Abstract
Objectives
The SARS-CoV-2 virus has spread worldwide, leading governments to implement mitigation measures. Understanding the reluctance to adhere to non-pharmacological interventions might help promote adherence to these measures. This study aimed to identify factors associated with non-adherence to the first lockdown in Portugal.
Study design
Cross-sectional study.
Methods
This study used data from a Portuguese community-based survey entitled ‘COVID-19 Barometer: Social Opinion’. Data were collected on risk perception, health status and social experiences using a snowball sampling technique. The event of interest corresponded to participants who reported not staying home during the lockdown period, serving as a proxy for non-adherence to lockdown. Logistic regression was used to identify factors associated with non-adherence to the first lockdown.
Results
Responses from 133,601 individual questionnaires that were completed during the first week of the first lockdown in 2020 were analysed. A minority of participants (5.6%) reported non-adherence to lockdown (i.e. leaving home for reasons other than essential situations). Working in the workplace was the factor with the strongest association of non-adherence to the lockdown. Several other factors were also associated with non-adherence to the first lockdown; namely, being a man, being a student, having a low level of education, having a low income, living alone or with a high-infection-risk professional (e.g. doctor, nurse, pharmaceutical, health technician, firefighter, police officer, military, essential services worker), perceiving the risk of getting COVID-19 to be high, not having social support in case of infection, feeling agitated, sad or anxious every day, and considering the preventive measures to be unimportant or inadequate.
Conclusions
Non-adherence to lockdown was associated with socio-economic, trust and perception factors. Future research should investigate the mechanisms underlying these associations to help identify the population groups who are most at risk of non-adherence.
Keywords: COVID-19, Lockdown, Adherence, Prevention, Non-pharmacological interventions
Introduction
At the end of 2019, a new coronavirus (SARS-CoV-2), which causes COVID-19, was found and rapidly spread worldwide. As of 19 May 2022, 519, 467, 357 cases and 6,277,833 deaths have been reported due to the SARS-CoV-2 virus.1 Restrictive measures were implemented to control the transmission of the virus, such as banning gatherings, closing public spaces, limiting working hours, introducing remote working as the preferred work environment, and promoting infection control measures, such as respiratory etiquette, frequent hand washing, reduction of facial touch and physical distancing.2 These measures reduced further COVID-19 transmission and mortality in several countries,3, 4, 5 including Portugal.6
Lockdowns have been one of the most widely implemented non-pharmaceutical interventions adopted by governments to help reduce the spread of SARS-CoV-2.7 , 8 In Portugal, the first national lockdown started on 22 March 2020 and people were asked to stay at home and leave only for essential reasons. Although the effectiveness of lockdowns relies on community adherence,9, 10, 11 citizens behave differently to restrictions.12 , 13 However, few studies have investigated which factors are associated with adherence to lockdown. To the best of the authors’ knowledge, only a few studies have explored factors associated with non-adherence to lockdown.14 , 15 These studies identified several factors related to stay-at-home order adherence, including age, education, geographical location, religious/spiritual beliefs, number of children, perceptions of physical health and social-emotional support.
In addition, several studies have explored the role of adherence to protective behaviours, such as the use of a mask,16 hand-washing17 and social distancing.18 Several factors associated with non-adherence to protective behaviours were similar to those identified in studies exploring non-adherence to lockdown. Some of the factors found associated with protective behaviours were gender,14 , 19, 20, 21, 22 age,21, 22, 23 geographical location,21 , 24 education level,22 , 24 , 25 household composition,14 , 20 income,19 , 24 work status,21 , 24 , 26 health status,20 , 27 health-related risk perception,11 , 20 , 22 perceived effectiveness of government ‘lockdown’ measures14 and trust in government and health authorities.28 Beliefs in specific conspiracy theories and political ideology, voting and political identification were also associated with less compliance with social distancing measures.29 In qualitative exploratory research, non-adherence to social distancing and social isolation during the COVID-19 pandemic was associated with financial losses, unclear government communication about physical distancing, observation of non-adherence in other individuals, and uncertainty about social reintegration and the future.19
The development and availability of a vaccine against COVID-19 and a high vaccination acceptance in several countries led to a reduction of non-pharmaceutical interventions. However, vaccination coverage varies between countries and continents.30 In addition, the need for a booster vaccination and the emergence of new variants might impact the current epidemiological situation. Thus, understanding adherence to non-pharmaceutical interventions remains crucial in the case of new outbreaks. A better understanding of the factors that are associated with compliance to lockdown measures could also help target health promotion messages to those non-adhering.31 , 32 Hence, this study aimed to assess and identify factors associated with non-adherence to the first lockdown in Portugal.
Methods
Study design and participants
Data were collected from the community-based survey entitled ‘COVID-19 Barometer: Social Opinion’.33 The questionnaire was administered online through the Microsoft Forms software program (Microsoft Corp). Invitations to participate were sent to existing contact networks and mailing lists, posted and promoted on social networks, and promoted to vulnerable groups through partnerships with patient associations, public health doctors and other healthcare professional groups. A snowball sampling technique was used, asking participants to forward the link to the questionnaire. The questionnaire was pretested to verify response times, ensure comprehensibility and resolve operational errors.
The survey asked questions on risk perception, health status and social experiences. Participants who answered the questionnaire between 21 and 27 March 2020 were included; participants not living in Portugal or who were aged <16 years were excluded.
Instruments
This study was interested in the responses to the question regarding preventive measures (i.e. ‘What recommendations from the health authorities did you take to prevent COVID-19 infection?’). The multiple option choice answers were: ‘No recommendations adopted’; ‘Leave home only in essential cases’; ‘Avoid touching common surfaces, such as handrails and door handles’; ‘Wash hands regularly’; ‘Cover mouth and nose when sneezing or coughing’; ‘Avoid contact with feverish or ill people’; ‘Avoid touching face’; ‘Avoid sharing food or personal utensils’; ‘Cook food properly’; ‘and ‘Prefer not to answer’. The dependent variable corresponds to the option ‘Leave home only in essential cases’. The outcome was categorised into two categories: ‘Yes’, corresponding to participants who stayed at home, and ‘No’, corresponding to participants who did not stay home (serving as a proxy for non-adherence to lockdown), which was the event of interest in this study. The questionnaire had another question assessing whether individuals stayed at home: ‘Are you at home, leaving only in situations of absolute necessity’, which was considered for a sensitivity analysis.
