Abstract
Recent molecular characterizations of Cryptosporidium parasites make it possible to differentiate the human-pathogenic Cryptosporidium parasites from those that do not infect humans and to track the source of Cryptosporidium oocyst contamination in the environment. In this study, we used a small-subunit rRNA-based PCR-restriction fragment length polymorphism (RFLP) technique to detect and characterize Cryptosporidium oocysts in 55 samples of raw surface water collected from several areas in the United States and 49 samples of raw wastewater collected from Milwaukee, Wis. Cryptosporidium parasites were detected in 25 surface water samples and 12 raw wastewater samples. C. parvum human and bovine genotypes were the dominant Cryptosporidium parasites in the surface water samples from sites where there was potential contamination by humans and cattle, whereas C. andersoni was the most common parasite in wastewater. There may be geographic differences in the distribution of Cryptosporidium genotypes in surface water. The PCR-RFLP technique can be a useful alternative method for detection and differentiation of Cryptosporidium parasites in water.
Consumption of contaminated water has been implicated as a major source of Cryptosporidium infection in various outbreak investigations and case control studies (22, 24). Surveys conducted in several regions of the United States revealed the presence of Cryptosporidium oocysts in 67 to 100% of wastewaters, 24 to 100% of surface waters, and 17 to 26.8% of drinking waters (11–13, 24). The identity and human-infective potential of these waterborne oocysts are not known, although it is likely that not all oocysts are from human-infecting Cryptosporidium species. Likewise, the source of oocyst contamination is not clear. Farm animal and human sewage discharges are generally considered the major sources of surface water contamination with C. parvum (15). Because Cryptosporidium infection is common in wildlife, it is conceivable that wildlife can also be a source of Cryptosporidium oocysts in water (24).
Currently, Cryptosporidium oocysts in environmental samples are identified largely by an immunofluorescent assay after concentration by methods such as the ICR method or method 1622/1623. Because the immunofluorescent assay detects oocysts of most Cryptosporidium spp., the species distribution of Cryptosporidium parasites in environmental samples cannot be assessed. Although many surface water samples contain Cryptosporidium oocysts, it is unlikely that all of these oocysts are from human-pathogenic species or genotypes, because only five genotypes of Cryptosporidium parasites (the C. parvum human, bovine, and dog genotypes, C. meleagridis, and C. felis) have been explicitly found in humans so far (17, 18, 32). Information on the source of C. parvum contamination is necessary for effective evaluation and selection of management practices to reduce Cryptosporidium contamination of surface water and the risk of cryptosporidiosis. Thus, identification of oocysts to species and strain levels is of public health importance.
The existence of host-adapted Cryptosporidium spp. and C. parvum genotypes makes it possible to develop species differentiation and genotyping tools to determine whether the Cryptosporidium oocysts found in water are from human-infective species and to track the source of Cryptosporidium oocyst contamination in water (16, 32). One such tool, the small-subunit (SSU) rRNA-based nested PCR-restriction fragment length polymorphism (RFLP) method, has been successfully used by us to differentiate Cryptosporidium species and C. parvum genotypes in clinical samples and storm water (29–31). In this study, we evaluated the use of this technique for detection and characterization of Cryptosporidium oocysts in samples of raw surface water and wastewater.
MATERIALS AND METHODS
Water samples and sample processing.
Samples of raw surface water and wastewater were used in this study. Most of the surface water samples were collected from the Milwaukee region of Lake Michigan, from rivers in Illinois, and from the Maryland portion of the Chesapeake Bay area. A few samples, however, were collected from rivers in Iowa, Missouri, and Texas (see Table 1). These samples were collected during 1999 and the first half of 2000. Samples from the Chesapeake Bay area were collected from sites located near wastewater discharges (samples from Choptank River, Severn River, and Miles River) or beef cattle farms (samples from Wye River, St. George's Creek, and Wicomico River), which were adjacent to the river. The allowable amount of waste discharge was 3.6 million gallons per day (MGD) at the Choptank River discharge site, 7.5 MGD at the Severn River discharge site, and 0.3 MGD at the Miles River discharge site. One sample from each of the sites was taken during the spring (May), summer (August), and fall (October) of 1999 to avoid seasonal fluctuations in oocyst contamination. Water samples were always taken downstream (less than 1 mile) of cattle operations or wastewater discharges. Almost all surface water samples were collected during base flow. All wastewater samples were collected from a wastewater treatment plant in Milwaukee, Wis., during the period from April to July 2000.
