This cross-sectional study examines the association between self-reported health-related social needs and acute care utilization among older adults enrolled in Medicare Advantage.
Key Points
Question
To what extent are self-reported health-related social needs (HRSNs) associated with acute care utilization among older adults enrolled in Medicare Advantage, and are there specific HRSNs that seem to matter more?
Findings
In this cross-sectional study of 56 155 older adults enrolled in Medicare Advantage, HRSNs were associated with statistically significantly higher rates of acute care utilization, with the largest association observed for avoidable hospital stays (53.3% increase). Unreliable transportation had the largest association with hospital stays and emergency department visits (marginal effects of 51.2 and 95.5 events per 1000 beneficiaries, respectively).
Meaning
Among older adults enrolled in Medicare Advantage, self-reported HRSNs are associated with increased rates of acute care utilization.
Abstract
Importance
There is increased focus on identifying and addressing health-related social needs (HRSNs). Understanding how different HRSNs relate to different health outcomes can inform targeted, evidence-based policies, investments, and innovations to address HRSNs.
Objective
To examine the association between self-reported HRSNs and acute care utilization among older adults enrolled in Medicare Advantage.
Design, Setting, and Participants
This cross-sectional study used data from a large, national survey of Medicare Advantage beneficiaries to identify the presence of HRSNs. Survey data were linked to medical claims, and regression models were used to estimate the association between HRSNs and rates of acute care utilization from January 1, 2019, through December 31, 2019.
Exposures
Self-reported HRSNs, including food insecurity, financial strain, loneliness, unreliable transportation, utility insecurity, housing insecurity, and poor housing quality.
Main Outcomes and Measures
All-cause hospital stays (inpatient admissions and observation stays), avoidable hospital stays, all-cause emergency department (ED) visits, avoidable ED visits, and 30-day readmissions.
Results
Among a final study population of 56 155 Medicare Advantage beneficiaries (mean [SD] age, 74.0 [5.8] years; 32 779 [58.4%] women; 44 278 [78.8%] White; and 7634 [13.6%] dual eligible for Medicaid), 27 676 (49.3%) reported 1 or more HRSNs. Health-related social needs were associated with statistically significantly higher rates of all utilization measures, with the largest association observed for avoidable hospital stays (incident rate ratio for any HRSN, 1.53; 95% CI, 1.35-1.74; P < .001). Compared with beneficiaries without HRSNs, beneficiaries with an HRSN had a 53.3% higher rate of avoidable hospitalization (incident rate ratio, 1.53; 95% CI, 1.35-1.74; P < .001). Financial strain and unreliable transportation were each independently associated with increased rates of hospital stays (marginal effects of 26.5 [95% CI, 14.2-38.9] and 51.2 [95% CI, 30.7-71.8] hospital stays per 1000 beneficiaries, respectively). All HRSNs, except for utility insecurity, were independently associated with increased rates of ED visits. Unreliable transportation had the largest association with increased hospital stays and ED visits, with marginal effects of 51.2 (95% CI, 30.7-71.8) and 95.5 (95% CI, 65.3-125.8) ED visits per 1000 beneficiaries, respectively. Only unreliable transportation and financial strain were associated with increased rates of 30-day readmissions, with marginal effects of 3.3% (95% CI, 2.0%-4.0%) and 0.4% (95% CI, 0.2%-0.6%), respectively.
Conclusions and Relevance
In this cross-sectional study of older adults enrolled in Medicare Advantage, self-reported HRSNs were common and associated with statistically significantly increased rates of acute care utilization, with variation in which HRSNs were associated with different utilization measures. These findings provide evidence of the unique association between certain HRSNs and different types of acute care utilization, which could help refine the development and targeting of efforts to address HRSNs.
Introduction
There is growing recognition of the consequences that upstream social factors have on downstream health outcomes.1 Within the Medicare program—where health-related social needs (HRSNs) such as food insecurity, financial strain, and unreliable transportation are estimated to affect roughly half of beneficiaries—policy makers, payers, and delivery organizations are increasingly investing in efforts to identify and address HRSNs.2,3,4,5 In 2016, the Centers for Medicare & Medicaid Services (CMS) launched the Accountable Health Communities (AHC) program to incentivize organizations to identify Medicare beneficiaries with unmet HRSNs and connect them to community resources.6,7 Outside of the AHC program, many delivery organizations participating in Medicare’s value-based payment models, such as accountable care organizations (ACOs), have been seeking to address HRSNs with the goal of improving health outcomes and reducing costs for their attributed populations.8,9 Within the Medicare Advantage program, plans may use new regulatory flexibility to directly address beneficiaries’ unmet HRSNs through supplemental benefits, and CMS may soon measure their ability to collect self-reported HRSN data.10,11
As more attention, investment, and innovation are directed toward addressing HRSNs, it is important that efforts are focused on the right priorities. Although prior research has linked specific HRSNs to specific health outcomes, the comparative and independent relationship between different, and often co-occurring, HRSNs on health outcomes among older adults is limited.12,13,14,15,16 A better understanding of how different HRSNs affect various outcomes can help support policy makers, payers, and delivery organizations in developing targeted, evidence-based, and financially sustainable programs to identify and address HRSNs.
Using data from a large national survey linked to medical claims, we sought to answer 3 questions. First, to what extent are the presence and burden of self-reported HRSNs associated with acute care utilization among older adults enrolled in Medicare Advantage? Second, does the association between HRSNs and acute care utilization differ for events that are potentially avoidable? Finally, are there specific self-reported HRSNs that are independently associated with acute care utilization?
