Abstract
Choosing a route to parenthood can be a difficult decision for individuals with Turner syndrome, who must consider the unlikely possibility of spontaneous pregnancy, the potential need for assisted reproductive technology such as in vitro fertilization (IVF), and the risks of pregnancy-related complications. In addition, there are other options for parenthood, such as surrogacy and adoption. The perspectives of individuals with Turner syndrome regarding routes to parenthood have not been described in the literature, despite thorough investigation into the feasibility and safety of pregnancy in this population. We conducted a novel online survey of 226 individuals with Turner syndrome to assess their interest in parenthood, their perspectives on available routes to parenthood, and the factors that influence their decision-making. One-quarter of the respondents were already parents, including 54.5% who had achieved pregnancy and 45.5% who adopted. Of those who were not parents, 68.5% expressed a desire to become a parent. Overall, participants had the strongest interest in adoption as a route to parenthood. Interest in adoption was significantly associated with fear of pregnancy-related risks to their health and the health of a future child. Participants also reported interest in pregnancy and IVF. Interest in both pregnancy and IVF were significantly associated with a desire to experience pregnancy and to have a biological child. This study provides important insights into the perspective of individuals with Turner syndrome with respect to building a family and serves as a valuable counseling resource for clinicians facilitating patient decision-making about options for parenthood.
Keywords: Turner syndrome, Pregnancy, Adoption, Surrogacy, Genetic counseling, Reproductive decision-making
Background
Turner syndrome is a multisystem genetic disorder characterized by the presence of one intact X chromosome and an absent or structurally abnormal second sex chromosome (Gravholt et al. 2017). Almost half of individuals with Turner syndrome have mosaicism in which there is a combination of 45,X and another cell line involving X or Y. In Turner syndrome, infertility, secondary to ovarian failure prior to or around the time of puberty, is common (Modi 2003). Many individuals with Turner syndrome report infertility as their primary challenge of living with the condition (Sutton et al. 2005).
The literature about pregnancy outcomes in Turner syndrome is growing (Calanchini et al. 2020; Grewal et al. 2021). In a review of 276 individuals with Turner syndrome, 87.7% did not have children, 9.1% chose to adopt, and only 3.2% had experienced pregnancy (Hadnott et al. 2011). While most individuals with Turner syndrome require oocyte donation to become pregnant, recent studies suggest that up to 8% of individuals with Turner syndrome can conceive without assisted reproductive technology; these are most likely individuals with a mosaic 45,X/46,XX karyotype (Bernard et al. 2016; Birkebaek et al. 2002; Bryman et al. 2011; Hadnott et al. 2011). However, pregnancy has risks to both the pregnant individual and fetus, regardless of spontaneous conception or use of assistive reproductive technology. Various factors involving the cardiovascular system during pregnancy and delivery increase the risk for aortic dissection or rupture, which can be unpredictable, sudden, and life-threatening (Silberbach et al. 2018). The risk of aortic dissection or rupture during pregnancy is greater in individuals who have hypertension, baseline aortic dilation, bicuspid aortic valve, or coarctation of the aorta, which are of increased prevalence in the Turner syndrome population (Gravholt et al. 2006, 2017, 2019). Other pregnancy-related complications associated with Turner syndrome that may impact maternal and fetal health include obesity, diabetes, thyroid dysfunction, hypertension, and preeclampsia (Calanchini et al. 2020; Chevalier et al. 2011; Gravholt et al. 2006, 2019; Grewal et al. 2021; Mercadal et al. 2011). Pregnancies in individuals with Turner syndrome are also associated with increased rates of spontaneous abortion, fetal chromosome abnormalities, low birth weight, and prematurity (Bernard et al. 2016; Bodri et al. 2006). Historically, the risk of pregnancy complications in Turner syndrome has led to recommendations to avoid pregnancy and consider gestational surrogacy or adoption as alternate routes to parenthood. However, recent data suggest risk can be managed by careful cardiovascular evaluation before, during, and after pregnancy (Calanchini et al. 2020).
Choosing a route to parenthood is a difficult decision that includes weighing the low possibility of spontaneous pregnancy, potential need for assisted reproductive technology, the risks to the individual carrying a pregnancy, and the risks to the fetus (Calanchini et al. 2020; Hadnott et al. 2011). At the same time, the desire for a biological child or the experience of pregnancy can be compelling (Sutton et al. 2005). To date, there is no literature on the perspectives of individuals with Turner syndrome on available paths to parenthood. A recent publication on the current state of clinical care and research in Turner syndrome (and other sex chromosome abnormalities) did not mention parenthood (Gravholt et al. 2020). The purpose of this study is to obtain self-reported information from individuals with Turner syndrome about interest in various routes to parenthood and factors that influence this decision. This study will provide insight into the complexity of parenthood decisions and will serve to advance care and better facilitate decision-making surrounding routes to parenthood.
