Abstract
OBJECTIVE
Finerenone significantly improved cardiorenal outcomes in patients with chronic kidney disease (CKD) and type 2 diabetes (T2D) in the Finerenone in Reducing Kidney Failure and Disease Progression in Diabetic Kidney Disease trial. We explored whether baseline HbA1c level and insulin treatment influenced outcomes.
RESEARCH DESIGN AND METHODS
Patients with T2D, urine albumin-to-creatinine ratio (UACR) of 30–5,000 mg/g, estimated glomerular filtration rate (eGFR) of 25 to <75 mL/min/1.73 m2, and treated with optimized renin–angiotensin system blockade were randomly assigned to receive finerenone or placebo. Efficacy outcomes included kidney (kidney failure, sustained decrease ≥40% in eGFR from baseline, or renal death) and cardiovascular (cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for heart failure) composite endpoints. Patients were analyzed by baseline insulin use and by baseline HbA1c <7.5% (58 mmol/mol) or ≥7.5%.
RESULTS
Of 5,674 patients, 3,637 (64.1%) received insulin at baseline. Overall, 5,663 patients were included in the analysis for HbA1c; 2,794 (49.3%) had baseline HbA1c <7.5% (58 mmol/mol). Finerenone significantly reduced risk of the kidney composite outcome independent of baseline HbA1c level and insulin use (Pinteraction = 0.41 and 0.56, respectively). Cardiovascular composite outcome incidence was reduced with finerenone irrespective of baseline HbA1c level and insulin use (Pinteraction = 0.70 and 0.33, respectively). Although baseline HbA1c level did not affect kidney event risk, cardiovascular risk increased with higher HbA1c level. UACR reduction was consistent across subgroups. Adverse events were similar between groups regardless of baseline HbA1c level and insulin use; few finerenone-treated patients discontinued treatment because of hyperkalemia.
CONCLUSIONS
Finerenone reduces kidney and cardiovascular outcome risk in patients with CKD and T2D, and risks appear consistent irrespective of HbA1c levels or insulin use.
Introduction
Chronic kidney disease (CKD) in patients with type 2 diabetes (T2D) is a major global health challenge, affecting an estimated 160 million people aged 20–79 years worldwide (1–3). Clinical guidelines for the management of CKD in patients with T2D recommend control of hypertension and hyperglycemia, with individualized targets for the level of HbA1c of <6.5% (48 mmol/mol) to <8% (64 mmol/mol), as well as the use of a renin–angiotensin system blocker (an ACE inhibitor or angiotensin receptor blocker [ARB]) and, more recently, a sodium–glucose cotransporter 2 inhibitor (SGLT-2i) (4–7).
Insulin is often used as a glucose-lowering agent in patients with CKD and T2D, especially in patients with moderate to severe CKD in whom many other glucose-lowering agents cannot be used (8). It has been suggested that insulin treatment may increased sodium retention and hypertension (9), and hyperinsulinemia has been associated with inflammation in patients with T2D (10). Insulin is often used when β-cell failure is apparent and oral agents have failed; thus, insulin use at baseline may be suggestive of patients with complicated diabetes (11).
Available evidence suggests that glycemic control influences kidney risk in patients with T2D. Observational data suggest that poor glycemic control increases the risk for progression of CKD in patients with T2D with moderately elevated albuminuria (12), and data from clinical trials have shown that intensive blood glucose control improves kidney outcomes in patient groups with T2D and T2D with mild CKD (13–15). However, evidence from large phase 3 trials regarding the relationship between glycemic control and disease outcomes in patients with moderate to severe CKD and T2D is lacking.
The prognostic implication and response to treatment with a mineralocorticoid receptor antagonist (MRA) relative to glycemic control as reflected by HbA1c levels is not well understood (16). Limited available data suggest that the nonselective steroidal MRA spironolactone may increase HbA1c levels in patients with and without diabetes, whereas the more selective steroidal MRA eplerenone has no effect on HbA1c levels (17,18). Finerenone is a novel, selective, nonsteroidal MRA that significantly reduced the risk of adverse kidney and cardiovascular (CV) outcomes in patients with CKD and T2D in the Finerenone in Reducing Kidney Failure and Disease Progression in Diabetic Kidney Disease (FIDELIO-DKD) phase 3 trial, without influencing HbA1c levels (19,20). The main aim of this analysis was to evaluate kidney, CV, and safety outcomes from the FIDELIO-DKD trial according to baseline HbA1c level, and to determine whether baseline glycemic control affects the previously reported benefits of treatment with finerenone. Furthermore, the effects of insulin treatment at baseline on efficacy and safety outcomes were investigated because of the interdependency of insulin treatment and glycemic control (serum HbA1c levels) in patients with CKD and T2D. As such, we hypothesized that finerenone would not influence HbA1c levels and that the treatment effect of finerenone would not be modified by HbA1c or by insulin use at baseline.
Research Design and Methods
Study Design and Participants
The study design of FIDELIO-DKD, a multicenter, randomized, double-blind, placebo-controlled, parallel-group, event-driven phase 3 trial, has been described previously (19,21). The trial was conducted in accordance with the principles of the Declaration of Helsinki; the protocol was approved by relevant regulatory authorities and ethics committees at each trial site, and written informed consent was obtained from all participants. Eligible patients were aged ≥18 years and had clinically diagnosed T2D as defined by the American Diabetes Association, with either moderately elevated albuminuria (defined as urine albumin-to-creatinine ratio [UACR] of 30 to <300 mg/g), an estimated glomerular filtration rate [eGFR] of 25 to <60 mL/min/1.73 m2, and a history of diabetic retinopathy, or severely elevated albuminuria (defined as UACR ≥300 to ≤5,000 mg/g) and an eGFR of 25 to <75 mL/min/1.73 m2. Patients with HbA1c >12% at screening were excluded. Furthermore, patients were required to have been treated with a maximum tolerated dose of an ACE inhibitor or ARB in accordance with the manufacturer’s label for ≥4 weeks prior to the screening visit and to have a serum potassium level ≤4.8 mmol/L at the run-in and screening visits. Patients with known nondiabetic kidney disease, chronic symptomatic heart failure with reduced ejection fraction (New York Heart Association class II–IV), a recent history of dialysis for acute kidney failure or a kidney transplant, or uncontrolled hypertension were excluded. The primary and secondary efficacy and safety outcomes have been reported previously (19). The study is registered with the EU Clinical Trials Register (EudraCT 2015-000990-11) and ClinicalTrials.gov (NCT02540993).
Procedures and Outcomes
Patients were randomly assigned (1:1) to receive once-daily oral treatment with finerenone (10 or 20 mg) or matched placebo; patients with an eGFR of 25 to <60 mL/min/1.73 m2 at the screening visit received a starting dose of 10 mg once daily, and those with an eGFR ≥60 mL/min/1.73 m2 received a starting dose of 20 mg once daily. An increase in the dose of study medication from 10 mg to the target dose of 20 mg once daily was encouraged after 1 month, provided the serum potassium level was ≤4.8 mmol/L and the eGFR was stable; a decrease in the dose from 20 to 10 mg once daily was allowed any time after the initiation of finerenone or placebo for safety reasons. During the study, healthcare providers were advised to follow local guidelines for the management of T2D, including recommendations for glycemic control; concomitant antidiabetic drugs were recorded by the investigators. Oral antidiabetics included dipeptidyl peptidase 4 inhibitors, SGLT-2is, biguanides, sulfonylureas, α-glucosidase inhibitors, meglitinides, and thiazolidinediones.
The primary kidney outcome was a composite of time to kidney failure, defined as chronic dialysis for >90 days, kidney transplantation, or a sustained eGFR of <15 mL/min/1.73 m2 confirmed after at least 4 weeks; a sustained ≥40% decrease in eGFR from baseline over at least 4 weeks; or renal death. The key secondary CV outcome was a composite of time to first onset of death from CV causes, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for heart failure. The secondary kidney outcome was a composite of kidney failure, a sustained ≥57% decrease in eGFR from baseline (for ≥4 weeks), or renal death. Other secondary outcomes, such as change in UACR from baseline to month 4, were explored. An independent clinical event committee blinded to treatment assignment adjudicated all reported outcome events, using definitions published previously (19). Safety outcomes included investigator-reported adverse events (AEs) and central laboratory assessment; events were considered as treatment emergent if they started or worsened during intake of study drug or up to 3 days after treatment interruption or discontinuation.
For this analysis, the impact of baseline HbA1c and insulin use (yes/no) on composite kidney and CV outcomes and safety in patients treated with finerenone or placebo was evaluated.
Statistical Analysis
Efficacy analyses were performed in the full analysis set (FAS), that is, all randomized patients without critical Good Clinical Practice violations. These prespecified subgroup analyses were exploratory and not designed to confirm or reject any predefined hypotheses. Analyses were performed according to each defined subgroup, that is, baseline HbA1c <7.5% (58 mmol/mol) versus baseline HbA1c ≥7.5% (58 mmol/mol), and baseline insulin use versus no baseline insulin use. The threshold value of 7.5% was used to define HbA1c subgroups at baseline, because the median HbA1c value in the study overall, as well as in each of the treatment arms, was 7.50%. All analyses were performed with SAS software, version 9.4 (SAS Institute).
Stratified log-rank testing was used to analyze the time-to-event superiority of finerenone versus placebo, and a stratified Cox proportional hazards regression model was used for hazard ratios (HRs). Stratification was according to geographic region and eGFR and UACR at screening (described previously) (19). A weighted Bonferroni–Holm procedure was used to test primary composite kidney and key secondary composite CV outcomes. Events were reported from randomization up to the end of study visit. Patients without an event were censored at the date of their last contact, with complete information on all components of their respective outcomes. The secondary efficacy outcome of change in UACR was analyzed with a linear mixed model, with all covariates entered as fixed effects and the subject effect entered as a random effect. Covariates in this analysis were treatment group (i.e., the treatment to which the patient was randomized to), visit, treatment-by-visit interaction, factors for the stratification levels, log-transformed baseline UACR value as a covariate nested within type of albuminuria, and log-transformed baseline value–by-visit interaction. To adjust the model for the within-subject variability of the repeated measures, we used an unstructured covariance pattern.
