Abstract
Ophthalmology, an outpatient surgical specialty, depends on regular in-person encounters to manage complex eye disease. The coronavirus disease 2019 (COVID-19) pandemic has brought about unprecedented challenges in how we take care of our patients. At Vanderbilt University Medical Center, we have gone to great lengths to implement expeditiously a telemedicine platform for safely and securely evaluating our patients during the pandemic. Since implementing live videoconference appointments in late March, 840 patients received ophthalmic care during a 12-week period among all subspecialties at the Vanderbilt Eye Institute. Of these, the majority (79.6%) were either return or postoperative visits. Live telehealth visits were more amenable to certain ophthalmic subspecialties, with paediatrics, neuro-ophthalmology and oculoplastics encounters making up 80.5% of all telemedicine visits. As demonstrated through this care model and our initial experience, live video telemedicine is a sustainable and safe care delivery approach to extend ophthalmic care delivery during the COVID-19 pandemic and even post pandemic.
Keywords: COVID-19, pandemic, telemedicine, ophthalmology
Introduction
The novel severe acute respiratory syndrome coronavirus 2 pandemic has fundamentally altered the practice of medicine. Safe, timely, effective health-care delivery has become increasingly challenging as providers look to protect their own health and the health of their patients. Necessary but non-urgent appointments and surgeries are being delayed, frequently for an indeterminate amount of time. Simultaneously, efforts to curb viral spread, including social distancing and lockdowns, are forcing patients to choose between receiving medical care and risking exposing themselves to coronavirus disease 2019 (COVID-19).
Telehealth leverages electronic information and telecommunications technologies to support, among other things, remote clinical care. Telehealth deployment has traditionally been associated with care in rural settings or as part of the disaster relief efforts.1 In ophthalmology, telemedicine has been mostly incorporated through ‘store-and-forward’ methods, most applicable for tele-emergency consults and screenings for diabetic eye disease and retinopathy of prematurity.2 Store-and-forward telemedicine has similarly been attempted for the detection and monitoring of neovascular age-related macular degeneration (AMD) and screening of glaucoma through digitally transmitted images.3,4 However, the utility of synchronous methods such as live videoconferencing has not been as well described in the literature.5 The limited implementation of synchronous telemedicine to this point reflects the complexity of properly examining the eye. Reliably checking the vision and intra-ocular pressure – two critical components of the eye exam – is elusive in a virtual environment. Even with improving and more cost-effective technology, the adoption of telemedicine in ophthalmology has been limited.
However, the sudden gap in health-care coverage created by the COVID-19 pandemic has spurred a rapid expansion of telemedicine efforts. Herein, we report our initial experience with more than 800 outpatient telehealth visits at a major academic ophthalmology centre.
Initial experience
In response to the COVID-19 pandemic, the American Academy of Ophthalmology (AAO) released recommendations on 18 March 2020, advising the cessation of any non-urgent or non-emergent care.6 In compliance with this important proposal, providers at the Vanderbilt Eye Institute proceeded with an approximate 70% reduction in daily clinic volumes for the month of April. This coincided with an enterprise-wide telehealth initiative to serve our patients while minimising exposure. Telemedicine was performed either by phone call or preferentially by audio-video social media using a secure platform. An institutional contract with Zoom (Zoom Video Communications, San Jose, CA) was used to link a virtual meeting within the Epic Electronic Medical Record (EMR) platform, and the physician and patient each accessed the visit via a ‘my health’ link. Billing used the new Centers for Medicare and Medicaid Services (CMS) guidelines for evaluation and management documentation with modifiers for telemedicine (GT) and catastrophic response (CR) appended.
