Abstract
Common and minor birth defects, such as spina bifida occulta (SBO) and lumbosacral transitional vertebra (LSTV), are largely asymptomatic and overlooked. However, it is important for clinicians to consider their potential impacts on spinal stability. Neuromuscular scoliosis (NMS) is an abnormal lateral curvature of the spine that affects children with pre-existing neuromuscular conditions that are often complex to manage. The purpose of this case report is to describe the association of dual lumbosacral anomalies with complicated NMS. A 12-year-old boy was brought to the chiropractor by his mother for a consultation and possible care for the boy's back pain, progressive scoliosis, and long-standing walking abnormality that worsened quickly in the past 12 months. His mother stated that the patient walked on the balls of his left foot instead of putting weight on the heel ever since he started learning to walk. He had visited several pediatricians and neurologists since childhood. No one had been able to solve his problems. Radiographs showed right thoracolumbar curve of Cobb angle 20°, left pelvic obliquity, a cleft in the L5 and S1, and articulation of the transverse processes of L5 with the bilateral sacral alae. The patient was diagnosed with NMS and functional leg length discrepancy attributed to SBO and a LSTV at L5 level. Multimodal chiropractic care and foot orthotics were used. After 18 months of interventions, normal spinal curve, heel-to-toe gait, and posture balance were retrieved successfully. To date, few reports have been published on the impacts of SBO along with LSTV upon the lumbosacral spine. This article will allow a better understanding of the potential impacts of these birth defects and considerable consequences they would have on the growing spine and, therefore, may help to alleviate their impacts.
Keywords: Birth defect, Lumbosacral transitional vertebra, Neuromuscular scoliosis, Spina bifida, Toe-walking
Introduction
Neuromuscular scoliosis (NMS) is an abnormal lateral curvature of the spine that affects children with pre-existing neuromuscular conditions [1]. Radiographs typically show a long C-shaped thoracolumbar curve with associated pelvic obliquity [2]. NMS occurs in approximately half of children with spina bifida [3] and typically becomes noticeable during the pubertal growth spurt. Factors that contribute to NMS include uneven mechanical forces, core instability, muscle weakness, and postural imbalance [4]. Scoliosis in children may also underlie the coexistence of multiple physiological impairments. It can be challenging to treat children with NMS due to the complexity of underlying comorbidities [2].
This is the first case report describing the association between NMS and co-existence of spina bifida occulta (SBO) and a lumbosacral transitional vertebra (LSTV) in the L5 level. These 2 birth defects are usually innocent and largely ignored. Nevertheless, simultaneous presence of 2 malformations at the same vertebral segment would result in different behaviors. This article allows a better understanding of the impacts of these lumbosacral malformations on biomechanics of the low back and complex consequences they would have on the growing spine and, therefore, may help to alleviate their impacts.
Case report
A 12-year-old boy presented to the clinic with complaints of spinal deformity and clumsy gait. His mother stated that the patient walked on the balls of his left foot instead of putting weight on the heel ever since he started learning to walk. He had no difficulty rising from a seated position but had a hard time standing up straight. In addition, he experienced recurrent lower back pain after participating in school sports activities. The medical history of the patient's family members did not include any neurological problems. Since childhood, he had visited several pediatricians and neurologists and was excluded from having neurological disorders. Twelve months ago, his symptoms had worsened quickly, and an ankle‐foot orthosis was attempted. He had also been treated at the school screening program for adolescent idiopathic scoliosis in the past 3 months. The treatment consisted of physiotherapy, stretching, and strengthening exercises (including heel walking and squats, walking on sloped and uneven terrain, and marching on the spot). The aforementioned treatments had only minimal effects. Henceforth, the patient was brought to the chiropractor by his mother for a consultation and possible intervention for the boy's complaints.
