Abstract
Vasomotor symptoms (VMS) are the most common symptoms among menopausal women; these include hot flashes and night sweats, and palpitations often occur along with hot flashes. Some studies in Mexico reported that around 50% of women presented with VMS mainly in the menopausal transition. It has been proven that VMS are not only triggered by an estrogen deficiency, but also by nutritional risk factors. Evidence of an association between nutritional risk factors and VMS is limited in Mexican women. The aim of this study is to identify nutritional risk factors associated with VMS in women aged 40–65 years. This is a comparative cross-sectional study, undertaken in a retrospective way. A sample group (n = 406 women) was divided into four stages according to STRAW+10 (Stages of Reproductive Aging Workshop): late reproductive, menopausal transition, early postmenopause, and late postmenopause. Hot flashes were present mainly in the early postmenopause stage (38.1%, p ≤ 0.001). Two or more VMS were reported in 23.2% of women in the menopausal transition stage and 29.3% in the early postmenopause stage (p < 0.001). The presence of VMS was associated with different nutritional risk factors (weight, fasting glucose levels, cardiorespiratory fitness, and tobacco use) in women living in the northeast of Mexico.
Keywords: vasomotor symptoms, risk factors, reproductive aging, menopause, women, Mexico
1. Introduction
Vasomotor symptoms (VMS) are the most common symptoms among menopausal women. These symptoms are short-term menopausal disorders, which include hot flashes and night sweats [1,2], and are often accompanied by palpitations [2]. According to STRAW+10 (Stages of Reproductive Aging Workshop) criteria, which is a “gold standard” that classifies women into stages of reproductive aging, VMS can appear in late menopausal transition but are more common in the early postmenopause [3,4]. Some studies in Mexico reported that VMS in women appear mainly in the menopausal transition, with a prevalence of 45% in women aged 45–55 years [5] and 47.63% in women aged 51–63 years [6].
It has been proven that VMS are not only triggered by estrogen deficiency, but also by different nutritional risk factors that can be modifiable and non-modifiable. Clinical practice guidelines for the menopausal stage [7,8,9], along with several other studies, delimitate that a body mass index higher or equal to 25, hypertension, and tobacco use are nutritional risk factors for VMS [10,11,12]. Their mechanism seems to relate to impaired heat conductance, blood flow, and hormones [12,13]. However, there is limited evidence concerning other factors such as fasting glucose ≥100 mg/dL, poor cardiorespiratory fitness, and excessive total fat intake.
There is also limited evidence concerning the nutritional factors associated with VMS in Mexican women. In Mexico, the prevalence of VMS has been reported but the associated risk factors have not [5,6]. A previous study has evaluated the social and nutritional factors associated with menopausal symptoms in Mexican women; however, there was no distinction of VMS, as nine different symptoms were arranged into one climacteric group [14]. These studies were carried out in central Mexico and there is limited evidence for the northeast region. The aim of this study is to identify nutritional risk factors associated with VMS in women aged 40–65 years in northeast Mexico.
2. Materials and Methods
2.1. Design and Subjects
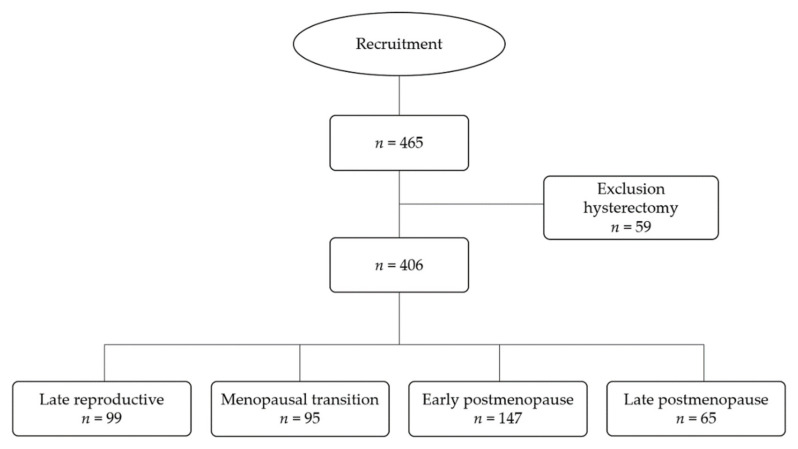
This is a cross-sectional study which was carried out from 2015 to 2017. Women enrolled in this study were 40–65 years of age, living in the metropolitan area of Monterrey, in Nuevo León state, Mexico. They were apparently healthy, they voluntarily agreed to participate, and all provided written informed consent. Exclusion criteria included illnesses that affected their habitual eating habits and having undergone a hysterectomy. Women with incomplete data were eliminated from the study analysis (Figure 1). A total of n = 406 women were included in the study, representative of the study population (560,115 women aged 40–65 years) of Nuevo León state in the year 2020. This was according to a finite population equation, with 5% error and 95% confidence intervals, considering a VMS proportion of 50% [15].
Figure 1.
Flowchart of the recruitment of the study population.
Women were invited to participate via physical flyers and social media. They were screened for the inclusion criteria via a telephone call and scheduled for an appointment at the Center for Research in Nutrition and Public Health of the Facultad de Salud Pública y Nutrición, Universidad Autónoma de Nuevo León (School of Public Health and Nutrition, Autonomous University of Nuevo León, translated into English).
This study followed the Declaration of Helsinki, and it was approved by the ethics committee of the Facultad de Salud Pública y Nutrición with protocol ID: 15–FaSPyN–SA–11.
2.2. Stages of Reproductive Aging (STRAW+10 Criteria)
A questionnaire was used to obtain data on menstrual cycles, including previous menstrual period, presence of blood flow or amenorrhea, and changes in length between cycles. According to the STRAW+10 criteria [3], women were classified into 4 stages of reproductive aging (Figure 1). Late reproductive was defined as “the presence of blood flow without changes or with short cycles.” Menopausal transition was defined as “the presence of blood flow with long cycles or with at least one interval of amenorrhea ≥60 days,” “amenorrhea <60 days and without changes,” or “amenorrhea ≥60 days.” Early postmenopause was defined as “amenorrhea ≥12 months, but ≤8 years,” and late postmenopause was defined as “amenorrhea >8 years” [3].
2.3. Vasomotor Symptoms
Vasomotor symptoms (VMS) were reported in a questionnaire and included hot flashes and night sweats. Palpitations were also registered, as they are often present along with hot flashes [2]. Women had the option to answer yes (presence) or no (absence). After the information was collected, 4 categories were established: (1) absence, (2) presence of hot flashes, (3) presence of night sweats or palpitations, and (4) presence of 2 or more VMS, including hot flashes, night sweats, and palpitations.
2.4. Nutrition Assessment
A nutrition assessment of participants was performed according to the Nutrition Care Process of the Academy of Nutrition and Dietetics [16] as follows:
2.4.1. Anthropometric Measurements
Body mass index (BMI) was determined by the formula BMI = weight (kg)/height2 (m2), using a scale (Seca 874, ± 0.1 kg, Azcapotzalco, Mexico) for the weight and a digital stadiometer (Seca 274, ± 2 mm, Azcapotzalco, Mexico) for the height. BMI was classified as obese ≥30 kg/m2, overweight 25–29.9 kg/m2, or normal weight 18.5–24.9 kg/m2 [17].
2.4.2. Biochemical Data
Venous blood samples were collected at fast, centrifuged at 3500 rpm for 12 min, and serum was obtained. The serum was frozen at −80 °C until assays were performed with the glucose oxidase/peroxidase method. Fasting glucose was obtained using A25 autoanalyzer (software version 4.1.1) (CV = 1.2%) (BioSystems S.A, Barcelona, Spain), according to the Norma Oficial Mexicana NOM–253–SSA1–2012 [9]. Fasting glucose was classified as high ≥100 mg/dL or normal <100 mg/dL [18]. Women on treatments using hypoglycemic drugs were also considered to have high fasting glucose levels.
