Abstract
Objective
Deaths by suicide correlate both spatially and temporally, leading to suicide clusters. This study aimed to estimate racial patterns in suicide clusters since 2000.
Method
Data from the US National Vital Statistics System included all ICD-10 coded suicide cases from 2000–2019 among American Indian/Alaska Native (AI/AN), Asian/Pacific Islander (A/PI), Black, or White youth and young adults, ages 5–34. We estimated age, period, and cohort (APC) trends and identified spatiotemporal clusters using the SaTScan space-time statistic, which identified lower- and higher-than-expected suicide rates (cold and hot clusters) in a prespecified area (150 km) and time interval (15 months). We also calculated the average proportion of deaths by suicide contained in clusters, to quantify the relative importance of spatiotemporal patterning as a driver of overall suicide rates.
Results
From 2010–2019, suicide rates increased from between 37% among AI/AN (95% CI: 1.22, 1.55) to 81% among A/PI (95% CI: 1.65, 2.01) groups. Suicide clusters accounted for 0.8–10.3% of all suicide deaths, across race groups. Since 2000, the likelihood of detecting cluster increased over time with considerable differences in the number of clusters in each racial group (4 among AI/AN to 72 among White youth). Among Black youth and young adults, 27 total clusters were identified, and hot clusters were concentrated in Southeastern and mid-Atlantic counties.
Conclusion
Suicide rates and clusters in youth and young adults have increased in the past two decades, requiring attention from policy makers, clinicians, and caretakers. Racially distinct patterns highlight opportunities to tailor individual- and population-level prevention efforts to prevent suicide deaths in emerging high-risk groups.
Keywords: racial health disparities, child and adolescent health, suicide clusters, age-period-cohort analysis, spatiotemporal analysis
Introduction
Suicide in the United States has been increasing throughout the 21st Century.1 From 1999–2017 suicide deaths increased in 44 of 50 US states, with 25 states reporting increases of >30%.2 Among ages 10–24, suicide rates increased by 57.4% from 2007–2018.3 Individual deaths by suicide correlate both spatially and temporally, leading to suicide clusters.4 These clusters represent an estimated 5–10% of all suicide deaths and are especially prevalent among adolescents and young adults.5 Along with overall rates, the number of suicide clusters has increased since 1999.6
Trends in suicide can be decomposed as a combination of age, period, and cohort effects, as each arises due to distinct causes. Cohort effects capture shared and potentially unique exposures of individuals born within a given historical context. Age effects capture biological and social processes that underlie development, and period effects capture external factors that impact subjects within a given temporal period across ages and cohorts.7 Recent evidence suggests that age patterns in suicide rates differ by racial status. Between 2001–2015, the suicide rate was approximately 42% lower among Black youths (1.26 per 100 000) than among white youths (2.16 per 100 000), ages 5–17. However, specifically among ages 5–12, suicide rates for Black children were roughly 2 times higher than white children. Patterns were reversed for ages 13–17.8 It is not known whether these trends signal changes in cohort trends, however. Also, evidence of disparities in suicide rates among the youngest children combined with the racialized structure of social and physical spaces in the US9 suggest that there may be concurrent race-specific trends in suicide clusters. However, to date no research has directly examined differences in spatiotemporal trends in suicide clusters by racial status.
Suicide clusters emerge through both social (i.e., person-to-person) transmission and shared contextual exposures. Social transmission may be driven by assortive mating, homophily,10 and exposure to inappropriate or graphic exposure to actual and fictionalized suicide information, especially increased media reporting, often in the wake of a high-profile suicide.11 Shared contextual exposures include landscape and climate, local economic conditions,12 and the availability and acceptability of lethal means such as firearms.13 Systematic differences in both the type and the effect of spatiotemporal exposures may be related to racial patterning in suicide trends. For example, Non-Hispanic Black Americans are more likely to be affected by declining economic and labor market conditions than their White counterparts,14 including in the context of the Covid-19 pandemic. Additionally, increases in so-called ‘hot spot’ and ‘quality of life’ policing strategies disproportionately target people and communities of color.1 The resulting encounters with police and increased police presence increases stress and mental health risk for minoritized residents.16 Further, exposure to racist images or instances of violence toward people of color have substantially increased through both traditional and digital/social media, even among children below the minimum age to create a social media account.17 Documenting where and when suicide clusters have been increasing, by race, might shed light on these mechanisms of suicide transmission.
Despite consistent evidence of increased prevalence and spatial patterning, few studies have estimated trends in suicide clusters in recent decades.18 Prior studies of spatial patterns have considered only a subset of states, which limits the overall generalizability to the US population, and there has been no consideration of racial heterogeneity. Long-term temporal investigations are similarly rare. A recent meta-analysis of global studies of temporal patterns in deaths by suicide found that of 50 total studies, only four considered trends longer than one year.18 An additional eight studies utilized age, period, and cohort models. Of these, one study analyzed trends in the United States, finding increasing trends among cohorts born after 1945,19 though trends among youth below age 15 were not investigated.
The current study describes racial differences in the distribution of suicide deaths among children, adolescents, and young adults (age range 5–34) in all United States counties from 2000–2019. Trends in suicide rates were estimated as age-period-cohort (APC) effects, and trends in suicide clusters were estimated using spatiotemporal cluster analysis. We also estimated the proportion of suicide deaths contained within clusters, to understand the magnitude of suicide clusters in the context of overall suicide rates.
Method
Data source and sample population
Death certificate information was retrieved from the US National Vital Statistics System for the periods 2000 to 2019. Death certificates filed and coded with the State Vital Registration Office were further processed by the National Center for Health Statistics to include International Classification of Disease, Tenth revision (ICD-10) causes of death. Suicide deaths were classified based on ICD-10 underlying cause of death codes X60-X84, Y87.0, and U03.20 Underlying cause(s) of death was determined by a coroner, medical examiner, or physician, while racial status (American Indian/Alaskan Native (AI/AN), Asian/Pacific Islander (A/PI), Black, or White) and age of death were recorded by the next of kin. Suicide deaths were aggregated by county of residence and month for cluster analyses. County-level population estimates by age and race were obtained from the National Center for Health Statistics and used to calculate unadjusted mortality rates and expected relative risks.
Statistical Analyses
Two complementary analyses were implemented. First, APC models estimated temporal trends over the study period. In order to follow birth cohorts over time, deaths were restricted to ages 5 to 15 in 2000 and followed up to a maximum age of 34 in 2019. Second, a cluster analysis of spatiotemporal trends in suicide deaths estimated the prevalence and location of suicide clusters among ages 5 to 25, the narrowest age range among youth with sufficient data to yield reliable model estimates. All analyses were implemented for the total sample and stratified by racial status.
Age-period-cohort analysis
Descriptive age, period, and cohort trends in suicide mortality rates were visualized with color-graduated hexagonal grids.21 Each hexagon within the grid represents the suicide rate for a unique age, period, and cohort, providing a clear and consolidated view of trends across each APC component.