In the span of four weeks, telemedicine visits grew to represent 18.5% of all visits conducted at the Vanderbilt Eye Institute. During the 12-week period following telemedicine implementation, paediatric and strabismus return and postoperative visits comprised the largest share (35.7%) of the telemedicine visits. Additionally, neuro-ophthalmology (22.4%) and oculoplastics (22.4%) were able to substitute a large portion of their in-person visits with telemedicine visits. Although the patients evaluated by telemedicine at our institution constituted a diverse group over a broad age range, the median age for this cohort was only 36.5 years (see Table 1). Triage visits (defined as unscheduled patient encounters for urgent eye conditions) for conjunctivitis and chalazia were also addressed over the telemedicine platform (Table 2), limiting unnecessary in-person exposure for patients and providers.
Table 1.
Distribution of telemedicine visits from 23 March to15 June 2020.
| Characteristics, N = 840 | Patients, n (%) |
|---|---|
| Age (years), median (IQR) | 36.5 (6.0–59.3) |
| Encounter department | |
| Adult comp | 11 (1.3) |
| Retina | 51 (6.1) |
| Glaucoma | 28 (3.3) |
| Cornea | 74 (8.8) |
| Neuro-ophthalmology | 188 (22.4) |
| Plastics | 188 (22.4) |
| Paeds comp/strabismus | 300 (35.7) |
| Encounter type | |
| New patient | 171 (20.4) |
| Return | 579 (68.9) |
| Postoperative | 90 (10.7) |
IQR: interquartile range.
Table 2.
Nature of triage visits managed over telemedicine.
| Diagnosis | n |
|---|---|
| Conjunctivitis | 15 |
| Chalazion | 12 |
| Scleritis/episcleritis | 9 |
| Visual disturbance | 9 |
| Dry eye syndrome | 8 |
| Ocular/periocular pain | 8 |
Not all ophthalmological sub-specialties were equally amenable to live telehealth visits, as highlighted by the challenges to implementation among glaucoma and retina services. Without being able to assess intra-ocular pressure reliably virtually, patient visits for advanced or uncontrolled glaucoma could not be indefinitely postponed. For the retina service, the overwhelming majority (70%) of in-person visits were for intravitreal injections of anti-vascular endothelial growth factor agents in the setting of potentially blinding conditions such as AMD. Patients with visits early in their postoperative course following intra-ocular surgery also represented a significant proportion of in-person examinations, given the inability to assess intra-ocular inflammation and view the posterior segment using current telemedicine technologies. Despite these limitations, every ophthalmic specialty was able to utilise the new telemedicine format successfully to some degree. Overall, there was a 69.8% reduction in-person visits (Table 3). These scheduled patients for non-urgent conditions (as deemed by the treating provider) were successfully postponed until ramp-up. A total of 18.5% of all visits were conducted virtually.
Table 3.
In-person volume reductions by ophthalmic subspecialty.
| Total | Cornea | Retina | Glaucoma | Paediatrics | Neuro-ophthalmology | Plastics | Optometry | |
|---|---|---|---|---|---|---|---|---|
| Average daily in-person visits before Coronavirus disease 2019 | 261.3 | 35.0 | 64.0 | 47.8 | 46.0 | 18.0 | 14.4 | 36.1 |
| Average daily in-person visits following telemedicine implementation | 79.0 | 12.9 | 24.2 | 12.7 | 11.9 | 8.3 | 5.0 | 4.0 |
| % Reduction | 69.8% | 63.3% | 62.1% | 73.4% | 74.1% | 54.3% | 64.9% | 88.8% |
Challenges to implementation
The use of telemedicine within ophthalmology poses several unique challenges. Our older patient population may struggle with the initial learning curve associated with telemedicine. The ophthalmic physical examination, which is limited in a virtual environment, is critical to the formulation of our diagnosis and treatment plan. The objective measures of ocular health, including visual acuity and intra-ocular pressure, may be difficult or impossible to obtain outside of the office setting. Additionally, as a procedure-based specialty, there is often no reasonable substitute for an in-person examination. Current attempts to address barriers to remote visual acuity testing have included designing an online eye chart to be distributed to patients prior to appointments, but this remains to be validated and has not been compared to office-measured Snellen visual acuity.7 Remote measurement of intra-ocular pressure provides similar challenges, with some suggestions even being made for the possible use of finger tension testing (comparing how hard the eye feels in comparison to familiar objects) as a possible solution.8 Newer technology, including the iCare Home Tonometer (iCare USA, Inc., Raleigh, NC) looks to circumvent the need for in-office visits to measure intra-ocular pressure. Home optic coherence tomography technology for conditions such as AMD is also in the pipeline. However, major gaps exist in the use of these remote methods, and further research focused on validation is necessary to enable their use for routine tele-ophthalmology care.