Methods
Setting and Participants
This study population was drawn from a national sample of Medicare Advantage beneficiaries who responded to a survey of HRSNs conducted from October 16, 2019, through February 29, 2020. Additional detail on the survey has been previously published2 and is available in the eMethods in the Supplement. The survey was adapted from the CMS AHC HRSN Screening Tool6,7 and administered to 431 215 noninstitutionalized Medicare Advantage beneficiaries enrolled in plans offered by Humana Inc. We limited the sample to beneficiaries who completed the full survey, were not contractually excluded from research, and were continuously enrolled from January 1, 2019, to December 31, 2019. Because our focus was on older adults, we excluded beneficiaries who were younger than 65 years.
This study was reviewed by the Humana Healthcare Research Human Subject Protection Office and deemed exempt from approval because it used all publicly available, deidentified data. We followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for cross-sectional studies.
Measures
Health-Related Social Needs
The survey assessed the presence of 7 HRSNs: (1) food insecurity, (2) financial strain, (3) loneliness, (4) unreliable transportation, (5) utility insecurity, (6) housing insecurity, and (7) poor housing quality. Survey responses were used to construct binary indicators for the presence of each of the 7 HRSNs, the presence of any HRSN, and a count of all reported HRSNs (see the eMethods in the Supplement for additional detail).
Participant Characteristics
For each beneficiary, we extracted age, sex, race and ethnicity, Medicare-Medicaid dual eligibility status, and Social Security disability status from enrollment files. Race and ethnicity were assessed according to the CMS beneficiary race and ethnicity codes and categorized as Black, White, other (including Asian, Hispanic, North American Native, and other race or ethnicity), and unknown owing to inaccuracies in classification for non-White and non-Black beneficiaries. Demographic characteristics were assessed as of December 31, 2019. Using the primary address during the survey period, we classified beneficiary residence according to US Census geographic region, zip code level population density, and Dartmouth Atlas of Health Care hospital referral region (HRR). We calculated the Elixhauser Comorbidity Index17,18,19 score for each participant using claims from January 1, 2019, through December 31, 2019.
Utilization
Utilization measures included inpatient admissions, observation stays, emergency department (ED) visits, and all-cause 30-day inpatient readmissions. We classified inpatient hospitalizations and observations stays together as hospital stays. All utilization measures were assessed using medical claims from January 1, 2019, through December 31, 2019.
We segmented hospital stays and ED visits into all-cause and potentially avoidable (hereafter referred to as avoidable) events under the hypothesis that HRSNs may have a disproportionate influence on avoidable utilization. Avoidable hospital stays were defined using the Agency for Healthcare Research and Quality Prevention Quality Indicators definition.20 Avoidable ED visits were defined using the New York University ED visit algorithm21,22,23 (see the eMethods in the Supplement for additional detail).
Statistical Analysis
We compared demographic and clinical characteristics between beneficiaries who reported any HRSN and those who reported no HRSNs using standardized mean differences, of which those greater than 0.25 were considered meaningful.24 We then calculated unadjusted rates of avoidable and all-cause hospital stays and ED visits, as well as 30-day readmissions, and compared these rates using t tests.
To estimate the association between HRSNs and all-cause hospital stays, avoidable hospital stays, all-cause ED visits, and avoidable ED visits, we constructed a series of negative binomial regression models that adjusted for age, sex, race and ethnicity, disability status, dual eligibility, and Elixhauser Comorbidity Index score, with HRR fixed effects. First, we estimated the association between the presence of any HRSN and acute care utilization. For each measure, we calculated the incidence rate ratio (IRR) associated with the presence of any HRSN (compared with no HRSNs), which allowed us to compare the magnitude of associations across utilization measures. Second, we estimated the association between cumulative HRSN burden and utilization. For this analysis, HRSN burden was capped at 5 to simplify the number of comparisons, to balance group size at the upper end of HRSN burden, and with the assumption that incremental needs would be less meaningful at high levels of HRSN burden. To enable comparison across groups, we calculated the IRR for different levels of HRSN burden (ie, 1, 2, 3, 4, or ≥5 HRSNs) on utilization measures, all compared with no HRSNs. Finally, we estimated the association between individual HRSNs and utilization. To account for the co-occurrence of multiple HRSNs, the main analysis included indicators for each of the 7 HRSNs in the regression model. Prior to including all HRSNs in the regression model, we checked for correlation between individual HRSNs. We also performed a series of regressions where each of the 7 HRSNs were modeled separately, still adjusting for the patient-level characteristics noted above. To aid interpretability, we calculated and report the marginal effect of HRSNs on utilization rates per 1000 beneficiaries. To estimate the association between HRSNs and 30-day readmissions, we performed a similar series of regressions but used logistic regression models.
Analyses were performed using SAS Enterprise Guide, version 8.3 (SAS Institute), from March 2021 to February 2022. All hypothesis tests were 2-sided, with P < .05 indicating significance.