2.4.3. Nutrition-Focused Physical Exam Findings
Systolic and diastolic blood pressure measurements were performed to the nearest 1 mmHg using a digital sphygmomanometer, according to the Norma Oficial Mexicana NOM–030–SSA2–2009 [19]. Two readings were taken 5 min apart and the average was calculated. Blood pressure was classified as hypertensive between ≥130 and ≥80 mmHg, elevated between 120–129 and <80 mmHg, or normal between <120 and <80 mmHg [20]. Women on treatments using antihypertensive drugs were considered to be hypertensive.
The cardiorespiratory fitness (CF) of the women was obtained by measuring the walking distance achieved in meters (m) during a six-minute (min) test, in a 15 m × 28 m field. The CF value was reported as meters per minute, using the formula CF = m/6 min. CF was determined as poor at <400 m/6 min or excellent at ≥400 m/6 min [21].
2.4.4. Food and Nutrition-Related History
Total fat intake was assessed by a validated Food Frequency Questionnaire (FFQ) [22]. Women were asked to report the frequency and measurements of their intake of 136 items, including foods and beverages. Total fat and energy intake was analyzed using the software Food Processor® version 15.0 (ESHA Research, Salem, OR, USA) and was reported in grams per day (g/day) [23].
2.4.5. Covariates
Women also reported tobacco use (yes or no), hormone use (yes or no), and date of birth to determine age (years). Daily physical activity was obtained from the Minnesota leisure-time physical activity (LTPA) questionnaire, in which women reported the frequency and time spent in different activities. Metabolic equivalents per day (MET/d) were calculated [24]. Intake of alcohol in milliliters per day (mL/day), and caffeine in milligrams per day (mg/d), was also analyzed from the FFQ answers (see Section 2.4.4).
2.5. Statistical Analysis
Data were analyzed for normality using the Kolmogorov–Smirnov test. Differences between groups (stages of reproductive aging) were determined using a chi-square test with the Marascuilo procedure to establish the categorical variables. The Kruskal–Wallis test with the Bonferroni adjustment was also used to determine the numerical variables (post hoc test). The presence of VMS in the 4 categories (absence of VMS, presence of hot flashes, presence of night sweats or palpitations, and presence of 2 or more VMS) were reported in frequency and percentage. Differences among categories were determined using a chi-square test with the Marascuilo procedure (post hoc test).
The dependent variable was the presence of VMS in the 4 categories (yes or no). Independent variables included BMI (obese ≥ 30 kg/m2, overweight 25–29.9 kg/m2, and normal 18.5–24.9 kg/m2), fasting glucose (high ≥100 mg/dL or normal <100 mg/dL), blood pressure (hypertensive between ≥130 and ≥80 mmHg, elevated between 120–129 and <80 mmHg, or normal between <120 and <80 mmHg), cardiorespiratory fitness (poor at <400 m/6 min or excellent at ≥400 m/6 min), total fat intake (excessive >30% from total kcal/d or adequate ≤30% from total kcal/d), and tobacco use (yes or no).
A multivariate logistic regression model was used to define statistical models of the nutritional factors (independent variables) associated with VMS (dependent variable). Odds ratios (OR) with 95% confidence intervals (95% CI) were calculated. Several models were proposed: an unadjusted model (Model 1); an adjusted model (Model 2) including covariates (age (years), hormone use (yes or no), and daily physical activity (MET/day)); and an adjusted model (Model 3) including covariates (stage of reproductive aging (late reproductive, menopausal transition, early postmenopause, or late postmenopause), hormone use (yes or no), daily physical activity (MET/d), alcohol intake (mL/day), and caffeine intake (mg/day)) [25,26,27]. Model 2 was adjusted to include age as a covariate because VMS follows a natural pattern according to lifespan [28]. Model 3 was adjusted to include the stage of reproductive aging because VMS can be present at different stages [4].
Prevalence ratios (PR) were calculated using the following formulas, derived from calculated odds ratios (OR) as previously proposed [29,30], where p1 is the prevalence of VMS in the reference group and z is the coefficient of regression divided by its standard error.
| (1) |
| (2) |
A p value of <0.05 was considered to be statistically significant. All analyses were performed using IBM SPSS® Statistics software, SPSS Inc., Chicago, IL, USA (version 25).
3. Results
Table 1 compares the descriptive characteristics in women grouped by stages of reproductive aging. A total of 24.4% of women were in the late reproductive stage, 23.4% were in menopausal transition, 36.2% were in early postmenopause, and 16.0% were in late postmenopause. The age of menopause was 48.6 years in women at the early postmenopause stage (n = 147) and 43.4 years in women in the late postmenopause stage (n = 65), while the average menopausal age (n = 212) was 47.0 years (data not shown).
Table 1.
Descriptive characteristics of women aged 40–65 years grouped according to STRAW+10.
| Late Reproductive | Menopausal Transition | Early Postmenopause | Late Postmenopause | p | |
|---|---|---|---|---|---|
| Number of women, n (%) | 99 (24.4) | 95 (23.4) | 147 (36.2) | 65 (16.0) | |
| Age, years | <0.001 | ||||
| Mean ± SD | 44.6 ± 3.3 a | 47.4 ± 3.5 b | 52.6 ± 4.1 c | 56.4 ± 4.0 d | |
| Median (Q1, Q3) | 44.0 (42.0, 47.0) | 48.0 (45.0, 50.0) | 52.0 (50.0, 55.0) | 53.0 (57.0, 59.0) | |
| Drug treatment, n (%) | |||||
| Hormonal | 7 (7.1) | 11 (11.6) | 13 (8.8) | 7 (10.8) | 0.715 |
| Hypoglycemic | 5 (5.1) | 8 (8.4) | 20 (13.6) | 7 (10.8) | 0.159 |
| Antihypertensive | 9 (9.1) | 10 (10.5) | 21 (14.3) | 15 (23.1) | 0.057 |
| BMI, kg/m2 | 0.018 | ||||
| Mean ± SD | 27.9 ± 5.4 a | 30.6 ± 6.7 b | 29.5 ± 5.6 ab | 30.1 ± 5.7 ab | |
| Median (Q1, Q3) | 27.6 (23.6, 31.1) | 29.9 (25.2, 33.9) | 28.1 (25.5, 32.8) | 29.4 (25.8, 34.5) | |
| Fasting glucose, mg/dL | 0.002 | ||||
| Mean ± SD | 95.4 ± 32.4 a | 97.5 ± 20.3 ab | 105.1 ± 37.6 b | 105.5 ± 33.3 b | |
| Median (Q1, Q3) | 91.0 (84.0, 99.0) | 95.0 (85.0, 103.0) | 98.0 (87.0, 108.0) | 98.0 (89.0, 111.5) | |
|
Blood pressure, mmHg Systolic Mean ± SD Median (Q1, Q3) Diastolic Mean ± SD Median (Q1, Q3) |
113.3 ± 15.0 a 110.5 (102.0, 119.5) a 72.4 ± 11.4 72.0 (65.0, 78.5) |
114.9 ± 13.3 a 114.0 (103.0, 123.5) 73.5 ± 10.0 73.5 (65.5, 82.5) |
118.2 ± 17.2 ab 115.0 (107.0, 126.5) 73.4 ± 12.1 73.0 (66.5, 81.5) |
121.1 ± 13.7 b 122.5 (111.5, 131.5) 72.9 ± 11.0 73.0 (65.0, 80.5) |
0.001 0.862 |
|
Cardiorespiratory fitness, m/6 min Mean ± SD Median (Q1, Q3) |
549.4 ± 69.0 544.3 (510.1, 601.5) |
559.8 ± 70.0 551.9 (513.8, 596.1) |
551.3 ± 85. 6 559.0 (507.6, 604.1) |
553.3 ± 67.9 541.5 (517.9, 603.4) |
0.877 |
| Total fat intake, %/d | 0.039 | ||||
| Mean ± SD | 36.9 ± 6.5 a | 36.6 ± 5.6 ab | 36.2 ± 5.9 ab | 34.3 ± 5.8 b | |
| Median (Q1, Q3) | 37.1 (33.0, 39.5) | 35.9 (32.6, 40.2) | 36.1 (32.0, 39.8) | 33.4 (30.2, 38.3) | |
| Tobacco use, n (%) | 6 (6.1) | 10 (10.5) | 12 (8.2) | 8 (12.3) | 0.507 |
BMI: body mass index; SD: standard deviation. Numerical data were analyzed using the Kruskal–Wallis test with the Bonferroni adjustment, and expressed as mean and standard deviation, and median and quartiles (Q1, Q3). Categorical data were analyzed using a chi-square test with the Marascuilo procedure, and expressed as cases and percentages, n (%). Superscripts a, b, c, d denote differences among groups. p < 0.05 denotes statistical significance.