Methods
Study design and recruitment
We sought the opinions of English-speaking adults (18 years or older) with Turner syndrome using a self-administered online survey. The main source of recruitment was a Facebook post distributed by the Turner Syndrome Society of the United States (TSSUS) across several Turner syndrome Facebook groups that are independent of TSSUS. The Facebook groups have international membership, and not all individuals are also members of TSSUS. In addition, a recruitment advertisement including the link to the survey was distributed in the November and December 2020 monthly newsletters of TSSUS. Lastly, information about the study was shared on Twitter by co-investigators. Enrollment took place between November 2020 and January 2021.
Instrumentation
The survey was designed by the research team, including a geneticist (AL), two genetic counselors (AC, MS), and two genetic counseling students (EF, ES). Survey commentary was provided by a 22-year-old woman with Turner syndrome. The instrument used novel close- and open-ended questions to capture demographic information, self-reported details about the participant’s Turner syndrome diagnosis, and experiences with and preferences for various paths to parenthood. The survey instrument also included four questions from a prior study focusing on the wish to conceive and concerns about developing cardiovascular complications during pregnancy in individuals with Turner syndrome (van Hagen et al. 2017). The survey utilized skip logic to determine which questions participants were presented with based on their parental status and interest in parenthood. Study data were collected and managed using REDCap (Research Electronic Data Capture), a secure web-based data collection application, hosted at Mass General Brigham (Harris et al. 2009, 2019).
Data analysis
Data were analyzed using R studio (RStudio Team, 2020). Spearman Rho analyses were performed to examine strength of association between factors influencing approach to parenthood, worry for personal health risks associated with pregnancy, and interest in routes to parenthood (pregnancy, IVF, adoption, surrogacy). Ordinal regression analysis was performed to assess effect of participant characteristics on interest in routes to parenthood. All reported relationships were statistically significant at the 0.05 level.
For questions using a 5-point Likert scale, responses were collapsed into 3 subcategories (“strong interest” = very or definitely interested, “interest” = slightly interested or interested, and “no interest” = not interested). Answers of “not sure” were excluded from analysis. Responses “very often” and “often” were combined in the analysis of frequency of worry associated with personal health risks associated with pregnancy.
Relationship status was combined for the responses “in a relationship” or “married” to indicate partnership, with all other responses grouped into “other.” Additionally, age at Turner syndrome diagnosis and age of learning about infertility in Turner syndrome were grouped into under or over age of 13 for analysis purposes.
Results
Recruitment results
There were a total of 292 survey responses. Sixty-six (22.6%) responses were incomplete and were removed from analysis. The 226 participants who completed all the questions presented to them in the survey were included in the analysis. Participant characteristics are summarized in Table 1. Their ages ranged from 18 to 71, with a mean age of 34. Most participants self-identified as white (89.4%) and female (98.2%). Regarding karyotype, 41.6% of participants reported they were not sure; 29.6% reported having 45,X; and 11.9% reported having 45,X/46,XX mosaicism.
Table 1.