Independent variables were divided into five dimensions: demographic, social, labour, health and perceptions (see Supplementary Table S1). These variables were selected based on the literature review on adherence to preventive measures during a pandemic.23 , 34, 35, 36, 37
Statistical analyses
Variables were described using absolute and relative frequencies, and multicollinearity was checked using the variance inflation factor. Logistic regression was fitted for each dimension (Supplementary Table S1). We estimated crude odds ratios (ORs) and adjusted odds ratios (aORs), and their corresponding 95% confidence intervals (95% CIs). Each regression was adjusted for the demographic dimensions of age, gender, education and region. A complete case analysis was performed because there was very little missing data.
The questionnaire had two questions whose interpretation could be similar (i.e. ‘What recommendations from the health authorities did you take to prevent COVID-19 infection’ and ‘Are you at home, leaving only in situations of absolute necessity’). Thus, a sensitivity analysis was carried out only using data from individuals who answered the first question with ‘Leave home only in essential cases’ and the second question positively.
The level of significance considered for all analyses was 5%. The data analysis was performed using SPSS Statistics 26 Software (IBM).
Ethical approval
Before completing the questionnaire, participants read the informed consent. Only participants who gave their informed consent could see the questionnaire and were included in the study. Participation in this study was voluntary and anonymous. Participants were not asked for personal information. The study was conducted in agreement with the Declaration of Helsinki, and the Ethics Committee of the National School of Public Health approved the protocol (approval number: CE/ENSP/CREE/3/2020).
Results
Data from 133,601 individuals were obtained from a community-based survey. Only 5.6% of participants reported non-adherence to lockdown (i.e. leaving home for reasons other than essential situations). Supplementary Table S2 presents the characteristics of the study population. Overall, more women (64.3%) and individuals with a university degree (69.0%) participated in the study. The majority of participants were aged between 26 and 65 years (86.4%) and lived in the Lisbon and Tagus Valley (47.5%) and the North (24.1%).
Demographic dimension
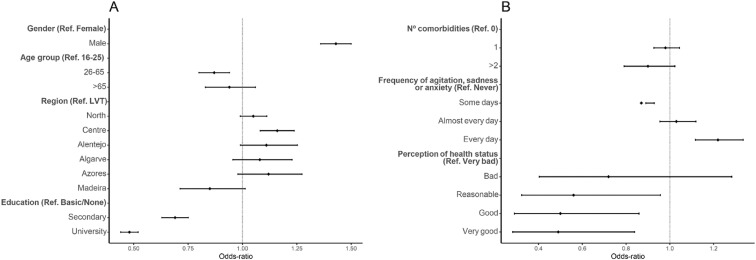
Men were more likely to non-adhere to lockdown than women (aOR: 1.43, 95% CI: [1.36; 1.50]). Individuals living in the Centre region were more likely to non-adhere to lockdown than individuals living in the Lisbon and Tagus Valley (aOR: 1.16, 95% CI: [1.08; 1.24]). Working-age adults (aged 26–65 years) were less likely to non-adhere to lockdown than young adults (aged 16–25 years) (aOR: 0.87, 95% CI: [0.80; 0.94]). Individuals with a higher level of education were also less likely to non-adhere to lockdown than individuals without education or with only a basic education (see Fig. 1 and Table 1 ).
Fig. 1.
Forest plot for non-adherence to lockdown. Adjusted odds ratio (adjusted for gender, age group, education and region) and the respective 95% confidence intervals are denoted by black dots and black lines, respectively. A — Forest plot of the demographic dimension. B — Forest plot of the health dimension.
Table 1.
Crude and adjusted odds of non-adherence to lockdown. Odds ratios were adjusted for the demographic dimensions (i.e. gender, age group, education and region)a.
| Dimension | Crude OR | 95% CI | Adjusted OR | 95% CI |
|---|---|---|---|---|
| Demographic dimension (N = 132,888) | ||||
| Gender (Ref. Female) | 1.51 | [1.44; 1.58] | 1.43 | [1.36; 1.50] |
| Age group, in years (Ref. 16, 17, 18, 19, 20, 21, 22, 23, 24, 25) | ||||
| 26–65 | 0.83 | [0.77; 0.90] | 0.87 | [0.80; 0.94] |
| >65 | 1.01 | [0.90; 1.14] | 0.94 | [0.83; 1.06] |
| Region (Ref. Lisbon and Tagus Valley) | ||||
| North | 1.07 | [1.01; 1.14] | 1.05 | [0.99; 1.11] |
| Centre | 1.19 | [1.12; 1.28] | 1.16 | [1.08; 1.24] |
| Alentejo | 1.14 | [1.02; 1.28] | 1.11 | [0.99; 1.25] |
| Algarve | 1.11 | [0.98; 1.26] | 1.08 | [0.96; 1.23] |
| Azores | 1.19 | [1.05; 1.36] | 1.12 | [0.98; 1.27] |
| Madeira | 0.85 | [0.72; 1.02] | 0.85 | [0.71; 1.01] |
| Education (Ref. Basic/No education) | ||||
| Secondary | 0.67 | [0.62; 0.73] | 0.69 | [0.63; 0.75] |
| University |
0.44 |
[0.41; 0.48] |
0.48 |
[0.44; 0.52] |
|
Social dimension (N = 130,119) | ||||
| Living alone (Ref. No) | 1.23 | [1.15;1,32] | 1.27 | [1.18; 1.36] |
| Living with the elderly or people with chronic illness (Ref. No) | 0.98 | [0.93; 1.03] | 1.01 | [0.95; 1.06] |
