;143:2787–2799. doi: 10.1002/ijc.31848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aune D., Chan D.S.M., Vieira A.R., Rosenblatt D.A.N., Vieira R., Greenwood D.C., Norat T. Fruits, vegetables and breast cancer risk: A systematic review and meta-analysis of prospective studies. Breast Cancer Res. Treat. 2012;134:479–493. doi: 10.1007/s10549-012-2118-1. [DOI] [PubMed] [Google Scholar]
- 14.Masala G., Assedi M., Bendinelli B., Ermini I., Sieri S., Grioni S., Sacerdote C., Ricceri F., Panico S., Mattiello A., et al. Fruit and vegetables consumption and breast cancer risk: The EPIC Italy study. Breast Cancer Res. Treat. 2012;132:1127–1136. doi: 10.1007/s10549-011-1939-7. [DOI] [PubMed] [Google Scholar]
- 15.Dong J.Y., Qin L.Q. Soy isoflavones consumption and risk of breast cancer incidence or recurrence: A meta-analysis of prospective studies. Breast Cancer Res. Treat. 2011;125:315–323. doi: 10.1007/s10549-010-1270-8. [DOI] [PubMed] [Google Scholar]
- 16.Wu A.H., Yu M.C., Tseng C.-C., Pike M.C. Epidemiology of soy exposures and breast cancer risk. Br. J. Cancer. 2008;98:9–14. doi: 10.1038/sj.bjc.6604145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Xiao Y., Xia J., Li L., Ke Y., Cheng J., Xie Y., Chu W., Cheung P., Kim J.H., Colditz G.A., et al. Associations between dietary patterns and the risk of breast cancer: A systematic review and meta-analysis of observational studies. Breast Cancer Res. 2019;21:16. doi: 10.1186/s13058-019-1096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cuenca-Micó O., Aceves C. Micronutrients and Breast Cancer Progression: A Systematic Review. Nutrients. 2020;12:3613. doi: 10.3390/nu12123613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Woo H.D., Park S., Oh K., Kim H.J., Shin H.R., Moon H.K., Kim J. Diet and Cancer Risk in the Korean Population: A Meta-analysis. Asian Pac. J. Cancer Prev. 2014;15:8509–8519. doi: 10.7314/APJCP.2014.15.19.8509. [DOI] [PubMed] [Google Scholar]
- 20.Kim Y., Han B.G. Cohort Profile: The Korean Genome and Epidemiology Study (KoGES) Consortium. Int. J. Epidemiol. 2017;46:e20. doi: 10.1093/ije/dyv316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Group H.E.S. The Health Examinees (HEXA) study: Rationale, study design and baseline characteristics. Asian Pac. J. Cancer Prev. APJCP. 2015;16:1591–1597. doi: 10.7314/apjcp.2015.16.4.1591. [DOI] [PubMed] [Google Scholar]
- 22.Wee J.H., Min C., Park M.W., Byun S.H., Lee H.-J., Park B., Choi H.G. The association of asthma and its subgroups with osteoporosis: A cross-sectional study using KoGES HEXA data. Allergy Asthma Clin. Immunol. 2020;16:1–8. doi: 10.1186/s13223-020-00482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kwon O., Kim H., Kim J., Hwang J.-Y., Lee J., Yoon M.O. The development of the 2020 dietary reference intakes for Korean population: Lessons and challenges. J. Nutr. Health. 2021;54:425–434. doi: 10.4163/jnh.2021.54.5.425. [DOI] [Google Scholar]
- 24.Block G. Vitamin C and cancer prevention: The epidemiologic evidence. Am. J. Clin. Nutr. 1991;53:270S–282S. doi: 10.1093/ajcn/53.1.270S. [DOI] [PubMed] [Google Scholar]
- 25.Lutsenko E.A., Cárcamo J.M., Golde D.W. Vitamin C prevents DNA mutation induced by oxidative stress. J. Biol. Chem. 2002;277:16895–16899. doi: 10.1074/jbc.M201151200. [DOI] [PubMed] [Google Scholar]
- 26.Xu X., Yu E., Liu L., Zhang W., Wei X., Gao X., Song N., Fu C. Dietary intake of vitamins A, C, and E and the risk of colorectal adenoma: A meta-analysis of observational studies. Eur. J. Cancer Prev. 2013;22:529–539. doi: 10.1097/CEJ.0b013e328364f1eb. [DOI] [PubMed] [Google Scholar]