The relationship of the primary composite kidney and key secondary composite CV outcomes with baseline HbA1c as a continuous variable was investigated post hoc using a Cox proportional hazards model with cubic B-splines of HbA1c with three equally spaced knots, stratified by region, albuminuria at screening, and eGFR at screening, and with treatment interaction as covariates. To investigate further the relationship between HbA1c and outcomes, additional spline models with the same covariates were fitted separately in each treatment group (i.e., finerenone and placebo). Safety analyses were performed in the safety analysis set, which consisted of all eligible, randomized patients who took at least one dose of study drug.
Results
Patients
A total of 5,734 patients were randomly assigned to an arm in the FIDELIO-DKD trial. After the prospective exclusion of 60 patients from all analyses because of critical Good Clinical Practice violations, 5,674 patients were assessed in the FAS. As baseline HbA1c data were missing for 11 patients, 5,663 patients were included in the analysis for HbA1c. The trial concluded after a median follow-up of 2.6 (interquartile range, 2.0–3.4) years, with vital status available for 99.7% of patients (19). In the FAS (n = 5,674), the mean duration of T2D was 16.6 years. Mean HbA1c at baseline was 7.7% (61 mmol/mol) and remained stable in the finerenone and placebo treatment groups over the duration of the study (19). The distribution of HbA1c at baseline in both treatment groups is shown in Supplementary Fig. 1. At baseline, the median HbA1c was 7.5% (58 mmol/mol). In a mixed-model analysis, the least-squares (LS) mean change from baseline in HbA1c over the trial period among patients with HbA1c <7.5% (58 mmol/mol) was 0.03% (95% CI –0.04% to 0.09%), and 0.07% (95% CI –0.02% to 0.16%) in patients with baseline HbA1c value ≥7.5% (58 mmol/mol) (Supplementary Fig. 2).
Of the 5,663 patients who were included in the HbA1c analysis, 2,794 (49.3%) had an HbA1c <7.5% (58 mmol/mol) (Table 1) at baseline. Of 5,674 patients in the FAS, 3,637 (64.1%) were treated with insulin at baseline and 469 (8.3% patients: n = 209 [7.4%] receiving finerenone; n = 260 [9.2%] receiving placebo) started treatment with insulin after the start of the study (Supplementary Table 1). Patients who were started on insulin after baseline were included in the subgroup without insulin at baseline.
Table 1.
Patient baseline characteristics stratified according to median HbA1c and insulin use at baseline
| Baseline HbA1ca | Baseline insulin use | |||
|---|---|---|---|---|
| <7.5% (n = 2,794) | ≥7.5% (n = 2,869)b | No (n = 2,037) | Yes (n = 3,637) | |
| Age, years, mean ± SD | 66.2 ± 9.3 | 65.0 ± 8.8 | 66.4 ± 9.4 | 65.1 ± 8.9 |
| Sex, male, n (%) | 2,073 (74.2) | 1,904 (66.4) | 1,469 (72.1) | 2,514 (69.1) |
| Race, n (%) | ||||
| White | 1,732 (62.0) | 1,855 (64.7) | 1,244 (61.1) | 2,348 (64.6) |
| Black/African American | 110 (3.9) | 153 (5.3) | 79 (3.9) | 185 (5.1) |
| Asian | 801 (28.7) | 636 (22.2) | 613 (30.1) | 827 (22.7) |
| Otherc | 151 (5.4) | 225 (7.8) | 101 (5.0) | 277 (7.6) |
| Systolic blood pressure, mmHg, mean ± SD | 137.6 ± 14.5 | 138.5 ± 14.3 | 137.2 ± 14.4 | 138.5 ± 14.3d |
| Diastolic blood pressure, mmHg, mean ± SD | 75.5 ± 9.8 | 76.2 ± 9.5 | 76.4 ± 9.7 | 75.5 ± 9.6d |
| Duration of diabetes, years, mean ± SD | 15.0 ± 8.8 | 18.1 ± 8.4 | 13.0 ± 8.0 | 18.6 ± 8.6 |
| HbA1c, %, mean ± SD (mmol/mol) | 6.6 ± 0.6 (48.6) | 8.7 ± 1.0 (71.6) | 7.0 ± 1.1e (53.0) | 8.0 ± 1.3d (63.9) |
| eGFR, mL/min/1.73 m2, mean ± SD | 44.0 ± 12.5 | 44.7 ± 12.6 | 45.1 ± 12.5 | 43.9 ± 12.6 |
| eGFR, mL/min/1.73 m2, n (%) | ||||
| <25 | 66 (2.4) | 69 (2.4) | 41 (2.0) | 94 (2.6) |
| 25 to <45 | 1,506 (53.9) | 1,469 (51.2) | 1,035 (50.8) | 1,946 (53.5) |
| 45 to <60 | 923 (33.0) | 974 (33.9) | 716 (35.1) | 1,184 (32.6) |
| ≥60 | 299 (10.7) | 357 (12.4) | 245 (12.0) | 411 (11.3) |
| UACR, mg/g, median (IQR) | 835 (445–1,567) | 864 (447–1,693) | 784 (443–1,482)f | 884 (448–1,715) |
| UACR, mg/g, n (%) | ||||
| <30 | 7 (0.3) | 16 (0.6) | 4 (0.2) | 19 (0.5) |
| 30 to <300 | 342 (12.2) | 343 (12.0) | 233 (11.4) | 452 (12.4) |
| ≥300 | 2,445 (87.5) | 2,509 (87.5) | 1,799 (88.3) | 3,164 (87.0) |
| Missing data | 1 (<0.1) | 2 (<0.1) | ||
| Serum potassium, mmol/L, mean ± SD | 4.35 ± 0.46 | 4.39 ± 0.46 | 4.35 ± 0.45 | 4.38 ± 0.46 |
| BMI, kg/m2, mean ± SD | 30.4 ± 5.9 | 31.8 ± 6.0 | 30.1 ± 5.7e | 31.7 ± 6.1 |
| History of CVD, n (%) | 1,233 (44.1) | 1,368 (47.7) | 836 (41.0) | 1,769 (48.6) |
| History of diabetic retinopathy | 1,156 (41.4) | 1,501 (52.3) | 697 (34.2) | 1,966 (54.1) |
| History of diabetic neuropathy | 591 (21.2) | 861 (30.0) | 349 (17.1) | 1,105 (30.4) |
| Current smoker, n (%) | 436 (15.6) | 368 (12.8) | 324 (15.9) | 482 (13.3) |
| Baseline medications, n (%) | ||||
| ACE inhibitors | 914 (32.7) | 1,022 (35.6) | 664 (32.6) | 1,278 (35.1) |
| ARBs | 1,875 (67.1) | 1,845 (64.3) | 1,367 (67.1) | 2,358 (64.8) |
| β-Blockers | 1,428 (51.1) | 1,535 (53.5) | 989 (48.6) | 1,979 (54.4) |
| Diuretics | 1,529 (54.7) | 1,681 (58.6) | 1,055 (51.8) | 2,159 (59.4) |
| Statins | 2,023 (72.4) | 2,182 (76.1) | 1,458 (71.6) | 2,757 (75.8) |
| Glucose-lowering therapies | 2,672 (95.6) | 2,842 (99.1) | 1,887 (92.6) | 3,637 (100) |
| Insulin and analogs | 1,353 (48.4) | 2,279 (79.4) | 0 | 3,637 (100) |
| Metformin | 1,264 (45.2) | 1,219 (42.5) | 1,146 (56.3) | 1,344 (37.0) |
| Sulfonylureas | 687 (24.6) | 639 (22.3) | 909 (44.6) | 418 (11.5) |
| DPP-4 inhibitors | 833 (29.8) | 686 (23.9) | 782 (38.4) | 740 (20.3) |
| GLP-1RAs | 158 (5.7) | 235 (8.2) | 11 (5.4) | 283 (7.8) |
| SGLT-2is | 100 (3.6) | 159 (5.5) | 86 (4.2) | 173 (4.8) |
| α-Glucosidase inhibitors | 173 (6.2) | 151 (5.3) | 137 (6.7) | 187 (5.1) |
| Meglitinides | 189 (6.8) | 133 (4.6) | 167 (8.2) | 156 (4.3) |
| TZDs | 124 (4.4) | 105 (3.7) | 135 (6.6) | 94 (2.6) |
CVD, cardiovascular disease; DPP-4, dipeptidyl peptidase 4; GLP-1RA, glucagon-like peptide 1 receptor agonist; IQR, interquartile range; TZD, thiazolidinedione.
Missing data for 11 patients (finerenone, n = 7; placebo, n = 4).
Missing data for 1 patient with HbA1c ≥7.5% at baseline.
Includes patients reporting multiple races.
Missing data for 5 patients.
Missing data for 6 patients.
Missing data for 1 patient.
Baseline Characteristics
By HbA1c Level
Patients with HbA1c ≥7.5% at baseline had a longer duration of T2D and a higher proportion had a history of CV disease compared with patients whose HbA1c was <7.5%. However, median UACR, mean eGFR, and mean serum potassium levels were similar in patients regardless of HbA1c (i.e., ≥7.5% or <7.5%) (Table 1). Overall, 48.4% and 79.4% of patients with HbA1c <7.5% and ≥7.5%, respectively, were being treated with insulin at baseline. Greater use of glucagon-like peptide 1 receptor agonists and SGLT-2is was observed in patients with baseline HbA1c ≥7.5% vs. <7.5% (Table 1).
By Insulin Use
Patients treated with insulin had a higher BMI, a longer duration of diabetes, and a higher UACR than did patients who did not receive insulin at baseline. Serum potassium and baseline eGFR values were similar between groups (Table 1).
