Abstract
The evidence base supporting the usefulness of traditional cognitive-behavioral therapy (CBT) and newer acceptance-based CBT treatments for generalized anxiety disorder (GAD) has grown over the past decades. GAD is prevalent among several Latino subgroups, particularly Puerto Ricans. However, there remains uncertainty regarding the appropriateness of these interventions for Spanish-speaking Latinos since they have been routinely excluded in both efficacy and effectiveness studies. As an initial step to bridge this gap, this pilot study examined the potential efficacy of two CBT interventions for GAD, traditional CBT and acceptance-based behavioral therapy (ABBT), in a sample of Spanish-speaking Latinos. Ninety primary care patients with GAD were randomly assigned to receive CBT (n=30), ABBT (n=30), or treatment as usual (TAU) (n=30). Excessive worry, the core feature of GAD, was assessed with the Penn State Worry Questionnaire (PSWQ), which is considered the gold standard measure of GAD-related worry. At follow-up, PSWQ scores for participants in the CBT and ABBT groups were statistically lower than those of the TAU group and statistically comparable to each other. CBT and ABBT reduced worry level to a greater degree than usual care by follow-up. Our findings provide preliminary, yet crucial data, which support the potential of both interventions targeting GAD symptoms among Spanish-speaking Latino primary care patients.
Keywords: Latinos, Generalized anxiety disorder, Cognitive-behavioral therapy, Acceptance-based behavioral therapy, Primary care
Introduction
Generalized anxiety disorder (GAD) is prevalent among Latinos (Alegrzía et al., 2008a,b; Asnaani, Richey, Dimaite, Hinton, & Hofmann, 2010). Data from the most recent epidemiological survey of mental disorders collected from representative samples of Latino adults in the United States revealed that 4.2% of Latinos experienced GAD in their lifetime (Meng, Alegria, Chan, & Liu, 2004). However, when the data were disaggregated differences emerged among Latino subgroups. The GAD lifetime prevalence rate was 6.0% for Puerto Ricans, 5.8% for Cubans, 4.1% for Mexicans, and 3.5% for other Latinos. Similarly, high rates of GAD have also been reported for Puerto Rico residents. Data drawn from a household probability sample survey of 3062 adults showed that the prevalence rate for past-year GAD was 5.2% (Canino et al., 2016).
The core feature of GAD is out-of-control, excessive worry regarding ordinary daily situations (American Psychiatric Association, 2013). People with GAD show an increased hypervigilance to danger, continually perceiving threats that exist just in the mind and in the imaginary future (Borkovec, Newman, & Castonguay, 2003; Goodwin, Yiend, & Hirsch, 2017). According to Borkovec et al. (Borkovec et al., 2003; Borkovec, Alcaine, & Behar, 2004), worry functions as a type of cognitive avoidance mechanism used to identify ways of preventing anticipated disasters and to cope with the emotional reactivity generated by the perceived threat. The high level of anxiety and uncontrollable worry limits the ability to conduct daily activities, leading to significant impairment (Alonso et al., 2004; Kessler et al., 2009; Stein et al., 2005), poor quality of life (Barrera & Norton, 2009; Mendlowicz & Stein, 2000), low work productivity (Revicki et al., 2012), and increased health care utilization (Bereza, Machado, & Einarson, 2009; Hoffman, Dukes, & Wittchen, 2008; Revicki et al., 2012).
GAD is the most common anxiety disorder seen in primary care, but it is often unrecognized as many patients usually present with somatic symptoms that are often attributed to physical disorders (Kroenke, Spitzer, Williams, Monahan, & Löwe, 2007; Wittchen et al., 2002). GAD frequently coexists with other psychological and medical health problems, such as depressive disorders and multiple cardiovascular, gastrointestinal, respiratory, and endocrine conditions (Culpepper, 2009; Kessler, Keller, & Wittchen, 2001). When GAD is comorbid with another condition, patient outcomes are poorer compared to those with GAD alone (Bélanger, Ladouceur, & Morin, 2005; Davidson, Feltner, & Dugar, 2010). Furthermore, GAD patients with comorbidities are among the highest utilizers of medical services (Deacon, Lickel, & Abramowitz, 2008). Liu, Tian, Liu, Nigatu, and Wang (2019) examined the impact of GAD on the course of cardiovascular disease, they found that while GAD contributes to increase the risk of cardiovascular disease (CVD), a reduction of GAD symptoms is associated with reduced risk of new-onset CVD. These findings highlight the need for improved recognition and treatment of GAD patients within the primary care population.
Cognitive-behavioral therapy (CBT) enjoys high clinical approval and empirical support for the treatment of GAD (Borkovec et al., 2004; Butler, Chapman, Forman, & Beck, 2006). Traditional CBT models for GAD address behavioral avoidance and worry as maladaptive coping strategies used by the individual in the attempt to problem-solve and reduce undesirable thoughts and emotions (Borkovec, 1994; Borkovec et al., 2004). Intervention components include cognitive therapy to deal with worry and cognitive biases, applied relaxation to address tension, self-monitoring, imaginal exposure to catastrophic images, and exposure to stressful situations to practice learned coping responses (Borkovec, Newman, Pincus, & Lytle, 2002; Borkovec & Ruscio, 2001; Borkovec et al., 2003). Findings from meta-analyses and systematic reviews show that traditional CBT significantly reduces GAD symptoms and is more effective than no treatment or alternative treatments (Borkovec & Ruscio, 2001; Cuijpers et al., 2014; Gould, Safren, Washington, & Otto, 2004). Furthermore, the benefits of CBT are comparable to those reported for pharmacological interventions and tend to be sustained over 6- and 12-month follow-up (Borkovec et al., 2002; Covin, Ouiment, Seeds, & Dozois, 2008; Cuijpers et al., 2014; Heuzenroeder et al., 2004; Mitte, 2005). However, even though traditional CBT has been extensively studied and is considered by many as a first treatment option for GAD, the proportion of individuals that attain clinically significant change following treatment is lower than rates usual for other anxiety disorders (Bolognesi, Baldwin, & Ruini, 2014; Borkovec et al., 2002; Newman, Llera, Erickson, Przeworski, & Castonguay, 2013).
CBT evidence-based treatments have expanded over the past years to improve therapeutic approaches that facilitate distancing from pathological worries and anxious thoughts. Findings from studies focused on further advancing CBT for GAD provide promising evidence for approaches that integrate mindfulness and acceptance-based strategies to cognitive-behavioral therapies, particularly acceptance-based behavioral therapy (ABBT) (Orsillo & Roemer, 2011; Roemer & Orsillo, 2009) for GAD. ABBT is characterized by a focus on altering how individuals react to their internal experiences (thoughts, emotions, sensations, and memories) instead of changing the content or frequency of the experiences themselves (O’connor, Munnelly, Whelan, & McHugh, 2018; Roemer, Williston, Eustis, & Orsillo, 2013). The basic premise underlying the therapy is that anxious responses can be kept from intensifying by responding with awareness, openness, and acceptance rather than efforts to control or avoid unwanted feelings (Orsillo & Roemer, 2005). Processes central to treatment, such as experiential acceptance, values clarification, and attention to the present moment, are targeted with a variety of clinical methods, including psychoeducation, self-monitoring, mindfulness practices, and behavior change strategies (Hayes-Skelton, Roemer, & Orsillo, 2013; Roemer & Orsillo, 2009). Research findings show that ABBT has been associated with considerable improvements in anxiety and depression symptoms (Hayes-Skelton et al., 2013; Roemer, Orsillo, & Salters-Pedneault, 2008; Treanor, Erisman, Salters-Pedneault, Roemer, & Orsillo, 2011). In an initial crossover study, in which randomized participants received ABBT immediately or where placed on a waiting list to receive it later, ABBT significantly reduced GAD symptoms to non-clinical levels at follow-up, with benefits sustained over further 9 months (Roemer et al., 2008). More recently, investigators examined the effectiveness of ABBT in comparison to an established CBT treatment (Hayes-Skelton et al., 2013) showing that both treatments led to significant change across treatment and follow-up.
Over the past decades, increased emphasis has been placed on the inclusion of minorities in clinical research (US Department of Health & Human Services, 2001a). However, despite the National Institutes of Health requirement of sufficient inclusion of racial minority groups in their funded clinical trials, systematic reviews of mental health clinical trials show consistently low representation of Latinos (Benuto, Bennett, & Casas, 2020; Mendoza, Williams, Chapman, & Powers, 2012; Williams, Powers, Yun, & Foa, 2010). Although the evidence base supporting the usefulness of both traditional and acceptance-based cognitive-behavioral therapies for GAD has grown over the past decades, there remains uncertainty regarding the appropriateness of these interventions for Spanish-speaking Latinos since they have been routinely excluded in treatment outcome studies (Lau, Chang, & Okazaki, 2010). We bridge this gap by assessing whether Spanish-speaking Latinos with GAD benefit from traditional or acceptance-based cognitive behavioral treatments. Specifically, this randomized pilot study compared two interventions, CBT and ABBT, versus treatment-as-usual to examine the potential efficacy of each intervention for the treatment of GAD in a sample of low-income, Latino, primary care patients. We focused on Latino patients disadvantaged by income because low socioeconomic status has been associated with adverse effects on mental health and limited access to mental health specialty care (Allen, Bafour, Bell, & Marmot, 2014; Anakwenze & Zuberi, 2013). The primary care setting is especially important for mental health care delivery in patients disadvantaged by income, education and minority status (Department of Health and Human Services, 2011; McGuire & Miranda, 2008).