There was a significant difference between stages of reproductive aging in terms of BMI (0.018), fasting glucose (p = 0.002), systolic blood pressure (p = 0.001), and total fat intake (p = 0.039). There were no differences between groups in cardiorespiratory fitness (p = 0.877) and tobacco use (p = 0.507). Women in the late reproductive stage showed a lower BMI (27.9 kg/m2), while women in menopausal transition presented a higher BMI (30.6 kg/m2). Fasting glucose was lower in women in the late reproductive stage (95.4 mg/dL) and highest in women in the late postmenopause stage (105.5 mg/dL). Women in the late postmenopause stage showed the highest systolic blood pressure (121.1 mmHg). Total fat intake was higher in women in the late reproductive stage (36.9%), and all groups had intakes above the recommendation of 30% of total energy from fat.
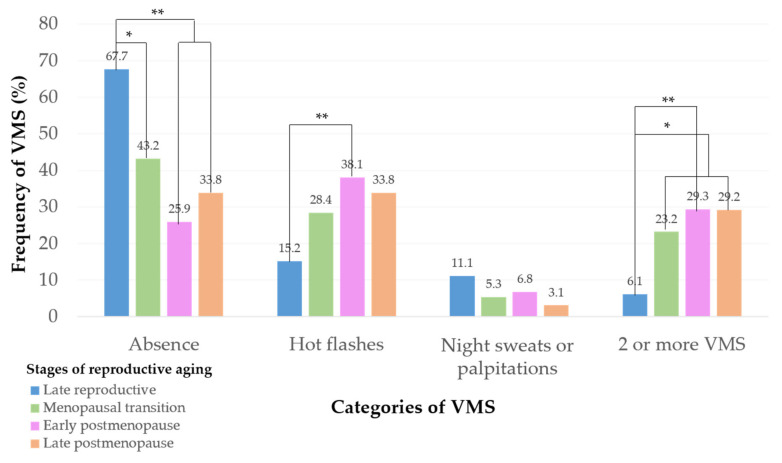
Prevalence of symptoms are reported as four categories (absence, hot flashes, night sweats or palpitations, and 2 or more VMS) (Figure 2). The study reveals that of all participants (n = 406), 41.4% experienced an absence of VMS and 29.6% presented with hot flashes only. An absence of VMS prevailed in women in the late reproductive stage (67.7%). Hot flashes were mainly reported in the early postmenopause stage (38.1%) followed by late postmenopause (33.8%). The presence of either night sweats or palpitations was reported mainly in women in the late reproductive stage (11.1%), although the presence of this category did not differ between different stages (p = 0.202). A combination of two or more VMS was reported by 23.2% of women in menopausal transition and 29.3% in early postmenopause; only 6.1% of women in the late reproductive stage presented with two or more VMS.
Figure 2.
Prevalence of vasomotor symptoms. Data were analyzed using a chi-square test with the Marascuilo procedure (post hoc test). They are expressed as percentages (%). * p < 0.01, ** p < 0.001.
The association between nutritional risk factors and VMS is shown in Table 2 for unadjusted and adjusted models. In Model 1 (unadjusted model), an overweight BMI (25–29.9 kg/m2) denoted a risk for the presence of hot flashes (PR 2.92, 95% CI: 1.66–6.32) (OR 3.24, 95% CI: 1.66–6.33, p = 0.001). The presence of either night sweats or palpitations was associated with high levels of fasting glucose (≥100 mg/dL) (OR 2.63, 95% CI: 1.09–6.37, p = 0.031) (PR 2.49, 95% CI: 1.09–6.33) and poor cardiorespiratory fitness (OR 15.01, 95% CI: 1.94–115.62, p = 0.009) (PR 8.03, 95% CI: 1.95–115.62). In addition, the presence of two or more VMS was associated with high fasting glucose levels (≥100 mg/dL) (OR 2.27, 95% CI: 1.29–3.99, p = 0.004) (PR 1.98, 95% CI: 1.29–3.98) and tobacco use (OR 3.19, 95% CI: 1.25–8.11, p = 0.015) (PR 2.25, 95% CI: 1.26–8.10).
Table 2.
Association between nutritional risk factors and vasomotor symptoms in women aged 40–65 years (n = 406).