We estimated age, period, and cohort effects in suicide rates using generalized linear models based on previously published guidance22 using methods to achieve distinct identifiable parameters. Models estimate a drift parameter, which represents the overall linear trend in rates as the sum of linear effects over time by period and cohort. Cohort and period effects were estimated as rate ratios, based on deviations of the drift parameter from the reference period (i.e., 2010) and cohort (i.e., 2000). Knots were assigned based on the quantiles of events in the overall model and were held constant across race-stratified models. Model fit was iteratively assessed as changes in deviance comparing nested models starting with age, sequentially adding period and cohort parameters. APC models were implemented in R version 4.0.3 using the ‘Epi’23 package.
Spatiotemporal cluster analysis
The aims of the spatiotemporal cluster analysis were two-fold. First, we calculated the proportion of all deaths by suicide that were included in a cluster, to quantify the relative magnitude of clusters in the context of total suicide rates by race. Second, we describe the spatiotemporal distribution of suicide clusters across racial groups.
Spatiotemporal clusters were identified using a space-time statistic, implemented in SaTScan.24 The space-time scan statistic is comprised of a cylindrical window with a base centered on a map grid point (e.g., county centroid), with a height corresponding to the cluster time interval. The cylindrical window considered all possible geographic areas and time intervals, up to a prespecified maximum size, in order to identify spatiotemporal clusters. The likelihood of each possible cluster was assessed using Poisson models and Monte Carlo simulations. A likelihood ratio test was used to compare the suicide risk within vs. outside the cylinder, estimated as a risk ratio. A cluster was confirmed when suicide risk ratios within a given cylinder differed at an alpha=0.01 error level. The magnitude of the risk ratio indicates the extent that the suicide risk differs within vs. outside of the cluster. ‘Hot’ clusters indicate higher-than-expected risks, and ‘cold’ clusters indicate lower-than-expected risks. For example, a cluster RR=2.0 indicates that, during that 15-month interval, suicides were twice as likely within that area than outside the cluster; a RR=0.5 suggests that suicides were half as likely within vs. outside a given cluster at that time. A separate scan was run in each racial group, to identify racially distinct patterns in suicide clusters.
In previous research to identify suicide clusters, the maximum size of clusters has varied widely, spanning temporal periods from days to years and spatial areas from school classrooms to counties.25 We specified the maximum cylinder radius and height parameters to 150 km and 15 months, in order to capture relatively localized clusters at a national scale. Additionally, suicide is a rare event among youth, and these parameters included the minimum sample sizes needed to achieve reliable model estimates. In a sensitivity analysis, we increased the parameters to 250 km and 21 months, to examine how sensitive the clusters were to any one set of specifications.
To calculate the proportions of all suicide deaths captured within a cluster, the denominator included all suicide deaths in the US that occurred throughout the duration of each cluster. Proportions were then averaged across all clusters for each racial group and type of cluster (i.e., hot or cold).
Results
Age-period-cohort analysis
Fit indices indicated that the model including age, period, and cohort parameters provided the best fit to the data (see Table S1, available online). Suicide rates and rate ratios for age, period, and cohort groups are presented in Figures 1 and 2, and in Tables S2 and S3, available online. Age rates were highest among AI/AN and lowest among A/PI groups, peaking at age 19 and age 22 at rates of 21.99 and 8.3 deaths per 100,000, respectively. Racial differences in suicide rates were consistent at all ages except among Black respondents, whose rates were second highest between ages 5–10, and second lowest between ages 11–30. Period rate ratios indicated that suicide rates generally increased over time across age. The greatest increases for all groups occurred between 2010–2019, during which time rate increases ranged from 37% among AI/AN (95% CI: 1.22, 1.55) youth to 81% among A/PI (95% CI: 1.65, 2.01) youth. Compared with the reference (2000), cohort rate ratios were somewhat curvilinear, decreasing until approximately 1994, then increasing thereafter among all groups. Cohort rate ratios were similar across race groups. Overall, trends point to increasing suicide rates, emerging earlier in more recently born cohorts, across all races.
Figure 1.
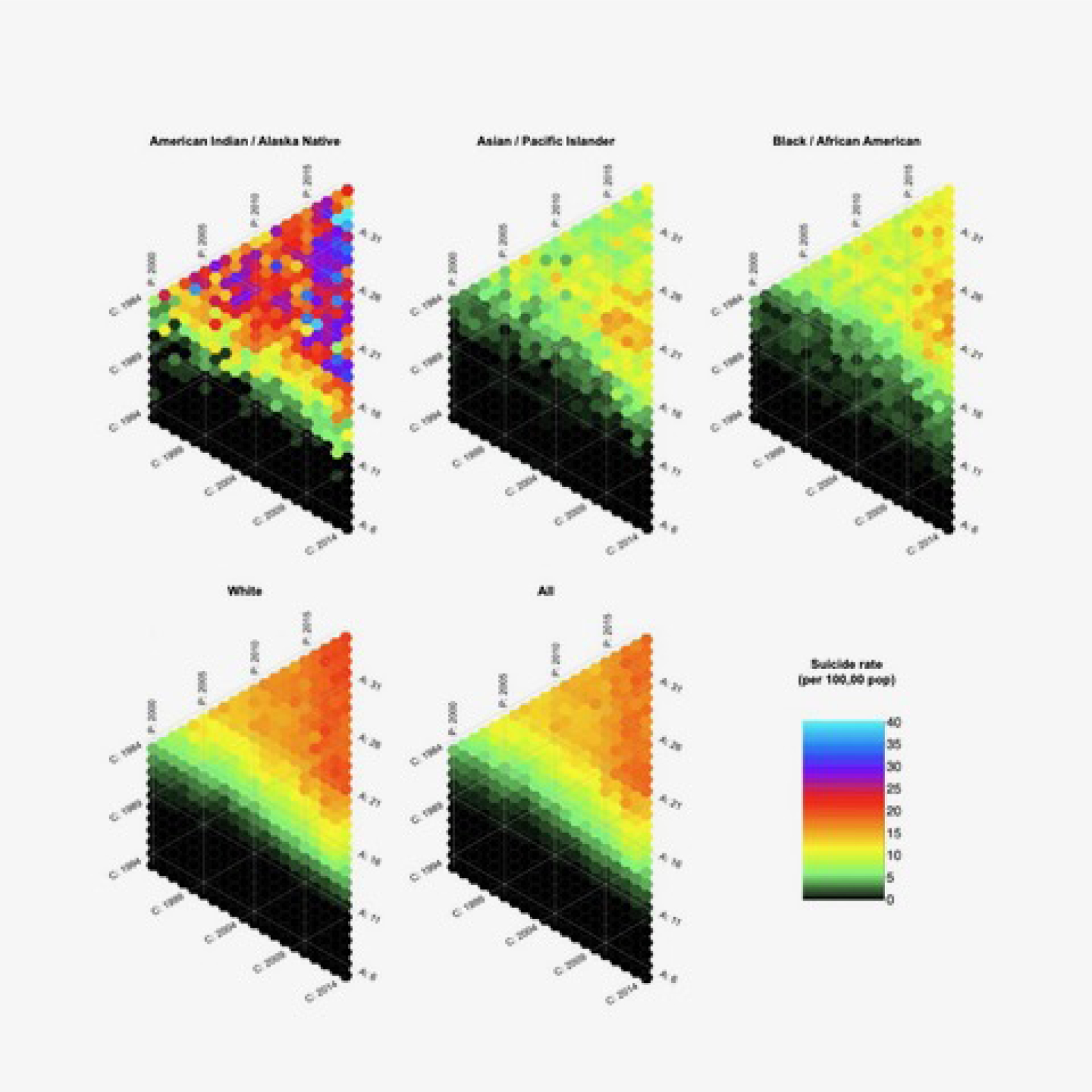
Color-Graduated Hexagonal Grids Representing the Suicide Rate for a Unique Age, Period, and Cohort By Race, Through 2019 Among Ages 5–34
Figure 2.