| Living with a high-infection-risk professional (Ref. No) | 1.31 | [1.23; 1.40] | 1.35 | [1.26; 1.44] |
| Social support in case of infection (Ref. Yes) | ||||
| None | 1.53 | [1.27; 1.84] | 1.44 | [1.19; 1.74] |
| Unsure | 1.13 | [0.97; 1.32] | 1.10 | [0.94; 1.28] |
| Not needed | 1.29 | [1.05; 1.58] | 1.26 | [1.02; 1.55] |
| Other |
1.25 |
[1.05; 1.48] |
1.22 |
[1.02; 1.46] |
|
Labour dimension (N = 99,574) | ||||
| Monthly household income (Ref. <650€) | ||||
| 651–1000€ | 0.83 | [0.74; 0.93] | 0.81 | [0.72; 0.91] |
| 1001–1500€ | 0.59 | [0.53; 0.66] | 0.62 | [0.55; 0.70] |
| 1501–2000€ | 0.51 | [0.45; 0.57] | 0.57 | [0.51; 0.65] |
| 2001–2500€ | 0.46 | [0.41; 0.53] | 0.53 | [0.47; 0.61] |
| > 2501€ | 0.48 | [0.42; 0.53] | 0.57 | [0.51; 0.65] |
| Unknown | 0.71 | [0.59; 0.85] | 0.85 | [0.70; 1.04] |
| Fear of losing income (Ref. Not concerned) | ||||
| Slightly concerned | 0.74 | [0.68; 0.81] | 0.83 | [0.76; 0.91] |
| Concerned | 0.88 | [0.81; 0.95] | 0.95 | [0.88; 1.04] |
| Very concerned | 0.91 | [0.84; 0.98] | 0.97 | [0.88; 1.05] |
| Occupation (Ref. Worker) | ||||
| Self-employed | 0.81 | [0.75; 0.87] | 0.93 | [0.86; 1.01] |
| Homemaker | 0.94 | [0.58; 1.54] | 1.01 | [0.60; 1.72] |
| Retired | 1.18 | [0.92; 1.52] | 1.83 | [1.40; 2.40] |
| Unemployed | 0.89 | [0.69; 1.15] | 1.05 | [0.79; 1.41] |
| Student | 0.99 | [0.88; 1.14] | 1.69 | [1.43; 1.99] |
| Other | 1.06 | [0.95; 1.19] | 1.08 | [0.95; 1.22] |
| Working mode (Ref. Remote work) | ||||
| At workplace | 4.75 | [4.48; 5.04] | 4.80 | [4.47; 5.15] |
| Suspended professional activity | 1.32 | [1.22; 1.43] | 1.23 | [1.12; 1.34] |
| High-infection-risk professional (Ref. No) |
1.96 |
[1.85; 2.08] |
0.92 |
[0.86; 0.99] |
|
Health dimension (N = 129,691) | ||||
| Number of comorbidities (Ref. 0) | ||||
| 1 | 1.04 | [0.98; 1.10] | 0.98 | [0.93; 1.04] |
| ≥2 | 1.08 | [0.95; 1.21] | 0.90 | [0.79; 1.02] |
| Frequency of agitation, sadness or anxiety (Ref. Never) | ||||
| Some days | 0.84 | [0.79; 0.89] | 0.87 | [0.89; 0.93] |
| Almost every day | 1.02 | [0.95; 1.10] | 1.03 | [0.95; 1.12] |
| Every day | 1.22 | [1.12; 1.33] | 1.22 | [1.12; 1.33] |
| Perception of health status (Ref. Very bad) | ||||
| Bad | 0.60 | [0.35; 1.01] | 0.72 | [0.40; 1.28] |
| Reasonable | 0.44 | [0.27; 0.71] | 0.56 | [0.32; 0.96] |
| Good | 0.37 | [0.23; 0.61] | 0.50 | [0.29; 0.86] |
| Very good |
0.35 |
[0.22; 0.58] |
0.49 |
[0.28; 0.84] |
|
Perceptions dimension (N = 126,301) | ||||
| Perception of the importance of the measures implemented by health authorities (Ref. Not important) | ||||
| Not very important | 0.63 | [0.46; 0.86] | 0.76 | [0.54; 1.07] |
| Important | 0.48 | [0.36; 0.64] | 0.75 | [0.54; 1.02] |
| Very important | 0.25 | [0.19; 0.34] | 0.44 | [0.33; 0.61] |
| Perception of the adequacy of measures implemented by the government (Ref. Not adequate) | ||||
| Not very adequate | 0.44 | [0.38; 0.50] | 0.67 | [0.56; 0.79] |
| Adequate | 0.32 | [0.28; 0.37] | 0.64 | [0.54; 0.76] |
| Very adequate | 0.29 | [0.25; 0.34] | 0.61 | [0.50; 0.74] |
| Confidence in the government's response to the pandemic (Ref. Not confident) | ||||
| Not very confident | 0.60 | [0.54; 0.65] | 0.86 | [0.77; 0.97] |
| Confident | 0.47 | [0.43; 0.52] | 0.81 | [0.71; 0.92] |
| Very confident | 0.49 | [0.44; 0.56] | 0.83 | [0.70; 0.98] |
| Confidence in the capacity of health services to respond to the pandemic (Ref. Not confident) | ||||
| Not very confident | 0.64 | [0.57; 0.71] | 0.91 | [0.80; 1.04] |
| Confident | 0.61 | [0.55; 0.67] | 1.00 | [0.88; 1.15] |
| Very confident | 0.69 | [0.60; 0.78] | 1.12 | [0.96; 1.31] |
| Self-perceived risk to get COVID-19 infection (Ref. Low/No risk) | ||||
| Moderate | 1.34 | [1.25; 1.41] | 1.38 | [1.29; 1.47] |
| High | 2.40 | [2.25; 2.57] | 2.37 | [2.21; 2.55] |
| Unknown | 1.21 | [1.11; 1.32] | 1.22 | [1.10; 1.35] |
| Self-perceived risk to develop severe disease (Ref. Low/No risk) | ||||
| Moderate | 1.14 | [1.07; 1.20] | 1.00 | [0.94; 1.06] |
| High | 1.36 | [1.28; 1.45] | 0.97 | [0.90; 1.05] |
| Unknown | 1.05 | [0.97; 1.14] | 0.95 | [0.86; 1.04] |
| Perceived risk to the population (Ref. Low/No risk) | ||||
| Moderate | 0.43 | [0.35; 0.53] | 0.50 | [0.41; 0.62] |
| High | 0.40 | [0.33; 0.48] | 0.45 | [0.36; 0.55] |
| Unknown | 0.43 | [0.33; 0.55] | 0.52 | [0.39; 0.69] |
OR, odds ratio; CI, confidence interval.
Bold indicates significant result.
In the sensitivity analysis, different results were observed regarding age and region. Older individuals were less likely to non-adhere to lockdown than young adults (Table 2 ).
Table 2.
Crude and adjusted odds of the sensitivity analysis of non-adherence to lockdown. Odds ratios were adjusted for the demographic dimensions (i.e. gender, age group, education and region)a.