Results
Study Population and Baseline Characteristics
There were 105 901 respondents and 325 575 nonrespondents to the HRSN survey (response rate of 24.5%). Among the respondents, 79 848 (75.4%) completed the full survey. Demographic and clinical characteristics were similar across survey respondents and nonrespondents and, among respondents, across survey completers and noncompleters (eTable 1 in the Supplement). After exclusions, the final study population included 56 155 beneficiaries (see eFigure in the Supplement for a depiction of participant flow through the study). Among the final study population, the mean (SD) age was 74.0 (5.8) years, 32 779 (58.4%) were women, 44 278 (78.8%) were White, 9651 (17.2%) were disabled, and 7634 (13.6%) were dually eligible for Medicare and Medicaid.
Among the final study population, 27 676 (49.3%) beneficiaries reported at least 1 HRSN. The most commonly reported HRSNs were financial strain, food insecurity, and poor housing quality. Table 124 compares demographic and clinical characteristics between beneficiaries reporting any HRSN and those reporting no HRSNs. Beneficiaries with HRSNs were more likely to be Black, dual eligible, and disabled, and had a higher burden of comorbidities. Although beneficiaries with HRSNs were more likely to be dual eligible and disabled, the majority of beneficiaries with HRSNs were neither dual eligible nor disabled. Beneficiaries with and without HRSNs were similar with respect to age, sex, and the region and population density of their residence. Financial strain and food insecurity were moderately correlated (ɸ = 0.50), with all other HRSN combinations weakly correlated (ɸ = 0.07-0.27) (eTable 2 in the Supplement).
Table 1. Baseline Characteristics of the Study Population.
| Characteristic | No. (%) | SMDa | ||
|---|---|---|---|---|
| Overall | Any HRSN | No HRSN | ||
| Total No. | 56 155 | 27 676 | 28 479 | NA |
| Age, mean (SD), y | 73.99 (5.84) | 73.57 (5.87) | 74.40 (5.78) | .14 |
| Sex | ||||
| Female | 32 779 (58.4) | 17 142 (61.9) | 15 637 (54.9) | .14 |
| Male | 23 376 (41.6) | 10 534 (38.1) | 12 842 (45.1) | .14 |
| Race and ethnicityb | ||||
| Black | 9135 (16.3) | 5995 (21.7) | 3140 (11.0) | .29 |
| White | 44 278 (78.8) | 20 230 (73.1) | 24 048 (84.4) | .28 |
| Other | 1996 (3.6) | 1145 (4.1) | 851 (3.0) | .06 |
| Unknown | 746 (1.3) | 306 (1.1) | 440 (1.5) | .04 |
| Geographic region | ||||
| Northeast | 1703 (3.0) | 902 (3.3) | 801 (2.8) | .03 |
| Midwest | 12 915 (23.0) | 5918 (21.4) | 6997 (24.6) | .08 |
| South | 33 866 (60.3) | 17 283 (62.4) | 16 583 (58.2) | .09 |
| West | 7671 (13.7) | 3573 (12.9) | 4098 (14.4) | .04 |
| Population density | ||||
| Urban | 34 919 (62.2) | 17 025 (61.5) | 17 894 (62.8) | .03 |
| Suburban | 13 980 (24.9) | 6865 (24.8) | 7115 (25.0) | .004 |
| Rural | 6050 (10.8) | 3228 (11.7) | 2822 (9.9) | .06 |
| Unknown | 1206 (2.1) | 558 (2.0) | 648 (2.3) | .02 |
| Dual Medicare and Medicaid eligible | 7634 (13.6) | 5830 (21.1) | 1804 (6.3) | .44 |
| Social Security disability eligible | 9651 (17.2) | 6691 (24.2) | 2960 (10.4) | .37 |
| Elixhauser Comorbidity Index score, mean (SD) | 2.94 (2.62) | 3.36 (2.78) | 2.53 (2.38) | .32 |
| HRSN burden | ||||
| 0 | NA | NA | 28 479 (100.0) | NA |
| 1 | NA | 13 553 (49.0) | NA | NA |
| 2 | NA | 7240 (26.2) | NA | NA |
| 3 | NA | 3948 (14.3) | NA | NA |
| 4 | NA | 1838 (6.6) | NA | NA |
| ≥5 | NA | 1097 (4.0) | NA | NA |
| Individual HRSNs | ||||
| Financial strain | NA | 18 544 (67.0) | NA | NA |
| Food insecurity | NA | 10 134 (36.6) | NA | NA |
| Poor housing quality | NA | 9765 (35.3) | NA | NA |
| Utility insecurity | NA | 5007 (18.1) | NA | NA |
| Unreliable transportation | NA | 3729 (13.5) | NA | NA |
| Housing insecurity | NA | 3134 (11.3) | NA | NA |
| Loneliness | NA | 2785 (10.1) | NA | NA |
Abbreviations: HRSN, health-related social need; NA, not applicable; SMD, standardized mean difference.
SMDs greater than 0.25 were considered to be meaningful.24
Race and ethnicity were assessed according to the Centers for Medicare & Medicaid Services beneficiary race and ethnicity codes, which reflect data reported to the Social Security Administration. The Other category includes Asian, Hispanic, North American Native, and other races or ethnicities.