- 27.Li P., Zhang H., Chen J., Shi Y., Cai J., Yang J., Wu Y. Association between dietary antioxidant vitamins intake/blood level and risk of gastric cancer. Int. J. Cancer. 2014;135:1444–1453. doi: 10.1002/ijc.28777. [DOI] [PubMed] [Google Scholar]
- 28.Lam T.K., Freedman N.D., Fan J.-H., Qiao Y.-L., Dawsey S.M., Taylor P.R., Abnet C. Prediagnostic plasma vitamin C and risk of gastric adenocarcinoma and esophageal squamous cell carcinoma in a Chinese population. Am. J. Clin. Nutr. 2013;98:1289–1297. doi: 10.3945/ajcn.113.061267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bo Y., Lu Y., Zhao Y., Zhao E., Yuan L., Lu W., Cui L., Lu Q. Association between dietary vitamin C intake and risk of esophageal cancer: A dose-response meta-analysis. Int. J. Cancer. 2015;138:1843–1850. doi: 10.1002/ijc.29838. [DOI] [PubMed] [Google Scholar]
- 30.Bandera E.V., Gifkins D.M., Moore D.F., McCullough M.L., Kushi L.H. Antioxidant vitamins and the risk of endometrial cancer: A dose–response meta-analysis. Cancer Causes Control. 2008;20:699–711. doi: 10.1007/s10552-008-9283-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Luo J., Shen L., Zheng D. Association between vitamin C intake and lung cancer: A dose-response meta-analysis. Sci. Rep. 2014;4:6161. doi: 10.1038/srep06161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang D., Xu P., Li Y., Wei B., Yang S., Zheng Y., Lyu L., Deng Y., Zhai Z., Li N., et al. Association of vitamin C intake with breast cancer risk and mortality: A meta-analysis of observational studies. Aging. 2020;12:18415–18435. doi: 10.18632/aging.103769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hu F., Wu Z., Li G., Teng C., Liu Y., Wang F., Zhao Y., Pang D. The plasma level of retinol, vitamins A, C and α-tocopherol could reduce breast cancer risk? A meta-analysis and meta-regression. J. Cancer Res. Clin. Oncol. 2015;141:601–614. doi: 10.1007/s00432-014-1852-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Salminen E.K., Lagström H.K., Heikkilä S.P., Salminen S.J. Does breast cancer change patients’ dietary habits? Eur. J. Clin. Nutr. 2000;54:844–848. doi: 10.1038/sj.ejcn.1601103. [DOI] [PubMed] [Google Scholar]
- 35.Marseglia L., Manti S., D’Angelo G., Nicotera A.G., Parisi E., Di Rosa G., Gitto E., Arrigo T. Oxidative stress in obesity: A critical component in human diseases. Int. J. Mol. Sci. 2014;16:378–400. doi: 10.3390/ijms16010378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Morris P.G., Hudis C.A., Giri D., Morrow M., Falcone D.J., Zhou X.K., Du B., Brogi E., Crawford C.B., Kopelovich L., et al. Inflammation and increased aromatase expression occur in the breast tissue of obese women with breast cancer. Cancer Prev. Res. 2011;4:1021–1029. doi: 10.1158/1940-6207.CAPR-11-0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heath A.K., Muller D., Brandt P.A.V.D., Papadimitriou N., Critselis E., Gunter M., Vineis P., Weiderpass E., Fagherazzi G., Boeing H., et al. Nutrient-wide association study of 92 foods and nutrients and breast cancer risk. Breast Cancer Res. 2020;22:5. doi: 10.1186/s13058-019-1244-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schlueter A.K., Johnston C.S. Vitamin C: Overview and Update. J. Evid.-Based Complement. Altern. Med. 2011;16:49–57. doi: 10.1177/1533210110392951. [DOI] [Google Scholar]
- 39.Dehghan M., Akhtar-Danesh N., McMillan C.R., Thabane L. Is plasma vitamin C an appropriate biomarker of vitamin C intake? A systematic review and meta-analysis. Nutr. J. 2007;6:41. doi: 10.1186/1475-2891-6-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vioque J., Weinbrenner T., Asensio L., Castelló A., Young I.S., Fletcher A. Plasma concentrations of carotenoids and vitamin C are better correlated with dietary intake in normal weight than overweight and obese elderly subjects. Br. J. Nutr. 2007;97:977–986. doi: 10.1017/S0007114507659017. [DOI] [PubMed] [Google Scholar]