Demographic information for surveyed participants
| Total participants (n = 226) | |
|---|---|
| Age (years) | |
| Mean (SD) | 34 (10.18%) |
| Range | 18–71 |
| Gendera | |
| Female | 222 (98.2%) |
| Non-binary | 4 (1.77%) |
| Decline to answer | 1 (0.4%) |
| Race/ethnicity | |
| White | 202 (89.4%) |
| Latinx/Hispanic | 11 (4.9%) |
| African-American/Black | 5 (2.2%) |
| Native American/Alaska Native/First Nations | 3 (1.3%) |
| South Asian | 3 (1.3%) |
| East/Southeast Asian | 1 (0.4%) |
| Caribbean | 1 (0.4%) |
| Karyotype | |
| Not sure | 94 (41.6%) |
| 45,X | 67 (29.6%) |
| 45,X/46,XX | 27 (11.9%) |
| 45,X/46,XY | 10 (4.4%) |
| 45,X,r(X) | 9 (4.0%) |
| 46,X,i(Xq) (mosaic/non-mosaic) | 8 (3.5%) |
| Other | 8 (3.5%) |
| 45,X/47,XXX | 3 (1.3%) |
| Parental status | |
| Not a parent | 168 (74.3%) |
| Parent | 58 (25.7%) |
| Age at diagnosis, years | |
| < 13 | 161 (71.2%) |
| ≥ 13 | 65 (28.8%) |
| Age learned of infertility, years | |
| < 13 | 90 (39.8%) |
| ≥ 13 | 100 (44.3%) |
| Not sure | 36 (15.9%) |
aBecause participants could select more than one answer, percentages do not add up to 100%
Successful routes to parenthood
Of the total 226 participants, 58 (25.7%) were parents. Of the 58 parents in our sample, 28 (48.3% of parents and 12.4% of the total cohort) reported carrying a pregnancy, 27 (46.6% of parents and 11.9% of the total cohort) adopted children, and 4 (6.9% of parents and 1.8% of the total cohort) reported being stepparents. Of those who personally carried a pregnancy, 75% used IVF. 95.2% of the pregnancies achieved by IVF used donor oocytes.
Current parenthood plans among parents and prospective parents
Among parents, 11 (19%) reported they were currently trying to expand their family, either by adoption (45.5%) or pursuing their own pregnancy (54.5%) (Table 2). Of those pursuing pregnancy, 66.7% reported they are pursuing IVF, all using donor oocytes.
Table 2.
Currently pursued routes to parenthood, by parental status. Participants could select more than one option
| Current route to parenthood | Parent, expanding family (n = 11) | Prospective parent (n = 32) |
|---|---|---|
| My own pregnancy | 6 (54.5%) | 19 (59.4%) |
| A partner’s pregnancy | — | 1 (3.1%) |
| A surrogate’s pregnancy | — | 6 (18.8%) |
| Adoption | 5 (45.5%) | 18 (56.3%) |
| Fostering | — | 1 (3.1%) |
Of the 168 participants who are not parents (74.3%), 68.5% expressed a desire to become one, 18.5% were not sure, and 13.1% did not want to become a parent. Thirty-two participants who are not parents (19%) reported they are currently pursuing routes to parenthood (“prospective parents”); 56.3% of prospective parents are pursuing adoption and 59.4% are pursuing their own pregnancy (Table 2). Ten (31.3%) prospective parents were pursuing more than one route. Of those pursuing their own pregnancy, 18.2% are using IVF and 42.1% of those are using oocyte donation. Surrogate pregnancy is being pursued by 18.8% of prospective parents and most are not using IVF (66.7%). A single participant reported using IVF with their own eggs for surrogate pregnancy (16.7%). Lastly, a small percentage of prospective parents reported pursuing foster care (3.1%) or a partner’s pregnancy (3.1%).
Interest in routes to parenthood
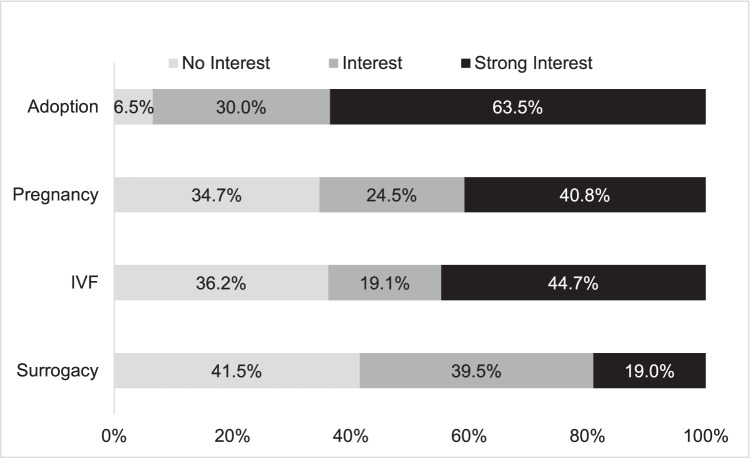
When asked to indicate their level of interest in different routes to parenthood, participants were most likely to report a strong interest in adoption (63.5%), followed by IVF (44.7%) and pregnancy (40.8%). Participants expressed less interest in surrogacy (Fig. 1).
Fig. 1.