TABLE 1.
Cryptosporidium genotypes in samples of surface water from various locations
| Sample location | Vol filtered (liters) | Total no. of samples | No. of positive samples | Species and/or genotypes(s)a |
|---|---|---|---|---|
| Lake Michigan, Linnwood, Wis. | 50.3–60 | 8 | 0 | |
| Lake Michigan, San Benito, Wis. | 10 | 2 | 0 | |
| Lake Michigan, Howard, Wis. | 50.0–63.1 | 3 | 0 | |
| Aurora, Ill. | 10 | 7 | 2 | C. parvum human genotype and C. baileyi (1), C. andersoni (1) |
| Decatur, Ill. | 10 | 2 | 0 | |
| Iowa City, Iowa | 20.8–24.2 | 2 | 1 | C. andersoni (1) |
| Kansas City, Mo. | 4.6–10.0 | 3 | 1 | C. andersoni (1) |
| St. Louis, Mo. | 10 | 1 | 1 | C. andersoni (1) |
| San Benito, Tex. | 3.0–10.0 | 5 | 0 | |
| Potomac River, Washington, D.C. | 10 | 1 | 1 | C. andersoni (1) |
| Chesapeake Bay, Choptank River, Cambridge, Md. | 50 | 3 | 2 | C. parvum human and bovine genotypes (2) |
| Chesapeake Bay, Severn River, Annapolis, Md. | 50 | 3 | 3 | C. parvum human and bovine genotypes (3) |
| Chesapeake Bay, mouth of Severn River, Annapolis South, Md. | 50 | 3 | 3 | C. parvum human and bovine genotypes (3) |
| Chesapeake Bay, Miles River, St. Michael's, Md. | 50 | 3 | 3 | C. parvum bovine genotype (2), C. parvum human and bovine genotypes (1) |
| Chesapeake Bay, Wye River, Pintail Point, Md. | 50 | 3 | 3 | C. parvum bovine genotype (3) |
| Chesapeake Bay, St. George's Creek, Lunderburg, Md. | 50 | 3 | 3 | C. parvum bovine genotype (3) |
| Chesapeake Bay, Wicomico River, Mt. Vernon, Md. | 50 | 3 | 2 | C. parvum bovine genotype (2) |
Numbers in parentheses are numbers of samples positive for each genotype or species.
Surface water samples were taken by filtering water through an Envirocheck filter (Pall Gelman Laboratory, Ann Arbor, Mich.) or a membrane disk (diameter, 393 mm; pore size, 3 μm; Millipore Corp., Bedford, Mass.) using previously described procedures (4, 7) and method 1623 procedures recommended by the U.S. Environmental Protection Agency (27). Membrane disks were used for river water samples from the Chesapeake Bay area, whereas Envirocheck filters were used for the rest of the surface water samples. In most cases the amount of water filtered was 50 liters when membrane disks were used and 10 liters or less when Envirocheck filters were used; the exceptions were samples from Lake Michigan, which were taken by filtering 50 to 60 liters of water (except for two samples) through Envirocheck filters. Wastewater was concentrated by centrifuging 10- or 50-ml portions of grab samples of raw wastewater at 1,000 × g for 10 min. Cryptosporidium oocysts in surface water and wastewater were further concentrated and purified by immunomagnetic separation (IMS) by using magnetic beads coated with an anticryptosporidial monoclonal antibody (Dynal, Inc., Lake Success, N.Y.) and the manufacturer's recommended procedures. Usually, only an aliquot of each surface water sample was processed by IMS because of the presence of excessive sediment.
DNA extraction.
IMS concentrates from surface water and wastewater were used for DNA extraction. They were subjected to five freeze-thaw cycles, incubated with 1 mg of proteinase K (Sigma, St. Louis, Mo.) per ml at 56°C for at least 1 h, and diluted with an equal volume of pure ethanol. Oocyst DNA was extracted by passing the oocyst-ethanol suspension through QIAamp DNA Mini isolate columns (Qiagen, Valencia, Calif.). DNA was stored at −20°C before it was used for PCR analysis.
PCR-RFLP analysis.
