Visual Abstract
Keywords: COVID-19, qualitative research, decision making, SARS-CoV-2, chronic kidney disease
Abstract
Background and objectives
Coronavirus disease 2019 (COVID-19) disrupted medical care across health care settings for older patients with advanced CKD. Understanding how shared decision making for kidney treatment decisions was influenced by the uncertainty of an evolving pandemic can provide insights for supporting shared decision making through the current and future public health crises.
Design, setting, participants, & measurements
We performed thematic and narrative analyses of semistructured interviews with patients (CKD stages 4 and 5, age 70+), care partners, and clinicians from Boston, Portland (Maine), San Diego, and Chicago from August to December 2020.
Results
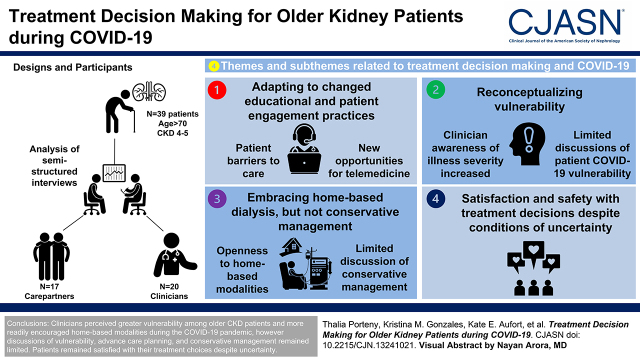
We interviewed 76 participants (39 patients, 17 care partners, and 20 clinicians). Among patient participants, 13 (33%) patients identified as Black, and seven (18%) had initiated dialysis. Four themes with corresponding subthemes emerged related to treatment decision making and the COVID-19 pandemic: (1) adapting to changed educational and patient engagement practices (patient barriers to care and new opportunities for telemedicine); (2) reconceptualizing vulnerability (clinician awareness of illness severity increased and limited discussions of patient COVID-19 vulnerability); (3) embracing home-based dialysis but not conservative management (openness to home-based modalities and limited discussion of conservative management and advanced care planning); and (4) satisfaction and safety with treatment decisions despite conditions of uncertainty.
Conclusions
Although clinicians perceived greater vulnerability among older patients CKD and more readily encouraged home-based modalities during the COVID-19 pandemic, their discussions of vulnerability, advance care planning, and conservative management remained limited, suggesting areas for improvement. Clinicians reported burnout caused by the pandemic, increased time demands, and workforce limitations, whereas patients remained satisfied with their treatment choices despite uncertainty.
Clinical Trial registry name and registration number:
Decision Aid for Renal Therapy (DART), NCT03522740
Introduction
In the United States, individuals with CKD have a three-fold higher likelihood of severe coronavirus disease 2019 (COVID-19) (1) compared with people without CKD (2), with older adults experiencing a disproportionate burden (3,4). With mortality among patients on dialysis diagnosed with COVID-19 exceeding 20% during the early months of the pandemic, patients with CKD and their loved ones were confronted with new risks and benefits associated with different CKD treatment modalities, posing challenges to decision making given heightened uncertainty (5–8).
Shared decision making is a process by which clinicians, patients, and care partners deliberate to make optimal informed health care decisions that align with patient priorities and values (9). Shared decision making is the ideal approach for older patients with CKD, for whom the differences in survival between dialysis and conservative management may be small, whereas differences in lifestyle and symptoms may be substantial (10–13). Kidney clinicians engaging in shared decision making should present information early about prognosis and the harms and benefits of different modalities (14,15). This should be followed by discussions that help patients and their caregivers consider their choice in the context of their values and preferences (16). Yet, few older adults experience shared decision making (17). Nephrologists often avoid discussing prognosis and delay treatment discussions until decisions are imminent, perhaps owing to beliefs that patient treatment preferences are unstable and influenced by evolving symptoms (18).
COVID-19 introduced additional uncertainty by altering the risks and benefits of treatment options in new and unknown ways, further complicating shared decision making. The pandemic also exacerbated communication challenges owing to sudden changes in practices, including telehealth, physical distancing policies, limited in-person education about treatment modalities, and restricted participation of care partners (19–22). COVID-19–related considerations may also have affected nephrologists’ approach to treatment recommendations, with shifts from the typical emphasis on in-center dialysis to more consideration of home-based modalities (5,23–25). This multisite qualitative study examines whether and how older adults with advanced CKD, care partners, and clinicians approached shared decision making in new ways during the COVID-19 pandemic, including how they perceived COVID-19 risks and how perceived COVID-19 risks affected the decision-making process.
Materials and Methods
Design, Setting, and Participants
This study was part of the multisite, mixed methods Decision Aid for Renal Therapy (DART) trial. From 2018 to 2019, the DART trial recruited 400 English-fluent patients age 70+ years with nondialysis CKD and eGFR <30 ml/min per 1.73 m2 receiving care at nephrology clinics in greater Boston, Portland (Maine), San Diego, and Chicago (18,26). From August to December 2020, a subset of patients, care partners, and nephrology clinicians was recruited for a qualitative study using purposive sampling to ensure balanced representation by age, sex, region, education, race, treatment preference, and years in practice (clinicians). The Tufts Health Sciences Institutional Review Board approved this study as the central institutional review board.
Interview Guide and Data Collection
On the basis of a literature review and clinical experience, a social scientist with expertise in qualitative methods and kidney disease (K.L.) designed three semistructured interview guides (patients, care partners, and clinicians) that were refined further with the DART team and the stakeholder advisory board (Supplemental Appendix 1). Following verbal informed consent, where study-related goals, harms, and benefits were shared, trained interviewers (K.M.G. and T.P.) conducted and recorded semistructured interviews by phone. Open-ended questions were used to examine patient, caregiver, and clinician perspectives about treatment decision making during the COVID-19 pandemic (Supplemental Appendix 2). Interview questions examined treatment preferences, quality of shared decision-making discussions, satisfaction with treatment choices, the pandemic’s effect on quality of life, presentation of treatment choices, and advanced care planning. Findings were discussed by the DART multidisciplinary stakeholder advisory board, which included patients, advocates, clinicians, and care partners (Supplemental Appendix 2). Study reporting reflects Consolidated Criteria for Reporting Qualitative Health Research (27). Supplemental Appendix 3 presents supplemental methodological information.
