Abstract
Background
Mentoring’s pivotal role in nurturing professional identity formation (PIF) owes much to its combined use with supervision, coaching, tutoring, instruction, and teaching. However the effects of this combination called the ‘mentoring umbrella’ remains poorly understood. This systematic scoping review thus aims to map current understanding.
Methods
A Systematic Evidence-Based Approach guided systematic scoping review seeks to map current understanding of the ‘mentoring umbrella’ and its effects on PIF on medical students and physicians in training. It is hoped that insights provided will guide structuring, support and oversight of the ‘mentoring umbrella’ in nurturing PIF. Articles published between 2000 and 2021 in PubMed, Scopus, ERIC and the Cochrane databases were scrutinised. The included articles were concurrently summarised and tabulated and concurrently analysed using content and thematic analysis and tabulated. The themes and categories identified were compared with the summaries of the included articles to create accountable and reproducible domains that guide the discussion.
Results
A total of 12201 abstracts were reviewed, 657 full text articles evaluated, and 207 articles included. The three domains identified were definitions; impact on PIF; and enablers and barriers. The mentoring umbrella shapes PIF in 3 stages and builds a cognitive base of essential knowledge, skills and professional attitudes. The cognitive base informs thinking, conduct and opinions in early supervised clinical exposure in Communities of practice (COP). The COPs’ individualised approach to the inculcation of desired professional characteristics, goals, values, principles and beliefs reshapes the individual’s identity whilst the socialisation process sees to their integration into current identities.
Conclusion
The mentoring umbrella’s provides personalised longitudinal support in the COP and socialisation process. Understanding it is key to addressing difficulties faced and ensuring holistic and timely support.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-022-03589-z.
Keywords: Mentoring, Supervision, Coaching, Teaching, Instruction, Professional Identity Formation, Communities of Practice
Introduction
Mentoring plays a critical role in nurturing professional identity formation (henceforth PIF) or helping medical students and physicians (henceforth physicians in training) “think, act and feel like physicians” [1]. This role is premised on the notion that mentoring’s personalised, longitudinal and holistic support helps physicians in training integrate the relevant professional values, beliefs, expectations, standards, codes of conduct, culture and principles of the medical profession into their individual identities [2]. However, efforts to understand mentoring’s precise role in PIF has been limited by the presence of a variety of different forms of mentoring [3–5] and its conflation with distinct practices such as role modelling, supervision, coaching, tutoring, teaching and instruction [6]. Two new developments promise to change this impasse and offer new insights into mentoring’s role in PIF.
The first is evidence that role modelling, supervision, coaching, tutoring, teaching and instruction take on characteristics that liken them to mentoring when applied in a longitudinal manner to enduring and personalised educational relationships [7]. Krishna et al. (2019) suggest overlaps with traditionally understood concepts of mentoring, allowing these approaches to be considered part of a larger concept called the ‘mentoring umbrella’.
The second is the notion that professional identity is part of a larger concept of identity and that self-concepts of identity are intimately related and informed by self-concepts of personhood or “what makes you, you” [8]. As such, the influence of effective mentoring on the PIF of physicians in training may be understood through the lens of personhood. This is especially useful amidst evidence that evaluations of self-concepts of personhood did allow for better appreciation of changing notions of identity particularly when current tools fail to effectively evaluate such evolving concepts.
Ring theory of personhood
Radha Krishna and Alsuwaigh [9]’s Ring Theory of Personhood (RToP) is a clinically evidenced tool that maps changing concepts of personhood and captures evolving notions of identity. The RToP suggests that personhood is comprised of the Innate, Individual, Relational and Societal Rings (Fig. 1) [10–12]. With each ring encapsulating the values, beliefs, and principles of the particular aspect of the clinician’s identity, each ring also represents the corresponding aspects of identity (Fig. 1) [12, 13].
Fig. 1.
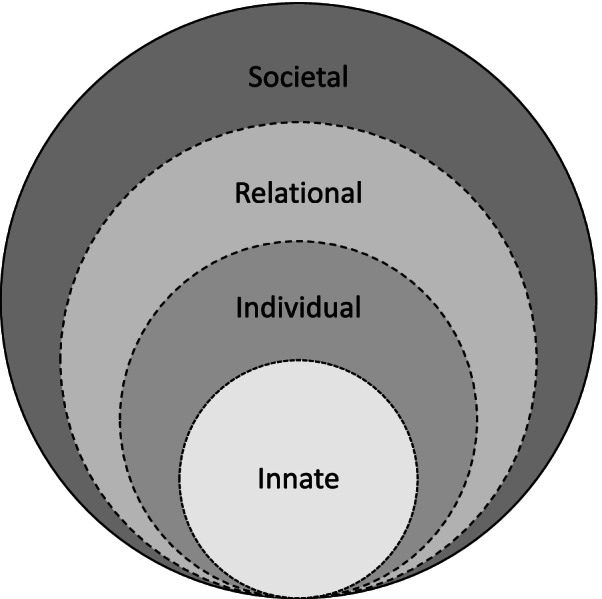
The Ring Theory of Personhood (RToP)
It is suggested that better understanding of these values, beliefs, and principles will reveal how a physician in training’s views their roles, responsibilities, and place within a team, family unit, professional community, and society and provide insights into the physician in training’s thinking, conduct and coping in the face of different situational, environmental, and/or relational influences [14–22].
At the core of the Ring Theory is the Innate Ring that houses the individual’s spiritual, religious and/or theist beliefs, values, moral ideals, and ethical principles. These are shaped by the individual’s demographical and historical features such as the ethnicity, culture, religion, family unit, gender, society, country, and social group they were born into. These considerations influence the individual’s Innate Identity and their thinking, goals, motivations, and actions.
The Individual Ring represents conscious function which includes the ability to think, feel, communicate, carry out actions, and interact with the environment. The Individual Ring houses the individual’s values, beliefs, principles, biases, preferences, thoughts, emotions, experiences, decision making and personality which shape Individual Identity.
The Individual Ring also acts to balance the thinking, goals, motivations, and actions drawn from the Innate, Relational and Societal Identities.
The Relational Ring consists of personal relationships deemed to be important to the individual, and the values and beliefs that stem from and inform these relationships. The Societal Ring contains societal, religious, professional, and legal expectations set out in the individual’s society to guide and police conduct. One’s professional identity resides here.
These identities may come into conflict when professional involvement in cases such as those involving palliative sedation, withdrawal or withholding of treatment, termination of pregnancy or familial determination arise.
Structured ‘mentoring umbrella’ approach
A structured ‘mentoring umbrella’ approach replete with a combination of mentoring, supervision, coaching, tutoring, teaching and instruction may be key to structuring and guiding this professional identity formation process. Indeed, Krishna et al. (2018) suggest that the most significant role of this holistic approach is its ability to support students, residents and junior doctors during periods of negotiation where new experiences and obstacles are either accepted, adapted to fit their particular circumstances or needs (compromised) or rejected [23]. Kuek, Ngiam [24], Ho, Kow [11], Ngiam, Ong [25], Chan, Chia [10] and Huang, Toh [13] suggest that ‘conflict’ sees the beliefs, values and principles housed in each of the four rings in ‘tension’ with professional norms and responsibilities introduced to each ring. If the ‘tension’ persists, dyssynchrony or identity dissonance arises [24]. This may increase the risk of burnout and a loss of interest in the profession [26–32]. Effectively supporting the processing and resolution of dyssynchrony will attenuate these risks.
With Sarraf-Yazdi et al. (2021) suggesting that mentoring helps each of the four identities adapt to the inculcation of these new professional values and responsibilities, evaluating elements of the ‘mentoring umbrella’ more closely may clarify its role within any proposed PIF focused training program.
Methods
A Systematic Evidence-Based Approach guided systematic scoping review (henceforth SSR in SEBA) is used to map what is known about the effects of mentoring, supervision, coaching, tutoring, teaching and instruction upon PIF [33–36]. Given its broader scope, we aim to study role modelling’s impact on PIF in a separate review.
This SSR in SEBA is overseen by an expert team comprised of medical librarians from the Yong Loo Lin School of Medicine (YLLSoM) and the National Cancer Centre Singapore (NCCS), and local educational experts and clinicians at NCCS, the Palliative Care Institute Liverpool, YLLSoM and Duke-NUS Medical School who guide, oversee and support all stages of SEBA to enhance the reproducibility and accountability of the process [37–49] (Fig. 2).
Fig. 2.

The SEBA Process
Stage 1 of SEBA: systematic approach
Determining the title
The research and expert teams set out the overarching goals, study population, context and remediation programs to be evaluated.
Inclusion criteria
The PICOS format was used to guide the inclusion criteria Table 1.
Table 1.
PICOs, inclusion criteria and exclusion criteria applied to database search
| PICOS | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | • Junior physicians, residents, and medical students |
Allied health specialties such as dietetics, nursing, psychology, chiropractic, midwifery, social work Specialists, consultants, attendings and physicians not in training programs Non-medical specialties such as clinical and translational science, veterinary, dentistry |
| Intervention |
• All forms of mentoring and o Mentoring processes o Mentor factors o Mentee factors o Mentoring relationship o Host organization o Outcomes of mentoring o Barriers to mentoring o Mentoring structure o Mentoring framework o Mentoring culture o Mentoring environment • Educational roles of mentoring: Supervision, coaching, role-modelling, teaching, and tutoring |
|
| Comparison | • Comparisons accounts of mentoring between mentoring programs, editorials, and perspective, reflective, narratives and opinions pieces | |
| Outcome |
• Personal outcomes of mentoring such as values, beliefs, identity as a medical professional etc • Professional development outcomes such as on career choices (including academia positions/careers) |
• Papers that did not discuss impact of mentoring on personal or professional development outcomes |
| Study design |
• All study designs are included o Descriptive papers o Qualitative, quantitative, and mixed study methods o Systematic review, literature reviews, and narrative reviews • Perspectives, opinion, commentary pieces, and editorials • Year: 1st January 2000 to 31st December 2020 |
Identifying the research question
To identify the research question, the expert and research teams were guided by the Population, Intervention, Comparison, Outcome and Study Design (PICOS) elements of the inclusion criteria [50, 51]. The primary research question was identified as follows: “What is known about the effect of mentoring, supervision, coaching, tutoring, teaching and instruction on professional identity formation amongst medical students, residents and junior doctors?”