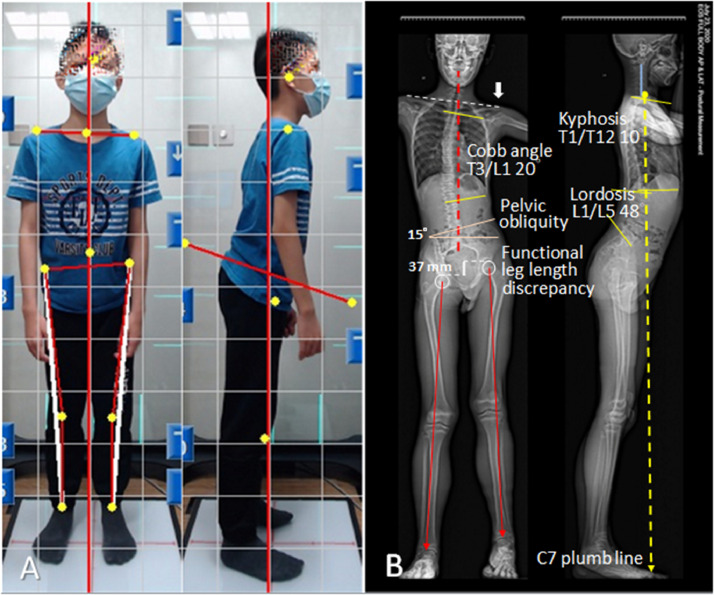
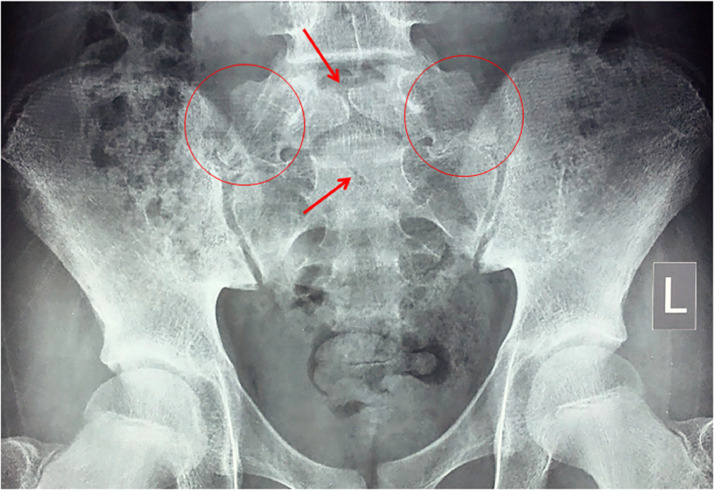
At the initial presentation, the patient walked with a left straight knee and toe-walking gait. Posture analysis revealed left dropped shoulder, forward stooped with a flat back posture, left lateral and anterior pelvic tilt, and functional leg length discrepancy (Fig. 1A). In the left lower limb, the thigh and calf presented a slightly lower caliber than that of the contralateral limb. The range of motion was normal in the back, hips, and knees, but reduced to 10° in neck extension. A right-convex thoracolumbar curve was observed. The skin overlying the lumbosacral region showed a dimple with a hairy patch. Spinal palpation revealed intersegmental restriction at C7-T1; T7-T10; and L2-L5 vertebral levels. Hypertonicity was palpable in the right upper trapezius, rhomboid and paraspinal muscles, and left quadratus lumborum. Neurological and laboratory results were normal. Radiographs showed a right thoracolumbar curve with a Cobb angle of 20°, left pelvic obliquity of 15°, nonfusion of the L5 vertebral arch and the S1 laminae, and pseudo-articulation of the bilateral L5 transverse processes with the sacrum (Figs. 1B and 2). The patient was diagnosed with NMS attributed to SBO and a LSTV at L5 vertebral segment.
Fig. 1.