Analyses
We conducted a thematic and narrative analysis of audiorecorded interviews that were transcribed verbatim. Sampling continued until thematic saturation was achieved and confirmed through deliberation by the research team for all COVID-19–related topics. Subsequently, the team developed two preliminary codebooks (patients/care partners and clinicians) deductively following the interview guide and inductively on the basis of emergent findings. At least three researchers (K.E.A., K.M.G., and T.P.) independently coded ten interviews, allowing for new codes to emerge inductively. The qualitative team revised the codebook and independently recoded the initial interviews and six additional transcripts using NVivo (version 11; QSR Int). Iterative deliberation yielded team consensus about coding discrepancies and emergent codes. The process was repeated for the remaining interviews. Codes were amended and organized into categories through a consensus process to reflect the range and variability of subthemes and to characterize both confirmatory and contradictory narratives. Emerging themes were then discussed and finalized by the research team (28).
Results
Among 76 participants, 20 were clinicians, 39 were patients, and 17 were care partners. Mean interview time was 30±11 minutes. Most (85%) clinicians were nephrologists. Of patient participants, 56% identified as non-Hispanic White, and 33% identified as non-Hispanic Black (Table 1).
Table 1.
Clinician, patient, and care partner participant characteristics
| Participant Characteristics | Clinician, n=20 | Patient, n=39 | Care Partner,a n=17 |
|---|---|---|---|
| Sex | |||
| Women | 10 (50) | 23 (59) | 12 (71) |
| Men | 10 (50) | 16 (41) | 5 (29) |
| Age, yr | |||
| 40–59 | 3 (18) | ||
| 60–69 | 3 (18) | ||
| 70–74 | 11 (28) | 3 (18) | |
| 75–79 | 15 (38) | 4 (23) | |
| 80–89 | 10 (26) | 4 (23) | |
| 90+ | 3 (8) | ||
| Clinician type | |||
| Nephrologist | 17 (85) | ||
| Physician assistant | 3 (15) | ||
| Region | |||
| Boston | 7 (35) | 8 (21) | 4 (23.5) |
| Chicago | 6 (30) | 15 (38) | 7 (41) |
| San Diego | 6 (30) | 13 (33) | 4 (23.5) |
| Maine | 1 (5) | 3 (8) | 2 (12) |
| Dialysis status | |||
| Receiving dialysis | 7 (18) | ||
| Nondialysis CKD | 32 (82) | ||
| Race | |||
| White participants | 22 (57) | 13 (76) | |
| Black participants | 13 (33) | 4 (24) | |
| Other | 4 (10) | ||
| Ethnicity | |||
| Hispanic/Latino | 3 (8) | 1 (6) | |
| Education level | |||
| High school | 5 (13) | 1 (6) | |
| Some college or technical school | 15 (38) | 6 (35) | |
| College graduate | 8 (21) | 4 (24) | |
| Postgraduate | 11 (28) | 6 (35) | |
| Care partner status | |||
| Has a care partner | 19 (49) | ||
| Does not have a care partnera | 20 (51) | ||
| Treatment preference | |||
| In-center HD | 14 (36) | ||
| Home HD | 1 (2.5) | ||
| Peritoneal dialysis | 5 (13) | ||
| Conservative care management | 13 (33) | ||
| Transplant | 1 (2.5) | ||
| Undecided | 5 (13) | ||
| Randomization | |||
| DART | 23 (59) | 11 (65) | |
| Usual care | 16 (41) | 6 (35) |
Data are presented as N (percentage). HD, hemodialysis; DART, decision aid for renal therapy.
Patient did not have a care partner enrolled in the DART study.
Four themes characterized participants’ experiences with shared decision making during the COVID-19 pandemic: (1) adapting to changed educational and patient engagement practices (patient barriers to care and new opportunities for telemedicine); (2) reconceptualizing vulnerability (clinician awareness of illness severity increased and limited discussions of patient COVID-19 vulnerability); (3) embracing home-based dialysis but not conservative management (openness to home-based modalities and limited discussions of conservative management and advanced care planning); and (4) satisfaction and safety with treatment decisions despite conditions of uncertainty (Table 2).
Table 2.