| Vasomotor Symptoms | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Hot Flashes | Night Sweats or Palpitations | 2 or More VMS | |||||||
| Nutritional Factors | OR (95% CI) | PR (95% CI) | p | OR (95% CI) | PR (95% CI) | p | OR (95% CI) | PR (95% CI) | p |
| BMI Obese, ≥30 kg/m2 | |||||||||
| Model 1, unadjusted a | 1.32 (0.65–2.67) | 1.30 (0.66–2.65) | 0.434 | 1.34 (0.38–4.70) | 1.33 (0.39–4.62) | 0.643 | 1.17 (0.57–2.40) | 1.16 (0.59–2.31) | 0.651 |
| Model 2, adjusted b | 1.46 (0.70–3.05) | 1.43 (0.71–3.01) | 0.306 | 1.35 (0.38–4.78) | 1.34 (0.39–4.65) | 0.635 | 1.27 (0.60–2.68) | 1.25 (0.61–2.65) | 0.524 |
| Model 3, adjusted c | 1.30 (0.62–2.72) | 1.28 (0.62–2.73) | 0.487 | 1.24 (0.34–4.49) | 1.24 (0.35–4.41) | 0.740 | 1.16 (0.54–2.47) | 1.15 (0.55–2.45) | 0.697 |
| BMI Overweight, 25–29.9 kg/m2 | |||||||||
| Model 1, unadjusted a | 3.24 (1.66–6.33) | 2.92 (1.66–6.32) | 0.001 | 2.49 (0.75–8.26) | 2.45 (0.75–8.25) | 0.135 | 1.12 (0.52–2.38) | 1.11 (0.53–2.38) | 0.768 |
| Model 2, adjusted b | 3.26 (1.63–6.52) | 2.93 (1.63–6.51) | 0.001 | 2.49 (0.74–8.31) | 2.45 (0.75–8.27) | 0.136 | 1.12 (0.52–2.45) | 1.11 (0.54–2.31) | 0.760 |
| Model 3, adjusted c | 3.26 (1.63–6.54) | 2.93 (1.63–6.52) | 0.001 | 2.23 (0.65–7.65) | 2.20 (0.65–7.61) | 0.200 | 1.08 (0.49–2.39) | 1.08 (0.52–2.24) | 0.836 |
| BMI Normal 18.5–24.9 kg/m2 was reference in all models | |||||||||
| Fasting glucose High, ≥100 mg/dL | |||||||||
| Model 1, unadjusted a | 1.47 (0.87–2.51) | 1.35 (0.87–2.48) | 0.149 | 2.63 (1.09–6.37) | 2.49 (1.09–6.33) | 0.031 | 2.27 (1.29–3.99) | 1.98 (1.29–3.98) | 0.004 |
| Model 2, adjusted b | 1.30 (0.75–2.25) | 1.23 (0.75–2.25) | 0.347 | 2.50 (1.02–6.11) | 2.38 (1.02–6.11) | 0.045 | 2.03 (1.13–3.63) | 1.81 (1.13–3.63) | 0.017 |
| Model 3, adjusted c | 1.29 (0.74–2.25) | 1.23 (0.75–2.23) | 0.361 | 2.67 (1.04–6.84) | 2.53 (1.05–6.80) | 0.039 | 1.94 (1.08–3.50) | 1.75 (1.08–3.48) | 0.027 |
| Fasting glucose Normal <100 mg/dL was reference in all models | |||||||||
| Cardiorespiratory fitness Poor, <400 m/6 min | |||||||||
| Model 1, unadjusted a | 1.53 (0.18–12.53) | 1.33 (0.19–12.17) | 0.689 | 15.01 (1.94–115.62) | 8.03 (1.95–115.62) | 0.009 | d | d | d |
| Model 2, adjusted b | 1.05 (0.11–9.32) | 1.03 (0.14–8.06) | 0.963 | 13.57 (1.63–113.01) | 7.63 (1.63–112.92) | 0.016 | d | d | d |
| Model 3, adjusted c | 1.06 (0.12–8.70) | 1.04 (0.14–8.23) | 0.956 | 16.17 (2.02–129.11) | 8.33 (2.03–129.05) | 0.009 | d | d | d |
| Cardiorespiratory fitness Excellent ≥400 m/6 min was reference in all models | |||||||||
| Blood pressure Hypertensive, systolic ≥130 mmHg or diastolic ≥80 mmHg | |||||||||
| Model 1, unadjusted a | 1.47 (0.86–2.50) | 1.37 (0.86–2.51) | 0.157 | 1.85 (0.76–4.50) | 1.80 (0.77–4.46) | 0.170 | 1.33 (0.73–2.40) | 1.29 (0.74–2.39) | 0.340 |
| Model 2, adjusted b | 1.20 (0.68–2.10) | 1.17 (0.69–2.09) | 0.519 | 1.66 (0.67–4.10) | 1.63 (0.68–4.06) | 0.267 | 1.11 (0.60–2.07) | 1.10 (0.62–2.00) | 0.727 |
| Model 3, adjusted c | 1.26 (0.72–2.22) | 1.21 (0.73–2.17) | 0.405 | 1.86 (0.75–4.63) | 1.81 (0.75–4.58) | 0.178 | 1.08 (0.58–2.03) | 1.07 (0.52–2.24) | 0.792 |
| Blood pressure Elevated, systolic 120–129 mmHg and diastolic 80 mmHg | |||||||||
| Model 1, unadjusted a | 0.65 (0.22–1.89) | 0.69 (0.22–1.93) | 0.437 | d | d | 0.979 | 1.56 (0.60–4.04) | 1.47 (0.60–4.03) | 0.358 |
| Model 2, adjusted b | 0.47 (0.15–1.43) | 0.51 (0.15–1.45) | 0.189 | d | d | 0.986 | 1.20 (0.44–3.25) | 1.18 (0.44–3.24) | 0.719 |
| Model 3, adjusted c | 0.58 (0.19–1.75) | 0.62 (0.19–1.76) | 0.336 | d | d | 0.989 | 1.50 (0.54–4.10) | 1.43 (0.55–4.10) | 0.429 |
| Blood pressure Normal <120 and <80 mmHg was reference in all models | |||||||||
| Total fat intake Excessive >30% of total energy intake | |||||||||
| Model 1, unadjusted a | 1.10 (0.60–2.02) | 1.09 (0.61–1.97) | 0.749 | 2.50 (0.65–9.49) | 2.47 (0.66–9.50) | 0.178 | 1.48 (0.72–3.03) | 1.46 (0.72–3.03) | 0.283 |
| Model 2, adjusted b | 1.41 (0.74–2.69) | 1.38 (0.74–2.68) | 0.295 | 2.78 (0.71–10.81) | 2.75 (0.72–10.79) | 0.140 | 1.85 (0.87–3.90) | 1.80 (0.88–3.90) | 0.106 |
| Model 3, adjusted c | 1.37 (0.72–2.61) | 1.34 (0.73–2.57) | 0.328 | 2.24 (0.57–8.69) | 2.22 (0.58–8.67) | 0.243 | 1.97 (0.92–4.21) | 1.91 (0.92–4.20) | 0.079 |
| Total fat intake Adequate ≤30% of total energy intake was reference in all models | |||||||||
| Tobacco use Yes | |||||||||
| Model 1, unadjusted a | 2.14 (0.84–5.42) | 1.64 (0.85–5.40) | 0.107 | 2.38 (0.55–10.30) | 2.19 (0.55–10.24) | 0.244 | 3.19 (1.25–8.11) | 2.25 (1.26–8.10) | 0.015 |
| Model 2, adjusted b | 1.96 (0.76–5.05) | 1.56 (0.76–5.05) | 0.163 | 2.18 (0.49–9.66) | 2.03 (0.50–9.60) | 0.303 | 2.89 (1.10–7.57) | 2.12 (1.11–7.55) | 0.030 |
| Model 3, adjusted c | 2.04 (0.78–5.31) | 1.60 (0.79–5.26) | 0.140 | 2.31 (0.52–10.29) | 2.14 (0.52–10.22) | 0.270 | 3.05 (1.14–8.13) | 2.19 (1.15–8.11) | 0.025 |
| Tobacco use No was reference in all models | |||||||||
VMS: vasomotor symptoms. BMI: body mass index. OR: odds ratio. PR: prevalence ratio. 95%CI: 95% confidence interval. a Model 1: unadjusted. b Model 2: adjusted for age, hormone use, and physical activity level. c Model 3: adjusted for stage of reproductive aging, hormone use, physical activity level, alcohol intake, and caffeine intake. d Insufficient cases for a statistical result. p < 0.05 denotes statistical significance.
After adjusting for age, hormone use, and physical activity level, Model 2 showed very similar results to Model 1 (unadjusted). Excessive weight (BMI 25–29.9 kg/m2) was a nutritional risk for the presence of hot flashes (PR 2.93, 95% CI: 1.63–6.51) (OR 3.26, 95% CI: 1.63–6.52, p = 0.001). Women were at risk of presenting with either night sweats or palpitations if fasting glucose levels were ≥100 mg/dL (PR 2.38, 95% CI: 1.02–6.11) (OR 2.50, 95% CI: 1.02–6.11, p = 0.045) and if they had poor cardiorespiratory fitness levels (PR 7.63, 95% CI: 1.63–112.92) (OR 13.57, 95% CI: 1.63–113.01, p = 0.016). Presence of two or more VMS was also associated with high fasting glucose levels (≥100 mg/dL) (PR 1.81, 95% CI: 1.13–3.63) (OR 2.03, 95% CI: 1.13–3.63, p = 0.017) and smoking habits (PR 2.12, 95% CI: 1.11–7.55) (OR 2.89, 95% CI: 1.10–7.57, p = 0.030).