Postural assessment using whole-body EOS system in the standing position. (A) Posture photography shows left dropped shoulder, anterior and left pelvic tilt, and stooped forward with a flat back posture. (B) Full-body radiographs exhibit a C-shaped right thoracolumbar curve with associated left pelvic obliquity, uneven shoulders, flattened cervical and thoracic curve, intensified lumbar lordosis, a smaller caliber of the left thigh and calf, and functional limb length discrepancy. The central sacral vertical line (dashed red line) represents the global axis, and the posterior vertebral line (blue line) highlights the cervical curvature. The C7 plumb line (dashed yellow line) should fall within 3 cm, either anterior or posterior, to the posterosuperior corner of the S1 endplate. The reference values for adolescents are 31.5°-39.2° for thoracic curve and 39.8°-45.6° for lumbar L1-L5 curve by means of the Cobb Method [5].
Fig. 2.
Anterior pelvis radiograph shows a midline defect at the vertebral arch of the L5, lack of midline fusion of the laminae of the S1 (arrows), and articulation of bilateral transverse processes of L5 with bilateral sacral alae (encircled in red), compatible with L5 and S1 spina bifida occulta and lumbosacral transitional vertebra.
Chiropractic intervention consisted of the following: spinal manipulation, mechanical spinal distraction, cervical extension-compression traction, and instrument-assisted soft tissue mobilization. To correct the scoliosis component and shoulder and pelvic imbalances, spinal manipulation was applied at the apex (T8) of the scoliotic curve and to the restricted vertebral segments. Mechanical distraction was applied laterally to counteract the spinal curvature and correct the scoliotic curve on the convex side. Cervical extension-compression traction was administered to adjust the abnormal posture. A handheld massage device (Strig, Korea) was used to massage hypertonic muscles for stabilizing the spine. Treatment sessions were scheduled 3 times per week for the first month. General lifestyle coaching, such as home exercises and proper posture, was also provided to help keep the spine in functional alignment.
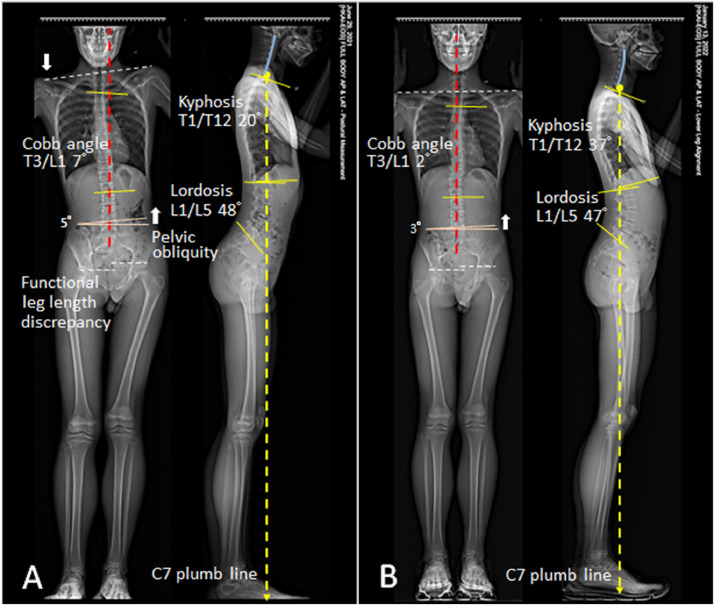
Improved range of motion of the neck was achieved after 4 weeks of treatment. Subsequently, specific stretching of the tight muscles was performed in each treatment session. Treatments were delivered 2 times weekly for an additional 5 months. At the 6-month follow-up, the spinal mobility returned to normal and back pain was fully relieved; the gait pattern and trunk posture significantly improved, and the patient was able to keep his feet flat on the floor. The patient only showed a minimum imbalance while standing. The treatment was continued once a week to maintain the corrected effects. At the 11th-month follow-up, his scoliosis and postural parameters continued to improve (Fig. 3A). A custom-made foot orthotic (shoe inserts) was prescribed to help the feet support and balance while walking. The patient continued manual correction once a week for an additional 6 months and gradually resumed normal activities. On the 18th month of re-evaluation, normal spinal curve, heel-to-toe gait, and posture balance were successfully retrieved (Fig. 3B). No treatment-related adverse events were observed.
Fig. 3.