Methods
Participants and procedures
Ninety primary care patients were recruited to the study. The mean age of the randomized sample was 41 years, with range from 18 to 64 years. Most were women (86.7%) and were married or cohabitating (45.6%). Forty-one percent were employed and almost 30% had not completed high school (Table 1). Eligible participants were adults attending participating primary care clinics for general medical treatment. Criteria for inclusion included: ages 18 to 64, scores of at least 5.7 on the Generalized Anxiety Disorder Questionnaire (GAD-Q-IV) (Newman et al., 2002) and 56 on the Penn State Worry Questionnaire (PSWQ) (Meyer, Miller, Metzger, & Borkovec, 1990), fluent Spanish speaker, willingness to be randomized to treatment condition, and the intention to use the clinic as their main source of medical care in the following six-month period. Patients were excluded if they had a health problem or other situation that interfered with participation (severe medical illness, suicidal ideation, significant cognitive problems), had a history of schizophrenia or psychotic disorder, used drugs during the past six months, scored positive on the Alcohol Use Disorders Identification Test (AUDIT-C) (Bradley et al., 1998), or were receiving mental health treatment.
Table 1.
Baseline demographic characteristics across groups.
| Characteristic | Total (n = 90) |
ABBT (n = 30) |
CBT (n = 30) |
TAU (n = 30) |
F/X2 | p | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |||
| Female | 78 | 86.7 | 26 | 86.7 | 25 | 83.3 | 27 | 90.0 | 0.14 | 0.71 |
| Age, m (SD) | 40.77 (11.2) | 39.7 (10.8) | 42.4 (10.9) | 40.2 (12.1) | 0.46 | 0.63 | ||||
| Married or cohabitating | 41 | 45.6 | 16 | 53.3 | 14 | 46.7 | 11 | 36.7 | 1.70 | 0.43 |
| High school or more | 64 | 71.1 | 24 | 80.0 | 23 | 76.7 | 17 | 56.7 | 4.65 | 0.10 |
| Employed | 37 | 41.1 | 12 | 40.0 | 15 | 50.0 | 10 | 33.3 | 1.74 | 0.42 |
SD: standard deviation.
A nonconsecutive convenience sample was drawn among patients presenting for physical health care at 10 primary care clinics, serving primarily low-income patients in urban areas of San Juan, Puerto Rico. Fig. 1 depicts the CONSORT flow diagram, which summarizes the recruitment and allocation of participants. Patients were individually approached by a research assistant while waiting for their medical appointment. In total, 5714 patients were screened for eligibility, over 80% of those approached agreed to participate. Screening interviews were conducted in private offices to ensure confidentiality. Three hundred and seven potential participants who appeared to be eligible for participation were invited for further assessment: 21 declined participation, 101 did not present for the assessment, and 185 completed the baseline assessment. A total of 130 patients with significant GAD symptoms were eligible for randomization, of these 40 were lost to further contact leaving a sample of 90 patients that were randomized: 30 to treatment as usual (TAU), 30 to ABBT, and 30 to CBT. Trained research staff with background in psychology was responsible for enrolling eligible participants using a number sequence developed by a computer random number generator. To obtain random assignment information for each participant, enrollment staff contacted the central office to receive information corresponding to the assigned treatment condition. Additional assessments were conducted in the primary care clinics where each participant was recruited. Assessments were arranged outside of treatment session and were conducted by assessors blind to randomization. Participants could stop therapy and continue with study assessments. In addition to baseline the following percentages completed week-20 and week-28 assessments: week-20, 90% TAU patients, 73.3% ABBT patients, and 73.3% CBT patients, and week-28, 96.7% TAU patients, 70% ABBT patients, and 86.7% CBT patients. Of the 60 patients randomized to ABBT and CBT, 12 (20%) did not initiate treatment. Among treatment initiators, treatment was completed (15 sessions or more) by 63.6% in the ABBT group and 42.3% in the CBT group. The average number of sessions attended was 12.8 for ABBT and 9 for CBT.
Fig. 1.
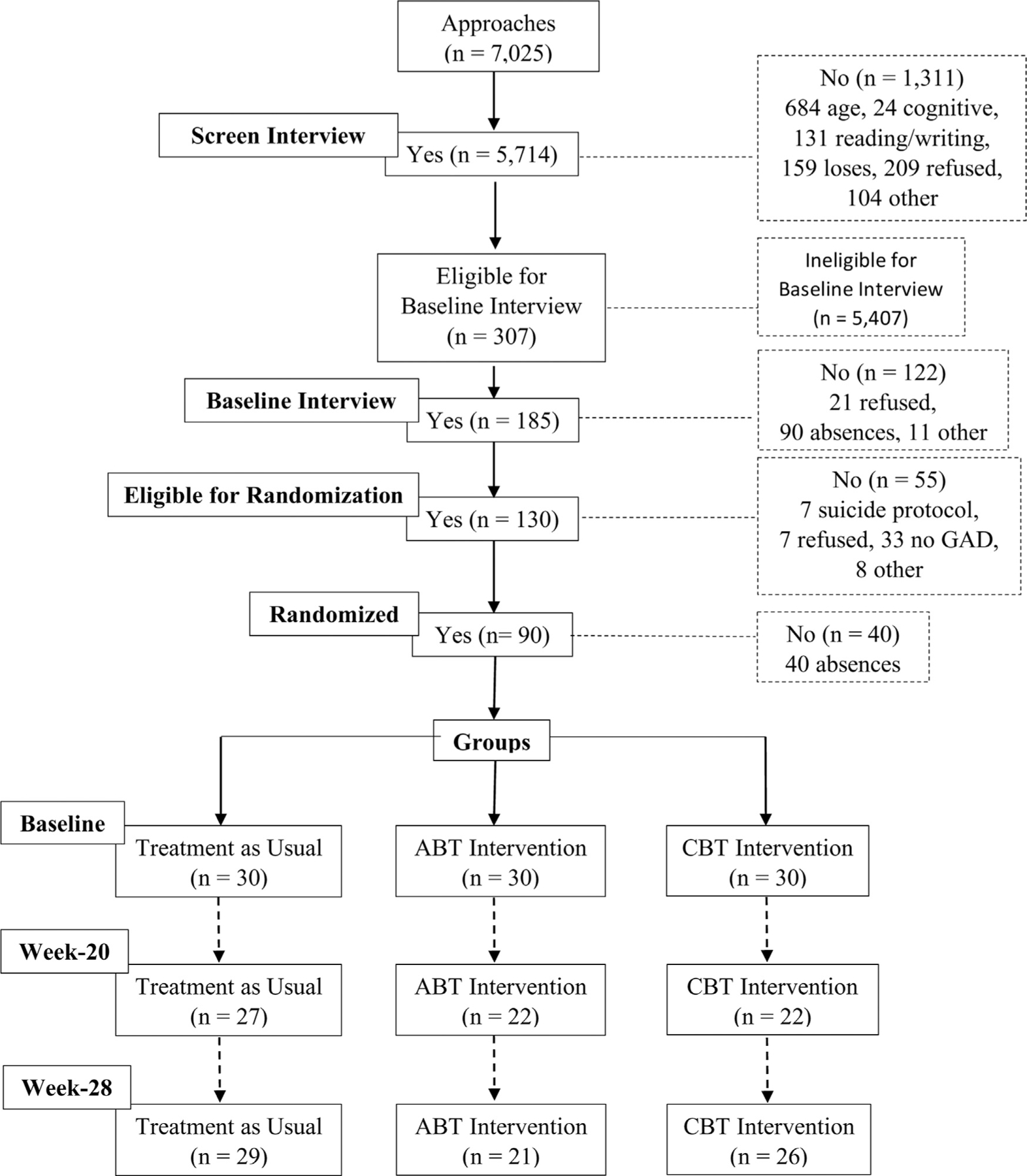
CONSORT flow diagram.