Model 3 was adjusted to include the stage of reproductive aging, hormone use, physical activity level, alcohol intake, and caffeine intake (Table 2), denoting consistency in results from Models 1 and 2. The presence of hot flashes was associated with an overweight BMI (25–29.9 kg/m2) (PR 2.93, 95% CI: 1.63–6.52) (OR 3.26, 95% CI: 1.63–6.54, p = 0.001). Levels of fasting glucose ≥100 mg/dL (PR 2.53, 95% CI: 1.05–6.80) (OR 2.67, 95% CI: 1.04–6.84, p = 0.039) and poor cardiorespiratory fitness (PR 8.33, 95% CI: 2.03–129.05) (OR 16.17, 95% CI: 2.02–129.11, p = 0.009) are risk factors associated with the presence of night sweats or palpitations. High fasting glucose ≥100 mg/dL (PR 1.75, 95% CI: 1.08–3.48) (OR 1.94, 95% CI: 1.08–3.50, p = 0.027) and tobacco use (PR 2.19, 95% CI: 1.15–8.11) (OR 3.05, 95% CI: 1.14–8.13, p = 0.025) denoted a risk for the presence of two or more VMS.
There was no association between blood pressure and total fat intake and the presence of VMS in any proposed model (unadjusted or adjusted).
4. Discussion
This observational study in women aged 40–65 years from Nuevo León state, in northeast Mexico, determined the association between nutritional risk factors and the presence of vasomotor symptoms. Menopausal onset was at 47.0 years; this is younger than women living in central Mexico, as previous studies have found that women from Queretaro started menopause at 49.1 years [5] and those from Mexico City at 50.0 years [6]. The onset of menopause at earlier ages, defined as early menopause (<45 years old), [31] could be due to some of the trigger factors that women reported in this study, such as tobacco use and an overweight or obese BMI [32]. Moreover, it has been demonstrated that menopause at early ages is related to a higher risk of cardiovascular disease and mortality, especially in women aged 50–78 years [33].
The experience of VMS is similar among Mexican women and follows a pattern that predominates in the early postmenopause stage. In this study, 29.6% of all women showed hot flashes, while 38.1% of women in the early postmenopause stage reported having this specific VMS. In a previous study in central Mexico, 21.3% of women aged 40–60 years reported having hot flashes, mainly during menopausal transition [34]. In other countries, such as India, the United Kingdom, Australia, and the United States of America, hot flashes were more frequently reported during the postmenopausal stage [35,36].
The presence of two or more VMS was reported in 22.2% of all women in the current study and was most frequently reported by early postmenopausal women (29.3%). However, previous studies have shown greater incidence of two VMS (hot flashes and night sweats) at the postmenopausal stage; this was found in 50.0% of women aged 24–44 years from the United States of America [11] and in 53.3% of women aged 40–65 years from India [35]. Therefore, in this study, the higher frequency of two or more VMS agrees with the STRAW+10 criteria, which suggests greater a likelihood of symptoms occurring during the early postmenopausal stage [3].
In this study, several women in the late reproductive stage also reported the presence of VMS; 15.2% had hot flashes and 11.1% had either night sweats or palpitations. Previous studies have reported night sweats in 40.0% and hot flashes in 29.0% of late reproductive women aged 35–55 years [37]. It is important to note that VMS can begin at earlier stages, such as the late reproductive stage, although in a low proportion due to estrogen reduction through constant aging and death of follicles [38]. Thus, assessment and diagnosis of VMS is relevant at earlier stages.
The association between nutritional factors and the presence of VMS was analyzed using three regression models to obtain the odds ratio (OR), and a formula using OR values to obtain the prevalence ratio (PR). These demonstrate the risks of women being overweight, having fasting glucose levels above 100 mg/mL, having a cardiorespiratory fitness below 400 m/6 min, and being a smoker. Adjustment of Models 2 and 3 for covariates did not affect the association. Poor cardiorespiratory fitness was the only risk factor with subtle changes in Model 3 that resulted in slightly higher risk and a wider 95% CI.
Hot flashes were associated with being overweight in this study population (BMI 25–29.9 kg/m2) at PR 2.92–2.93 and OR 3.24–3.26 (p = 0.001 in all models). Overweight and obese BMIs have previously been associated with the presence of VMS, as reported in the clinical practice guidelines [7,8] and in some studies from Scotland [10], North America [27,39], Australia [40], and South Korea [26]. Women showing a higher BMI tend to have an excess of body fat; visceral fat increases by up to 20% during the postmenopausal stage [41]. In this study, obesity was not associated with hot flashes, which may be because more obese women were at later stages, such as the late postmenopause stage, in which hot flashes were less frequently reported, similar to a previous study [39]. Excessive fat does not allow heat conduction through the skin; therefore, the body tries to release it by maximizing vasodilation, which increases the central body temperature beyond the sweating threshold [13,42]. However, our findings may also suggest that the mechanisms of estrone, associated with a decrease in hot flashes, are naturally occurring in our study of postmenopausal women [39,43].
Fasting glucose levels above 100 mg/dL were associated with either night sweats or palpitations and with two or more VMS. A Swedish study in women aged 50–64 years reported night sweats as the only VMS associated with high glucose levels (p < 0.05) [44]. In a longitudinal study of Australian women aged 45–50 years, it was stated that there was a significant association between night sweats and diabetes (OR 1.91, 99% CI: 1.08–3.35, p < 0.001) in an adjusted model including similar covariates as this study: age, educational level, length of time, BMI, physical activity level, tobacco use, alcohol intake, menopausal status, and hormone use [45]. Therefore, chronic hyperglycemia could be a strong associated factor. High levels of glucose have been associated with insomnia, because the hypothalamic-pituitary-adrenal axis is altered [46]. This axis also regulates steroid and adrenal secretions [47], so its alteration impacts VMS occurrence.
The association between high blood pressure and VMS could be due to the increased activity of the sympathetic nervous system [48], and thus the increased activity of the adrenalin and sweat glands [49]. Although models in this study showed non-significant results when systolic and diastolic blood pressures were elevated or at hypertension levels, other authors have reported significant associations [44,50]. A study from Sweden in postmenopausal women, aged 50–64 years, reported an association between the presence of night sweats and systolic blood pressure (OR 2.07, p < 0.001) [44]. In addition, women in the United States of America aged 45–54 years who were under antihypertensive treatment had 1.80 times greater risk of presenting with hot flashes (p <0.05) [50].
Fat intake was not associated with the presence of VMS in any model (unadjusted or adjusted). Intake of foods high in fat, especially saturated fat obtained from animal sources such as red or white meat, can increase levels of LDL cholesterol (low-density lipoprotein) [51], and therefore increase the presence of VMS [44]. This is supported by findings of studies in Australian women aged 45–50 years, in which those who followed a high-fat diet presented a significant risk for the presence of both hot flashes and night sweats (unadjusted model, OR 1.16, p = 0.002) [52]. Additionally, a study of women aged 40–85 years in the United States of America, who were in menopausal transition and postmenopause, VMS were higher among those who consumed more red and white meat, seafood, and dairy, while an absence of VMS was presented among women consuming a plant-based diet [53].