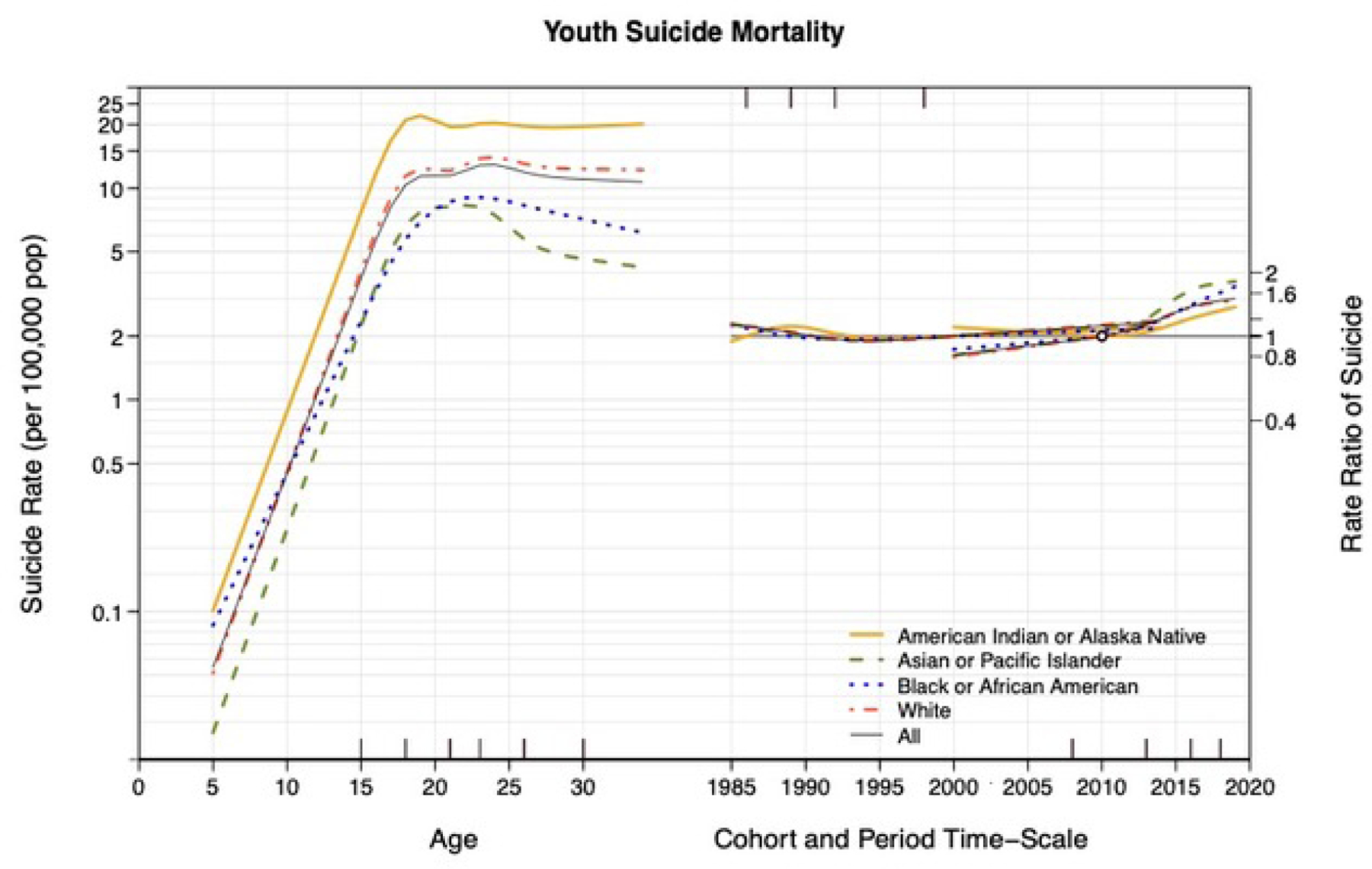
Age-Period-Cohort Estimates of Completed Suicides by Race, Through 2019 Among Ages 5–34
Spatiotemporal cluster analysis
Table 1 presents the percentages of all suicide deaths that are included in any spatiotemporal cluster for each racial group. The proportion of all suicide deaths captured within the hot clusters was 10.3% (AI/AN), 2.7% (A/PI), 1.7% (Black), and 0.8% (White), and within cold clusters, the proportions ranged from 1.7% to 8.8%.
Table 1.
Percentages of All Suicides That Are Included in Any Spatiotemporal Cluster, Based on a Maximum Cylinder Radius and Height Parameters of 150 km and 15 Months
| Racial group | Hot clusters (%) | Cold clusters (%) |
|---|---|---|
| All | 0.7 | 1.5 |
| American Indian/Alaskan Native | 10.3 | 8.8 |
| Asian/Pacific Islander | 2.7 | 4.7 |
| Black | 1.7 | 2.2 |
| White | 0.8 | 1.7 |
Note: percentages are calculated as the number of all suicide deaths captured within a cluster, divided by the total number of suicide deaths that occurred throughout the duration of each cluster in the US.
The spatiotemporal cluster model results are presented visually in two figures. Figure 3 presents the clusters temporally, and Figure 4 presents the clusters spatially. Clusters are assigned the same unique number in the two figures to facilitate comparison between them. Higher numbers represent more recent clusters.
Figure 3.
