Abstract
Primary hydatid disease of the skeletal muscle without systemic involvement is rare. Since the infection appears on clinical examination to be a soft-tissue tumor. It is important to have a preoperative radiological evaluation, particularly with magnetic resonance imaging (MRI) to avoid biopsy or improper cyst management during surgery. We present a unique case of a primary hydatid cyst manifesting as an expanding soft-tissue mass in a 31-year-old woman's left thigh with magnetic resonance imaging revealed a very suggestive aspect of hydatid cyst in the adductor muscles and shows the interaction between cysts and nearby structures. The cyst was surgically removed, and macroscopic and microscopic histopathological examinations confirmed the diagnosis of muscular hydatidosis.
Keywords: Primary hydatidosis, Intramuscular hydatid cyst, imaging
Introduction
Hydatidosis is an infectious disease that is endemic in Morocco, and it is caused by the cestode Echinococcus. Primary hosts are dogs, wolves and coyotes, while the intermediate hosts are sheep, cattle, and deer. Human transmission occurs through ingestion of infected food or water, or by direct contact with animal hosts. Although the liver and lungs are the most usually affected organs [2]. Soft tissue hydatid disease is unusual even in endemic areas [2] and primary hydatidosis of the skeletal muscle is extremely rare [3], [4], [5]. Since the infection appears on clinical examination to be a soft-tissue tumor, it is important to have a preoperative radiological evaluation, particularly with magnetic resonance imaging (MRI) that shows a various imaging features to avoid biopsy or improper cyst management during surgery [6]. The currently recommended treatment combines chemotherapy and surgical eradication of the lesion [4]. We report clinical and imaging manifestations of primary intramuscular hydatidosis in a 31 year old woman.
Case Report
A 31 year old woman living in a rural area, without significant medical or surgical history, was admitted with an enlarging soft-tissue mass in her medial left upper thigh (Fig. 1). She had first noticed it one year previously. She had no fever, chills, weight loss, or trauma history. The clinical examination revealed a fixed mass measuring 7 × 4 cm that was not tender, there were no signs of inflammation of the superficial skin or lymphadenopathy. Her hip and knee joints exhibited normal ranges of motion, and she had equal peripheral pulses in both lower limbs.
Fig. 1.
The clinical finding. Swelling mass in the adductor compartment of upper left tigh (Arrow).
Plain X-rays of the left femur showed no bone involvement or calcification.
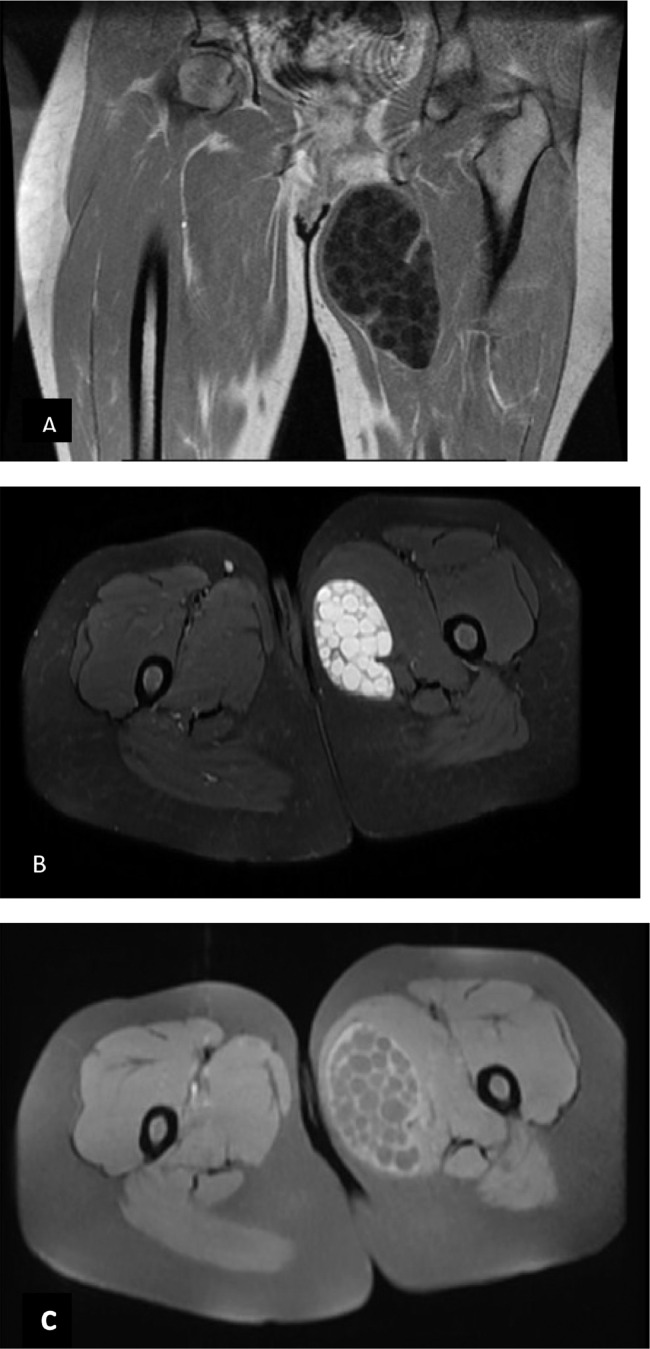
On magnetic resonance imaging (MRI), a cystic mass was seen in the adductor muscles of the left upper thigh. The mass was hypointense on T1-weighted spin echo sequences and hyperintense on T2-weighted gradient echo and fat-saturated images, and it contained smaller cysts (daughter cysts) (Fig. 2), the cyst present a moderate peripheral enhancement after injection of Gadolinium, also the internal cysts. The MR imaging characteristics of the lesion were regarded as diagnostic for a hydatid cyst.