Cryptosporidium oocysts in water samples were identified to the species and genotype levels by a previously described PCR-RFLP technique (29, 30), except that a 3-bp correction was made in the sequence of the reverse primer for primary PCR. Each sample was analyzed at least three times by the PCR-RFLP method by using different volumes of the DNA preparation (0.25, 0.5, and 1 μl) for PCR. Briefly, an approximately 1,325-bp PCR product was amplified first in a primary PCR by using primers 5′-TTCTAGAGCTAATACATGCG-3′ and 5′-CCCATTTCCTTCGAAACAGGA-3′. A total of 35 cycles were carried out; each of these consisted of 94°C for 45 s, 55°C for 45 s, and 72°C for 1 min. There was also an initial hot start at 94°C for 3 min and a final extension at 72°C for 7 min. A secondary 826- to 864-bp PCR product (depending on the isolate) was then amplified from 2 μl of the primary PCR mixture by using primers 5′-GGAAGGGTTGTATTTATTAGATAAAG-3′ and 5′-AAGGAGTAAGGAACAACCTCCA-3′. The cycling conditions were identical to those used for the primary PCR.
To differentiate Cryptosporidium spp. and C. parvum genotypes, 20 μl of each secondary PCR product was digested in a 50-μl (total volume) reaction mixture containing 20 U of SspI (New England BioLabs, Beverly, Mass.) 20 U of VspI (GIBCO BRL, Grand Island, N.Y.) and 5 μl of the appropriate restriction buffer at 37°C for 1 h, as described previously (29, 30). Because C. andersoni and C. muris had identical SspI and VspI restriction patterns, they were differentiated by digesting secondary PCR products with 20 U of DdeI (New England BioLabs) at 37°C for 1 h under conditions recommended by the supplier. Digested products were fractionated on a 2.0% agarose gel and visualized by ethidium bromide staining. Cryptosporidium spp. and C. parvum genotypes were differentiated by their band patterns. All diagnoses were confirmed by RFLP analysis of additional, independent PCR products from the same sample. The accuracy of the RFLP analysis technique was also examined by performing a sequencing analysis of the secondary PCR products with an ABI377 autosequencer (Perkin-Elmer, Foster City, Calif.).
RESULTS
A total of 55 surface water samples and 49 wastewater samples were used in this study. Examination of IMS concentrates by PCR analysis indicated that 25 of the surface water samples and 12 of the wastewater samples were positive for Cryptosporidium. When the surface water samples were examined, none of the 13 samples from Lake Michigan contained Cryptosporidium, but 19 of 21 samples from rivers in the Chesapeake Bay area were positive for Cryptosporidium (Tables 1 and 2).
TABLE 2.
Cryptosporidium genotypes in samples of raw wastewater from a wastewater treatment plant in Milwaukee
| Month | Sample vol (ml) | Total no. of samples | No. of positive samples | Species and/or genotypea |
|---|---|---|---|---|
| April | 10 | 13 | 2 | C. andersoni and C. muris (1), C. andersoni and C. parvum bovine genotype (1) |
| May | 10 | 15 | 2 | C. andersoni (1), C. muris (1) |
| June | 10 | 12 | 6 | C. andersoni (3), C. parvum dog genotype (1), C. felis (1), C. parvum human genotype and C. andersoni (1) |
| July | 50 | 9 | 2 | C. andersoni (1), unknown genotype (1) |
Numbers in parentheses are numbers of samples positive for each genotype or species.
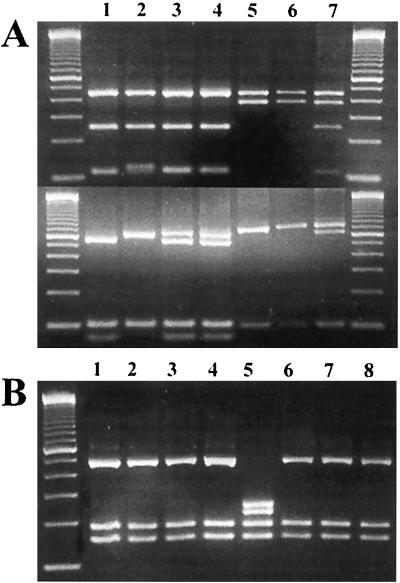
Restriction analysis of secondary PCR products with SspI and VspI revealed the presence of C. parvum human and bovine genotypes, C. baileyi, and C. andersoni-C. muris in surface water samples and C. parvum human, bovine, and dog genotypes, C. felis, C. andersoni-C. muris, and an unknown Cryptosporidium genotype in wastewater samples (Fig. 1A). C. andersoni and C. muris were differentiated from each other by DdeI digestion of the secondary PCR products. The PCR products of C. andersoni yielded bands at 20, 156, 186, and 470 bp, and three bands were visible on an agarose gel. In contrast, the PCR products of C. muris yielded bands at 20, 156, 186, 224, and 247 bp, and four bands were visible (Fig. 1B). Sequence analysis of all of the PCR products yielded DNA sequences identical to those which we previously obtained from humans or animals infected with C. parvum human, bovine, and dog genotypes, C. felis, C. andersoni, C. muris, and C. baileyi (data not shown). The unknown Cryptosporidium genotype was identical to a Cryptosporidium wildlife genotype (W3) which we previously identified in storm water (31).