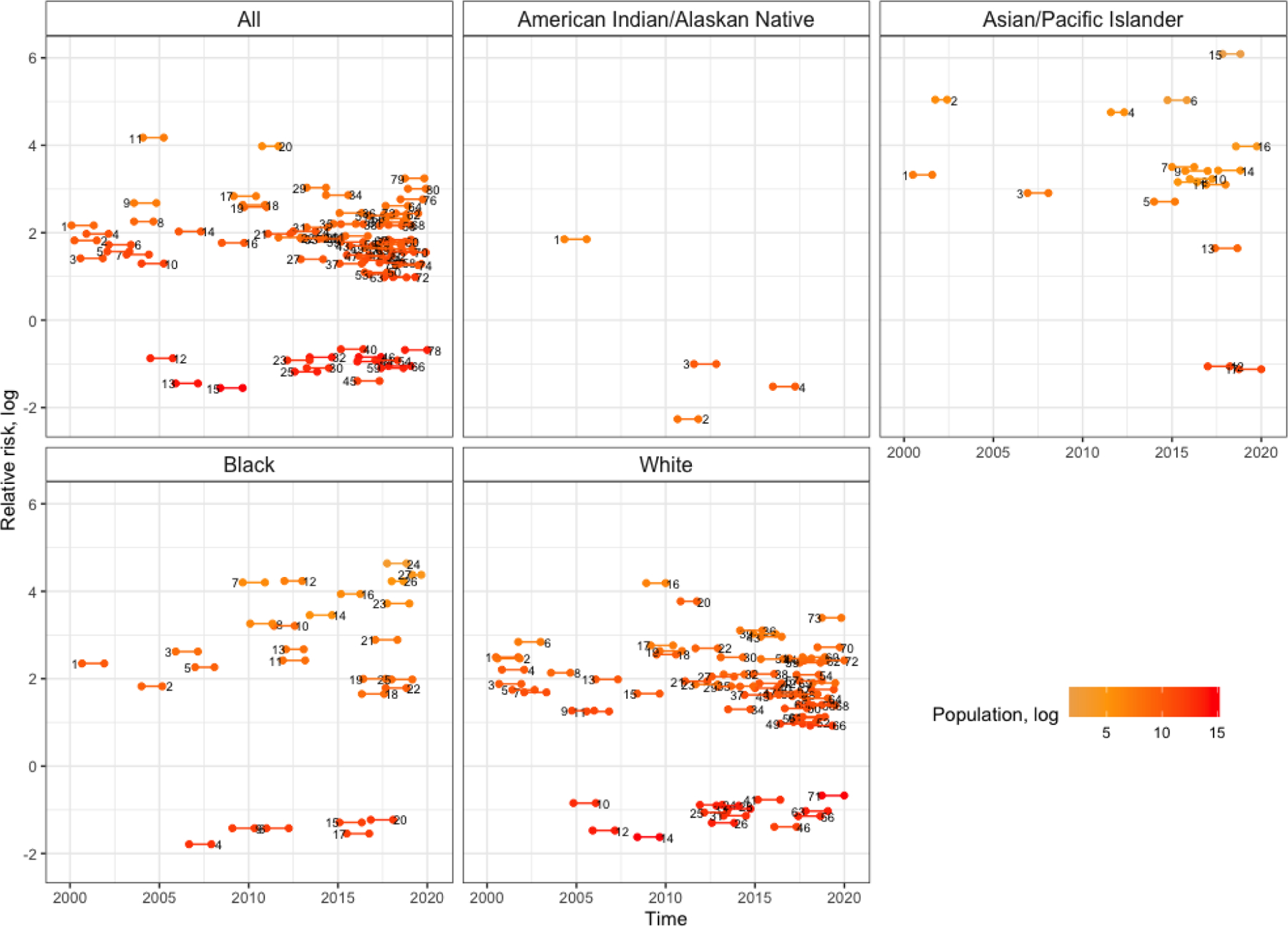
Temporal Clusters in Suicide Rates by Race, From 2000–2019 Among Ages 5–25 Note: Spatiotemporal parameters: ≤ 150km and ≤ 15 months
Figure 4.
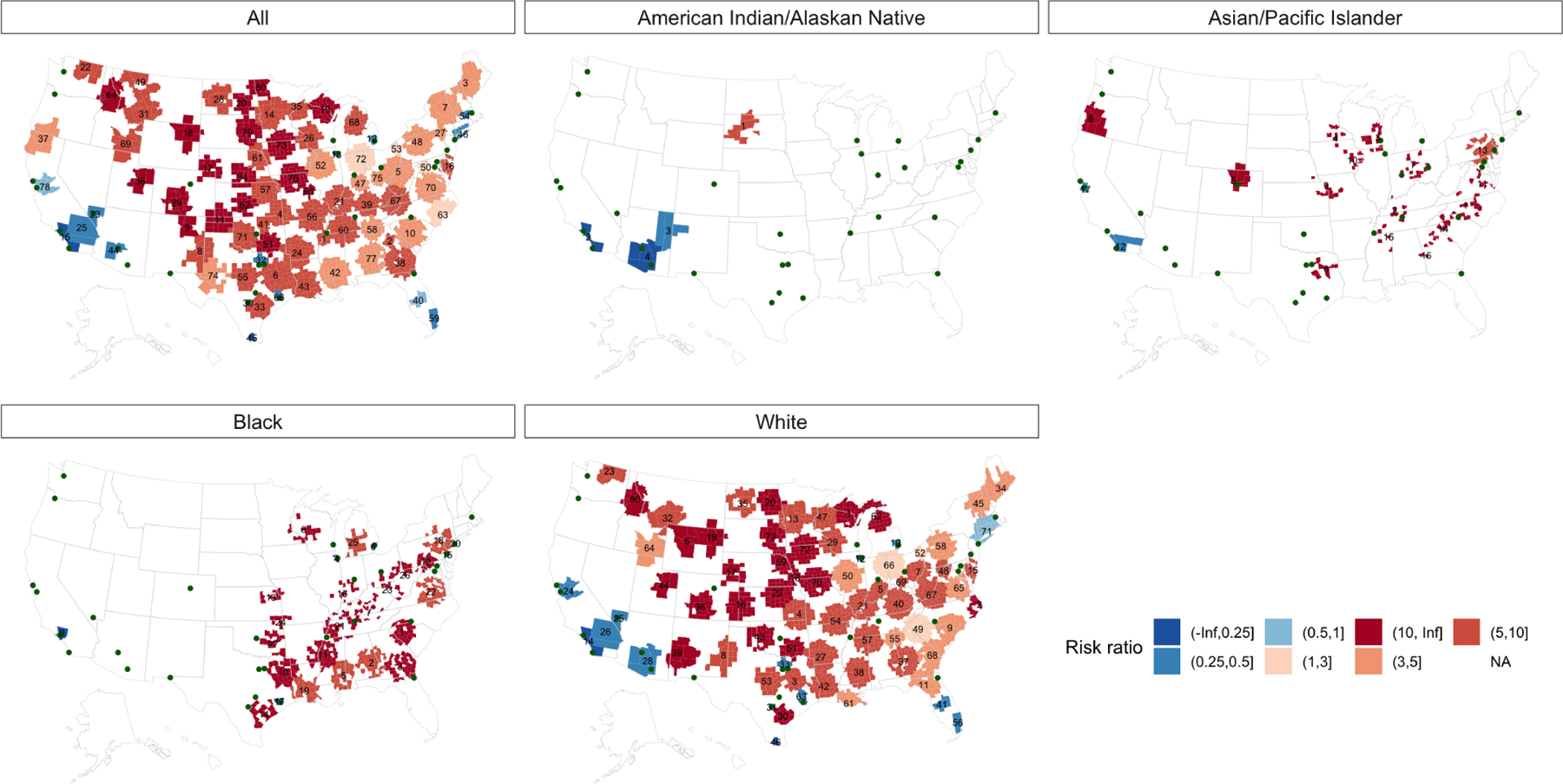
Spatial Clusters in Suicide Rates by Race, From 2000–2019 Among Ages 5–25 Note: Spatiotemporal parameters: ≤ 150km And ≤ 15 months
In the temporal clusters (see Figure 3), each line represents one cluster with the nodes indicating the start and end points. The y-axis refers to the risk ratio magnitude, where positive numbers are hot clusters and negative numbers are cold clusters. For all age groups, suicide clusters were found to be increasingly likely throughout the study period. Overall, 80 temporal clusters were identified, though the number of clusters varied substantially between groups, ranging from 4 among AI/AN individuals to 72 among White individuals, respectively. Among Black individuals, 27 clusters were identified, and the magnitude of the cluster risk ratios increased over time, indicating that suicide risk within clusters were increasingly greater than those outside of them. The majority were ‘hot’ clusters (i.e., greater than expected suicide rates), though ‘cold’ clusters (i.e., lower than expected suicide rates), also increased over time.