HRSN Burden and Acute Care Utilization
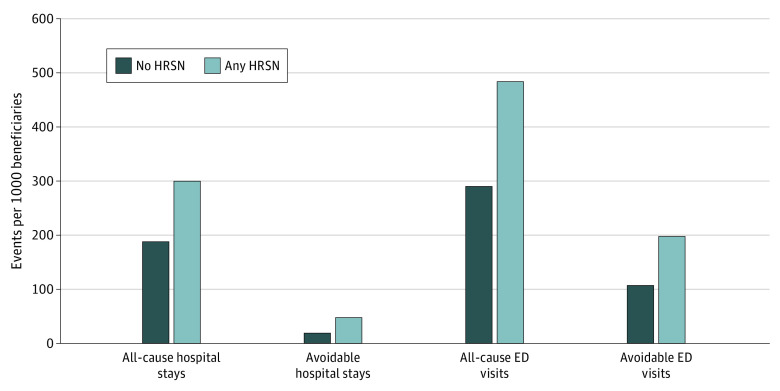
Figure 120,21,22 presents unadjusted rates of hospital stays and ED visits for beneficiaries with and without HRSNs. Beneficiaries with HRSNs vs those without had statistically significantly higher rates of all-cause hospital stays (299.7 vs 188.0 per 1000 beneficiaries; P < .001), avoidable hospital stays (47.7 vs 19.1; P < .001), all-cause ED visits (483.4 vs 290.1; P < .001), and avoidable ED visits (197.5 vs 107.1; P < .001).
Figure 1. Unadjusted Rates of Acute Care Utilization by Presence of Health-Related Social Needs (HRSNs).
Hospital stays are an aggregate of inpatient admissions and observation stays. Avoidable hospital stays were defined using the Agency for Healthcare Research and Quality Prevention Quality Indicators definition.20 Avoidable emergency department (ED) visits were defined using the New York University ED visit algorithm and subsequent algorithm patch.21,22 All differences between beneficiaries with and without HRSNs across the 4 categories were statistically significant, with P values <.001.
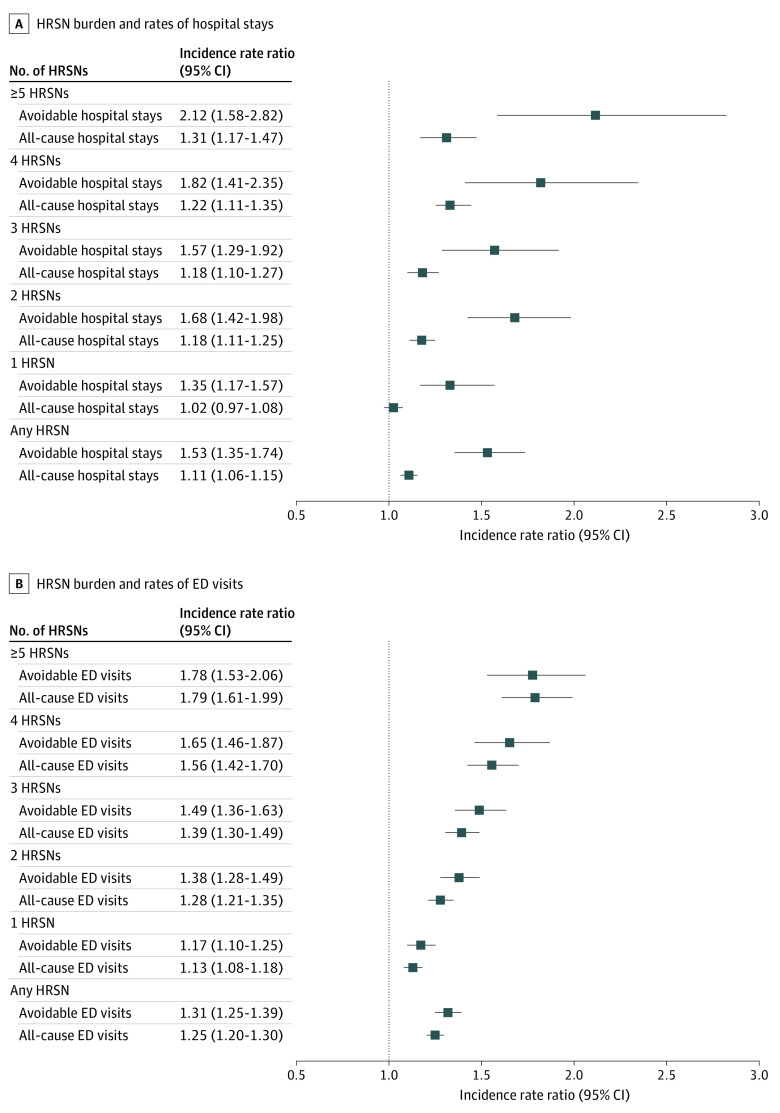
In adjusted analyses, the presence of any HRSN was statistically significantly associated with increased rates of all utilization measures (Figure 220,21,22). The magnitude of the association varied by measure, with the largest association observed for avoidable hospital stays. Compared with beneficiaries without any HRSN, beneficiaries with HRSNs had 53.3% higher rates of avoidable hospitalizations (IRR, 1.53; 95% CI, 1.35-1.74; P < .001) and 32.0% higher rates of avoidable ED visits (IRR, 1.32; 95% CI, 1.25-1.39; P < .001). The association between the presence of any HRSN and increased rates of all-cause ED visits (IRR, 1.25; 95% CI, 1.20-1.30; P < .001) was larger than that for all-cause hospital stays (IRR, 1.11; 95% CI, 1.06-1.15; P < .001).
Figure 2. Association Between Health-Related Social Need (HRSN) Burden and Rates of Hospital Stays or Emergency Department (ED) Visits.
