Graphical abstract
Keywords: Pulmonary hypertension, Right ventricle, Echocardiography, Free wall strain, Imaging
Highlights
-
•
RV function is an important prognostic factor in pulmonary arterial hypertension.
-
•
Several echocardiographic parameters are needed for a complete RV function assessment.
-
•
RV postsystolic strain patterns have a prognostic impact in IPAH.
-
•
RV postsystolic strain patterns may help in evaluating treatment response.
Introduction
A 37-year-old woman presented with severe idiopathic pulmonary arterial hypertension (IPAH) with mild right ventricular (RV) dysfunction. Right ventricular function is an important prognostic factor in IPAH, and several echocardiographic parameters are needed for a complete assessment. Three postsystolic strain patterns (I-III) of the RV free wall have been described and are associated with functional class and RV dysfunction in IPAH. Pattern I has been associated with normal RV size and function; pattern II with mild to absent RV dysfunction with an increased risk of functional class deterioration and hospitalization; and pattern III with severe RV dilation and dysfunction and worse clinical outcomes. In this case, classic echocardiographic parameters such as tricuspid annular plane systolic excursion (TAPSE), fractional area change (FAC), and tissue Doppler systolic annular velocity (TDI S’) showed mild RV dysfunction. The evaluation was complemented with an evaluation of the RV postsystolic strain pattern that resulted in a type II pattern. Since type II pattern has been associated with early-stage disease with a high risk of clinical worsening in patients with mild to absent RV dysfunction, this finding helped to better stratify clinical worsening risk in this patient. Treatment with ambrisentan and tadalafil was initiated, and after 6 months, clinical and echocardiographic parameters improved; the postsystolic strain pattern paralleled this improvement, changing from type II to type I.
Case Presentation
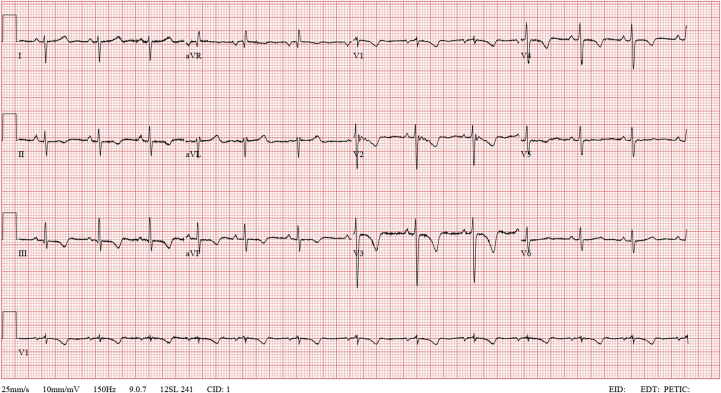
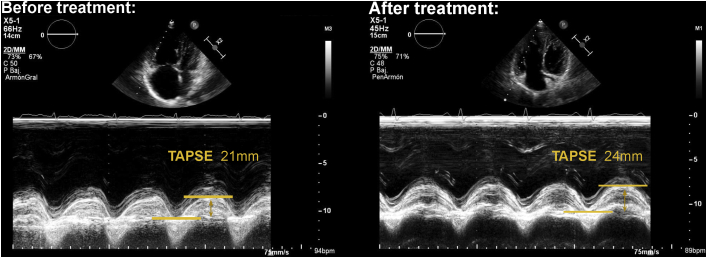
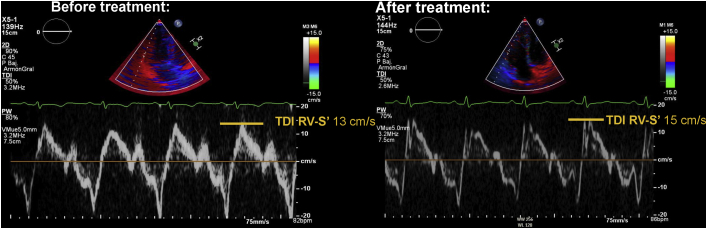