Comparison of treatment outcomes over time. (A) The same patient shown in Fig. 1 demonstrated significant improvement in global spinal curve, radiographic parameters, and postural control 11 months after treatment initiation. (B) On the 18th month re-evaluation, the patient achieved a retrieval of posture balance and heel-to-toe gait. Radiograph demonstrates a gradual normalization of the spinal curve and most postural parameters.
Discussion
Spina bifida (also called myelodysplasia or neural tube defect) is a term used to describe a set of birth defects that involve incomplete closure of the spinal column during the first month of embryonic development. The condition varies in degree, from mild (no symptoms) to severe (nerve damage). “Spina bifida occulta (SBO)” is the mildest form and most common type of this malformation, which results in a small cleft in 1 or 2 vertebrae (mostly L5 or S1). The spinal cord, meninges, and overlying skin remain intact [6]. The condition is most commonly asymptomatic and needs no treatment. SBO presents in 15% of the Chinese adults (n = 1061), and may go undetected [7]. Other types of spina bifida are meningocele and myelomeningocele, both of which are characterized by a fluid-filled sac bulging through a spinal cleft.
Lumbosacral transitional vertebrae (LSTVs) are also a common birth defect of the spine in which an articulation or fusion is formed between the L5 vertebra and the sacrum either on one or both sides [8]. LSTVs can be seen around 26% (range 16%-36%) of general population and are referred to as an “anatomical variant” since most of them do not affect overall functioning [9]. As a matter of fact, as a result of hypomobility at the involved level and hypermobility at the upper level [10], it is reasonable to presume that the LSTV can impact biomechanics and functions of the lumbosacral and paraspinal structures over time [8,9]. Increased lumbar lordosis [11], L5 dysmorphism [11], degeneration of the superior disk [12], lumbar disk herniation [13], sacroiliac joint dysfunction [10], and scoliosis [9] are unintended consequences of the LSTVs reported in literature.
Lumbar radiographs were retrospectively studied on 148 young people (with a median age of 23 years) with lower back pain, Li et al. found 17 cases (11.49%) with LSTV. Out of these, 8 patients also had SBO (8/17, 47%) [14]. In another review of pelvic radiographs of 64 patients with lower back pain along with LSTV, Sharma et al. found 27 (42.18%) patients (with median age of 36 years) also had SBO. Co-existence of LSTV and SBO appears to be common in patients attending for evaluation of back pain [15]. LSTV and SBO are largely asymptomatic and overlooked. However, the co-existence of LSTV and SBO at the same level, as seen in this case, would result in different behaviors. There is a scarcity of case reports describing the association between NMS and the presence of LSTV and SBO.
Scoliosis is an abnormal lateral spinal curvature with a Cobb angle of ≥10° measured on a standing coronal radiograph [16]. Scoliosis in the pediatric population can be classified as idiopathic, congenital, and neuromuscular, and syndromic in etiology [17]. Neuromuscular scoliosis (NMS) is caused by a neurological or muscular condition that impairs the ability to control of the muscles supporting the spine. NMS often gets worse during the growth spurts. During adolescence, the 5 sacral vertebrae fuse into an immobile sacrum. The sacrum articulates superiorly with the fifth lumbar vertebra, bilaterally with the ilia, and caudally with the coccyx [18]. With regard to this case (Fig. 2), the lumbosacral malformations jeopardize the balance of forces across the lumbosacral and sacroiliac joints, which in turn lead to strain or weakness in the supporting muscles and compromised motor control. Over time, the spine becomes unstable, resulting in low back pain, curving of the spine, and postural and gait abnormalities.
The management of NMS is a complex and meticulous service for such populations, as the spinal curve is often progressive and may impact trunk stability, muscle strength, and physiological and psychological functions [1]. Factors affecting the progression of scoliosis include female sex, skeletal maturity, symmetry and stability of the spine, handedness, gait, and posture [4,19]. Currently, there is no known cure for NMS; however, the condition can be managed with an effective multidisciplinary collaboration. External bracing may prevent spinal curvature from worsening during periods of growth spurt but not to correct the curve. Surgeries for NMS are relatively complex and with a high risk for severe complications, because of the complexity of underlying comorbidities [2]. There has been emerging evidence to suggest that manipulative therapy can stabilize curve progression and even correct some degree of curves in adolescent idiopathic scoliosis [16]. This report illustrates the potential role of multimodal chiropractic care to play in managing patients with complicated NMS.
