Abstract
Ethnoveterinary practices and ethnobotanical knowledge serve as potential therapeutic approaches used to manage and prevent cattle diseases within poor communities in developing nations. Most of the knowledge and practices remain inadequately documented and threatened with extinction in the future. This study aimed to explore the ethnoveterinary practices and knowledge on plants used to treat cattle diseases in two communities of the Ramotshere Moiloa local municipality, South Africa. A semi-structured interview guide, snowball, and purposive technique were used to collect data and recruit 90 participants. Three ethnobotanical indices (informant consensus factor (Fic), use-value (UV), and relative frequency of citation (RFC) were used for quantitative analysis. A total of 64 medicinal plants from 32 families (dominated by Compositae, Fabaceae, and Asparagaceae) were used to treat 27 cattle diseases. The plants with a high frequency of citation and RFC were Gomphocarpus fruticosus (75, 0.83), Opuntia ficus-indica (74, 0.82), Schkuhria pinnata and Portulaca oleracea (73, 0.81), Solanum lichtensteinii (70, 0.77), and Senna italica. In addition, Schkuhria pinnata and Aloe greatheadii (0.077) had the highest UV. About 28.13% of 64 identified plants were documented as ethnoveterinary medicine for treating cattle ailments, for the first time. The remedies were mainly either prepared as a decoction (52.04%), ground, or prepared as an infusion (16.33%). The plants were administered either orally (69.79%) or topically (30.2%). The ailments with a high frequency of citations were: wounds and constipation (76); arthralgia and retained placenta (69); and lumpy skin disease (68). The categories with the highest number of plants used were gastrointestinal problems (53), skin problems (33), respiratory problems (25), and fertility/reproduction disorders (21). The highest Fic score was cited for tick-borne diseases (1), followed by musculoskeletal systems (Fic = 0.89), and general system infection (Fic = 0.88). The current findings contribute to the documentation and preservation of valuable knowledge from indigenous communities for extensive use. Additionally, ethnoveterinary uses of Portulaca oleracea, Securidaca longipedunculata, and Plumbago zeylanica were recorded for the first time. Further scientific evaluation of the most cited and indigenous/native plants is recommended to establish their therapeutic potential and possible integration into the conventional veterinary sector for the welfare of cattle.
Keywords: Batswana, biodiversity, endemic, gastrointestinal problems, ethnobotanical survey, indigenous diagnostics, indigenous knowledge, wounds
1. Introduction
Cattle production plays a key role in the rural economies of developing countries in terms of food security, poverty alleviation, and diverse cultural activities, particularly in rural communities [1,2]. Due to their use as draft animals and their ability to convert low-quality forage into energy-dense muscle and milk, cattle provide a significant source of food and nutrition, much-needed income, and nitrogen-rich manure for replenishing soils and other uses [3,4]. They also fulfil a wide variety of socio-cultural roles. However, cattle in rural areas are often susceptible to various diseases [5]. Changes in population and climate, technology, lifestyles, consumer demands, markets, and other factors are driving rapid change in cattle production. These factors are influencing the way cattle are being produced, improving the livelihoods of people, and sometimes threatening cattle diversity at the local, national, and regional herd levels [6,7,8]. Healthy, well-cared-for, and productive cattle contribute to the sustainable, healthier, and inclusive future livelihood of the communities. The clinical service of the public veterinary service is believed to be inefficient and seen to have minimal effect on animal health [9]. Therefore, maintaining and restoring the health and well-being of the cattle is a critical responsibility for the community members who depend on them.
Farmers and cattle herders in rural communities rely on ethnoveterinary medicine (EVM) as a sustainable alternative to western veterinary practices. Ethnoveterinary medicine encompasses a variety of systems and knowledge of maintaining animal health that is based on beliefs, traditional knowledge, skills, methods, medicinal plants, metaphysics, surgical procedures, technologies, and teachings that are used in healing livestock [10]. The popularity of EVM is often attributed to its ability to improve folk pharmacotherapy which is locally available, economically feasible, accessible, and culturally appropriate [11]. Furthermore, the practice includes a set of empirical observations of the environment and self-management [9]. According to McGaw and Eloff [8], studies in EVM are necessary because plants contain a wide range of phytochemicals. These plants can provide the lead candidates for drug discovery and development of active products, which are useful in managing the health of livestock. In South Africa, the rich and unique flora have been well-utilised in traditional medicine, thereby creating more interest in the potential of medicinal plants [12,13]. As a megadiverse country with a rapidly growing population, the incessant loss of biodiversity justifies the need to document the plant resources, especially the native plants which can be considered as endemic or indigenous [14].
Cattle diseases are major veterinary health problems, which are experienced by livestock farmers in developing countries. Recently, the Conventional Veterinary Services and Drug Resistance reported a rise in the number of cattle diseases that are affecting cattle production [15]. The situation has been compounded by the inaccessibility of veterinary services by rural cattle breeders and the escalating cost of veterinary services. Despite the existing efforts [1,8,16,17,18], there is a paucity of documentation and scientific data regarding the knowledge and practices of ethnoveterinary medicine among different ethnic groups globally.
The majority of indigenous diagnostic and ethnobotanical knowledge methods used in cattle healthcare have been passed down from generation to generation, mainly by word of mouth and apprenticeship [19,20]. Currently, such indigenous knowledge is held by the community’s elders and the limited young members with interest in learning how to use it [21]. Furthermore, EVM is often locally and culturally specific due to differences in disease epidemiology, culture, and biodiversity. Therefore, if not documented, the immense knowledge, skills, and experience accumulated over generations may become extinct in developing countries because of migrations, urbanisation, and technological development [22,23]. Thus, this study explored the indigenous diagnostic and ethnobotanical skills, methods, and processes used to treat cattle diseases and other husbandry indications among Batswana in two communities in the Ramotshere Moiloa local municipality, South Africa.
2. Results and Discussion
2.1. Socio-Demographic Data of Participants in the Study
A total of 90 community members with ages ranging from 18 to 95 years participated in this study (Table 1). The dominant age group, who constituted about 40% of the participants, were aged 61 and above and are regarded as elders in the communities. Generally, indigenous knowledge on the use of EVM is mostly limited to older people in the communities [24,25,26,27,28]. In the current study, all (100%) of the participants acquired knowledge about indigenous diagnostic skills and ethnobotanical knowledge about diseases from elders. This indicates the relative transmission of indigenous practices from one generation to the next one. The environment and experience of others remain two of the most active means to transmit knowledge about the medicinal values of plants [29,30]. This also indicates that the knowledge is facing a threat, which has a negative impact on the use of ethnoveterinary medicine. Likewise, Giday and Teklehaymanot [31] acknowledged that indigenous knowledge is declining among the younger generation in Africa. However, ethnoveterinary medicine is still prevalent in remote villages of the Ramotshere Moiloa local municipality. The need to preserve the indigenous knowledge, which is at risk of being lost due to the modern lifestyle, remains pertinent [23].
Table 1.
Demographic information of participants engaged in the study (n = 90).
| Characteristic of Participants | Category | Frequency | Distribution (%) |
|---|---|---|---|
|
18–30 | 12 | 13 |
| 31–40 | 15 | 17 | |
| 41–50 | 12 | 13 | |
| 51–60 | 15 | 17 | |
| 61 and above | 36 | 40 | |
|
Male | 75 | 83 |
| Female | 15 | 17 | |
|
5–10 | 12 | 13 |
| 11–15 | 9 | 10 | |
| 16–20 | 15 | 17 | |
| 21–30 | 15 | 17 | |
| 31–40 | 15 | 17 | |
| 41 and above | 24 | 27 | |
|
Subsistence | 84 | 93 |
| Commercial | 6 | 7 | |
|
Medicinal plants only | 40 | 44.4 |
| Combination of medicinal plants and conventional medicine | 50 | 55.6 |
Gender plays a significant part in ethnoveterinary medicine, and the distribution of the participants by gender was 83% male and 17% female. A similar and common pattern indicated that livestock remain mostly in the care of males rather than females [16,32,33]. In Ethiopia, Assefa, and Bahiru [34] indicated that cattle rearing is under the command of males, which influences the imbalanced gender ratio in the practice of ethnoveterinary healthcare. On the other hand, the dominance of females was evidenced in a few studies from countries such as India [35] and China [28].
About 27% of the participants had extensive (more than 40 years) experience in cattle production (Table 1). In the Alaknanda catchment of Uttarakhand in India and the Buyi people of Southwest Guizhou in China, elderly people and male participants were more experienced and had more traditional knowledge of cattle production [28,35]. In the current study, 93% of participants were practicing subsistence farming, whereas a few (7%) engaged in commercial systems. The participants treated the cattle diseases/conditions using medicinal plants (44.4%) or the combination of medicinal plants and conventional medicine (55.6%). Similar results were reported in Eastern Cape, South Africa [36,37]. The use of both methods depended on the availability of funds to procure the conventional medicine, availability of veterinary services, knowledge of indigenous diagnostic methods and plants, value of the animal, and seriousness of the condition [38].
2.2. Common Cattle Diseases Treated Using Ethnoveterinary Medicine
Based on the Ruminant Veterinary Association of South Africa [39] and the classification in a previous study [40], the identified cattle diseases were classified into nine categories (Table 2). An inventory of disease conditions identified by the participants was recorded in a generated database with descriptions of disease categories, names in English and Setswana (local name), signs, and symptoms, causes, affected sex and age, and seasonality of outbreak. When compared to the western veterinary medical system, the naming of ailments by indigenous people did not always discriminate between ailments and symptoms of diseases. This is due to the fact that indigenous ailment nomenclature focuses on symptoms, but diseases in western veterinary science are based on aetiological knowledge [9].
Table 2.