A 37-year-old woman presented at the cardiology outpatient clinic for exertional dyspnea (World Health Organization functional class III) and effort syncope 2 months after giving birth. Physical examination revealed no peripheral edema, murmur, or pulmonary crackles. She was well perfused, and oxygen saturation was 99% on room air. An electrocardiogram showed negative T waves in right precordial and inferior leads (Figure 1). An echocardiogram showed RV dilatation with RV end-diastolic area of 30.1 cm2, RV midcavity diameter of 43 mm, and basal diameter of 42 mm. It also showed mild RV dysfunction (Video 1) with FAC of 31%, TAPSE of 21 mm, and TDI S’ of 13 mm/sec (Figures 2 and 3), a prominent systolic D shape suggesting pressure overload (Video 2), moderate tricuspid regurgitation, and estimated pulmonary artery (PA) systolic pressure (PASP) of 73 mm Hg with a nondilated and collapsible inferior vena cava of 1.6 cm (Figure 4). Noninvasive right ventricle– (RV-) PA coupling evaluation with the TAPSE/PASP ratio showed a value of 0.29, suggesting progressive uncoupling. The left ventricle (LV) was nondilated (end-diastolic biplanar volume of 58 mL) with a left ventricular (LV) ejection fraction of 64%. There was no evidence of cardiac shunt (Qp/Qs = 1). The patient was referred to the emergency department for further evaluation.
Figure 1.
Electrocardiogram at clinical presentation showing sinus rhythm at 75 bpm, left posterior fascicular block, and T-wave inversion in inferior and precordial leads.
Figure 2.
Echocardiography: apical four-chamber, M-mode TAPSE evaluation. Left panel: TAPSE before treatment was 21 mm. Right panel: TAPSE after treatment was 24 mm.
Figure 3.
Echocardiography: apical four-chamber, TDI S′ evaluation. Left panel: TDI S′ before treatment was 13 cm/sec. Right panel: TDI S′ after treatment was 15 cm/sec.
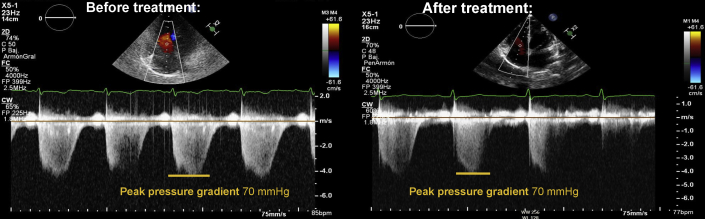
Figure 4.
Tricuspid regurgitation peak systolic pressure gradient before and after treatment. Apical four-chamber, systolic transtricuspid CW Doppler. Left panel: transtricuspid peak systolic pressure gradient before treatment was 70 mm Hg, inferior vena cava was nondilated and collapsible, and PASP was estimated at 73 mm Hg. Right panel: transtricuspid peak systolic pressure gradient after treatment was 70 mm Hg, inferior vena cava was nondilated and collapsible, and PASP was estimated at 73 mm Hg, virtually the same measure that was found before treatment.
Medical History
The patient had no cardiovascular risk factors or personal or family history of cardiovascular, pulmonary, or autoimmune disease. She had previously had two uncomplicated pregnancies and denied a history of chest pain, arthritis, or skin lesions suggestive of autoimmune disease.