Searching
In keeping with Pham, Rajić [52]’s recommendations on ensuring a viable and sustainable research process, the research team confined the searches to articles published between 1st January 2000 to 31st December 2020 to account for prevailing manpower and time constraints. Additional ‘snowballing’ of references of the included articles ensured a more comprehensive review of the articles [53].
Extracting and charting
Using an abstract screening tool, the research team independently reviewed abstracts to be included and employed ‘negotiated consensual validation’ to achieve consensus on the final list of articles to be included [54].
Stage 2 of SEBA: split approach
The split approach [55] sees concurrent analysis of the included articles by three independent teams. The first team summarised and tabulated the articles in keeping with recommendations drawn from RAMESES publication standards by Wong, Greenhalgh [56] and “Guidance on the conduct of narrative synthesis in systematic reviews” by Popay, Roberts [57]. The second team used the approach to thematic analysis by Braun and Clarke [58] to find meaning and patterns in the data whilst the third team employed the approach to directed content analysis by Hsieh and Shannon [59] to “identifying and operationalizing a priori coding categories” from “The Development of Professional Identity” by Cruess and Cruess [2]. ‘Negotiated consensual validation’ was used as a means of peer debrief in all three teams to further enhance the validity of the findings [60].
Stage 3 of SEBA: jigsaw perspective
The Jigsaw Perspective employs Phases 4 to 6 of France et al. [61]’s adaptation of Noblit et al. [62]’s seven phases of meta- ethnographic approach to view the themes and categories as pieces of a jigsaw puzzle where overlapping/complementary pieces are combined to create a bigger piece of the puzzle referred to as themes/categories. This process would see themes and subthemes compared with the categories and subcategories identified. These similarities were verified by comparing the codes contained within them. If they are complementary in nature, then the subtheme and subcategory are combined to create a bigger piece of the jigsaw puzzle Table 2.
Table 2.
Subthemes and subcategories
| Subthemes | Subcategories |
|---|---|
| The Impact of Mentoring, Supervision, Coaching, Teaching and Instruction on Personhood: RToP | Innate Ring; Individual Ring; Relational Ring; Societal Ring |
| Barriers and Enablers | Mentoring and its Roles; Communities; Learners; Institutions; Others |
Stage 4 of SEBA: Funnelling
Themes/categories were compared with the tabulated summaries (Additional file 1: Appendix A). The funnelled domains created from this process forms the basis of the discussion’s ‘line of argument’.
Results
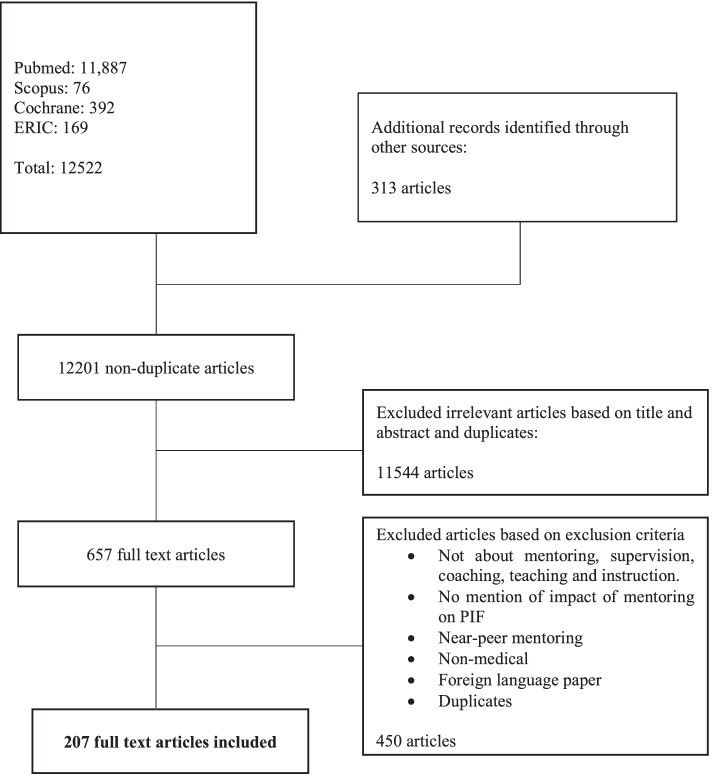
A total of 12201 abstracts were reviewed, 657 full text articles evaluated, and 207 articles included and coded. A total of 176 of the 207 articles were data-driven while 31 articles were opinion driven (commentaries, editorials, letters, perspectives, reflections) (Fig. 3). Of the data driven articles, 55 were quantitative studies, 75 were qualitative studies, 33 were mixed studies, and 13 were literature and systematic reviews.
Fig. 3.
PRISMA flow chart
There were 163 articles on mentoring, 26 articles on supervision, 18 articles on coaching, 46 articles on teaching and 8 articles on instruction. There were a few articles that covered a variety of forms of mentoring.
Themes and categories identified
Scrutiny of the themes and categories from thematic and content analysis were consistent with one another. To avoid repetition, we discuss the themes identified using both approaches in tandem. The funnelled domains identified were:
A definition for each of the elements of the mentoring umbrella
How each element within the mentoring environment impacts PIF
Enablers and barriers to mentoring, supervision, coaching, teaching and instruction’s effects on PIF.
Domain 1
Defining mentoring, supervision, coaching, teaching and instruction. From the included articles it is possible to delineate an understanding of mentoring supervision, coaching, teaching and instruction. These are summarised in Table 3.
Table 3.
Definitions and descriptors of mentoring and its roles
| Mentoring | ▪ “Dynamic, context dependent, goal sensitive, mutually beneficial relationship between an experienced clinician and junior clinicians and or undergraduates that is focused upon advancing the development of the mentee.” [63] |
|---|---|
| Teaching |
▪ Impart knowledge and guide studies by precept, examples or experience [63]. ▪ Teaching in the clinical environment is defined as teaching and learning focused on, and usually directly involving, patients and their problems [64] |
| Coaching |
▪ Coaching is an inherently creative activity of bringing forth knowledge, wisdom, and insight [65]. ▪ A coach works with a student to continually improve his/her performance, usually on areas that the student deems weak [66]. ▪ The coaching process involves asking questions [66], listening deeply [65], keenly observing [65, 67], evaluating and identifying gaps [68], providing specific and concrete feedback [67, 68], creating goals, exploring solutions, and holding the individual accountable [68], supporting reflection [65, 66, 69], setting goals [69], developing a comprehensive study plan [69] and ensuring a commitment to learning [65]. ▪ Coaching can also improve their emotional intelligence, durability, wellbeing, and resilience [66]. ▪ In medical education, two main types of coaching have been described [68]: • Coaching in clinical skills: coach directly observes the learner in the clinical setting and then engages in the coaching process for the improvement of a specific skill such as procedural training [68] • Academic coaching: coaches guide learners to achieve their fullest potential by indirectly evaluating performance via review of objective assessments [68]: o (a) self-reflection; o (b) specific, measurable, achievable, relevant and time-based (SMART) goal setting; o (c) the development of comprehensive study plans with deliberate use of effective learning strategies including spaced retrieval practice and elaboration, and o (d) self-care. • Teaching faculty members supported the streamlined, collaborative approach. Academic coaches offered timely oversight and early identification of students requiring support [69]. |
| Instruction |
▪ None of the articles defined instruction. ▪ According to the UNESCO International Bureau of Education, instruction is defined as: “The creation and implementation of purposefully developed plans for guiding the process by which learners gain knowledge and understanding, and develop skills, attitudes, appreciations and values.” [70] |
| Supervision |
▪ Supervision may be seen “as an intervention, a working alliance, a method, a process and a professional activity.” [71] ▪ Supervision may be conceived of as “…a joint endeavour in which a practitioner with the help of a supervisor, attends to their clients, themselves as part of their client practitioner relationships and the wider systemic context, and by so doing improves the quality of their work, transforms their client relationships, continuously develops themselves, their practice and the wider profession.” [72] ▪ Clinical supervision has been defined as the “provision of guidance and feedback on matters of personal, professional and educational development in the context of a trainee’s experience of providing safe and appropriate patient care” [73]. |
Domain
Impact of mentoring, supervision, coaching, teaching and instruction impact PIF
To effectively evaluate the impact of the elements of the mentoring umbrella on PIF, we discuss each of them in turn through the lens of the RtoP.
Mentoring
Mentoring supports minority groups with guidance and networking opportunities [74–76] and helps female mentees balance their career demands and family responsibilities [77–81], underlying its role in the Innate Ring.
In the Individual Ring mentoring helps support the mentee’s career, personal, research and academic goals, beliefs, values, and motivations by boosting confidence [80, 82–89], discipline [89] resilience [90, 91], and self-efficacy of the mentee [86]. Mentoring also supports reflective practice [74, 87, 92, 93] which increases career satisfaction [94], and boosts work-life balance [95–98], and reduces burnout and disillusionment [99].
Within the Relational Ring mentoring is credited with enhancing parenting skills [100], and improving relationships with family members [93, 98]. In the Societal Ring, mentoring improves networking [101], sponsorship [102], interprofessional practice [98] and patient interactions [103].