Kidney Outcomes According to HbA1c Level and Insulin Use at Baseline
By HbA1c Level
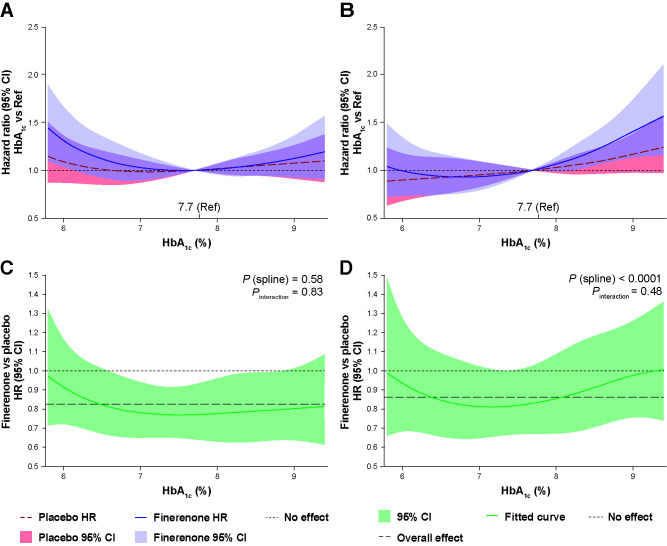
No clear relationship was observed between baseline HbA1c level and the risk of experiencing a primary kidney outcome event, after adjusting for confounding baseline variables, irrespective of treatment assignment. Thus, as an example, patients with a baseline HbA1c of 6.5% (48 mmol/mol) or 9.0% (75 mmol/mol) had a similar risk of experiencing an event as those with a baseline HbA1c of 7.7% (61 mmol/mol) (Fig. 1A).
Figure 1.
Cox proportional hazards model for the primary kidney outcomes and key secondary CV outcome in the FAS, with cubic B-splines of HbA1c with three equally spaced knots stratified by region, and albuminuria and eGFR at screening. The model was fitted separately by treatment group for the primary kidney composite outcome (A) and the key secondary CV outcome (B), and with treatment interaction as a covariate for the primary kidney composite outcome (C) and the key secondary CV composite outcome (D). The reference (Ref) is mean HbA1c (%) at baseline.
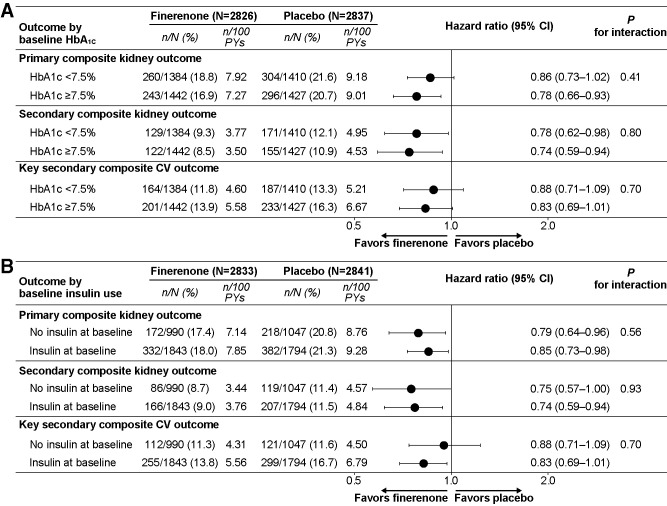
As previously reported, the incidence of the primary composite kidney outcome was significantly lower with finerenone versus placebo in the overall population of FIDELIO-DKD (HR 0.82; 95% CI 0.73–0.93; P = 0.001) (19). In this analysis, the primary kidney outcome occurred in fewer patients treated with finerenone compared with those who received placebo in both the HbA1c <7.5% and ≥7.5% groups (18.8% vs. 21.6% of patients with HbA1c <7.5% [HR 0.86; 95% CI 0.73–1.02]; 16.9% vs. 20.7% of patients with HbA1c ≥7.5% [HR 0.78; 95% CI 0.66–0.93]; Pinteraction = 0.41) (Fig. 2 and Supplementary Fig. 3). The treatment effect of finerenone was consistent when HbA1c was modeled as a continuous variable (Pinteraction for finerenone vs. placebo = 0.8334) (Fig. 1B). Incidence of the secondary composite kidney outcome followed a similar pattern, with fewer events in patients treated with finerenone compared with those who received placebo in both groups (9.3% vs. 12.1% of patients with HbA1c <7.5% [HR 0.78; 95% CI 0.62–0.98]; 8.5% vs. 10.9% of patients with baseline HbA1c ≥7.5% [HR 0.74; 95% CI 0.59–0.94]; Pinteraction = 0.80) (Fig. 2).
Figure 2.
Composite kidney outcome (time to kidney failure, a sustained ≥40% decrease in eGFR from baseline over at least 4 weeks; or death from renal causes), secondary composite kidney outcome (time to kidney failure, a sustained ≥57% decrease in eGFR from baseline over at least 4 weeks; or death from renal causes), and CV outcomes (time to first onset of death from CV causes, nonfatal myocardial infarction, nonfatal stroke, or hospitalization for heart failure) according to HbA1c level at baseline (A) and insulin use at baseline (B). PY, patient-year.
In the overall population, finerenone was associated with a 31% greater reduction in UACR from baseline to month 4 versus placebo (HR 0.69; 95% CI 0.66–0.71) (19). A mixed-model analysis (accounting for differences in baseline characteristics) indicated a similar reduction in UACR at month 4 with finerenone versus placebo regardless of baseline HbA1c value (ratio of LS means 0.67 [95% CI 0.64–0.71; P < 0.0001] with HbA1c <7.5%; and 0.70 [95% CI 0.66–0.74; P < 0.0001] with HbA1c ≥7.5% (Supplementary Fig. 4).
By Insulin Use
The primary composite kidney outcome occurred in fewer patients treated with finerenone than in those who received placebo in patients with or without insulin use at baseline (18.0% vs. 21.3% of patients with insulin at baseline [HR 0.85; 95% CI 0.73–0.98]; 17.4% vs. 20.8% of patients without insulin at baseline [HR 0.79; 95% CI 0.64–0.96]; Pinteraction = 0.56) (Fig. 2 and Supplementary Fig. 5). Incidence of the secondary composite kidney outcome followed a similar pattern (Fig. 2).
The mixed-model analysis showed a similar reduction in UACR at month 4 with finerenone versus placebo regardless of baseline insulin use (ratio of LS means 0.68 [95% CI 0.64–0.73], P < 0.0001 without insulin use at baseline; 0.68 [95% CI 0.65–0.72], P < 0.0001 with baseline insulin use) (Supplementary Fig. 6).
CV Outcomes According to HbA1c Level and Insulin Use at Baseline
By HbA1c Level
After adjusting for confounding baseline variables, a relationship was observed between baseline HbA1c level and the risk of experiencing a CV event. Patients with a baseline HbA1c of 6.5% had a similar risk of experiencing an event as those with a baseline HbA1c of 7.7%, whereas those with a baseline HbA1c of 9.0% had an ∼30% higher risk of experiencing an event than did the reference population (Fig. 1C).
In the overall population, the key secondary composite CV outcome was lower with finerenone compared with placebo in the overall population (HR 0.86; 95% CI 0.75–0.99; P = 0.03) (19,20). In this analysis, the incidence of the key secondary CV outcome followed a similar pattern, with finerenone treatment resulting in a lower incidence of the secondary CV outcome compared with placebo (HR 0.88 [95% CI 0.71–1.09] for HbA1c <7.5%; HR 0.83 [95% CI 0.69–1.01] for HbA1c ≥7.5%; Pinteraction = 0.70) (Fig. 2 and Supplementary Fig. 3). Results were consistent when HbA1c was modeled as a continuous variable (Pinteraction for finerenone vs. placebo = 0.4802) (Fig. 1D).
By Insulin Use
The incidence of the key secondary CV outcome also was lower in patients treated with finerenone compared with those who received placebo, with a nonsignificant trend showing greater risk reduction with baseline insulin use (HR 0.82 [95% CI 0.69–0.97] with insulin use at baseline vs. HR 0.95 [95% CI 0.74–1.23] without insulin at baseline; Pinteraction = 0.33) (Fig. 2 and Supplementary Fig. 5).
The rates of events for the primary composite kidney outcome and the key secondary CV outcome were lower with finerenone versus placebo irrespective of baseline treatment with any oral antidiabetic, any oral antidiabetic but not insulin, or insulin only (P values for the interaction were not significant for any groups) (Supplementary Fig. 7A and B).
Safety
In the overall population, 151 finerenone-treated patients (5.3%) versus 194 placebo-treated patients (6.9%) experienced hypoglycemia, and hyperglycemia occurred in 75 (2.7%) versus 78 (2.8%) patients, respectively. Diabetes-related AEs occurred in 52 finerenone-treated (1.8%) patients versus 77 placebo-treated patients (2.7%); and diabetes control was inadequate in 57 finerenone-treated patients (2.0%) versus 77 placebo-treated patients (2.7%). No difference in diabetic ketoacidosis was observed between treatment groups (n = 7 [0.2%] patients in both arms).
The incidence of any treatment-emergent AE was similar with finerenone and placebo, irrespective of baseline HbA1c level or insulin use (Table 2 and Supplementary Table 2). The incidence of hypoglycemia tended to be lower with finerenone than with placebo, particularly in patients with higher HbA1c levels and in those receiving insulin at baseline (Supplementary Tables 3 and 4). A similar trend was observed for hypoglycemia and hyperglycemia as serious AEs, with lower incidence reported for finerenone versus placebo with higher HbA1c levels and baseline insulin use (Supplementary Tables 5 and 6). There was also no increase in the incidence of urinary tract infections with finerenone versus placebo in either HbA1c subgroup, irrespective of baseline HbA1c level and insulin use. The incidence of any treatment-emergent, hyperkalemia-related AE was greater in patients treated with finerenone than in those who received placebo, with an approximately twofold increase with finerenone in both subgroups; however, no patients died and few patients discontinued the study drug due to hyperkalemia in either treatment arm in both subgroups (Table 2 and Supplementary Table 2).
Table 2.