Sample quotes from study participants
| Themes and Exemplary Quotes |
|---|
| Theme 1: Adapting educational and patient engagement practices |
| Patient barriers to care |
| (1a) “Before the virus, I would go with her. Our children … were able to go with her for a couple of visits … get a tour, see what the equipment looks like.… It gave us a better feel for the home dialysis.” (Care partner 16) |
| (1b) “We have a dialysis modality teaching class that used to be in person, and it seems like that has fallen through the cracks somehow.… They've had some issues. I think people working from home on the administrative side, has allowed for things to fall through the cracks. There's a less in-person support.” (Clinician 7) |
| (1c) “I go to see the doctor by myself, or my husband and I go to the grocery store, and that's about it. [It makes me feel] more isolated.” (Patient 15) |
| (1d) “Since [COVID-19] started, [care partner] can no longer come in with me. He just drops me off and then picks me up at the end. I miss him being there.” (Patient 6) |
| (1e) “My oldest daughter, who lives five minutes away, she goes to the store for us. We don't have any contact with people.” (Patient 15) |
| (1f) “So, some of our patients didn't feel they even understood how to use the technology or didn't realize they could do phone visits until … I think some of our kidney patients ended up not following up with us for a few months. So, there was a few patients, we're talking about sort of negative side effects, there was a few patients who didn't have proper medical care because of the shutdown. And so, there were a few people who got hospitalized, they needed to start dialysis or things like that.” (Clinician 2) |
| New opportunities for telemedicine |
| (1g) “I actually prefer to do [telehealth] rather than have to hike up and go over to the medical center.… Obviously, it's much, much easier for me to send an email to my doctor and the next day I'll get a response for all of my doctors. So I really like it that way.” (Patient 15) |
| (1h) “No, there wasn’t anything that made it difficult. I was comfortable with it, I understood what the purpose was.” (Patient 14) |
| (1i) “If [I] wasn't there at the appointment, then I would worry if I remembered everything and did I tell her everything? It's sort of the same thing. So for the most part, they've been on the phone, which has been very helpful.” (Care partner 17) |
| (1j) “So what was relevant to telehealth sometimes, is that the patient might have a relative at home with them. And they also probably have access to the medications a little bit easier. So from that standpoint, the logistics of that is a lot easier.” (Clinician 7) |
| Theme 2: Reconceptualizing vulnerability and discussing it with patients |
| Clinicians awareness of illness severity increased |
| (2a) “During the period where it was bad, there was a lot of anxiety and doctors and patients worried about things, and physicians and nurses were concerned as well.” (Clinician 1) |
| (2b) “My dialysis shift was particularly hit hard … I take care of about 22 patients … nine of them contracted [COVID-19] and six of them died. It was very difficult for me … for the other patients … the nursing staff. We were woke to the reality that these are really sick people who are very vulnerable.” (Clinician 14) |
| (2c) “We had a nurse at the end of the hall dialyzing two [COVID-19] patients in their room at once … I was going there to provide moral support to the nurse.” (Clinician 6) |
| (2d) “[We were worried about] not [having] enough ventilators or dialysis machines or dialysis fluid, that [patients] might have to have unilateral DNRs based on the opinion of multiple doctors from different teams.” (Clinician 3) |
| (2e) “A big part of why it was so stressful is just the logistics of getting someone dialysis in a safe manner, that's safe for the patient as well as the nurse. And I guess ourselves too.” (Clinician 13) |
| Limited discussions about COVID-19 vulnerability |
| (2f) “Don’t walk around with doom and gloom on your shoulders. We’ll see how it goes and hopefully you don’t get it, but if you do, it’s not a death sentence. And that’s kind of been my approach.” (Clinician 3) |
| (2g) “It's hard to be on dialysis.… It's enough for [patients] to know they're high risk. I don't want to terrify them.” (Clinician 17) |
| (2h) “You have to be cognizant about what we're recommending … it has significant mental effects on our population, which is high risk for developing depression due their comorbidities.” (Clinician 4) |
| (2i) “I think [patients] … realize that there's not a lot of opportunity for them to do anything different.… They understand the risks … and that's pretty much the hands they're dealt.” (Clinician 17) |
| (2j) “[Clinicians] haven't told me anything to anybody about anything and they haven't told me about any [COVID-19 risks].” (Patient 29) |
| (2k) “I'm aware of my vulnerability … I am extremely careful about going out … I am being very cautious.” (Patient 20) |
| (2l) “I sort of keep back because I'm told I'm a high risk person because of age and because of dialysis, that I need to stay away from people. And so my husband and I pretty much stay right in the house.” (Patient 1) |
| (2m) “[I] know the risk [of COVID-19] just from reading the news and so forth.” (Patient 37) |
| (2n) “Before the doctor walks in, I've seen four people [in the nephrology clinic]. They've given me marching orders. Not one … has ever said a word to me about coronavirus. I've always wondered why.” (Patient 29) |
| (2o) “What effect would [COVID-19] have with [my] kidney disease?” (Patient 26) |
| (2p) “My doctor suggested that, unless I have an emergency, I stay away from the hospital … I appreciated it because I've always been the kind of person that went.” (Patient 22) |
| (2q) “They told me what to do and how to do it … that's what I do.” (Patient 2) |
| Theme 3: Embracing home-based dialysis but not conservative management |
| Openness to home-based dialysis |
| (3a) “There are changes related to the added risk of [infection at] in-center dialysis, and the realistic assessment of utility given the acute and serious medical condition. We probably are doing a better job of saying [in-center] is not a good idea to start. I think maybe there's also been a bit of a shift towards [home] dialysis as a result [of COVID-19].” (Clinician 1) |
| (3b) “The pandemic highlights the bad [of dialysis] because when patients ask about risks or benefit, I mention one benefit of being at home is that you don't have to go out three times a week and interact in a group setting.’” (Clinician 8) |
| (3c) “[COVID-19] has solidified my decision to avoid [in-center hemo and transplant].” (Patient 39) |
| Limited discussions of conservative management and advanced care planning |
| (3d) “I'm a huge fan of [discussing CM with patients] .… with or without [COVID-19], I’m not going to change [how I approach CM conversations].” (Clinician 3) |
| (3e) “[CM] is not the primary focus of [their] discussion. [Treatment] discussions haven't really changed…. [and] don't even mention [COVID-19].” (Clinician 6) |
| (3f) “I’m not sure if this is a manifestation of [COVID-19] or the way that our thinking is evolving, but CM is becoming more accepted viable option to present to patients.” (Clinician 12) |
| (3g) “I think that … COVID-19 … increase(s) the comfort level of people talking about what they want to do if [they] got really sick … it enables a better, easier, conversation. [Otherwise], it's really hard for them to make those decisions ahead of time.” (Clinician 10) |
| (3h) “We have [discussed advanced care planning] in the past, but not during this time now.” (Care partner 11) |
| Theme 4: Satisfaction and safety with treatment decisions under conditions of uncertainty |
| (4a) “There was no reason to [change treatment] at this point, nothing.” (Care partner 15) |
| (4b) “No, I don't think [COVID-19's] had an effect on my decision.” (Patient 3) |
| (4c) “From what he's read, there are more infections in the dialysis in-center. That's concerning to him, he would not want to go there because of that.” (Care partner 5) |
| (4d) “I was never afraid of getting infected at the center where I go. They're very careful … I would be just as prone to getting something at home. So, I did not consider [home dialysis].” (Patient 8) |
| (4e) “I'm really glad that I'm doing this at home where I can maintain my standard of sanitariness … I'm grateful for having made that choice even though COVID-19 hadn't been part of the discussion.” (Patient 15) |
| (4f) “I would have [chosen conservative management] today under the [COVID-19] restrictions; [it seems] difficult to do dialysis especially at treatment centers. [I] probably want to stay away from those places even more so today than before.” (Patient 37) |
Each participant is assigned a random number for data safety purposes. COVID-19, coronavirus disease 2019; DNR, do not resuscitate; CM, conservative management.