Treatment conditions
Cognitive-Behavioral Therapy
CBT for GAD consisted of 15 individual sessions of 1.5 hours. Sessions were delivered weekly, except for a separation of two weeks before the final session. The intervention followed a manualized CBT intervention for GAD developed by Borkovec et al. (2003). The manual was translated to Spanish and culturally adapted to include language, idioms, and examples relevant to Latino culture (Bernal, Jiménez-Chafey, & Domenech Rodríguez, 2009). Special emphasis was placed on the attainment of conceptual and cultural equivalence, while maintaining fidelity to the active core elements in the English CBT manual. The intervention is based on four main components: self-monitoring, applied relaxation training, cognitive therapy, and the rehearsal of learned coping responses (Borkovec & Sharpless, 2004; Borkovec et al., 2003). Central to CBT treatment is teaching participants to identify early anxiety cues that trigger their responses and interpretations of threat. Self-monitoring activities focus on helping them take notice of their interior and exterior experiences, with the goal of increasing recognition of their perceptions of threat and worrisome thoughts about the imagined future. Participants were encouraged to use applied relaxation techniques learned during treatment to cope with anxiety and worry. Targeted muscle relaxation exercises aimed to increase participants’ ability to rapidly produce relaxation to interrupt emerging anxiety and worry spirals. Meanwhile, cognitive therapy strategies allowed generating more accurate interpretations and perspectives of threat and worrisome reactions. The accuracy of cognitions was examined through the evaluation of their logic, probability, and past evidence, using strategies such as, decatastrophizing, worry outcome diary, and the Socratic method. The practice and implementation of newly learned relaxation and cognitive coping responses was emphasized throughout treatment to facilitate replacing habitual perspectives of worrisome activity with more adaptive ones.
Acceptance-based Behavioral Therapy
ABBT for GAD was delivered in 16 weekly sessions, the first four lasting 90 minutes and the rest 60 minutes. The ABBT implemented in this trial was based on a culturally adapted, Spanish version of the manualized intervention for GAD developed by Roemer and Orsillo (2009). While maintaining fidelity to the core elements of the English ABBT manual, the Spanish version includes language, idioms, and examples relevant to Latino culture (Bernal et al., 2009). ABBT includes behavioral elements derived from traditional CBT, while cognitive strategies that focus on correcting dysfunctional thoughts and emotions were replaced with strategies that promote psychological processes based on acceptance and mindfulness. ABBT clinical strategies, including psychoeducation, self-monitoring, and mindfulness practices, intend to demonstrate that the avoidance or suppression of unwanted internal states is not always helpful and could even contribute to worsen anxiety (Roemer & Orsillo, 2009; Roemer et al., 2013). Instead of focusing on controlling internal experiences ABBT familiarized participants with an acceptance-based behavioral model of anxiety, and facilitated the application of skills that fostered expanded awareness of the present moment and willingness to experience unwanted internal experiences. The focus was on increasing engagement in personally meaningful actions by facilitating behaviors that were consistent with participants’ personal values rather than motivated by worry, anxiety, and avoidance of thoughts, sensations, and feelings viewed as threatening and dangerous.
Treatment as usual
Patients randomly assigned to receive TAU were informed of their condition and the mental health resources available in keeping with their insurance coverage. Physicians were informed via a standardized form included in the medical record that the patient had been assigned to TAU. Patients were encouraged to discuss GAD treatment options with their provider. The standard of care in the participating primary care clinics was that patients were referred to the mental health system of care for specialized mental health treatment. The specialized sector of care provided pharmacological or psychological treatment. The amount of time spent in treatment and the strategies used could vary among providers. This was a pragmatic intervention that aimed to explore the outcome of a typical referral.
Therapists
Two female licensed psychologists, with three and five years of clinical experience, were the main therapists in this trial. To reduce the confounding of therapist effects they delivered CBT and ABBT. They received ABBT training from Drs. Roemer and Orsillo and CBT training from Dr. Borkovec. All sessions were recorded, and a random sample was reviewed. For fifty percent of ABBT and CBT participants, one session was randomly chosen from sessions 1‒5, one from 6‒11, and one from 12‒16, when available. A total of 71 (ABBT = 36; CBT = 35) sessions were rated for adherence to the respective protocols by doctoral students in clinical psychology. For each session an adherence checklist listed the required components which were considered as proxy measures for therapy essential elements. Around 95% of the required components were covered for both ABBT (94.47%) and CBT (95.20%).
Outcome measures
Penn State Worry Questionnaire (PSWQ)
The PSWQ (Meyer et al., 1990) is a 16-item self-report assessment designed to measure worry. The items measure the occurrence, intrusiveness, intensity, and other characteristics of an individual’s experience with worry. Each item is rated on a 5-point Likert scale ranging from 1 (not at all typical of me) to 5 (very typical of me). Possible scores range from 16‒80, with a recommended cut-off score of 45 or higher to identify high worrying individuals (Behar, Alcaine, Zuellig, & Borkovec, 2003). The PSWQ has shown excellent reliability and validity (Brown, Antony, & Barlow, 1992; Fresco, Heimberg, Mennin, & Turk, 2002). The Spanish version of the PSWQ has demonstrated appropriate test-retest reliability, high internal consistency, and good convergent and discriminant validity (Nuevo-Benítez, Montorio-Cerrato, & Ruiz-Díaz, 2002; Rodríguez-Biglieri, 2011). In the current study, the PSWQ demonstrated good internal consistency at pre-treatment (α = .80). It was administered at baseline and week-28 assessments.
Patient Health Questionnaire (PHQ-9)
The PHQ-9 (Spitzer, Kroenke, & Williams, 1999) is a 9-item, self-report scale that assesses the presence of the nine DSM-IV diagnostic criteria for major depression. Each item asks patients to indicate the frequency with which they experienced the depressive symptom, scored on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). Possible scores range from 0 to 27, with higher scores indicating increased levels of depression symptoms. The PHQ-9 has demonstrated good psychometric properties and has been shown to have excellent discriminatory power to identify patients with depression (Williams et al., 2005). Psychometric studies sustain the validity of the Spanish version of the PHQ-9 (Diez-Quevedo, Rangil, Sanchez-Planell, Kroenke, & Spitzer, 2001; Baader et al., 2012). Internal consistency in the current study was excellent at pre-treatment (α = .90). Participants completed the PHQ-9 at baseline and week-28.
Depression and Anxiety Stress Scale (DASS-21)
The DASS-21 (Lovibond & Lovibond, 1995) is a 21-item, self-report questionnaire that measures distress in three different subscales: depression, anxiety, and stress. Each subscale consists of 7 items rated on a 4-point Likert scale ranging from 0 (did not apply to me at all) to 3 (applied to me very much or most of the time). Scores on the DASS-21 are multiplied by two to calculate the final score. Higher scores indicate greater levels of symptoms. The depression subscale assesses hopelessness, low self-esteem, and lack of involvement. The anxiety subscale assesses autonomic arousal, skeletal muscle symptoms, situational anxiety, and subjective experience of anxious arousal. The stress subscale assesses tension, agitation, over reaction, and impatience. The DASS-21 demonstrates high internal consistency and concurrent validity indicating that it distinguishes well between features of depression, anxiety, and stress (Antony, Cox, Enns, Bieling, & Swinson, 1998). The psychometric properties and factor structure of the Spanish version of the DASS-21were comparable to those of the English version (Daza, Novy, Stanley, & Averill, 2002). In the current study, the subscales demonstrated good internal consistency at baseline with Cronbach’s alpha coefficients of 0.84 for the depression subscale, 0.83 for the anxiety subscale, and 0.86 for the stress subscale. The DASS-21 was administered at baseline, week-20, and week-28.
Statistical analysis
Descriptive statistics, including frequencies, means, and standard deviations, were estimated to examine sample demographic and clinical characteristics. Distributions for the intervention and control groups were examined for baseline equivalency by using t tests for continuous data and chi square tests for categorical data. To test the effect of two treatments for GAD (CBT and ABBT) versus treatment-as-usual we compared changes from baseline to posttreatment on an intention-to-treat basis. Treatment effects for each dependent measure were estimated primarily through the group-by-time interactions, followed by pairwise comparisons for the three groups. Different covariance structures were examined to determine the best one for our data. A compound symmetry covariance matrix was specified to account for the within-patient correlation among repeated assessments. The model adjusted by outcome baseline values when appropriate. Calculations were conducted using PROC MIXED and GLIMMIX procedures in SAS software, version 9.4 (SAS Institute Inc., 2013). In accordance with Jacobson and Traux (1991), clinically significant change was examined by calculating a reliable change index for the PSWQ. For each treatment group, the standard deviation of the baseline measurement and a reliability coefficient of 0.93, as informed by Meyer et al. (1990), was used to identify the proportion of participants in each group who met the criteria for reliable change on the PSWQ.
Results
Primary outcomes: worry, anxiety, and stress symptoms
PSWQ
Mean scores on the PSWQ scale for both ABBT and CBT groups show that the level of worry improved from the high range at baseline to the moderate range at follow-up, whereas mean scores for usual care participants remained at a high level (Table 2). Mixed-effects regression models evidence statistically significant main effects for the interaction between time and treatment (F = 3.09, p < .051). As shown in Table 3, pairwise comparisons indicate that in comparison to TAU both ABBT (t = −2.69, p = .008) and CBT participants (t = −3.27, p = .001) demonstrated significantly greater reductions in worry. When comparing outcomes between participants in the ABBT group versus those in the CBT group, no significant differences were observed at follow-up (t = 0.59, p = .557). Based on criteria for clinically significant change, 57% of the ABBT group, 60% of the CBT group, and 43% of the TAU group were classified as having achieved a reliable decrease in PSWQ scores. In addition, a significant increase in PSWQ scores at follow-up was identified for 20% of the TAU group.
Table 2.