Incident rate ratios are calculated from negative binomial regression models estimating the association between HRSNs and utilization measures. Models adjust for age, sex, race and ethnicity, disability status, dual eligibility status, and Elixhauser Comorbidity Index score, with hospital referral region fixed effects. For all incident rate ratios, the reference population is beneficiaries with no HRSNs. Hospital stays were an aggregate of inpatient admissions and observation stays. Avoidable hospital stays were defined using the Agency for Healthcare Research and Quality Prevention Quality Indicators definition.20 Avoidable ED visits were defined using the New York University ED visit algorithm and subsequent algorithm patch.21,22
Also shown in Figure 2 are the associations between different levels of HRSN burden and acute care utilization. A dose-response trend was observed for all measures, with increasing HRSN burden associated with higher rates of utilization, though the differences observed at higher levels of HRSN burden (eg, 2 HRSNs compared with 3, 4, or ≥5 HRSNs) were not statistically significant. The association between increasing HRSN burden and increased rates of utilization was largest for avoidable hospital stays.
Compared with beneficiaries without any HRSNs, beneficiaries with HRSNs had statistically significantly higher rates of 30-day readmissions (9.5% vs 19.2% per 1000 beneficiaries; P < .001). When adjusted for beneficiary characteristics, the association between the presence of any HRSN and odds of 30-day readmission was not statistically significant. Full regression results are provided in eTable 3 in the Supplement.
Individual HRSNs and Acute Care Utilization
The associations between individual HRSNs and hospital stays and ED visits are summarized in Table 2.20,21,22 Financial strain and unreliable transportation were each associated with increased rates of all-cause and avoidable hospital stays. Among all-cause hospital stays, unreliable transportation had the largest association, with a marginal effect of 51.2 (95% CI, 30.7-71.8) hospital stays per 1000 beneficiaries. Among avoidable hospital stays, financial strain had the largest association, with a marginal effect of 14.7 (95% CI, 9.4-20.0) avoidable hospital stays per 1000 beneficiaries. All HRSNs except for utility insecurity were associated with statistically significantly increased rates of all-cause ED visits. Similar to hospital stays, unreliable transportation had the largest association for all-cause ED visits, with a marginal effect of 95.5 (95% CI, 65.3-125.8) ED visits per 1000 beneficiaries. Unlike hospital stays, loneliness had a large and statistically significant association with all-cause ED visits (marginal effect of 80.6 [95% CI, 46.9-114.3] ED visits per 1000 beneficiaries). The patterns of associations between individual HRSNs and avoidable ED visits were similar to all-cause ED visits, with the exception of housing insecurity, which was not associated with increased rates of avoidable ED visits. In analyses that modeled each individual HRSN separately, housing insecurity and food insecurity were also associated with all-cause and avoidable hospital stays, and all HRSNs were associated with all-cause and avoidable ED visits (eTable 4 in the Supplement). Only unreliable transportation and financial strain were statistically significantly associated with 30-day readmission rates, with marginal effects of 3.3% (95% CI, 2.0%-4.0%) and 0.4% (95% CI, 0.2%-0.6%), respectively.
Table 2. Association Between Individual Health-Related Social Needs (HRSNs) and Rates of Hospital Stays and Emergency Department (ED) Visits.
| HRSN | Marginal effect of HRSN on rates of utilization per 1000 beneficiaries (95% CI)a | |||
|---|---|---|---|---|
| Hospital stays | ED visits | |||
| All causeb | Avoidablec | All cause | Avoidabled | |
| Food insecurity | 11.9 (−2.9 to 26.7) | 2.0 (−4.1 to 8.2) | 50.9 (29.6 to 72.2)e | 20.8 (9.0 to 32.6)e |
| Financial strain | 26.5 (14.2 to 38.9)e | 14.7 (9.4 to 20.4)e | 37.6 (20.5 to 54.8)e | 18.6 (8.9 to 28.3)e |
| Loneliness | 7.1 (−13.7 to 27.9) | 1.8 (−6.9 to 10.5) | 80.6 (46.9 to 114.3)e | 44.4 (25.1 to 63.8)e |
| Unreliable transportation | 51.2 (30.7 to 71.8)e | 10.9 (2.2 to 19.5)e | 95.5 (65.3 to 125.8)e | 26.8 (10.9 to 42.6)e |
| Utility insecurity | −6.5 (−23.0 to 10.0) | −0.4 (−7.4 to 6.7) | 11.6 (−12.1 to 35.3) | 6.0 (−7.3 to 19.3) |
| Housing insecurity | 17.2 (−4.2 to 38.7) | 3.8 (−5.3 to 12.9) | 44.6 (13.7 to 75.6)e | 7.1 (−9.3 to 23.6) |
| Poor housing quality | −7.3 (−20.2 to 5.7) | 1.6 (−4.2 to 7.3) | 20.4 (1.8 to 39.1)e | 17.2 (6.5 to 27.8)e |
Calculated from negative binomial regression models estimating the association between individual HRSNs and utilization measures. Models adjust for age, sex, race and ethnicity, disability status, dual eligibility status, Elixhauser Comorbidity Index score, and all other individual HRSNs, with hospital referral region fixed effects. The reference group for all marginal effects is beneficiaries not reporting that specific HRSN.
Hospital stays are an aggregate of inpatient admissions and observation stays.