Adapting to Changed Educational and Patient Engagement Practices
Patient Barriers to Care.
Restrictive visitation policies and fewer in-person classes impeded patients’ and care partners’ ability to learn about all potential treatment modalities (quote 1a in Table 2). One clinician explained that when administrative personnel started working remotely, they could no longer support in-person classes (quote 1b in Table 2). Visitation restrictions and physical distancing burdened patients with CKD seeking care and their care partners, increasing social isolation and anxiety about CKD complications (quotes 1c and 1d in Table 2). Some patients became increasingly reliant on family for self-care and assistance with health care (quote 1e in Table 2). Occasionally, technology gaps led to care delays, which subsequently increased the risk of CKD complications and hospitalizations (quote 1f in Table 2).
New Opportunities for Telemedicine.
Although challenging for some, most participants expressed an openness to using telehealth to mitigate education and patient engagement constraints. Patients appreciated the convenience of telehealth, and many stated they were comfortable using telehealth for kidney care (quotes 1g and 1h in Table 2). Care partners described the usefulness of participating in telehealth appointments (quote 1i in Table 2). Similarly, clinicians emphasized how telehealth improved care partner engagement and quality care (quote 1j in Table 2).
Reconceptualizing Vulnerability
Although risks related to COVID-19 influenced clinicians’ perceptions of patients’ vulnerability, patients reported that discussions about COVID-19 risks were limited and not integrated into shared decision-making conversations.
Clinicians’ Awareness of Illness Severity Increased.
Clinicians described the difficulty and emotional toll of caring for patients on dialysis with COVID-19, and many described burnout. Although clinicians had viewed their patients as complex, treating patients on dialysis with COVID-19 reminded clinicians of the severity of their patients’ condition as “sick people who are very vulnerable” and the potential mortality risks (quotes 2a and 2b in Table 2). Clinicians were also concerned about resource scarcities, including ventilators; potential supply shortages; and the infection risk of caring for patients with COVID-19 in dialysis units (quotes 2c–2e in Table 2).
Limited Discussions of Patient Coronavirus Disease 2019 Vulnerability.
Clinicians struggled to discuss COVID-19 risk with patients, trying to balance encouragement with caution (quote 2f in Table 2). Clinicians expressed concerns about increasing patient fear (quote 2g in Table 2) and depression among a population at risk of depression (quote 2h in Table 2). Although some clinicians described risks to their patients, clinicians felt limited in their ability to help (quote 2i in Table 2). Thus, despite recognition of patient vulnerability, few clinicians said they discussed this with patients. When discussions about COVID-19 did occur, clinicians described emphasizing safety measures, not increased vulnerability or possible CKD progression, morbidity, or mortality tied to COVID-19 (quote 2j in Table 2).
Many patients learned about their high vulnerability to COVID-19 from the media, and some expressed that they would have preferred to discuss their heightened risk with clinicians (quotes 2k–2m in Table 2). When asked about discussions with clinicians regarding COVID-19 risks in the context of treatment decision making, some participants said they had “none whatsoever” (Patient 14) and wondered why that was the case (quote 2n in Table 2). Lack of discussions with clinicians left patients with unaddressed concerns about their increased vulnerability as patients with CKD (quote 2o in Table 2). When conversations did occur, patients expressed appreciation and noted the effect on their behavior (quotes 2p and 2q in Table 2).
Embracing Home-Based Dialysis but Not Conservative Management
Openness to Home-Based Modalities.
With greater recognition of older patients’ vulnerability and potential higher risk associated with in-center dialysis, many clinicians described a shift from their self-described prepandemic tendency of encouraging in-center hemodialysis (HD) toward greater openness to home dialysis. Many clinicians stated that they newly viewed home-based dialysis as safer, more comfortable, and more convenient (quotes 3a and 3b in Table 2). Similarly, some patients who were leaning toward home HD explained that COVID-19 had solidified decisions to avoid in-center HD and transplant (quote 3c in Table 2).
Limited Discussions of Conservative Management and Advanced Care Planning.
Although clinicians described being supportive of home dialysis due to COVID-19, few said they changed their presentation of conservative management, and few stated they promoted this option (quotes 3d and 3e in Table 2). However, a minority of clinicians said the pandemic made it easier to broach conservative management discussions and discuss it as a more palatable option for patients (quote 3f in Table 2).
Some clinicians perceived that the heightened risk of COVID-19 increased patients’ comfort in discussing quality of life and advanced care planning (quote 3g in Table 2). However, when patients were asked if COVID-19 had triggered discussions around advanced care planning with their kidney clinicians, patients largely said they either had not had these discussions or had “taken care of that” before the pandemic (quote 3h in Table 2).