Intent-to-treat analyses of primary and secondary measures
| Outcome | ABBT |
CBT |
TAU |
Group | Time | F | Group × Time | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Mean | 95% CI | n | Mean | 95% CI | n | Mean | 95% CI | |||||
| PSWQ | |||||||||||||
| Baseline | 30 | 66.73 | 64.24 to 69.23 | 29 | 67.76 | 65.01 to 70.51 | 30 | 66.67 | 64.46 to 68.88 | 0.05 | < .001 | 3.09 | 0.051 |
| Follow-up | 21 | 45.95 | 38.21 to 53.69 | 26 | 48.27 | 41.67 to 54.87 | 29 | 59.93 | 54.06 to 65.80 | ||||
| DASANX | |||||||||||||
| Baseline | 30 | 22.60 | 19.05 to 26.15 | 30 | 26.67 | 22.22 to 31.11 | 30 | 18.33 | 14.51 to 22.16 | 0.14 | < .001 | 3.29 | 0.013 |
| Week 20 | 22 | 11.64 | 7.64 to 15.64 | 22 | 13.27 | 8.08 to 18.47 | 27 | 12.67 | 8.67 to 16.66 | ||||
| Follow-up | 21 | 11.81 | 6.98 to 16.64 | 26 | 14.15 | 9.16 to 19.14 | 29 | 13.59 | 9.75 to 17.42 | ||||
| DASSTR | |||||||||||||
| Baseline | 30 | 30.00 | 26.49 to 33.51 | 30 | 29.73 | 26.01 to 33.46 | 30 | 22.87 | 19.37 to 26.37 | 0.07 | < .001 | 4.30 | 0.003 |
| Week 20 | 22 | 15.73 | 11.02 to 20.43 | 21 | 14.29 | 8.51 to 20.06 | 27 | 19.19 | 15.13 to 23.24 | ||||
| Follow-up | 21 | 14.95 | 9.79 to 20.12 | 26 | 18.00 | 12.47 to 23.53 | 29 | 17.72 | 13.31 to 22.14 | ||||
| PHQ-9 | |||||||||||||
| Baseline | 30 | 14.50 | 12.43 to 16.57 | 30 | 16.07 | 14.33 to 17.81 | 30 | 12.10 | 10.16 to 14.04 | 0.08 | < .001 | 5.34 | 0.007 |
| Follow-up | 19 | 6.89 | 4.01 to 9.78 | 25 | 9.88 | 7.14 to 12.62 | 26 | 11.08 | 8.72 to 13.43 | ||||
| DASDEP | |||||||||||||
| Baseline | 30 | 21.80 | 18.59 to 25.01 | 29 | 24.00 | 19.69 to 28.31 | 30 | 17.20 | 14.08 to 20.32 | 0.09 | < .001 | 3.63 | 0.008 |
| Week 20 | 22 | 9.82 | 5.79 to 13.85 | 22 | 10.64 | 6.25 to 15.03 | 27 | 12.81 | 8.82 to 16.81 | ||||
| Follow-up | 21 | 9.24 | 4.70 to 13.78 | 26 | 13.15 | 8.55 to 17.76 | 29 | 12.76 | 9.10 to 16.42 | ||||
PSWQ: Penn State Worry Questionnaire; DASANX: DASS-21 Anxiety Subscale; DASSTR: DASS-21 Stress Subscale; PHQ-9: Patient Health Questionnaire; DASDEP: DASS-21 Depression Subscale.
Table 3.
Pairwise comparisons for pre- and follow-up outcome measures scores.
| Measure | Treatment | t value; p |
|---|---|---|
| PSWQ | TAU vs. ABBT | −2.69; 0.008 |
| TAU vs. CBT | −3.27; 0.001 | |
| ABBT vs. CBT | 0.59; 0.557 | |
| DASANX | TAU vs. ABBT | −1.86; 0.065 |
| TAU vs. CBT | −2.55; 0.011 | |
| ABBT vs. CBT | 0.60; 0.551 | |
| DASSTR | TAU vs. ABBT | −2.61; 0.010 |
| TAU vs. CBT | −1.36; 0.175 | |
| ABBT vs. CBT | −1.32; 0.189 | |
| PHQ-9 | TAU vs. ABBT | −2.96; 0.004 |
| TAU vs. CBT | −3.74; 0.001 | |
| ABBT vs. CBT | 0.84; 0.404 | |
| DASDEP | TAU vs. ABBT | −2.38; 0.019 |
| TAU vs. CBT | −1.96; 0.052 | |
| ABBT vs. CBT | −0.48; 0.636 |
PSWQ: Penn State Worry Questionnaire; DASANX: DASS-21 Anxiety Subscale; DASSTR: DASS-21 Stress Subscale; PHQ-9: Patient Health Questionnaire; DASDEP: DASS-21 Depression Subscale.
DASS-21 anxiety subscale
As Table 2 shows, baseline mean DASS-21 anxiety subscale scores were significantly different among the three treatment groups (ABBT: 22.60, 95% CI: 19.05 to 26.15; CBT: 26.67, 95% CI: 22.22 to 31.11; TAU: 18.33, 95% CI: 14.51 to 22.16). Mean scores for both ABBT and CBT participants improved from extremely severe anxiety at baseline to moderate anxiety at follow-up (ABBT: 11.81, 95% CI: 6.98 to 16.64; CBT: 14.15, 95% CI: 9.16 to 19.14). Meanwhile, the mean scores for TAU participants shifted from the severe anxiety range at baseline to moderate anxiety at follow-up (TAU: 13.59, 95% CI: 9.75 to 17.42). Intent to treat analysis yielded a significant result for the time-by-group interaction (F = 3.29, p < .01) (Table 2). Pairwise comparisons show that at follow-up the CBT group was associated with significantly greater improvement in anxiety symptoms than the TAU group (t = −2.55, p = .011) (Table 3). In comparison to the TAU group, the ABBT group showed a marginally significant improvement (t = −1.86, p = .065). No significant differences in anxiety symptoms were found when comparing ABBT and CBT participants at follow-up (t = 0.60, p = .551).
DASS-21 stress subscale
Findings for the DASS-21 stress subscale showed significant differences in baseline mean scores among the three treatment groups (ABBT: 30, 95% CI: 26.49 to 33.51; CBT: 29.73, 95% CI: 26.01 to 33.46; TAU: 22.87, 95% CI: 19.37 to 26.37). Levels of stress improved for both ABBT and CBT participants from severe level at baseline to mild at follow-up (ABBT: 14.95, 95% CI: 9.79 to 20.12; CBT: 18, 95% CI: 12.47 to 23.53) (Table 2). Whereas mean scores improved for usual care participants from moderate at baseline to mild at follow-up (17.72, 95% CI: 13.31 to 22.14). Findings showed a significant interaction effect between time and treatment (F = 4.30, p < .01). At follow-up, in comparison to the TAU group participants in the ABBT group demonstrated a significantly greater improvement (t = −2.61, p = .010). Outcomes did not differ significantly when comparing CBT versus TAU participants (t = −1.36, p = .175) and ABBT versus CBT participants (t = −1.32, p = .189) (Table 3).
Secondary outcomes: depression symptoms
PHQ-9
Mean PHQ-9 scores differed significantly at baseline among the three treatment groups (ABBT: 14.50, 95% CI: 12.43 to 16.57; CBT: 16.07, 95% CI: 14.33 to 17.81; TAU: 12.10, 95% CI: 10.16 to 14.04) (Table 2). Baseline depression severity mean scores were at the moderately severe level for the ABBT and CBT groups and at the moderate level for the TAU group. Depression severity level shifted to mild for the ABBT group (6.89, 95% CI: 4.01 to 9.78) and moderate for the CBT group (9.88, 95% CI: 7.14 to 12.62), while severity level remained moderate for the TAU group. The interaction effect for time and treatment was significant (F = 5.34, p < .007). Table 3 shows that in comparison to TAU both ABBT (t = −2.96, p = .004) and CBT (t = −3.74, p = .001) were associated with significantly greater reductions in depression severity at follow-up. Outcomes for the ABBT group versus the CBT group were not significantly different at follow-up (t = 0.84, p = .404).
DASS-21 depression subscale
Baseline mean DASS-21 depression subscale scores showed significant differences among the three groups (ABBT: 21.80, 95% CI: 18.59 to 25.01; CBT: 24.00, 95% CI: 19.69 to 28.31; TAU: 17.20, 95% CI: 14.08 to 20.32). Mean scores improved from severe depression for both ABBT and CBT participants at baseline, to a normal range for those in ABBT and mild depression for those in CBT at follow-up (ABBT: 9.24, 95% CI: 4.70 to 13.78; CBT: 13.15, 95% CI: 8.55 to 17.76). Scores for TAU participants improved from the moderate level at baseline to mild depression at follow-up (TAU: 12.76, 95% CI: 9.10 to 16.42). Mixed-effects regression estimates yielded a significant result for the time-by-group interaction (F = 3.63, p < .008) (Table 2). At follow-up, ABBT participants showed a significantly greater reduction in depression symptoms in comparison to those in TAU (t = −2.38, p = .019), whereas CBT participants demonstrated a marginally significant reduction (t = −1.96, p = .052) in comparison to those in TAU (Table 3). When comparing outcomes between those in ABBT versus those in the CBT (t = −0.48, p = .636), no significant differences emerged.