- 41.Selhub J. Folate, vitamin B12 and vitamin B6 and one carbon metabolism. J. Nutr. Health Aging. 2002;6:39–42. [PubMed] [Google Scholar]
- 42.Ames B.N. DNA damage from micronutrient deficiencies is likely to be a major cause of cancer. Mutat. Res. Mol. Mech. Mutagen. 2001;475:7–20. doi: 10.1016/S0027-5107(01)00070-7. [DOI] [PubMed] [Google Scholar]
- 43.Mocellin S., Briarava M., Pilati P. Vitamin B6 and Cancer Risk: A Field Synopsis and Meta-Analysis. JNCI: J. Natl. Cancer Inst. 2016;109 doi: 10.1093/jnci/djw230. [DOI] [PubMed] [Google Scholar]
- 44.Larsson S.C., Orsini N., Wolk A. Vitamin B6 and Risk of Colorectal Cancer: A Meta-analysis of Prospective Studies. JAMA. 2010;303:1077–1083. doi: 10.1001/jama.2010.263. [DOI] [PubMed] [Google Scholar]
- 45.Wei D.-H., Mao Q.-Q. Vitamin B6, vitamin B12 and methionine and risk of pancreatic cancer: A meta-analysis. Nutr. J. 2020;19:111. doi: 10.1186/s12937-020-00628-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu W., Kang S., Zhang D. Association of vitamin B6, vitamin B12 and methionine with risk of breast cancer: A dose-response meta-analysis. Br. J. Cancer. 2013;109:1926–1944. doi: 10.1038/bjc.2013.438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zeng J., Gu Y., Fu H., Liu C., Zou Y., Chang H. Association Between one-carbon metabolism-related vitamins and risk of breast cancer: A systematic review and meta-analysis of prospective studies. Clin. Breast Cancer. 2020;20:e469–e480. doi: 10.1016/j.clbc.2020.02.012. [DOI] [PubMed] [Google Scholar]
- 48.Clasen J.L., Heath A.K., Van Puyvelde H., Huybrechts I., Park J.Y., Ferrari P., Johansson M., Scelo G., Ulvik A., Midttun Ø., et al. A comparison of complementary measures of vitamin B6 status, function, and metabolism in the European Prospective Investigation into Cancer and Nutrition (EPIC) study. Am. J. Clin. Nutr. 2021;114:338–347. doi: 10.1093/ajcn/nqab045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Moreno-Navarrete J.M., Jove M., Ortega F., Xifra G., Ricart W., Obis È., Pamplona R., Portero-Otin M., Fernández-Real J.M. Metabolomics uncovers the role of adipose tissue PDXK in adipogenesis and systemic insulin sensitivity. Diabetologia. 2016;59:822–832. doi: 10.1007/s00125-016-3863-1. [DOI] [PubMed] [Google Scholar]
- 50.Merigliano C., Mascolo E., Burla R., Saggio I., Vernì F. The relationship between vitamin B6, diabetes and cancer. Front. Genet. 2018;9:388. doi: 10.3389/fgene.2018.00388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ahn Y., Kwon E., Shim J.E., Park M.K., Joo Y., Kimm K., Park C., Kim D.H. Validation and reproducibility of food frequency questionnaire for Korean genome epidemiologic study. Eur. J. Clin. Nutr. 2007;61:1435–1441. doi: 10.1038/sj.ejcn.1602657. [DOI] [PubMed] [Google Scholar]
- 52.Cho S., Shin A., Song D., Park J.K., Kim Y., Choi J.-Y., Kang D., Lee J.-K. Validity of self-reported cancer history in the health examinees (HEXA) study: A comparison of self-report and cancer registry records. Cancer Epidemiol. 2017;50:16–21. doi: 10.1016/j.canep.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 53.Key T.J., Balkwill A., Bradbury K., Reeves G.K., Kuan A.S., Simpson R.F., Green J., Beral V. Foods, macronutrients and breast cancer risk in postmenopausal women: A large UK cohort. Int. J. Epidemiol. 2018;48:489–500. doi: 10.1093/ije/dyy238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.World Cancer Research Fund International/American Institute for Cancer Research Continuous Update Project Report: Diet, Nutrition, Physical Activity and Breast Cancer. 2017. [(accessed on 20 February 2022)]. Available online: Wcrf.org/breast-cancer-2017.