| Dimension | Crude OR | 95% CI | Adjusted OR | 95% CI |
|---|---|---|---|---|
| Demographic dimension (N = 120,975) | ||||
| Gender (Ref. Female) | 1.81 | [1.69; 1.94] | 1.76 | [1.64; 1.89] |
| Age group, in years (Ref. 16, 17, 18, 19, 20, 21, 22, 23, 24, 25) | ||||
| 26-65 | 0.91 | [0.81; 1.04] | 0.95 | [0.84; 1.08] |
| >65 | 0.30 | [0.23; 0.39] | 0.26 | [0.20; 0.34] |
| Region (Ref. Lisbon and Tagus Valley) | ||||
| North | 1.02 | [0.94; 1.12] | 0.98 | [0.89; 1.07] |
| Centre | 1.23 | [1.11; 1.36] | 1.17 | [1.06; 1.29] |
| Alentejo | 1.30 | [1.10; 1.53] | 1.23 | [1.04; 1.45] |
| Algarve | 1.05 | [0.86; 1.27] | 0.99 | [0.82; 1.20] |
| Azores | 1.12 | [0.91; 1.37] | 1.00 | [0.82; 1.23] |
| Madeira | 0.49 | [0.35; 0.69] | 0.46 | [0.33; 0.65] |
| Education (Ref. Basic/No education) | ||||
| Secondary | 0.75 | [0.66; 0.86] | 0.73 | [0.64; 0.84] |
| University |
0.44 |
[0.39; 0.50] |
0.45 |
[0.40; 0.51] |
|
Social dimension (N = 118,481) | ||||
| Living alone (Ref. No) | 1.26 | [1.14; 1.39] | 1.25 | [1.12; 1.39] |
| Living with the elderly or people with chronic illness (Ref. No) | 0.83 | [0.77; 0.91] | 0.86 | [0.79; 0.94] |
| Living with a high-infection-risk professional (Ref. No) | 1.40 | [1.27; 1.54] | 1.44 | [1.30; 1.60] |
| Social support in case of infection (Ref. Yes) | ||||
| None | 1.71 | [1.31; 2.22] | 1.62 | [1.23; 2.12] |
| Unsure | 1.24 | [1.00; 1.54] | 1.22 | [0.97; 1.53] |
| Not needed | 1.40 | [1.03; 1.89] | 1.34 | [0.98; 1.83] |
| Other |
1.09 |
[0.83; 1.43] |
1.08 |
[0.82; 1.44] |
|
Labour dimension (N = 107,076) | ||||
| Monthly household income (Ref. <650€) | ||||
| 651–1000€ | 0.96 | [0.82; 1.13] | 0.94 | [0.79; 1.11] |
| 1001–1500€ | 0.61 | [0.52; 0.72] | 0.66 | [0.55; 0.78] |
| 1501–2000€ | 0.55 | [0.47; 0.65] | 0.67 | [0.56; 0.81] |
| 2001–2500€ | 0.49 | [0.41; 0.59] | 0.62 | [0.51; 0.75] |
| >2501€ | 0.50 | [0.42; 0.59] | 0.68 | [0.56; 0.81] |
| Unknown | 0.61 | [0.46; 0.81] | 0.95 | [0.69; 1.29] |
| Fear of losing income (Ref. Not concerned) | ||||
| Slightly concerned | 0.66 | [0.59; 0.74] | 0.78 | [0.68; 0.88] |
| Concerned | 0.72 | [0.65; 0.81] | 0.81 | [0.72; 0.92] |
| Very concerned | 0.73 | [0.66; 0.81] | 0.88 | [0.78; 1.00] |
| Occupation (Ref. Worker) | ||||
| Self-employed | 0.66 | [0.59; 0.74] | 0.90 | [0.80; 1.02] |
| Retired | 0.27 | [0.14; 0.55] | 0.58 | [0.29; 1.20] |
| Unemployed | 0.35 | [0.20; 0.60] | 0.88 | [0.47; 1.63] |
| Student | 0.59 | [0.47; 0.74] | 2.29 | [1.73; 3.03] |
| Other | 0.97 | [0.82; 1.14] | 1.03 | [0.85; 1.24] |
| Working mode (Ref. Remote work) | ||||
| At workplace | 19.5 | [17.49; 21.74] | 21.89 | [19.32;24.81] |
| Suspended professional activity | 1.14 | [0.96; 1.36] | 1.15 | [0.95; 1.39] |
| High-infection-risk professional (Ref. No) |
2.96 |
[2.74; 3.21] |
0.74 |
[0.67; 0.81] |
|
Health dimension (N = 118,140) | ||||
| Number of comorbidities (Ref. 0) | ||||
| 1 | 0.81 | [0.74; 0.89] | 0.82 | [0.74; 0.90] |
| ≥2 | 0.66 | [0.53; 0.83] | 0.66 | [0.52; 0.83] |
| Frequency of agitation, sadness or anxiety (Ref. Never) | ||||
| Some days | 0.73 | [0.67; 0.80] | 0.77 | [0.70; 0.84] |
| Almost every day | 0.98 | [0.87; 1.09] | 1.01 | [0.89; 1.13] |
| Every day | 1.25 | [1.11; 1.41] | 1.28 | [1.13; 1.46] |
| Perception of health status (Ref. Very bad) | ||||
| Bad | 0.57 | [0.21; 1.51] | 0.66 | [0.22; 1.94] |
| Reasonable | 0.66 | [0.27; 1.63] | 0.80 | [0.29; 2.19] |
| Good | 0.63 | [0.26; 1.54] | 0.75 | [0.27; 2.04] |
| Very good |
0.64 |
[0.26; 1.57] |
0.76 |
[0.28; 2.07] |
|
Perceptions dimension (N = 115,046) | ||||
| Perception of the importance of the measures implemented by health authorities (Ref. Not important) | ||||
| Not very important | 0.64 | [0.42; 0.96] | 0.74 | [0.47; 1.19] |
| Important | 0.48 | [0.33; 0.70] | 0.79 | [0.51; 1.21] |
| Very important | 0.20 | [0.13; 0.28] | 0.37 | [0.24; 0.57] |
| Perception of the adequacy of measures implemented by the government (Ref. Not adequate) | ||||
| Not very adequate | 0.35 | [0.30; 0.42] | 0.56 | [0.45; 0.70] |
| Adequate | 0.23 | [0.19; 0.27] | 0.54 | [0.43; 0.69] |
| Very adequate | 0.17 | [0.14; 0.21] | 0.49 | [0.37; 0.64] |
| Confidence in the government's response to the pandemic (Ref. Not confident) | ||||
| Not very confident | 0.53 | [0.47; 0.61] | 0.87 | [0.73; 1.03] |
| Confident | 0.36 | [0.32; 0.41] | 0.77 | [0.64; 0.93] |
| Very confident | 0.28 | [0.23; 0.34] | 0.67 | [0.51; 0.87] |
| Confidence in the capacity of health services to respond to the pandemic (Ref. Not confident) | ||||
| Not very confident | 0.59 | [0.50; 0.69] | 0.91 | [0.76; 1.09] |
| Confident | 0.51 | [0.44; 0.59] | 1.02 | [0.85; 1.23] |
| Very confident | 0.52 | [0.43; 0.63] | 1.15 | [0.91; 1.44] |
| Self-perceived risk to get COVID-19 infection (Ref. Low/No risk) | ||||
| Moderate | 2.06 | [1.85; 2.29] | 2.22 | [1.98; 2.48] |
| High | 5.00 | [4.49; 5.56] | 5.49 | [4.89; 6.18] |
| Unknown | 1.18 | [1.00; 1.39] | 1.26 | [1.04; 1.52] |
| Self-perceived risk to develop severe disease (Ref. Low/No risk) | ||||
| Moderate | 1.19 | [1.10; 1.31] | 0.94 | [0.86; 1.03] |
| High | 1.05 | [0.94; 1.16] | 0.64 | [0.60; 0.72] |
| Unknown | 0.88 | [0.78; 1.00] | 0.85 | [0.73; 0.99] |
| Perceived risk to the population (Ref. Low/No risk) | ||||
| Moderate | 0.39 | [0.29; 0.51] | 0.43 | [0.32; 0.58] |
| High | 0.32 | [0.25; 0.42] | 0.34 | [0.26; 0.46] |
| Unknown | 0.32 | [0.22; 0.46] | 0.41 | [0.27; 0.64] |
OR, odds ratio; CI, confidence interval.