Avoidable hospital stays were defined using the Agency for Healthcare Research and Quality Prevention Quality Indicators definition.20
Avoidable ED visits were defined using the New York University ED visit algorithm and subsequent algorithm patch.21,22
Statistical significance at the P < .05 level.
Discussion
In this study of older adults enrolled in Medicare Advantage, we found that self-reported HRSNs were common and associated with statistically significantly increased rates of acute care utilization. As policy makers, payers, and delivery organizations increase investments to identify and address HRSNs, several of the present findings have important implications.
First, we found that HRSNs were widespread, with roughly half of Medicare Advantage beneficiaries reporting at least 1 HRSN. Although HRSNs were more common among dual-eligible and disabled beneficiaries, the majority of Medicare Advantage beneficiaries with HRSNs were neither dual eligible nor disabled. These findings support efforts by CMS, Medicare Advantage plans, and care delivery organizations to achieve population-level screening for HRSNs among all older adults and to underscore the need to address HRSNs in the broader Medicare program, not just among specific groups of high-need patients.11,25,26 Notwithstanding the need for broadly focused efforts, the disproportionate burden of HRSNs among specific racial and socioeconomic subgroups of Medicare Advantage beneficiaries necessitates some focused initiatives to improve health equity.
Second, we found a statistically significant association between the presence of HRSNs and increased rates of acute care utilization, even after adjusting for clinical and demographic characteristics, including dual eligibility for Medicare and Medicaid. The independent association between HRSNs and acute care utilization supports a continued focus on HRSNs as a contributory driver of poor outcomes and avoidable health care utilization, and motivates experimentation with social risk adjustment for payment and quality measurement.11,27,28 It also raises the possibility that addressing HRSNs may lead to reductions in downstream utilization, possibly creating a sustainable financing model for investments by payers and risk-bearing delivery organizations to address HRSNs.29 Of course, the present findings represent associations between HRSNs and utilization and do not provide causal evidence that addressing HRSNs will reduce utilization. But this notion is supported by evidence that interventions targeting HRSNs can improve health outcomes and produce health care savings by reducing ED visits and hospitalizations.30
That we observed a statistically significant association between HRSNs and acute care utilization among older adults enrolled in Medicare Advantage is especially salient in light of recent efforts by Congress and CMS to give Medicare Advantage plans increased flexibility to directly address HRSNs through supplemental benefits.10 The uptake of these benefits has grown in recent years,31,32 and the present findings should support continued efforts by Medicare Advantage plans to design, offer, and evaluate the effect of supplemental benefits aimed at addressing HRSNs.
Third, we found that the magnitude of the association between HRSNs and utilization was largest for avoidable hospital stays. This finding has multiple possible interpretations, including that HRSNs may contribute to worse control of chronic conditions (eg, diabetes), resulting in preventable decompensations or otherwise treatable complications. It may also reflect findings from prior studies indicating that many patients with HRSNs also experience poor access to primary and preventive care.12,13,14,15,33 A better understanding of the mechanisms by which HRSNs mediate poor outcomes could help with the development and targeting of efforts to reduce avoidable hospitalizations.
Finally, there was considerable heterogeneity in the association between individual HRSNs and different measures of acute care utilization. Financial strain and unreliable transportation were each independently associated with increased rates of hospital stays. In contrast, almost all HRSNs studied were independently associated with increased ED use. Only financial strain and unreliable transportation were associated with increased odds of 30-day readmissions. Interestingly, some HRSNs that have been the subject of considerable interest and investment, such as food and housing insecurity,34,35 were not uniformly associated with increases in acute care utilization.
This complexity and heterogeneity will require payers and delivery organizations to make strategic and nuanced decisions about which HRSNs to screen for and address when attempting to improve health outcomes. For a program or initiative aimed at reducing readmissions, it may be appropriate to focus disproportionately on transportation and financial strain. Whereas efforts to address recurrent ED utilization may need to tackle a more expansive set of HRSNs. The consistent association between unreliable transportation and acute care utilization motivates specific attention to this HRSN, which has already been a focus of supplemental benefit offerings by MA plans31,32 and innovations within delivery organizations.36
Limitations
This study has several limitations. First, owing to the observational design, we were unable to directly assess the causal relationship between HRSNs and acute care utilization, and there is likely to be some bidirectional causality in that disease progression and acute care utilization could lead to an increased burden of HRSNs, just as HRSNs could lead to disease progression and acute care utilization. Second, we did not explore interaction effects between different HRSNs or between HRSNs and demographic characteristics. Third, the study population was restricted to older adults and reflects that of a single, albeit large and national, Medicare Advantage plan. As a result, the findings may not generalize to other Medicare populations. Fourth, we captured self-reported HRSNs at a single point in time and examined utilization in a period that largely preceded the survey; HRSNs can change over time, and their pattern of association with utilization may differ when considered prospectively. Fifth, the measurement of HRSNs was subject to survey nonresponse bias. Although we found no evidence of this on observable characteristics, we could not assess for nonresponse by the presence of HRSNs, so the results could undercount the true extent of HRSNs in the study population. Finally, the ascertainment of HRNSs was limited to those included in the survey which, while adapted from a widely used instrument, may assess HRSNs in a different manner or cover different HRSNs than other instruments.