Supervision
Supervision’s effect on the Individual Ring includes increasing interest in a particular field [104–107], influencing career decisions [104, 105, 107, 108], boosting personal development/growth [71, 106, 109–112] and personal skills [110] and improves career satisfaction [110, 113]. In the Societal Ring, supervision enhances academic [3, 110, 114–117], research [104, 110], decision making skills [109] and clinical [71, 73, 107, 109, 114, 116–122] competencies and supports socialisation of a professional identity [115, 118, 123, 124].
Teaching
In the Individual Ring, teaching improves interest in a particular field [104–106, 125–127], influences career decisions [104, 105], nurtures personal development/growth [106, 110, 128–139] and boosts career satisfaction [110, 139, 140]. In the Societal Ring, teaching increases academic [74, 110, 127, 132, 135, 141] clinical [118, 119, 128, 129, 131–135, 138, 141–153] and research [104, 110, 126, 154–156] competencies [110, 118, 119, 130, 136, 137, 139, 143, 149, 155, 157, 158].
Within the Societal Ring, teaching advances networking [74, 141], career goals [110, 126, 151] and research outputs [104, 110, 126, 151], improves interprofessional working [104, 118, 135, 141, 149], patient interactions [118, 128, 131, 133–135, 138, 141, 142, 146, 147, 149, 157, 159], social identity and a sense of community [141].
Coaching
In the Individual Ring, coaching influences career decisions [104], boosts personal development/growth [65, 66, 68, 69, 110, 139, 160–162] and career satisfaction [66, 110].
In addition, coaching improves academic [65, 68, 69, 110, 117, 162, 163] clinical [65, 117, 160, 164–166] and research [104, 110] competencies [3, 110, 139, 160, 164, 165] in the Societal Ring.
Instruction
In the Individual Ring, instruction improves skills [133] and time management [167] and in the Societal Ring it improves clinical competencies [133, 147, 149, 157, 167, 168] and interactions with patients [133, 147, 149, 157] and fellow professionals [149, 167].
Domain 3
There are factors that enhance (enablers) and hinder (barriers) the impact of mentoring, supervision, coaching, teaching and instruction upon PIF. These may be divided into mentee, mentor and institutional factors.
Mentee-related
Mentee related factors influencing the efficacy of the mentoring umbrella include being motivated, proactive, invested in the mentoring process and relationships, reflective, willingness to take feedback and make necessary adaptations and assign sufficient time to training [35, 82, 83, 97, 102, 118, 169–176].
Mentor-related
Mentor related factors consider all the roles played under the aegis of the mentoring umbrella. These include being motivated and invested in mentoring, having the abilities, availabilities and experience required, possessing good listening and communication skills, a commitment to self-improvement and learning, being open to feedback and learning from the mentee, being able to provide holistic and longitudinal support and understanding and abiding by the expectations and standards of practice expected of a mentor [74, 78, 80, 83, 86, 87, 89, 95, 170, 177, 178].
Institution-related
The host organization plays a critical role in matching, training, supporting and structuring the training process. The implementation of protected time and formal recognition of participation in mentoring help maintain motivation.
The host organization also plays a part in establishing clear codes of conduct, roles and responsibilities and expectations of all stakeholders, structuring the mentoring process, providing it a formal place in the curriculum, assessing and overseeing the program [3, 80, 83, 84, 87, 89, 90, 97, 100, 118, 170, 174]. This is especially important when considering the hidden and informal curriculum influence workplace culture; career choice; impact upon the mentoring environment [67, 86, 90, 93, 100, 102, 113, 130, 179, 180]; and acknowledgment and personal and team investment in the efforts of the mentoring umbrella [71, 77, 82, 118, 130, 181].
Stage 5 of SEBA: analysis of evidence-based and Non-data driven Literature
The themes drawn from evidenced-based publications were compared with those from non-data based articles (grey literature, opinion, perspectives, editorial, letters) found that the themes from both groups to be similar and non-data based articles did not bias the analysis untowardly.
Most of the included articles were data-driven (175 out of 207) whilst the remaining articles were non-data-based articles (grey literature, commentaries, opinion, perspectives, editorial, letters). Despite non-data-based articles forming a small minority of articles, we examined themes drawn from the non-data-driven publications and compared them with those from data-based articles (grey literature, opinion, perspectives, editorial, letters). This process revealed similarities between the two groups suggesting that non-data-based articles did not bias the analysis untowardly.
A majority of articles only stated the outcomes of the mentoring umbrella without addressing mechanisms via which they exert their influence [65–69, 71, 74, 75, 86, 93, 94, 97, 100, 109, 118, 123, 130, 149, 150, 177, 182]. Given how mechanism papers formed the minority, there were concerns that non-mechanism papers would bias the data. There were also no papers describing the mechanism via which instruction influences personhood. Regardless, most of the mechanisms described were consistent with each other as well as the data derived from non-mechanism papers.
Discussion
Stage 6 of SEBA: synthesis of SSR in SEBA
In answering its primary question, this SSR in SEBA of the mentoring umbrella’s effects on PIF provides a number of insights into the mentoring umbrella’s influence on the stages of PIF development and the role of the host organization.
When applied longitudinally to an individualised learning relationship, across different settings involving one learner or a small group of learners with common goals, abilities and experiences, the mentoring umbrella provides an individualised perspective of development. This approach accounts for the physician-in-training’s and the instructor’s, teacher’s, coach’s, supervisor’s and tutor’s abilities, availabilities, attitudes, context, competencies, demographics, experiences, goals, motivations, and needs, in addition to building upon the physician in training’s successes, failures and reflections to enhance their longer term development. The overlapping elements within the mentoring umbrella provide synergistic support in addressing the influences of the physician-in-training’s societal, professional, clinical, academic, research, and personal considerations, the regnant sociocultural considerations, the influence of prevailing healthcare and educational system and the impact of the local hidden, informal and formal curriculum, upon PIF. This affirms the notion that the mentoring umbrella may be applied widely and in the stage based manner that allows them mentoring umbrella to shape PIF.
The mentoring umbrella’s influence on PIF
Stage One. Building a personalised cognitive base
The first stage of mentoring umbrella’s influence on PIF begins with the building of a ‘cognitive base’ of knowledge, skills, relevant expectations, roles, responsibilities around the physician-in-training’s goals, abilities, milestones, experience and setting. The cognitive base also inculcates regnant standards of professionalism and sociocultural considerations. Much of this personalisation in this stage falls upon tutoring, teaching and instruction.
Applied longitudinally, the mentoring umbrella also advance mutual understanding, trust and open communication, networking, interprofessional collaborations, research output, and enhances clinical and research competencies.
Stage Two. Codes of Practice (COP)s
Early exposure to clinical practice builds upon a personalised cognitive base and occurs in communities of practice. Barab et al. (2004) define CoPs as “a persistent, sustaining social network of individuals who share and develop an overlapping knowledge base, set of beliefs, values, history and experiences focused on a common practice and/or enterprise” [183]. Here the mentoring umbrella facilitates personalised clinical exposure, supports the application and appraisal of knowledge, skills and competencies, provides feedback and oversees remedial exercises. In remedial processes the coaching and supervision elements of the mentoring umbrella focus attention on competency gaps and boost confidence in the learner’s Individual and Societal Rings.
Stage Three. The socialisation process
Cruess et al. (2015) [184] describes the socialisation process as “a representation of self, achieved in stages over time during which the characteristics, values, and norms of the medical profession are internalised, resulting in an individual thinking, acting and feeling like a physician”.
Whilst technically part of the COP, the precise mechanism in which the socialisation process helps the integration of new values, beliefs and principles are integrated into current identities remains unclear. However it does appear that within the socialisation process the mentoring umbrella provides physicians in training with personalised, responsive, appropriate and timely support as they confront ethical, cultural, philosophical, religious and social issues that conflict with their Innate, Individual, Relational and Societal values, beliefs and principles. Here, coaching’s ability to observe [65, 67], listen deeply [65], keenly question (218), evaluate and identify gaps [68], explore solutions [65, 66, 69], provide specific and concrete feedback [67, 68], support reflection [65, 66, 69], set goals [69], develop a comprehensive study plan [69] and hold the individual accountable [68] helps focus efforts on particular areas of identity inculcation, career readiness [185], remediation of professional identities and character education [186]. Critically, coaching and supervision provide this help whilst being sensitive to the learner’s wellbeing, and goals [66]. Instruction impacts identity development in Individual and Societal aspects of personhood. These combinations of approaches would be critical to the provision of affirmation, feedback, facilitated reflection, career guidance, holistic and longitudinal support, introduction of a variety of opportunities and resources, sharing networks and “stress inoculation” important to facilitating reflection, the provision of feedback [187, 188]. Addressing dyssynchrony also highlights the role of the mentor in assessing and supporting the mentees. This continuous multipronged approach facilitates the nurturing of an enduring and personalised mentoring relationship.
The role of the host organization
This review also underscores the role of the host organisation [82, 171] in structuring effective mentoring relationships [170, 173, 174]. Echoing recent reviews on mentoring, the host organisation plays a critical role in the selection and matching of motivated mentees and trained and experienced mentors who share complementary goals. The host organization plays a critical role in establishing a common code of conduct, oversight [189] and assessment [190] process, as well as a supportive and nurturing environment. The host organization must also provide longitudinal ‘protected time’, support and recognition of trained mentors over the course of a mentee’s developmental journey. A further aspect in a mentor’s armamentarium must be access to user-friendly and robust communication platforms that enable timely, personal and appropriate feedback. Such a platform will also aid gathering of input on the mentee’s situation, development, goals and needs.
Here, the various aspects of the mentoring umbrella encapsulate many of the primary influences upon PIF set out by Cruess and colleagues (2015, 2018, 2019) [2, 23, 184]. Pending further studies, it may yet be possible to suggest that purposeful, structured nurturing of PIF is a mentored process.