Discussion
Although GAD has been found to be prevalent among several Latino subgroups, particularly Puerto Ricans, appropriate evidence-based treatments for this population are missing (Alegría et al., 2007; Alegría, Alvarez, Ishikawa, DiMarzio, & McPeck, 2016). The randomized pilot study reported here was designed to examine the potential efficacy of two interventions for GAD, traditional CBT and ABBT, in a sample of Spanish-speaking Latino primary care patients. Excessive worry, the core feature of GAD, was assessed with the PSWQ, which is considered the gold standard measure of GAD-related worry. At follow-up, PSWQ scores for participants in the CBT and ABBT groups were statistically lower than those of the TAU group and statistically comparable to each other. Our results demonstrate that CBT and ABBT resulted in clinically significant improvements. This improvement was evidenced in a sample within a high range baseline worry level. This study also evaluated changes in other primary and secondary outcomes. Overall, symptoms of general anxiety and depression improved over time for most of the outcome measures for clients receiving either CBT or ABBT. No significant benefit of one treatment over the other was evidenced for either general anxiety or depression symptoms. Overall, our findings suggest that both traditional CBT and ABBT are promising interventions for the treatment of Spanish-speaking Latinos with GAD. These results are in line with previous studies that support the efficacy of traditional and newer CBT approaches for GAD in predominantly non-Hispanic White populations (Borkovec et al., 2004; Butler et al., 2006; Hunot, Churchill, Teixeira, & Silva de Lima, 2007; Orsillo & Roemer, 2011; Otte, 2011; Roemer & Orsillo, 2009).
Several limitations in the interpretation of our data need to be considered. This study is subject to the potential biases associated with a pilot study. First, the small sample size and low retention rates limited generalizability and statistical power. Although subjects were recruited from multiple sites, these were mainly in low-income urban areas, limiting information for participants from other socioeconomic groups. Dropout rates before initiating treatment and during treatment were high. These findings are consistent with multiple studies that document poor initiation and retention in mental health treatment for low-income and ethnic minority populations (Arnow et al., 2007; Bados, Balaguer, & Saldaña, 2007; Blanco et al., 2007; Kozhimannil, Trinacty, Busch, Huskamp, & Adams, 2011; Santiago, Kaltman, & Miranda, 2013). Future studies with larger sample sizes are needed to further evaluate any treatment effects, as well as systemic, cultural, and individual barriers that may impact access and retention in mental health care. A second limitation was that study recruiters did not systematically select patients for screening in primary care reception rooms; this may subject the data to some selection bias. A third limitation was the use of a brief follow-up period. Studies using a longer follow-up period of six-months or twelve-months are needed to evaluate whether study findings can be maintained over time. Despite these limitations, findings from this trial can be viewed as early data that support the potential efficacy of traditional CBT and ABBT for Spanish-speaking Latinos with GAD.
To our knowledge, this is the first randomized trial to investigate the use of both traditional and newer CBT approaches for the treatment of GAD in Spanish-speaking primary care patients. Our findings are particularly important because they provide evidence in favor of the potential benefits of traditional CBT and ABBT for low-income, Spanish speaking Latinos in primary care settings. Substantial evidence sustains that Latinos’ mental health care needs are largely unfulfilled. In comparison with non-Hispanic Whites, studies have demonstrated that Latinos rely more on primary care providers for mental health care and are less likely to receive guideline congruent treatment for mental health problems (Alegría et al., 2002a,b, 2016; Chapa, 2004; Hogan, 2003; Lagomasino et al., 2005; Cabassa, Zayas, & Hansen, 2006; Institute of Medicine, 2003; US Department of Health and Human Services, 2001b).
A major goal of the Healthy People national initiative is to improve mental health by ensuring access to appropriate, quality mental health services (Office of Disease Prevention and Health Promotion, 2020). Monitoring activities led by the Agency for Healthcare Research and Quality (Mompe et al., 2015) to examine progress in health care for Latinos revealed that mental health care was worsening. For many measures of mental health care Latinos received worse quality of care than non-Hispanic Whites, showing no narrowing of disparities overtime. Alegría et al. (2016) sustain that a major factor that has contributed to the persistence of mental health care disparities is the mistaken assumption that evidence-based treatments are easily available for diverse populations. They highlight that the scant availability of linguistic and culturally competent services is a key barrier to mental health care access for minority populations. According to a 2015 report by the Migration Policy Institute about 25.1 million persons in the United States were identified as limited English proficient (LEP), defined as speaking English less than very well (Zong & Batalova, 2015). Spanish speakers comprised approximately 64% (16.2 million) of the US total LEP population. Both LEP Latinos and English proficient Latinos are more likely to be under-educated and poor in comparison to non-Hispanic Whites (Brach & Chevarley, 2008). Studies which have examined mental health treatment engagement, report lower initiation and retention rates for the poor, racial/ethnic minorities, and those who are LEP (Aguilera, Garza, & Muñoz, 2010; Alegría et al., 2008a,b; Arnow et al., 2007; Blanco et al., 2007; Caplan & Whittemore, 2013; Chavira et al., 2014; Miranda and Cooper, 2004; Santiago et al., 2013; Vega et al., 2007). To address disparities in mental health treatment engagement for this population, researchers underscore the need to take into consideration the role of personal, family, and society stigma as it affects the willingness to seek care, language barriers, self-reliant attitudes, economic considerations (i.e. work demands, transportation, child care, insurance), and the limited availability of suitable empirically supported treatments (Alegría et al., 2002a,b; Alegría et al., 2008a,b; Benuto, Gonzalez, Reinosa-Segovia, & Duckworth, 2019; Caplan & Whittemore, 2013; Cardemil et al., 2010; Nadeem et al., 2007; Pincay & Guarnaccia, 2007; Vega, Rodriguez, & Ang, 2010).
With the large population of Spanish-speaking US citizens in Puerto Rico and LEP Spanish speakers in the US, effective treatments for Spanish-speaking Latinos with GAD are needed if high quality mental health care is to be achieved. As a first step to address this challenge, this randomized trial pilot tested two CBT based interventions for GAD, traditional CBT and ABBT. Our findings provide preliminary, yet crucial data, which support the potential of the ABBT and CBT Spanish translated and culturally adapted manualized interventions for targeting GAD symptoms among low-income, Spanish-speaking Latinos. Both interventions for GAD yielded positive outcomes. However, similar to other studies among poor and ethnic minority populations, treatment initiation and retention rates among our participants were low (Aguilera et al., 2010; Blanco et al., 2007; Caplan & Whittemore, 2013; Santiago et al., 2013). These findings highlight the need to address the multiple individual, logistic, and systemic barriers to mental health care engagement faced by low-income Latinos. Thus, it is important that future research further explore treatment effects, as well as engagement strategies relevant for improving the quality and effectiveness of GAD treatment for low-income, Spanish-speaking Latinos.
Conclusion
This pilot RCT is the first to explore the potential benefits of two CBT based interventions for the treatment of Spanish-speaking Latino primary care patients with GAD. Study findings provide a preliminary evidence base that supports the promise of traditional CBT and newer ABBT to improve GAD outcomes. Future research should expand upon these findings to increase understanding of the best approaches to provide treatment to low-income Spanish-speaking Latinos with GAD.
Acknowledgements
We would like to thank Drs. Tom Borkovec, Lizabeth Roemer, and Susan Orsillo who provided training to therapists. Thanks also to all primary care patients that participated in our study.
Funding
This research was supported by the National Institute of Mental Health (NIMH; MH90599).
Footnotes
Disclosure of interest
The authors declare that they have no competing interest.
Ethical approval
The study protocol was approved by the University of Puerto Rico, Medical Sciences Campus Institutional Review Board.