Bold indicates significant result.
Health dimension
Individuals who felt agitated, sad or anxious some days were less likely to non-adhere to lockdown than individuals who never experienced these feelings (aOR: 0.87, 95% CI: [0.89; 0.93]). On the other hand, individuals who felt agitated, sad or anxious every day were more likely to non-adhere to lockdown than those who had never experienced these feelings (aOR: 1.22, 95% CI: [1.12; 1.33]). Individuals with a reasonable or good perception of their health status were less likely to non-adhere than individuals who perceived their health status as very bad (Fig. 1 and Table 1).
In the sensitivity analysis, health perception was no longer significant. However, we found that participants with comorbidities were less likely to non-adhere than participants without comorbidities (Table 2).
Social dimension
Individuals living alone or with high-infection-risk professionals were more likely to non-adhere to lockdown (aOR: 1.27, 95% CI: [1.18; 1.36] and aOR: 1.35, 95% CI: [1.26; 1.44], respectively). Individuals without social support or who do not need social support were more likely to non-adhere to lockdown than individuals who would receive social support in case of infection (aOR: 1.44, 95% CI: [1.19; 1.74] and aOR: 1.26, 95% CI: [1.02; 1.55], respectively) (Table 1).
The results were similar in the sensitivity analysis. Individuals living with the elderly or with people with chronic diseases were less likely to non-adhere to lockdown than individuals who were not living with the elderly or with people with chronic diseases (Table 2).
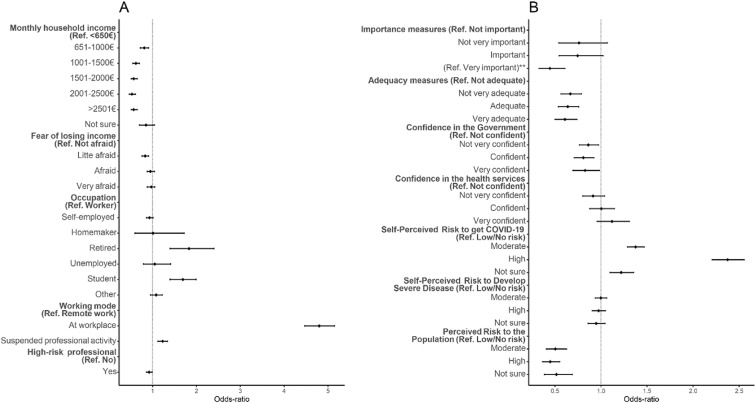
Labour dimension
Individuals with higher monthly household incomes were less likely to non-adhere to lockdown than individuals with a monthly household income below €650 (Fig. 2 and Table 1). Individuals who were slightly concerned about losing income were less likely to non-adhere to lockdown than individuals who were not concerned about losing income (aOR: 0.83, 95% CI: [0.76; 0.91]). Retired individuals and students were more likely to non-adhere to lockdown than workers (aOR: 1.83, 95% CI: [1.40; 2.40], and aOR: 1.69, 95% CI: [1.43; 1.99], respectively). High-infection-risk professionals were less likely to non-adhere to lockdown than non–high-infection-risk professionals (aOR: 0.92, 95% CI: [0.86; 0.99]). This study also found a strong association between working at the workplace and remote work (aOR: 4.80, 95% CI: [4.47; 5.15]). Individuals working at the workplace were more likely to non-adhere to lockdown than individuals who were working remotely. Individuals who suspended their working activities were also more likely to non-adhere to lockdown than individuals who were working remotely (aOR: 1.23, 95% CI: [1.12; 1.34]) (Fig. 2 and Table 1).
Fig. 2.
Forest plot for non-adherence to lockdown. Adjusted odds ratio (adjusted for gender, age group, education and region) and the respective 95% confidence intervals are denoted by black dots and black lines, respectively. A — Forest plot of the labour dimension. B — Forest plot of the perceptions dimension.
The results were similar in the sensitivity analysis. No evidence was found of an association for individuals who suspended their work activities and retired individuals (Table 2).
Perceptions dimension
Individuals who perceived the measures implemented by the health authorities as very important were less likely to non-adhere to lockdown than individuals who perceived them as not important (aOR: 0.44, 95% CI: [0.33; 0.61]). Individuals who perceived the measures implemented to be inadequate were more likely to non-adhere than individuals who found them adequate or not very adequate. Similarly, individuals without any confidence in the government's response to the pandemic were more likely to non-adhere than individuals who had some level of confidence. Regarding the risk of getting COVID-19, individuals who perceived their risk to be moderate, high or were unsure were more likely to non-adhere to lockdown than those who perceived their risk as low or null. On the other hand, individuals who perceived the population risk of getting COVID-19 as moderate, high or unsure were less likely to non-adhere than those who perceived the population risk as low or null (Fig. 2 and Table 1).
Results were similar in the sensitivity analysis (Table 2).
Discussion
The main objective of this study was to identify factors associated with non-adherence to the first lockdown in Portugal. The present study found that a minority of participants (5.6%) reported non-adherence to lockdown (i.e. leaving home for reasons other than essential situations). The study found that the following factors were associated with non-adherence to lockdown: being a man, having a lower level of education, living alone, living with a professional at high risk of getting infected, having no support in case of infection, belonging to a low-income household, being a student, continuing to work at the workplace, having a higher risk perception of becoming infected, feeling agitated, sad or anxious every day, not having confidence in the government and considering mitigation measures as unimportant or inappropriate.
Demographic, social and labour dimensions
Participants who continued working at the workplace had an almost five-fold increased likelihood of non-adherence to lockdown than participants who worked from home. Other studies have also indicated that work-related conditions might influence preventive behaviours.26 Workers who cannot transition to remote working were less likely to adhere to lockdown or adopt preventive behaviours, such as social distancing.24 , 38 It could be hypothesised that travelling to work could lead to other unnecessary trips. This idea could also be corroborated by the fatalism effect, in which an individual believes that their exposure to risk makes it practically inevitable that they will be infected, thereby reducing the adoption of preventive behaviours.39, 40, 41 As remote working was one of the most implemented lockdown measures, further studies should replicate the present study findings to ascertain the real effect of remote working on adherence to lockdown.