Overall safety and treatment-emergent, hyperkalemia-related events in patients according to median HbA1c level at baseline
| Baseline HbA1c | ||||
|---|---|---|---|---|
| <7.5% | ≥7.5% | |||
| Finerenone (n = 1,382) | Placebo (n = 1,407) | Finerenone (n = 1,439) | Placebo (n = 1,421) | |
| Any investigator-reported AE | 1,206 (87.3) | 1,229 (87.3) | 1,258 (87.4) | 1,246 (87.7) |
| Related to study drug | 312 (22.6) | 221 (15.7) | 333 (23.1) | 228 (16.0) |
| Leading to discontinuation | 98 (7.1) | 92 (6.5) | 108 (7.5) | 75 (5.3) |
| Any SAE | 415 (30.0) | 448 (31.8) | 485 (33.7) | 523 (36.8) |
| Related to study drug | 23 (1.7) | 16 (1.1) | 24 (1.7) | 18 (1.3) |
| Leading to discontinuation | 36 (2.6) | 39 (2.8) | 38 (2.6) | 39 (2.7) |
| AE with outcome death | 15 (1.1) | 23 (1.6) | 16 (1.1) | 28 (2.0) |
| Investigator-reported hyperkalemia-related AEsa | ||||
| Any AE | 253 (18.3) | 124 (8.8) | 262 (18.2) | 131 (9.2) |
| Related to study drug | 157 (11.4) | 60 (4.3) | 175 (12.2) | 75 (5.3) |
| Leading to discontinuation | 28 (2.0) | 13 (0.9) | 36 (2.5) | 12 (0.8) |
| Any SAE | 22 (1.6) | 2 (0.1) | 21 (1.5) | 10 (0.7) |
| Related to study drug | 12 (0.9) | 1 (<0.1) | 13 (0.9) | 4 (0.3) |
| Leading to hospitalization | 19 (1.4) | 2 (0.1) | 20 (1.4) | 6 (0.4) |
| Central laboratory assessment of serum potassium levels, mmol/L, n/N (%) | ||||
| >5.5 | 292/1,369 (21.3) | 119/1,383 (8.6) | 302/1,410 (21.4) | 137/1,389 (9.9) |
| >6.0 | 61/1,374 (4.4) | 18/1,389 (1.3) | 65/1,422 (4.6) | 20/1,404 (1.4) |
Data reported as n (%) unless otherwise indicated.
MedDRA, Medical Dictionary for Regulatory Activities; SAE, serious adverse event.
Reported using the MedDRA-preferred terms “hyperkalemia” and “blood potassium increased.”
Baseline systolic blood pressure was marginally higher in the group receiving insulin at baseline group than in those who were not receiving insulin at baseline (138.5 vs. 137.2 mmHg, respectively) (Table 1). There was an ∼3 mmHg decrease in systolic blood pressure with finerenone compared with placebo at month 1 relative to baseline, and this was observed in patients with or without insulin use at baseline (Supplementary Fig. 8). No change in body weight was observed with finerenone compared with placebo in patients with or without insulin use at baseline (Supplementary Fig. 9).
CONCLUSIONS
In the FIDELIO-DKD study, finerenone significantly reduced the primary composite kidney outcome and the key secondary CV composite outcome compared with placebo in patients with CKD and T2D, without affecting HbA1c levels. These subgroup analyses demonstrated that the benefits of finerenone in patients with CKD and T2D were consistent irrespective of HbA1c level or insulin use at baseline. These results expand on previous analyses from FIDELIO-DKD that demonstrated benefits of finerenone on kidney and CV outcomes are also independent of SGLT-2i or glucagon-like peptide 1 receptor agonist use at baseline (22,23).
Results of the Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes Mellitus Patients–Removing Excess Glucose (EMPA-REG OUTCOME) trial indicated significant heterogeneity in the primary composite CV outcome between patients with T2D at high risk of CV events with HbA1c <8.5% (69.4 mmol/mol) compared with HbA1c ≥8.5%, suggesting empagliflozin has no CV benefits in patients with HbA1c ≥8.5%, although the effects of empagliflozin to limit incident or worsening nephropathy were consistent irrespective of HbA1c level (24,25). These data suggest that HbA1c levels may contribute to differences in CV efficacy results. Therefore, it was of interest to evaluate whether poor glycemic control or increased HbA1c levels in patients with CKD and T2D would alter the beneficial kidney and CV outcomes observed with finerenone treatment. Reassuringly, the results of the present analysis suggest that, unlike other approved therapies aiming to reduce kidney and CV risk, finerenone delays CKD progression and reduces CV events in patients with CKD and T2D regardless of baseline HbA1c levels. Similar findings were observed in patients receiving or not receiving insulin at baseline. This strengthens our results because of the considerable overlap between both patient subgroups, with almost 80% of patients with HbA1c ≥7.5% receiving insulin at baseline. For all outcomes, fewer events occurred with finerenone than with placebo, with no significant interactions according to HbA1c level or insulin use at baseline. Although the P value for interaction for the secondary CV outcomes was not significant, there was a trend toward a larger risk reduction with baseline insulin use. A similar finding was noted in the Comparison of Outcomes in Patients in New York Heart Association Class II Heart Failure When Treated With Eplerenone or Placebo in Addition to Standard Heart Failure Medicines trial, in which greater CV benefits of the steroidal MRA eplerenone were observed in patients with insulin-treated diabetes than in patients with diabetes not treated with insulin (26). Because finerenone has a modest effect of lowering blood pressure, promoting natriuresis, and, perhaps, inhibiting inflammation, it may counteract the sodium retention, hypertension, and inflammation associated with insulin use or hyperinsulinemia (9,10). However, more analyses are required to determine whether the benefits of finerenone are greater when a patient is receiving insulin.
Modeling of serum HbA1c levels as a continuous variable suggests that a higher baseline HbA1c level is associated with an increased risk of experiencing CV events, a finding that was observed in both the finerenone and placebo treatment groups in the present study; in contrast, HbA1c levels did not influence the risk of CKD progression in either group, which is an interesting dichotomous observation. These results contrast with what is known about intensive glycemic control and kidney and CV events in patients with T2D without CKD or with mild CKD. The UK Prospective Diabetes Study (UKPDS) demonstrated that intensive glucose-lowering therapy in patients with newly diagnosed T2D significantly reduced microvascular complications, including a decrease in the progression of albuminuria, when compared with standard therapy, whereas no beneficial effect on CV events was observed (13). In the Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) trial, intensive glucose control significantly reduced the risk of end-stage kidney disease, microalbuminuria, and macroalbuminuria in patients with T2D without CKD or with mild CKD, with greater long-term benefits in patients with more preserved kidney function (14,15). And last, in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, researchers showed that the use of intensive therapy to target normal HbA1c levels did not significantly reduce CV events when compared with standard therapy and had limited benefits on kidney-specific outcomes in patients with T2D and high CV risk (27,28). The main reason for the disparities between our results and these studies could be because the data analyses carried out in the present study used a single point-in-time assessment of HbA1c levels at baseline and HbA1c was well controlled, whereas in UKPDS, ADVANCE, and ACCORD, researchers evaluated intensive HbA1c lowering over time. Another reason could be the different medication used (e.g., previous studies did not include patients receiving SGLT-2is or glucagon-like peptide 1 receptor agonists). Patients with a later stage of CKD were observed in this study, compared with patients in the UKPDS, ADVANCE, and ACCORD trials (13–15,27,28).
In the FIDELIO-DKD trial, finerenone was associated with a higher overall risk of hyperkalemia than was placebo, but discontinuation due to hyperkalemia was infrequent in patients receiving finerenone (19). These findings were reflected in this analysis, with no notable differences observed on the basis of baseline HbA1c level or baseline insulin use. An interesting observation was that fewer hypoglycemia AEs and serious AEs tended to be observed with finerenone than with placebo, particularly in the patient subgroups with HbA1c ≥7.5% (58 mmol/mol) and those treated with insulin at baseline. The reason for this is unclear because finerenone has no effect on HbA1c levels. One hypothesis is that higher incidence of insulin use in the placebo arm may increase risk of hypoglycemic events, but the possibility that this may be a chance finding cannot be ruled out and more data are needed. Additionally, there was no imbalance in hyperglycemia events between treatment arms and no increase in the incidence of diabetic ketoacidosis or urinary tract infections with finerenone across subgroups. These findings distinguish finerenone from the SGLT-2is, which have been associated with an increased risk of diabetic ketoacidosis and serious urinary tract infections (29,30). Further insight may be provided by the results of the recently completed Finerenone in Reducing Cardiovascular Mortality and Morbidity in Diabetic Kidney Disease (FIGARO-DKD) study. FIGARO-DKD will offer the opportunity for the relationship between baseline HbA1c levels and baseline insulin use to be further investigated in a larger population, including patients with mild CKD and with lower insulin use at baseline (31).
As a secondary analysis of a phase 3 trial, this analysis has some limitations. Namely, patients were not stratified according to baseline insulin use or HbA1c level. Moreover, changes in treatment for diabetes were permitted during the study; although approximately two-thirds of the population was receiving insulin at baseline, insulin was also initiated as a new medication during the study, but this occurred in less than 10% of all patients in the FAS.
Conclusion
The results of this secondary analysis of the FIDELIO-DKD study suggest that finerenone protects the kidneys and CV system of patients with advanced CKD and T2D independent of HbA1c level or insulin use and without reducing HbA1c, and thus offers an important advance in treatment for patients with CKD and T2D.
Article Information
Acknowledgments. The authors are indebted to the patients who have participated in this trial, the FIDELIO-DKD study investigators, the study centers that supported the trial, and the study teams. Medical writing assistance was provided by Dr. Oyinkan Adesakin of Chameleon Communications International, and was funded by Bayer AG.
Funding. The FIDELIO-DKD trial was conducted and funded by Bayer AG.