Interest in routes to parenthood among parents and prospective parents
Certain participant characteristics influenced the participants’ interest in parenthood routes. Participant age was inversely related to their interest in routes to parenthood. Specifically, for every one-year increase in age, there is about a 5% decrease in the odds of reporting interest in pregnancy (log(odds) = − 0.048, SE = 0.015, t = − 3.242), adoption (log(odds) = − 0.048, SE = 0.015, t = − 3.035), and IVF (log(odds) = − 0.05, SE = 0.015, t = − 3.451). For each year increase in age, the odds of reporting interest in surrogacy decreased by about 3% (log(odds) = − 0.03, SE = 0.014; t = − 2.061).
When compared to non-parents, the odds of parents reporting interest in certain routes to parenthood was lower by (1) 51% for IVF (log(odds) = − 0.722, SE = 0.296, t = − 2.437); (2) 55% for adoption (log(odds) = − 0.791, SE = 0.325, t = − 2.435); and (3) 79% for surrogacy (log(odds) = − 1.57, SE = 0.326, t = − 4.809). Odds of reporting interest in adoption lowered by 47% (log(odds) = − 0.63, SE = 0.295, t = − 2.132) for those married or in a relationship.
No other participant characteristics had a significant effect on interest in routes to parenthood.
Factors influencing interest in routes to parenthood
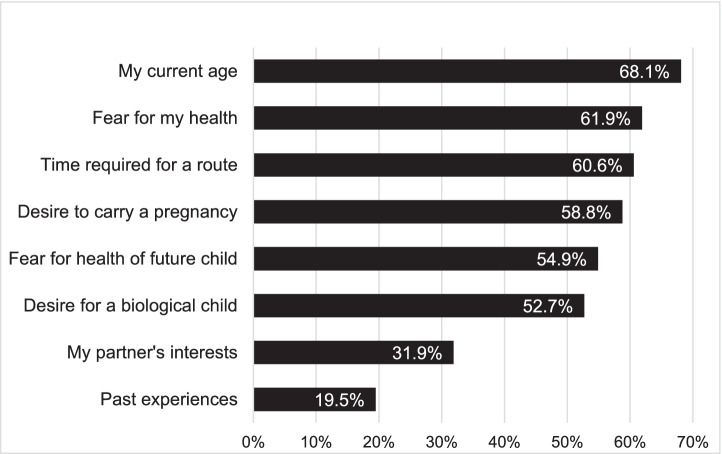
Participants reported that many factors influenced their approach to parenthood (Fig. 2). The most common factor was their age (68.1% of participants), followed by fear for their health (61.9%), time required for a route (60.6%), desire to carry a pregnancy (58.8%), fear for health of a future child (54.9%), and desire for a biological child (52.7%). Additionally, partner’s interests were a factor for 31.9% of the overall cohort and 61.5% of participants in a relationship or married.
Fig. 2.
Factors influencing approach to parenthood. Percentage reflects those who responded yes to whether the factor is influencing their approach
Association between factors influencing approach to parenthood and interest in routes to parenthood
As shown in Table 3, the desire to experience pregnancy and the desire to have a biological child were both significantly associated with an interest in using pregnancy as a route to parenthood (p < 0.001 for both) and an interest in IVF (p < 0.0001 and p < 0.0001, respectively). The time required for a route was associated with interest in adoption (p < 0.05) and surrogacy (p < 0.05).
Table 3.
Factors associated with interest in routes to parenthood. Significant associations between factors influencing approach to parenthood and interest in routes to parenthood
| Route of interest | Associated factor | rs | p-value | |
|---|---|---|---|---|
| Adoption | Fear pregnancy could have a negative influence on my: | Aorta | 0.2012 | < 0.01 |
| Heart | 0.1484 | < 0.05 | ||
| Fear for my health | 0.1402 | < 0.05 | ||
| Fear for health of a future child | 0.1607 | < 0.05 | ||
| Time required for a route | 0.1769 | < 0.05 | ||
| Pregnancy | Desire to carry a pregnancy | 0.5712 | < 0.0001 | |
| Desire for a biological child | 0.3899 | < 0.0001 | ||
| IVF | Desire to carry a pregnancy | 0.4889 | < 0.0001 | |
| Desire for a biological child | 0.2402 | < 0.0001 | ||
| Surrogacy | Time required for a route | 0.1769 | < 0.05 | |
Fears associated with pregnancy
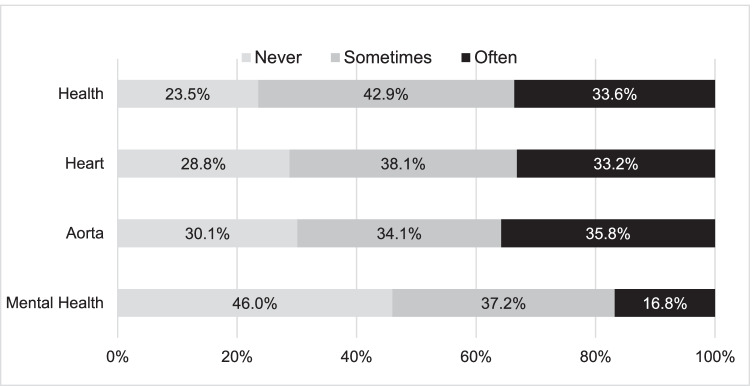
Approximately one-third of participants reported that they are often afraid that pregnancy could have a negative influence on their aorta dimension (35.8%), overall health (33.6%), and heart (33.2%). However, fear about overall health was generally the most prevalent, with 76.5% feeling afraid often or sometimes. Only one-quarter to one-third of patients were never worried about pregnancy-related risks to their cardiovascular or overall health. Responses are summarized in Fig. 3.