Fig. 2.
MRI images of hydatid cyst within adductor muscles containing daughter cysts occupying almost the entire volume of the mother cyst. (A) T1 weighted spin echo Coronal image demonstrates multiple daughter cysts showing lower signal intensity, (B) T2 weighted gradient echo and Fat saturated axial image the daughter cysts are hyperintense signal, and (C) T1weighted and fat saturated image after intravenious injection of gadolinium showing diffuse pericystic enhancement.
Abdominal ultrasonography and radiographs of the chest showed no evidence of hepatic or pulmonary involvement, and the diagnosis of a primary muscular hydatid disease was made.
Initial laboratory analysis was normal. The hydatid serology was negative.
The cystic mass within the left adductor muscles was resected en bloc under general anaesthesia, leaving wide surgical margins (Fig. 3), with no complications in the immediate follow-up period. Macroscopic and microscopic histopathological examinations of the specimen confirmed the diagnosis of a hydatid cyst. Adjunctive albendazole chemotherapy (400 mg/day) was prescribed for 3 months.
Fig. 3.
Intraoperative view of the mass. Macroscopic aspect.
Discussion
Hydatic disease is a zoonotic disease caused by the echinococcus parasite, which is a member of the Taeniidae family, most commonly caused by the larvae of Echinococcus granulosus, E. multilocularis, E. vogeli, or E. oligarthrus [1]. Hydatid disease can affect every organ system or anatomical place in the human body, however the liver (50%-77%), and lungs (15%-47%) are the most commonly affected organs [2,5]. Primary muscle involvement is extremely uncommon, occurring in just around 3% of all hydatidosis patients [4,[7], [17]]. It has been suggested that the muscle provides an unfavourable environment for the parasite due to the presence of lactic acid [8,9], and because of their contractility [10]. Parasitic cysts usually form around the muscles of the neck, trunk and roots of the limbs [10], like in our case, perhaps because there is a rich vascularization and less muscular activity in these regions.
The clinical symptomology is vague and nonspecific, which frequently leads to a diagnosis delay. The nonspecific clinical picture can be characterized as a painless non inflammatory tumefaction that grows in volume over time while the patient's general health is preserved [10]. However, problems such as nerve compressions or infections that mimic an acute abscess or a malignant tumor reveal a certain number of cysts [6,10].
Ultrasonography should be the first diagnostic tool used for detection of hydatid disease of soft tissue [11] by showing the muscle mass's cystic nature, whereas the CT and MRI images reveal the cyst's location, size, and appearance [10]. The high resolution of MRI for cystic mass detects the presence of daughter cysts while CT best depicts calcifications. For clear identification of affected structures and surgical planning, MRI is the best choice [12,13]. It is also an effective means of making a differential diagnosis [11].
MRI imaging can reveal multitude patterns of intramuscular hydatidosis, based on the stage of evolution of the cyst [21], [22], [23]. In the stage of the simple viable hydatid cyst, the cyst's wall is isointense relative to the fluid in the cyst on T1-weighted images, and shows as a low signal intensity rim surrounding the high-signal intensity contents on T2-weighted images (also known as the "rim sign"). In the stage of a hydatid cyst with daughter cysts, the contents of the mother and daughter cysts are generally isointense on both T1- and T2-weighted images. In the stage of a hydatid cyst with detached parasitic membranes, the membranes are seen floating inside the cyst and show dark on both T1- and T2-weighted images. At the final stage of development, spontaneous collapse and calcification of the cyst occur, leaving a zone of calcification in the host tissues [18]. In this case, MRI was able to demonstrate the multivesicular cyst containing multiple daughter cysts.