Limitations
One of the main limitations of this study was its inability to differentiate residents and junior doctors in training from more senior doctors such as consultants, attendings, specialists and senior consultants who have completed their training and physicians who are not in training programs. This limited the number of articles included. In addition, difficulties separating these groups also made analysis of the data difficult given the different levels of experience, roles, responsibilities and needs amongst the included groups of physicians given the diversity of the training programs and different settings and educational and healthcare programs adopted.
Moreover, whilst this study was intended to analyse the wide range of current literature on mentoring and PIF programs, our review was limited by a lack of consistent reporting of current programs. Furthermore, most of the included papers were largely drawn from North American and European practices potentially limiting the applicability of these findings in other healthcare settings. This was compounded by our focus upon articles that were published in English.
Whilst taking into account the limited resources and availability of the research and experts teams and limiting the review to the specified dates to increase the chances of completing the review, this too could have seen important articles excluded.
Conclusion
This SSR in SEBA highlights the role of mentoring umbrella in nurturing PIF. Whilst the three stages built on posits by Cruess and colleagues remain to be evidenced, it does underline the need for longitudinal and holistic evaluation of the mentoring umbrella’s impact on PIF. Further understanding of the mentoring umbrella and its role in PIF also demands better appreciation of the need for personalised, holistic and longitudinal assessments and individualised and timely support. These gaps represent some of the key areas for future studies seemingly as the role of portfolios and longitudinal assessment measures to enhance support of evolving concepts of PIF develop.
Supplementary Information
Additional file 1: Appendix A. Tabulated Summaries
Acknowledgements
The authors would like to dedicate this paper to the late Dr. S Radha Krishna whose advice and ideas were integral to the success of this study.
Abbreviations
- CoP
Community of Practice
- PICOs
Population, Intervention, Comparison, Outcome and Study Design
- PIF
Professional Identity Formation
- SSR
Systematic Scoping Review
- SEBA
Systematic Evidence-Based Approach
- RToP
Ring Theory of Personhood
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- YLLSoM
Yong Loo Lin School of Medicine
- NCCS
National Cancer Centre Singapore
Authors’ contributions
All authors were involved in data curation, formal analysis, investigation, preparing the original draft of the manuscript as well as reviewing and editing the manuscript. All authors have read and approved the manuscript.
Funding
No funding was received for this review.
Availability of data and materials
All data generated or analysed during this review are included in this published article and its supplementary files.
Declarations
Ethics approval and consent to participate
NA
Consent for publication
NA
Competing interests
All authors have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Merton RΚ. In: The Student-Physician: Introductory Studies in the Sociology of Medical Education. Merton RK, Reader GG, Kendall P, editors. Harvard University Press; 2013. pp. 3–80. [Google Scholar]
- 2.Cruess SR, Cruess RL. The Development of Professional Identity. Vol. 17. In: Swanwick T, Forrest K, O'Brien BC, editors. Understanding Medical Education: Evidence, Theory, and Practice, Third Edition. 2018. [Google Scholar]
- 3.Radha Krishna LK, Renganathan Y, Tay KT, et al. Educational roles as a continuum of mentoring’s role in medicine – a systematic review and thematic analysis of educational studies from 2000 to 2018. BMC Med Educ. 2019;19(1):439. doi: 10.1186/s12909-019-1872-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Krishna L, Toh YP, Mason S, et al. Mentoring stages: A study of undergraduate mentoring in palliative medicine in Singapore. PLoS One. 2019;14(4):e0214643. doi: 10.1371/journal.pone.0214643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krishna L, Tay KT, Yap HW, et al. Combined novice, near-peer, e-mentoring palliative medicine program: A mixed method study in Singapore. PLoS One. 2020;15(6):–e0234322. [DOI] [PMC free article] [PubMed]
- 6.Wahab M, Ikbal M, Jingting W, et al. Creating Effective Interprofessional Mentoring Relationships in Palliative Care- Lessons from Medicine, Nursing, Surgery and Social Work. J Palliat Care Med. 2016; 01/01;06.
- 7.Buddeberg-Fischer B, Herta KD. Formal mentoring programmes for medical students and doctors--a review of the Medline literature. Med Teach. 2006;28(3):248–257. doi: 10.1080/01421590500313043. [DOI] [PubMed] [Google Scholar]
- 8.Krishna LK, Alsuwaigh R. Understanding the fluid nature of personhood - the ring theory of personhood. Bioethics. 2015;29(3):171–181. doi: 10.1111/bioe.12085. [DOI] [PubMed] [Google Scholar]
- 9.Radha Krishna LK, Alsuwaigh R. Understanding the fluid nature of personhood - the ring theory of personhood. Bioethics. 2015;29(3):171–181. doi: 10.1111/bioe.12085. [DOI] [PubMed] [Google Scholar]
- 10.Chan N, Chia J, Ho C, et al. Extending the Ring Theory of Personhood to the Care of Dying Patients in Intensive Care Units. Asian Bioethics Rev. 2021;14:1. doi: 10.1007/s41649-021-00192-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ho CY, Kow CS, Chia CHJ, et al. The impact of death and dying on the personhood of medical students: a systematic scoping review. BMC Med Educ. 2020;20(1):516. doi: 10.1186/s12909-020-02411-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vig PS, Lim JY, Lee RWL, et al. Parental bereavement – impact of death of neonates and children under 12 years on personhood of parents: a systematic scoping review. BMC Palliat Care. 2021;20(1):136. doi: 10.1186/s12904-021-00831-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Huang H, Toh RQE, Chiang CLL, et al. Impact of Dying Neonates on Doctors' and Nurses' Personhood: A Systematic Scoping Review. J Pain Symptom Manage. 2021;14. [DOI] [PubMed]
- 14.Alsuwaigh R. How do English-speaking Cancer Patients Conceptualise Personhood? Ann Acad Med Singapore. 2015;44(6):207–217. [PubMed] [Google Scholar]
- 15.Arai K, Saiki T, Imafuku R, et al. What do Japanese residents learn from treating dying patients? The implications for training in end-of-life care. BMC Med Educ. 2017;17(1):205. doi: 10.1186/s12909-017-1029-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ho CY, Kow CS, Chia CHJ, et al. The impact of death and dying on the personhood of medical students: a systematic scoping review. BMC Med Educ. 2020;20(1):516. doi: 10.1186/s12909-020-02411-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khandelwal A, Nugus P, Elkoushy MA, et al. How we made professionalism relevant to twenty-first century residents. Med Teach. 2015;37(6):538–542. doi: 10.3109/0142159X.2014.990878. [DOI] [PubMed] [Google Scholar]
- 18.Kim S, Choi S. The Medical Professionalism of Korean Physicians: Present and Future. BMC Med Ethics. 2015;26(16):56. doi: 10.1186/s12910-015-0051-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Krishna LK, Alsuwaigh R, Miti PT, et al. The influence of the family in conceptions of personhood in the palliative care setting in Singapore and its influence upon decision making. Am J Hosp Palliat Care. 2014;31(6):645–654. doi: 10.1177/1049909113500136. [DOI] [PubMed] [Google Scholar]
- 20.Kuek JTY, Ngiam LXL, Kamal NHA, et al. The impact of caring for dying patients in intensive care units on a physician's personhood: a systematic scoping review. Philos Ethics Humanit Med. 2020;15(1):12. doi: 10.1186/s13010-020-00096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Krishna LK, Yong CY, Koh SM. The role of palliative rehabilitation in the preservation of personhood at the end of life. BMJ Case Rep. 2014;9:2014. doi: 10.1136/bcr-2014-204780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wei SS, Krishna LKR. Respecting the wishes of incapacitated patients at the end of life [Report]. Ethics & Medicine: An International Journal of Bioethics. 2016 2016 Spring //;32:15+.