Satisfaction and Safety with Treatment Decisions Despite Conditions of Uncertainty
Patients described that their preferences for kidney failure treatment remained stable during the pandemic, largely driven by the desires to maintain quality of life and beliefs about treatment safety. Patients often described their preferred treatment as the safest during COVID-19, irrespective of the modality chosen (quotes 4a and 4b in Table 2). Although all patients described selecting the treatment modality that would limit their COVID-19 exposure, beliefs about which treatment was safest varied. One care partner whose husband was leaning toward home dialysis explained that reading about dialysis in-center infections increased his concern about in-center dialysis (quote 4c in Table 2). Yet, patients on in-center HD shared a contradictory view; one patient on in-center HD explained that dialysis sessions “[had] been going smoothly” and “[felt] strongly [that she] couldn’t be in a safer place” (Patient 6). Patients receiving in-center dialysis stated that strict safety protocols in facilities contributed to their feeling of safety (quote 4d in Table 2). Participants receiving home dialysis before the pandemic were similarly satisfied that their treatment choice was safest as they were able to control their exposures at home (quote 4e in Table 2). Another participant explained that the pandemic solidified her prior choice of conservative management because the pandemic’s restrictions underscored her perception of the logistic difficulties associated with in-center dialysis (quote 4f in Table 2).
Discussion
In this multisite qualitative study evaluating the effect of the COVID-19 pandemic on communication and shared decision making, we found that aspects of shared decision making improved by increasing discussion of home-based treatment modalities and acknowledgment of the prognosis of many older frail patients. Yet, lack of discussions of COVID-19–related risks, fewer education options, and still inconsistent discussions of advanced care planning and conservative management left patients with unaddressed concerns, with them navigating the emerging COVID-19 guidance on their own. Importantly, despite heightened uncertainty, patients’ preferences for treatment modality remained stable, and most perceived their chosen modality to be the safest. These findings underscore the importance of shared decision making, even under conditions of uncertainty, and highlight opportunities for improvement.
We found that clinicians reported a shift toward recommending home dialysis during the pandemic, whereas discussions of conservative management remained rare. Furthermore, participants reported that potential COVID-19 risks were not integrated into their clinician discussions or decision making, indicating new and ongoing challenges to policy goals for CKD quality care. Medicare fee for service spends 23% of its budget on CKD beneficiaries. To reduce costs while supporting patient choice, the Executive Order on Advancing American Kidney Health promoted home dialysis and kidney transplant (29). Early in the pandemic, heightened fears of COVID-19 associated with the mandatory congregate in-center HD environment are likely to have contributed to increased discussions of home dialysis (23,30–33). It will be important to determine if the qualitative findings here are supported by empirical evidence of increased uptake of home dialysis and if any increases persist as the pandemic abates. What our study demonstrates is that reframing the risks and benefits of treatment modalities can lead to shifts in clinician views and practices.
Conservative care offered similar benefits to home dialysis for this population when it comes to avoiding COVID-19 infection. Yet, as was found in our study and consistent with prepandemic research, many nephrologists still did not engage in these discussions or describe conservative management as an option (34). Clinicians can champion the goals of the Advancing American Kidney Health Initiative by enhancing presentation of the many options for treating advanced CKD and by improving the shared decision-making process both during the pandemic and in the future. Clinicians can ask patients directly about their concerns regarding safety and quality of life and share up-to-date data about COVID-19 risks and treatment options for individuals with CKD.
Our findings also suggest that shared decision making in CKD can be improved by clinicians engaging in discussions to elicit preferences for advanced care planning. If treatment decisions have already been made, advanced care planning can help patients and their caregivers prepare for possible future setbacks by discussing possible scenarios and clarifying their treatment preferences (18). Discussions with patients should include not only the role of nonpharmaceutical prevention measures but also vaccination and potential therapies should patients contract severe acute respiratory syndrome coronavirus 2.
Our study found that during the pandemic, patients and care partners had persistent questions about their vulnerability and the effects of COVID-19 on kidney disease and treatments, and these were not always addressed. Potential clinician-level barriers to discussions included time constraints, the emotional toll of the pandemic, and lack of training. For patients with chronic disease, a lack of opportunity to discuss concerns about COVID-19 may increase anxiety and depression and amplify disparities among the most vulnerable (34–36). Our results clarify the need to engage older patients in discussions about evolving risk during uncertain situations. Training that enables clinicians to approach decision-making discussions to gracefully include all risks, including those that are new or uncertain, within a health equity lens while also helping patients to hope for the best but prepare for the worst should also be developed and implemented.
Attention also needs to be directed toward the high levels of burnout in nephrology caused by the pandemic, demands on time, and workforce limitations, indicating a critical need to improve tools for clinicians (37,38). Evidence suggests that the level of mental health distress experienced by nephrologists during the pandemic has put them at risk for developing mental health disorders (39). Furthermore, studies indicate that fewer trainees are electing to pursue nephrology, partly as a result of their perceived lack of work-life balance in this specialty (40). Accordingly, there is a need to incorporate novel educational tools and strategies to reduce burnout as well as recruit and retain nephrology trainees.
As we think about the future, our findings suggest an openness to telemedicine, as participants perceived this form of care to be convenient; it also gave care partners the ability to participate in clinical encounters when in-person care was restricted. This openness may provide an opportunity to help improve work-life balance by improving efficiency and quality care. For example, openness to virtual encounters may also suggest a willingness to engage with other virtual tools, including web-based decision aids that can facilitate subsequent shared decision-making conversations for older patients with CKD with clinicians by providing a previsit balanced description of the options and their pros and cons (e.g., effect on prognosis and the role of patient preferences and treatment decisions) (26).