The basic objectives of chiropractic intervention of this patient with spinal deformity and clumsy gait were to stabilize curve progression and prevent further neurological complications. According to the guidelines of the International Scientific Society on Scoliosis Orthopaedic and Rehabilitation Treatment, the success of conservative treatments is defined by preventing a curve progression of ≤5° (stabilization) or even a decrease of the curve of ≥6° (correction) from baseline values [20]. Chiropractic care consisting of multimodal interventions was used for this patient to restore an appropriate spinal curvature and gait pattern by strengthening core muscles, adjusting spinal loading and body posture, and allowing reasonable function to support body's natural alignment [16]. The foot orthotics contributing to a balanced foundation and stabilized pelvis might also have help improving postural performance and gait function.
This study has some limitations. First, this retrospective single-case study lacks of a control group to compare outcomes. Second, it is difficult to actually get to a logical assertion about the effectiveness of chiropractic intervention when the pathophysiology of patient's problems (progressive scoliosis and long-standing gait abnormality) remains unclear. Furthermore, the follow-up period was limited. Even with the aforementioned limitations, the chiropractic care for the management of complicated NMS showed a success in restoring spinal curvature and gait performance in the patient with SBO and a LSTV at L5 level. The mechanisms of action that contributed to the observed changes in this study warrant further in-depth analysis.
Conclusion
SBO and LSTV are usually asymptomatic and largely ignored. Simultaneous presence of these 2 malformations at the same vertebral segment would result in different behaviors. Thus, awareness of anatomical variants in the lumbosacral spine is important for clinicians when managing spinal deformities, and may prevent serious complications following appropriate interventions.
Patient consent
This case report has been prepared after obtaining a written informed consent from the patient's legal guardian to publish the case details. Because this was a retrospective study, it did not require approval from an ethics committee.
Footnotes
Competing Interests: All authors declare no conflict of interest.
References
- 1.Murphy RF, Mooney JF., 3rd Current concepts in neuromuscular scoliosis. Curr Rev Musculoskelet Med. 2019;12(2):220–227. doi: 10.1007/s12178-019-09552-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loughenbury PR, Tsirikos AI. Current concepts in the treatment of neuromuscular scoliosis: clinical assessment, treatment options, and surgical outcomes. Bone Joint Open. 2022;3(1):85–92. doi: 10.1302/2633-1462.31.BJO-2021-0178.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heyns A, Negrini S, Jansen K, Moens P, Schelfaut S, Peers K, et al. The prevalence of scoliosis in spina bifida subpopulations: a systematic review. Am J Phys Med Rehabil. 2018;97(11):848–854. doi: 10.1097/PHM.0000000000000966. [DOI] [PubMed] [Google Scholar]
- 4.Allam AM, Schwabe AL. Neuromuscular scoliosis. PM R. 2013;5(11):957–963. doi: 10.1016/j.pmrj.2013.05.015. [DOI] [PubMed] [Google Scholar]
- 5.Furlanetto TS, Sedrez JA, Candotti CT, Loss JF. Reference values for Cobb angles when evaluating the spine in the sagittal plane: a systematic review with meta-analysis. Motricidade. 2018;14(2-3):115–128. doi: 10.6063/motricidade.10890. doi: [DOI] [Google Scholar]
- 6.Bhandari J, Thada PK. StatPearls. StatPearls Publishing; Treasure Island (FL): 2022. Neural tube disorders. [Internet]PMID: 32310363. [Google Scholar]