Investigations
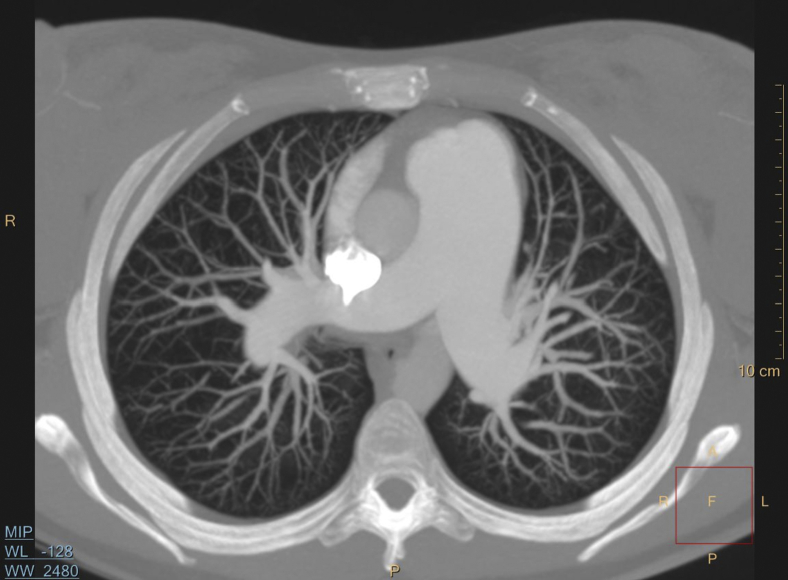
Based on the echocardiographic findings, the main differential diagnosis was pulmonary embolism. A computed tomography angiography showed the main PA was dilated (38 mm; Figure 5), with no pulmonary embolism. No parenchymal lung disease, anomalous pulmonary venous drainage, or interatrial or interventricular communications were found. Pulmonary function tests showed a slight reduction (63%) of the diffusing lung capacity for carbon monoxide. A pulmonary ventilation/perfusion scan was also normal. Right heart catheterization showed severe precapillary pulmonary hypertension (PASP, 98 mm Hg; diastolic PA pressure, 43 mm Hg; mean PA pressure, 66 mm Hg; wedge pressure, 10 mm Hg; cardiac output, 5.3 L/minute; cardiac index, 3.25 L/minute/m2, and pulmonary vascular resistance, 11 Wood units).
Figure 5.
Computed tomography angiography, thick-slice maximum intensity projection image, axial display showing pulmonary vessels without pulmonary embolism and main PA dilation (38 mm).
Blood tests were normal, and liver, thyroid, and kidney functions were within the normal range. Natriuretic peptide (NT-proBNP) was high (1,754 ng/L). Routine screening for connective tissue disease and screening for HIV and hepatitis viruses were negative.
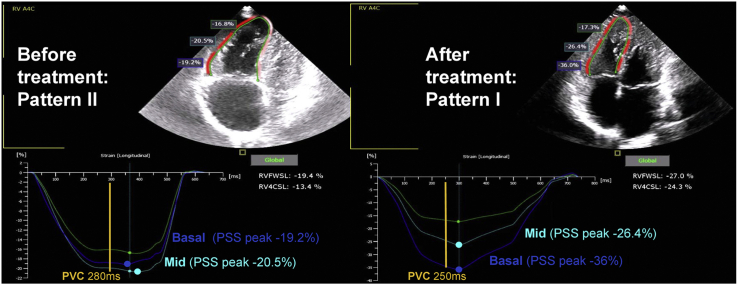
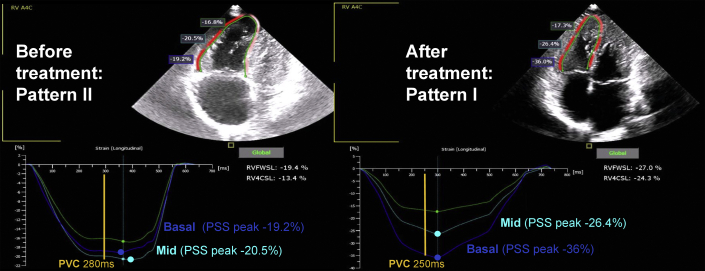
Idiopathic pulmonary arterial hypertension was diagnosed based on these results. The RV functional assessment was completed with a strain analysis showing an RV free-wall longitudinal strain (RVFWLS) of –19.4% (normal value, –37.2% to –20.8% from the World Alliance of Societies of Echocardiography study1) and a type II postsystolic strain pattern (Figure 6, Video 3). Both of these findings, RVFWLS and the postsystolic strain pattern, together with the TAPSE/PASP, contributed to a high risk of clinical worsening and progression to RV-PA uncoupling.
Figure 6.
