Abstract
Introduction
While strong associations exist between social determinants of health (SDOH), socioeconomic status, and smoking, these factors are not routinely assessed in tobacco treatment programs (TTP). This study addresses this gap by evaluating a composite metric of SDOH and a measure of access to care to determine program reach before and after the implementation of telehealth tobacco treatment delivery.
Aims and Methods
We examined inpatient data from a large TTP during two comparable time periods from April 1, 2019 to September 30, 2019 (pre-telehealth) and from April 1, 2020 to September 30, 2020 (telehealth). The populations were compared using point-of-care data, including 5-digit zip codes mapped to the CDC’s Social Vulnerability Index (SVI) and driving distance (in 60-min increments) to the study hospital. Chi-square tests for homogeneity were performed for SVI and driving distance comparisons.
Results
While distance distributions were significantly different between the pre-telehealth and telehealth populations (χ 2 = 13.5 (df = 3, N = 3234), p = .004, no significant differences existed in the proportion of SVI categories between the two populations (χ 2 = 5.8 (df = 3, N = 3234), p = .12). In the telehealth population, patients with the highest SVI vulnerability had the greatest proportions living >1 h from the hospital.
Conclusions
This study offers a novel evaluation of tobacco treatment in relation to an SDOH metric (SVI) and care access (distance to the hospital) for inpatient populations. Patient reach, including to those with high vulnerabilities, remained consistent in a transition to telehealth. These methods can inform future reach and engagement of patients who use tobacco products, including patients with high vulnerability or who reside at greater distances from treatment programs.
Implications
This study provides the first analysis of inpatient tobacco use treatment (TUT) transition to telehealth delivery of care during the COVID-19 pandemic using the CDC’s SVI metric and patient distance to the hospital. The transition resulted in consistent reach to patients at the highest vulnerability. These findings can inform efforts to evaluate SDOH measures and improve reach, engagement, and research on telehealth delivery of inpatient TUT.
Introduction
Tobacco use, the single most preventable cause of disease, disability, and death in the United States, accounted for nearly half a million deaths in 2019 and resulted in $170 billion spent in direct medical care for adults.1 Ample evidence supports strong associations between social determinants of health (SDOH) and smoking. However, SDOH are not routinely assessed in many tobacco treatment programs, despite the fact that socioeconomic status (SES) is one of the most salient factors associated with smoking, along with education, income, employment, and insurance status. In 2019, the prevalence of current tobacco use was highest among those whose highest educational attainment was a GED (43.7%) and whose annual household income was less than $35 000.2
Although many tobacco cessation strategies have led to decreased tobacco use rates in groups of higher SES, there is still a pressing need for programs that target and serve lower SES groups and racial/ethnic minority groups.3–5 Inpatient tobacco use treatment (TUT) is an effective way to reach patients with limited access to healthcare and to prevent re-hospitalization.6 Hospitalization provides a teachable moment for new or renewed motivation for patients to engage in tobacco use reduction and cessation discussions.7
The University of North Carolina (UNC) Tobacco Treatment Program (TTP) provides inpatient TUT to a largely underserved population, many of whom have limited outpatient access to tobacco treatment services. The average smoking rate for adults in North Carolina was 17.4% in 2018, higher than the national average of 14%.8,9 Tobacco use disproportionately impacts certain groups of North Carolinians, with rates much greater for people with education levels less than a high school diploma, annual household incomes of less than $15 000, functional disabilities, or rural residence (Supplementary File 1).
In March 2020, the UNC TTP swiftly pivoted from an in-person to a virtual (telehealth) treatment program to continue providing TUT and address inpatients’ increased challenges during the COVID-19 pandemic. Smoking and tobacco-related comorbidities, such as respiratory disease, cardiovascular disease, and cancer malignancy emerged as clear risk factors for severe COVID-19 outcomes.10 Simultaneously, individuals with tobacco use disorder reported increased tobacco use during the pandemic.11 And people with tobacco use disorder, especially those who are part of communities of color, experienced disproportionate rates of COVID-19 infection, hospitalization, and death, indicating the critical importance of inpatient TUT programs.12
Telehealth is often delivered via audio and video formats through the use of electronic devices, such as smartphones, tablets, or computers. These technology-dependent methods of care delivery can increase disparities in care for groups with lower SES. The TTP used hospital bedside phones (available in patients’ rooms to allow patients to converse with family/support persons) to deliver telephonic TUT. This care provision removed common outpatient telehealth care hindrances, such as equipment, financial, and broadband access barriers. This transition to telehealth resulted in significantly increased reach for the TTP, described in detail in our earlier manuscript.13
With such a rapid transition and future telehealth insurance coverage still uncertain, it is important to evaluate the characteristics of patients served by the different modes of treatment (in-person vs. telehealth) with an eye toward SES, SDOH, and equitable care delivery. This study addresses these knowledge gaps at one TTP by evaluating the feasibility of using a composite metric of SDOH and a measure of access to care to determine program reach. The two hypotheses evaluated in this study were:
Data collected during TUT delivery are useful as measures of patients’ SDOH and access to care.