In the spatial clusters (see Figure 4), colors indicate the magnitude of cluster risk ratios, where red shades are hot clusters and blue are cold. In the total sample, hot clusters were identified in nearly every region of the US; clusters with the greatest magnitude (i.e., the largest rates within vs. outside of the cluster) were found in the Great Plains, the Upper Midwest, and the Southwest regions. Cold clusters were identified in urban areas, including San Francisco, Los Angeles, Phoenix, Dallas, Houston, Chicago, Detroit, Miami, New York, and Boston. The overall pattern corresponded closely with the spatial clustering among White individuals given that Whites comprised the majority of suicide deaths, while patterns were more spatially limited for other racial groups.
Among Black individuals, hot clusters were identified throughout Southeastern and Mid-Atlantic states, while cold clusters were found in urban areas, including Los Angeles, Houston, Chicago, Detroit, Philadelphia, and New York City. Among AI/AN groups, one hot cluster was identified in South Dakota, while cold clusters were identified in Los Angeles, Phoenix/Tucson, and Northeastern Arizona. Among A/PI groups, 14 hot clusters were identified throughout the country, while two cold clusters were identified in San Diego and San Francisco metro areas.
Sensitivity analysis
The results of the sensitivity analysis, with maximum cluster radius of 250 km and duration of 21 months is presented in Figures S1 and S2, available online, and the percent of all suicide deaths that were included in any spatiotemporal cluster for each group is presented in Table S4, available online. As expected, clusters were larger and more likely, given the increased cylinder sizes, though models identified similar spatiotemporal patterning in general. The percent of all suicide deaths included in any cluster was generally consistent with those identified when using the smaller cylinder sizes.
Discussion
This study aimed to describe racial differences in the distribution of suicide death among children, adolescents, and young adults in the United States over nearly 20 years, using both APC and spatiotemporal cluster analyses. We highlight five main findings. First, stratified age rates in the APC analysis confirm the high risk of suicide among Black youth at the youngest ages, compared with A/PI and White peers. Second, APC models identified significant increases in suicide rates across cohort and period, though no substantial trend differences were identified across race groups. Third, the percentage of all suicide deaths included in a spatiotemporal cluster varied substantially across racial groups. Fourth, the results of the spatiotemporal analysis also indicate that suicide clusters have become increasingly likely over time, and distinct urban/rural patterns in cold/hot suicide clusters were similar across race groups. Fifth, racially distinct geographic patterns were also identified.
Following a decade of decline, age, period, and cohort trends in suicide rates among American youth indicate steadily increasing risk in the 21st Century.26 Our study identified both similarities and differences in APC trends across racial groups. By age, rates increased substantially during adolescence then peaked between ages 20–25. The inter-group differences in trends were consistent, except in Black youth, who shifted from the second-highest childhood rates (ages 5–10), lower than only AI/AN youth, to the second lowest from ages 11–34, higher than only A/PI youth. This age pattern mirrors recent evidence of a similar age-related racial disparity,8 which is counter to the typically cited pattern of low suicide rates in Black youth at all ages. Increasing age trends reflect interacting biological, behavioral, and social changes as individuals transition out of childhood, as well as substance use and mental health problems.27 Developmentally, the understanding of the nature and meaning of death and suicide changes profoundly throughout this period, as children become cognitively able to grasp the finality of death and many begin to experience death indirectly, through the loss of grandparents, pets, and others. Children as young as age 5 have been shown to understand death and suicide and distinguish death from sleep.28 At the same time, episodic memory deficits,29 impulsivity, and risk-taking,30 may increase the risk of transitioning from suicidal thoughts to behavior. A developmental perspective may prove useful for understanding these emerging age trends and racial differences by highlighting whether experiences with death and self-harm are becoming more prevalent at younger ages, and whether experiences differ by race. In addition, parents, teachers, and other caretakers must take suicidal thoughts and behaviors seriously in young children. Future research should seek to further validate suicide screening tools in young children,29 explore possible cross-racial differences in risk, and evaluate the potential for differential misclassification of suicide risk on the basis of racial status.
Race by age patterns may be specifically influenced by differences in social exposures. For example, exposure to racialized stressors may be a salient risk factor for Black children, who at later ages are socialized to employ protective coping strategies31 and strengthen social support networks and racial identities which may buffer the risk. These processes may explain similar patterns of lower risk of depression and anxiety disorders among Black vs. White individuals.32 The impact of racial socialization remains equivocal for young children and may differ between racial groups. For example, a recent meta-analysis found that the impact of racial socialization was beneficial to the self-perceptions of African American youth; however, the impact appeared negative among Asian-Americans.33 Strengthening racial and cultural identity and pride may be important clinical components of suicide prevention, though any intervention should be informed by the unique social and historical experiences of each racial/ethnic group.32 In general, more longitudinal research is needed to understand how interactions between the social environment and developmental processes influence racial patterns in youth suicide risk, in order to tailor primary prevention strategies to the appropriate cultural and racial context.34
We also identified small but statistically significant cohort effects, suggesting that suicide rates are increasing in more recently born groups. Cohort effects reflect the shared exposures of a group born during the same historical period. Increasing income inequality and diminished economic opportunities from adolescence into early adulthood35 may partially contribute to overall suicide trends. There were no clear differences in cohort effects across races, suggesting that age-specific patterns may not be changing over time, and suicide rates are increasing for all racial groups in similar ways.