Duality of Interest. P.R. reports receiving personal fees from Bayer during the conduct of the study, research support and personal fees from AstraZeneca and Novo Nordisk, and personal fees from Astellas, Boehringer Ingelheim, Eli Lilly and Company, Gilead, Merck, Merck Sharp & Dohme, Mundipharma, Sanofi, and Vifor Pharma. All fees are given to Steno Diabetes Center Copenhagen. E.B. is a member of the FIDELIO-DKD steering committee. R.A. has received personal fees and nonfinancial support from Bayer Healthcare Pharmaceuticals during the conduct of the study; personal fees and nonfinancial support from Akebia Therapeutics, AstraZeneca, Boehringer Ingelheim, Eli Lilly and Company, Fresenius Medical Care AG and Company, Janssen Pharmaceuticals, Relypsa, Sanofi, and Vifor Pharma; personal fees from Ironwood Pharmaceuticals, Lexicon Pharmaceuticals, Merck & Company, and Reata Pharmaceuticals; and nonfinancial support from E.R. Squibb & Sons, Opko Pharmaceuticals, and Otsuka America Pharmaceutical. R.A. is a member of data safety monitoring committees for AstraZeneca and Ironwood Pharmaceuticals, a member of steering committees of randomized trials for Akebia Therapeutics, Bayer, Janssen Pharmaceuticals, and Relypsa; a member of adjudication committees for AbbVie, Bayer, Boehringer Ingelheim, and Janssen Pharmaceuticals; has served as associate editor of the American Journal of Nephrology and Nephrology Dialysis and Transplantation and has been an author for UpToDate; and has received research grants from the National Institutes of Health and the U.S. Veterans Administration. S.D.A. has received research support from Abbott Vascular and Vifor International, and personal fees from Abbott Vascular, Bayer, Boehringer Ingelheim, B.R.A.H.M.S., Cardiac Dimensions, Impulse Dynamics, Novartis, Servier Pharmaceuticals, and Vifor International. G.F. reports receiving lecture fees and/or that he is a committee member of trials and registries sponsored by Amgen, Bayer, Boehringer Ingelheim, Medtronic, Novartis, Servier Pharmaceuticals, and Vifor Pharma; has received research support from the European Union; and is a senior consulting editor for JACC Heart Failure. B.P. has received consultant fees from Ardelyx, AstraZeneca, Bayer, Boehringer Ingelheim, Brainstorm Medical, Cereno Scientific, G3 Pharmaceuticals, KBP Biosciences, Phasebio Pharmaceuticals, Sanofi/Lexicon, Sarfez Pharmaceuticals, scPharmaceuticals, SQ Innovation, Tricida, and Vifor/Relypsa; has stock options for Ardelyx, Brainstorm Medical, Cereno Scientific, G3 Pharmaceuticals, KBP Biosciences, Sarfez, scPharmaceuticals, SQ Innovation, Tricida, and Vifor/Relypsa (Galencia Group); and holds a patent for site-specific delivery of eplerenone to the myocardium (U.S. patent 9931412) and a provisional patent for histone-acetylation-modulating agents for the treatment and prevention of organ injury (U.S. provisional patent 63/045,784). L.M.R. reports receipt of consultancy fees from Bayer. P.G. serves or has served on the speakers’ bureau for Abbott, Bayer, Boehringer Ingelheim, Insulet Corporation, Medtronic, Merck Sharp & Dohme, Novo Nordisk, and F. Hoffmann-La Roche AG. Financial compensation for these activities has been received by Katholieke Universiteit Leuven. Katholieke Universiteit Leuven received, for P.G., nonfinancial support for travel from A. Menarini Diagnostics, Medtronic, Roche, and Sanofi. All disclosures were unrelated to the present work. R.J.M. has received research grants from Grey Innovations, Medtronic, Novo Nordisk, Servier Pharmaceuticals, St. Vincent’s Research Foundation, The Diabetes Australia Research Program, The Juvenile Diabetes Research Foundation, The National Health and Medical Research Council of Australia, and The Rebecca L. Cooper Medical Research Foundation; honoraria for lectures from AstraZeneca, Boehringer Ingelheim, Eli Lilly and Company, Merck Sharp & Dohme, Novartis, Novo Nordisk, and Sanofi Aventis; is on advisory boards for AstraZeneca, the Boehringer Ingelheim–Eli Lilly Diabetes Alliance, Merck Sharp & Dohme, and Novo Nordisk; has received travel support from AstraZeneca, Boehringer Ingelheim, Novo Nordisk, and Sanofi; and has been a principal investigator for industry-sponsored clinical trials run by AbbVie, Bayer, Janssen-Cilag, Novo Nordisk, and Sanofi. J.W. has received research support from AstraZeneca, Boehringer Ingelheim, Eli Lilly and Company, Merck Sharp & Dohme, Novo Nordisk, and Sanofi; honoraria for lectures from AstraZeneca, Eli Lilly and Company, Merck Sharp & Dohme, and Novo Nordisk. A.J., M.B., and L.R. are full-time employees of Bayer AG, Division Pharmaceuticals, Germany. C.S. is a full-time employee of Bayer PLC, United Kingdom. G.L.B. has received research funding, paid to the University of Chicago Medicine, from Bayer during the conduct of the study. He also reports research funding, paid to the University of Chicago Medicine, from Novo Nordisk and Vascular Dynamics; he consulted for and received personal fees from Alnylam Pharmaceuticals, Merck and Company, and Relypsa; is an editor of the American Journal of Nephrology, Nephrology, and Hypertension, a section editor of UpToDate, and an associate editor of Diabetes Care and Hypertension Research. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. The Executive Committee designed the study in conjunction with the sponsor, Bayer AG. PR researched the data and wrote manuscript. E.B., R.A., S.D.A., G.F., B.P., L.M.R., P.G., R.J.M., J.W., A.J., and G.L.B. researched the data, reviewed and edited the manuscript and contributed to the discussion. M.B. and L.R. reviewed and edited the manuscript and contributed to the discussion. C.S. analyzed the data, reviewed and edited the manuscript, and contributed to the discussion. P.R. and A.J. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. The data included in this manuscript were presented in part at the American Diabetes Association 81st Scientific Sessions (virtual), 25–29 June 2021.
Footnotes
ClinicalTrials.gov reg. no. NCT02540993, clinicaltrials.gov, and EU Clinical Trials Register no. 2015-000990-11, https://www.clinicaltrialsregister.eu/
This article contains supplementary material online at https://doi.org/10.2337/figshare.17701001.
A complete list of the FIDELIO-DKD Investigators can be found in the supplementary material online.
This article is featured in a podcast available at diabetesjournals.org/journals/pages/diabetes-core-update-podcasts.
Contributor Information
on behalf of the FIDELIO-DKD Investigators:
Augusto Vallejos, Richard MacIsaac, Guntram Schernthaner, Pieter Gillard, Maria Eugenia F. Canziani, Theodora Temelkova-Kurktschiev, Ellen Burgess, Sheldon Tobe, Fernando González, Zhi-Hong Liu, Andrés Ángelo, Cadena Bonfanti, Carlos Francisco Jaramillo, Martin Prazny, Peter Rossing, Jorma Strand, Michel Marre, Roland Schmieder, Christoph Wanner, Pantelis A. Sarafidis, Juliana Chan, László Rosivall, Joseph Eustace, Ehud Grossman, Yoram Yagil, Giuseppe Remuzzi, Daisuke Koya, Takashi Wada, Magdalena Madero Rovalo, Ron Gansevoort, Adriaan Kooy, Trine Finnes, Froilan De Leon, Janusz Gumprecht, Fernando Teixeira e Costa, Alexander Dreval, Anantharaman Vathsala, Aslam Amod, Sin Gon Kim, Byung Wan Lee, Julio Pascual Santos, Bengt-Olov Tengmark, Michel Burnier, Chien-Te Lee, Sukit Yamwong, Ramazan Sari, Kieran McCafferty, Borys Mankovsky, Sharon Adler, Linda Fried, Robert Toto, Mark Williams, Tran Quang Khanh, Diego Aizenberg, Inés Bartolacci, Diego Besada, Julio Bittar, Mariano Chahin, Alicia Elbert, Elizabeth Gelersztein, Alberto Liberman, Laura Maffei, Federico Pérez Manghi, Hugo Sanabria, Gloria Viñes, Alfredo Wassermann, Walter Abhayaratna, Shamasunder Acharya, Elif Ekinci, Darren Lee, Peak Mann Mah, Craig Nelson, David Packham, Alexia Pape, Simon Roger, Hugo Stephenson, Michael Suranyi, Gary Wittert, Elizabeth Vale, Martin