Distribution of cattle diseases, causes, seasonality, sex, signs, and symptoms reported by participants in the study area. Nur denotes the number of usage reports for a certain disease category, whereas Nt denotes the variety of plants cited for the treatment of that specific ailment category, Fic = informant consensus factor.
| Disease Categories |
Diseases | Local Name | Citation | Nur | Nt | Fic | Signs and Symptoms | Causes | Sex | Seasonality of Diseases |
|---|---|---|---|---|---|---|---|---|---|---|
| Gastrointestinal problems | 120 | 53 | 0.56 | |||||||
| Dysentery | Letsholo le lehibidu | 4 | 1 | Same as diarrhoea, the difference is the colour, dysentery faeces are reddish | Unspecified | Both | All seasons | |||
| Diarrhoea | Letsholo | 32 | 23 | Watery faeces and pass them often, faeces are unusual colour and smell, sometimes blood in the faeces, back legs are dirty with faeces, become weak, tired, loss of appetite, appearing distressed and restless, weight loss, eyes sink into the head | Eating dry or green grass Feeding on grass containing worms (Kgorosane) |
Both | Summer Spring |
|||
| Bile reflux | Gala | 8 | 1 | Gall bladder is large and full of brown/green liquid, loss of appetite, loss of weight, dry nose, drowsy, and brownish sclera | Green grass | Both | Summer | |||
| Constipation | Go shokega mala | 76 | 28 | Passing dry, small, and hard faeces, no sign of faeces passed in the night, little dark urine, looking distressed when it passes faeces or urine, loss of appetite | Low intake of fluids | Both | All seasons | |||
| Tilt the affected ear downwards and may roll or lean to the affected side. | Unknown | Both | All seasons | |||||||
| General system infection | 63 | 8 | 0.88 | Weight loss, restless, loss of appetite, weak and tired, and has become very thin. | Not eating well | Both | All seasons | |||
| Ear pain | Bolwetsi jwa ditsebe | 25 | 3 | Stiff shoulders, loss of weight, loss of appetite, feeling bubbles under the skin, weak and tired, swelling legs, high fever | Change of seasons Insects in the grass Heat |
Both | Autumn and Winter | |||
| Malnutrition | Sekwepe | 10 | 1 | Saliva comes from the mouth, high fever, loss of appetite, blood in the urine, faeces, or milk, swelling under the jaw, neck, chest, and abdomen, become sick suddenly, difficulty breathing, collapse and die, dark blood comes from the mouth, nose, or anus when it is dead | Insects in the soil Too much blood |
Both | All seasons | |||
| Blackquarter | Serotswana | 5 | 1 | Difficulty in breathing, looking distressed and restless, lame, and cannot walk normally | Unknown | Both | All seasons | |||
| Anthrax | Lebete | 5 | 1 | Painful shoulders, isolation, stiff shoulders, loss of appetite, losing weight, walking with head down looking like it is carrying a heavy load, breathing heavy | Kicking stones Heat |
Both | All seasons | |||
| Heart problems | Bolowetsi jwa pelo | 10 | 1 | Tilt the affected ear downwards and may roll or lean to the affected side. | Unknown | Both | All seasons | |||
| Aphosphorisis | Mokokomalo/Magetla/lamsiekte | 8 | 1 | Weight loss, restless, loss of appetite, weak and tired, and has become very thin | Not eating well | Both | All seasons | |||
| Fertility/Reproduction disorders | 81 | 21 | 0.75 | |||||||
| Pain afterbirth | Ditlhabi tsa morago ga pelegi | 1 | 1 | Redness around vulva, swelling, warmth | Dystocia process of pulling the dead calf | Female | Summer–Autumn | |||
| Retained placenta | Motlhana | 69 | 10 | Placenta hanging from the vulva for a long time, smell bad if stay for a long time, restless | Unknown | Female | Summer–Autumn | |||
| Dystocia | Go farelwa | 11 | 10 | Breathing fast and heavily, moves from time to time/restless, unable to give birth | Not eating well Not enough water Running |
Female | Summer–Autumn | |||
| Skin problem | 190 | 33 | 0.83 | |||||||
| Foot rot | Dintho tsa dikgato | 5 | 1 | Swelling between the two hooves and legs, limping and lifting the affected leg, the flesh between the two claws that looks damaged, hard, or cut, wound or cut is smelling bad | Cow walking in the rainwater | Both | Summer | |||
| Abscess | Ditlhagala/Knopsik | 41 | 14 | Hard, hot, and painful swelling on the body but often just under the skin, that becomes soft, grey/white/green/yellow fluid comes out when it bursts, foot smells or is hot and painful, loss of appetite | Rainwater Dirty blood |
Both | Summer Spring Autumn |
|||
| Lumpy skin disease | Ditompola | 68 | 1 | Lots of saliva, clear discharge comes from the eyes and grey/white mucus from the nose, weak and tired, hard lumps appear on the body, hair around and on the lumps stands up, loss of appetite | Change of seasons | Both | Summer | |||
| Wounds | Dintho | 76 | 17 | A cut on any outside part of the body, loss of appetite | Cut from objects | Both | All seasons | |||
| Internal and external parasites | 91 | 12 | 0.87 | |||||||
| Worms | Dibokwana | 50 | 10 | Weight loss, loss of appetite, skin rough, swelling throat, breathing problem, bloody diarrhoea with mucus, dehydration | Bad food. | Both | All seasons | |||
| Ticks | Dikgoa | 41 | 2 | Licking and rubbing at the bite sites, lack of energy, loss of condition, tick sores and ulceration, pale parts around the eyes due to anaemia | Exposed to the cattle with ticks | Both | All seasons | |||
| Musculoskeletal systems | 124 | 14 | 0.89 | |||||||
| Muscle pain | Ditlhabi | 10 | 4 | Facial expressions | Diseases | Both | All seasons | |||
| Arthralgia | Ditlhabi tsa malokololo | 69 | 8 | Facial expressions | Diseases | Both | All seasons | |||
| Fracture | Go robega | 45 | 2 | Lame and limp, hold a broken leg off the ground and does not put any weight on that leg, when pressed under the foot it feels the pain, and swelling around the broken leg when touched you can feel broken ends of the bone, look distressed and restless, you can hear a grinding noise of the broken bones | Objects Kicking stones Losing step when running |
Both | All seasons | |||
| Respiratory problems | 100 | 25 | 0.76 | |||||||
| Cough | Go gotlhola | 42 | 23 | Lost weight, looks weak and tired, cough most of the time, loses appetite, sneeze, white/yellow mucus coming out of the nose, the problem with breathing | Change of seasons Cold |
Both | Summer– Winter |
|||
| Lung diseases | Lamsik/makgwafo a botlhoko | 9 | 1 | Loss of appetite, appearing distressed and restless, weight loss, has become thin, breathing problems | Heat | Mostly Female | Spring | |||
| Lung congestion | Galbater/metsi mo mafatlheng | 45 | 1 | Not eating as much as normal, weight loss, looking distressed and restless, breathing problems | Eating dry grass | Both | Autumn– Winter | |||
| Tick-borne | 5 | 1 | 1 | |||||||
| Heartwater | Bolwetsi jwa metsi mo pelo | 5 | 1 | Diarrhoea and signs of bleeding from the anus, move-in violent and convulsive, blood in faeces, grinding their teeth, lifting their legs up very high when they walk, loss of appetite, the sac around the heart, chest, and abdomen is full of fluid, collapse and die | Ticks | Both | All seasons | |||
| Eye problem | 55 | 10 | 0.83 | |||||||
| Eye infection | Botlhoko jwa matlho | 55 | 10 | Walks into objects, quick movement when an object comes towards the eye, the eye is red, and the eyelids are swollen, it blinks a lot and avoids bright sunlight, watery/yellowish discharge that smell bad comes out of an eye, look distressed and restless, the skin under the eyelids turn red, loss of appetite | Sharp objects pricking, insects, flies, or dust | Both | All seasons |
The participants identified 27 cattle diseases prevalent in the study area (Table 2). The most often cited ailments were wounds and constipation (76); arthralgia and retained placenta (69); and lumpy skin disease (68). The categories with the highest plant species used were gastrointestinal problems (53), skin problem (33), respiratory problem (25), and fertility/reproduction disorders (21). The informant consensus factor (Fic) is determined by the availability of plants in the study area for ailments treatment. The Fic values in this study varied from 0.56 to 1, with an average of 0.80, indicating a high level of agreement among the participants on the use of plants to treat cattle ailments. Tick-borne diseases had the highest Fic (1), followed by musculoskeletal systems (Fic = 0.89), and general system infection (Fic = 0.88). The high Fic values observed in this study show reasonably reliable knowledge of medicinal plants among the participants. A high Fic value is commonly associated with a few specific plants that have high use reports for treating a single disease category, whereas low values are associated with plants that have almost equal or high UR, implying a lower level of agreement among participants on the use of these plants to treat a specific disease category.
2.3. Diagnostic Skills, Treatment Methods, and Endpoint Determination
Participants reported signs and symptoms of cattle diseases/conditions, which they use for diagnosis. Seventy-five distinct clinical signs and symptoms of disease were reported by participants in this study. The most common ones were weight loss, loss of appetite, swelling, weakness and tiredness, breathing problem, distress, restless and discomfort, and blood in the faeces (Table 2). Different clinical signs and symptoms were based on the identified diseases. The current findings suggest a high degree of common perception between ethnoveterinary medicine and conventional veterinary systems. The descriptions of cattle ailments were mostly not like that of the conventional veterinary system, as the participants used signs and symptoms. In some cases, there were some similarities. For example, in terms of tick infestation, participants identified six distinct clinical signs and symptoms corresponding closely to conventional veterinary system concepts of external parasites conditions.
2.4. Plants identified as Ethnoveterinary Medicine for Treating Cattle Diseases
In this study, 64 plants were documented as medicine used against cattle diseases (Table 3). The current inventory was higher when compared to those documented in previous studies conducted in the North West Province [25,33,40]. This study reports on new plants that were not documented in earlier studies [25,33]. Particularly, 18 plants (28.13%) were described as ethnoveterinary medicine in treating cattle for the first-time (Table 3). The RFC indicates the local importance of plant species with reference to the participants, who cited the uses of these plants [41]. In the study, the RFC ranged from 0.12 to 0.83. Based on the RFC values, the most cited plant species were Gomphocarpus fruticosus (L.) W.T.Aiton (0.83), Opuntia ficus-indica (L.) Mill. (0.82), Schkuhria pinnata (Lam.) Kuntze ex Thell. and Portulaca oleracea L. (0.81), and Solanum lichtensteinii Willd. (0.77).
Table 3.