Conclusions
In this cross-sectional study of older adults enrolled in Medicare Advantage plans offered by a large national insurer, self-reported HRSNs were common and associated with statistically significantly increased rates of acute care utilization, with variation in which HRSNs were associated with different types of utilization. These findings provide evidence of the unique association between certain HRSNs and acute care utilization, which could help refine the development and targeting of efforts to address these needs among older adults.
eMethods. Supplemental Methods
eTable 1. Comparison of Survey Respondents and Non-Respondents, and Survey Completers and Non-Completers
eTable 2. Correlation between Individual Health-Related Social Needs
eFigure. Participant Flow Through the Study
eTable 3. Complete Regression Results
eTable 4. Association between Individual Health-Related Social Needs and Rates of Hospital Stays and ED Visits, with Each HRSN Modeled Independently
References
- 1.National Academies of Sciences, Engineering, and Medicine . Integrating Social Care Into the Delivery of Health Care: Moving Upstream to Improve the Nation’s Health. The National Academies Press; 2019. [PubMed] [Google Scholar]
- 2.Long CL, Franklin SM, Hagan AS, et al. Health-related social needs among older adults enrolled in Medicare Advantage. Health Aff (Millwood). 2022;41(4):557-562. doi: 10.1377/hlthaff.2021.01547 [DOI] [PubMed] [Google Scholar]
- 3.Madden JM, Shetty PS, Zhang F, et al. Risk factors associated with food insecurity in the Medicare population. JAMA Intern Med. 2020;180(1):144-147. doi: 10.1001/jamainternmed.2019.3900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Engelberg Anderson JK, Jain P, Wade AJ, Morris AM, Slaboda JC, Norman GJ. Indicators of potential health-related social needs and the association with perceived health and well-being outcomes among community-dwelling Medicare beneficiaries. Qual Life Res. 2020;29(6):1685-1696. doi: 10.1007/s11136-019-02410-7 [DOI] [PubMed] [Google Scholar]
- 5.Horwitz LI, Chang C, Arcilla HN, Knickman JR. Quantifying health systems’ investment in social determinants of health, by sector, 2017–19. Health Aff (Millwood). 2020;39(2):192-198. doi: 10.1377/hlthaff.2019.01246 [DOI] [PubMed] [Google Scholar]
- 6.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. Accountable health communities—addressing social needs through Medicare and Medicaid. N Engl J Med. 2016;374(1):8-11. doi: 10.1056/NEJMp1512532 [DOI] [PubMed] [Google Scholar]
- 7.Billioux A, Verlander K, Anthony S, Alley D. Standardized screening for health-related social needs in clinical settings: the accountable health communities screening tool. National Academy of Medicine . May 30, 2017. Accessed June 7, 2022. https://nam.edu/standardized-screening-for-health-related-social-needs-in-clinical-settings-the-accountable-health-communities-screening-tool/
- 8.Fraze T, Lewis VA, Rodriguez HP, Fisher ES. Housing, transportation, and food: how ACOs seek to improve population health by addressing nonmedical needs of patients. Health Aff (Millwood). 2016;35(11):2109-2115. doi: 10.1377/hlthaff.2016.0727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray GF, Rodriguez HP, Lewis VA. Upstream with a small paddle: how ACOs are working against the current to meet patients’ social needs. Health Aff (Millwood). 2020;39(2):199-206. doi: 10.1377/hlthaff.2019.01266 [DOI] [PubMed] [Google Scholar]
- 10.CMS finalizes Medicare Advantage and Part D payment and policy updates to maximize competition and coverage. News release. Centers for Medicare & Medicaid Services . April 1, 2019. Accessed June 7, 2022. https://www.cms.gov/newsroom/press-releases/cms-finalizes-medicare-advantage-and-part-d-payment-and-policy-updates-maximize-competition-and
- 11.Advance notice of methodological changes for Calendar Year (CY) 2023. for Medicare Advantage (MA) capitation rates and Part C and Part D payment policies. Centers for Medicare and Medicaid Services . February 2, 2022. Accessed June 7, 2022. https://www.cms.gov/files/document/2023-advance-notice.pdf
- 12.Acquah I, Hagan K, Valero-Elizondo J, et al. Delayed medical care due to transportation barriers among adults with atherosclerotic cardiovascular disease. Am Heart J. 2022;245:60-69. doi: 10.1016/j.ahj.2021.11.019 [DOI] [PubMed] [Google Scholar]
- 13.LaRosa ART, Claxton J, O’Neal WT, et al. Association of household income and adverse outcomes in patients with atrial fibrillation. Heart. 2020;106(21):1679-1685. doi: 10.1136/heartjnl-2019-316065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Martin P, Liaw W, Bazemore A, Jetty A, Petterson S, Kushel M. Adults with housing insecurity have worse access to primary and preventive care. J Am Board Fam Med. 2019;32(4):521-530. doi: 10.3122/jabfm.2019.04.180374 [DOI] [PubMed] [Google Scholar]
- 15.Gundersen C, Ziliak JP. Food insecurity and health outcomes. Health Aff (Millwood). 2015;34(11):1830-1839. doi: 10.1377/hlthaff.2015.0645 [DOI] [PubMed] [Google Scholar]
- 16.Berkowitz SA, Meigs JB, DeWalt D, et al. Material need insecurities, control of diabetes mellitus, and use of health care resources: results of the Measuring Economic Insecurity in Diabetes study. JAMA Intern Med. 2015;175(2):257-265. doi: 10.1001/jamainternmed.2014.6888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. doi: 10.1097/00005650-199801000-00004 [DOI] [PubMed] [Google Scholar]