FIG. 1.
Genotyping of Cryptosporidium oocysts in water with a SSU rRNA-based PCR-RFLP technique. (A) Differentiation of Cryptosporidium spp. and C. parvum genotypes by digestion of the secondary PCR products with SspI (upper panel) and VspI (lower panel). Lane 1, C. parvum human genotype (sample 574); lane 2, C. parvum bovine genotype (sample 5F); lanes 3 and 4, C. parvum human and bovine genotypes (samples 1F and 2F); lane 5, C. andersoni (sample 104); lane 6, C. muris (sample 194); lane 7, C. parvum bovine genotype and C. andersoni (sample 163). (B) Differentiation of C. andersoni from C. muris by digestion of the secondary PCR products with DdeI. Lanes 1 through 4 and 6 through 8, C. andersoni (samples 104, 99, 98, 641, 192, 224, and 225); lane 5, C. muris (sample 194).
C. parvum, (both human and bovine genotypes) was the predominant Cryptosporidium sp. found in surface water; 10 samples contained the C. parvum human genotype, and 19 samples contained the C. parvum bovine genotype. C. andersoni was also detected at a moderate frequency (five samples) in surface water samples. With the exception of one sample, the C. parvum human genotype was found only in surface water samples from the Chesapeake Bay area, along with the C. parvum bovine genotype (Table 1). In contrast, C. andersoni was the major Cryptosporidium sp. found in wastewater, occurring in eight samples (Table 2). Many surface water and wastewater samples contained more than one Cryptosporidium genotype; this was especially true of surface water samples from rivers in the Chesapeake Bay area (Tables 1 and 2).
DISCUSSION
Numerous attempts have been made to apply PCR techniques to detection of Cryptosporidium oocysts in water samples (1–3, 6, 10, 14, 19–21, 23, 25, 26, 28). In most of these studies the workers used water seeded with Cryptosporidium oocysts, and various degrees of success were reported. One major obstacle is the presence of PCR inhibitors in water, which are coextracted with DNA and inhibit PCR amplification of the target DNA. This has greatly reduced the sensitivity of PCR detection of oocysts in various water samples. The PCR inhibitors can be removed by IMS (8, 9). This practice led to successful detection of Cryptosporidium oocysts in water samples from the 1993 outbreak in Milwaukee, Wis., by a Cryptosporidium genus-specific PCR technique (9) and to genotyping of C. parvum parasites in surface and filter backwash water samples by an integrated cell culture-PCR technique (3). Results of the present study indicate that in conjunction with IMS, the SSU rRNA-based PCR-RFLP technique which we previously developed for differentiating Cryptosporidium spp. and C. parvum genotypes in clinical samples has the specificity and sensitivity needed for analysis of Cryptosporidium oocysts in water samples.
Eight Cryptosporidium parasites that commonly occur in humans, farm animals, pets, or wildlife were found in surface water and wastewater samples used in this study. The high frequency of detection of the C. parvum human and bovine genotypes and C. andersoni (a gastric Cryptosporidium parasite of juvenile and adult cattle) is congruent with the previous theory that humans and farm animals are two major sources of Cryptosporidium oocyst contamination in surface water at locations where this type of contamination potentially occurs (15, 22). This is in contrast with Cryptosporidium parasites in storm runoff water from a feral area, in which there is a high frequency of Cryptosporidium genotypes from wildlife (31). There may be geographic differences in Cryptosporidium oocyst contamination of surface water, because the Cryptosporidium oocyst detection rate for river water samples from the Chesapeake Bay area was much higher than those for samples from other areas, and no Cryptosporidium oocysts were detected in water from Lake Michigan. This was expected, because the sampling sites in the Chesapeake Bay area were located near potential sources of contamination of water with Cryptosporidium oocysts (i.e., wastewater discharges and runoff from large commercial cattle farms) (5). Three of six rivers examined in this region frequently contained C. parvum human genotype oocysts, a finding congruent with these sampling sites' locations near wastewater discharges.