- 23.Cruess SR, Cruess RL, Steinert Y. Supporting the development of a professional identity: General principles. Med Teach. 2019;41(6):641–649. doi: 10.1080/0142159X.2018.1536260. [DOI] [PubMed] [Google Scholar]
- 24.Kuek JTY, Ngiam LXL, Kamal NHA, et al. The impact of caring for dying patients in intensive care units on a physician’s personhood: a systematic scoping review. Philos Ethics Humanit Med. 2020;15(1):12. doi: 10.1186/s13010-020-00096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ngiam LXL, Ong YT, Ng JX, et al. Impact of Caring for Terminally Ill Children on Physicians: A Systematic Scoping Review. American Journal of Hospice and Palliative Medicine®. 2020:1049909120950301. [DOI] [PubMed]
- 26.Dias MPS. Medical students' experiences of moral distress-a cross-sectional observational, web-based multicentre study. 2020. [Google Scholar]
- 27.Weber E, Gray S. How Should Integrity Preservation and Professional Growth Be Balanced during Trainees' Professionalization? AMA J Ethics. 2017;19(6):544–549. doi: 10.1001/journalofethics.2017.19.6.ecas2-1706. [DOI] [PubMed] [Google Scholar]
- 28.Monrouxe L, Shaw M, Rees C. Antecedents and Consequences of Medical Students' Moral Decision Making during Professionalism Dilemmas. AMA J Ethics. 2017;19(6):568–577. doi: 10.1001/journalofethics.2017.19.6.medu1-1706. [DOI] [PubMed] [Google Scholar]
- 29.Miller BM. How Should Resident Physicians Respond to Patients' Discomfort and Students' Moral Distress When Learning Procedures in Academic Medical Settings? AMA J Ethics. 2017;19(6):537–543. doi: 10.1001/journalofethics.2017.19.6.ecas1-1706. [DOI] [PubMed] [Google Scholar]
- 30.Thurn T, Anneser J. Medical Students' Experiences of Moral Distress in End-of-Life Care. J Palliat Med. 2020;23(1):116–120. doi: 10.1089/jpm.2019.0049. [DOI] [PubMed] [Google Scholar]
- 31.Perni S, Pollack LR, Gonzalez WC, et al. Moral distress and burnout in caring for older adults during medical school training. BMC Med Educ. 2020;20(1):84. doi: 10.1186/s12909-020-1980-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oliver D. David Oliver: Moral distress in hospital doctors. BMJ. 2018;360:k1333. doi: 10.1136/bmj.k1333. [DOI] [PubMed] [Google Scholar]
- 33.Krishna LKR, Tan LHE, Ong YT, et al. Enhancing Mentoring in Palliative Care: An Evidence Based Mentoring Framework. J Med Educ Curric Dev. 2020. 10.1177/2382120520957649. [DOI] [PMC free article] [PubMed]
- 34.Ngiam LXL, Ong YA-O, Ng JX, et al. Impact of Caring for Terminally Ill Children on Physicians: A Systematic Scoping. Review. 2021; (1938-2715 (Electronic)). [DOI] [PubMed]
- 35.Kow CS, Teo YH, Teo YN, et al. A systematic scoping review of ethical issues in mentoring in medical schools. BMC Med Educ. 2020;20(1):246. doi: 10.1186/s12909-020-02169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bok C, Ng CH, Koh JWH, et al. Interprofessional communication (IPC) for medical students: a scoping review. BMC Med Educ. 2020;20(1):372. doi: 10.1186/s12909-020-02296-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kow CS, Teo YH, Teo YN, et al. A systematic scoping review of ethical issues in mentoring in medical schools. BMC Med Educ. 2020;20(1):1–10. doi: 10.1186/s12909-020-02169-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bok C, Ng CH, Koh JWH, et al. Interprofessional communication (IPC) for medical students: a scoping review. BMC Med Educ. 2020;20(1):372. doi: 10.1186/s12909-020-02296-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Krishna LKR, Tan LHE, Ong YT, et al. Enhancing Mentoring in Palliative Care: An Evidence Based Mentoring Framework. J Med Educ Curric Dev. 2020;7(7). 10.1177/2382120520957649. [DOI] [PMC free article] [PubMed]
- 40.Ong RRS, Seow REW, Wong RSM, et al. A Systematic Scoping Review of Narrative Reviews in Palliative Medicine Education. Palliative Medicine & Care: Open Access. 2020;7(1):1–22. [Google Scholar]
- 41.Bok C, Ng CH, Koh JWH, et al. Interprofessional communication (IPC) for medical students: a scoping review. BMC Med Educ. 2020;20(1):1–17. doi: 10.1186/s12909-020-02296-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ho CY, Kow CS, Chia CHJ, et al. The impact of death and dying on the personhood of medical students: a systematic scoping review. BMC Med Educ. 2020;20(1):1–16. doi: 10.1186/s12909-020-02411-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hong DZ, Lim AJS, Tan R, et al. A Systematic Scoping Review on Portfolios of Medical Educators. J Med Educ Curric Dev. 2021;8. 10.1177/23821205211000356. [DOI] [PMC free article] [PubMed]
- 44.Kuek JTY, Ngiam LXL, Kamal NHA, et al. The impact of caring for dying patients in intensive care units on a physician’s personhood: a systematic scoping review. Philos Ethics Humanit Med. 2020;15(1):1–16. doi: 10.1186/s13010-020-00096-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tay KT, Ng S, Hee JM, et al. Assessing Professionalism in Medicine–A Scoping Review of Assessment Tools from 1990 to 2018. J Med Educ Curric Dev. 2020;7. 10.1177/2382120520955159. [DOI] [PMC free article] [PubMed]
- 46.Tay KT, Tan XH, Tan LHE, et al. A systematic scoping review and thematic analysis of interprofessional mentoring in medicine from 2000 to 2019. J Interprof Care. 2020:1–13. [DOI] [PubMed]
- 47.Zhou YC, Tan SR, Tan CGH, et al. A systematic scoping review of approaches to teaching and assessing empathy in medicine. BMC Med Educ. 2021;21(1):1–15. doi: 10.1186/s12909-020-02436-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mah ZH, Wong RSM, Seow REW, et al. A Systematic Scoping Review of Systematic Reviews in Palliative Medicine Education. Palliative Medicine & Care: Open Access 2020;7(1):1-12.
- 49.Kamal NHA, Tan LHE, Wong RSM, et al. Enhancing education in Palliative Medicine: the role of Systematic Scoping Reviews. Palliative Medicine & Care: Open Access. 2020 7(1):1-11.
- 50.Peters MD, Godfrey CM, Khalil H, et al. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–146. doi: 10.1097/XEB.0000000000000050. [DOI] [PubMed] [Google Scholar]
- 51.Peters M, Godfrey C, McInerney P, et al. The Joanna Briggs Institute reviewers' manual 2015: methodology for JBI scoping reviews 2015 [cited. http://joannabriggs.org/assets/docs/sumari/Reviewers-Manual_Methodology-for-JBI-Scoping-Reviews_2015_v1.pdf
- 52.Pham MT, Rajić A, Greig JD, et al. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods. 2014;5(4):371–385. doi: 10.1002/jrsm.1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Pham MA-O, Rajić A, Greig JD, et al. A scoping review of scoping reviews: advancing the approach and enhancing the consistency. (1759-2887 (Electronic)). [DOI] [PMC free article] [PubMed]
- 54.Sandelowski M, Barroso J. Handbook for synthesizing qualitative research. Springer Publishing Company; 2006. [Google Scholar]
- 55.Ng YX, Koh ZYK, Yap HW, et al. Assessing mentoring: A scoping review of mentoring assessment tools in internal medicine between 1990 and 2019. 2020 (1932-6203 (Electronic)). [DOI] [PMC free article] [PubMed]
- 56.Wong G, Greenhalgh T, Westhorp G, et al. RAMESES publication standards: meta-narrative reviews. BMC Med. 2013;11(1):20. doi: 10.1186/1741-7015-11-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version. 2006;1:b92.
- 58.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- 59.Hsieh H-F, Shannon SE. Three Approaches to Qualitative Content Analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 60.Sambunjak D, Straus SE, Marušić A. Mentoring in academic medicine: a systematic review. JAMA. 2006;296(9):1103–1115. doi: 10.1001/jama.296.9.1103. [DOI] [PubMed] [Google Scholar]
- 61.France EF, Wells M, Lang H, et al. Why, when and how to update a meta-ethnography qualitative synthesis. Syst Rev. 2016;5(1):44. doi: 10.1186/s13643-016-0218-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Noblit GW, Hare RD. Meta-ethnography : synthesizing qualitative studies. Newbury Park, Sage Publications; 1988. English
- 63.Agzarian J, Blackmon SH, Cassivi SD, et al. Moving to the other side of the table-transitioning from residency to faculty and the value of mentorship. J Thorac Dis. 2019;11(Suppl 7):S1018–s1021. doi: 10.21037/jtd.2019.04.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Spencer J. Learning and teaching in the clinical environment. BMJ. 2003;326(7389):591–594. doi: 10.1136/bmj.326.7389.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Smith JM. Surgeon Coaching: Why and How. J Pediatr Orthop. 2020;40(Suppl 1):S33–s37. doi: 10.1097/BPO.0000000000001541. [DOI] [PubMed] [Google Scholar]
- 66.Mikhaiel JP, Pollack J, Buck E, et al. Graduating With Honors in Resilience: Creating a Whole New Doctor. Glob Adv Health Med. 2020;9. 10.1177/2164956120976356. [DOI] [PMC free article] [PubMed]
- 67.Stalmeijer RE, Dolmans DH, Wolfhagen IH, et al. Cognitive apprenticeship in clinical practice: can it stimulate learning in the opinion of students? Adv Health Sci Educ Theory Pract. 2009;14(4):535–546. doi: 10.1007/s10459-008-9136-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wolff M, Morgan H, Jackson J, et al. Academic coaching: Insights from the medical student’s perspective. Med Teach. 2020;42(2):172–177. doi: 10.1080/0142159X.2019.1670341. [DOI] [PubMed] [Google Scholar]
- 69.Lee ICJ, Koh H, Lai SH, et al. Academic coaching of medical students during the COVID-19 pandemic. Med Educ. 2020;54(12):1184–1185. doi: 10.1111/medu.14272. [DOI] [PubMed] [Google Scholar]
- 70.UNESCO. International Bureau of Education. Instruction. 2022; Available from: http://www.ibe.unesco.org/en/glossary-curriculum-terminology/i/instruction.