It has been suggested that a decrease in VMS may be observed with improving cardiorespiratory fitness [54,55]. Cardiorespiratory fitness was associated with improved health (p < 0.001), emotions (p = 0.05), and occupational quality of life (p = 0.03), suggesting a positive effect on reduced menopausal symptoms in women aged 45–60 years in the United States of America [55]. However, there has been no reported association with hot flashes and night sweats in Spanish women aged 45–60 years [56]. In the present study, poor cardiorespiratory fitness was the nutritional factor with the highest association to either night sweats or palpitations (PR 7.63–8.33; OR 13.57–16.17, p < 0.05). Women who had been physically active since menopausal transition had more protection from VMS. A higher cardiorespiratory fitness level decreases the activation of the sympathetic nervous system, which narrows the blood vessels of the body; in turn, the thermoneutral zone maintains homeostasis [57].
Tobacco use has been reported by different studies as a nutritional risk factor for VMS. Cigarettes are composed of different metals that serve as endocrine disruptors which alter the hormonal balance, so estrogens can be affected until they trigger VMS [12,58]. Women that have been smoking for many years may be at increased risk of having VMS. In a longitudinal study, current smokers aged 24–44 years showed 2.5 times greater risk of having hot flashes and night sweats (95% CI: 1.5–5.3, p <0.05) after adjusting for age, hormone level, BMI, hormone use, marital status, and parity [11]. A study of women in the late reproductive stage and the menopausal transition stage from the United States of America, aged 42–52 years, showed an association between the presence of VMS (hot flashes and night sweats), the number of cigarettes smoked (unadjusted model, OR 1.6, 95% CI: 1.3–1.9, p < 0.05), and passive smoke exposure (unadjusted model, OR 1.3, 95% CI: 1.2–1.4, 0.05) [59].
Strengths and Limitations
The main strength of the current study is that it has determined the association between nutritional risk factors and the presence of vasomotor symptoms in women aged 40–65 years from Nuevo León state, in northeast Mexico. The analysis of prevalence and risk is also a strength of this study as it avoids over- or underestimation of this association; however, data could not be compared against other publications. A limitation of this study is the lack of precision in the responses of presence of VMS, as women were questioned in a dichotomous way (yes or no) without considering frequency or intensity. The analysis of some nutritional variables, such as blood pressure and cardiorespiratory function, was limited due to an insufficient number of cases when assessing the categories of VMS. Intakes of subtypes of fat were not analyzed. For future research, it is recommended that women present a similar intake of alcohol and caffeine for more uniformity in those covariates, which may achieve greater precision in adjusted models. In addition, longitudinal studies are needed to infer specific causes or to determine strong risk factors for this specific population.
5. Conclusions
The presence of VMS was associated with different nutritional risk factors (weight, fasting glucose levels, cardiorespiratory fitness, and tobacco use) in women living in northeast Mexico. This association was independent of covariates including age, stage of reproductive aging, hormone use, reported physical activity, alcohol intake, and caffeine intake. This evidence supports the need for updating these nutritional risk factors in clinical practice guidelines and its application as an instrument in primary health care services, which assist women at different stages of reproductive aging, at local and national levels.
Acknowledgments
The authors especially thank the participants for their enthusiastic collaboration and the personnel for outstanding support and exceptional effort. CIBEROBN is an initiative of Instituto de Salud Carlos III, Spain.
Author Contributions
A.T., Y.B., E.S.-P. and J.A.T. designed the study; A.T. and Y.B. wrote the protocol; A.T. recruited the participants and collected samples; Y.B. and J.L.J. conducted the statistical analysis; A.T., Y.B. and J.A.T. wrote the first draft of the manuscript, and all authors (A.T., Y.B., E.S.-P., R.S., J.L.J., V.L., E.R., R.P., C.B. and J.A.T.) commented on previous versions of the manuscript. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the ethics committee of the Facultad de Salud Pública y Nutrición of the protocol ID: 15–FaSPyN–SA–11.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. The results and writing of this manuscript followed the Committee on Publication Ethics (COPE) guidelines on how to deal with potential acts of misconduct, maintaining integrity of the research and its presentation following the rules of good scientific practice, the trust in the journal, the professionalism of scientific authorship, and the entire scientific endeavor. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
There are restrictions on the availability of data for this trial, due to the signed consent agreements around data sharing, which only allow access to external researchers for studies following the project purposes. Those wishing to access the trial data used in this study can make a request to pep.tur@uib.es.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
C.B. and J.A.T. are funded by the Instituto de Salud Carlos III through the CIBEROBN CB12/03/30038, which is co-funded by the European Regional Development Fund. The funding sponsors had no role in the design of the study, in the collection, analysis, or interpretation of the data, in the writing of the manuscript, or in the decision to publish the results.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Biglia N., Cagnacci A., Gambacciani M., Lello S., Maffei S., Nappi R. Vasomotor symptoms in menopause: A biomarker of cardiovascular disease risk and other chronic diseases? Climacteric. 2017;20:306–312. doi: 10.1080/13697137.2017.1315089. [DOI] [PubMed] [Google Scholar]
- 2.Hoffman B., Schorge J., Schaffer J., Halvorson L., Bradshaw K., Cunningham F. Williams Ginecología. 2nd ed. McGraw-Hill Interamericana Editores; Mexico City, Mexico: 2014. [Google Scholar]
- 3.Harlow S., Gass M., Hall J., Lobo R., Maki P., Rebar R., Sherman S., Sluss P., De Villiers T. Executive summary of the Stages of Reproductive Aging Workshop + 10: Addressing the unfinished agenda of staging reproductive aging. Menopause. 2012;19:387–395. doi: 10.1097/gme.0b013e31824d8f40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woods N., Mitchell E. Symptoms during the perimenopause: Prevalence, severity, trajectory, and significance in women’s lives. Am. J. Med. 2005;118:14S–24S. doi: 10.1016/j.amjmed.2005.09.031. [DOI] [PubMed] [Google Scholar]
- 5.Carranza S., Sandoval C. Comparación de la frecuencia y magnitud de los síntomas vasomotores en mujeres pre y posmenopáusicas de la Ciudad de México. Ginecol. Obstet. Méx. 2013;81:127–132. [PubMed] [Google Scholar]
- 6.Ortiz G., Arellano A., Sánchez A., Salazar C., Escobar L., Zavala A. Descripción demográfica, bioquímica y sintomática según los estadios reproductivos STRAW+10 en mujeres mexicanas en la peri y postmenopausia. Ginecol. Obstet. Méx. 2020;88:29–40. doi: 10.24245/gom.v88i1.3282. [DOI] [Google Scholar]
- 7.Ministerio de Sanidad, Servicios Sociales e Igualdad (MSSSI) Guía de Práctica Clínica Sobre el Abordaje de Síntomas Vasomotores y Vaginales Asociados a la Menopausia y la Postmenopausia. [(accessed on 29 March 2021)]. Available online: https://portal.guiasalud.es/wp-content/uploads/2018/12/GPC_571_Menopausia_AETSA_herram.pdf.
- 8.Secretaría de Salud (SSA) Guía de Práctica Clínica: Atención al Climaterio y Menopausia. [(accessed on 29 March 2021)]. Available online: http://evaluacion.ssm.gob.mx/pdf/gpc/eyr/SS-019-08.pdf.
- 9.Secretaría de Salud (SSA) Norma Oficial Mexicana NOM-035-SSA2-2012, Para la Prevención y Control de Enfermedades en la Perimenopausia y Postmenopausia de la Mujer. Criterios Para Brindar Atención Médica. [(accessed on 29 March 2021)]. Available online: https://www.cndh.org.mx/sites/default/files/doc/Programas/VIH/Leyes%20y%20normas%20y%20reglamentos/Norma%20Oficial%20Mexicana/NOM-035-SSA2-2012.pdf.