References
- Aguilera A, Garza MJ, & Muñoz RF (2010). Group cognitive-behavioral therapy for depression in Spanish: Culture-sensitive manualized treatment in practice. Journal of clinical psychology, 66(8), 857–867. 10.1002/jclp.20706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Ríos R, Vera M, Calderón J, Rusch D, et al. (2002). Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatric services, 53(12), 1547–1555. 10.1176/appi.ps.53.12.1547 [DOI] [PubMed] [Google Scholar]
- Alegría M, Chatterji P, Wells K, Cao Z, Chen CN, Takeuchi D, et al. (2008). Disparity in depression treatment among racial and ethnic minority populations in the United States. Psychiatric Services, 59(11), 1264–1272. 10.1176/appi.ps.59.11.1264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Alvarez K, Ishikawa RZ, DiMarzio K, & McPeck S (2016). Removing obstacles to eliminating racial and ethnic disparities in behavioral health care. Health Affairs, 35(6), 991–999. 10.1377/hlthaff.2016.0029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Canino G, Ríos R, Vera M, Calderón J, Rusch D, et al. (2002). Inequalities in use of specialty mental health services among Latinos, African Americans, and non-Latino whites. Psychiatric Services, 53(12), 1547–1555. 10.1176/appi.ps.53.12.1547 [DOI] [PubMed] [Google Scholar]
- Alegría M, Canino G, Shrout PE, Woo M, Duan N, Vila D, et al. (2008). Prevalence of Mental Illness in Immigrant and Non-Immigrant US Latino Groups. American Journal of Psychiatry, 165(3), 359–369. 10.1176/appi.ajp.2007.07040704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegría M, Mulvaney-Day N, Torres M, Polo A, Cao Z, & Canino G (2007). Prevalence of psychiatric disorders across Latino subgroups in the United States. American Journal of Public Health, 97(1), 68–75. 10.2105/AJPH.2006.087205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen J, Balfour R, Bell R, & Marmot M (2014). Social determinants of mental health. Interna-tional Review of Psychiatry, 26(4), 392–407. 10.3109/09540261.2014.928270 [DOI] [PubMed] [Google Scholar]
- Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. (2004). Disability and quality of life impact of mental disorders in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandinavica, 109(s420), 38–46. 10.1111/j.1600-0047.2004.00329.x [DOI] [PubMed] [Google Scholar]
- Anakwenze U, & Zuberi D (2013). Mental health and poverty in the inner city. Health & Social Work, 38(3), 147–157 (http://www.ncbi.nlm.nih.gov/pubmed/24437020) [DOI] [PubMed] [Google Scholar]
- Antony MM, Cox BJ, Enns MW, Bieling PJ, & Swinson RP (1998). Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment, 10(2), 176–181. 10.1037/1040-3590.10.2.176 [DOI] [Google Scholar]
- Arnow BA, Blasey C, Manber R, Constantino MJ, Markowitz JC, Klein DN, et al. (2007). Dropouts versus completers among chronically depressed outpatients. Journal of Affective Disorders, 97(1‒3), 197–202. 10.1016/j.jad.2006.06.017 [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition Arlington, VA: American Psychiatric Association. [Google Scholar]
- Asnaani A, Richey JA, Dimaite R, Hinton DE, & Hofmann SG (2010). A cross-ethnic comparison of lifetime prevalence rates of anxiety disorders. The Journal of Nervous and Mental Disease, 198(8), 551–555. 10.1097/NMD.0b013e3181ea169f [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baader T, Molina JL, Venezian S, Rojas C, Farías R, Fierro-Freixenet C, et al. (2012). Validación y utilidad de laencuesta PHQ-9 (Patient Health Questionnaire) en el diagnós-tico de depresión en pacientes usuarios de atención primariaen Chile. Revista Chilena de Neuro-Psiquiatria, 50(1), 10–22. 10.4067/s0717-92272012000100002 [DOI] [Google Scholar]
- Bados A, Balaguer G, & Saldaña C (2007). The efficacy of cognitive-behavioral therapy and the problem of dropout. Journal of Clinical Psychology, 63(6), 585–592. 10.1002/jclp.20368 [DOI] [PubMed] [Google Scholar]
- Barrera TL, & Norton PJ (2009). Quality of life impairment in generalized anxiety disorder, social phobia, and panic disorder. Journal of Anxiety Disorders, 23(8), 1086–1090. 10.1016/j.janxdis.2009.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behar E, Alcaine O, Zuellig AR, & Borkovec TD (2003). Screening for generalized anxiety disorder using the Penn State Worry Questionnaire: A receiver operating characteristic analysis. Journal of Behavior Therapy and Experimental Psychiatry, 34(1), 25–43. 10.1016/S0005-7916(03)00004-1 [DOI] [PubMed] [Google Scholar]
- Bélanger L, Ladouceur R, & Morin CM (2005). Generalized anxiety disorder and health care use. Canadian family physician/Médecin de famille canadien, 51(10), 1362–1368 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1479795/pdf/jCFP_v051_pg1363.pdf. PMID: 16926971) [PMC free article] [PubMed] [Google Scholar]
- Benuto LT, Bennett NM, & Casas JB (2020). Minority participation in randomized controlled trials for prolonged exposure therapy: A systematic review of the literature. Journal of Traumatic Stress, 33(4), 420–431. 10.1002/jts.22539 [DOI] [PubMed] [Google Scholar]
- Benuto LT, Gonzalez F, Reinosa-Segovia F, & Duckworth M (2019). Mental health literacy, stigma, and behavioral health service use: The case of Latinx and Non-Latinx Whites. J Racial Ethn Health Disparities, 6(6), 1122–1130. 10.1007/s40615-019-00614-8 [DOI] [PubMed] [Google Scholar]
- Bereza BG, Machado M, & Einarson TR (2009). Systematic review and quality assessment of economic evaluations and quality-of-life studies related to generalized anxiety disorder. Clinical Therapeutics, 31(6), 1279–1308. 10.1016/j.clinthera.2009.06.004 [DOI] [PubMed] [Google Scholar]
- Blanco C, Patel S, Liu L, Jiang H, Lewis-Fernández R, Schmit A, et al. (2007). National trends in ethnic disparities in mental health care. Medical Care, 45(11), 1012–1019. 10.1097/MLR.0b013e3180ca95d3 [DOI] [PubMed] [Google Scholar]
- Bernal G, Jiménez-Chafey MI, & Domenech Rodríguez MM (2009). Cultural adaptation of treatments: A resource for considering culture in evidence-based practice. Professional Psychology: Research and Practice, 40(4), 361–368. 10.1037/a0016401 [DOI] [Google Scholar]
- Bolognesi F, Baldwin DS, & Ruini C (2014). Psychological interventions in the treatment of generalized anxiety disorder: A structured review. Journal of Psychopathology, 20, 111–126 (http://www.jpsychopathol.it/wp-content/uploads/2015/07/02-Bolognesi1.pdf) [Google Scholar]
- Borkovec TD, & Sharpless B (2004). Generalized anxiety disorder: Bringing cognitive behavioral therapy into the valued present. In Hayes S, Follette V, & Linehan M (Eds.), New directions in behavior therapy (pp. 209–242). New York: Guilford Press. [Google Scholar]
- Borkovec TD (1994). The nature, functions, and origins of worry. In Davey GCL, & Tallis F (Eds.), Wiley series in clinical psychology. Worrying: Perspectives on theory, assessment and treatment (pp. 5–33). New York: John Wiley & Sons; (https://psycnet.apa.org/record/1994-97842-001) [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, & Lytle R (2002). A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology, 70(2), 288–298 (http://www.ncbi.nlm.nih.gov/pubmed/11952187) [PubMed] [Google Scholar]
- Borkovec TD, & Ruscio AM (2001). Psychotherapy for generalized anxiety disorder. The Journal of Clinical Psychiatry, 62(Suppl. 1), 37–42 (discussion 43‒5. http://www.ncbi.nlm.nih.gov/pubmed/11414549) [PubMed] [Google Scholar]
- Borkovec TD, Alcaine OM, & Behar E (2004). Avoidance theory of worry and generalized anxiety disorder. In Heimberg RG, Turk CL, & Mennin DS (Eds.), Generalized anxiety disorder: Advances in research and practice pp. 77–108. New York, NY US: Guilford Press. https://psycnet.apa.org/record/2004-16375-004 [Google Scholar]
- Borkovec Thomas, D., Newman MG, & Castonguay LG (2003). Cognitive-behavioral therapy for generalized anxiety disorder with integrations from interpersonal and experiential therapies. CNS Spectrums, 8(05), 382–389. 10.1017/S1092852900018642 [DOI] [PubMed] [Google Scholar]
- Brach C, & Chevarley FM (2008). Demographics and health care access and utilization of limited-English-Proficient and English-Proficient Hispanics. Research Findings, 28 (Agency for Healthcare Research and Quality, Rockville, MD. http://meps.ahrq.gov/mepsweb/data_files/publications//rf28/rf28.pdf. Accessed April 8,2020). [Google Scholar]
- Bradley KA, McDonell MB, Bush K, Kivlahan DR, Diehr P, & Fihn SD (1998). The AUDIT Alcohol Consumption Questions. Alcoholism: Clinical & Experimental Research, 22(8), 1842. 10.1097/00000374-199811000-00034 [DOI] [PubMed] [Google Scholar]
- Brown TA, Antony MM, & Barlow D (1992). Psychometric properties of the Penn State Worry Questionnaire in a clinical anxiety disorders sample. Behaviour research and therapy, 30(1), 33–37. 10.1016/0005-7967(92)90093-V [DOI] [PubMed] [Google Scholar]
- Butler AC, Chapman JE, Forman EM, & Beck AT (2006). The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review, 26(1), 17–31. 10.1016/J.CPR.2005.07.003 [DOI] [PubMed] [Google Scholar]