Right ventricular postsystolic strain patterns before and after vasodilator treatment in IPAH, apical four-chamber RV-focused view for RV longitudinal strain evaluation. Left panel: RV longitudinal strain curve before vasodilator treatment showing an RVFWLS of –19.4% (normal value –37.2% to –20.8%)1 and an RV postsystolic strain pattern type II showing a steady negative plateau from peak systolic strain through early diastole, followed by a positive downward shift toward the baseline. Right panel: RV strain curve 6 months after initiation of vasodilator treatment showing an RVFWLS of –27% and an RV postsystolic strain pattern type I showing a downward shift of the curve after peak systolic strain toward the baseline, followed by end-diastolic straight curve. PSS peak, Postsystolic strain peak; PVC, Pulmonary valve closure.
Management
The patient started daily treatment with ambrisentan 10 mg and tadalafil 40 mg. Six months later, her symptoms had improved to World Health Organization functional class I and NT-proBNP was normal (118 ng/L). A follow-up serial echocardiogram showed the RV was less dilated (RV end-diastolic area, 21.1 cm2; RV midcavity diameter, 35 mm; basal diameter, 41 mm) with preserved systolic function (FAC, 40%; TAPSE, 24 mm; and TDI S’, 15 mm/sec; Videos 4, 5; Figures 2 and 3). Tricuspid regurgitation was mild, inferior vena cava measured 1.5 cm and inspiratory collapse was present, and PASP was estimated at 73 mm Hg just as previously seen (Figure 4). Right ventricular strain improved, showing an RVFWLS of –27% and a type I postsystolic strain pattern (Figure 6, Video 6). The TAPSE/PASP ratio showed an improvement from 0.28 to 0.33. Left ventricle parameters remained unaffected (end-diastolic biplanar volume of 58 mL and LV ejection fraction of 63%).
Discussion
Idiopathic pulmonary arterial hypertension is a severe clinical condition that results in progressive right heart failure due to chronic pressure overload. Current pulmonary hypertension guidelines for diagnostic workup include right heart catheterization to establish diagnosis, a transthoracic echocardiography to rule out left heart disease, a ventilation/perfusion lung scan to exclude chronic thromboembolic pulmonary hypertension, a chest computed tomography scan and pulmonary functional tests to exclude parenchymal lung disease, and routine screening of connective tissue disease, hepatitis, and HIV.2
Evaluation of RV function is recommended as a prognostic factor in IPAH together with parameters such as right atrial area and pericardial effusion.3 Current guidelines and position papers on RV echocardiographic assessment4,5 recommend the use of several parameters to better distinguish normal from abnormal RV function. Parameters such as TAPSE, FAC, TDI S’, and, more recently, RVFWLS are the most commonly used parameters for this assessment.
In January 2021, Badagliacca et al6 reported the prognostic impact of three postsystolic strain patterns of the RV free wall in a cohort of patients with IPAH reflecting progressive RV dyssynchrony. Pattern I was defined as a strain-time curve with a prompt downward return to baseline after the systolic peak with an end-diastolic straight line. This finding was associated with normal RV size and function. Pattern II corresponded to a strain-time curve with a postsystolic plateau followed by a return to baseline in end diastole. Even though patients with pattern II had mild to absent RV dysfunction, this condition predicted worse clinical outcomes than pattern I, such as functional class worsening and heart failure hospitalizations. Pattern III was defined as a postsystolic curve slowly and gradually moving toward baseline. This pattern was associated with severe functional class deterioration and severe RV dilation and dysfunction. It predicted worse clinical outcomes than pattern II.
Based on these results, Badaggliaca et al suggested that pattern II reflected an early stage of the disease with a high risk of clinical worsening and considered this finding to be of clinical value for risk stratification.
Here we report a case of IPAH with RV dilation and mild RV dysfunction parameters with mildly reduced FAC and RVFWLS but normal TAPSE and TDI S’; in addition to these findings, the postsystolic strain pattern type II suggested a poor prognosis. Pulmonary vasodilator treatment was initiated with good clinical response, and the RV strain postsystolic pattern changed from pattern II to pattern I within 6 months. Remarkably, RV echocardiographic improvement paralleled functional class improvement, despite the lack of a significant reduction in the estimated PASP. In addition, there was a mildly improved TAPSE/PASP ratio, which suggested an improvement in the RV-PA coupling.