After injection of gadolinium, the cysts can present moderate peripheral enhancement because of the pericyst's vascularization. However, with cyst superinfection, greater enhancement is noted related to the hypervascularization of the pericyst as well as the acute inflammation of the surrounding soft tissues [6,10].
Muscle hydatid cyst can mimic a benign or malignant tumor, an abscess in case of fissuring or disinfection, a lipoma, or a calcified hematoma [24].
Serologic tests are useful when they are positive, but they are false negative in half of the cases of primary intramuscular hydatidosis [11], as in our patient's case. The sensitivity rate of the IHA has been reported to be 67 %. Although serology tests such as IHA can contribute in diagnosis, reliance only on them is not advised [19,20].
It is importance to avoid open or percutaneous needle biopsy especially in geographic regions where hydatidosis is endemic, and improper handling during surgery, as these procedures may cause the cyst contents to rupture and disseminate, rupture can enable secondary cysts to occur [10,14].
To prevent recurrence, thorough total surgical excision of the cyst (or drainage if the cyst is in a difficult site) and total irrigation of the surrounding soft tissue with hypertonic saline are currently the treatments of choice. Following surgery, these techniques might be combined with the use of systemic antiparasitic medications [11,15,16]. After surgery, the patient should have a long-term clinical examination to detect recurrence.
Conclusion
Intramuscular infection by E. granulosus may mimic a soft-tissue tumor, resulting in inappropriate cyst rupture and the risk of anaphylaxis and organ dissemination. As a result, preoperative diagnosis is critical, and MRI is an accurate method for preoperative diagnosis and surgical planning. Because of the increased risk of recurrence, local inoculation, and diffusion, biopsies should be avoided.
Guarantor of submission
The corresponding author is the guarantor of submission.
AUTHOR'S CONTRIBUTIONS
All authors contributed to this work. All authors have read and approved the final version of the manuscript.
Patient consent statement
Written informed consent for publication was obtained from patient.
Footnotes
Competing Interests: The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
- 1.Pedrosa I., Saiz A., Arrazola J., Ferreiros J., Pedrosa C.S. Hydatid disease: radiologic and pathologic features and complications. Radiographics. 2000;3:795–817. doi: 10.1148/radiographics.20.3.g00ma06795. 2000. [DOI] [PubMed] [Google Scholar]
- 2.Comert R.B., Aydingoz U., Ucaner A., &Arikan M. Water-lily sign on MR imaging of primary intramuscular hydatidosis of sartorius muscle. Skeletal Radiol. 2003;32(7):420–423. doi: 10.1007/s00256-003-0661-x. [DOI] [PubMed] [Google Scholar]
- 3.Guthrie JA, Lawton JO, Chalmers AG. Case report: the MR appearances of primary intramuscular hydatiddisease. Clin Radiol. 1996;51:377–379. doi: 10.1016/s0009-9260(96)80122-x. [DOI] [PubMed] [Google Scholar]
- 4.Tatari H., Baran Ö., Sanlıdağ T., Göre O., Ak D., Manisalı M., et al. Primary intramuscular hydatidosis of supraspinatus muscle. Arch Orthopaed Trauma Surg. 2001;121(1-2):93–94. doi: 10.1007/pl00013775. [DOI] [PubMed] [Google Scholar]
- 5.Bayram M, Sirikci A. Hydatic cyst locatedintermuscular area of the forearm: MR imaging findings. Eur J Radiol. 2000;36:130–132. doi: 10.1016/s0720-048x(00)00188-1. [DOI] [PubMed] [Google Scholar]
- 6.JerbiOmezzine S., Abid F., Mnif H., Hafsa C., Thabet I., Abderrazek A., et al. Primary hydatid disease of the thigh. A rare location. Orthopaed Traumatol. 2010;96(1):90–93. doi: 10.1016/j.rcot.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 7.Rask MR, Lattig GJ. Primary intramuscular hydatidosisof the sartorius. J Bone Joint Surg Am. 1970;52:582–584. [PubMed] [Google Scholar]