Although Cryptosporidium was not detected in surface water from the Milwaukee portion of Lake Michigan and only 10 to 50 ml of wastewater was examined for each sample, Cryptosporidium oocysts were detected in raw wastewater from Milwaukee at a moderate frequency. The high rate of detection of C. andersoni in wastewater was probably the result of effluents from cattle slaughterhouses in the city. This hypothesis is supported by the fact that mature cattle are more likely to be infected with C. andersoni than with the C. parvum bovine genotype, which was detected in wastewater at a much lower frequency. The biggest slaughterhouse in the city processes 1,800 beef cattle daily and drains its contents into the city sewage system after satisfying city specifications (amount of fat, size of meat chunks, etc.). The slaughterhouse is less than 5 miles upstream of the Jones Island wastewater treatment plant, where we collected composite samples.
Likewise, the C. muris oocysts in wastewater were probably from rodents, which are expected to be present in a wastewater distribution system in abundance. Urban runoff may also have been a contributing factor in Cryptosporidium oocysts in wastewater, because the C. parvum dog genotype, C. felis, and an unknown Cryptosporidium genotype from wildlife were also detected in wastewater at low frequencies. The low rate of detection of the C. parvum human genotype in wastewater from a major metropolitan area is surprising, because it is likely that a major component of the wastewater in this area is human sewage. However, sampling was done during the period from April to July, when the incidence of human cryptosporidiosis is generally low.
In summary, the results of this study show the usefulness of the SSU rRNA-based PCR-RFLP technique for differentiating Cryptosporidium spp. and the C. parvum genotype and for tracking Cryptosporidium contamination sources in water. Extensive genotyping of water samples from various matrices (source water, finished water, wastewater, river storm water, combined sewer overflow) and environmental settings (feral, rural, urban, recreational) is needed in order to obtain a better understanding of the distribution of Cryptosporidium spp. in various waters, the human infection potential of waterborne Cryptosporidium oocysts, and the contributions of humans, farm animals, companion animals, wildlife, and other factors, such as sanitation, wastewater discharge, agriculture, recreation, and weather, to Cryptosporidium oocyst contamination of water in certain settings. Such information would be useful for scientific management of watersheds and for source water protection.
ACKNOWLEDGMENTS
This work was supported in part by an interagency agreement between the Centers for Disease Control and Prevention and the U.S. Environmental Protection Agency (DW 75937984-01-1) and by Maryland Sea Grant R/F-88.
We thank Birhane Dashew and Clem Ng for sample preparation and microscopy and Daniel Colley and Mary Bartlett for suggestions for improving the manuscript.