Individuals with lower household incomes were also more likely to non-adhere to the lockdown, which is in line with results from other studies.24 , 34 This finding could represent individuals with lower incomes who might work in precarious conditions and who were unable to work from home or those who have fewer savings to help them during lockdowns.24 , 34 Providing support or means of subsistence for certain families can be a way of mitigating these differences. The literature shows that compliance with public health recommendations is higher when living standards are maintained. Governments that provide economic reassurance (e.g. wage compensation or temporarily suspending reimbursements to the state),26 food support19 or free Internet access at home25 might experience higher rates of adherence to lockdown. Similarly, individuals with lower levels of education were also more likely to non-adhere to the lockdown. However, this association was not found in all studies.22 , 24 , 42 The present study also showed that students were more likely to non-adhere to lockdown, and men were more likely to non-adhere. Both findings have been documented in other studies.14 , 19 , 20 , 23 , 24 , 26
Socially, individuals without a support system in case of infection or individuals living alone were more likely to non-adhere to the lockdown. These results were corroborated by other studies.14 , 26 Surprisingly, living with a high-infection-risk professional (e.g. doctor, nurse, pharmaceutical, health technician, firefighter, police officer, military, essential services worker) increased the odds of non-adherence, which might be explained by the increased exposure to risk and the fatalism effect discussed previously.39, 40, 41
Health and perception dimensions
A strong association was found between the self-perceived risk of getting infected and non-adherence to lockdown. This association has been shown in other studies and could also be related to the fatalism effect.39, 40, 41 Having a high self-perceived risk of getting infected, or being unsure of their risk, seems intuitively more associated with adopting protective behaviours. However, the literature shows that fear associated with a higher perception of risk can trigger paradoxical actions, exacerbate already existing stressors of the COVID-19 pandemic and produce unintended consequences, such as denial, backlash, avoidance, defensiveness, depression, anxiety, increased risk behaviour and a feeling of lack of control.43 Nevertheless, fear is a natural response to the pandemic. Thus, communication messages should explore fear using an optimistic approach. Some studies suggest that exploiting the fear of being infected can be helpful in certain situations, such as pandemics, especially alongside effective messages by the health authorities encouraging the adoption of preventive behaviours.45
The idea of infecting vulnerable people can trigger the adoption of behaviours such as physical distancing.46 In this situation, people are more likely to make sacrifices, such as staying at home to protect individuals they can relate to. This idea is corroborated by the ‘Victim Effect’, which refers to the likelihood of helping strangers with whom we empathise compared with unknown individuals. This effect persists even when anonymity is maintained,47 for instance, personalising risk communication referring to our grandparents instead of individuals aged >65 years.47, 48, 49
Individuals who did not trust the government were found to have an increased likelihood of non-adherence to the lockdown. This association has been shown in other studies14 and during the H1N1 influenza outbreak.50 According to the Trust and Cooperation Model, trust is an important factor in risk management because it affects public judgment when assessing the harm and benefits of a measure. Hence, people with high levels of trust in institutions are more likely to accept recommendations.51 A lack of confidence in the capability of authorities to manage a public health crisis can feed uncertainty and scepticism about their recommendations.52 Risk communication should therefore focus on building trust in close collaboration with health services and the media.11
The present study also suggests that poor health perception was positively associated with non-adherence to lockdown. This is in line with other analyses that showed that neither having a previous medical condition increased the adoption of preventive behaviours24 nor having a previous health problem was a significant factor in self-protection.53
Limitations and strengths
The present study does not represent the Portuguese population because more women, participants living in Lisbon and Tagus Valley and participants with higher levels of education responded to the questionnaire, which does not correspond to the national demographics.54 The results may also be subject to sampling bias as some households in Portugal do not have access to the Internet (or have only limited access). The present study sample is likely to include more respondents sensitive to health issues (i.e. a non-response bias). Another limitation of this work is related to the dependent variable. Participants might have understood ‘essential cases’ differently. These limitations might affect the generalisability of the current results. Nevertheless, the study included a large sample, allowing a better understanding of non-adherence to lockdown in the studied population. The dissemination of an online questionnaire is a safe and effective way to reach the population, which is an essential factor to consider during a pandemic. Another advantage relates to the variety of themes analysed in the questionnaire, which provides a better view of how these factors might be interconnected and should be further explored.
Future work and challenges
Although several countries have a high COVID-19 vaccination rate, the need for booster vaccinations and the emergence of new strains might bring further restrictions. Some authors have studied COVID-19 vaccine booster hesitancy and found that acceptance decreases over time.55, 56, 57 Thus, it is important to fully understand non-adherence to lockdowns and other preventive measures. Although the present study sheds some light on certain factors associated with non-adherence, human intentions change over time, especially during a pandemic. A longitudinal study is essential to assess changes in the population responses to the pandemic (i.e. the factors associated with non-adherence to the lockdown identified in the present study may not be present at other stages of the pandemic).
Conclusion
Understanding the factors associated with non-adherence to lockdown can support the development of specific policies to mitigate social and economic inequalities and communication messages tailored to priority populations.
Author statements
Acknowledgements
We thank all the participants who answered the questionnaire for their contribution to this study.
Ethical approval
The study was conducted in agreement with the Declaration of Helsinki, and the Ethics Committee of the National School of Public Health approved the protocol (approval number: CE/ENSP/CREE/3/2020).
Funding
None declared.
Competing interests
None declared.