- 71.Barham D, de Beer W, Clark H. The role of professional supervision for palliative care doctors in New Zealand: a quantitative survey of attitudes and experiences. N Z Med J. 2019;132(1501):10–20. [PubMed] [Google Scholar]
- 72.Hawkins P, Robin S. Supervision in the Helping Professions. UK: McGraw Hill Open University Press; 2012. [Google Scholar]
- 73.Kilminster S, Cottrell D, Grant J, et al. AMEE Guide No. 27: Effective educational and clinical supervision. Med Teach. 2007;29(1):2–19. doi: 10.1080/01421590701210907. [DOI] [PubMed] [Google Scholar]
- 74.Haque W, Gurney T, Reed WG, et al. Key Attributes of a Medical Learning Community Mentor at One Medical School. Med Sci Educ. 2019;29(3):721–730. doi: 10.1007/s40670-019-00746-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Beanlands RA, Robinson LJ, Venance SL. An LGBTQ+ mentorship program enriched the experience of medical students and physician mentors. Can Med Educ J. 2020;11(6):e159–e162. doi: 10.36834/cmej.69936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Latham K, Dong T, Schreiber D, et al. Uniformed Services University Medical Student Mentorship Experiences and Gender From 2010 to 2017. Mil Med. 2020;185(7-8):e1277–e1283. doi: 10.1093/milmed/usaa064. [DOI] [PubMed] [Google Scholar]
- 77.Berman L, Rosenthal MS, Curry LA, et al. Attracting surgical clerks to surgical careers: role models, mentoring, and engagement in the operating room. J Am Coll Surg. 2008;207(6):793–800. doi: 10.1016/j.jamcollsurg.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 78.Henry-Noel N, Bishop M, Gwede CK, et al. Mentorship in Medicine and Other Health Professions. J Cancer Educ. 2019;34(4):629–637. doi: 10.1007/s13187-018-1360-6. [DOI] [PubMed] [Google Scholar]
- 79.Tomizawa Y. Role Modeling for Female Surgeons in Japan. Tohoku J Exp Med. 2019;248(3):151–158. doi: 10.1620/tjem.248.151. [DOI] [PubMed] [Google Scholar]
- 80.Rodenhauser P, Rudisill JR, Dvorak R. Skills for Mentors and Protégés Applicable to Psychiatry. Acad Psychiatry. 2000;24:14–27. doi: 10.1007/BF03340067. [DOI] [Google Scholar]
- 81.Marshall AL, Dversdal RK, Murphy M, et al. WOMENtorship: The #WomenInMedicine perspective. Med Teach. 2020;42(2):228–230. doi: 10.1080/0142159X.2019.1671967. [DOI] [PubMed] [Google Scholar]
- 82.Hee JM, Yap HW, Ong ZX, et al. Understanding the Mentoring Environment Through Thematic Analysis of the Learning Environment in Medical Education: a Systematic Review. J Gen Intern Med. 2019;34(10):2190–2199. doi: 10.1007/s11606-019-05000-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hawkins A, Jones K, Stanton A. A mentorship programme for final-year students. Clin Teach. 2014;11(5):345–349. doi: 10.1111/tct.12149. [DOI] [PubMed] [Google Scholar]
- 84.Cowan F, Flint S. The importance of mentoring for junior doctors. BMJ. 2012.
- 85.Drolet BC, Sangisetty S, Mulvaney PM, et al. A mentorship-based preclinical elective increases exposure, confidence, and interest in surgery. Am J Surg. 2014;207(2):179–186. doi: 10.1016/j.amjsurg.2013.07.031. [DOI] [PubMed] [Google Scholar]
- 86.Kalén S, Ponzer S, Silén C. The core of mentorship: medical students' experiences of one-to-one mentoring in a clinical environment. Adv Health Sci Educ. 2012;17(3):389–401. doi: 10.1007/s10459-011-9317-0. [DOI] [PubMed] [Google Scholar]
- 87.Kalén S, Stenfors-Hayes T, Hylin U, et al. Mentoring medical students during clinical courses: a way to enhance professional development. Med Teach. 2010;32(8):e315–e321. doi: 10.3109/01421591003695295. [DOI] [PubMed] [Google Scholar]
- 88.Mihalynuk T, Bates J, Page G, et al. Student learning experiences in a longitudinal clerkship programme. Med Educ. 2008;42(7):729–732. doi: 10.1111/j.1365-2923.2008.03040.x. [DOI] [PubMed] [Google Scholar]
- 89.Ogunyemi D, Solnik MJ, Alexander C, et al. Promoting residents' professional development and academic productivity using a structured faculty mentoring program. Teach Learn Med. 2010;22(2):93–96. doi: 10.1080/10401331003656413. [DOI] [PubMed] [Google Scholar]
- 90.Toh YP, Lam B, Soo JJE, et al. Developing Palliative Care Physicians through Mentoring Relationships. 2017. [Google Scholar]
- 91.Kaewpila W, Thaipisuttikul P, Awirutworakul T, et al. Depressive disorders in Thai medical students: an exploratory study of institutional, cultural, and individual factors. Int J Med Educ. 2020;11:252–260. doi: 10.5116/ijme.5fbe.4ce5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Jordan J, Watcha D, Cassella C, et al. Impact of a Mentorship Program on Medical Student Burnout. AEM Educ Train. 2019;3(3):218–225. doi: 10.1002/aet2.10354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rabatin JS, Lipkin M, Jr, Rubin AS, et al. A year of mentoring in academic medicine: case report and qualitative analysis of fifteen hours of meetings between a junior and senior faculty member. J Gen Intern Med. 2004;19(5 Pt 2):569–573. doi: 10.1111/j.1525-1497.2004.30137.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Bhatnagar V, Diaz S, Bucur PA. The Need for More Mentorship in Medical School. Cureus. 2020;12(5):e7984. doi: 10.7759/cureus.7984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Honavar SG. Mentoring is a serious business. Indian J Ophthalmol. 2019;67(12):1915–1917. doi: 10.4103/ijo.IJO_2161_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Leslie K, Lingard L, Whyte S. Junior faculty experiences with informal mentoring. Med Teach. 2005;27(8):693–698. doi: 10.1080/01421590500271217. [DOI] [PubMed] [Google Scholar]
- 97.Lin CD, Lin BY, Lin CC, et al. Redesigning a clinical mentoring program for improved outcomes in the clinical training of clerks. Med Educ Online. 2015;20:28327. doi: 10.3402/meo.v20.28327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Omary MB. Mentoring the Mentor: Another Tool to Enhance Mentorship. Gastroenterology. 2008;135(1):13–16. doi: 10.1053/j.gastro.2008.05.065. [DOI] [PubMed] [Google Scholar]
- 99.Louie M, Moulder JK, Wright K, et al. Mentoring millennials in surgical education. Curr Opin Obstet Gynecol. 2019;31(4):279–284. doi: 10.1097/GCO.0000000000000546. [DOI] [PubMed] [Google Scholar]
- 100.Wetter DA. Personal reflections on mentorship as a pathway toward sustaining a joyful dermatologic practice: Part I: Influential mentors during training and early career. Clin Dermatol. 2020;38(1):126–128. doi: 10.1016/j.clindermatol.2019.06.005. [DOI] [PubMed] [Google Scholar]
- 101.McDaniel CE, Rooholamini SN, Desai AD, et al. A Qualitative Evaluation of a Clinical Faculty Mentorship Program Using a Realist Evaluation Approach. Acad Pediatr. 2020;20(1):104–112. doi: 10.1016/j.acap.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 102.Patel N, Awan O. Mentorship and Sponsorship: Are You in Good Hands? Curr Probl Diagn Radiol. 2020;49(1):–1. [DOI] [PubMed]
- 103.Thiedke C, Blue AV, Chessman AW, et al. Student observations and ratings of preceptor's interactions with patients: the hidden curriculum. Teach Learn Med. 2004;16(4):312–316. doi: 10.1207/s15328015tlm1604_2. [DOI] [PubMed] [Google Scholar]
- 104.Harrison LM, Woods RJ, McCarthy MC, et al. Development and implementation of a sustainable research curriculum for general surgery residents: A foundation for developing a research culture. Am J Surg. 2020;220(1):105–108. doi: 10.1016/j.amjsurg.2019.09.028. [DOI] [PubMed] [Google Scholar]
- 105.Hu A. Reflections: Starting an Otolaryngology Medical Student Interest Group. Otolaryngol Head Neck Surg. 2020;162(2):155–156. doi: 10.1177/0194599819886121. [DOI] [PubMed] [Google Scholar]
- 106.Keser Z, Rodriguez YA, Tremont J, et al. The role of residents in medical students’ neurology education: current status and future perspectives. BMC Med Educ. 2020;20(1):115. doi: 10.1186/s12909-020-02036-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Santen SA, Wolff MS, Saxon K, et al. Factors Affecting Entrustment and Autonomy in Emergency Medicine: "How much rope do I give them?". West J Emerg Med. 2019;20(1):58–63. doi: 10.5811/westjem.2018.10.39843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Ng CWQ, Syn NL, Hussein RBM, et al. Push and pull factors, and the role of residents in nurturing medical students' interest in surgery as a career option in a multicultural Asian context: Results of a prospective national cohort study. Am J Surg. 2020;220(6):1549–1556. doi: 10.1016/j.amjsurg.2020.04.036. [DOI] [PubMed] [Google Scholar]
- 109.Gill SD, Stella J, Blazeska M, et al. Distant supervision of trainee emergency physicians undertaking a remote placement: A preliminary evaluation. Emerg Med Australas. 2020;32(3):446–456. doi: 10.1111/1742-6723.13440. [DOI] [PubMed] [Google Scholar]
- 110.Iloh GUP, Chukwuonye ME, Onya ON, et al. Mentoring in a resource-constrained context: A single-institutional cross-sectional study of the prevalence, benefits, barriers and predictors among post-graduate medical college fellows and members in South-Eastern Nigeria. Niger Postgrad Med J. 2019;26(1):38–44. doi: 10.4103/npmj.npmj_173_18. [DOI] [PubMed] [Google Scholar]
- 111.Nothnagle M, Goldman R, Quirk M, et al. Promoting self-directed learning skills in residency: a case study in program development. Acad Med. 2010;85(12):1874–1879. doi: 10.1097/ACM.0b013e3181fa02a4. [DOI] [PubMed] [Google Scholar]