In addition to the difficulties inherent to ophthalmology, any institution looking to expand telemedicine services during this time must anticipate several personnel-related challenges. Significant preparatory work was required by the front-desk staff, ophthalmic technicians and providers to ensure the seamless conduct of these electronic visits. Information technology support was critical in ensuring access to the necessary equipment and software, as well as staff training. Early on in the process, patients and providers both frequently reported difficulties setting up virtual encounters. Additionally, providers experiencing delays during their in-person clinic were unable to logon for telemedicine visits at the predetermined times, sometimes missing the encounter altogether. A concerted effort was required of management to incorporate a feasible plan and then continuously elicit feedback and calibrate the process. In addition to the operational requirements and infrastructure necessary to perform telemedicine, success of the programme hinged on patient and provider buy-in.
Steps to ensuring success
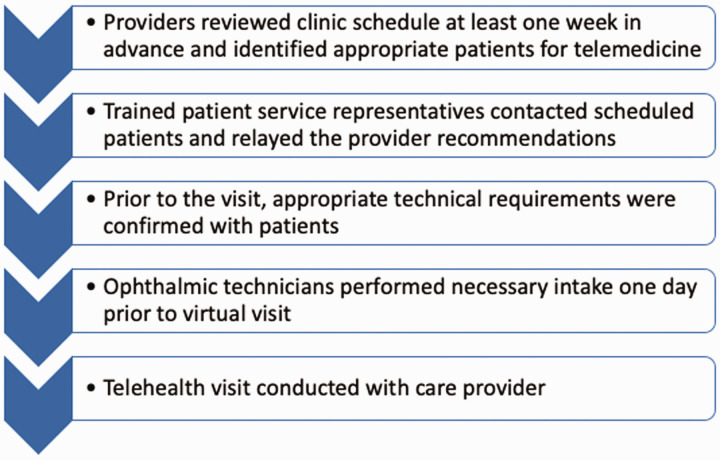
Several factors contributed to the success of our telehealth programme (see Figure 1). Providers need to review the clinic schedules in advance and stratify patients into different categories based on level of urgency. A colour-coded system was adopted within the Epic EMR to convey which patients required in-person evaluations and which patients were suitable for telemedicine visits, as deemed by the treating provider. Trained patient service representatives worked tirelessly to contact scheduled patients and relay the provider recommendations. Vanderbilt University School of Medicine students volunteered to teach patients remotely how to set up their computers or smartphones with the appropriate technical requirements prior to their visit. Additionally, technical staff contacted patients before their scheduled visits to confirm there were no changes in health status and medications. Small time-saving steps such as these are critical to widespread implementation of telemedicine.
Figure 1.
Process flow for telemedicine visits.
We needed a mechanism to minimise virtual wait times. Early in the process, a protocol was set up to manage the patient queue and prevent patients from waiting for the visit to begin. In response to patients’ concerns about waiting for an indeterminate amount of time in front of a computer screen, patients were spaced out appropriately throughout the day and contacted if their provider was delayed. Our secure, HIPAA-compliant Epic integration of Zoom allowed for easy transitions between in-person and virtual visits throughout the day. In-office technical support was available for providers who had difficulty.