- 8.Merkle EM, Schulte M, Vogel J, Tomczak R, RieberA Kern P, et al. Musculoskeletal involvement in cystic echinococcosis: report of eight casesand review of the literature. AJR Am J Roentgenol. 1997;168:1531–1534. doi: 10.2214/ajr.168.6.9168719. [DOI] [PubMed] [Google Scholar]
- 9.Sreeramulu P.N., Krishnaprasad, Girishgowda S.L. Gluteal region musculoskeletal hydatid cyst: case report and review of literature. Ind J Surg. 2010;72(S1):302–305. doi: 10.1007/s12262-010-0096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kazakos C., Galanis V., Verettas D.-A., Polychronidis A., Simopoulos C. Primary hydatid disease in femoral muscles. J Int Med Res. 2005;33(6):703–706. doi: 10.1177/147323000503300613. [DOI] [PubMed] [Google Scholar]
- 11.Durakbasa M., Kose O., Islam N., &Kilicoglu G. A primary hydatid cyst of the gracilis: a case report. J Orthopaed Surg. 2007;15(1):118–120. doi: 10.1177/230949900701500127. [DOI] [PubMed] [Google Scholar]
- 12.Memis A, Arkun R, Bilgen I, Ustun EE. Primary soft tissue hydatid disease: report of two cases with MRI characteristics. Eur Radiol. 1999;9:1101–1103. doi: 10.1007/s003300050798. [DOI] [PubMed] [Google Scholar]
- 13.Polat P, Kantarci M, Alper F, Suma S, Koruyucu MB, Okur A. Hydatid disease from head to toe. Radiographics. 2003;23:475–494. doi: 10.1148/rg.232025704. [DOI] [PubMed] [Google Scholar]
- 15.Özkoç G, Akpınar S, Hersekli MA, Özalay M, Tandogan R. Primary hydatid disease of the quadriceps muscle: a rare localization. Arch Orthopaed Trauma Surg. 2003;123(6):314–316. doi: 10.1007/s00402-003-0512-1. [DOI] [PubMed] [Google Scholar]
- 14.Ates M., Karakaplan M. Hydatid cyst in the biceps and gluteus muscles: case report. Surg Infect. 2007;8(4):475–478. doi: 10.1089/sur.2006.040. [DOI] [PubMed] [Google Scholar]
- 16.Dudkiewicz I, Salai M, Apter S. Hydatid cystpresenting as a soft-tissue thigh mass in a child. ArchOrthop Trauma Surg. 1999;119:474–475. doi: 10.1007/s004020050025. [DOI] [PubMed] [Google Scholar]
- 17.al-Sayed M, al-Mousa M, al-Salem AH. A hydatid cyst at an unusual site. Trop Geogr Med. 1992;44:275–277. [PubMed] [Google Scholar]
- 18.Salai M, Apter S, Dudkiewicz I, Chechik A, Itzchak Y. Magnetic resonance imaging of hydatid cyst in skeletal muscle. J Comput Assist Tomogr. 1999;23:331–332. doi: 10.1097/00004728-199903000-00031. [DOI] [PubMed] [Google Scholar]
- 19.Durakbasa CU, Tireli GA, Sehiralti V, Sander S, Tosyali AN, Mutus M. An audit on pediatrichydatid disease of uncommon localization: incidence, diagnosis, surgical approach, and outcome. J Pediatr Surg. 2006;41:1457–1463. doi: 10.1016/j.jpedsurg.2006.04.024. [DOI] [PubMed] [Google Scholar]
- 20.Prousalidis J, Tzardinoglou K, Sgouradis L, Katsohis C, Aletras H. Uncommon sites of hydatid disease. World J Surg. 1998;22:17–22. doi: 10.1007/s002689900343. [DOI] [PubMed] [Google Scholar]
- 21.García-Díez A.I., Ros Mendoza L.H., Villacampa V.M., Cózar M., Fuertes M.I. MRI evaluation of soft tissue hydatid disease. Eur Radiol. 2000;10:462–466. doi: 10.1007/s003300050077. [DOI] [PubMed] [Google Scholar]
- 22.Von Sinner W, Strake L, Clarke D, Sharif H. MRimaging in hydatid disease. AJR. 1991;157:741–745. doi: 10.2214/ajr.157.4.1892028. [DOI] [PubMed] [Google Scholar]
- 23.Diez G, Mendoza LHR, Villacampa VM, Cozar M, Fuertes MI. MRI evaluation of soft tissue hyaditid disease. Eur Radiol. 2000;10:462–466. doi: 10.1007/s003300050077. [DOI] [PubMed] [Google Scholar]
- 24.Benhaddou H., Margi M., Kissra M., Benhmamouche M.N. Le kyste hydatique du muscle trapezius: une localisation inhabituelle. Archives de Pédiatrie. 2010;17(3):263–265. doi: 10.1016/j.arcped.2009.11.027. [DOI] [PubMed] [Google Scholar]