Medicinal plants used to treat various cattle ailments in the Ramotshere Moiloa local municipality (FC = number of participants who reported using a certain species, UV = use-value, Ui = the number of uses stated by each participant for a specific species, RFC = relative frequency of citation, * = plants possibly identified for the first time used for treating cattle diseases as no records were found). The nomenclature of all the collected plant species has been updated using The World Flora Online (http://www.worldfloraonline.org/, accessed on 22 March 2022). I Indigenous and $ introduced/cultivated/naturalised plants were based on Plants of Southern Africa (POSA) (http://posa.sanbi.org/, accessed on 16 June 2022) and the African Plant Database (https://africanplantdatabase.ch/, accessed on 22 June 2022).
| Scientific Name Voucher Specimen Number |
Local Name | Family | FC | Ui | UV | RFC | Plant Part(s) | Disease/ Ailments Treated |
Mode of Preparation | Administration Route |
|---|---|---|---|---|---|---|---|---|---|---|
|
IAcrotome inflata Benth. MVCHA 01 |
Mogato | Lamiaceae | 15 | 2 | 0.022 | 0.16 | Leaves | Cough | Decoction | Oral |
| Whole plant | Wounds | Burn | Topical | |||||||
| IAloe greatheadii Schönland MVCHA 02 | Kgopane e nyane | Xanthorrhoeaceae | 20 | 7 | 0.077 | 0.22 | Leaves | Constipation, diarrhoea, retained placenta | Decoction or infusion | Oral |
| Ticks, abscesses. Wounds, muscle pain | Ground | Topical | ||||||||
|
$Aloe vera (L.) Burm.f. MVCHA 03 |
Kgopane ya thaba | Xanthorrhoeaceae | 67 | 3 | 0.033 | 0.74 | Leaves | Abscess, wounds | Ground | Topical |
| Retained placenta, diarrhoea | Decoction or infusion | Oral | ||||||||
| $* Amaranthus cruentus L. MVCHA 05 | Modinakana | Amaranthaceae | 12 | 1 | 0.011 | 0.13 | Whole plant | constipation | Ground | Oral |
| $Amaranthus spinosus L. MVCHA 04 | Setlepetlepe | Amaranthaceae | 12 | 3 | 0.033 | 0.13 | Roots and leaves | Abscess, wounds | Poultice | Topical |
| Whole plant | Ear pain | Ground | Topical | |||||||
| IAptosimum elongatum (Hiern) Engl. MVCHA 06 | Ditantanyane | Scrophulariaceae | 11 | 1 | 0.011 | 0.12 | Whole plant | Arthralgia | Decoction | Oral |
| IArtemisia afra Jacq. ex Willd. MVCHA 07 | Lengana | Compositae | 69 | 4 | 0.044 | 0.76 | Leaves | Cough, intestinal worms, arthralgia | Decoction | Oral |
| Ear pain | Ground | Topical | ||||||||
| I* Asparagus africanus Lam. (Asparagus cooperi Baker) MVCHA08 | Thokabotswaro | Asparagaceae | 15 | 1 | 0.011 | 0.16 | Roots and stems | Malnutrition | Infusion | Oral |
| IAsparagus laricinus Burch. MVCHA 09 | Lesitwane | Asparagaceae | 20 | 1 | 0.011 | 0.22 | Whole plant | Muscle pain | Decoction | Oral |
| IAsparagus suaveolens Burch. MVCHA 010 | Motantanyane | Asparagaceae | 15 | 1 | 0.011 | 0.16 | Whole plant | Dystocia | Decoction | Oral |
| I* Babiana hypogea Burch. MVCHA 011 | Thuge | Iridaceae | 20 | 2 | 0.022 | 0.22 | Leaves | Abscess, muscle pain | Infusion | Oral |
|
$* Boerhavia diffusa L. MVCHA 018 |
Moetapele | Nyctaginaceae | 45 | 3 | 0.033 | 0.5 | Leaves and stems | Eye infection, abscess, wounds | Decoction | Topical |
| IBoophone disticha (L.f.) Herb. MVCHA 012 | Lesoma/Mathubadudifala | Amaryllidaceae | 45 | 1 | 0.011 | 0.5 | Leaves, roots, and bulb | Constipation | Decoction | Oral |
| IBulbine abyssinica A.Rich. MVCHA 013 | Makgabenyane | Xanthorrhoeaceae | 30 | 3 | 0.033 | 0.33 | Leaves | Abscess, wounds | Grounded | Topical |
| ICassine transvaalensis (Burtt Davy) Codd [Elaeondendron transvaalense (Burtt Davy) R.H. Archer] MVCHA 014 | Mojelemane | Celastraceae | 12 | 1 | 0.011 | 0.13 | Barks | Diarrhoea | Decoction | Oral |
| I* Centella asiatica (L.) Urb. MVCHA 015 | Setimamolelo | Apiaceae | 12 | 4 | 0.044 | 0.13 | Leaves | Wound, abscess, eye infection | Poultice | Topical |
| Whole plant | Diarrhoea | Decoction | Oral | |||||||
|
I* Cleome gynandra L. MVCHA 016 |
Rothwe | Cleomaceae | 35 | 6 | 0.066 | 0.38 | Flower | Eye infection, ear problem | Grounded | Topical |
| leaves | Wounds | Grounded | Topical | |||||||
| Roots and leaves | Cough, constipation, intestinal worms | Infusion or decoction | Oral | |||||||
| ICombretum hereroense Schinz MVCHA 017 | Tsholakhudu | Combretaceae | 25 | 4 | 0.044 | 0.27 | Leaves | Cough, pains, dysentery, constipation | Decoction | Oral |
| ICroton gratissimus Burch. MVCHA 019 | Moologa | Euphorbiaceae | 22 | 2 | 0.022 | 0.24 | Flower | Eye infection, ear problem | Grounded | Topical |
| IDicerocaryum senecioides (Klotzsch) Abels (Sesamum senecioides (Klotzsch) Bung & Christenh. MVCHA 020 | Tshetlho ya mamitlwa a mabedi | Pedaliaceae | 57 | 3 | 0.033 | 0.63 | Leaves | Blackquarter | Poultice | Topical |
| Whole plant | Retained placenta, dystocia | Poultice and infusion | Oral | |||||||
| IDichrostachys cinerea (L.) Wight & Arn. MVCHA 021 | Moselesele | Fabaceae | 23 | 4 | 0.044 | 0.25 | Barks | Retained placenta, dystocia, fracture, arthralgia | Poultice | Topical |
| IDicoma macrocephala DC. MVCHA 022 | Tlhonya | Compositae | 34 | 1 | 0.011 | 0.37 | Roots | Diarrhoea | Infusion | Oral |
| IDrimia sanguinea (Schinz) Jessop MVCHA 023 | Sekaname | Hyacinthaceae | 45 | 3 | 0.033 | 0.5 | Bulb | Retained placenta, intestinal worms, constipation | Infusion | Oral |
|
$* Dysphania ambrosioides (L.) Mosyakin & Clemants MVCHA 024 |
Tlhatlhabadimo | Amaranthaceae | 56 | 2 | 0.022 | 0.62 | Whole plant | Cough, constipation | Infusion | Oral |
| IElephantorrhiza burkei Benth. MVCHA 026 | Mositsane | Fabaceae | 68 | 4 | 0.044 | 0.75 | Roots | Cough, constipation, retained placenta | Decoction | Oral |
| Diarrhoea | Ground | Topical | ||||||||
| Barks | Cough | Decoction | Oral | |||||||
| IEuclea undulata Thunb. MVCHA 070 | Morobe | Ebenaceae | 67 | 6 | 0.066 | 0.74 | Leaves | Wounds | Poultice | Topical |
| Bark and roots | Diarrhoea, arthralgia | Decoction | Oral | |||||||
| Roots | Cough, constipation, retained placenta | Decoction | Oral | |||||||
| $* Euphorbia balbisii Boiss (Euphorbia serpens Kunth) MVCHA 027 | Lwetsane | Euphorbiaceae | 12 | 2 | 0.022 | 0.13 | Leaves and roots | Diarrhoea, intestinal worms | Decoction | Oral |
| IGomphocarpus fruticosus (L.) W.T.Aiton MVCHA 028 | Motimola/sebogamaswi | Apocynaceae | 75 | 4 | 0.044 | 0.83 | Whole plant | Constipation, retained placenta, cough, bile reflux | Infusion | Oral |
|
IGrewia flava DC. MVCHA 029 |
Moretlwa | Malvaceae | 23 | 2 | 0.022 | 0.25 | Roots | Diarrhoea, dystocia | Infusion | Oral |
| I* Grewia flavescens Juss. MVCHA 030 | Motsotsojane | Malvaceae | 34 | 3 | 0.033 | 0.37 | Leaves | Pain, wounds, diarrhoea | Infusion | Oral |
| IHarpagophytum procumbens (Burch.) DC. ex Meisn. MVCHA 031 | Lematla/Sengaparile | Pedaliaceae | 45 | 6 | 0.066 | 0.5 | Tuber | Dystocia, pain after birth | Decoction | Oral |
| Abscess, fracture, muscle pain | Ground | Topical | ||||||||
| Roots, leaves, and fruit | Retained placenta | Decoction | Oral | |||||||
|
IHelichrysum candolleanum H.Buek MVCHA 032 |
Phateyangaka | Compositae | 56 | 1 | 0.011 | 0.62 | Roots, leaves and fruit | Retained placenta | Decoction | Oral |
|
IHypoxis hemerocallidea Fisch., C.A. Mey. & Avé-Lall. MVCHA 034 |
Maledu/Tshuku ya poo | Hypoxidaceae | 69 | 4 | 0.044 | 0.76 | Whole plant | Cough, dystocia, arthralgia, constipation | Decoction | Oral |
| IJatropha zeyheri Sond. MVCHA 035 | Seswagadi | Euphorbiaceae | 67 | 3 | 0.033 | 0.74 | Root | Eye infections, constipation | Maceration | Topical |
| Retained placenta | Decoction | Topical | ||||||||
|
IKleinia longiflora DC. MVCHA 036 |
Mosimama | Compositae | 65 | 1 | 0.011 | 0.72 | Whole plant | Eye infection | Poultice | Topical |
| I* Lippia scaberrima Sond. MVCHA 037 | Mosukutswane | Verbenaceae | 54 | 1 | 0.011 | 0.6 | Leaves | Cough | Decoction | Oral |
|
$* Malva neglecta Wallr. MVCHA 038 |
Tikamotse | Malvaceae | 43 | 4 | 0.044 | 0.47 | Leaves and flowers | Constipation, wounds, abscess, cough | Decoction | Oral |
| $Malvastrum coromandelianum (L.) Garcke MVCHA 054 | Thobega | Malvaceae | 12 | 4 | 0.044 | 0.13 | Leaves | Diarrhoea, abscess, wounds, ear pain | Decoction | Oral |
|
I* Mentha aquatica L. MVCHA 039 |
Kgobedimetsing | Lamiaceae | 32 | 1 | 0.011 | 0.35 | Leaves | Cough | Decoction | Oral |
| $Opuntia ficus-indica (L.) Mill. MVCHA 040 | Toorofeye | Cactaceae | 74 | 5 | 0.055 | 0.82 | Leaves and stem | Diarrhoea, constipation, eye infections | Decoction | Oral |
| Flower | Retained placenta, abscess | Ground | Topical | |||||||
| Bulb | Retained placenta | Maceration | Topical | |||||||
| IOzoroa paniculosa (Sond.) R. Fern. & A. Fern. MVCHA 042 | Monokana | Anacardiaceae | 24 | 2 | 0.022 | 0.26 | Roots | Cough, muscle pain | Decoction | Oral |
| IPeltophorum africanum Sond. MVCHA 043 | Mosetlha | Fabaceae | 35 | 5 | 0.055 | 0.38 | Roots | Wounds, muscle pain | Decoction | Oral |
| Stem and root | Diarrhoea, constipation | Decoction | Oral | |||||||
| Root, Leaves, and bark | Intestinal worms | Decoction | Oral | |||||||