REFERENCES
- 1.Chung E, Aldom J E, Carreno R A, Chagla A H, Kostrzynska M, Lee H, Palmateer G, Trevors J T, Unger S, Xu R, De Grandis S A. PCR-based quantitation of Cryptosporidium parvum in municipal water samples. J Microbiol Methods. 1999;38:119–130. doi: 10.1016/s0167-7012(99)00087-1. [DOI] [PubMed] [Google Scholar]
- 2.Chung E, Aldom J E, Chagla A H, Kostrzynska M, Lee H, Palmateer G, Trevors J T, Unger S, Degrandis S. Detection of Cryptosporidium parvum oocysts in municipal water samples by the polymerase chain reaction. J Microbiol Methods. 1998;33:171–180. [Google Scholar]
- 3.Di Giovanni G D, Hashemi F H, Shaw N J, Abrams F A, LeChevallier M W, Abbaszadegan M. Detection of infectious Cryptosporidium parvum oocysts in surface and filter backwash water samples by immunomagnetic separation and integrated cell culture-PCR. Appl Environ Microbiol. 1999;65:3427–3432. doi: 10.1128/aem.65.8.3427-3432.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fayer R, Lewis E J, Trout J M, Graczyk T K, Jenkins M C, Higgins J, Xiao L, Lal A A. Cryptosporidium parvum in oysters from commercial harvesting sites in the Chesapeake Bay. Emerg Infect Dis. 1999;5:706–710. doi: 10.3201/eid0505.990513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fayer R, Graczyk T K, Lewis E J, Trout J M, Farley C A. Survival of infectious Cryptosporidium parvum oocysts in seawater and Eastern oysters (Crassostrea virginica) in the Chesapeake Bay. Appl Environ Microbiol. 1998;64:1070–1074. doi: 10.1128/aem.64.3.1070-1074.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gibbons C L, Rigi F M, Awad-El-Kariem F M. Detection of Cryptosporidium parvum and C. muris oocysts in spiked backwash water using three PCR-based protocols. Protist. 1998;149:127–134. doi: 10.1016/S1434-4610(98)70017-3. [DOI] [PubMed] [Google Scholar]
- 7.Graczyk T K, Cranfield M R, Fayer R. Recovery of waterborne oocysts of Cryptosporidium parvum from water samples by the membrane-filter dissolution method. Parasitol Res. 1997;83:121–125. doi: 10.1007/s004360050221. [DOI] [PubMed] [Google Scholar]
- 8.Hallier-Soulier S, Guillot E. An immunomagnetic separation polymerase chain reaction assay for rapid and ultra-sensitive detection of Cryptosporidium parvum in drinking water. FEMS Microbiol Lett. 1999;176:285–289. doi: 10.1111/j.1574-6968.1999.tb13674.x. [DOI] [PubMed] [Google Scholar]
- 9.Johnson D W, Pieniazek N J, Griffin D W, Misener L, Rose J B. Development of a PCR protocol for sensitive detection of Cryptosporidium oocysts in water samples. Appl Environ Microbiol. 1995;61:3849–3855. doi: 10.1128/aem.61.11.3849-3855.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kostrzynska M, Sankey M, Haack E, Power C, Aldom J E, Chagla A H, Unger S, Palmateer G, Lee H, Trevors J T, De Grandis S A. Three sample preparation protocols for polymerase chain reaction based detection of Cryptosporidium parvum in environmental samples. J Microbiol Methods. 1999;35:65–71. doi: 10.1016/s0167-7012(98)00106-7. [DOI] [PubMed] [Google Scholar]
- 11.LeChevallier M W, Norton W D, Lee R G. Giardia and Cryptosporidium spp. in filtered drinking water supplies. Appl Environ Microbiol. 1991;57:2617–2621. doi: 10.1128/aem.57.9.2617-2621.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.LeChevallier M W, Norton W D, Lee R G. Occurrence of Giardia and Cryptosporidium spp. in surface water supplies. Appl Environ Microbiol. 1991;57:2610–2616. doi: 10.1128/aem.57.9.2610-2616.1991. . (Erratum, 58:780, 1992.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Madore M S, Rose J B, Gerba C P, Arrowood M J, Sterling C R. Occurrence of Cryptosporidium oocysts in sewage effluents and selected surface waters. J Parasitol. 1987;73:702–705. [PubMed] [Google Scholar]
- 14.Mayer C L, Palmer C J. Evaluation of PCR, nested PCR, and fluorescent antibodies for detection of Giardia and Cryptosporidium species in wastewater. Appl Environ Microbiol. 1996;62:2081–2085. doi: 10.1128/aem.62.6.2081-2085.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meinhardt P L, Casemore D P, Miller K B. Epidemiologic aspects of human cryptosporidiosis and the role of waterborne transmission. Epidemiol Rev. 1996;18:118–136. doi: 10.1093/oxfordjournals.epirev.a017920. [DOI] [PubMed] [Google Scholar]
- 16.Morgan U M, Xiao L, Fayer R, Lal A A, Thompson R C A. Variation in Cryptosporidium: towards a taxonomic revision of the genus. Int J Parasitol. 1999;29:1733–1751. doi: 10.1016/s0020-7519(99)00109-5. [DOI] [PubMed] [Google Scholar]