Data availability statement
The data underlying this article will be shared on reasonable request to the corresponding author.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.puhe.2022.07.001.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- 1.ECDC . 2022. COVID-19 situation update worldwide, as of week 19, updated 19 May 2022 [Internet]. Situation updates on COVID-19.https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases [cited 2022 May 26]. Available from: [Google Scholar]
- 2.Brauner J.M., Mindermann S., Sharma M., Johnston D., Salvatier J., Gavenčiak T., et al. The effectiveness of eight nonpharmaceutical interventions against COVID-19 in 41 countries. Science (80) 2020 2020.05.28.20116129. [Google Scholar]
- 3.Flaxman S., Mishra S., Gandy A., Unwin H.J.T., Mellan T.A., Coupland H., et al. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature. 2020;584(7820):257–261. doi: 10.1038/s41586-020-2405-7. [DOI] [PubMed] [Google Scholar]
- 4.Cowling B.J., Ali S.T., Ng T.W.Y., Tsang T.K., Li J.C.M., Fong M.W., et al. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5(5):e279–e288. doi: 10.1016/S2468-2667(20)30090-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walker P.G., Whittaker C., Watson O., Baguelin M., Ainslie K.E.C., Bhatia S., et al. Imperial College COVID-19 Response Team; 2020 March. p. 19. (The global impact of COVID-19 and strategies for mitigation and suppression). [Google Scholar]
- 6.Peixoto V.R., Vieira A., Aguiar P., Carvalho C., Thomas D.R., Abrantes A. Initial assessment of the impact of the emergency state lockdown measures on the 1st wave of the COVID-19 epidemic in Portugal. Acta Med Port. 2020;33(11):733–741. doi: 10.20344/amp.14129. [DOI] [PubMed] [Google Scholar]
- 7.López L., Rodó X. The end of social confinement and COVID-19 re-emergence risk. Nat Human Behav [Internet] 2020;4(7):746–755. doi: 10.1038/s41562-020-0908-8. Available from: [DOI] [PubMed] [Google Scholar]
- 8.Desvars-Larrive A., Dervic E., Haug N., Niederkrotenthaler T., Chen J., Di Natale A., et al. A structured open dataset of government interventions in response to COVID-19. Sci Data. 2020;7(1):1–9. doi: 10.1038/s41597-020-00609-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raude J.S.M. Lay perceptions of the pandemic influenza threat. Eur J Epidemiol. 2009;24(7):339–342. doi: 10.1007/s10654-009-9351-x. [DOI] [PubMed] [Google Scholar]
- 11.Webster R.K., Brooks S.K., Smith L.E., Woodland L., Wessely S., Rubin G.J. How to improve adherence with quarantine: rapid review of the evidence. Publ Health. 2020;182:163–169. doi: 10.1016/j.puhe.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sparrow R., Dartanto T., Hartwig R. Indonesia under the new normal: challenges and the way ahead. Appl Artif Intell. 2020;56(3):269–299. [Google Scholar]
- 13.Zhao S.Z., Wong J.Y.H., Wu Y., Choi E.P.H., Wang M.P., Lam T.H. Social distancing compliance under covid-19 pandemic and mental health impacts: a population-based study. Int J Environ Res Publ Health. 2020;17(18):1–11. doi: 10.3390/ijerph17186692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith L.E., Amlôt R., Lambert H., Oliver I., Robin C., Yardley L., et al. Factors associated with adherence to self-isolation and lockdown measures in the UK: a cross-sectional survey. Publ Health. 2020;187:41–52. doi: 10.1016/j.puhe.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lemacks J.L., Greer T., Aras S., Abbott L., Willis D., Gipson J., et al. Social determinants of health related to stay-at-home order adherence and social distancing attitudes among a diverse Deep South population. BMC Publ Health. 2021;21(2145):1–11. doi: 10.1186/s12889-021-12093-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li H., Yuan K., Sun Y.K., Zheng Y.B., Xu Y.Y., Su S.Z., et al. Efficacy and practice of facemask use in general population: a systematic review and meta-analysis. Transl Psychiatry. 2022;12 doi: 10.1038/s41398-022-01814-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang S., Li L.Z., van Antwerpen N., Suparman S., Gayatri M., Sari N.P., et al. Hand hygiene and mask-wearing practices during COVID-19 among healthcare workers: misinformation as a predictor. Am J Trop Med Hyg. 2021;105(6):1483–1489. doi: 10.4269/ajtmh.21-0463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gratz K.L., Richmond J.R., Woods M.A.S.E., Dixon-gordon M.S.K.L., Scamaldo K.M., Rose M.A.J.P., et al. Adherence to social distancing guidelines throughout the COVID- 19 pandemic : the roles of pseudoscientific beliefs , trust , political party Affiliation , and risk perceptions. Ann Behav Med. 2021;55:399–412. doi: 10.1093/abm/kaab024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams S.N., Armitage C.J., Tampe T., Dienes K. Public perceptions and experiences of social distancing and social isolation during the COVID-19 pandemic: a UK-based focus group study. BMJ Open. 2020;10(e039334) doi: 10.1136/bmjopen-2020-039334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pollak Y., Dayan H., Shoham IB R. Predictors of adherence to public health instructions during the COVID-19 pandemic. Psychiatr Clin Neurosci. 2020 doi: 10.1111/pcn.13122. [DOI] [PubMed] [Google Scholar]
- 21.Villela EF. de M., Lopez R.V.M., Sato A.P.S., Oliveira FM de, Waldman E.A., Bergh R Van den, et al. COVID-19 outbreak in Brazil: adherence to national preventive measures and impact on people's lives. BMC Publ Health. 2021;21(152) doi: 10.1186/s12889-021-10222-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bish A., Michie S. Demographic and attitudinal determinants of protective behaviours during a pandemic: a review. Br J Health Psychol. 2010;15(4):797–824. doi: 10.1348/135910710X485826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Park Crystal L., Russell Beth S., Fendrich Michael, Finkelstein-Fox Lucy, Hutchison Morica, Becker J. Americans' COVID-19 stress, coping, and adherence to CDC guidelines. J Gen Intern Med. 2020;35(8):2296–2303. doi: 10.1007/s11606-020-05898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Papageorge N.W., Zahn M.V., Jamison J.C., Tripodi E., Zahn M.V., Jamison J.C., et al. 2020. (Socio-demographic factors associated with self-protecting behavior during the COVID-19 pandemic). IZA Discussin Papers 13333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soofi M., Najafi F., Karami-Matin B. Using insights from behavioral economics to mitigate the spread of COVID-19. Appl Health Econ Health Pol. 2020;18(3):345–350. doi: 10.1007/s40258-020-00595-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hills S., Eraso Y. Factors associated with non-adherence to social distancing rules during the COVID-19 pandemic: a logistic regression analysis. BMC Publ Health. 2021;21(1):1–25. doi: 10.1186/s12889-021-10379-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Teasdale E., Santer M., Geraghty A.W.A., Little P., Yardley L. Public perceptions of non-pharmaceutical interventions for reducing transmission of respiratory infection: systematic review and synthesis of qualitative studies. BMC Publ Health. 