| I* Phyllanthus maderaspatensis L. MVCHA 044 | Mositwane | Phyllanthaceae | 30 | 3 | 0.033 | 0.33 | Whole plant | Eye infection | Ground | Topical |
| Roots | Constipation, diarrhoea | Decoction | Oral | |||||||
| I* Plumbago zeylanica L. MVCHA 045 | Masegomabe | Plumbaginaceae | 57 | 2 | 0.022 | 0.63 | Whole plant | Cough, intestinal worms | Decoction | Oral |
|
$* Portulaca oleracea L. MVCHA 046 |
Selele | Portulacaceae | 73 | 5 | 0.055 | 0.81 | Whole plant | Constipation, eye infection, muscle pain, wounds, intestinal worms | Decoction | Oral |
| IPouzolzia mixta Solms MVCHA 047 | Mongololo | Urticaceae | 68 | 3 | 0.033 | 0.75 | Roots and leaves | Retained placenta | Maceration | Oral |
| Roots | Diarrhoea | Decoction | Oral | |||||||
| Constipation | Infusion | Oral | ||||||||
|
$Ricinus communis L. MVCHA 048 |
Mokhura | Euphorbiaceae | 13 | 2 | 0.022 | 0.14 | Leaves | Constipation, eye infection | Infusion | Oral |
| I* Sansevieria hyacinthoides (L.) Druce [Dracaena hyacinthoides (L.) Mabb.] MVCHA 049 | Moshokelatsebe | Ruscaceae | 24 | 2 | 0.022 | 0.26 | Leaves | Retained placenta | Poultice | Topical |
| Whole plant | Cough | Decoction | Oral | |||||||
| $Schkuhria pinnata (Lam.) Kuntze ex Thell. MVCHA 050 | Santlhoko | Compositae | 73 | 7 | 0.077 | 0.81 | Whole plant | Eye infection, wounds, abscess | Ground | Topical |
| Diarrhoea, constipation, heartwater, lung congestion | Decoction | Oral | ||||||||
| ISearsia lancea (L.f.) F.A.Barkley MVCHA 051 | Moshabela | Anacardiaceae | 30 | 3 | 0.033 | 0.33 | Roots, leaves, and stem | Abscess | Poultice | Roots, leaves and stem |
| Roots | Constipation, diarrhoea | Infusion | Roots | |||||||
| ISearsia pyroides (Burch.) Moffett MVCHA 052 | Bohitlha | Anacardiaceae | 57 | 6 | 0.066 | 0.63 | Leaves | Cough | Decoction | Oral |
| Leaves | Cough, dystocia, constipation, diarrhoea, intestinal worms, arthralgia | Decoction | Oral | |||||||
| $* Securidaca longipedunculata Fresen. MVCHA 053 | Mmaba | Polygalaceae | 68 | 4 | 0.044 | 0.75 | Roots | Cough, Dystocia, constipation, muscle pain | Ground | Topical |
| ISenecio consanguineus DC. MVCHA 033 | Compositae | 67 | 3 | 0.033 | 0.74 | Whole plant | Cough, wounds, constipation | Decoction | Oral | |
|
ISenna italica Mill. MVCHA 055 |
Sebetebete | Fabaceae | 55 | 7 | 0.077 | 0.61 | Leaves | Constipation, abscess, anthrax, aphosphorosis, lung diseases | Decoction | Oral |
| Bark | Pain, diarrhoea, constipation | Decoction | Oral | |||||||
| ISolanum lichtensteinii Willd. MVCHA 059 | Tolwane | Solanaceae | 70 | 1 | 0.011 | 0.77 | Whole plant | Ticks | Poultice | Topical |
| $Solanum nigrum L. MVCHA 060 | Makgonatsotlhe | Solanaceae | 33 | 1 | 0.011 | 0.36 | Roots | Intestinal worms | infusion | Oral |
| ISolanum campylacanthum A. Rich. (Solanum panduriforme Dunal) MVCHA 071 | Tolwane enyane | Solanaceae | 44 | 2 | 0.022 | 0.48 | Roots | Diarrhoea | Infusion | Oral |
| Leaves | Eye infection | Maceration | Topical | |||||||
| ITarchonanthus camphoratus L. MVCHA 061 | Mohatlha | Compositae | 33 | 1 | 0.011 | 0.36 | Roots | Intestinal worms | infusion | Oral |
| ITerminalia sericea Burch. ex DC. MVCHA 062 | Mogonono | Combretaceae | 44 | 1 | 0.011 | 0.48 | Leaves and stem | Cough | Decoction | Oral |
| ITeucrium sessiliforum Benth. (Teucrium trifidum Retz.) MVCHA 063 | Lethe la noga | Lamiaceae | 55 | 3 | 0.033 | 0.61 | Leaves and roots | Cough, diarrhoea, constipation | Decoction | Oral |
|
ITribulus terrestris L. MVCHA 064 |
Tshetlho | Zygophyllaceae | 66 | 5 | 0.055 | 0.73 | Leaves | Arthralgia | Ground | Oral |
| Whole plant | Dystocia, retained placenta | Decoction | Oral | |||||||
| . | Constipation | Decoction | Oral | |||||||
| I* Turbina oblongata A. Meeuse (Ipomoea oblongata E.Mey ex Choisy) MVCHA 065 | Mokatelo | Convolvulaceae | 11 | 4 | 0.044 | 0.12 | Roots | Cough, wounds, muscle pain, diarrhoea | Decoction | Oral |
| IVachellia karroo (Hayne) Banfi & Galasso MVCHA 066 | Mooka | Fabaceae | 67 | 1 | 0.011 | 0.74 | Bark | Lumpy skin disease | Decoction | Oral |
| IZiziphus mucronata Willd. MVCHA 068 | Sekgalo | Rhamnaceae | 40 | 6 | 0.066 | 0.44 | Roots | Dystocia, diarrhoea, arthralgia | Decoction | Oral |
| Leaves | Wounds, foot rot | Ground | Topical | |||||||
| Whole plant | Eye infection | Decoction | Oral |
The use-value (UV) is a measure of the types of uses attributed to a particular plant species. In the present study, Schkuhria pinnata (Lam.) Kuntze ex Thell., Senna italica Mill., and Aloe greatheadii Schönland had the highest UV (0.077) followed by Cleome gynandra L., Harpagophytum procumbens (Burch.) DC. ex Meisn., Ximenia caffra Sond. (0.066), and Ziziphus mucronata Willd., Senna italica Mill., Portulaca oleracea L., and Opuntia ficus-indica (L) (0.055) (Table 3). The extent to which a species may be employed is determined by its UV; hence, plantss with a high UV are more exploited in the research area to treat more diseases than those with a low UV. Plants with a higher number of use reports (UR) had higher UV, whereas plants with fewer UR by participants had lower UVs, whereas plants with fewer Ui reported by participants had lower UV. Generally, plants that are utilised repeatedly are more likely to be physiologically active [42]. Given that UV and RFC values are dynamic and alter with location and people’s awareness, UV and RFC values may vary from area to area and even within the same study area [43]. Plants with lower UV and RFC values are not necessarily unimportant, but their low values may indicate that the participants are unaware of the uses of these plants and, as a result, that understanding of their use is at risk of not being passed down to future generations, and thus this knowledge may eventually disappear. Some of the documented plants are indigenous to the study area and are well-known to the participants. As a result, their specialised qualities for healing various ailments have become well-known and well-established among the participants. Plants with higher UV and RFC are likely to be good candidates for future research. It will be essential to subject these plants to pharmacological, phytochemical, and biological investigation to establish their therapeutic potential and the potential development of low-cost products [44].
In the current study, the recorded medicinal plants consisted of indigenous (native) and non-endemic plants used against various cattle diseases by the participants of Ramotshere Moloa local municipality. Among the plants, 50 (78.1%) were indigenous/native while 14 (21.8%) were introduced/cultivated/naturalised (Table 3). High levels of usage of these indigenous/native species, particularly those with high use categories, might be of conservation concern if conducted in an unsustainable manner [14]. Thus, there is a great need to discover new biologically active compounds from herbal plants and develop novel drugs. Few studies are available about EVM plants and their constituents with antimicrobial activities [1,8], and these indigenous plants may contain pharmaceutically essential compounds. To further understand the uniqueness of this EVM, a more in-depth study of how these indigenous plants is used and selected, as well as a comparison study with other sites/locations within South Africa is required. In addition, a closer look at the local conservation status is required to build a sustainable use plan for these valuable plant resources [23].
2.5. Therapeutic Uses of Combined Medicinal Plants
Participants in the current study reported nine (14.1%) plants from the inventory that had numerous indications (uses), as poly-plant remedies. These results reflect the diversity of ethnic knowledge and heterogeneity in cultural practices. For example, participants reported using a combination of the leaves of Artemisia afra Jacq. ex Willd., Mentha aquatica L., Dicoma macrocephala DC., and Lippia scaberrima Sond., and mixing them with donkey milk to cure cough, intestinal worms, and joints pain. A decoction of Drimia sanguinea (Schinz) Jessop bulb and the roots of Elephantorrhiza burkei Benth. and Senna italica Mill. was administered orally to treat intestinal worms. To treat constipation, a decoction of the roots of Elephantorrhiza burkei Benth., Peltrophorum africanum Sond., and Jatropha zeyheri Sond. is administered orally. The potency of using a combination of different plants or plant parts increased compared to using a single plant to cure a disease is well-recognised [25,40,45]. Validation and transmission of this knowledge to livestock raising farmers all over the world so that they know the best plant material near them for the specific ailment will benefit people not only in impoverished nations but also in the developed world [46]. The use of two or more plants exemplifies the notion of synergy, which highlights that the combination of plants might result in higher therapeutic efficacy [32,47].