Study strengths include the large multisite qualitative study with racially and geographically diverse participants who represented a spectrum of modality choices and preferences. This study included the key stakeholders engaged in shared decision making: patients, care partners, and clinicians. Limitations include an under-representation of Hispanic patients and non-English speakers, populations that are highly vulnerable and disproportionately affected by both COVID-19 and CKD. Another limitation is recall bias due to the time lapse between when the treatment decision-making conversation occurred and the interview, which could affect what one remembers from a conversation. We attempted to mitigate recall bias by interviewing patients and care partners proximal to clinical encounters, typically a few weeks after a visit to accommodate patients’ scheduling preferences. Patient and care partner interviews were conducted after the randomization and the exposure to a decision aid. Participants on dialysis (20%) had already made their treatment choice, allowing for the understanding of patients’ preference at different stages of decision making. The absence of balance in treatment preferences may have led to an over-representation of those who prefer dialysis over other options. Additionally, perceptions regarding the effect of COVID-19 could vary over time and by region, reflecting the differing effects of the pandemic on participants’ experiences.
The vulnerability of older patients with CKD to COVID-19 affected shared decision making during the pandemic. To improve shared decision making during the pandemic and its aftermath, clinicians should promote and encourage conversations with patients who want to talk about COVID-19 with an emphasis on safety and quality of life, including the risks posed to them by COVID-19 and the effect of COVID-19 on treatment options. These discussions should present all options, including conservative management, and incorporate advanced care planning. Clinician burnout must be addressed with adequate resources and appropriate training. Training should enable approaching difficult conversations and bring awareness toward ongoing disparities in patient treatment, with the goal of improving shared decision making to optimize patient-centered care.
Disclosures
K.E. Aufort reports research funding from Tufts University. G. Di Perna reports employment with Maine General Kidney Care and ownership interest in Crowdstrike and Palantir. E.J. Gordon reports the following honoraria and travel reimbursements for presentations and meetings: Advisory Committee on Blood and Tissue Safety and Availability (ACBTSA), the National Heart, Lung, and Blood Institute (NHLBI) Data and Safety Monitoring Board (DSMB), a National Institutes of Health ad hoc study section grant reviewer, and National Institute of Allergy and Infectious Disease (NIAID) DSMB. E.J. Gordon reports serving as a member of ACBTSA, an associate editor for American Journal of Transplantation, an associate editor for Narrative Inquiry in Bioethics, a member of National Academies of Science, Engineering and Medicine (NASEM) Committee, a member of NHLBI DSMB, and a member of NIAID DSMB and other interests or relationships as a member of the American Society of Transplantation Inclusion, Diversity, Equity and Access to Life (AST IDEAL) Task Force, a member of the AST Living Donor Community of Practice, and cochair of AST Psychosocial and Ethics Community of Practice (PSECOP). E. Gordon's husband is a partner in Halock Security Labs, which is not related to health care. T. Isakova reports consultancy agreements with Akebia Therapeutics, Inc.; honoraria from Akebia Therapeutics, Inc.; consulting honoraria from Akebia Therapeutics, Inc., Kyowa Kirin Co., Ltd., and LifeSci Capital, LLC; and serving as an associate editor of American Journal of Kidney Diseases. S. Koch-Weser reports ownership interest in Performa Rowing LLC and research funding from the AB InBEV Foundation, which is fully funded by AB InBev. K. Ladin reports research funding from Dialysis Clinics, Inc., The Greenwall Foundation, National Institute of Nursing-National Institute of Nursing Research (NIN-NINR), the Patient-Centered Outcomes Research Institute, and Paul Teschan Research Fund 2021-08; serving in an advisory or leadership role for the Data Safety and Monitoring Board of the National Institute of Diabetes and Digestive and Kidney Diseases; and serving as chair of the ethics committee of Organ Procurement and Transplantation Network (OPTN) and United Network for Organ Sharing (UNOS). D.E. Rifkin reports serving as feature editor of American Journal of Kidney Diseases; serving on the American Board of Internal Medicine (ABIM) Nephrology Exam Committee; and serving as a coinvestigator of the US site for the Study of Heart and Kidney Protection With Empagliflozin (EMPA-KIDNEY) study (pending). A. Rossi reports employment with Piedmont Transplant Institute. D.E. Weiner reports research funding from Bayer (site principal investigator [PI]), CSL Behring (site PI), and Goldfinch Bio (site PI), with all compensation paid to Tufts Medical Center; consulting honoraria from Akebia Therapeutics (paid to Dialysis Clinics, Inc.) and Cara Therapeutics; serving as a member of the American Society of Nephrology (ASN) Quality and Policy Committees, an ASN representative to Kidney Care Partners (KCP), Medical Director of Clinical Research at Dialysis Clinics, Inc., Editor-in-Chief of Kidney Medicine, and Co–Editor-in-Chief of National Kidney Foundation's Primer on Kidney Diseases, 8th Edition; serving on the scientific advisory board of the National Kidney Foundation; and other interests or relationships as a member of the data monitoring committee of the Feasibility of Hemodialysis with GARNET in Chronic Hemodialysis Patients with a Bloodstream Infection trial (Avania Contract Research Organization [CRO]), a member of the safety and clinical events committee for A Prospective, Multi-Center, Open-Label Assessment of Efficacy and Safety of Quanta SC+ for Home Hemodialysis trial (Avania CRO), and chair of the adjudications committee of the Veterans Affairs Lung Cancer Surgery Or Stereotactic Radiotherapy (VALOR) trial (George Institute, CRO; sponsored by Tricida). J.B. Wong reports serving as a panel member of the American Association for the Study of Liver Disease and Infectious Diseases Society of America, Recommendations for Testing, Managing, and Treating Hepatitis C; associate statistical editor of Annals of Internal Medicine; a member of the publications committee of the Massachusetts Medical Society; Interim Chief Scientific Officer of Tufts Medical Center; and a member of the US Preventive Services Task Force. All remaining authors have nothing to disclose.