- 17.Morgan U M, Weber R, Xiao L, Sulaiman I, Thompson R C A, Ndiritu W, Lal A A, Moore A, Deplazes P. Molecular characterization of Cryptosporidium isolates obtained from human immunodeficiency virus-infected individuals living in Switzerland, Kenya, and the United States. J Clin Microbiol. 2000;38:1180–1183. doi: 10.1128/jcm.38.3.1180-1183.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pieniazek N J, Bornay-Llinares F J, Slemenda S B, da Silva A J, Moura I N, Arrowood M J, Ditrich O, Addiss D G. New Cryptosporidium genotypes in HIV-infected persons. Emerg Infect Dis. 1999;5:444–449. doi: 10.3201/eid0503.990318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rochelle P A, De Leon R, Johnson A, Stewart M H, Wolfe R L. Evaluation of immunomagnetic separation for recovery of infectious Cryptosporidium parvum oocysts from environmental samples. Appl Environ Microbiol. 1999;65:841–845. doi: 10.1128/aem.65.2.841-845.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rochelle P A, De Leon R, Stewart M H, Wolfe R L. Comparison of primers and optimization of PCR conditions for detection of Cryptosporidium parvum and Giardia lamblia in water. Appl Environ Microbiol. 1997;63:106–114. doi: 10.1128/aem.63.1.106-114.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rochelle P A, Ferguson D M, Handojo T J, De Leon R, Stewart M H, Wolfe R L. An assay combining cell culture with reverse transcriptase PCR to detect and determine the infectivity of waterborne Cryptosporidium parvum. Appl Environ Microbiol. 1997;63:2029–2037. doi: 10.1128/aem.63.5.2029-2037.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rose J B. Environmental ecology of Cryptosporidium and public health implications. Annu Rev Public Health. 1997;18:135–161. doi: 10.1146/annurev.publhealth.18.1.135. [DOI] [PubMed] [Google Scholar]
- 23.Sluter S D, Tzipori S, Widmer G. Parameters affecting polymerase chain reaction detection of waterborne Cryptosporidium parvum oocysts. Appl Microbiol Biotechnol. 1997;48:325–330. doi: 10.1007/s002530051057. [DOI] [PubMed] [Google Scholar]
- 24.Smith H V, Rose J B. Waterborne cryptosporidiosis: current status. Parasitol Today. 1998;14:14–22. doi: 10.1016/s0169-4758(97)01150-2. [DOI] [PubMed] [Google Scholar]
- 25.Stinear T, Matusan A, Hines K, Sandery M. Detection of a single viable Cryptosporidium parvum oocyst in environmental water concentrates by reverse transcription-PCR. Appl Environ Microbiol. 1996;62:3385–3390. doi: 10.1128/aem.62.9.3385-3390.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Toze S. PCR and the detection of microbial pathogens in water and wastewater. Water Res. 1999;33:3545–3556. [Google Scholar]
- 27.U. S. Environmental Protection Agency. Method 1622: Cryptosporidium and Giardia in water by filtration/IMS/FA. Washington, D.C.: Office of Research and Development, U.S. Government Printing Office; 1997. [Google Scholar]
- 28.Wiedenmann A, Kruger P, Botzenhart K. PCR detection of Cryptosporidium parvum in environmental samples—a review of published protocols and current developments. J Ind Microbiol Biotechnol. 1998;21:150–166. [Google Scholar]
- 29.Xiao L, Escalante L, Yang C F, Sulaiman I, Escalante A A, Montali R J, Fayer R, Lal A A. Phylogenetic analysis of Cryptosporidium parasites based on the small-subunit rRNA gene locus. Appl Environ Microbiol. 1999;65:1578–1583. doi: 10.1128/aem.65.4.1578-1583.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xiao L, Morgan U M, Limor J, Escalante A, Arrowood M, Shulaw W, Thompson R C A, Fayer R, Lal A A. Genetic diversity within Cryptosporidium parvum and related Cryptosporidium species. Appl Environ Microbiol. 1999;65:3386–3391. doi: 10.1128/aem.65.8.3386-3391.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xiao L, Alderisio K, Limor J, Royer M, Lal A A. Identification of species and sources of Cryptosporidium oocysts in storm waters with a small-subunit rRNA-based diagnostic and genotyping tool. Appl Environ Microbiol. 2000;66:5492–5498. doi: 10.1128/aem.66.12.5492-5498.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Xiao L, Morgan U M, Fayer R, Thompson R C A, Lal A A. Cryptosporidium systematics and implications for public health. Parasitol Today. 2000;15:287–292. doi: 10.1016/s0169-4758(00)01699-9. [DOI] [PubMed] [Google Scholar]