- Cabassa LJ, Zayas LH, & Hansen MC (2006). Latino Adults’ access to mental health care: A review of epidemiological studies. Administration and policy in mental health, 33(3), 316–330. 10.1038/jid.2014.371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caplan S, & Whittemore R (2013). Barriers to treatment engagement for depression among Latinas. Issues in mental health nursing, 34(6), 412–424. 10.3109/01612840.2012.762958 [DOI] [PubMed] [Google Scholar]
- Cardemil EV, Kim S, Davidson T, Sarmiento IA, Ishikawa RZ, Sanchez M, et al. (2010). Developing a culturally appropriate depression prevention program: Opportunities and challenges. Cognitive and Behavioral Practice, 17(2), 188–197. 10.1016/j.cbpra.2010.01.005 [DOI] [Google Scholar]
- Canino G, Vila D, Santiago-Batista K, Garcia P, Velez-Baez G, & Moreda-Alegria A (2016). Need assessment study of mental health and substance use disorders and service utilization among adult population of Puerto Rico. Final report (Accessed March 16, 2020). http://www.assmca.pr.gov/BibliotecaVirtual/Estudios/Need%20Assessment%20Study%20of%20Mental%20Health%20and%20Substance%20of%20Puerto%20Rico%202016.pdf
- Chapa T (2004). Mental health services in primary care settings for racial and ethnic minority populations (Accessed March 16, 2020). https://minorityhealth.hhs.gov/Assets/pdf/Checked/1/Mental_Health_Services_in_Primary_Care_Settings_for_Racial2004.pdf
- Chavira DA, Golinelli D, Sherbourne C, Stein MB, Sullivan G, Bystritsky A, et al. (2014). Treatment engagement and response to CBT among Latinos with anxiety disorders in primary care. Journal of consulting and clinical psychology, 82(3), 392–403. 10.1037/a0036365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covin R, Ouimet AJ, Seeds PM, & Dozois DJA (2008). A meta-analysis of CBT for pathological worry among clients with GAD. Journal of Anxiety Disorders, 22(1), 108–116. 10.1016/j.janxdis.2007.01.002 [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Sijbrandij M, Koole S, Huibers M, Berking M, & Andersson G (2014). Psychological treatment of generalized anxiety disorder: A meta-analysis. Clinical Psychology Review, 34(2), 130–140. 10.1016/j.cpr.2014.01.002 [DOI] [PubMed] [Google Scholar]
- Culpepper L (2009). Generalized anxiety disorder and medical illness. The Journal of Clinical Psychiatry, 70(Suppl. 2), 20–24 (http://www.ncbi.nlm.nih.gov/pubmed/19371503) [DOI] [PubMed] [Google Scholar]
- Davidson JRT, Feltner DE, & Dugar A (2010). Management of generalized anxiety disorder in primary care. The Primary Care Companion to The Journal of Clinical Psychiatry, 12(2), 109–115. 10.4088/PCC.09r00772blu [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daza P, Novy DM, Stanley MA, & Averill P (2002). The depression anxiety stress scale-21: Spanish translation and validation with a Hispanic sample. Journal of Psychopathology and Behavioral Assessment, 24(3), 195–205. 10.1023/A:1016014818163 [DOI] [Google Scholar]
- Deacon B, Lickel J, & Abramowitz JS (2008). Medical utilization across the anxiety disorders. Journal of Anxiety Disorders, 22(2), 344–350. 10.1016/J.JANXDIS.2007.03.004 [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services. (2011). HHS action plan to reduce racial and ethnic health disparities (Accessed February 18, 2020). https://www.minorityhealth.hhs.gov/npa/files/Plans/HHS/HHS_Plan_complete.pdf
- Diez-Quevedo C, Rangil T, Sanchez-Planell L, Kroenke K, & Spitzer RL (2001). Validation and utility of the patient health questionnaire in diagnosing mental disorders in 1003 general hospital Spanish inpatients. Psychosomatic medicine, 63(4), 679–686. 10.1097/00006842-200107000-00021 [DOI] [PubMed] [Google Scholar]
- Fresco DM, Heimberg RG, Mennin DS, & Turk CL (2002). Confirmatory factor analysis of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 40(3), 313–323. 10.1016/s0005-7967(00)00113-3 [DOI] [PubMed] [Google Scholar]
- Goodwin H, Yiend J, & Hirsch CR (2017). Generalized Anxiety Disorder, worry and attention to threat: A systematic review. Clinical Psychology Review, 54, 107–122. 10.1016/j.cpr.2017.03.006 [DOI] [PubMed] [Google Scholar]
- Gould RA, Safren SA, Washington DO, & Otto MW (2004). A meta-analytic review of cognitive-behavioral treatments. In Heimberg RG, Turk CL, & Mennin DS (Eds.), Generalized anxiety disorder: Advances in research and practice New York, NY, USA: Guifors Publications, Inc; (https://psycnet.apa.org/record/2004-16375-010) [Google Scholar]
- Hayes-Skelton SA, Roemer L, & Orsillo SM (2013). A randomized clinical trial comparing an acceptance-based behavior therapy to applied relaxation for generalized anxiety disorder. Journal of Consulting and Clinical Psychology, 81(5), 761–773. 10.1037/a0032871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heuzenroeder L, Donnelly M, Haby MM, Mihalopoulos C, Rossell R, Carter R, et al. (2004). Cost-effectiveness of psychological and pharmacological interventions for generalized anxiety disorder and panic disorder. Australian & New Zealand Journal of Psychiatry, 38(8), 602–612. 10.1080/j.1440-1614.2004.01423.x [DOI] [PubMed] [Google Scholar]
- Hoffman DL, Dukes EM, & Wittchen H-U (2008). Human and economic burden of generalized anxiety disorder. Depression and Anxiety, 25(1), 72–90. 10.1002/da.20257 [DOI] [PubMed] [Google Scholar]
- Hogan MF (2003). President’s new freedom commission on mental health. Psychiatric Services, 54(11), 1467–1474. 10.1176/appi.ps.54.11.1467 [DOI] [PubMed] [Google Scholar]
- Hunot V, Churchill R, Teixeira V, & Silva de Lima M (2007). Psychological therapies for generalised anxiety disorder. Cochrane Database of Systematic Reviews, 1 10.1002/14651858.CD001848.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2003). Unequal treatment: Confronting racial and ethnic disparities in health care Washington, DC: The National Academies Press; ( 10.17226/12875) [DOI] [PubMed] [Google Scholar]
- Jacobson NS, & Traux P (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of consulting and clinical psychology, 59(1), 12–19. 10.1037//0022-006x.59.1.12 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Keller MB, & Wittchen HU (2001). The epidemiology of generalized anxiety disorder. The Psychiatric Clinics of North America, 24(1), 19–39 (http://www.ncbi.nlm.nih.gov/pubmed/11225507) [DOI] [PubMed] [Google Scholar]
- Kessler Ronald, C., Aguilar-Gaxiola S, Alonso J, Chatterji S, Lee S, et al. (2009). The global burden of mental disorders: An update from the WHO World Mental Health (WMH) surveys. Epidemiologia e Psichiatria Sociale, 18(1), 23–33 (http://www.ncbi.nlm.nih.gov/pubmed/19378696) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozhimannil KB, Trinacty CM, Busch AB, Huskamp HA, & Adams AS (2011). Racial and ethnic disparities in postpartum depression care among low-income women. Psychiatric Services, 62(6), 619–625. 10.1176/ps.62.6.pss6206_0619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, Monahan PO, & Löwe B (2007). Anxiety disorders in primary care: Prevalence, impairment, comorbidity, and detection. Annals of Internal Medicine, 146(5), 317–325 (http://www.ncbi.nlm.nih.gov/pubmed/17339617) [DOI] [PubMed] [Google Scholar]
- Lagomasino IT, Dwight-Johnson M, Miranda J, Zhang L, Liao D, Duan N, et al. (2005). Disparities in depression treatment for Latinos and site of care. Psychiatric Services, 56(12), 1517–1523. 10.1176/appi.ps.56.12.1517 [DOI] [PubMed] [Google Scholar]
- Lau AS, Chang DF, & Okazaki S (2010). Methodological challenges in treatment outcome research with ethnic minorities. Cultural diversity & ethnic minority psychology, 16(4), 573–580. 10.1037/a0021371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Tian Y, Liu Y, Nigatu YT, & Wang J (2019). Relationship between major depressive disorder, generalized anxiety disorder and coronary artery disease in the US general population. Journal of psychosomatic research, 119, 8–13. 10.1016/j.jpsychores.2019.01.007 [DOI] [PubMed] [Google Scholar]
- Lovibond SH, & Lovibond PF (1995). Manual for the Depression Anxiety & Stress Scales (2nd ed.). Sydney, NSW: Psychology Foundation of Australia. [Google Scholar]
- McGuire TG, & Miranda J (2008). Racial and ethnic disparities in mental health care: Evidence and policy implications. Health affairs (Project Hope), 27(2), 393–403. 10.1377/hlthaff.27.2.393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendlowicz MV, & Stein MB (2000). Quality of life in individuals with anxiety disorders. American Journal of Psychiatry, 157(5), 669–682. 10.1176/appi.ajp.157.5.669 [DOI] [PubMed] [Google Scholar]
- Mendoza DB, Williams MT, Chapman LK, & Powers M (2012). Minority inclusion in randomized clinical trials of panic disorder. Journal of Anxiety Disorders, 26(5), 574–582. 10.1016/j.janxdis.2012.02.011 [DOI] [PubMed] [Google Scholar]
- Meng X-L, Alegria M, Chen C-N, & Liu J (2004). A nonlinear hierarchical model for estimating prevalence rates with small samples, http://stat.columbia.edu/∼jcliu/paper/prevalence.jsm.meng.final.pdf.