2014;14:589. doi: 10.1186/1471-2458-14-589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Han Q., Zheng B., Cristea M., Agostini M., Belanger J., Gutzkow B., et al. Trust in government regarding COVID-19 and its associations with preventive health behaviour and prosocial behaviour during the pandemic: a cross-sectional and longitudinal study. Psychol Med. 2021;26:1–11. doi: 10.1017/S0033291721001306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gualda E., Krouwel A., Palacios-gálvez M., Morales-marente E. Social distancing and COVID-19: factors associated with compliance with social distancing norms in. Front Psychol. 2021;12:1–15. doi: 10.3389/fpsyg.2021.727225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ye Y., Zhang Q., Wei X., Cao Z., Yuan H., Zeng D.D. Equitable access to COVID-19 vaccines makes a life-saving difference to all countries. Nat Human Behav. 2022;6(February):207–216. doi: 10.1038/s41562-022-01289-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vosoughi S., Roy D., Aral S. The spread of true and false news online. Science (80) 2018;359(6380):1146–1151. doi: 10.1126/science.aap9559. [DOI] [PubMed] [Google Scholar]
- 32.Soper G.A. The lessons of the pandemic. Science (80) 1919;49(1274):501–506. doi: 10.1126/science.49.1274.501. [DOI] [PubMed] [Google Scholar]
- 33.Pedro A.R., Gama A., Soares P., Moniz M., Laires P.A., Dias S. COVID-19 barometer: social opinion - what do the Portuguese think in this time of COVID-19? Port J Public Heal. 2020;38(suppl 1):42–50. [Google Scholar]
- 34.Atchison C., Bowman L., Vrinten C., Redd R., Pristera P., Eaton J., et al. Early perceptions and behavioural responses during the COVID-19 pandemic: a cross-sectional survey of UK adults. BMJ Open. 2021;11(1):e043577. doi: 10.1136/bmjopen-2020-043577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Setbon M., Le Pape M.C., Létroublon C., Caille-Brillet A.L., Raude J. The public's preventive strategies in response to the pandemic influenza A/H1N1 in France: distribution and determinants. Prev Med (Baltim) [Internet] 2011;52(2):178–181. doi: 10.1016/j.ypmed.2010.11.010. Available from: [DOI] [PubMed] [Google Scholar]
- 36.Czeisler M.É., Tynan M.A., Howard M.E., Honeycutt S., Fulmer E.B., Kidder D.P., et al. Public attitudes, behaviors, and beliefs related to COVID-19, stay-at-home orders, nonessential business closures, and public health guidance — United States, New York City, and Los Angeles, May 5–12, 2020. Morb Mortal Wkly Rep. 2020;69 doi: 10.15585/mmwr.mm6924e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Clark C., Davila A., Regis M., Kraus S. Predictors of COVID-19 voluntary compliance behaviors: an international investigation. Glob Transit. 2020;2:76–82. doi: 10.1016/j.glt.2020.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eastwood K., Durrheim D., Francis J.L., Tursan d'Espaignet E., Duncan S., Islam F., et al. Knowledge about pandemic influenza and compliance with containment measures among Australians. Bull World Health Organ. 2009;87:588–594. doi: 10.2471/BLT.08.060772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.West R., Michie S., Rubin G.J., Amlôt R. Applying principles of behaviour change to reduce SARS-CoV-2 transmission. Nat Hum Behav. 2020;4:451–459. doi: 10.1038/s41562-020-0887-9. [DOI] [PubMed] [Google Scholar]
- 40.Akesson J., Ashworth-Hayes S., Hahn R., Metcalfe R., Rasooly I. Natlional Bureau of Economic Research; 2020. (Fatalism, beliefs, and behaviors during the COVID-19 pandemic). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jimenez T., Restar A., Helm P.J., Cross R.I., Barath D., Arndt J. Fatalism in the context of COVID-19: perceiving coronavirus as a death sentence predicts reluctance to perform recommended preventive behaviors. SSM Popul Health. 2020;11 doi: 10.1016/j.ssmph.2020.100615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pedersen M.J., Favero N. Social distancing during the COVID-19 pandemic: who are the present and future noncompliers? Publ Adm Rev. 2020;80(5):805–814. doi: 10.1111/puar.13240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stolow J.A., Moses L.M., Lederer A.M., Carter R. How fear appeal approaches in COVID-19 health communication may be harming the global community. Health Educ Behav. 2020;47(4):531–535. doi: 10.1177/1090198120935073. [DOI] [PubMed] [Google Scholar]
- 45.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lunn P., Timmons S., Barjaková M., Belton C., Julienne H., Lavin C. Motivating social distancing during the COVID-19 pandemic: an online experiment. Soc Sci Med. 2020;265 doi: 10.1016/j.socscimed.2020.113478. [DOI] [PubMed] [Google Scholar]
- 47.Jenni K., Loewenstein G. Explaining the identifiable victim effect. J Risk Uncertain. 1997;14(3):235–257. [Google Scholar]
- 48.Small D.A., Loewenstein G. Helping a victim or helping the victim: altruism and identifiability. J Risk Uncertain. 2003;26(1):5–16. [Google Scholar]
- 49.Pfattheicher S., Nockur L., Böhm R., Sassenrath C., Petersen M.B. The emotional path to action: empathy promotes physical distancing and wearing of face masks during the COVID-19 pandemic. Psychol Sci. 2020;31(11):1363–1373. doi: 10.1177/0956797620964422. [DOI] [PubMed] [Google Scholar]
- 50.Rubin G.J., Amlôt R., Page L., Wessely S. Public perceptions, anxiety, and behaviour change in relation to the swine flu outbreak: cross sectional telephone survey. BMJ. 2009;339(7713):156. doi: 10.1136/bmj.b2651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Siegrist Michael, Timothy C., Earle H.G. Test of a trust and confidence Model in the applied context of electromagnetic field (EMF) risks. Risk Anal. 2003;(23):705–716. doi: 10.1111/1539-6924.00349. [DOI] [PubMed] [Google Scholar]
- 52.Vaughan E., Tinker T. Effective health risk communication about pandemic influenza for vulnerable populations. Am J Publ Health. 2009;99(Suppl. 2) doi: 10.2105/AJPH.2009.162537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rooij B Van, Bruijn AL De, Folmer C.R., Kooistra E., Kuiper M.E., Brownlee M., et al. Compliance with COVID-19 mitigation measures in the United States. PsyArXiv Prepr. 2020:1–40. [Google Scholar]
- 54.Instituto Nacional de Estatística . 2012. Censos 2011. Resultados definitivos - Portugal. [Google Scholar]
- 55.Koh S.W.C., Tan H.M., Lee W.H., Mathews J., Young D. COVID-19 vaccine booster hesitancy among healthcare workers: a retrospective observational study in Singapore. Vaccines. 2022;10(464):1–12. doi: 10.3390/vaccines10030464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lounis M., Bencherit D., Rais M.A., Riad A. COVID-19 vaccine booster hesitancy (VBH) and its drivers in Algeria: national cross-sectional survey-based study. Vaccines. 2022;10(621):1–14. doi: 10.3390/vaccines10040621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yoshida M., Kobashi Y., Kawamura T., Shimazu Y., Nishikawa Y., Omata F., et al. Factors associated with COVID-19 vaccine booster hesitancy: a retrospective cohort study, Fukushima Vaccination Community Survey. Vaccines. 2022;10(4):515. doi: 10.3390/vaccines10040515. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.