- 10.Duffy O., Iversen L., Aucott L., Hannaford P. Factors associated with resilience or vulnerability to hot flushes and night sweats during the menopausal transition. Menopause. 2012;20:383–392. doi: 10.1097/gme.0b013e31827655cf. [DOI] [PubMed] [Google Scholar]
- 11.Ford K., Sowers M., Crutchfield M., Wilson A., Jannausch M. A longitudinal study of the predictors of prevalence and severity of symptoms commonly associated with menopause. Menopause. 2005;12:308–317. doi: 10.1097/01.GME.0000163869.89878.D9. [DOI] [PubMed] [Google Scholar]
- 12.Anderson D., Chung H., Seib C., Dobson A., Kuh D., Brunner E., Crawford S., Avis N., Gold E., Greendale G., et al. Obesity, smoking, and risk of vasomotor menopausal symptoms: A pooled analysis of eight cohort studies. Am. J. Obstet. Gynecol. 2019;222:478.e1–478.e17. doi: 10.1016/j.ajog.2019.10.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thurston R., Sowers M., Chang Y., Sternfeld B., Gold E., Johnston J., Matthews K. Adiposity and reporting of vasomotor symptoms among midlife women. Am. J. Epidemiol. 2008;167:78–85. doi: 10.1093/aje/kwm244. [DOI] [PubMed] [Google Scholar]
- 14.Vega G., Hernández A., Leo G., Vega J., Escartin M., Luengas J., Guerrero M. Incidencia y factores relacionados con el síndrome climatérico en una población de mujeres mexicanas. Rev. Chil. Obstet. Ginecol. 2007;72:314–320. doi: 10.4067/S0717-75262007000500007. [DOI] [Google Scholar]
- 15.Instituto Nacional de Estadística y Geografía e Informática (INEGI) Población Total por Entidad Federativa y Grupo Quinquenal de edad Según Sexo, Serie de Años Censales de 1990 a 2020. [(accessed on 2 May 2022)]. Available online: https://www.inegi.org.mx/app/tabulados/interactivos/?pxq=Poblacion_Poblacion_01_e60cd8cf-927f-4b94-823e-972457a12d4b&idrt=123&opc=t.
- 16.Academy of Nutrition and Dietetics (AND) Abridged Nutrition Care Process Terminology (NCPT). Reference Manual: Standardized Terminology for the Nutrition Care Process. [(accessed on 14 February 2022)]. Available online: https://www.eatrightstore.org/product-type/books/abridged-ncpt-reference-manual.
- 17.World Health Organization (WHO) Obesity: Preventing and Managing the Global Epidemic. Geneva. [(accessed on 21 May 2021)]. Available online: https://apps.who.int/iris/handle/10665/63854.
- 18.American Diabetes Association (ADA) American Diabetes Association Standards of Medical Care in Diabetes 2019. Diabetes Care. 2019;42:S1–S193. doi: 10.2337/dc19-Sint01. [DOI] [PubMed] [Google Scholar]
- 19.Secretaria de Salud (SSA) Norma Oficial Mexicana NOM-030-SSA2-2009, Para la Prevención, Detección, Diagnóstico, Tratamiento y Control de la Hipertensión Arterial Sistémica. [(accessed on 21 May 2021)]. Available online: https://www.cndh.org.mx/DocTR/2016/JUR/A70/01/JUR-20170331-NOR21.pdf.
- 20.Whelton P., Carey R., Aronow W., Casey D., Collins K., Dennison C., DePalma S., Gidding S., Jamerson K., Jones D., et al. 2017 ACC/AHA/AAPA/ ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: Executive summary: A report of the American College of Cardiology/American Heart Association task force on Clinical Practice Guidelines. Hypertension. Am. Heart Assoc. J. 2018;71:1269–1324. doi: 10.1161/HYP.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 21.Giannitsi S., Bougiakli M., Bechlioulis A., Kotsia A., Michalis L., Naka K. 6-minute walking test: A useful tool in the management of heart failure patients. Ther. Adv. Cardiovasc. Dis. 2019;13:1753944719870084. doi: 10.1177/1753944719870084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tijerina A., Tur J.A. Development and validation of a semiquantitative food frequency questionnaire to assess dietary intake in 40-65-year-old Mexican women. Ann. Nutr. Metab. 2020;76:73–82. doi: 10.1159/000506920. [DOI] [PubMed] [Google Scholar]
- 23.Academia Nacional de Medicina (ANM) Guías Alimentarias y de Actividad Física en Contexto de Sobrepeso y Obesidad en la Población Mexicana. Documentos de Postura. [(accessed on 8 April 2022)]. Available online: https://www.anmm.org.mx/publicaciones/CAnivANM150/L29_ANM_Guias_alimentarias.pdf.
- 24.Prevención con Dieta Mediterránea (PREDIMED) Cuestionario de Actividad Física en el Tiempo Libre de Minnesota. [(accessed on 8 April 2022)]. Available online: http://www.predimed.es/uploads/8/0/5/1/8051451/activ_fisica.pdf.
- 25.Enomoto H., Terauchi M., Odai T., Kato K., Iizuka M., Akiyoshi M., Miyasaka N. Independent association of palpitation with vasomotor symptoms and anxiety in middle-aged women. Menopause. 2021;28:741–747. doi: 10.1097/GME.0000000000001776. [DOI] [PubMed] [Google Scholar]
- 26.Ryu K., Park H., Kwon D., Yang K., Kim Y., Yi K., Shin J., Hur J., Kim T. Vasomotor symptoms and metabolic syndrome in Korean postmenopausal women. Menopause. 2015;22:1239–1245. doi: 10.1097/GME.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 27.Thurston R., Chang Y., Mancuso P., Matthews K. Adipokines, adiposity, and vasomotor symptoms during the menopause transition: Findings from the Study of Women’s Health Across the Nation. Fertil. Steril. 2013;100:793–800.e1. doi: 10.1016/j.fertnstert.2013.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Avis N., Crawford S., Greendale G., Bromberger J., Everson S., Gold E., Hess R., Joffe H., Kravitz H., Tepper P., et al. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern. Med. 2015;175:531–539. doi: 10.1001/jamainternmed.2014.8063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schiaffino A., Rodríguez M., Pasarín M.I., Regidor E., Borrell C., Fernández E. Odds ratio o razón de proporciones? Su utilización en estudios transversales. Gac. Sanit. 2003;17:51. doi: 10.1016/S0213-9111(03)71694-X. [DOI] [PubMed] [Google Scholar]
- 30.Strömberg U. Prevalence odds ratio v prevalence ratio. Occup. Environ. Med. 1994;51:143. doi: 10.1136/oem.51.2.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Edwards H., Duchesne A., Au A., Einstein G. The many menopauses: Searching the cognitive research literature for menopause types. Menopause. 2019;26:45–65. doi: 10.1097/GME.0000000000001171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pelosi E., Simonsick E., Forabosco A., Garcia J., Schlessinger D. Dynamics of the ovarian reserve and impact of genetic and epidemiological factors on age of menopause. Biol. Reprod. 2015;92:130. doi: 10.1095/biolreprod.114.127381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhang X., Liu L., Song F., Song Y., Dai H. Ages at menarche and menopause, and mortality among postmenopausal women. Maturitas. 2019;130:50–56. doi: 10.1016/j.maturitas.2019.10.009. [DOI] [PubMed] [Google Scholar]
- 34.Dorador M., Orozco G. Síntomas psicológicos en la transición menopáusica. Rev. Chil. Obstet. Ginecol. 2018;83:228–239. doi: 10.4067/s0717-75262018000300228. [DOI] [Google Scholar]
- 35.Khatoon F., Sinha P., Shahid S., Gupta U. Assessment of menopausal symptoms using modified menopause rating scale (MRS) in women of Northern India. Int. J. Reprod. Contracept. Obstet. Gynecol. 2018;7:947–951. doi: 10.18203/2320-1770.ijrcog20180871. [DOI] [Google Scholar]