- 7.Wu JW, Xing YR, Wen YB, Li TF, Xie JF, Feng QD, et al. Prevalence of spina bifida occulta and its relationship with overactive bladder in middle-aged and elderly Chinese people. Int Neurourol J. 2016;20(2):151–158. doi: 10.5213/inj.1630464.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Matson DM, Maccormick LM, Sembrano JN, Polly DW. Sacral dysmorphism and lumbosacral transitional vertebrae (lSTV) review. Int J Spine Surg. 2020;14(1):S14–S19. doi: 10.14444/6075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chu ECP, Huang KHK, Shum JSF. Lumbosacral transitional vertebra as a potential contributing factor to scoliosis: a report of two cases. Asia-Pac Chiropr J. 2020;1:007. doi: 10.46323/2021007. [DOI] [Google Scholar]
- 10.Illeez OG, Atıcı A, Ulger EB, Kulcu DG, Ozkan FU, Aktas I. The transitional vertebra and sacroiliac joint dysfunction association. Eur Spine J. 2018;27(1):187–193. doi: 10.1007/s00586-016-4879-4. [DOI] [PubMed] [Google Scholar]
- 11.Mahato NK. Disc spaces, vertebral dimensions, and angle values at the lumbar region: a radioanatomical perspective in spines with L5-S1 transitions. Clinical article. J Neurosurg Spine. 2011;15(4):371–379. doi: 10.3171/2011.6.SPINE11113. [DOI] [PubMed] [Google Scholar]
- 12.Lee CS, Ha JK, Kim DG. The clinical importance of lumbosacral transitional vertebra in patients with adolescent idiopathic scoliosis. Spine. 2015;40(17):E964–E970. doi: 10.1097/BRS.0000000000000945. [DOI] [PubMed] [Google Scholar]
- 13.Kurt EE, Turkyilmaz AK, Dadali Y, Erdem HR, Tuncay F. Are transitional vertebra and spina bifida occulta related with lumbar disc herniation and clinical parameters in young patients with chronic low back pain? Eurasian J Med. 2016;48(3):177–180. doi: 10.5152/eurasianjmed.2016.0285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li W, Xiong Z, Dong C, Song J, Zhang L, Zhou J, et al. Distribution and imaging characteristics of spina bifida occulta in young people with low back pain: a retrospective cross-sectional study. J Orthop Surg Res. 2021;16(1):151. doi: 10.1186/s13018-021-02285-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sharma A, Kumar A, Kapila A. Co-existence of spina bifida occulta and lumbosacral transitional vertebra in patients presenting with lower back pain. Reumatologia. 2022;60(1):70–75. doi: 10.5114/reum.2022.114171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chu ECP, Chakkaravarthy DM, Huang KHK, Ho VWK, Lo FS, Bhaumik A. Changes in radiographic parameters following chiropractic treatment in 10 patients with adolescent idiopathic scoliosis: a retrospective chart review. Clin Pract. 2020;10(3):1258. doi: 10.4081/cp.2020.1258.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Levy BJ, Schulz JF, Fornari ED, Wollowick AL. Complications associated with surgical repair of syndromic scoliosis. Scoliosis. 2015;10:14. doi: 10.1186/s13013-015-0035-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chung A, Lashkari N, Stanton E, Qureshi OA, Buser Z, Wang JC. Chapter 15- Lumbosacral CT. In: Louie PK, An HS, Samartzis D, editors. Atlas of spinal imaging: phenotypes, measurements, and classification systems (1st ed.). pp. 211-224. Elsevier. 2022. Paperback ISBN: 9780323761116. doi: 10.1016/B978-0-323-76111-6.00010-9.
- 19.Yoo YJ, Park JG, Jo L, Hwang Y, Yoon MJ, Kim JS, et al. Factors influencing the progression and direction of scoliosis in children with neurological disorders. Children (Basel) 2022;9(1):81. doi: 10.3390/children9010081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Negrini S, Donzelli S, Aulisa AG, Czaprowski D, Schreiber S, de Mauroy JC, et al. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018;13:3. doi: 10.1186/s13013-017-0145-8. [DOI] [PMC free article] [PubMed] [Google Scholar]