2.6. Plant Families Used to Treat Cattle Diseases
In terms of family diversity, 32 families were used to treat and manage cattle diseases in the study area (Figure 1). The families with the largest number of plant species used to treat cattle were Compositae with seven species and Fabaceae and Asparagaceae (five species). Compositae and Fabaceae are the most widely used families in ethnoveterinary studies [18,48,49,50]. Similar studies have been reported where participants mostly used the members of Compositae for the preparation of EVM for the treatment of different livestock diseases [40,51,52]. Furthermore, the widespread use of plants from these dominant families might be attributed to strong traditional beliefs, availability, ease of harvesting, and storage, as well as the evidence of bioactive compounds with therapeutic effect against cattle ailments. However, the trend for plant families utilised to cure cattle ailments in the selected communities differs from those used in other locations in South Africa [33,53].
Figure 1.
Frequency of the 32 plant families used in the treatment of cattle diseases in the Ramotshere Moiloa local municipality, North West Province, South Africa.
2.7. Distribution of Plant Parts Used to Treat Cattle Diseases
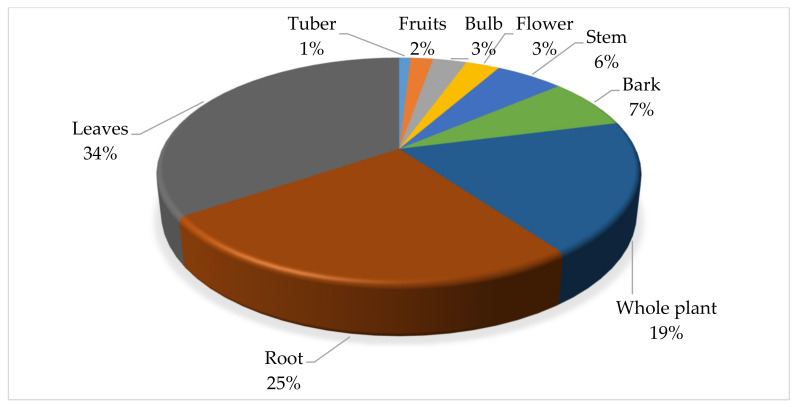
In the study area, different plant parts were used for the preparation of remedies for treating cattle diseases (Figure 2). The most frequently used plant parts were the leaves (34.55%), roots (25.45%), and whole plant (19.09%). The preference of leaves in treating cattle ailments is due to their easy availability, easy harvesting, and simplicity in remedy preparation. Leaves are the storage site of diverse pools of phytochemicals, the renewable parts of plants, and for a conservation perspective, their collection may not result in the fatality of the mother plants [54]. A similar trend whereby the leaves were the dominant plant part used in medicine preparation for treating cattle diseases was reported in other studies [51,55,56,57,58]. However, in some cases, the roots were identified as the commonly used plant parts [9,33,40]. Roots were the second most commonly utilised plant part, which might be attributed to the fact that roots remain in the soil and are easily accessible even during extended dry seasons in arid and semi-arid environments [59]. However, this is frequently not suggested because it is harmful and unsustainable, putting plant species at risk of extinction [60].
Figure 2.
Distribution (%) of plant parts value used in the treatment of cattle diseases in Ramotshere Moiloa local municipality, North West Province, South Africa. (n = 110).
2.8. Method of Preparation and Route of Administration of Medicinal Plants Used to Treat Cattle Diseases
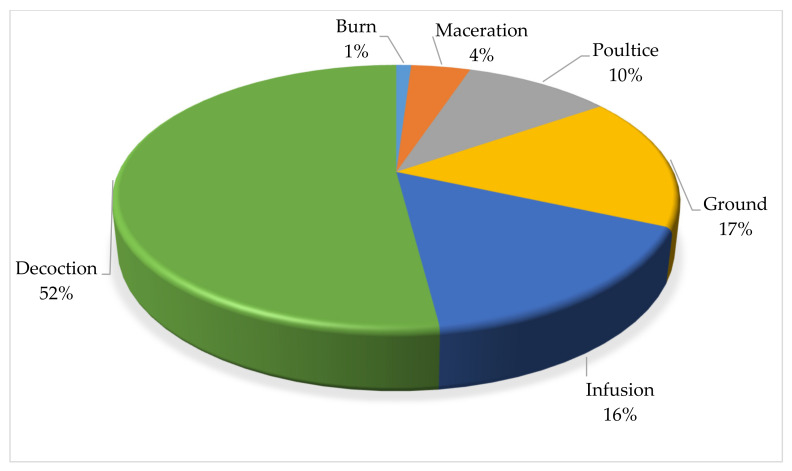
As depicted in Figure 3, the herbal remedies were mainly prepared as decoction (52.04%), ground, and infusion (16.33%). Other ways of preparation were maceration, poulticing, and burning which cumulatively accounted for 31.63%. Decoction is the process of boiling plant components in water and then allowing the liquid to cool before administering. Decoction is a popularpreparation methodthat has been mentioned in several different research studies [48,61,62]. The preparation method differs from other study areas including Karamoja in Uganda [63], the Mana Angetu district of south-eastern Ethiopia [64], and Yalo Woreda in the Afar regional state, Ethiopia [65], where crushing and pounding were the most common methods. The widespread usage of decoction might be attributed to the fact that boiling can accelerate biological processes, resulting in the greater availability of several active compounds [66]. However, preparation procedures vary based on the type of sickness being treated, the location of the condition, and the medicinal components to be extracted [67].
Figure 3.
Distribution (%) of preparation methods for plants used in the treatment of cattle diseases in Ramotshere Moiloa local municipality, North West Province, South Africa (n = 98).
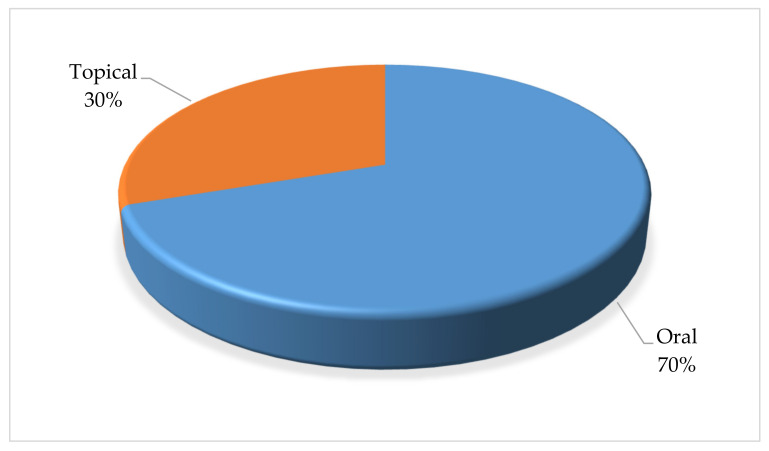
Furthermore, the local communities use a variety of methods to administer the plants when treating cattle diseases (Figure 4). The route of administration for the plants was oral (69.79%) and topical (30.2%). Oral administration is a simple and non-invasive form of systemic treatment. The route allows for the rapid absorption and distribution of the prepared medicines and allowing for sufficient curative power to be delivered [68]. Across many African cultures, oral administration of medicinal plants is the most common route used to treat disease in cattle, as this ensures fast and direct interaction with different plant compounds at the site of action [69,70,71].
Figure 4.
Distribution (%) pattern for the administration of plants used in the treatment of cattle diseases in Ramotshere Moiloa local Municipality, North West Province, South Africa (n = 96).
3. Materials and Methods
3.1. Study Area
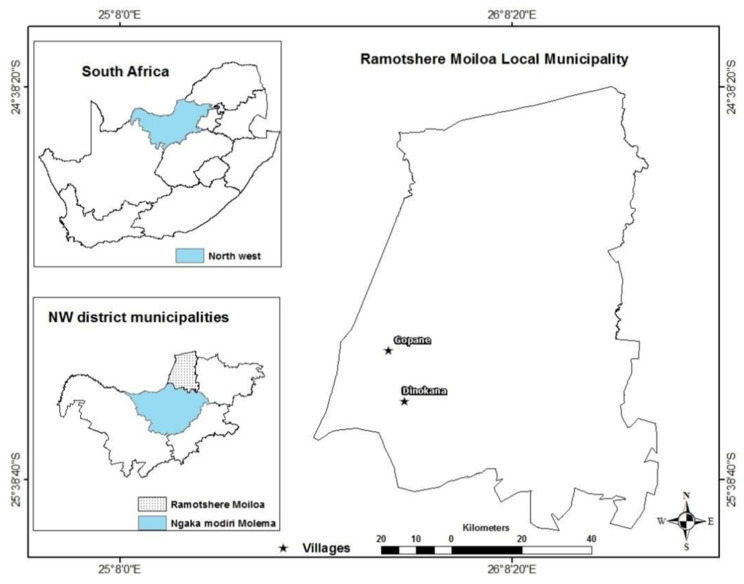
This study was conducted in the Gopane (25.3175° S, 25.8231° E) and Dinokana (25.456° S, 25.8799° E) villages of the Ramotshere Moiloa local municipality (25.5623° S, 26.1001° E) located in the Ngaka Modiri Molema district municipality, North West Province of South Africa (Table S1 and Figure 5). Dinokana and Gopane are bordered to the north by Botswana, to the east by Moses Kotane and Kgetleng River local municipalities, and to the south by Ditsobotla and Mafikeng local municipalities [72]. The two communities are dominantly rural area under the leadership of traditional leader and municipality councillors. The area is rich in floras with potential diverse applications [73]. The total surface of both communities is 104,882 km2. Livestock and agricultural productions provide a significant contribution to the rural economy in the study region, and most rural farming systems transport and generate money both directly and indirectly.
Figure 5.
Location of the Dinokana and Gopane villages in the Ramotshere Moiloa local municipality, North West Province, South Africa.
The households are active in agricultural activities such as livestock (16,443) and vegetable (1110) production. Particularly, cattle production, consisting of 11,892 households, remains the highest agricultural activity in these communities. The annual income category of agricultural household heads starts from R1 to above R1 228,800 [72], and according to the Ruminant Veterinary Association of South Africa [39], the most prevalent animal diseases in the study are internal parasites, external parasites, tick-borne diseases, insect transmittable diseases, venereal diseases, bacterial diseases, and protozoal diseases. The two communities were selected due to the rich plant biodiversity which serves as an important medicinal resource [74]. Increased population growth, cultural changes such as the rapid shift toward allopathic medicine, and the spread of modern education contribute to the destruction of medicinal plant habitats and the increasing loss of indigenous knowledge due to changes in community inhabitants. Previously, Van der Merwe, Swan, and Botha [33] documented the ethnoveterinary medicine knowledge of the Madikwe community and Ndou [40] focused on the EVM in Mahikeng, whereas another study focused on the medicinal plants used for retained placenta [25].