- 36.Zhu D., Chung H., Dobson A., Pandeya N., Anderson D., Kuh D., Hardy R., Brunner E., Avis N., Gold E., et al. Vasomotor menopausal symptoms and risk of cardiovascular disease: A pooled analysis of six prospective studies. Am. J. Obstet. Gynecol. 2020;1:1.e1–1.e16. doi: 10.1016/j.ajog.2020.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Coslov N., Richardson M., Fugate N. Symptom experience during the late reproductive stage and the menopausal transition: Observations from the Women Living Better survey. Menopause. 2021;28:1012–1025. doi: 10.1097/GME.0000000000001805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ata B., Seyhan A., Seli E. Diminished ovarian reserve versus ovarian aging. Curr. Opin. Obstet. Gynecol. 2019;31:139–147. doi: 10.1097/GCO.0000000000000536. [DOI] [PubMed] [Google Scholar]
- 39.Gold E., Crawford S., Shelton J., Tepper P., Crandall C., Greendale G., Matthews K., Thurston R., Avis N. Longitudinal analysis of changes in weight and waist circumference in relation to incident vasomotor symptoms: The Study of Women’s Health Across the Nation (SWAN) Menopause. 2017;24:9–26. doi: 10.1097/GME.0000000000000723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zeleke B., Bell R., Billah B., Davis S. Vasomotor and sexual symptoms in older Australian women: A cross-sectional study. Fertil. Steril. 2015;105:149–155. doi: 10.1016/j.fertnstert.2015.09.017. [DOI] [PubMed] [Google Scholar]
- 41.Kapoor E., Collazo M., Faubion S. Weight gain in women at midlife: A concise review of the pathophysiology and strategies for management. Mayo Clin. Proc. 2017;92:1552–1558. doi: 10.1016/j.mayocp.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 42.Freedman R. Hot flashes: Behavioral treatments, mechanisms, and relation to sleep. Am. J. Med. 2005;118:124–130. doi: 10.1016/j.amjmed.2005.09.046. [DOI] [PubMed] [Google Scholar]
- 43.Costanian C., Zangiabadi S., Bahous S., Deonandan R., Tamim H. Reviewing the evidence on vasomotor symptoms: The role of traditional and non-traditional factors. Climacteric. 2020;23:213–223. doi: 10.1080/13697137.2019.1711051. [DOI] [PubMed] [Google Scholar]
- 44.Gast G., Samsioe G., Grobbee D., Nilsson P., Van der Schouw Y. Vasomotor symptoms, estradiol levels and cardiovascular risk profile in women. Maturitas. 2010;66:285–290. doi: 10.1016/j.maturitas.2010.03.015. [DOI] [PubMed] [Google Scholar]
- 45.Herber G., Mishra G., Van Der Y., Brown W., Dobson A. Risk factors for night sweats and hot flushes in midlife: Results from a prospective cohort study. Menopause. 2013;20:953–959. doi: 10.1097/GME.0b013e3182844a7c. [DOI] [PubMed] [Google Scholar]
- 46.D’Aurea C., Poyares D., Piovezan R., Passos G., Tufik S., De Mello M. Objective short sleep duration is associated with the activity of the hypothalamic-pituitary-adrenal axis in insomnia. Arq. Neuro-Psiquiatr. 2015;73:516–519. doi: 10.1590/0004-282X20150053. [DOI] [PubMed] [Google Scholar]
- 47.Son Y., Ubuka T., Tsutsui K. Regulation of stress response on the hypothalamic-pituitary-gonadal axis via gonadotropin-inhibitory hormone. Front. Neuroendocrinol. 2022;64:100953. doi: 10.1016/j.yfrne.2021.100953. [DOI] [PubMed] [Google Scholar]
- 48.Franco O., Muka T., Colpani V., Kunutsor S., Chowdhury S., Chowdhury R., Kavousi M. Vasomotor symptoms in women and cardiovascular risk markers: Systematic review and meta-analysis. Maturitas. 2015;81:353–361. doi: 10.1016/j.maturitas.2015.04.016. [DOI] [PubMed] [Google Scholar]
- 49.Alshak M., Das J. StatPearls Publishing: Neuroanatomy, Sympathetic Nervous System. [(accessed on 23 April 2022)]; Available online: https://www.ncbi.nlm.nih.gov/books/NBK542195. [PubMed]
- 50.Gallicchio L., Miller S., Kiefer J., Greene T., Zacur H., Flaws J. Risk factors for hot flashes among women undergoing the menopausal transition: Baseline results from the Midlife Women’s Health Study. Menopause. 2015;22:1098–1107. doi: 10.1097/GME.0000000000000434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bergeron N., Chiu S., Williams P., King S., Krauss R. Effects of red meat, white meat, and nonmeat protein sources on atherogenic lipoprotein measures in the context of low compared with high saturated fat intake: A randomized controlled trial. Am. J. Clin. Nutr. 2019;110:24–33. doi: 10.1093/ajcn/nqz035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cor G., Gast H., Mishra G. Fruit, Mediterranean-style, and high-fat and -sugar diets are associated with the risk of night sweats and hot flushes in midlife: Results from a prospective cohort study. Am. J. Clin. Nutr. 2013;97:1092–1099. doi: 10.3945/ajcn.112.049965. [DOI] [PubMed] [Google Scholar]
- 53.Beezhold B., Radnitz C., McGrath R., Feldman A. Vegans report less bothersome vasomotor and physical menopausal symptoms than omnivores. Maturitas. 2018;112:12–17. doi: 10.1016/j.maturitas.2018.03.009. [DOI] [PubMed] [Google Scholar]
- 54.Elavsky S., McAuley E. Personality, menopausal symptoms, and physical activity outcomes in middle-aged women. Personal. Individ. Differ. 2009;46:123–128. doi: 10.1016/j.paid.2008.09.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Flesaker M., Serviente C., Troy L., Witkowski S. The role of cardiorespiratory fitness on quality of life in midlife women. Menopause. 2021;28:431–438. doi: 10.1097/GME.0000000000001719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aparicio V., Borges M., Ruiz P., Coll I., Acosta P., Špacírová Z., Soriano A. Association of objectively measured physical activity and physical fitness with menopause symptoms. The Flamenco Project. Climacteric. 2017;20:456–461. doi: 10.1080/13697137.2017.1329289. [DOI] [PubMed] [Google Scholar]
- 57.Elavsky S., Gonzales J., Proctor D., Williams N., Henderson V. Effects of physical activity on vasomotor symptoms: Examination using objective and subjective measures. Menopause. 2012;19:1095–1103. doi: 10.1097/gme.0b013e31824f8fb8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Arias M., Castro L., Barreiro J., Cabanas P. Una revisión sobre los disruptores endocrinos y su posible impacto sobre la salud de los humanos. Rev. Esp. Endocrinol. Pediátrica. 2020;11:33–53. doi: 10.3266/RevEspEndocrinolPediatr.pre2020.Nov.619. [DOI] [Google Scholar]
- 59.Gold E., Block G., Crawford S., Lachance L., FitzGerald G., Miracle H., Sherman S. Lifestyle and demographic factors in relation to vasomotor symptoms: Baseline results from the Study of Women’s Health Across the Nation. Am. J. Epidemiol. 2004;159:1189–1199. doi: 10.1093/aje/kwh168. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
There are restrictions on the availability of data for this trial, due to the signed consent agreements around data sharing, which only allow access to external researchers for studies following the project purposes. Those wishing to access the trial data used in this study can make a request to pep.tur@uib.es.