- 55.Hunter D.J., Willett W.C. Nutrition and breast cancer. Cancer Causes Control. 1996;7:56–68. doi: 10.1007/BF00115638. [DOI] [PubMed] [Google Scholar]
- 56.Li J., Koh W.-P., Jin A.-Z., Yuan J.-M., Yu M.C., Butler L.M. Calcium intake is not related to breast cancer risk among Singapore Chinese women. Int. J. Cancer. 2013;133:680–686. doi: 10.1002/ijc.28027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zhang C.-X., Ho S.C., Fu J.-H., Cheng S.-Z., Chen Y.-M., Lin F.-Y. Dairy products, calcium intake, and breast cancer risk: A Case-Control study in China. Nutr. Cancer. 2010;63:12–20. doi: 10.1080/01635581.2010.516478. [DOI] [PubMed] [Google Scholar]
- 58.Chen P., Hu P., Xie D., Qin Y., Wang F., Wang H. Meta-analysis of vitamin D, calcium and the prevention of breast cancer. Breast Cancer Res. Treat. 2009;121:469–477. doi: 10.1007/s10549-009-0593-9. [DOI] [PubMed] [Google Scholar]
- 59.Adzersen K.-H., Jess P., Freivogel K.W., Gerhard I., Bastert G. Raw and cooked vegetables, fruits, selected micronutrients, and breast cancer risk: A Case-Control study in Germany. Nutr. Cancer. 2003;46:131–137. doi: 10.1207/S15327914NC4602_05. [DOI] [PubMed] [Google Scholar]
- 60.Park B., Lee J., Kim J. Imbalanced nutrient intake in cancer survivors from the examination from the nationwide health examination Center-Based cohort. Nutrients. 2018;10:212. doi: 10.3390/nu10020212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tayyem R.F., Mahmoud R.I., Marei L.S., Oncologist K.H.C.C.M. The Intake of Some Nutrients is Associated with the Risk of Breast Cancer: Results from Jordanian Case-Control Study. Curr. Res. Nutr. Food Sci. J. 2020;8:12–24. doi: 10.12944/CRNFSJ.8.1.02. [DOI] [Google Scholar]
- 62.Kabat G.C., Miller A.B., Jain M., Rohan T.E. Dietary iron and heme iron intake and risk of breast cancer: A prospective cohort study. Cancer Epidemiol. Biomark. Prev. 2007;16:1306–1308. doi: 10.1158/1055-9965.EPI-07-0086. [DOI] [PubMed] [Google Scholar]
- 63.Ronco A.L., Espinosa E., Calderón J.M. A case-control study on heme/non-heme iron and breast cancer risk. Ann. Clin. Nutr. 2018;3:1011. [Google Scholar]
- 64.Chang V.C., Cotterchio M., Khoo E. Iron intake, body iron status, and risk of breast cancer: A systematic review and meta-analysis. BMC Cancer. 2019;19:543. doi: 10.1186/s12885-019-5642-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hunter D.J., Manson J.E., Colditz G.A., Stampfer M.J., Rosner B., Hennekens C.H., Speizer F.E., Willett W.C. A prospective study of the intake of vitamins C, E, and A and the risk of breast cancer. N. Engl. J. Med. 1993;329:234–240. doi: 10.1056/NEJM199307223290403. [DOI] [PubMed] [Google Scholar]
- 66.Longnecker M., Newcomb P.A., Mittendorf R., Greenberg E.R., Willett W.C. Intake of carrots, spinach, and supplements containing vitamin A in relation to risk of breast cancer. Cancer Epidemiol. Biomark. Prev. 1997;6:887–892. [PubMed] [Google Scholar]
- 67.He J., Gu Y., Zhang S. Vitamin A and breast cancer survival: A systematic review and meta-analysis. Clin. Breast Cancer. 2018;18:e1389–e1400. doi: 10.1016/j.clbc.2018.07.025. [DOI] [PubMed] [Google Scholar]
- 68.Egnell M., Fassier P., Lécuyer L., Zelek L., Vasson M.-P., Hercberg S., Latino-Martel P., Galan P., Deschasaux M., Touvier M. B-vitamin intake from diet and supplements and breast cancer risk in middle-aged women: Results from the prospective NutriNet-Santé cohort. Nutrients. 2017;9:488. doi: 10.3390/nu9050488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Fereidani S.S., Eini-Zinab H., Heidari Z., Jalali S., Sedaghat F., Rashidkhani B. Nutrient patterns and risk of breast cancer among Iranian women: A case- control study. Asian Pac. J. Cancer Prev. 2018;19:2619–2624. doi: 10.22034/APJCP.2018.19.9.2619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Arthur R.S., Kirsh V.A., Rohan T.E. Dietary B-Vitamin intake and risk of breast, endometrial, ovarian and colorectal cancer among Canadians. Nutr. Cancer. 2019;71:1067–1077. doi: 10.1080/01635581.2019.1597904. [DOI] [PubMed] [Google Scholar]