3.2. Ethnobotanical Survey
An ethnobotanical field survey was conducted from August 2019 to October 2020 (Spring until Summer) in the Dinokana and Gopane villages of the Ramotshere Moiloa local municipality, South Africa (Figure 5). Snowballing was used to recruit and screen eligible participants [75,76]. Ninety participants (83% were male and 17% female) were purposively selected to participate in the study. The age of participants ranged from 18 to 95 and the participants consisted of indigenous knowledge holders, farmers, and cattle herders. The experience and knowledge of participants on the theme of the study, and their interest in participating, were applied as the inclusion criteria [77].
A face-to-face interview using a semi-structured interview guide prepared in English and translated to Setswana (local language) was used to collect data, after presenting the purpose of the study to the participants, and data was subsequently translated to English. The semi-structured interview guide yielded insightful knowledge for the researcher to develop and generate a rich understanding of the knowledge and skills related to ethnoveterinary [78]. The data collection questionnaire was divided into three sections to obtain required information. Two phases were followed to collect data. The first phase was interviews, and the second involved a field walk and the collection of plants. Following the Alexiades and Sheldon [79] technique, responses of participants that contradicted each other were not considered for analysis. The data generated from individual interviews were cross-checked with other participants in the same villages to obtain reliable information in the study area [80].
The Faculty of Natural and Agricultural Sciences Research Ethics Committee (FNASREC) at the North-West University reviewed and approved the study (Ethics approval number: NWU-01228-19-S9). Traditional authorities in the local municipality granted permission and access to conduct the study in the communities. Prospective participants were approached to seek their consent to participate in the study following detailed and clear explanation on the purpose of the research. The North West Department of Rural, Environmental, and Agricultural Development (NW-READ) granted authorisation for plants collection in the two villages (Permit number HQ 26/01/18-006 NW).
Field observations were conducted in study areas to collect the plants mentioned during interviews. Plants were identified by participants and collected by researchers during field walks. Plants used to treat cattle diseases were collected using standard procedures/techniques [81]. Voucher specimens for the plants were prepared and deposited in the SD Phalatse (UNWH) and AP Goossens Herbarium (PUC) at the North-West University. The nomenclature of all the collected plants was verified using The World Flora Online (http://www.worldfloraonline.org/, accessed on 22 March 2022).
3.3. Data Analysis
Thematic content and ethnobotanical indices were used to analyse the data collected on indigenous diagnostic skills and ethnobotanical knowledge provided by participants. Thematic content analysis was used to analyse qualitative data [82]. Following the interviews, the data was transcribed and verified for coherence and saturation. The information from various participants was compared to each other to uncover trends and themes. The emergent themes were linked to data sections with corresponding codes such as participant socio-demographic information, frequently identified cattle ailments, diagnostic procedure, and medicinal plant usage process. When no new data, codes, or themes came from the material, it was considered that saturation had been reached. The ethnobotanical knowledge data were analysed using informant consensus factor (Fic), use-value (UV), and relative frequency of citation (RFC) as described below:
Informant consensus factor (Fic): relevant for the categories of diseases to identify the agreement of participants on the reported cures for the group of diseases [83], which was calculated as follows:
where Nur denotes the number of usage reports for a certain ailments category and Nt denotes the number of plants listed for the treatment of that ailment category.
Use value (UV): denotes the relative significance of species recognized locally [84]. The UV was used to identify the plants with the highest utilisation translating to the most frequently mentioned in the treatment of cattle disease [85]. It was calculated as follows:
where Ui: is the number of uses stated by each participant for a specific species and N: denotes the total number of participants. If a plant secures a high UV score, that indicates that there are many use reports for that plant, whereas a low score indicates fewer use reports cited by the participants.
Relative frequency of citation (RFC): as described by Tardío and Pardo-de-Santayana [86], this measures the agreement among participants on the reported plants. This index calculates the local relevance of each species by dividing the number of participants who mention the species’ use, also known as frequency of citation (FC), by the number of target participants included in the study (N). The RFC index was calculated using the following formula:
where FC is the number of participants who reported using a certain species and N denotes the total number of participants in the research. The factor has a value range of 0 to 1, with a high value indicating a high rate of participant consensus.
4. Conclusions
The selected communities are primarily rural in nature, and cattle farmers are exploring their biodiversity and indigenous knowledge practices for meeting the animal health needs and productivity. Based on the current findings, an inventory of 64 medicinal plants from 32 families with a specific indigenous/native rate of 78.1% used to treat 27 cattle ailments from nine categories was documented, with 18 new plants. Three diagnostic skills, 75 distinct clinical signs and symptoms of disease, and two endpoint determinations were reported to understand cattle diseases. Leaves as a plant part, decoction as a preparation method, and oral as an administration route were found to be the most frequently used systems in treating cattle diseases. The plants were prepared as monotherapy and combination. Even though the research area in the Ramotshere Moiloa local municipality was shown to be rich in medicinal plant variety, efforts to study the plants and the indigenous knowledge connected with them are currently limited. To avert additional losses, local communities and responsible entities must conserve therapeutic plants. Furthermore, plants with a high potential based on the applicable ethnobotanical indices should be selected for additional research, such as phytochemical analysis and pharmacological and toxicological studies.
Acknowledgments
We sincerely appreciate the willingness and active engagement by all the participants (Gopane and Dinokana villages) involved in the research. Sincere gratitude to Stefan Seibert for assisting with the identification and preparation of voucher specimen of the plants. We thank the tribal authority for allowing access to the study area and the research participants. We appreciate the valuable discussions and inputs by Kutullo Shai and Ebenezer Kwabena Frimpong. We thank the North-West University for institutional support.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/plants11131784/s1, Table S1: Demographic information of the study areas.
Author Contributions
Conceptualization, M.V.C., M.M. and A.O.A.; methodology, M.V.C.; formal analysis, M.V.C., J.A.A. and M.S.; investigation, M.V.C., J.A.A. and M.S.; resources, M.M. and A.O.A.; writing—original draft preparation, M.V.C.; writing—review and editing, J.A.A., M.S., M.M. and A.O.A.; supervision, M.M. and A.O.A.; project administration, A.O.A.; funding acquisition, A.O.A. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
The Faculty of Natural and Agricultural Sciences Research Ethics Committee (FNASREC) of the North-West University reviewed and approved (NWU-01228-19-S9) the research. In compliance with the Nagoya Protocol on Access to Genetic Resources and the Fair and Equitable Sharing of Benefits Arising from their Utilization to the Convention on Biological Diversity.
Informed Consent Statement
Informed consent was obtained from all the participants involved in the study. The study participants from the Gopane and Dinokana villages of the Ramotshere Moiloa local municipality retain the authorship of traditional knowledge documented in this publication. Therefore, any use of the documented information, other than for scientific publications, requires the prior consent of the traditional knowledge holders and their agreement on access to benefits resulting from any commercial use.
Data Availability Statement
Primary data collected during the survey are available upon request to the corresponding author of this manuscript.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in: the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Funding Statement
M.V.C. received financial support from the North-West University (NWU) Grow Our Timber scholarship, NWU Faculty of Natural and Agricultural Sciences postgraduate bursary, and Kopano Youth Club. A.O.A. acknowledges the financial support from the National Research Foundation (NRF Indigenous Knowledge Systems Grant no: 118585), Pretoria, South Africa. North-West University provided the article processing cost.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chakale M.V., Mwanza M., Aremu A.O. Ethnoveterinary knowledge and biological evaluation of plants used for mitigating cattle diseases: A critical insight into the trends and patterns in South Africa. Front. Vet. Sci. 2021;891:710884. doi: 10.3389/fvets.2021.710884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Varijakshapanicker P., Mckune S., Miller L., Hendrickx S., Balehegn M., Dahl G.E., Adesogan A.T. Sustainable livestock systems to improve human health, nutrition, and economic status. Anim. Front. 2019;9:39–50. doi: 10.1093/af/vfz041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mottet A., Teillard F., Boettcher P., De’Besi G., Besbes B. Domestic herbivores and food security: Current contribution, trends and challenges for a sustainable development. Animal. 2018;12:s188–s198. doi: 10.1017/S1751731118002215. [DOI] [PubMed] [Google Scholar]