Finally, APC models identified period effects indicating that suicide rates have increased by an average of about 50% since 2000, across all ages in the sample. In addition, suicide among children under age 15 increased during the last 10 years for all racial groups (see Figure 1). Period effects may be driven by policy or other widespread changes that occur at a specific time point. The increasing presence of social media has also been investigated as a cause of increasing suicide trends. Traditional media coverage of suicide deaths of community members and celebrities has been shown to increase suicide deaths;5,11 however, to date, evidence regarding the use of social media and suicide risk overall is equivocal.36 There are many real and artifactual (e.g., reverse causation) ways that social media may influence suicidal behaviors, and more research is needed to understand the complexities around how social media might affect the mental health and suicide risk of youth growing up today, and whether online content guidelines, akin to those recommended for traditional media,37 may be beneficial in preventing the emergence of suicide clusters.
Spatiotemporal clusters accounted for 0.8% to 10.3% of all concurrent suicide deaths. While within the range of recent estimates,5 variation across racial groups was substantial. The highest proportion was found among AI/AN individuals, which partially reflects the spatial concentration of these populations in tribal communities and reservations. These results may indicate the clinical utility of identifying high-risk individuals based on their location within a cluster. While the low percentages among A/PI, Black, and White racial groups suggest that the vast majority of suicide deaths do not occur within a cluster, knowing where and when suicide deaths may be more likely to occur could provide a useful supplement to existing individual-level risk prediction tools. More generally, the use of group-level measures in clinical risk assessments is gaining increasing attention, as the appreciation for the social and spatial determinants of health become more widespread.38
Consistent with the APC analysis, the results of the spatiotemporal analysis identified an increasing likelihood of suicide clusters in space and time. These analyses contribute valuable information to the surveillance of suicide deaths beyond population and state-level rates and highlight the importance of addressing area-level factors in order to reverse suicide trends. Important distinctions emerged between urban and non-urban counties. Cold suicide clusters were identified in many of the largest cities across the US, highlighting urban centers as areas with lower-than-expected suicide rates. In contrast, hot suicide clusters representing areas with higher-than-expected suicide rates were identified in non-urban areas. Additionally, temporal trends suggested that both hot and cold clusters are becoming more likely over time. Together, these findings extend prior research showing that adolescent suicide risk decreases with urbanicity in the US, and that urban/non-urban differences appear to be increasing over time.
There are many explanations for these patterns. Health care access,39 social support,40 means restrictions,41 and economic growth and opportunity are all greater in urban areas and likely contribute to suicide rates. The prevention of suicide clusters in rural areas requires interventions at both the individual and community levels, for example identifying and supporting those at high-risk while also taking steps to alleviate poverty, increase economic opportunity, foster social connectedness, and reduce access to firearms.
Additionally, the occurrence of a suicide may be more visible in rural areas, potentially increasing the occurrence of imitation suicide deaths. Deaths by suicide may be amplified by traditional or social media increasing the spatiotemporal reach and likelihood that a cluster may emerge. Whether suicide clusters emerge as a result of imitation or are primarily driven by geographic clustering of structural predictors of suicide is a longstanding debate in suicide cluster research, and both are likely important pathways.42 Future research is needed to directly interrogate these potential geospatial mechanisms.
When stratified by racial status, three localized patterns emerged. First, Black youth suicide clusters were most likely to emerge throughout the rural Eastern US, spanning from East Texas to Georgia, through Appalachia, and as far north as Wisconsin, Michigan, and New York. To our knowledge, this is the first study to identify this distinct racial pattern. The distribution is likely due in part to the cumulative burden faced by minority groups living in the rural US, which is reflected in a consistent racial patterning of risk factors for poor health, including greater stress and inflammation,43 lower socioeconomic status, and lower health care availability.44 The health impact of this burden is seen across the lifecourse, as similar geographic patterning is found in the rates of cardiovascular disease, stroke,45 HIV,46 and most recently, the prevalence of COVID cases, hospitalizations, and deaths.47 A second pattern that emerged was the specificity of suicide clusters in non-coastal Western states. Previous research has highlighted this region as one with disproportionately high suicide rates and prevalence of suicide clusters.6 While our models identified several clusters in non-coastal Western states, nearly all of them were present among White youth only. This finding suggests that the discussion of geographic suicide risk factors (e.g., altitude) should be discussed with attention to racial heterogeneity. A third localized finding was distinct among AI/AN youth. Spatiotemporal models identified a multi-county cold cluster in Northeastern Arizona, which comprises Apache tribal territories. Of all groups, this was the only cold cluster that was not centered around an urban area. Historically, Native American communities have experienced extremely high suicide rates, up to 10 times higher than other groups in some places.48 Our analysis confirmed this; across all ages, suicide rates were consistently highest among AI/AN youth. This particular protective cluster may be a direct result of a community surveillance system and suicide prevention program, developed by researchers and Tribal authorities to address the specific risk factors for suicide in their communities. From 2001–2012, the ‘Celebrating Life Surveillance System’ decreased the suicide rate among ages 15–24 by 23%.49 Programs like this are proof that interventions can significantly reduce suicide risk, even where it is highest, provided they are tailored to the relevant racial, geographic, and social context of the target communities. This need has become even more urgent given the widespread social, economic, and physical health consequences of the COVID-19 pandemic and the implications for adolescent mental health and suicide risk.
This analysis should be interpreted in light of several limitations. First, the SaTScan algorithm is data-driven and will find the outliers in any given distribution. Nonetheless, varying the temporal and spatial parameters in a sensitivity analysis did give us confidence that the general patterns we report reflect meaningful patterns and are not solely an artifact of any one set of parameters in the statistical model. Findings should be replicated using more theory driven methods which allow for greater control of a priori cluster identification settings. Second, suicide deaths may be misclassified on death certificates, differentially by racial identity, such that racial minority groups are more likely to be undercounted.50 In effect, suicide rates among non-White racial groups may be higher than observed, though it is unknown whether this misclassification has changed over time and would thus influence APC trends. Also, it is unlikely to bias the spatiotemporal cluster analyses, assuming that all race-specific suicide deaths are similarly misclassified, whether they occur within a cluster or not. Third, small sample sizes prohibited us from considering group heterogeneity in more detail, especially differences by Hispanic ethnicity and among children, adolescents, and young adults separately. Spatiotemporal patterns between these groups are likely important and should be considered in future research. Finally, this descriptive study is an initial step toward understanding the patterns of suicide clusters in a way that may help to identify emerging high-risk groups based on racialized identity and geography. Accordingly, inferential claims regarding the causes of these patterns cannot be made without further analysis. More research is needed to understand the mechanisms driving racial differences in suicide clusters, with the goal of implementing effective and tailored suicide prevention and postvention strategies.