Clodi, Christoph Ebenbichler, Evelyn Fliesser-Görzer, Ursula Hanusch, Michael Krebs, Karl Lhotta, Bernhard Ludvik, Gert Mayer, Peter Neudorfer, Bernhard Paulweber, Rudolf Prager, Wolfgang Preiß, Friedrich Prischl, Gerit-Holger Schernthaner, Harald Sourij, Martin Wiesholzer, Peter Doubel, Wendy Engelen, Jean-Michel Hougardy, Jean-Marie Krzesinski, Bart Maes, Marijn Speeckaert, Koen Stas, Luc van Gaal, Hilde Vanbelleghem, Daniela Antunes, Roberto Botelho, Claudia Brito, Luis Canani, Maria Eugenia Canziani, Maria Cerqueira, Rogerio de Paula, Freddy Eliaschewitz, Carlos Eduardo Figueiredo, Adriana Forti, Miguel Hissa, Maurilo Leite, Jr, Emerson Lima, Irene Noronha, Bruno Paolino, Nathalia Paschoalin, Raphael Paschoalin, Roberto Pecoits Filho, Marcio Pereira, Evandro Portes, Dalton Precoma, Rosangela Rea, Miguel Riella, Joao Eduardo Salles, Eduardo Vasconcellos, Sergio Vencio, Emiliya Apostolova, Radostina Boshnyashka, Ghassan Farah, Dimitar Georgiev, Valentina Gushterova, Neli Klyuchkova, Mariya Lucheva, Petya Manova, Dotska Minkova, Boyan Nonchev, Mariyana Pichmanova, Zhulieta Prakova, Rangel Rangelov, Rosen Rashkov, Pavel Stanchev, Bilyana Stoyanovska-Elencheva, Zhivko Tagarev, Theodora Temelkova-Kurktschieva, Svetla Vasileva, Mariana Yoncheva-Mihaylova, Paul Barre, Brian Carlson, James Conway, Serge Cournoyer, Richard Dumas, Sameh Fikry, Richard Goluch, Pavel Hamet, Randolph Hart, Sam Henein, Joanne Liutkus, Francois Madore, Valdemar Martinho, Giuseppe Mazza, Philip McFarlane, Dennis O'Keefe, Sean Peterson, Daniel Schwartz, Daniel Shu, Andrew Steele, Guy Tellier, Karthik Tennankore, George Tsoukas, Richard Tytus, Louise Vitou, Michael Walsh, Stanley Weisnagel, Igor Wilderman, Jean-Francois Yale, Jorge Cobos, Juan Godoy, Sergio Lobos, Juan Carlos Palma, Juan Carlos Prieto, Eliana Reyes, Carmen Romero, Victor Saavedra, Mario Vega, Ruifang Bu, Hanqing Cai, Nan Chen, Qinkai Chen, Dejun Chen, Jinluo Cheng, Youping Dong, Junwu Dong, Tianjun Guan, Chuanming Hao, Wen Huang, Fangfang Jiang, Minxiang Lei, Ling Li, Zhonghe Li, Xuemei Li, Jingmei Li, Yan Li, Xinling Liang, Bo Liang, Fang Liu, Yinghong Liu, Yuantao Liu, Zhihong Liu, Gang Long, Guoyuan Lu, Weiping Lu, Yibing Lu, Ping Luo, Jianhua Ma, Zhaohui Mo, Jianying Niu, Ai Peng, Jiansong Shen, Feixia Shen, Bingyin Shi, Qing Su, Zhuxing Sun, Shuifu Tang, Nanwei Tong, Hao Wang, Xinjun Wang, Lihua Wang, Guixia Wang, Jianqin Wang, Yangang Wang, Li Wang, Jiali Wei, Tianfeng Wu, Chaoqing Wu, Changying Xing, Fei Xiong, Xudong Xu, Ning Xu, Tiekun Yan, Jinkui Yang, Aiping Yin, Longyi Zeng, Hao Zhang, Yanlin Zhang, Ying Zhang, Wenjing Zhao, Zhiquan Zhao, Hongguang Zheng, Ling Zhong, Dalong Zhu, Yongze Zhuang, Clara Arango, Sandra Barrera, Nelly Beltrán López, Diego Benitez, Guillermo Blanco, Andrés Cadena, Julian Coronel, Carlos Cure, Carlos Durán, Alexander González, Gustavo Guzmán, Eric Hernández, Jaime Ibarra, Carlos Jaramillo, Nicolás Jaramillo, William Kattah, Dora Molina, Gregorio Sánchez, Mónica Terront, Freddy Trujillo, Miguel Urina, Ruben Vargas, Iván Villegas, Hernán Yupanqui, Dino Alferi, Michal Brada, Jiri Brezina, Petr Bucek, Tomas Edelsberger, Drahomira Gulakova, Jitka Hasalova Zapletalova, Olga Hola, Lucie Hornova, Jana Houdova, Helena Hrmova, David Karasek, Sarka Kopecka, Richard Kovar, Eva Krcova, Jiri Kuchar, Vlasta Kutejova, Hana Lubanda, Ivo Matyasek, Magdalena Mokrejsova, Libor Okenka, Jiri Pumprla, Pavel Tomanek, Jesper Bech, Jens Faber, Gunnar Gislason, Jørgen Hangaard, Grzegorz Jaroslaw Pacyk, Claus Juhl, Thure Krarup, Morten Lindhardt, Sten Madsbad, Joan Nielsen, Ulrik Pedersen-Bjergaard, Per Poulsen, Ole Rasmussen, Karoline Schousboe, Mikko Honkasalo, Kari Humaloja, Kristiina Kananen, Ilkka Kantola, Arvo Koistinen, Pirkko Korsoff, Jorma Lahtela, Sakari Nieminen, Tuomo Nieminen, Karita Sadeharju, Sakari Sulosaari, Bertrand Cariou, François Chantrel, Sylvaine Clavel, Christian Combe, Jean-Pierre Fauvel, Karim Gallouj, Didier Gouet, Bruno Guerci, Dominique Guerrot, Maryvonne Hourmant, Alexandre Klein, Christophe Mariat, Rafik Mesbah, Yannick Le Meur, Arnaud Monier, Olivier Moranne, Pierre Serusclat, Benoit Vendrely, Bruno Verges, Philippe Zaoui, Christoph Axthelm, Andreas Bergmann, Andreas L. Birkenfeld, Hermann Braun, Klaus Busch, Christel Contzen, Stefan Degenhardt, Karl Derwahl, Thomas Giebel, Andreas Hagenow, Hermann Haller, Christoph Hasslacher, Thomas Horacek, Wolfgang Jungmair, Christof Kloos, Thorsten Koch, Thilo Krüger, Anja Mühlfeld, Joachim Müller, Andreas Pfützner, Frank Pistrosch, Ludger Rose, Lars Rump, Volker Schettler, Ingolf Schiefke, Heike Schlichthaar, Bernd Schröppel, Thomas Schürholz, Helena Sigal, Lutz Stemler, Georg Strack, Heidrun Täschner, Nicole Toursarkissian, Diethelm Tschöpe, Achim Ulmer, Markus van der Giet, Bernhard R. Winkelmann, Ioannis Boletis, Erifili Hatziagelaki, Ioannis Ioannidis, Theodora Kounadi, Ioanna Makriniotou, Dorothea Papadopoulou, Aikaterini Papagianni, Ploumis Passadakis, Ioannis Stefanidis, Tai Pang Ip, Paul Lee, On Yan Andrea Luk, Angela Wang, Vincent Yeung, Dora Bajcsi, Peter Danos, Eleonora Harcsa, Szilvia Kazup, Katalin Keltai, Robert Kirschner, Julianna Kiss, Laszlo Kovacs, Beata Lamboy, Botond Literati-Nagy, Margit Mileder, Laszlo Nagy, Ebrahim Noori, Gabor Nyirati, Gizella Petro, Karoly Schneider, Albert Szocs, Szilard Vasas, Krisztina Wudi, Zsolt Zilahi, Marianna Zsom, Joe Eustace, John Holian, Donal Reddan, Yvonne O'Meara, Rosane Abramof Ness, Faiad Adawi, Zaher Armaly, Shaul Atar, Sydney Ben Chetrit, Noa Berar Yanay, Gil Chernin, Mahmud Darawsha, Shai Efrati, Mazen Elias, Evgeny Farber, Mariela Glandt, Majdi Halabi, Khaled Khazim, Idit Liberty, Ofri Mosenzon, Assy Nimer, Doron Schwartz, Julio Wainstein, Robert Zukermann, Aneliya Ilieva Parvanova, Angelo Avogaro, Giovanni Giorgio Battaglia, Maurizio Tiziano Bevilacqua, Enzo Bonora, Carlo Antonio Bossi, Paolo Calabrò, Franco Luigi Cavalot, Roberto Cimino, Mario Gennaro Cozzolino, Salvatore David, Michele Emdin, Enrico Fiaccadori, Paolo Fiorina, Carlo Bruno Giorda, Maria Cristina Gregorini, Gaetano La Manna, Davide Carlo Maggi, Roberta Manti, Giancarla Meregalli, Antonello Pani, Norberto Perico, PierMarco Piatti, Antonio Pisani, Antonio Ettore Pontiroli, Paola Ponzani, Gennaro Santorelli, Domenico Santoro, Renzo Scanziani, Ugo Teatini, Giancarlo Tonolo, Roberto Trevisan, Anna Maria Veronelli, Giorgio Luciano Viviani, Hideo Araki, Osamu Ebisui, Naruhiro Fujita, Ryuichi Furuya, Yoshiyuki Hamamoto, Masahiro Hatazaki, Terumasa Hayashi, Takayuki Higashi, Yoshihide Hirohata, Shuji Horinouchi, Masayuki Inagaki, Masao Ishii, Tamayo Ishiko, Hideaki Jinnouchi, Hidetoshi Kanai, Daisuke Kanda, Hideo Kanehara, Masayuki Kashima, Kiyoe Kato, Takeshi Katsuki, Katsunori Kawamitsu, Satsuki Kawasaki, Fumi Kikuchi, Hidetoshi Kikuchi, Kunihisa Kobayashi, Junko Koide, Miyuki Kubota, Yoshiro Kusano, Hajime Maeda, Sunao Matsubayashi, Kazunari Matsumoto, Yasuto Matsuo, Naoki Matsuoka, Hiroaki Miyaoka, Satoshi Murao, Mikihiro Nakayama, Jun Nakazawa, Takashi Nomiyama, Masayuki Noritake, Takayuki Ogiwara, Hiroshi Ohashi, Hideki Okamoto, Takeshi Osonoi, Nobuhiro Sasaki, Taiji Sekigami, Taro Shibasaki, Hirotaka Shibata, Junji Shinoda, Hiroshi Sobajima, Kazuya Sugitatsu, Toshiyuki Sugiura, Toru Sugiyama, Daisuke Suzuki, Hiroyuki Suzuki, Masaaki Suzuki, Asami Takeda, Asami Tanaka, Seiichi Tanaka, Izumi Tsunematsu, Makoto Ujihara, Daishiro Yamada, Masayo Yamada, Kazuo Yamagata, Ken Yamakawa, Fumiko Yamakawa, Yoshimitsu Yamasaki, Yuko Yambe, Taihei Yanagida, Hidekatsu Yanai, Tetsuyuki Yasuda, Dovile Kriauciuniene, Jurate Lasiene, Antanas Navickas, Lina Radzeviciene, Egle Urbanaviciene, Gediminas Urbonas, Audrone Velaviciene, Rohana Abd Ghani, Nor Azizah Aziz, Li Yuan Lee, Chek Loong Loh, Norhaliza Mohd Ali, Nurain Mohd Noor, Nik Nur Fatnoon, Nik Ahmad, Jeyakantha Ratnasingam, Wan Hasnul Halimi Bin, Wan Hasan, Wan Mohd