Fig. 3.
Fears associated with pregnancy. Participants were asked how often they have felt afraid pregnancy could have a negative influence on their health, heart, aorta, or mental health
As shown in Table 3, there were significant associations between interest in adoption as a route to parenthood and fear that pregnancy could have a negative influence on the aorta (p < 0.01) or heart (p < 0.05). Interest in adoption was also associated with fear for overall personal health (p < 0.05) and fear for health of a future child (p < 0.05).
Individuals born with a congenital heart defect had 1.9 times higher odds (compared to those born without a congenital heart defect) of feeling afraid that pregnancy could have a negative influence on their heart (log(odds) = 0.63, SE = 0.289, t = 2.198) and had twice as high odds of reporting feeling afraid about their aorta (log(odds) = 0.7, SE = 0.292, t = 2.393).
Discussions about parenthood
Participants most often discussed their approach to parenthood with a friend (70.8%), followed by a parent or guardian (64.8%), or a partner (54.9%). Only a minority (7.1%) reported discussing with no one (Table 4).
Table 4.
Individuals with whom the participants discussed their approach to parenthood. Other = Turner syndrome social media groups and coworkers
| Total participants (n = 226) | |
|---|---|
| Person | |
| Friend | 160 (70.8%) |
| Parent or guardian | 145 (64.2%) |
| Partner | 124 (54.9%) |
| Sibling | 84 (37.2%) |
| Medical provider | 82 (36.3%) |
| Mental health professional | 46 (20.4%) |
| No one | 16 (7.1%) |
| Religious leader | 12 (5.3%) |
| Teacher | 6 (2.7%) |
| Other | 6 (2.7%) |
| Medical provider | |
| Endocrinologist | 58 (25.7%) |
| Primary care doctor | 45 (19.9%) |
| Obstetrician | 34 (15.0%) |
| Cardiologist | 32 (14.2%) |
| Geneticist | 14 (6.2%) |
Eighty-two participants (36.3%) reported discussing parenthood with a medical provider, most commonly an endocrinologist (25.7%), followed by a primary care doctor (19.9%), obstetrician (15.0%), cardiologist (14.2%), and geneticist (6.2%).
Speaking with a cardiologist had no significant effect on interest in routes to parenthood or fears about pregnancy-associated health risks. Speaking with a medical provider had no significant effect on interest in routes to parenthood, but did demonstrate a significant effect on the odds of reporting feeling afraid pregnancy could have a negative influence on their heart. Specifically, those who spoke with a medical provider (compared to those who did not) had (1) twice as high odds of being afraid of a negative influence on their heart (log(odds) = 0.72, SE = 0.261, t = 2.737); (2) 1.7 times higher odds of being afraid of a negative influence on their aorta (log(odds) = 0.55, SE = 0.259, t = 2.122); and (3) 2.1 times higher odds of being afraid of negative effects on their health overall (log(odds) = 0.73, SE = 0.260, t = 2.806).
Discussion
In our study, we investigated the attitudes towards parenthood in a cohort of 226 individuals with Turner syndrome ascertained through an advocacy organization and independent Facebook groups. The findings demonstrated a strong interest in parenthood in the Turner syndrome community. Approximately 25% of our cohort were already parents, and among those who are not parents, 68.5% expressed a desire to be a parent and 15.8% were unsure. While different paths to parenthood were experienced or desired by participants, adoption was the approach most favored by those who are interested in becoming a parent. Many factors played a role in decisions about parenthood, including participant age, time required for a route to parenthood, health-related pregnancy risks, risks to future children, and desire to experience pregnancy or have a biological child.