- 4.Banda L.J., Tanganyika J. Livestock provide more than food in smallholder production systems of developing countries. Anim. Front. 2021;11:7–14. doi: 10.1093/af/vfab001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Jaarsveld B.D.L., Pieters B.D.H., Potgieter E.D.B., van Wyk G.D.N., Pfitzer K.D.S., Trümpelmann L.D., Malan S.L.D.M., Beytel N.D.A., Niebuhr P.R.D., Kroon W.S.D.K. Monthly Report on Livestock Disease Trends as Informally Reported by Veterinarians Belonging to the Ruminant Veterinary Association of South Africa (RuVASA), a Group of the South African Veterinary Association. Ruminant Veterinary Association of South Africa; Pretoria, South Africa: 2017. p. 28. [Google Scholar]
- 6.Dovie D.B., Shackleton C.M., Witkowski E. Valuation of communal area livestock benefits, rural livelihoods and related policy issues. Land Use Policy. 2006;23:260–271. doi: 10.1016/j.landusepol.2004.08.004. [DOI] [Google Scholar]
- 7.Maikhuri R. Eco-energetic analysis of animal husbandry in traditional societies of India. Energy. 1992;17:959–967. doi: 10.1016/0360-5442(92)90045-2. [DOI] [Google Scholar]
- 8.McGaw L.J., Eloff J.N. Ethnoveterinary use of southern African plants and scientific evaluation of their medicinal properties. J. Ethnopharmacol. 2008;119:559–574. doi: 10.1016/j.jep.2008.06.013. [DOI] [PubMed] [Google Scholar]
- 9.Tabuti J.R., Dhillion S.S., Lye K.A. Ethnoveterinary medicines for cattle (Bos indicus) in Bulamogi county, Uganda: Plant species and mode of use. J. Ethnopharmacol. 2003;88:279–286. doi: 10.1016/S0378-8741(03)00265-4. [DOI] [PubMed] [Google Scholar]
- 10.McCorkle C.M., Mathias-Mundy E. Ethnoveterinary medicine in Africa. Africa. 1992;62:59–93. doi: 10.2307/1160064. [DOI] [Google Scholar]
- 11.McCorkle C.M. An introduction to ethnoveterinary research and development. J. Ethnobiol. 1986;6:129–149. [Google Scholar]
- 12.Viljoen A., Sandasi M., Vermaak I. The role of the South African Journal of Botany as a vehicle to promote medicinal plant research–A bibliometric appraisal. S. Afr. J. Bot. 2019;122:3–10. doi: 10.1016/j.sajb.2018.07.024. [DOI] [Google Scholar]
- 13.Light M., Sparg S., Stafford G., Van Staden J. Riding the wave: South Africa’s contribution to ethnopharmacological research over the last 25 years. J. Ethnopharmacol. 2005;100:127–130. doi: 10.1016/j.jep.2005.05.028. [DOI] [PubMed] [Google Scholar]
- 14.Hoveka L.N., van der Bank M., Bezeng B.S., Davies T.J. Identifying biodiversity knowledge gaps for conserving South Africa’s endemic flora. Biodivers. Conserv. 2020;29:2803–2819. doi: 10.1007/s10531-020-01998-4. [DOI] [Google Scholar]
- 15.Wall B., Mateus A., Marshall L., Pfeiffer D., Lubroth J., Ormel H., Otto P., Patriarchi A. Drivers, Dynamics and Epidemiology of Antimicrobial Resistance in Animal Production. Food and Agriculture Organization of the United Nations; Rome, Italy: 2016. [Google Scholar]
- 16.Beinart W., Brown K. African Local Knowledge & Livestock Health: Diseases & Treatments in South Africa. Wits University Press; Johannesburg, South Africa: 2013. [Google Scholar]
- 17.Van der Merwe D. Master’s Thesis. University of Pretoria; Pretoria, South Africa: 2000. Use of ethnoveterinary medicinal plants in cattle by Setswana-speaking people in the Madikwe area of the North West Province. [DOI] [PubMed] [Google Scholar]
- 18.McGaw L.J., Famuyide I.M., Khunoana E.T., Aremu A.O. Ethnoveterinary botanical medicine in South Africa: A review of research from the last decade (2009 to 2019) J. Ethnopharmacol. 2020;257:112864. doi: 10.1016/j.jep.2020.112864. [DOI] [PubMed] [Google Scholar]
- 19.Bredemus B. A Consensual Qualitative Research Analysis of Prominent Multicultural Psychotherapy Researchers’ Career Experiences. The Chicago School of Professional Psychology ProQuest Dissertations Publishing; Chicago, IL, USA: 2021. [Google Scholar]
- 20.Eisner H. What Makes the Systems Engineer Successful? Various Surveys Suggest an Answer. CRC Press; Boca Raton, FL, USA: 2020. [Google Scholar]
- 21.Bruchac M. Indigenous knowledge and traditional knowledge. Encycl. Glob. Archaeol. 2014;10:3814–3824. doi: 10.1007/978-1-4419-0465-2_10. [DOI] [Google Scholar]
- 22.Hecht S., Yang A.L., Basnett B.S., Padoch C., Peluso N.L. People in Motion, Forests in Transition: Trends in Migration, Urbanization, and Remittances and Their Effects on Tropical Forests. Volume 142 CIFOR; Bogor, Indonesia: 2015. [Google Scholar]
- 23.Crane P.R., Ge S., Hong D.-Y., Huang H.-W., Jiao G.-L., Knapp S., Kress W.J., Mooney H., Raven P.H., Wen J. The Shenzhen Declaration on Plant Sciences-Uniting plant sciences and society to build a green, sustainable Earth. J. Syst. Evol. 2017;55:59–61. doi: 10.1111/jse.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ahmed M.J., Murtaza G. A study of medicinal plants used as ethnoveterinary: Harnessing potential phytotherapy in Bheri, district Muzaffarabad (Pakistan) J. Ethnopharmacol. 2015;159:209–214. doi: 10.1016/j.jep.2014.11.016. [DOI] [PubMed] [Google Scholar]
- 25.Moichwanetse B.I., Ndhlovu P.T., Sedupane G., Aremu A.O. Ethno-veterinary plants used for the treatment of retained placenta and associated diseases in cattle among Dinokana communities, North West Province, South Africa. S. Afr. J. Bot. 2020;132:108–116. doi: 10.1016/j.sajb.2020.04.005. [DOI] [Google Scholar]
- 26.Nyahangare E.T., Mvumi B.M., Mutibvu T. Ethnoveterinary plants and practices used for ecto-parasite control in semi-arid smallholder farming areas of Zimbabwe. J. Ethnobiol. Ethnomed. 2015;11:30. doi: 10.1186/s13002-015-0006-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shang X., Tao C., Miao X., Wang D., Wang Y., Yang Y., Pan H. Ethno-veterinary survey of medicinal plants in Ruoergai region, Sichuan province, China. J. Ethnopharmacol. 2012;142:390–400. doi: 10.1016/j.jep.2012.05.006. [DOI] [PubMed] [Google Scholar]
- 28.Shen S., Qian J., Ren J. Ethnoveterinary plant remedies used by Nu people in NW Yunnan of China. J. Ethnobiol. Ethnomed. 2010;6:24. doi: 10.1186/1746-4269-6-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chaachouay N., Benkhnigue O., Fadli M., El Ibaoui H., Zidane L. Ethnobotanical and ethnopharmacological studies of medicinal and aromatic plants used in the treatment of metabolic diseases in the Moroccan Rif. Heliyon. 2019;5:e02191. doi: 10.1016/j.heliyon.2019.e02191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hamilton A.C. Medicinal plants, conservation and livelihoods. Biodivers. Conserv. 2004;13:1477–1517. doi: 10.1023/B:BIOC.0000021333.23413.42. [DOI] [Google Scholar]
- 31.Giday M., Teklehaymanot T. Ethnobotanical study of plants used in management of livestock health problems by Afar people of Ada’ar District, Afar Regional State, Ethiopia. J. Ethnobiol. Ethnomed. 2013;9:8. doi: 10.1186/1746-4269-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moreki J., Tshireletso K., Okoli I. Potential use of ethnoveterinary medicine for retained placenta in cattle in Mogonono, Botswana. J. Anim. Prod. Adv. 2012;2:303–309. [Google Scholar]
- 33.Van der Merwe D., Swan G., Botha C. Use of ethnoveterinary medicinal plants in cattle by Setswana-speaking people in the Madikwe area of the North West Province of South Africa. J. S. Afr. Vet. Assoc. 2001;72:189–196. doi: 10.4102/jsava.v72i4.651. [DOI] [PubMed] [Google Scholar]
- 34.Assefa A., Bahiru A. Ethnoveterinary botanical survey of medicinal plants in Abergelle, Sekota and Lalibela districts of Amhara region, Northern Ethiopia. J. Ethnopharmacol. 2018;213:340–349. doi: 10.1016/j.jep.2017.11.024. [DOI] [PubMed] [Google Scholar]
- 35.Phondani P., Maikhuri R., Kala C. Ethnoveterinary uses of medicinal plants among traditional herbal healers in Alaknanda catchment of Uttarakhand, India. Afr. J. Tradit. Complement. Altern. Med. 2010;7:195–206. doi: 10.4314/ajtcam.v7i3.54775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Masika P., Sonandi A., Van Averbeke W. Perceived causes, diagnosis and treatment of babesiosis and anaplasmosis in cattle by livestock farmers in communal areas of the central Eastern Cape Province, South Africa. J. S. Afr. Vet. Assoc. 1997;68:40–44. doi: 10.4102/jsava.v68i2.867. [DOI] [PubMed] [Google Scholar]
- 37.Masika P., Van Averbeke W., Sonandi A. Use of herbal remedies by small-scale farmers to treat livestock diseases in central Eastern Cape Province, South Africa. J. S. Afr. Vet. Assoc. 2000;71:87–91. doi: 10.4102/jsava.v71i2.685. [DOI] [PubMed] [Google Scholar]
- 38.Nabukenya I., Rubaire-Akiiki C., Olila D., Ikwap K., Höglund J. Ethnopharmacological practices by livestock farmers in Uganda: Survey experiences from Mpigi and Gulu districts. J. Ethnobiol. Ethnomed. 2014;10:9. doi: 10.1186/1746-4269-10-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.RVASA . Monthly Report on Livestock Disease Trends as Informally Reported by Veterinarians Belonging to the Ruminant Veterinary Association of South Africa (RuVASA), a Group of the South African Veterinary Association. Ruminant Veterinary Association of South Africa (RuVASA); Pretoria, South Africa: 2021. [Google Scholar]
- 40.Ndou R.V. Master’s Thesis. North-West University; Mafikeng, South Africa: 2018. A Study of Ethnoveterinary Medicine in the North West Province. [Google Scholar]
- 41.Bano A., Ahmad M., Hadda T.B., Saboor A., Sultana S., Zafar M., Khan M.P.Z., Arshad M., Ashraf M.A. Quantitative ethnomedicinal study of plants used in the skardu valley at high altitude of Karakoram-Himalayan range, Pakistan. J. Ethnobiol. Ethnomed. 2014;10:43. doi: 10.1186/1746-4269-10-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amjad M.S., Qaeem M.F., Ahmad I., Khan S.U., Chaudhari S.K., Zahid Malik N., Shaheen H., Khan A.M. Descriptive study of plant resources in the context of the ethnomedicinal relevance of indigenous flora: A case study from Toli Peer National Park, Azad Jammu and Kashmir, Pakistan. PLoS ONE. 2017;12:e0171896. doi: 10.1371/journal.pone.0171896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leonti M. The relevance of quantitative ethnobotanical indices for ethnopharmacology and ethnobotany. J. Ethnopharmacol. 2022;288:115008. doi: 10.1016/j.jep.2022.115008. [DOI] [PubMed] [Google Scholar]