Izani, Wan Mohamed, Sandro Avila Pardo, Miriam Bastidas Adrian, Alfredo Chew Wong, Jorge Escobedo de la Peña, Guillermo Fanghänel Salmón, Guillermo González Gálvez, Ramiro Gutiérrez Ochoa, Saúl Irizar Santana, Gustavo Méndez Machado, Luis Nevarez Ruiz, Denisse Ramos Ibarra, Gabriel Ramos López, Leobardo Sauque Reyna, Gustavo Solache Ortiz, Rafael Valdez Ortiz, Juan Villagordoa Mesa, R.C. Bakker, J.N.M. Barendregt, A.H. Boonstra, Willem Bos, C.B. Brouwer, M. van Buren, Marielle Krekels, Ruud J.M. van Leendert, Louis A.G. Lieverse, P.T. Luik, E. Lars Penne, Peter Smak Gregoor, Liffert Vogt, John Baker, Veronica Crawford, Rick Cutfield, Peter Dunn, Jeremy Krebs, Kingsley Nirmalaraj, Russell Scott, Nine Smuts, Erik Eriksen, Hans Høivik, Thomas Karlsson, Peter Scott Munk, Maria Radtke, Knut Risberg, Jan Rocke, Leidulv Solnør, Aud-Eldrid Stenehjem, Anne-Beathe Tafjord, Glenda Pamugas, Araceli Panelo, Ronald Perez, Maribel Tanque, Louie Tirador, Michael Villa, Patrycja Butrymowicz, Kazimierz Ciechanowski, Grazyna Cieslik, Edward Franek, Michal Hoffmann, Jolanta Krzykowska, Ilona Kurnatowska, Katarzyna Landa, Adam Madrzejewski, Katarzyna Madziarska, Stanislaw Mazur, Piotr Napora, Michal Nowicki, Anna Ocicka-Kozakiewicz, Barbara Rewerska, Teresa Rusicka, Jan Ruxer, Ewa Skokowska, Andrzej Stankiewicz, Tomasz Stompor, Agnieszka Tiuryn-Petrulewicz, Katarzyna Wasilewska, Bogna Wierusz-Wysocka, Renata Wnetrzak-Michalska, Edgar Almeida, Rosa Ballesteros, Carlos Barreto, Idalina Beirao, Rita Birne, Cesar Esteves, Jose Guia, Susana Heitor, Olinda Marques, Pedro Melo, Fernando Nolasco, Amalia Pereira, Cristina Roque, Francisco Rosario, Gil Silva, Ana Silva, Ana Vila Lobos, Gregorio Cortes-Maisonet, Amaury Roman-Miranda, Adrian Albota, Cornelia Bala, Hortensia Barbonta, Elena Caceaune, Doina Catrinoui, Ciprian Constantin, Adriana Dumitrescu, Nicoleta Mindrescu, Cristina Mistode, Gabriela Negrisanu, Adriana Onaca, Silvia Paveliu, Ella Pintilei, Lavinia Pop, Amorin Popa, Alexandrina Popescu, Gabriela Radulian, Iosif Szilagyi, Liana Turcu, Georgeta Vacaru, Adrian Vlad, Mikhail Antsiferov, Mikhail Arkhipov, Andrey Babkin, Olga Barbarash, Vitaliy Baranov, Elena Chernyavskaya, Arkadiy Demko, Anton Edin, Polina Ermakova, Valentin Fadeev, Albert Galyavich, Leyla Gaysina, Ivan Gordeev, Irina Ipatko, Marina Kalashnikova, Yuriy Khalimov, Vadim Klimontov, Zhanna Kobalava, Elena Kosmacheva, Natalya Koziolova, Lyudmila Kvitkova Sergey Levashov, Roman Libis, Vyacheslav Marasaev, Natalia Malykh, Vladimir Martynenko, Sofya Malyutina, Imad Merai, Ashot Mkrtumyan, Galina Nechaeva, Nina Petunina, Shamil Palyutin, Leonid Pimenov, Elena Rechkova, Tatyana Rodionova, Oksana Rymar, Ruslan Sardinov, Olga Semenova, Alexander Sherenkov, Oleg Solovev, Elena Smolyarchuk, Leonid Strongin, Olga Ukhanova, Nadezhda Verlan, Natalya Vorokhobina, Davyd Yakhontov, Sergey Yakushin, Elena Zakharova, Alsu Zalevskaya, Olga Zanozina, Elena Zhdanova, Larisa Zhukova, Tatyana Zykova, Chee Fang Sum, Sufi Muhummad Suhail, Ru San Tan, Edmund Wong, Jana Babikova, Ingrid Buganova, Andrej Dzupina, Zuzana Ochodnicka, Dalibor Sosovec, Denisa Spodniakova, Fayzal Ahmed, Sindeep Bhana, Larry Distiller, Dirkie Jansen van Rensburg, Mukesh Joshi, Shaifali Joshi, Deepak Lakha, Essack Mitha, Gracjan Podgorski, Naresh Ranjith, Brian Rayner, Paul Rheeder, Mohamed Sarvan, Mary Seeber, Heidi Siebert, Mohammed Tayob, Julien Trokis, Dorothea Urbach, Louis van Zyl, Bum-Soon Choi, Moon Gi Choi, ChoonHee Chung, YouCheol Hwang, ChongHwa Kim, InJoo Kim, JaeHyeon Kim, SinGon Kim, SungGyun Kim, Tae Hee Kim, WooJe Lee, ByungWan Lee, Kang Wook Lee, Kook-Hwan Oh, Ji Eun Oh, Yun Kyu Oh, Dong-Jin Oh, Junbeom Park, Seok Joon Shin, Su-Ah Sung, Jae Myung Yu, Irene Agraz, Francisco Javier Ampudia, Hanane Bouarich, Francesca Calero, Cristina Castro, Secundino Cigarrán Guldris, Josep Cruzado Garrit, Fernando de Álvaro, Josep Galcerán, Olga González Albarrán, Julio Hernández Jaras, Meritxell Ibernón, Francisco Martínez Deben, Ma Dolores Martínez Esteban, José María Pascual Izuel, Judith Martins, Juan Mediavilla, Alfredo Michán, Esteban Poch, Manuel Polaina Rusillo, Carlos Sánchez Juan, Rafael Santamaría Olmo, José Julián, Segura de la Morena, Alfonso Soto, Maribel Troya, Annette Bruchfeld, Dan Curiac, Ken Eliasson, Malin Frank, Gregor Guron, Olof Hellberg, Margareta Hellgren, Hans Larnefeldt, Carl-Johan Lindholm, Magnus Löndahl, Erik Rein-Hedin, Inga Soveri, Jonas Spaak, Daniel Ackermann, Stefan Bilz, Christian Forster, Stefan Kalbermatter, Andreas Kistler, Antoinette Pechére-Bertschi, Bernd Schultes, Chiz-Tzung Chang, Cheng-Chieh Hung, Ju-Ying Jiang, Shuei-Liong Lin, Der-Cherng Tarng, Shih-Te Tu, Mai-Szu Wu, Ming-Ju Wu, Chaicharn Deerochanawong, Chagriya Kitiyakara, Vuddhidej Ophascharoensuk, Chatlert Pongchaiyakul, Bancha Satirapoj, Necmi Eren, Ibrahim Gul, Okan Gulel, Ismail Kocyigit, Abdulbaki Kumbasar, Idris Sahin, Burak Sayin, Talat Tavli, Sedat Ustundag, Yavuz Yenicerioglu, Iryna Bondarets, Volodymyr Botsyurko, Viktoriia Chernikova, Oleksandra Donets, Ivan Fushtey, Mariia Grachova, Anna Isayeva, Dmytro Kogut, Julia Komisarenko, Nonna Kravchun, Kateryna Malyar, Liliya Martynyuk, Vitaliy Maslyanko, Halyna Myshanych, Larysa Pererva, Nataliia Pertseva, Oleksandr Serhiyenko, Ivan Smirnov, Liubov Sokolova, Vasyl Stryzhak, Maryna Vlasenko, Ahmad AbouSaleh, Jonathan Barratt, Cuong Dang, Hassan Kahal, Adam Kirk, Anne Kilvert, Sui Phi Kon, Dipesh Patel, Sam Rice, Arutchelvam Vijayaraman, Yuk-ki Wong, Martin Gibson, Mona Wahba, Reza Zaidi, Idalia Acosta, Atoya Adams, Dilawar Ajani, Slamat Ali, Radica Alicic, Amer Al-Karadsheh, Sreedhara Alla, D. Allison, Nabil Andrawis, Ahmed Arif, Ahmed Awad, Masoud Azizad, Michael Bahrami, Shweta Bansal, Steven Barag, Ahmad Barakzoy, Mark Barney, Joshua Barzilay, Khalid Bashir, Jose Bautista, Srinivasan Beddhu, Diogo Belo, Sabrina Benjamin, Ramin Berenji, Anuj Bhargava, Jose Birriel, Stephen Brietzke, Frank Brosius, Osvaldo Brusco, Anna Burgner, Robert Busch, Rafael Canadas, Maria Caramori, Jose Cardona, Christopher Case, Humberto Cruz, Ramprasad Dandillaya, Dalia Dawoud, Zia Din, Bradley Dixon, Ankur Doshi, James Drakakis, Mahfouz El Shahawy, Ashraf El-Meanawy, Mohammed El-Shahawy, John Evans, George Fadda, Umar Farooq, Roland Fernando, Raymond Fink, Brian First, David Fitz-Patrick, John Flack, Patrick Fluck, Leon Fogelfeld, Vivian Fonseca, Juan Frias, Claude Galphin, Luis Garcia-Mayol, Gary Goldstein, Edgar Gonzalez, Francisco Gonzalez-Abreu, Ashwini Gore, David Grant, Violet Habwe, Maxine Hamilton, Jamal Hammoud, Stuart Handelsman, Israel Hartman, Glenn Heigerick, Andrew Henry, German Hernandez, Carlos Hernandez-Cassis, Carlos Herrera, Joachim Hertel, Wenyu Huang, Rogelio Iglesias, Ali Iranmanesh, Timothy Jackson, Mahendra Jain, Kenneth Jamerson, Karen Johnson, Eric Judd, Joshua Kaplan, Zeid Kayali, Bobby Khan, Muhammad Khan, Sourabh Kharait, M. Sue Kirkman, Nelson Kopyt, Wayne Kotzker, Csaba Kovesdy, Camil Kreit, Arvind Krishna, Saeed Kronfli, Keung Lee, Derek LeJeune, Brenda Lemus, Carlos Leon-Forero, Douglas Linfert, Henry Lora, Alexander Lurie, Geetha Maddukuri, Alexander Magno, Louis Maletz, Sreedhar Mandayam, Mariana Markell, Ronald Mayfield, Caroline Mbogua, Dierdre McMullen, Carl Meisner, Stephen Minton, Bharat Mocherla, Rajesh Mohandas, Manuel Montero, Moustafa Moustafa, Salil Nadkarni, Samer Nakhle, Jesus Navarro, Nilda Neyra, Romanita Nica, Philip Nicol, Paul Norwood, Visal Numrungroad, Richard O'Donovan, A. Odugbesan, Jorge Paoli-Bruno, Samir Parikh, Rakesh Patel, Aldo Peixoto, Pablo Pergola, Alan Perlman, Karlton Pettis, Roberto Pisoni, Mirela Ponduchi, Jorge Posada, Sharma Prabhakar, Jai Radhakrishnan, Mahboob Rahman, Rupesh Raina, Anjay Rastogi, Efrain Reisin, Marc Rendell, David Robertson, Michael Rocco, Hugo Romeu, Sylvia Rosas, Jack Rosenfeld, Dennis Ross, Jeffrey Rothman, Lance Rudolph, Yusuf Ruhullah, Gary Ruoff, Jeffrey Ryu, Mandeep Sahani, Ramin Sam, Garfield Samuels, William Sanchez, Vladimir Santos, Scott Satko, Sanjeev Saxena, David Scott, Gilberto Seco, Melvin Seek, Harvey Serota, Tariq Shafi, Nauman Shahid, Michael Shanik, Santosh Sharma, Arjun Sinha, James Smelser, Mark Smith, Kyaw Soe, Richard Solomon, Eugene Soroka, Joseph Soufer, Bruce Spinowitz, Leslie Spry, Rosa Suarez, Bala Subramanian, Harold Szerlip, Aparna Tamirisa, Stephen Thomson, Tuan-Huy Tran, Richard Treger, Gretel Trullenque, Thomas Turk, Guillermo Umpierrez, Daniel Urbach, Martin Valdes, Shujauddin Valika, Damaris Vega, Peter Weissman, Adam Whaley-Connell, Jonathan Winston, Jonathan Wise, Alan Wynne, Steven Zeig, Phuong Chu, Lam Van Hoang, Tran Khanh, Nguyen Thi Phi Nga, Pham Nguyen Son, and Lan Phuong Tran