Patient reach in relation to Social Vulnerability Indices and care access (as distance to the hospital) would not be significantly different in the telehealth and pre-telehealth populations.
Methods
Institutional Settings
UNC Health is the academic health system for the School of Medicine at the University of North Carolina—Chapel Hill. The UNC TTP provides tobacco treatment services to inpatients at the 950-bed UNC Medical Center in Chapel Hill and the 83-bed UNC Hillsborough Hospital.
Clinical Interventions
Tobacco treatment specialists (TTSs) initiated outreach to all patients in this study. If agreeable to participation, patients received 10- to 20-min in-person (pre-telehealth population) or telephonic (telehealth population) TUT with counseling and tobacco cessation medication recommendations as appropriate (eg, nicotine replacement including patches, gum, lozenges). For telephonic visits, TTSs used cell phones from their homes, connecting via a health care system-approved platform to the patients’ hospital bedside landline phone (requiring no use of patients’ personal equipment).
Data
Inclusion criteria: Patients treated by the UNC TTP team during the time periods from April 1, 2019 to September 30, 2019 (pre-telehealth) and from April 1, 2020 to September 30, 2020 (telehealth). TUT telehealth services were fully operational by April 1, 2020. Pre-telehealth and telehealth populations were chosen from the same months in consecutive years to account for seasonal variability in inpatient populations. Flowsheet data obtained at the point-of-care included patient demographics with 5-digit zip codes. This study was reviewed and approved by the UNC Human Subjects Institutional Review Board.
Measurements
Frequency: Counts of patient demographics (Supplementary File 2).
Measures of Social Determinants of Health
Social Vulnerability Index (SVI): A measure of SDOH for patients in the two populations was evaluated using the 5-digit zip code from each patient mapped to the zip code’s respective county. Counties were then mapped to the Centers for Disease Control and Prevention (CDC) SVI.14 This SVI tool has both county and US Census Tract level data and has been used to evaluate SDOH and impact on outcomes of interest including COVID-19 incidence and risk factors.15 The SVI is reflective of four themes comprised of 15 social factors that can translate to greater or lesser vulnerability to hazards, such as infectious disease outbreaks or natural disasters. The four themes are SES, household composition and disability, minority status and language, and housing and transportation. The 15 social factors making up the SVI are included in Supplementary File 3. The SVI ranges from 0 to 1 with 0 being the lowest vulnerability and 1 being the highest vulnerability.
Distance from the main UNCH hospital as a measure of access to care using hour thresholds (ie, 1–60, 61–120, 121–180, and ≥181 min).16
Analyses
Descriptive statistics and chi-square tests were performed using SPSS V27 software. Full chi-square results for all demographics were reported in a separate manuscript with demographic frequencies summarized in this manuscript’s Supplementary File 2.13 For the chi-square tests of SVI and distance from the hospital, statistically significant differences in distributions for variables with >1 df, were further evaluated with post hoc analysis of 2 × 2 variable category comparisons using the Dunn-Bonferroni method with standardized, adjusted residuals and a Bonferroni-adjusted p value to account for multiple comparisons. Five-digit zip code data were mapped to counties, then the SVI value using the CDC site. Data from this telehealth study were aggregated and reported using the CDC’s four levels of SVI to reflect a low (0–0.25), low-moderate (0.2501–0.50), moderate-high (0.5001–0.75), and high (0.7501–1.00) vulnerability index. Patient zip codes were also used to identify each patient’s driving distance, aggregated, and presented using hour thresholds (ie, 0–60, 61–120, 121–180, and ≥181 min). Java software V8 was used to create algorithms to accomplish mapping of zip codes, SVIs, and driving distances (in minutes).
Results
Chi-square tests for homogeneity showed no significant difference in proportion of SVI categories between the pre-telehealth and telehealth populations (χ 2 = 5.8 (df = 3, N = 3234), p = .12). The pre-telehealth and telehealth populations had similar proportions of patients at each SVI with the greatest proportions at the highest vulnerability index for each time period and less than 1% of each respective population at the lowest vulnerability (Table 1). Distance category distributions were significantly different between the pre-telehealth and telehealth populations (χ 2 = 13.5 (df = 3, N = 3234), p = .004). Post hoc analysis with Bonferroni Correction (p = .006) showed significant differences in the proportion of patients with zip codes ≤60 and 61–120 min to the hospital. In the telehealth population compared to the pre-telehealth population, there were proportionally more patients in the ≤60-min distance (p < .001) and proportionally fewer patients in the 61–120 min (p = .002). In both populations, the greatest proportion of patients lived within 1-h driving distance to the hospital (Table 1).
Table 1.