Emerging youth suicide clusters in the US require urgent attention from those engaged in suicide prevention, including public health professionals, clinicians, and parents. Spatiotemporal methods represent important epidemiological tools for suicide surveillance and prevention and may provide a useful supplement to existing clinical risk assessments. The current study provides additional evidence of high-risk groups and geographic areas that can inform and focus interventions to prevent suicide deaths and injuries from attempted suicide. Racial differences in spatiotemporal patterns of suicide and suicide clusters suggest that interventions, drawing on a combination of evidence-based strategies, should be tailored with attention to population heterogeneity in order to effectively reduce individual and population suicide risk.
Supplementary Material
Acknowledgments
Funding was provided by the National Institute of Mental Health (5R01MH121410, Keyes/Shaman).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
This article is part of a special series devoted to addressing bias, bigotry, racism, and mental health disparities through research, practice, and policy. The series is edited by Assistant Editor Eraka Bath, MD, Deputy Editor Wanjikũ F.M. Njoroge, Associate Editor Robert R. Althoff, MD, PhD, and Editor-in-Chief Douglas K. Novins, MD.
Disclosure: Drs. Platt, Pamplin II, Olfson, Gould, Martínez-Alés, Shaman, Keyes, Mss. Gimbrone and Rutherford, and Mr. Kandula have reported no biomedical financial interests or potential conflicts of interest.
Contributor Information
Jonathan M. Platt, University of Iowa College of Public Health, Iowa City.
John R. Pamplin, II, Center for Urban Science and Progress, New York University, New York and the Grossman School of Medicine, New York University, New York.
Catherine Gimbrone, Mailman School of Public Health, Columbia University, New York..
Caroline Rutherford, Mailman School of Public Health, Columbia University, New York..
Sasikiran Kandula, Mailman School of Public Health, Columbia University, New York..
Mark Olfson, Mailman School of Public Health, Columbia University, New York. Columbia University Irving Medical Center and New York State Psychiatric Institute, New York..
Madelyn S. Gould, Mailman School of Public Health, Columbia University, New York. Columbia University Irving Medical Center and New York State Psychiatric Institute, New York..
Gonzalo Martínez-Alés, Mailman School of Public Health, Columbia University, New York..
Jeffrey Shaman, Mailman School of Public Health, Columbia University, New York..
Katherine Keyes, Mailman School of Public Health, Columbia University, New York..
References
- 1.Curtin SC, Warner M, Hedegaard H. Increases in suicide in the United States, 19992014. NCHS Data Brief Published online 2016. [PubMed] [Google Scholar]
- 2.Stone DM, Simon TR, Fowler KA, et al. Vital Signs: Trends in State Suicide Rates — United States, 1999–2016 and Circumstances Contributing to Suicide — 27 States, 2015. Morbidity and Mortality Weekly Report 2018;67(22):617–624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Curtin SC. State suicide rates among adolescents and young adults aged 10–24: United States, 2000–2018 Published online 2020. [PubMed] [Google Scholar]
- 4.Gould MS, Wallenstein S, Davidson L. Suicide clusters: A critical review. Suicide and Life - Threatening Behavior 1989;19(1):17–29. [DOI] [PubMed] [Google Scholar]
- 5.Hawton K, Hill NT, Gould M, John A, Lascelles K, Robinson J. Clustering of suicides in children and adolescents. The Lancet Child & Adolescent Health 2020;4(1):58–67. [DOI] [PubMed] [Google Scholar]
- 6.Sy KTL, Shaman J, Kandula S, Pei S, Gould M, Keyes KM. Spatiotemporal clustering of suicides in the US from 1999 to 2016: a spatial epidemiological approach. Soc Psychiatry Psychiatr Epidemiol 2019;54(12):1471–1482. doi: 10.1007/s00127-019-01736-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yang Y Age/period/cohort distinctions. Encyclopedia of health and aging Published online 2007:20–22. [Google Scholar]
- 8.Bridge JA, Horowitz LM, Fontanella CA, et al. Age-related racial disparity in suicide rates among US youths from 2001 through 2015. JAMA pediatrics 2018;172(7):697–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams DR, Collins C. Racial residential segregation: a fundamental cause of racial disparities in health. Public health reports Published online 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng Q, Li H, Silenzio V, Caine ED. Suicide Contagion: A Systematic Review of Definitions and Research Utility. PLOS ONE 2014;9(9):e108724. doi: 10.1371/journal.pone.0108724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Niederkrotenthaler T, Fu KW, Yip PSF, et al. Changes in suicide rates following media reports on celebrity suicide: A meta-analysis. Journal of Epidemiology and Community Health Published online 2012. doi: 10.1136/jech-2011-200707 [DOI] [PubMed] [Google Scholar]
- 12.Lundin A, Hemmingsson T. Unemployment and suicide. The Lancet Published online 2009. doi: 10.1016/S0140-6736(09)61202-2 [DOI] [PubMed] [Google Scholar]
- 13.Kalesan B, Villarreal MD, Keyes KM, Galea S. Gun ownership and social gun culture. Injury Prevention 2016;22(3). doi: 10.1136/injuryprev-2015-041586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoynes H, Miller DL, Schaller J. Who suffers during recessions? Journal of Economic perspectives 2012;26(3):27–48. [Google Scholar]
- 15.Shapiro A Reform predictive policing. Nature News 2017;541(7638):458. [DOI] [PubMed] [Google Scholar]
- 16.Geller A, Fagan J, Tyler T, Link BG. Aggressive policing and the mental health of young urban men. American journal of public health 2014;104(12):2321–2327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tynes B, Hiss S, Ryan A, Rose C. Discrimination in school vs. online contexts, mental health and motivation among diverse adolescents in the US. The social psychology of the classroom international handbook Published online 2015:112–121. [Google Scholar]
- 18.Galvão PVM, Silva HRS e, Silva CMFP da. Temporal distribution of suicide mortality: A systematic review. Journal of Affective Disorders 2018;228:132–142. doi: 10.1016/j.jad.2017.12.008 [DOI] [PubMed] [Google Scholar]
- 19.Phillips J A changing epidemiology of suicide? The influence of birth cohorts on suicide rates in the United States. Social Science & Medicine 2014;114:151–160. doi: 10.1016/j.socscimed.2014.05.038 [DOI] [PubMed] [Google Scholar]
- 20.Hedegaard H, Curtin SC, Warner M. Increase in suicide mortality in the United States, 1999–2018 Published online 2020. Accessed January 4, 2021. https://www.cdc.gov/nchs/products/databriefs/db362.htm