In our cohort, the rates of pregnancy and adoption were similar among parents, but adoption was the approach most favored by those who are interested in becoming a parent. Interest in adoption correlated with a fear that pregnancy could have a negative influence on their heart and aorta and 62% of the cohort reported that fear for their health was a factor influencing their approach to parenthood. Compared to a previous study by van Hagen et al. (2017) on concerns related to cardiovascular complications during pregnancy, our participants were more worried about pregnancy-related cardiovascular risks (71% vs 58%). These results emphasize the importance of patient-provider communication about individualized risk for poor pregnancy outcomes (Gravholt et al. 2017). Furthermore, despite strong interest in adoption, only 11.9% of the overall cohort had successfully adopted and 19.3% were currently pursuing adoption. While not explored in the current study, there may be obstacles to adoption that could be mitigated with additional supports.
It seemed inconsistent that those who cited the amount of time required for a route to parenthood influenced their approach were more likely to have an interest in adoption or surrogacy. This may reflect a knowledge gap about the time required for adoption or surrogacy. Additionally, interest in IVF and surrogacy demonstrated a statistically significant association. This may potentially be due to a desire to use one’s own oocytes and have a surrogate to carry the pregnancy.
Similar interest levels in pregnancy and IVF may be reflective of participant knowledge that IVF may be necessary for conception in this population given high rates of ovarian failure (Modi 2003). A desire to experience pregnancy and to have a biological child both had a signification association with interest in pregnancy. Overall, 53% of participants reported that a desire for a biological child was influencing their approach to parenthood and 59% desired carrying a pregnancy. As ovarian tissue and oocyte cryopreservation technology advances for those with Turner syndrome, fulfilling this desire for a biological child may become more feasible (Gravholt et al. 2019; Jeve et al. 2019; Kristensen and Andersen 2018). With monitoring and care from an interdisciplinary team, pregnancy may be as well (Calanchini et al. 2020; Donadille et al. 2019). Compared with a similarly sized cohort reported by Hadnott et al. (2011), our cohort included nearly four times (12.4% vs 3.2%) more individuals who had experienced pregnancy, which could be due to sampling bias and/or reflect changes in practice and advancements in the multidisciplinary care of these individuals over the past decade.
Participants most often discussed parenthood with friends and parents or guardians. Only about one-third of participants reported discussing their approach to parenthood with a medical provider, most often an endocrinologist. Speaking with a medical provider was significantly correlated with fear that pregnancy could have a negative influence on the heart or aorta. These findings highlight not only the need for education for and by providers, but also the important role that family and friends play in the decision-making process.
Future research
Future research directions may include a study of barriers to the adoption process for those with Turner syndrome given the strong interest within this cohort and disproportionately low rates of adoption. Exploration of the impact of financial barriers on attitudes towards routes to parenthood may also be informative. Informational resources about adoption targeted towards individuals with Turner syndrome may be appropriate. Future research into interest in oocyte cryopreservation in an adolescent population will have utility as these options become more readily available (Jeve et al. 2019; Kristensen and Andersen 2018; Oktay et al. 2016).
Limitations
The study cohort was relatively homogenous and therefore may not be generalizable to a more racially and ethnically diverse population with Turner syndrome. We recruited a sample of convenience through a patient advocacy organization and Turner syndrome Facebook groups which may lead to sampling bias. Clinical information obtained for this study was self-reported and not verified by review of medical records. Many participants could not recall or did not know their karyotype, limiting our ability to analyze results by karyotype. Lastly, it is possible that survey responses were influenced by the introduction of topics in the survey questions themselves and may not reflect previously held perspectives.
Conclusion
In summary, members of the Turner syndrome community have a strong interest in parenthood and consider multiple paths to achieve that goal. Individuals weigh many factors when considering options for parenthood including age, time demands, and the potential for poor health and pregnancy outcomes. A greater understanding of a patient’s attitudes towards parenthood will assist providers in counseling and facilitating informed decision-making surrounding options for parenthood.
Acknowledgements
This study was completed in partial fulfillment of the requirements of the first author’s Master of Science degree in Genetic Counseling from MGH Institute of Health Professions. The authors would like to extend a thank you to all survey participants and the Turner Syndrome Society of the United States for their support in our recruitment efforts.