In pulmonary hypertension the RV undergoes a morphological and functional adaptation to chronic pressure overload. Initially, coupling of the RV to the arterial load is achieved by increased contractility, concentric hypertrophy, and mild dilation. This process eventually leads to further dilation, hypertrophy, RV dysfunction, and RV dyssynchrony, resulting in reduced RV stroke volume and LV filling with progressive reduction of cardiac output.7 The echocardiographic evaluation of this process must be integrative of several echocardiographic parameters due to the broad spectrum of possible situations. In the setting of pressure or volume overload, RV initial adaptations may lead to a discrepancy between RV transversal shortening parameters (e.g., FAC%) and longitudinal shortening parameters (e.g., TAPSE) since the latter can be enhanced by initially increased contractility.8 Right ventricular systolic function interpretation in this situation is challenging, and newer echocardiographic parameters, such as RVFWLS, are emerging as more predictive options than conventional parameters in patients with pulmonary arterial hypertension.9,10
In the case that we present here, RV longitudinal shortening parameters such as TAPSE and TDI S’ were normal despite an impaired transversal shortening measured by FAC and RVFWLS, and in this context, finding a type II RV postsystolic strain pattern helped us to better understand and assess RV systolic dysfunction.
As reported in previous works,6 RV postsystolic patterns are reproducible, have prognostic impact, and may help to better define risk in patients with mild dysfunction as in the case we presented. In addition, we want to highlight that since RV postsystolic strain patterns reflect disease severity and are easily reproducible, they may be useful to evaluate treatment response as reported in this case, even though there is still a lack of evidence for this use and further investigation is needed.
Conclusion
No single echocardiographic parameter is sufficiently accurate to evaluate RV function, and an integrative approach is usually needed. Right ventricular postsystolic strain patterns add a new tool to assess RV compromise in IPAH and may be of interest in addition to other parameters to identify RV dysfunction early, establish prognosis, and guide patient response to treatment.
Footnotes
Conflicts of interest: The authors reported no actual or potential conflicts of interest relative to this document.
Supplementary data related to this article can be found at https://doi.org/10.1016/j.case.2022.03.005.
Supplementary Data
Pretreatment echocardiogram, apical four-chamber RV-focused view showing RV dilatation and mild dysfunction with FAC of 31% and TAPSE of 21 mm.
Pretreatment echocardiogram, parasternal short-axis midventricular level showing an LV systolic D shape suggesting RV pressure overload.
Pretreatment echocardiogram, apical four-chamber RV-focused view for RV longitudinal strain assessment showing an RVFWLS of –19.4% (normal value, –37.2% to –20.8%)1 and an RV postsystolic strain pattern type II showing a steady negative plateau from peak systolic strain through early diastole, followed by a positive downward shift toward baseline.
Follow-up serial echocardiogram after 6 months of pulmonary vasodilator treatment. Apical four-chamber, RV-focused view showing a less dilated RV with preserved systolic function. FAC was 40%, and TAPSE was 24 mm.
Follow-up serial echocardiogram after 6 months of pulmonary vasodilator treatment. Parasternal short-axis midventricular level showing an improvement in LV systolic D shape compared with the previous echocardiography.
Follow-up serial echocardiogram, apical four-chamber RV-focused view for RV longitudinal strain assessment after 6 months of pulmonary vasodilator treatment showing an RVFWLS of –27% (normal value, –37.2% to –20.8%)1 and an RV postsystolic strain pattern type I showing a downward shift of the curve after peak systolic strain toward the baseline, followed by end-diastolic straight curve.