Funding
This work was supported by George M. O’Brien Kidney Research Center at Northwestern University grants NU-GoKIDNEY and P30DK114857; National Institutes of Health (NIH)/National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grants R01DK110087, P30DK114857, and U2CDK129917; and Patient-Centered Outcomes Research Institute (PCORI) grant CDR-2017C1-6297.
Supplementary Material
Acknowledgments
The authors thank Noah D’Arcangelo, Olivia Bronzi, and Julia Perugini for their excellent research assistance.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
Author Contributions
K. Ladin and D.E. Weiner conceptualized the study; K.E. Aufort, G. Di Perna, K.M. Gonzales, E.J. Gordon, T. Isakova, S. Koch-Weser, K. Ladin, S. Levine, T. Porteny, D.E. Rifkin, A. Rossi, D.E. Weiner, and J.B. Wong were responsible for data curation; K.E. Aufort, G. Di Perna, K.M. Gonzales, E.J. Gordon, T. Isakova, S. Koch-Weser, K. Ladin, S. Levine, T. Porteny, D.E. Rifkin, A. Rossi, D.E. Weiner, and J.B. Wong were responsible for investigation; K.E. Aufort, G. Di Perna, K.M. Gonzales, E.J. Gordon, T. Isakova, S. Koch-Weser, K. Ladin, S. Levine, T. Porteny, D.E. Rifkin, A. Rossi, D.E. Weiner, and J.B. Wong were responsible for formal analysis; K.E. Aufort, G. Di Perna, K.M. Gonzales, E.J. Gordon, T. Isakova, S. Koch-Weser, K. Ladin, S. Levine, T. Porteny, D.E. Rifkin, A. Rossi, D.E. Weiner, and J.B. Wong were responsible for methodology; K. Ladin and D.E. Weiner were responsible for funding acquisition; K. Ladin and D.E. Weiner provided supervision; K. Ladin and T. Porteny wrote the original draft; and K.E. Aufort, G. Di Perna, K.M. Gonzales, E.J. Gordon, T. Isakova, S. Koch-Weser, K. Ladin, S. Levine, T. Porteny, D.E. Rifkin, A. Rossi, D.E. Weiner, and J.B. Wong reviewed and edited the manuscript.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.13241021/-/DCSupplemental.
Supplemental Appendix 1. DART stakeholder advisory board.
Supplemental Appendix 2. Patient, care partner, and clinician interview scripts.
Supplemental Appendix 3. Methodological supplement.
References
- 1.Henry BM, Lippi G: Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection. Int Urol Nephrol 52: 1193–1194, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pakhchanian H, Raiker R, Mukherjee A, Khan A, Singh S, Chatterjee A: Outcomes of COVID-19 in CKD patients: A multicenter electronic medical record cohort study. Clin J Am Soc Nephrol 16: 785–786, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ziemba R, Campbell KN, Yang TH, Schaeffer SE, Mayo KM, McGann P, Quinn S, Roach J, Huff ED: Excess death estimates in patients with end-stage renal disease - United States, February-August 2020. MMWR Morb Mortal Wkly Rep 70: 825–829, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Novick TK, Rizzolo K, Cervantes L: COVID-19 and kidney disease disparities in the United States. Adv Chronic Kidney Dis 27: 427–433, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsu CM, Weiner DE, Aweh G, Miskulin DC, Manley HJ, Stewart C, Ladik V, Hosford J, Lacson EC, Johnson DS, Lacson E Jr.: COVID-19 among US dialysis patients: Risk factors and outcomes from a national dialysis provider. Am J Kidney Dis 77: 748–756.e1, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Petrilli CM, Jones SA, Yang J, Rajagopalan H, O’Donnell L, Chernyak Y, Tobin KA, Cerfolio RJ, Francois F, Horwitz LI: Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: Prospective cohort study. BMJ 369: m1966, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Valeri AM, Robbins-Juarez SY, Stevens JS, Ahn W, Rao MK, Radhakrishnan J, Gharavi AG, Mohan S, Husain SA: Presentation and outcomes of patients with ESKD and COVID-19. J Am Soc Nephrol 31: 1409–1415, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weiner DE, Watnick SG: Hemodialysis and COVID-19: An Achilles’ heel in the pandemic health care response in the United States. Kidney Med 2: 227–230, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Oskoui T, Pandya R, Weiner DE, Wong JB, Koch-Weser S, Ladin K: Advance care planning among older adults with advanced non–dialysis-dependent CKD and their care partners: Perceptions versus reality? Kidney Med 2: 116–124, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Loon IN, Goto NA, Boereboom FTJ, Verhaar MC, Bots ML, Hamaker ME: Quality of life after the initiation of dialysis or maximal conservative management in elderly patients: A longitudinal analysis of the Geriatric assessment in OLder patients starting Dialysis (GOLD) study. BMC Nephrol 20: 108, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fu R, Sekercioglu N, Mathur MB, Couban R, Coyte PC: Dialysis initiation and all-cause mortality among incident adult patients with advanced CKD: A meta-analysis with bias analysis. Kidney Med 3: 64–75.e1, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Foote C, Kotwal S, Gallagher M, Cass A, Brown M, Jardine M: Survival outcomes of supportive care versus dialysis therapies for elderly patients with end-stage kidney disease: A systematic review and meta-analysis. Nephrology (Carlton) 21: 241–253, 2016 [DOI] [PubMed] [Google Scholar]
- 13.Ladin K, Lin N, Hahn E, Zhang G, Koch-Weser S, Weiner DE: Engagement in decision-making and patient satisfaction: A qualitative study of older patients’ perceptions of dialysis initiation and modality decisions. Nephrol Dial Transplant 32: 1394–1401, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams AW: Older adults with CKD and acute kidney failure: Do we know enough for critical shared decision making? J Am Soc Nephrol 25: 5–8, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yu X, Nakayama M, Wu M-S, Kim Y-L, Mushahar L, Szeto CC, Schatell D, Finkelstein FO, Quinn RR, Duddington M: Shared decision-making for a dialysis modality. Kidney Int Rep 7: 15–27, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Murray MA, Bissonnette J, Kryworuchko J, Gifford W, Calverley S: Whose choice is it? Shared decision making in nephrology care. Semin Dial 26: 169–174, 2013 [DOI] [PubMed] [Google Scholar]