- Meyer TJ, Miller ML, Metzger RL, & Borkovec TD (1990). Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 28(6), 487–495. 10.1016/0005-7967(90)90135-6 [DOI] [PubMed] [Google Scholar]
- Miranda J, & Cooper LA (2004). Disparities in care for depression among primary care patients. Journal of General Internal Medicine, 19(2), 120–126. 10.1111/j.1525-1497.2004.30272.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitte K (2005). Meta-analysis of cognitive-behavioral treatments for generalized anxiety disorder: A comparison with pharmacotherapy. Psychological Bulletin, 131(5), 785–795. 10.1037/0033-2909.131.5.785 [DOI] [PubMed] [Google Scholar]
- Mompe A, Alemu G, Barton B, Breen N, Bryce S, Mueller C, et al. (2015). 2014 National Healthcare Quality and Disparities Report Chartbook on Rural Health Care (Accessed April 12, 2020). http://www.ahrq.gov/research/findings/nhqrdr/index.html
- Nadeem E, Lange HM, Edge D, Fongwa M, Berlin T, & Miranda J (2007). Does stigma keep poor young immigrant and US-born Black and Latina women from seeking mental health care? Psychiatric Services, 58(12), 1547–1554. 10.1176/appi.ps.58.12.1547 [DOI] [PubMed] [Google Scholar]
- Newman MG, Llera SJ, Erickson TM, Przeworski A, & Castonguay LG (2013). Worry and generalized anxiety disorder: A review and theoretical synthesis of evidence on nature, etiology, mechanisms, and treatment. Annual Review of Clinical Psychology, 9, 275–297. 10.1146/annurev-clinpsy-050212-185544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Zuellig AR, Kachin KE, Constantino MJ, Przeworski A, Erickson T, et al. (2002). Preliminary reliability and validity of the generalized anxiety disorder questionnaire-IV: A revised self-report diagnostic measure of generalized anxiety disorder. Behavior Therapy, 33(2), 215–233. 10.1016/S0005-7894(02)80026-0 [DOI] [Google Scholar]
- Nuevo-Benítez R, Montorio-Cerrato I, & Ruiz-Díaz MÁ (2002). Application of the Penn State Worry Questionnaire (PSWQ) to elderly population. Ansiedad Estrés, 8(2), 157–172 (https://www.actaspsiquiatria.es/repositorio/20/114/ESP/20-114-ESP-117-24-885536.pdf) [Google Scholar]
- O’connor M, Munnelly A, Whelan R, & Mchugh L (2018). The efficacy and acceptability of third-wave behavioral and cognitive eHealth treatments: A systematic review and meta-analysis of randomized controlled trials. Behavior Therapy, 49(3), 459–475. 10.1016/j.beth.2017.07.007 [DOI] [PubMed] [Google Scholar]
- Office of Disease Prevention and Health Promotion. (2020). Mental Health and Mental Disorders. Healthy People 2020 US Department of Health and Human Services; (https://www.healthypeople.gov/2020/topics-objectives/topic/mental-health-and-mental-disorders. Accessed March 17, 2020) [Google Scholar]
- Orsillo SM, & Roemer L (2011). The mindful way through anxiety: Break free from chronic worry and reclaim your life New York, NY: The Guilford Press. [Google Scholar]
- Orsillo SM, & Roemer L (2005). Acceptance and mindfulness-based approaches to anxiety: Conceptualization and treatment New York: Springer Science + Business Media, LCC. [Google Scholar]
- Otte C (2011). Cognitive behavioral therapy in anxiety disorders: Current state of the evidence. Dialogues in Clinical Neuroscience, 13(4), 413–421 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3263389/pdf/DialoguesClinNeurosci-13-413.pdf) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pincay IE, & Guarnaccia PJ (2007). ‘‘It’s like going through an earthquake’’: Anthropological perspectives on depression among Latino immigrants. Journal of immigrant and minority health/Center for Minority Public Health, 9(1), 17–28. 10.1007/s10903-006-9011-0 [DOI] [PubMed] [Google Scholar]
- Revicki DA, Travers K, Wyrwich KW, Svedsäter H, Locklear J, Mattera MS, et al. (2012). Humanistic and economic burden of generalized anxiety disorder in North America and Europe. Journal of Affective Disorders, 140(2), 103–112. 10.1016/j.jad.2011.11.014 [DOI] [PubMed] [Google Scholar]
- Rodríguez-Biglieri RVG (2011). Psychometric characteristics of the Penn State Worry Questionnaire in an Argentinean sample: A cross-cultural contribution. The Spanish journal of psychology, 14(1), 452–463. 10.5209/rev_sjop.2011.v14.n1.41 [DOI] [PubMed] [Google Scholar]
- Roemer L, & Orsillo S (2009). Mindfulness and acceptance-based behavioral therapies in practice New York, NY: The Guiford Press. [Google Scholar]
- Roemer L, Orsillo SM, & Salters-Pedneault K (2008). Efficacy of an acceptance-based behavior therapy for generalized anxiety disorder: Evaluation in a randomized controlled trial. Journal of Consulting and Clinical Psychology, 76(6), 1083–1089. 10.1037/a0012720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Williston SK, Eustis EH, & Orsillo SM (2013). Mindfulness and acceptance-based behavioral therapies for anxiety disorders. Current Psychiatry Reports, 15(11), 410. 10.1007/s11920-013-0410-3 [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. (2013). Version 9.4 Cary, NC: SAS Institute Inc. [Google Scholar]
- Santiago CD, Kaltman S, & Miranda J (2013). Poverty and mental health: How do low-income adults and children fare in psychotherapy? Journal of clinical psychology, 69(2), 115–126. 10.1002/jclp.21951 [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, & Williams JBW (1999). Validation and utility of a self-report version of PRIME-MD. JAMA, 282(18), 1737–1744 (https://jamanetwork.com/journals/jama/fullarticle/192080) [DOI] [PubMed] [Google Scholar]
- Stein MB, Roy-Byrne PP, Craske MG, Bystritsky A, Sullivan G, Pyne JM, et al. (2005). Functional impact and health utility of anxiety disorders in primary care outpatients. Medical Care, 43(12), 1164–1170 (http://www.ncbi.nlm.nih.gov/pubmed/16299426) [DOI] [PubMed] [Google Scholar]
- Treanor M, Erisman SM, Salters-Pedneault K, Roemer L, & Orsillo SM (2011). Acceptance-based behavioral therapy for GAD: Effects on outcomes from three theoretical models. Depression and Anxiety, 28(2), 127–136. 10.1002/da.20766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services. (2001a). NIH policy and guidelines on the inclusion of women and minorities as subjects in clinical research (Accessed November 18, 2020). https://grants.nih.gov/policy/inclusion/women-and-minorities/guidelines.html
- US Department of Health and Human Services. (2001b). Mental health: Culture, race, and ethnicity—A supplement to mental health: A report of the surgeon general Rockville, MD: US Department of Health and Human Services Administration, Center for Mental Health Services; (https://www.ncbi.nlm.nih.gov/books/NBK44243/. Accessed April 21, 2020) [PubMed] [Google Scholar]
- Vega W, Karno M, Alegria M, Alvidrez J, Bernal G, Escamilla M, et al. (2007). Research issues for improving treatment of US Hispanics with persistent mental disorders. Psychiatric services, 58(3), 385–394. 10.1176/ps.2007.58.3.385 [DOI] [PubMed] [Google Scholar]
- Vega WA, Rodriguez MA, & Ang A (2010). Addressing stigma of depression in Latino primary care patients. General hospital psychiatry, 32(2), 182–191. 10.1016/j.genhosppsych.2009.10.008 (Epub 2009 Dec 5) [DOI] [PubMed] [Google Scholar]
- Williams M, Powers M, Yun YG, & Foa E (2010). Minority participation in randomized controlled trials for obsessive‒compulsive disorder. Journal of Anxiety Disorders, 24(2), 171–177. 10.1016/j.janxdis.2009.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LS, Brizendine EJ, Plue L, Bakas T, Tu W, Hendrie H, et al. (2005). Performance of the PHQ-9 as a screening tool for depression after stroke. Stroke, 36(3), 635–638. 10.1161/01.STR.0000155688.18207.33 [DOI] [PubMed] [Google Scholar]
- Wittchen H-U, Kessler RC, Beesdo K, Krause P, Hofler M, & Hoyer J (2002). Generalized anxiety and depression in primary care: Prevalence, recognition, and management. Journal of Clinical Psychiatry, 63(8), 24–34 (https://www.psychiatrist.com/jcp/article/Pages/2002/v63s08/v63s0805.aspx) [PubMed] [Google Scholar]
- Zong J, & Batalova J (2015). The limited English proficient population in the United States (Accessed April 7, 2020). https://www.migrationpolicy.org/article/limited-english-proficient-population-united-states