- 112.Ras T, Schweitzer B, Bresick G, et al. Training family physicians: A qualitative exploration of experiences of registrars in a family medicine training programme in Cape Town, South Africa. S Afr Fam Pract. 2004;62(1):e1–e6. doi: 10.4102/safp.v62i1.5023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lennon MJ, McGrail MR, O'Sullivan B, et al. Understanding the professional satisfaction of hospital trainees in Australia. Med Educ. 2020;54(5):419–426. doi: 10.1111/medu.14041. [DOI] [PubMed] [Google Scholar]
- 114.Farnan JM, Petty LA, Georgitis E, et al. A systematic review: the effect of clinical supervision on patient and residency education outcomes. Acad Med. 2012;87(4):428–442. doi: 10.1097/ACM.0b013e31824822cc. [DOI] [PubMed] [Google Scholar]
- 115.McKenzie S, Burgess A, Mellis C. "A Taste of Real Medicine": Third Year Medical Students' Report Experiences of Early Workplace Encounters. Adv Med Educ Pract. 2020;11:717–725. doi: 10.2147/AMEP.S230946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Rustici MJ, Moreira M, Buchanan J, et al. Educational Benefits of Allowing Pediatrician Supervision of Emergency Medicine Residents. J Grad Med Educ. 2020;12(2):185–192. doi: 10.4300/JGME-D-19-00426.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Sheng AY, Clark A, Amanti C. Supervision of Resident Physicians. Emerg Med Clin North Am. 2020;38(2):339–351. doi: 10.1016/j.emc.2020.02.004. [DOI] [PubMed] [Google Scholar]
- 118.Brown J, Reid H, Dornan T, et al. Becoming a clinician: Trainee identity formation within the general practice supervisory relationship. Med Educ. 2020;54:1005–1993. doi: 10.1111/medu.14203. [DOI] [PubMed] [Google Scholar]
- 119.Insetta Emily R, Christmas C. A Novel Intimate Partner Violence Curriculum for Internal Medicine Residents: Development, Implementation, and Evaluation. MedEdPORTAL. 2020;16:10905. doi: 10.15766/mep_2374-8265.10905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Shojania KG, Fletcher KE, Saint S. Graduate medical education and patient safety: a busy--and occasionally hazardous--intersection. Ann Intern Med. 2006;145(8):592–598. doi: 10.7326/0003-4819-145-8-200610170-00008. [DOI] [PubMed] [Google Scholar]
- 121.Itani KM, DePalma RG, Schifftner T, et al. Surgical resident supervision in the operating room and outcomes of care in Veterans Affairs hospitals. Am J Surg. 2005;190(5):725–731. doi: 10.1016/j.amjsurg.2005.06.042. [DOI] [PubMed] [Google Scholar]
- 122.Trowbridge RL, Almeder L, Jacquet M, et al. The effect of overnight in-house attending coverage on perceptions of care and education on a general medical service. J Grad Med Educ. 2010;2(1):53–56. doi: 10.4300/JGME-D-09-00056.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Dorsey JK, Beason AM, Verhulst SJ. Relationships Matter: Enhancing Trainee Development with a (Simple) Clerkship Curriculum Reform. Teach Learn Med. 2019;31(1):76–86. doi: 10.1080/10401334.2018.1479264. [DOI] [PubMed] [Google Scholar]
- 124.Sinai J, Tiberius RG, de Groot J, et al. Developing a training program to improve supervisor-resident relationships, step 1: defining the types of issues. Teach Learn Med. 2001;13(2):80–85. doi: 10.1207/S15328015TLM1302_2. [DOI] [PubMed] [Google Scholar]
- 125.Mansour I, Dyer S, Chhabra N. Impact of Resident-Paired Schedule on Medical Student Education and Impression of Residency Programs. West J Emerg Med. 2020;22(1):15–19. doi: 10.5811/westjem.2020.12.48761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Rothberg MB, Kleppel R, Friderici JL, et al. Implementing a resident research program to overcome barriers to resident research. Acad Med. 2014;89(8):1133–1139. doi: 10.1097/ACM.0000000000000281. [DOI] [PubMed] [Google Scholar]
- 127.Shah P, Zuckerman SP, Thompson C, et al. First-Year Radiology Residents Teaching Anatomy to First-Year Medical Students: A Symbiotic Relationship. Curr Probl Diagn Radiol. 2020;49(3):157–160. doi: 10.1067/j.cpradiol.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 128.Back AL, Arnold RM, Baile WF, et al. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med. 2007;167(5):453–460. doi: 10.1001/archinte.167.5.453. [DOI] [PubMed] [Google Scholar]
- 129.Balmer DF, Giardino AP, Richards BF. The dance between attending physicians and senior residents as teachers and supervisors. Pediatrics. 2012;129(5):910–915. doi: 10.1542/peds.2011-2674. [DOI] [PubMed] [Google Scholar]
- 130.Chapman L, Mysko C, Coombridge H. Development of teaching, mentoring and supervision skills for basic training registrars: a frustrated apprenticeship? Intern Med J. 2021;51(11):1847–1853. doi: 10.1111/imj.14935. [DOI] [PubMed] [Google Scholar]
- 131.Dornan T, Boshuizen H, King N, et al. Experience-based learning: a model linking the processes and outcomes of medical students' workplace learning. Med Educ. 2007;41(1):84–91. doi: 10.1111/j.1365-2929.2006.02652.x. [DOI] [PubMed] [Google Scholar]
- 132.Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(10 Suppl):S70–S81. doi: 10.1097/00001888-200410001-00022. [DOI] [PubMed] [Google Scholar]
- 133.Fallowfield L, Jenkins V, Farewell V, et al. Efficacy of a Cancer Research UK communication skills training model for oncologists: a randomised controlled trial. Lancet. 2002;359(9307):650–656. doi: 10.1016/S0140-6736(02)07810-8. [DOI] [PubMed] [Google Scholar]
- 134.Fallowfield L, Jenkins V, Farewell V, et al. Enduring impact of communication skills training: results of a 12-month follow-up. Br J Cancer. 2003;89(8):1445–1449. doi: 10.1038/sj.bjc.6601309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Jochemsen-van der Leeuw HG, van Dijk N, Wieringa-de WM. Assessment of the clinical trainer as a role model: a Role Model Apperception Tool (RoMAT) Acad Med. 2014;89(4):671–677. doi: 10.1097/ACM.0000000000000169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Lees MC, Zheng B, Daniels LM, et al. Factors Affecting the Development of Confidence Among Surgical Trainees. J Surg Educ. 76(3):674–83. [DOI] [PubMed]
- 137.Lefkowitz A, Meitar D, Kuper A. Can doctors be taught virtue?. J Eval Clin Pract 2021 27(3):543-548 doi.org/10.1111/jep.13398. [DOI] [PubMed]
- 138.Liénard A, Merckaert I, Libert Y, et al. Is it possible to improve residents breaking bad news skills? A randomised study assessing the efficacy of a communication skills training program. Br J Cancer. 2010;103(2):171–177. doi: 10.1038/sj.bjc.6605749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Lin YK, Yen-Ju Lin B, Chen DY. Do teaching strategies matter? Relationships between various teaching strategies and medical students' wellbeing during clinical workplace training. Med Teach. 2020;42(1):39–45. doi: 10.1080/0142159X.2019.1648777. [DOI] [PubMed] [Google Scholar]
- 140.Hauer KE, Wachter RM, McCulloch CE, et al. Effects of hospitalist attending physicians on trainee satisfaction with teaching and with internal medicine rotations. Arch Intern Med. 2004;164(17):1866–1871. doi: 10.1001/archinte.164.17.1866. [DOI] [PubMed] [Google Scholar]
- 141.Celenza A, Rogers IR. Qualitative evaluation of a formal bedside clinical teaching programme in an emergency department. Emerg Med J. 2006;23(10):769–773. doi: 10.1136/emj.2006.037796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Brown RF, Butow PN, Boyle F, et al. Seeking informed consent to cancer clinical trials; evaluating the efficacy of doctor communication skills training. Psychooncology. 2007;16(6):507–516. doi: 10.1002/pon.1095. [DOI] [PubMed] [Google Scholar]
- 143.Edwards K, Cozens T. Establishing a regular systems-based teaching programme for core medical trainees within a district general hospital. Future Healthc J. 2019;6(Suppl 2):32–33. doi: 10.7861/futurehealth.6-2-s32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Gibson LE, White-Dzuro GA, Lindsay PJ, et al. Ensuring competency in focused cardiac ultrasound: a systematic review of training programs. J Intensive Care. 2020;8(1):93. doi: 10.1186/s40560-020-00503-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Glenn-Cox S, Hird K, Sweetman G, et al. Radiology teaching for interns: Experiences, current practice and suggestions for improvement. J Med Imaging Radiat Oncol. 2019;63(4):454–460. doi: 10.1111/1754-9485.12896. [DOI] [PubMed] [Google Scholar]
- 146.Kelly M, Sturman N, Pakchung D. Teaching and learning in general practice: ethical and legal considerations for GP teachers and medical students. Med J Aust. 2020;212(9):403–405.e1. doi: 10.5694/mja2.50593. [DOI] [PubMed] [Google Scholar]
- 147.Butow P, Cockburn J, Girgis A, et al. Increasing oncologists' skills in eliciting and responding to emotional cues: evaluation of a communication skills training program. Psychooncology. 2008;17(3):209–218. doi: 10.1002/pon.1217. [DOI] [PubMed] [Google Scholar]
- 148.Davies JH, Tan K, Jenkins HR. The current status of senior house officer postgraduate education in a single region. Med Educ. 2000;34(5):367–370. doi: 10.1046/j.1365-2923.2000.00518.x. [DOI] [PubMed] [Google Scholar]
- 149.Finset A, Ekeberg O, Eide H, et al. Long term benefits of communication skills training for cancer doctors. Psychooncology. 2003;12(7):686–693. doi: 10.1002/pon.691. [DOI] [PubMed] [Google Scholar]
- 150.Gilligan C, Brubacher SP, Powell MB. Assessing the training needs of medical students in patient information gathering. BMC Med Educ. 2020;20(1):61. doi: 10.1186/s12909-020-1975-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Koea J, Rahiri J-L, Ronald M. Affirmative action programmes in postgraduate medical and surgical training—A narrative review. Med Educ 2021 55(3):309-316 doi.org/10.1111/medu.14350. [DOI] [PubMed]