- 71.Yu L., Tan Y., Zhu L. Dietary vitamin B2 intake and breast cancer risk: A systematic review and meta-analysis. Arch. Gynecol. Obstet. 2016;295:721–729. doi: 10.1007/s00404-016-4278-4. [DOI] [PubMed] [Google Scholar]
- 72.Hutchinson J., Lentjes M.A., Greenwood D.C., Burley V.J., Cade J.E., Cleghorn C.L., Threapleton D.E., Key T.J., Cairns B.J., Keogh R.H., et al. Vitamin C intake from diary recordings and risk of breast cancer in the UK Dietary Cohort Consortium. Eur. J. Clin. Nutr. 2011;66:561–568. doi: 10.1038/ejcn.2011.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Rohan T.E., Howe G.R., Friedenreich C.M., Jain M., Miller A.B. Dietary fiber, vitamins A, C, and E, and risk of breast cancer: A cohort study. Cancer Causes Control. 1993;4:29–37. doi: 10.1007/BF00051711. [DOI] [PubMed] [Google Scholar]
- 74.Bengtsson Y., Sandsveden M., Borgquist S., Manjer J. Serum zinc and dietary intake of zinc in relation to risk of different breast cancer subgroups and serum levels as a marker of intake: A prospective nested case-control study. Breast Cancer Res. Treat. 2021;189:571–583. doi: 10.1007/s10549-021-06318-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jouybari L., Kiani F., Akbari A., Sanagoo A., Sayehmiri F., Aaseth J., Chartrand M.S., Sayehmiri K., Chirumbolo S., Bjørklund G. A meta-analysis of zinc levels in breast cancer. J. Trace Elem. Med. Biol. 2019;56:90–99. doi: 10.1016/j.jtemb.2019.06.017. [DOI] [PubMed] [Google Scholar]
- 76.Zhang S.M., Willett W.C., Selhub J., Hunter D.J., Giovannucci E.L., Holmes M.D., Colditz G.A., Hankinson S.E. Plasma folate, vitamin B6, vitamin B12, homocysteine, and risk of breast cancer. J. Natl. Cancer Inst. 2003;95:373–380. doi: 10.1093/jnci/95.5.373. [DOI] [PubMed] [Google Scholar]
- 77.Lajous M., Lazcano-Ponce E., Hernandez-Avila M., Willett W., Romieu I. Folate, Vitamin B6, and Vitamin B12 intake and the risk of breast cancer among Mexican women. Cancer Epidemiol. Biomark. Prev. 2006;15:443–448. doi: 10.1158/1055-9965.EPI-05-0532. [DOI] [PubMed] [Google Scholar]
- 78.Chen P., Li C., Li X., Li J., Chu R., Wang H. Higher dietary folate intake reduces the breast cancer risk: A systematic review and meta-analysis. Br. J. Cancer. 2014;110:2327–2338. doi: 10.1038/bjc.2014.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Kim J.H., Lee J., Jung S.Y., Kim J. Dietary factors and female breast cancer risk: A prospective cohort study. Nutrients. 2017;9:1331. doi: 10.3390/nu9121331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Hu J., La Vecchia C., de Groh M., Negri E., Morrison H., Mery L. Dietary cholesterol intake and cancer. Ann. Oncol. 2011;23:491–500. doi: 10.1093/annonc/mdr155. [DOI] [PubMed] [Google Scholar]
- 81.Garcia-Estevez L., Moreno-Bueno G. Updating the role of obesity and cholesterol in breast cancer. Breast Cancer Res. 2019;21:35. doi: 10.1186/s13058-019-1124-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying the results of out study are not publicly available because of KoGES data policy. Data are available from the Division of Genetic Epidemiology and Health Index, Korea Center for Disease Control and Prevention, for researchers who meet the criteria for access to confidential data.