- 44.Van Wyk B.-E. The potential of South African plants in the development of new medicinal products. S. Afr. J. Bot. 2011;77:812–829. doi: 10.1016/j.sajb.2011.08.011. [DOI] [Google Scholar]
- 45.Dold A.P., Cocks M.L. Traditional veterinary medicine in the Alice district of the Eastern Cape Province, South Africa: Research in action. S. Afr. J. Sci. 2001;97:375–379. [Google Scholar]
- 46.Gesler W.M. The Cultural Geography of Health Care. University of Pittsburgh; Pittsburgh, PA, USA: 1992. [Google Scholar]
- 47.Giday M., Ameni G. An ethnobotanical survey of plants of veterinary importance in two woredas of Southern Tigray, Northern Ethiopia. SINET Ethiop. J. Sci. 2003;26:123–136. doi: 10.4314/sinet.v26i2.18208. [DOI] [Google Scholar]
- 48.Miara M.D., Bendif H., Ouabed A., Rebbas K., Hammou M.A., Amirat M., Greene A., Teixidor-Toneu I. Ethnoveterinary remedies used in the Algerian steppe: Exploring the relationship with traditional human herbal medicine. J. Ethnopharmacol. 2019;244:112164. doi: 10.1016/j.jep.2019.112164. [DOI] [PubMed] [Google Scholar]
- 49.Chaachouay N., Azeroual A., Bencharki B., Douira A., Zidane L. Ethnoveterinary medicines plants for animal therapy in the Rif, North of Morocco. S. Afr. J. Bot. 2022;147:176–191. doi: 10.1016/j.sajb.2021.12.037. [DOI] [Google Scholar]
- 50.Prakash P., Kumar M., Pundir A., Puri S., Prakash S., Kumari N., Thakur M., Rathour S., Jamwal R., Janjua S. Documentation of Commonly Used Ethnoveterinary Medicines from Wild Plants of the High Mountains in Shimla District, Himachal Pradesh, India. Horticulturae. 2021;7:351. doi: 10.3390/horticulturae7100351. [DOI] [Google Scholar]
- 51.Njoroge G.N., Bussmann R.W. Herbal usage and informant consensus in ethnoveterinary management of cattle diseases among the Kikuyus (Central Kenya) J. Ethnopharmacol. 2006;108:332–339. doi: 10.1016/j.jep.2006.05.031. [DOI] [PubMed] [Google Scholar]
- 52.Rahmatullah M., Ferdausi D., Mollik A., Jahan R., Chowdhury M.H., Haque W.M. A survey of medicinal plants used by Kavirajes of Chalna area, Khulna district, Bangladesh. Afr. J. Tradit. Complement. Altern. Med. 2010;7:91–97. doi: 10.4314/ajtcam.v7i2.50859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Khunoana E.T., Madikizela B., Erhabor J.O., Nkadimeng S.M., Arnot L., Van Wyk I., McGaw L.J. A survey of plants used to treat livestock diseases in the Mnisi community, Mpumalanga, South Africa, and investigation of their antimicrobial activity. S. Afr. J. Bot. 2019;126:21–29. doi: 10.1016/j.sajb.2019.07.026. [DOI] [Google Scholar]
- 54.Chinsembu K., Negumbo J., Likando M., Mbangu A. An ethnobotanical study of medicinal plants used to treat livestock diseases in Onayena and Katima Mulilo, Namibia. S. Afr. J. Bot. 2014;94:101–107. doi: 10.1016/j.sajb.2014.06.007. [DOI] [Google Scholar]
- 55.Kushwaha K. Medicinal plants used to cure the cattle diseases in Korea District of Chhatisgarh. Int. J. Pharm. Life Sci. 2020;11:6889–6892. [Google Scholar]
- 56.Luseba D., Van der Merwe D. Ethnoveterinary medicine practices among Tsonga speaking people of South Africa. Onderstepoort J. Vet. Res. 2006;73:115–122. doi: 10.4102/ojvr.v73i2.156. [DOI] [PubMed] [Google Scholar]
- 57.Tanzin R., Ghosh K.C., Jahan R., Khatun A., Rahmatullah M. An ethnoveterinary survey of medicinal plants used to treat cattle diseases in Birishiri area, Netrakona district, Bangladesh. Adv. Nat. Appl. Sci. 2010;4:10–14. [Google Scholar]
- 58.Traore L., Yaro V., Soudre A., Ouedraogo-Kone S., Ouedraogo D., Yougbare B., Zoma B., Hien M., Guissou M.-L., Traore A. Indigenous knowledge of veterinary medicinal plant use in cattle treatment in southwestern Burkina Faso (West Africa) S. Afr. J. Bot. 2020;128:189–199. doi: 10.1016/j.sajb.2019.09.015. [DOI] [Google Scholar]
- 59.Getaneh S., Girma Z. An ethnobotanical study of medicinal plants in Debre Libanos Wereda, Central Ethiopia. Afr. J. Plant Sci. 2014;8:366–379. [Google Scholar]
- 60.Moyo M., Aremu A.O., Van Staden J. Medicinal plants: An invaluable, dwindling resource in sub-Saharan Africa. J. Ethnopharmacol. 2015;174:595–606. doi: 10.1016/j.jep.2015.04.034. [DOI] [PubMed] [Google Scholar]
- 61.Gakuubi M.M., Wanzala W. A survey of plants and plant products traditionally used in livestock health management in Buuri district, Meru County, Kenya. J. Ethnobiol. Ethnomed. 2012;8:39. doi: 10.1186/1746-4269-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ul Hassan H., Murad W., Tariq A., Ahmad A. Ethnoveterinary study of medicinal plants in Malakand Valley, district Dir (lower), Khyber Pakhtunkhwa, Pakistan. Ir. Vet. J. 2014;67:6. doi: 10.1186/2046-0481-67-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gradé J.T., Tabuti J.R., Van Damme P. Ethnoveterinary knowledge in pastoral Karamoja, Uganda. J. Ethnopharmacol. 2009;122:273–293. doi: 10.1016/j.jep.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 64.Lulekal E., Kelbessa E., Bekele T., Yineger H. An ethnobotanical study of medicinal plants in Mana Angetu District, southeastern Ethiopia. J. Ethnobiol. Ethnomed. 2008;4:10. doi: 10.1186/1746-4269-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Teklehaymanot T. An ethnobotanical survey of medicinal and edible plants of Yalo Woreda in Afar regional state, Ethiopia. J. Ethnobiol. Ethnomed. 2017;13:40. doi: 10.1186/s13002-017-0166-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mussarat S., Amber R., Tariq A., Adnan M., AbdElsalam N.M., Ullah R., Bibi R. Ethnopharmacological assessment of medicinal plants used against livestock infections by the people living around Indus river. BioMed Res. Int. 2014;2014:616858. doi: 10.1155/2014/616858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Yigezu Y., Haile D.B., Ayen W.Y. Ethnoveterinary medicines in four districts of Jimma zone, Ethiopia: Cross sectional survey for plant species and mode of use. BMC Vet. Res. 2014;10:76. doi: 10.1186/1746-6148-10-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Teklay A., Abera B., Giday M. An ethnobotanical study of medicinal plants used in Kilte Awulaelo District, Tigray Region of Ethiopia. J. Ethnobiol. Ethnomed. 2013;9:65. doi: 10.1186/1746-4269-9-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bussmann R.W. Ethnobotany of the Samburu of Mt. Nyiru, South Turkana, Kenya. J. Ethnobiol. Ethnomed. 2006;2:35. doi: 10.1186/1746-4269-2-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gradé J.T. Ph.D. Thesis. Ghent University; Ghent, Belgium: 2008. Ethnoveterinary Knowledge in Pastoral Karamoja, Northern Uganda. [Google Scholar]
- 71.Yineger H., Kelbessa E., Bekele T., Lulekal E. Ethnoveterinary medicinal plants at bale mountains national park, Ethiopia. J. Ethnopharmacol. 2007;112:55–70. doi: 10.1016/j.jep.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 72.StatsSA Ramotshere Moiloa. [(accessed on 8 August 2021)]; Available online: http://www.statssa.gov.za/?page_id=993&id=ramotshere-moiloa-municipality.
- 73.Madziwa M.B.N. Final Ecological Report for the Proposed 88KV Petrusdam Switch Station, Ramotshere Moiloa Local Municipality (Ward 17), North–West Province. 2017. [(accessed on 8 August 2021)]. Available online: https://sahris.sahra.org.za/sites/default/files/additionaldocs/Final%20Petrusdam%20Switch%20Station%20Biodiversity%20Report.pdf.
- 74.Itholeng K.B.I. Master’s Thesis. North-West University; Potchefstroom, South Africa: 2007. The Indigenous Knowledge of the Local Community Towards Weeds and Alien Invasive Plants in the Dinokana Area, North-West Province. [Google Scholar]
- 75.Heckathorn D.D. Respondent-driven sampling: A new approach to the study of hidden populations. Soc. Probl. 1997;44:174–199. doi: 10.2307/3096941. [DOI] [Google Scholar]
- 76.Kish L. Survey Sampling. John Wiley and Sons Inc.; New York, NY, USA: 1995. [Google Scholar]
- 77.Mason J. Researching Your Own Practice: The Discipline of Noticing. Psychology Press; New York, NY, USA: 2002. [Google Scholar]
- 78.Adams R.S., Daly S.R., Mann L.M., Dall’Alba G. Being a professional: Three lenses into design thinking, acting, and being. Des. Stud. 2011;32:588–607. doi: 10.1016/j.destud.2011.07.004. [DOI] [Google Scholar]
- 79.Alexiades M.N., Sheldon J. Selected Guidelines for Ethnobotanical Research: A Field Manual (Advances in Economic Botany Vol. 10) The New York Botanical Garden Press; New York, NY, USA: 1996. [Google Scholar]
- 80.Kongsager R. Data Collection in the Field: Lessons from Two Case Studies Conducted in Belize. Qual. Rep. 2021;26:1218–1232. doi: 10.46743/2160-3715/2021.4744. [DOI] [Google Scholar]
- 81.Victor J.E., Koekemoer M., Fish L., Smithies S.J., Mössmer M. Herbarium Essentials: The Southern African Herbarium User Manual. SABONET; Pretoria, South Africa: 2004. Southern African Botanical Diversity Network Report No. 25. [Google Scholar]
- 82.Heckathorn D.D. Comment: Snowball versus respondent-driven sampling. Sociol. Methodol. 2011;41:355–366. doi: 10.1111/j.1467-9531.2011.01244.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Heinrich M., Ankli A., Frei B., Weimann C., Sticher O. Medicinal plants in Mexico: Healers’ consensus and cultural importance. Social Sci. Med. 1998;47:1859–1871. doi: 10.1016/S0277-9536(98)00181-6. [DOI] [PubMed] [Google Scholar]
- 84.Vitalini S., Iriti M., Puricelli C., Ciuchi D., Segale A., Fico G. Traditional knowledge on medicinal and food plants used in Val San Giacomo (Sondrio, Italy)—An alpine ethnobotanical study. J. Ethnopharmacol. 2013;145:517–529. doi: 10.1016/j.jep.2012.11.024. [DOI] [PubMed] [Google Scholar]
- 85.Hudaib M., Mohammad M., Bustanji Y., Tayyem R., Yousef M., Abuirjeie M., Aburjai T. Ethnopharmacological survey of medicinal plants in Jordan, Mujib Nature Reserve and surrounding area. J. Ethnopharmacol. 2008;120:63–71. doi: 10.1016/j.jep.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 86.Tardío J., Pardo-de-Santayana M. Cultural Importance Indices: A comparative analysis based on the useful wild plants of Southern Cantabria (Northern Spain) Econ. Bot. 2008;62:24–39. doi: 10.1007/s12231-007-9004-5. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Primary data collected during the survey are available upon request to the corresponding author of this manuscript.