- 152.Thomson O'Brien MA, Freemantle N, Oxman AD, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2001;2009(2):Cd003030. doi: 10.1002/14651858.CD003030. [DOI] [PubMed] [Google Scholar]
- 153.Forsetlund L, Bjørndal A, Rashidian A, et al. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2009;2009(2):Cd003030. doi: 10.1002/14651858.CD003030.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Edwards R, White M, Gray J, et al. Use of a journal club and letter-writing exercise to teach critical appraisal to medical undergraduates. Med Educ. 2001;35(7):691–694. doi: 10.1046/j.1365-2923.2001.00972.x. [DOI] [PubMed] [Google Scholar]
- 155.Gaetke-Udager K, Brown RKJ, Centonze CP, et al. Advanced Quality Training in Radiology: Inaugural Report of a 2-Year Program. AJR Am J Roentgenol. 2019;5:1–9. doi: 10.2214/AJR.18.20734. [DOI] [PubMed] [Google Scholar]
- 156.Marušic A, Marušic M. Teaching Students How to Read and Write Science: A Mandatory Course on Scientific Research and Communication in Medicine. Acad Med. 2003;78(12):1235–1239. doi: 10.1097/00001888-200312000-00007. [DOI] [PubMed] [Google Scholar]
- 157.Razavi D, Merckaert I, Marchal S, et al. How to optimize physicians' communication skills in cancer care: results of a randomized study assessing the usefulness of posttraining consolidation workshops. J Clin Oncol. 2003;21(16):3141–3149. doi: 10.1200/JCO.2003.08.031. [DOI] [PubMed] [Google Scholar]
- 158.Herr KD, George E, Agarwal V, et al. Aligning the Implicit Curriculum with the Explicit Curriculum in Radiology. Acad Radiol. 2020;27(9):1268–1273. doi: 10.1016/j.acra.2019.12.028. [DOI] [PubMed] [Google Scholar]
- 159.Goelz T, Wuensch A, Stubenrauch S, et al. Specific training program improves oncologists' palliative care communication skills in a randomized controlled trial. J Clin Oncol. 2011;29(25):3402–3407. doi: 10.1200/JCO.2010.31.6372. [DOI] [PubMed] [Google Scholar]
- 160.El-Gabri D, McDow AD, Quamme SP, et al. Surgical Coaching for Advancement of Global Surgical Skills and Capacity: A Systematic Review. J Surg Res. 2020;246:499–505. doi: 10.1016/j.jss.2019.09.039. [DOI] [PubMed] [Google Scholar]
- 161.Malling B, de Lasson L, Just E, et al. How group coaching contributes to organisational understanding among newly graduated doctors. BMC Med Educ. 2020;20(1):193. doi: 10.1186/s12909-020-02102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Wolff M, Stojan J, Buckler S, et al. Coaching to improve self-directed learning. Clin Teach 2020 17(4):408-412 doi.org/10.1111/tct.13109. [DOI] [PubMed]
- 163.Marcus CH, Newman LR, Winn AS, et al. TEACH and repeat: Deliberate practice for teaching. Clin Teach 2020 17(6):688-694 doi.org/10.1111/tct.13205. [DOI] [PubMed]
- 164.Graddy R, Reynolds SS, Wright SM. Longitudinal resident coaching in the outpatient setting: A novel intervention to improve ambulatory consultation skills. Perspect Med Educ. 2020;9(3):186–190. doi: 10.1007/s40037-020-00573-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Guerrasio J, Brooks E, Rumack CM, et al. The Evolution of Resident Remedial Teaching at One Institution. Acad Med. 2019;94(12):1891–1894. doi: 10.1097/ACM.0000000000002894. [DOI] [PubMed] [Google Scholar]
- 166.Timberlake MD, Stefanidis D, Gardner AK. Examining the impact of surgical coaching on trainee physiologic response and basic skill acquisition. Surg Endosc. 2018;32(10):4183–4190. doi: 10.1007/s00464-018-6163-7. [DOI] [PubMed] [Google Scholar]
- 167.Thomas EJ, Williams AL, Reichman EF, et al. Team training in the neonatal resuscitation program for interns: teamwork and quality of resuscitations. Pediatrics. 2010;125(3):539–546. doi: 10.1542/peds.2009-1635. [DOI] [PubMed] [Google Scholar]
- 168.Judson TJ, Press MJ, Detsky AS. Saving without compromising: Teaching trainees to safely provide high value care. Healthc (Amst) 2019;7(1):4–6. doi: 10.1016/j.hjdsi.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 169.Sng JH, Pei Y, Toh YP, et al. Mentoring relationships between senior physicians and junior doctors and/or medical students: A thematic review. Med Teach. 2017;39(8):866–875. doi: 10.1080/0142159X.2017.1332360. [DOI] [PubMed] [Google Scholar]
- 170.Fornari A, Murray TS, Menzin AW, et al. Mentoring program design and implementation in new medical schools. Med Educ Online. 2014;19:24570. doi: 10.3402/meo.v19.24570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Chia EWY, Tay KT, Xiao S, et al. The Pivotal Role of Host Organizations in Enhancing Mentoring in Internal Medicine: A Scoping Review. J Med Educ Curric Dev. 2020. 10.1177/2382120520956647. [DOI] [PMC free article] [PubMed]
- 172.Brook EM, Hu CH, Li X, et al. The Influence of Mentors in Orthopedic Surgery. Orthopedics. 2020;43(1):e37–e42. doi: 10.3928/01477447-20191122-02. [DOI] [PubMed] [Google Scholar]
- 173.Hart RA, Eltorai AEM, Yanney K, et al. Update on Mentorship in Orthopaedic Resident Education: A Report from the American Orthopaedic Association. J Bone Joint Surg Am. 2020;102(5):e20. doi: 10.2106/JBJS.18.00697. [DOI] [PubMed] [Google Scholar]
- 174.Hauer KE, Teherani A, Dechet A, et al. Medical students' perceptions of mentoring: a focus-group analysis. Med Teach. 2005;27(8):732–734. doi: 10.1080/01421590500271316. [DOI] [PubMed] [Google Scholar]
- 175.Tan YS, Teo SWA, Pei Y, et al. A framework for mentoring of medical students: thematic analysis of mentoring programmes between 2000 and 2015. Adv Health Sci Educ Theory Pract. 2018;23(4):671–697. doi: 10.1007/s10459-018-9821-6. [DOI] [PubMed] [Google Scholar]
- 176.Chong JY, Ching AH, Renganathan Y, et al. Enhancing mentoring experiences through e-mentoring: a systematic scoping review of e-mentoring programs between 2000 and 2017. Adv Health Sci Educ Theory Pract. 2020;25(1):195–226. doi: 10.1007/s10459-019-09883-8. [DOI] [PubMed] [Google Scholar]
- 177.Cochran A, Elder WB, Neumayer LA. Characteristics of Effective Mentorship for Academic Surgeons: A Grounded Theory Model. Ann Surg. 2019;269(2):269–274. doi: 10.1097/SLA.0000000000002487. [DOI] [PubMed] [Google Scholar]
- 178.Dolmans DH, Wolfhagen IH, Essed GG, et al. The impacts of supervision, patient mix, and numbers of students on the effectiveness of clinical rotations. Acad Med. 2002;77(4):332–335. doi: 10.1097/00001888-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 179.Farrington R, Collins L, Fisher P, et al. Clinical Debrief: learning and well-being together. Clin Teach 2019 16(4):329-334 https://doi.org/10.1111/tct.13055. [DOI] [PMC free article] [PubMed]
- 180.Tran K, Tran GT, Fuller R. West Yorkshire Mentor Scheme: teaching and development. Clin Teach. 2014;11(1):48–52. doi: 10.1111/tct.12058. [DOI] [PubMed] [Google Scholar]
- 181.Lanier WL, Rose SH. The Contemporary Medical Community: Leadership, Mentorship, and Career Choices. Mayo Clin Proc. 2008;83(9):974–977. doi: 10.4065/83.9.974. [DOI] [PubMed] [Google Scholar]
- 182.Wasserstein AG, Quistberg DA, Shea JA. Mentoring at the University of Pennsylvania: results of a faculty survey. J Gen Intern Med. 2007;22(2):210–214. doi: 10.1007/s11606-006-0051-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Barab S, MaKinster J, Scheckler R. Designing system dualities: characterizing an online professional development. In: Barab S, Kling R, Gray J, editors. In Designing for virtual communities in the service of learning. Cambridge: Cambridge University Press; 2004. [Google Scholar]
- 184.Cruess RL, Cruess SR, Boudreau JD, et al. A schematic representation of the professional identity formation and socialization of medical students and residents: a guide for medical educators. Acad Med. 2015;90(6):718–725. doi: 10.1097/ACM.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 185.Hur Y, Cho AR, Song EJ, et al. Evaluation of a systematic career coaching program for medical students in Korea using the Career Readiness Inventory. J Educ Eval Health Prof. 2018;15(0):10. doi: 10.3352/jeehp.2018.15.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Hur Y. Definition of character for medical education based on expert opinions in Korea. J Educ Eval Health Prof. 2021;18(0):26–20. doi: 10.3352/jeehp.2021.18.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Ardekani A, Hosseini SA, Tabari P, et al. Student support systems for undergraduate medical students during the COVID-19 pandemic: a systematic narrative review of the literature. BMC Med Educ. 2021;21(1):352. doi: 10.1186/s12909-021-02791-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.White S, Foster R, Marks J, et al. The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis. BMC Psychiatry. 2020;20(1):534. doi: 10.1186/s12888-020-02923-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Chua WJ, Cheong CWS, Lee FQH, et al. Structuring Mentoring in Medicine and Surgery. A Systematic Scoping Review of Mentoring Programs Between 2000 and 2019. J Contin Educ Health Prof. 2020;40(3):158–168. doi: 10.1097/CEH.0000000000000308. [DOI] [PubMed] [Google Scholar]
- 190.Ng YX, Koh ZYK, Yap HW, et al. Assessing mentoring: A scoping review of mentoring assessment tools in internal medicine between 1990 and 2019. PLoS One. 2020;15(5):–e0232511. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Appendix A. Tabulated Summaries
Data Availability Statement
All data generated or analysed during this review are included in this published article and its supplementary files.