- 21.Jalal H, Burke DS. Hexamaps for Age–Period–Cohort Data Visualization and Implementation in R. Epidemiology 2020;31(6):e47–e49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clayton D, Schifflers E. Models for temporal variation in cancer rates. II: age–period–cohort models. Statistics in medicine 1987;6(4):469–481. [DOI] [PubMed] [Google Scholar]
- 23.Carstensen B, Plummer M, Laara E, Hills M, Carstensen MB. Package ‘Epi.’ A package for statistical analysis in epidemiology Published on CRAN Published online 2013. [Google Scholar]
- 24.Kulldorff M Information Management Services, Inc. SaTScan v9. 6: Software for the spatial and space-time scan statistics 2018. Published online 2019. [Google Scholar]
- 25.Niedzwiedz C, Haw C, Hawton K, Platt S. The definition and epidemiology of clusters of suicidal behavior: a systematic review. Suicide and Life-Threatening Behavior 2014;44(5):569–581. [DOI] [PubMed] [Google Scholar]
- 26.Martínez-Alés G, Pamplin JR, Rutherford C, et al. Age, period, and cohort effects on suicide death in the United States from 1999 to 2018: moderation by sex, race, and firearm involvement. Molecular Psychiatry Published online April 7, 2021:1–9. doi: 10.1038/s41380-021-01078-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cash SJ, Bridge JA. Epidemiology of Youth Suicide and Suicidal Behavior. Curr Opin Pediatr 2009;21(5):613–619. doi: 10.1097/MOP.0b013e32833063e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Normand CL, Mishara BL. The development of the concept of suicide in children. OMEGA-Journal of Death and Dying 1992;25(3):183–203. [Google Scholar]
- 29.Huber RS, Sheth C, Renshaw PF, Yurgelun-Todd DA, McGlade EC. Suicide ideation and neurocognition among 9-and 10-year old children in the Adolescent Brain Cognitive Development (ABCD) study. Archives of suicide research Published online 2020:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McGirr A, Renaud J, Bureau A, Seguin M, Lesage A, Turecki G. Impulsive-aggressive behaviours and completed suicide across the life cycle: a predisposition for younger age of suicide. Psychological medicine 2008;38(3):407. [DOI] [PubMed] [Google Scholar]
- 31.Erausquin JT, McCoy TP, Bartlett R, Park E. Trajectories of Suicide Ideation and Attempts from Early Adolescence to Mid-Adulthood: Associations with Race/Ethnicity. J Youth Adolescence 2019;48(9):1796–1805. doi: 10.1007/s10964-019-01074-3 [DOI] [PubMed] [Google Scholar]
- 32.Reynolds JE, Gonzales- Backen MA. Ethnic-Racial Socialization and the Mental Health of African Americans: A Critical Review. Journal of Family Theory & Review 2017;9(2):182–200. doi: 10.1111/jftr.12192 [DOI] [Google Scholar]
- 33.Wang MT, Henry DA, Smith LV, Huguley JP, Guo J. Parental ethnic-racial socialization practices and children of color’s psychosocial and behavioral adjustment: A systematic review and meta-analysis. American Psychologist 2020;75(1):1. [DOI] [PubMed] [Google Scholar]
- 34.Joe S, Canetto SS, Romer D. Advancing prevention research on the role of culture in suicide prevention. Suicide and Life-Threatening Behavior 2008;38(3):354–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Padmanathan P, Bould H, Winstone L, Moran P, Gunnell D. Social media use, economic recession and income inequality in relation to trends in youth suicide in high-income countries: a time trends analysis. Journal of affective disorders 2020;275:58–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sedgwick R, Epstein S, Dutta R, Ougrin D. Social media, internet use and suicide attempts in adolescents. Current Opinion in Psychiatry 2019;32(6):534–541. doi: 10.1097/YCO.0000000000000547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pirkis J, Blood RW, Beautrais A, Burgess P, Skehan J. Media guidelines on the reporting of suicide. Crisis 2006;27(2):82–87. [DOI] [PubMed] [Google Scholar]
- 38.Andermann A Screening for social determinants of health in clinical care: moving from the margins to the mainstream. Public Health Reviews 2018;39(1):19. doi: 10.1186/s40985-018-0094-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rost K, Fortney J, Fischer E, Smith J. Use, quality, and outcomes of care for mental health: the rural perspective. Medical Care Research and Review 2002;59(3):231–265. [DOI] [PubMed] [Google Scholar]
- 40.Cantrell C, Valley-Gray S, Cash RE. Suicide in rural areas: risk factors and prevention. Rural mental health: Issues, policies, and best practices Published online 2012:213–228. [Google Scholar]
- 41.Brent DA, Bridge J. Firearms availability and suicide: Evidence, interventions, and future directions. American Behavioral Scientist 2003;46(9):1192–1210. [Google Scholar]
- 42.Baller RD, Richardson KK. Social integration, imitation, and the geographic patterning of suicide. American Sociological Review Published online 2002:873–888. [Google Scholar]
- 43.Geronimus AT, Bound J, Waidmann TA, Hillemeier MM, Burns PB. Excess mortality among blacks and whites in the United States. New England journal of medicine 1996;335(21):1552–1558. [DOI] [PubMed] [Google Scholar]
- 44.Mansfield CJ, Wilson JL, Kobrinski EJ, Mitchell J. Premature mortality in the United States: the roles of geographic area, socioeconomic status, household type, and availability of medical care. American Journal of Public Health 1999;89(6):893–898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Boan Andrea D, Wuwei (Wayne) Feng, Bruce Ovbiagele, et al. Persistent Racial Disparity in Stroke Hospitalization and Economic Impact in Young Adults in the Buckle of Stroke Belt. Stroke 2014;45(7):1932–1938. doi: 10.1161/STROKEAHA.114.004853 [DOI] [PubMed] [Google Scholar]
- 46.Sullivan PS, Woodyatt C, Koski C, et al. A data visualization and dissemination resource to support HIV prevention and care at the local level: analysis and uses of the AIDSVu Public Data Resource. Journal of medical Internet research 2020;22(10):e23173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mahajan UV, Larkins-Pettigrew M. Racial demographics and COVID-19 confirmed cases and deaths: a correlational analysis of 2886 US counties. Journal of Public Health 2020;42(3):445–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dorgan BL. The tragedy of Native American youth suicide. Psychological Services 2010;7(3):213. [Google Scholar]
- 49.Cwik MF, Tingey L, Maschino A, et al. Decreases in Suicide Deaths and Attempts Linked to the White Mountain Apache Suicide Surveillance and Prevention System, 2001–2012. Am J Public Health 2016;106(12):2183–2189. doi: 10.2105/AJPH.2016.303453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Mohler B, Earls F. Trends in adolescent suicide: misclassification bias? American Journal of Public Health 2001;91(1):150. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