- 18.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130-1139. doi: 10.1097/01.mlr.0000182534.19832.83 [DOI] [PubMed] [Google Scholar]
- 19.Klabunde CN, Potosky AL, Legler JM, Warren JL. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53(12):1258-1267. doi: 10.1016/S0895-4356(00)00256-0 [DOI] [PubMed] [Google Scholar]
- 20.Guide to prevention quality indicators: hospital admission for ambulatory care sensitive conditions. Agency for Healthcare Research and Quality . October 2001. Accessed June 7, 2022. https://www.ahrq.gov/downloads/pub/ahrqqi/pqiguide.pdf
- 21.Billings J, Parikh N, Mijanovich T. Emergency department use in New York City: a substitute for primary care? Issue Brief (Commonw Fund). 2000;(433):1-5. [PubMed] [Google Scholar]
- 22.Johnston KJ, Allen L, Melanson TA, Pitts SR. “Patch” to the NYU emergency department visit algorithm. Health Serv Res. 2017;52(4):1264-1276. doi: 10.1111/1475-6773.12638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ballard DW, Price M, Fung V, et al. Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med Care. 2010;48(1):58-63. doi: 10.1097/MLR.0b013e3181bd49ad [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stuart EA. Matching methods for causal inference: a review and a look forward. Stat Sci. 2010;25(1):1-21. doi: 10.1214/09-STS313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seshamani M, Fowler E, Brooks-LaSure C. Building on the CMS strategic vision: working together for a stronger Medicare. Centers for Medicare & Medicaid Services . January 11, 2022. Accessed June 7, 2022. https://www.cms.gov/blog/building-cms-strategic-vision-working-together-stronger-medicare
- 26.Magnan S. Social determinants of health 201 for health care: plan, do, study, act. National Academy of Medicine . June 21, 2021. Accessed June 7, 2022. https://nam.edu/social-determinants-of-health-201-for-health-care-plan-do-study-act/ [DOI] [PMC free article] [PubMed]
- 27.Agrawal SK, Shrank WH. Clinical and social risk adjustment-reconsidering distinctions. N Engl J Med. 2020;382(17):1581-1583. doi: 10.1056/NEJMp1913993 [DOI] [PubMed] [Google Scholar]
- 28.Nerenz DR, Austin JM, Deutscher D, et al. Adjusting quality measures for social risk factors can promote equity in health care. Health Aff (Millwood). 2021;40(4):637-644. doi: 10.1377/hlthaff.2020.01764 [DOI] [PubMed] [Google Scholar]
- 29.Shrank WH, Keyser DJ, Lovelace JG. Redistributing investment in health and social services—the evolving role of managed care. JAMA. 2018;320(21):2197-2198. doi: 10.1001/jama.2018.14987 [DOI] [PubMed] [Google Scholar]
- 30.Tsega M, Lewis C, McCarthy D, Shah T, Coutts K. Review of evidence for health-related social needs interventions. Commonwealth Fund . July 2019. Accessed June 7, 2022. https://www.commonwealthfund.org/sites/default/files/2019-07/COMBINED_ROI_EVIDENCE_REVIEW_7.15.19.pdf
- 31.Kornfield T, Kazan M, Frieder M, Duddy-Tenbrunsel R, Donthi S, Fix A. Medicare Advantage plans offering expanded supplemental benefits: a look at availability and enrollment. Commonwealth Fund . February 10, 2021. Accessed June 7, 2022. https://www.commonwealthfund.org/publications/issue-briefs/2021/feb/medicare-advantage-plans-supplemental-benefits
- 32.Murphy-Barron C, Buzby EA, Pittinger S. Overview of Medicare Advantage supplemental healthcare benefits and review of Contract Year 2022 offerings. Millman . February 2022. Accessed June 7, 2022. https://bettermedicarealliance.org/wp-content/uploads/2022/03/MA-Supplemental-Benefits-Milliman-Brief_20220225.pdf
- 33.Cole MB, Nguyen KH. Unmet social needs among low-income adults in the United States: associations with health care access and quality. Health Serv Res. 2020;55(suppl 2):873-882. doi: 10.1111/1475-6773.13555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.De Marchis EH, Torres JM, Benesch T, et al. Interventions addressing food insecurity in health care settings: a systematic review. Ann Fam Med. 2019;17(5):436-447. doi: 10.1370/afm.2412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oronce CIA, Miake-Lye IM, Begashaw MM, Booth M, Shrank WH, Shekelle PG. Interventions to address food insecurity among adults in Canada and the US: a systematic review and meta-analysis. JAMA Health Forum. 2021;2(8):e212001. doi: 10.1001/jamahealthforum.2021.2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berkowitz SA, Ricks KB, Wang J, Parker M, Rimal R, DeWalt DA. Evaluating a nonemergency medical transportation benefit for accountable care organization members. Health Aff (Millwood). 2022;41(3):406-413. doi: 10.1377/hlthaff.2021.00449 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Supplemental Methods
eTable 1. Comparison of Survey Respondents and Non-Respondents, and Survey Completers and Non-Completers
eTable 2. Correlation between Individual Health-Related Social Needs
eFigure. Participant Flow Through the Study
eTable 3. Complete Regression Results
eTable 4. Association between Individual Health-Related Social Needs and Rates of Hospital Stays and ED Visits, with Each HRSN Modeled Independently