References
- 1. Nelson RG, Grams ME, Ballew SH, et al.; CKD Prognosis Consortium . Development of risk prediction equations for incident chronic kidney disease. JAMA 2019;322:2104–2114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wu B, Bell K, Stanford A, et al. Understanding CKD among patients with T2DM: prevalence, temporal trends, and treatment patterns—NHANES 2007-2012. BMJ Open Diabetes Res Care 2016;4:e000154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. International Diabetes Federation . IDF Diabetes Atlas. 9th ed. Brussels, Belgium, International Diabetes Federation, 2019 [Google Scholar]
- 4. Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group . KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int 2020;98:S1–S115 [DOI] [PubMed] [Google Scholar]
- 5. American Diabetes Association . 6. Glycemic targets: standards of medical care in diabetes–2021. Diabetes Care 2021;44(Suppl. 1):S73–S84 [DOI] [PubMed] [Google Scholar]
- 6. Buse JB, Wexler DJ, Tsapas A, et al. 2019 update to: Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2020;63:221–228 [DOI] [PubMed] [Google Scholar]
- 7. American Diabetes Association . 11. Microvascular complications and foot care: standards of medical care in diabetes-2021. Diabetes Care 2021;44(Suppl. 1):S151–S167 [DOI] [PubMed] [Google Scholar]
- 8. Gor D, Gerber BS, Walton SM, Lee TA, Nutescu EA, Touchette DR. Antidiabetic drug use trends in patients with type 2 diabetes mellitus and chronic kidney disease: a cross-sectional analysis of the National Health and Nutrition Examination Survey. J Diabetes 2020;12:385–395 [DOI] [PubMed] [Google Scholar]
- 9. Rutherford PA, Thomas TH, Wilkinson R. Insulin resistance and hypertension--implications for treatment. Postgrad Med J 1991;67:869–875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhou MS, Wang A, Yu H. Link between insulin resistance and hypertension: what is the evidence from evolutionary biology? Diabetol Metab Syndr 2014;6:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Korytkowski M. When oral agents fail: practical barriers to starting insulin. Int J Obes Relat Metab Disord 2002;26(Suppl. 3):S18–S24 [DOI] [PubMed] [Google Scholar]
- 12. Rossing K, Christensen PK, Hovind P, Tarnow L, Rossing P, Parving HH. Progression of nephropathy in type 2 diabetic patients. Kidney Int 2004;66:1596–1605 [DOI] [PubMed] [Google Scholar]
- 13. UK Prospective Diabetes Study (UKPDS) Group . Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 14. Perkovic V, Heerspink HL, Chalmers J, et al.; ADVANCE Collaborative Group . Intensive glucose control improves kidney outcomes in patients with type 2 diabetes. Kidney Int 2013;83:517–523 [DOI] [PubMed] [Google Scholar]
- 15. Wong MG, Perkovic V, Chalmers J, et al.; ADVANCE-ON Collaborative Group . Long-term benefits of intensive glucose control for preventing end-stage kidney disease: ADVANCE-ON. Diabetes Care 2016;39:694–700 [DOI] [PubMed] [Google Scholar]
- 16. Korol S, Mottet F, Perreault S, Baker WL, White M, de Denus S. A systematic review and meta-analysis of the impact of mineralocorticoid receptor antagonists on glucose homeostasis. Medicine (Baltimore) 2017;96:e8719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yamaji M, Tsutamoto T, Kawahara C, et al. Effect of eplerenone versus spironolactone on cortisol and hemoglobin A1(c) levels in patients with chronic heart failure. Am Heart J 2010;160:915–921 [DOI] [PubMed] [Google Scholar]
- 18. Zhao JV, Xu L, Lin SL, Schooling CM. Spironolactone and glucose metabolism, a systematic review and meta-analysis of randomized controlled trials. J Am Soc Hypertens 2016;10:671–682 [DOI] [PubMed] [Google Scholar]
- 19. Bakris GL, Agarwal R, Anker SD, et al.; FIDELIO-DKD Investigators . Effect of finerenone on chronic kidney disease outcomes in type 2 diabetes. N Engl J Med 2020;383:2219–2229 [DOI] [PubMed] [Google Scholar]
- 20. Filippatos G, Anker SD, Agarwal R, et al.; FIDELIO-DKD Investigators . Finerenone and cardiovascular outcomes in patients with chronic kidney disease and type 2 diabetes. Circulation 2021;143:540–552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bakris GL, Agarwal R, Anker SD, et al.; on behalf of the FIDELIO-DKD study investigators; FIDELIO-DKD study investigators . Design and baseline characteristics of the Finerenone in Reducing Kidney Failure and Disease Progression in Diabetic Kidney Disease Trial. Am J Nephrol 2019;50:333–344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rossing P, Filippatos G, Agarwal R, et al. Finerenone in predominantly advanced CKD and T2D with or without SGLT-2i therapy. Kidney Int Rep 2022;7:36–45. DOI: https://doi.org/10.1016/j.ekir.2021.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Rossing P, Agarwal R, Anker SD, et al. Efficacy and safety of finerenone in patients with chronic kidney disease and type 2 diabetes by GLP-1RA treatment: a subgroup analysis from the FIDELIO-DKD trial. Diabetes Obes Metab 2022;24:125–134. DOI: https://doi.org/10.1111/dom.14558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Zinman B, Wanner C, Lachin JM, et al.; EMPA-REG OUTCOME Investigators . Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015;373:2117–2128 [DOI] [PubMed] [Google Scholar]
- 25. Wanner C, Inzucchi SE, Lachin JM, et al.; EMPA-REG OUTCOME Investigators . Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med 2016;375:323–334 [DOI] [PubMed] [Google Scholar]
- 26. Ferreira JP, Lamiral Z, McMurray JJV, et al. Impact of insulin treatment on the effect of eplerenone: insights from the EMPHASIS-HF Trial. Circ Heart Fail 2021;14:e008075. [DOI] [PubMed] [Google Scholar]
- 27. Patel A, MacMahon S, Chalmers J, et al.; ADVANCE Collaborative Group . Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560–2572 [DOI] [PubMed] [Google Scholar]
- 28. Ismail-Beigi F, Craven T, Banerji MA, et al.; ACCORD trial group . Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet 2010;376:419–430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Douros A, Lix LM, Fralick M, et al.; Canadian Network for Observational Drug Effect Studies (CNODES) Investigators . Sodium-glucose cotransporter-2 inhibitors and the risk for diabetic ketoacidosis: a multicenter cohort study. Ann Intern Med 2020;173:417–425 [DOI] [PubMed] [Google Scholar]
- 30. U.S. Food and Drug Administration, FDA Drug Safety Commission . FDA revises labels of SGLT2 inhibitors for diabetes to include warnings about too much acid in the blood and serious urinary tract infections. Accessed 21 July 2021. Available from https://www.fda.gov/drugs/drug-safety-and-availability/fda-revises-labels-sglt2-inhibitors-diabetes-include-warnings-about-too-much-acid-blood-and-serious#:~:text=FDA%20has%20added%20warnings%20about,and%20serious%20urinary%20tract%20infections
- 31. Ruilope LM, Agarwal R, Anker SD, et al.; FIGARO-DKD study investigators . Design and baseline characteristics of the Finerenone in Reducing Cardiovascular Mortality and Morbidity in Diabetic Kidney Disease Trial. Am J Nephrol 2019;50:345–356 [DOI] [PMC free article] [PubMed] [Google Scholar]