References
- 1.Addetia K., Miyoshi T., Citro R., Daimon M., Gutierrez Fajardo P., Kasliwal R.R., et al. Two-dimensional echocardiographic right ventricular size and systolic function measurements stratified by sex, age, and ethnicity: results of the World Alliance of Societies of Echocardiography study. J Am Soc Echocardiogr. 2021;34:1148–1157. doi: 10.1016/j.echo.2021.06.013. [DOI] [PubMed] [Google Scholar]
- 2.Frost A., Badesch D., Gibbs J.S.R., Gopalan D., Khanna D., Manes A., et al. Diagnosis of pulmonary hypertension. Eur Respir J. 2019;53:1801904. doi: 10.1183/13993003.01904-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vonk Noordegraaf A., Chin K.M., Haddad F., Hassoun P.M., Hemnes A.R., Hopkins S.R., et al. Pathophysiology of the right ventricle and of the pulmonary circulation in pulmonary hypertension: an update. Eur Respir J. 2019;53:1801900. doi: 10.1183/13993003.01900-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lang R.M., Badano L.P., Mor-Avi V., Afilalo J., Armstrong A., Ernande L., et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28:1–39.e14. doi: 10.1016/j.echo.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Farmakis I.T., Demerouti E., Karyofyllis P., Karatasakis G., Stratinaki M., Tsiapras D., et al. Echocardiography in pulmonary arterial hypertension: is it time to reconsider its prognostic utility? J Clin Med. 2021;10:2826. doi: 10.3390/jcm10132826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Badagliacca R., Pezzuto B., Papa S., Poscia R., Manzi G., Pascaretta A., et al. Right ventricular strain curve morphology and outcome in idiopathic pulmonary arterial hypertension. JACC Cardiovasc Imaging. 2021;14:162–172. doi: 10.1016/j.jcmg.2020.08.017. [DOI] [PubMed] [Google Scholar]
- 7.Vonk Noordegraaf A., Westerhof B.E., Westerhof N. The relationship between the right ventricle and its load in pulmonary hypertension. J Am Coll Cardiol. 2017;69:236–243. doi: 10.1016/j.jacc.2016.10.047. [DOI] [PubMed] [Google Scholar]
- 8.Giusca S., Dambrauskaite V., Scheurwegs C., D’hooge J., Claus P., Herbots L., et al. Deformation imaging describes right ventricular function better than longitudinal displacement of the tricuspid ring. Heart. 2010;96:281–288. doi: 10.1136/hrt.2009.171728. [DOI] [PubMed] [Google Scholar]
- 9.Wright L., Dwyer N., Wahi S., Marwick T.H. Relative importance of baseline and longitudinal evaluation in the follow-up of vasodilator therapy in pulmonary arterial hypertension. JACC Cardiovasc Imaging. 2019;12:2103–2111. doi: 10.1016/j.jcmg.2018.08.017. [DOI] [PubMed] [Google Scholar]
- 10.Muraru D., Haugaa K., Donal E., Stankovic I., Voigt J.U., Petersen S.E., et al. Right ventricular longitudinal strain in the clinical routine: a state-of-the-art review. Eur Heart J Cardiovasc Imaging. 2022:jeac022. doi: 10.1093/ehjci/jeac022. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Pretreatment echocardiogram, apical four-chamber RV-focused view showing RV dilatation and mild dysfunction with FAC of 31% and TAPSE of 21 mm.
Pretreatment echocardiogram, parasternal short-axis midventricular level showing an LV systolic D shape suggesting RV pressure overload.
Pretreatment echocardiogram, apical four-chamber RV-focused view for RV longitudinal strain assessment showing an RVFWLS of –19.4% (normal value, –37.2% to –20.8%)1 and an RV postsystolic strain pattern type II showing a steady negative plateau from peak systolic strain through early diastole, followed by a positive downward shift toward baseline.
Follow-up serial echocardiogram after 6 months of pulmonary vasodilator treatment. Apical four-chamber, RV-focused view showing a less dilated RV with preserved systolic function. FAC was 40%, and TAPSE was 24 mm.
Follow-up serial echocardiogram after 6 months of pulmonary vasodilator treatment. Parasternal short-axis midventricular level showing an improvement in LV systolic D shape compared with the previous echocardiography.
Follow-up serial echocardiogram, apical four-chamber RV-focused view for RV longitudinal strain assessment after 6 months of pulmonary vasodilator treatment showing an RVFWLS of –27% (normal value, –37.2% to –20.8%)1 and an RV postsystolic strain pattern type I showing a downward shift of the curve after peak systolic strain toward the baseline, followed by end-diastolic straight curve.