Author contribution
All authors contributed to the study and survey design. Data collection was performed by Erin Falsey with recruitment assistance from the Turner Syndrome Society of the United States (TSSUS). Data analysis was performed by Erin Falsey. The first draft of the manuscript was written by Erin Falsey with critical feedback from Allison Cirino and Angela Lin. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Declarations
Ethics approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Human subject approval was obtained from Mass General Brigham Institutional Review Board (Protocol #: 2020P002140).
Informed consent
Informed consent was obtained from all study participants.
Animal studies
No non-human animal studies were carried out by the authors for this article.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Bernard V, Donadille B, Zenaty D, Courtillot C, Salenave S, Brac de la Perrière A, Albarel F, Fèvre A, Kerlan V, Brue T, Delemer B, Borson-Chazot F, Carel J-C, Chanson P, Léger J, Touraine P, Christin-Maitre S. Spontaneous fertility and pregnancy outcomes amongst 480 women with Turner syndrome. Hum Reprod. 2016;31(4):782–788. doi: 10.1093/humrep/dew012. [DOI] [PubMed] [Google Scholar]
- Birkebaek N, Crüger D, Hansen J, Nielsen J, Bruun-Petersen G. Fertility and pregnancy outcome in Danish women with Turner syndrome: Turner syndrome and fertility. Clin Genet. 2002;61(1):35–39. doi: 10.1034/j.1399-0004.2002.610107.x. [DOI] [PubMed] [Google Scholar]
- Bodri D, Vernaeve V, Figueras F, Vidal R, Guillén JJ, Coll O. Oocyte donation in patients with Turner’s syndrome: a successful technique but with an accompanying high risk of hypertensive disorders during pregnancy. Hum Reprod. 2006;21(3):829–832. doi: 10.1093/humrep/dei396. [DOI] [PubMed] [Google Scholar]
- Bryman I, Sylvén L, Berntorp K, Innala E, Bergström I, Hanson C, Oxholm M, Landin-Wilhelmsen K. Pregnancy rate and outcome in Swedish women with Turner syndrome. Fertil Steril. 2011;95(8):2507–2510. doi: 10.1016/j.fertnstert.2010.12.039. [DOI] [PubMed] [Google Scholar]
- Calanchini M, Aye CYL, Orchard E, Baker K, Child T, Fabbri A, Mackillop L, Turner HE. Fertility issues and pregnancy outcomes in Turner syndrome. Fertil Steril. 2020;114(1):144–154. doi: 10.1016/j.fertnstert.2020.03.002. [DOI] [PubMed] [Google Scholar]
- Chevalier N, Letur H, Lelannou D, Ohl J, Cornet D, Chalas-Boissonnas C, Frydman R, Catteau-Jonard S, Greck-Chassain T, Papaxanthos-Roche A, Dulucq M.-C, Couet M.-L, Cédrin-Durnerin I, Pouly J.-L, Fénichel P, & the French Study Group for Oocyte Donation. (2011). Materno-fetal cardiovascular complications in turner syndrome after oocyte donation: insufficient prepregnancy screening and pregnancy follow-up are associated with poor outcome. J Clin Endocrinol Metab 96(2), E260–E267. 10.1210/jc.2010-0925 [DOI] [PubMed]
- Donadille B, Bernard V, Christin-Maitre S. How can we make pregnancy safe for women with Turner syndrome? Am J Med Genet C Semin Med Genet. 2019;181(1):34–41. doi: 10.1002/ajmg.c.31682. [DOI] [PubMed] [Google Scholar]
- Gravholt CH, Landin-Wilhelmsen K, Stochholm K, Eilersen Hjerrild B, Ledet T, Born Djurhuus C, Sylvén L, Baandrup U, Østergaard Kristensen B, Sandahl Christiansen J. Clinical and epidemiological description of aortic dissection in Turner’s syndrome. Cardiol Young. 2006;16(5):430–436. doi: 10.1017/S1047951106000928. [DOI] [PubMed] [Google Scholar]
- Gravholt CH, Andersen NH, Conway GS, Dekkers OM, Geffner ME, Klein KO, Lin AE, Mauras N, Quigley CA, Rubin K, Sandberg DE, Sas TCJ, Silberbach M, Söderström-Anttila V, Stochholm K, van Alfen-van derVelden JA, Woelfle J, Backeljauw PF. Clinical practice guidelines for the care of girls and women with Turner syndrome: proceedings from the 2016 Cincinnati International Turner Syndrome Meeting. Eur J Endocrinol. 2017;177(3):G1–G70. doi: 10.1530/EJE-17-0430. [DOI] [PubMed] [Google Scholar]