- 17.Frazier R, Levine S, Porteny T, Tighiouart T, Wong JB, Isakova T, Koch-Weser S, Gordon EJ, Wiener DE, Ladin K: Shared decision-making among older adults with advanced chronic kidney disease [published online ahead of print March 26, 2022]. Am J Kidney Dis 10.1053/j.ajkd.2022.02.017 [DOI] [PubMed] [Google Scholar]
- 18.Ladin K, Neckermann I, D’Arcangelo N, Koch-Weser S, Wong JB, Gordon EJ, Rossi A, Rifkin D, Isakova T, Weiner DE: Advance care planning in older adults with CKD: Patient, care partner, and clinician perspectives. J Am Soc Nephrol 32: 1527–1535, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uvais NA, Aziz F, Hafeeq B: COVID-19-related stigma and perceived stress among dialysis staff. J Nephrol 33: 1121–1122, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nair D, Malhotra S, Lupu D, Harbert G, Scherer JS: Challenges in communication, prognostication and dialysis decision-making in the COVID-19 pandemic: Implications for interdisciplinary care during crisis settings. Curr Opin Nephrol Hypertens 30: 190–197, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCartney M, Sullivan F, Heneghan C: Information and rational decision-making: Explanations to patients and citizens about personal risk of COVID-19. BMJ Evid Based Med 26: 143, 2020 [DOI] [PubMed] [Google Scholar]
- 22.Martin DE, Parsons JA, Caskey FJ, Harris DCH, Jha V: Ethics of kidney care in the era of COVID-19. Kidney Int 98: 1424–1433, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yerram P, Misra M: Home dialysis in the coronavirus disease 2019 era. Adv Chronic Kidney Dis 27: 442–446, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Barber SJ, Kim H: COVID-19 worries and behavior changes in older and younger men and women. J Gerontol B Psychol Sci Soc Sci 76: e17–e23, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wong SPY, Hebert PL, Laundry RJ, Hammond KW, Liu C-F, Burrows NR, O’Hare AM: Decisions about renal replacement therapy in patients with advanced kidney disease in the US Department of Veterans Affairs, 2000–2011. Clin J Am Soc Nephrol 11: 1825–1833, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ladin K, Porteny T, Perugini JM, Gonzales KM, Aufort KE, Levine SK, Wong JB, Isakova T, Rifkin D, Gordon EJ, Rossi A, Koch-Weser S, Wiener DE: Perceptions of telehealth vs in-person visits among older adults with advanced kidney disease, care partners, and clinicians. JAMA Netw Open 4: e2137193, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tong A, Sainsbury P, Craig J: Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int J Qual Health Care 19: 349–357, 2007 [DOI] [PubMed] [Google Scholar]
- 28.Chase S, editor: Narrative Inquiry: Multiple Lenses, Approaches and Voices, 3rd Ed., Thousand Oaks, CA, Sage Publications, 2005 [Google Scholar]
- 29.Pearson J, Turenne M, Leichtman A: The executive order on kidney care: An opportunity to improve outcomes for individuals with kidney disease. Kidney Int Rep 4: 1519–1522, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Brown EA, Perl J: Increasing peritoneal dialysis use in response to the COVID-19 pandemic: Will it go viral? J Am Soc Nephrol 31: 1928–1930, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilkie M, Davies S: Peritoneal dialysis in the time of COVID-19. Perit Dial Int 40: 357–358, 2020 [DOI] [PubMed] [Google Scholar]
- 32.Stern LD, Waikar S, editors: Time to Expand Access and Utilization of Home Dialysis: Lessons from the COVID-19 Pandemic, Amsterdam, Elsevier, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sloan CE, Coffman CJ, Sanders LL, Maciejewski ML, Lee SD, Hirth RA, Wang V: Trends in peritoneal dialysis use in the United States after Medicare payment reform. Clin J Am Soc Nephrol 14: 1763–1772, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Umucu E, Lee B: Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabil Psychol 65: 193–198, 2020 [DOI] [PubMed] [Google Scholar]
- 35.Browne T, Grandinetti A: Please do not forget about us: The need for patient-centered care for people with kidney disease and are at high risk for poor COVID-19 outcomes. Am J Transplant 20: 3267–3268, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Greenberg N: Mental health of health-care workers in the COVID-19 era. Nat Rev Nephrol 16: 425–426, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lederer E, Lebowitz J: Current state of the workforce in nephrology. Adv Chronic Kidney Dis 27: 281–290.e1, 2020 [DOI] [PubMed] [Google Scholar]
- 38.Butler CR, Wong SPY, Wightman AG, O’Hare AM: US clinicians’ experiences and perspectives on resource limitation and patient care during the COVID-19 pandemic. JAMA Netw Open 3: e2027315, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mc Keaveney C, Reid J, Carswell C, Bonner A, de Barbieri I, Johnston W, Maxwell AP, O’Riordan J, Strini V, Walsh I, Noble H: Experiences of renal healthcare practitioners during the COVID-19 pandemic: A multi-methods approach. BMC Nephrol 22: 301, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nair D, Brereton L, Hoge C, Plantinga LC, Agrawal V, Soman SS, Choi MJ, Jaar BG; National Kidney Foundation Education Committee : Burnout among nephrologists in the United States: A survey study. Kidney Med 4: 100407, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.