Importantly, the relaxing of telehealth restrictions from the CMS created an environment where providers could easily facilitate virtual visits and receive appropriate compensation for the time they were spending with patients.9 Our patient payor mix consists of approximately 48% Medicare, 37% private and 10% Medicaid/TennCare. Alleviating the logistical and billing constraints greatly accelerated implementation. In an effort to accommodate patients residing outside of Tennessee, Vanderbilt Medical Group was able to secure state medical licences quickly en masse from neighbouring states.
Looking to the future
The COVID-19 pandemic poses several hurdles to safe and effective health-care delivery. The medical community has been forced to adapt to a rapidly changing practice environment. This emergent necessity for telemedicine answers allowed our eye-care providers to identify methods to provide safe, effective care through video visits, including triaging new symptoms, ensuring disease stability and confirming adherence to therapy. The accelerated implementation of telehealth across medicine reflects the dedication of practitioners to continue providing care to patients during these uncertain times. Additional research regarding the role of remote examinations can further facilitate the use of telemedicine in ophthalmology. The hope is that even in the post-COVID era, these efforts to institute a secure and reliable telemedicine platform will continue to bear fruit.
As of 29 June 2020, Vanderbilt University Medical Center has undertaken more than 122,000 telemedicine visits across all specialties. We are learning more about which patients can be safely evaluated virtually. The information we collect will help refine future iterations of our telecare platform, easing burden on both patients and providers. We anticipate that certain components of what we learn will persist, such as streamlined patient queues and an optimised patient care flow, including a virtual waiting room for telehealth ophthalmology visits. Furthermore, as technology continues to advance, we should be able to make more accurate and meaningful ocular health assessments over telemedicine. As the tools at our disposal expand, so too will our ability to utilise telemedicine to preserve our patients’ vision while limiting potentially redundant in-person evaluations.
Footnotes
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship and/or publication of this article: S.P. – Alcon (GS); S.H. – none; and S.D. – Gobiquity, Gensight, Olleyes and Nevakar (C).
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: Supported by an unrestricted department award from Research to Prevent Blindness.
ORCID iD: Shriji Patel https://orcid.org/0000-0003-1200-0254
References
- 1.Lurie N, Carr BG.The role of telehealth in the medical response to disasters. JAMA Intern Med 2018; 178: 745–746. [DOI] [PubMed] [Google Scholar]
- 2.Rathi S, Tsui E, Mehta N, et al. The current state of teleophthalmology in the United States. Ophthalmology 2017; 124: 1729–1734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li B, Powell A-M, Hooper PL, et al. Prospective evaluation of teleophthalmology in screening and recurrence monitoring of neovascular age-related macular degeneration: a randomized clinical trial. JAMA Ophthalmol 2015; 133: 276–282. [DOI] [PubMed] [Google Scholar]
- 4.Bergua A, Mardin CY, Horn FK.Tele-transmission of stereoscopic images of the optic nerve head in glaucoma via Internet. Telemed J E Health 2009; 15: 439–444. [DOI] [PubMed] [Google Scholar]
- 5.Caffery LJ, Taylor M, Gole G, et al. Models of care in tele-ophthalmology: a scoping review. J Telemed Telecare 2019; 25: 106–122. [DOI] [PubMed] [Google Scholar]
- 6.American Academy of Ophthalmology. Important coronavirus updates for ophthalmologists, https://www.aao.org/headline/alert-important-coronavirus-context (accessed 19 April 2020).
- 7.Williams AM, Kalra G, Commiskey PW, et al. Ophthalmology practice during the coronavirus disease 2019 pandemic: the University of Pittsburgh experience in promoting clinic safety and embracing video visits. Ophthalmol Ther. Epub ahead of print 6 May 2020. DOI: 10.1007/s40123-020-00255-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saleem SM, Pasquale LR, Sidoti PA, et al. Virtual ophthalmology: telemedicine in a COVID-19 era. Am J Ophthalmol. Epub ahead of print 30 April 2020. DOI: 10.1016/j.ajo.2020.04.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Medicare and Medicaid Services. Medicare telemedicine health care provider fact sheet, https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet (accessed 2 July 2020).