- Gravholt CH, Viuff MH, Brun S, Stochholm K, Andersen NH. Turner syndrome: mechanisms and management. Nat Rev Endocrinol. 2019;15(10):601–614. doi: 10.1038/s41574-019-0224-4. [DOI] [PubMed] [Google Scholar]
- Gravholt CH, Tartaglia N, Disteche C. Sex chromosome aneuploidies in 2020-the state of care and research in the world. Am J Med Genet C: Semin Medical Genet. 2020;184(2):197–201. doi: 10.1002/ajmg.c.31808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grewal J, Valente AM, Egbe AC, Wu FM, Krieger EV, Sybert VP, van Hagen IM, Beauchesne LM, Rodriguez FH, Broberg CS, John A, Bradley EA, Roos-Hesselink JW. Cardiovascular outcomes of pregnancy in Turner syndrome. Heart. 2021;107(1):61–66. doi: 10.1136/heartjnl-2020-316719. [DOI] [PubMed] [Google Scholar]
- Hadnott TN, Gould HN, Gharib AM, Bondy CA. Outcomes of spontaneous and assisted pregnancies in Turner syndrome: the U.S. National Institutes of Health experience. Fertil Steril. 2011;95(7):2251–2256. doi: 10.1016/j.fertnstert.2011.03.085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeve YB, Gelbaya T, Fatum M (2019) Time to consider ovarian tissue cryopreservation for girls with Turner’s syndrome: an opinion paper. Hum Reprod Open 2019(3): hoz016. 10.1093/hropen/hoz016 [DOI] [PMC free article] [PubMed]
- Kristensen SG, Andersen CY. Cryopreservation of ovarian tissue: opportunities beyond fertility preservation and a positive view into the future. Front Endocrinol. 2018;9:347. doi: 10.3389/fendo.2018.00347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercadal BA, Imbert R, Demeestere I, Englert Y, Delbaere A. Pregnancy outcome after oocyte donation in patients with Turner’s syndrome and partial X monosomy. Hum Reprod. 2011;26(8):2061–2068. doi: 10.1093/humrep/der166. [DOI] [PubMed] [Google Scholar]
- Modi DN. Accelerated germ cell apoptosis in sex chromosome aneuploid fetal human gonads. Mol Hum Reprod. 2003;9(4):219–225. doi: 10.1093/molehr/gag031. [DOI] [PubMed] [Google Scholar]
- Oktay K, Bedoschi G, Berkowitz K, Bronson R, Kashani B, McGovern P, Pal L, Quinn G, Rubin K. Fertility preservation in women with turner syndrome: a comprehensive review and practical guidelines. J Pediatr Adolesc Gynecol. 2016;29(5):409–416. doi: 10.1016/j.jpag.2015.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RStudio Team (2020). RStudio: integrated development for R. RStudio, PBC, Boston, MAhttp://www.rstudio.com/
- Silberbach M, Roos-Hesselink JW, Andersen NH, Braverman AC, Brown N, Collins RT, De Backer J, Eagle KA, Hiratzka LF, Johnson WH, Kadian-Dodov D, Lopez L, Mortensen KH, Prakash SK, Ratchford EV, Saidi A, van Hagen I, Young LT, & On behalf of the American Heart Association Council on Cardiovascular Disease in the Young; Council on Genomic and Precision Medicine; and Council on Peripheral Vascular Disease (2018) Cardiovascular health in Turner syndrome: a scientific statement from the American Heart Association. Circulation: Genomic and Precis Med 11(10). 10.1161/HCG.0000000000000048 [DOI] [PubMed]
- Sutton EJ, McInerney-Leo A, Bondy CA, Gollust SE, King D, Biesecker B. Turner syndrome: four challenges across the lifespan. Am J Med Genet A. 2005;139A(2):57–66. doi: 10.1002/ajmg.a.30911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hagen IM, Duijnhouwer AL, Ten Kate-Booij MJ, Dykgraaf RHM, Duvekot JJ, Utens EMWJ, Roos-Hesselink JW. Wish to conceive and concerns to develop cardiovascular complications during pregnancy in patients with Turner syndrome. J Psychosom Obstet Gynecol. 2017;38(1):45–52. doi: 10.1080/0167482X.2016.1216961. [DOI] [PubMed] [Google Scholar]