SVI and Distance in Minutes From the Hospital by Population
| Pre-telehealth patient count (%) | Telehealth patient count (%) | |
|---|---|---|
| Total no. of patients | 1424a | 1810 |
| Social Vulnerability Index (SVI) | ||
| 0–0.2500 = low vulnerability | 4 (0.3%) | 7 (0.4%) |
| 0.2501–0.5000 = low–moderate vulnerability | 503 (35.3%) | 621 (34.3%) |
| 0.5001–0.7500 = moderate-high vulnerability | 174 (12.2%) | 273 (15.1%) |
| 0.7501–1.00 = high vulnerability | 743 (52.2%) | 909 (50.2%) |
| Minutes to hospital by personal vehicle | ||
| 0–60 | 772 (54.2%) | 1098 (60.7%) |
| 61–120 | 482 (33.8%) | 525 (29.0%) |
| 121–180 | 133 (9.3%) | 149 (8.2%) |
| ≥181 | 37 (2.6%) | 38 (2.1%) |
aPre-telehealth population for zip code mapping contained 1426 patients—two additional pre-telehealth patients with zip codes of “99 999” were not included in the analysis.
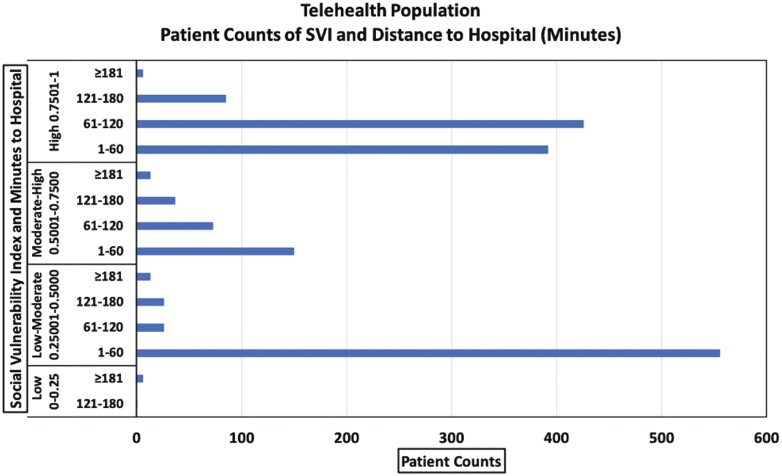
The telehealth population patient counts by distance from the main UNC hospital, stratified by SVI, are provided in Figure 1. Patients with the highest vulnerability, according to the SVI, had the greatest proportions living more than 1 h from the hospital. Most patients with low-moderate vulnerability lived within 1 h of the hospital.
Figure 1.
Telehealth population: patient counts of SVI reported by distance in minutes from the hospital.
Discussion
Some studies have shown outpatient telehealth use was more common in urban and high SES communities.17 This study of inpatient telehealth found that a large proportion of patients treated using telehealth methods were in the highest SVI vulnerability category. This finding speaks to the ability and willingness of patients at the highest vulnerability categories to participate in care delivered via telehealth when equipment and connectivity are made available. These findings also show how the treatment team continued to reach out to these patients to provide TUT despite pandemic restrictions to in-person care, consistent with the call to focus on marginalized populations disproportionately affected by tobacco use.4,5
Comparing telehealth and pre-telehealth counts of patients served showed higher counts in each SVI category in the telehealth period (Table 1). The majority of the telehealth population at the highest vulnerability needed to travel more than 1 h to obtain care at this academic hospital (Figure 1). These data reinforce the importance of efforts to provide continued TUT, during and after hospitalization, for at-risk patients to support their tobacco reduction or cessation journeys. For many, traveling large distances means living in rural environments, and these patients face multiple barriers to TUT, including fewer health care providers, less income, and higher rates of uninsurance.18
Counts of patients in each distance category also increased in the telehealth period compared to the pre-telehealth period (Table 1). In the telehealth period, the TTP served a slightly smaller proportion of patients with zip codes in the 61- to 120-min category, compared to the pre-telehealth period. It is possible that this relatively small proportional decline in patients living further from the hospital reflected COVID-19-induced health care hesitancy,19 coupled with preexisting transportation difficulties, resulting in fewer people who lived further from the hospital seeking inpatient care. This resulted in proportionally fewer patients from these greater distances receiving associated inpatient telehealth TUT.13
This work identified that patients at the highest SVI and distance from the hospital did engage in inpatient telehealth for TUT, providing evidence that telehealth could mitigate some SDOH barriers to TUT. Additionally, this work provides evidence for the feasibility of an SDOH and care access evaluation, using point-of-care data and validated tools, to inform TTP outreach and engagement efforts.
Limitations
Several important limitations exist. These analyses reflect experiences and data from one academic medical center with associated limits to generalizability. As a retrospective study with secondary use of electronic health record (EHR) data, correlations, and patterns in data can be found, but causality cannot be ascertained. Additionally, with secondary use of EHR data, there can be challenges with data not collected for research purposes (eg, missing, incomplete data). Fortunately, this study’s dataset had only two missing zip code values (0.06% missing data) resulting in no significant impact on the final results.
The CDC’s validated SVI metric uses county-level data which may not adequately reflect full variability in SES indicators across a county. Despite county-level SES variability, the SVI has been successfully used in prior studies of SES.15 The SVI could be used by other TTPs to evaluate SES data readily collected during care delivery (ie, 5-digit zip codes). Likewise, the use of zip code-derived driving distances to the main hospital of the Medical Center, as one measure of access to care, has limitations, including variability of distance depending on a patient’s exact address or access to a private vehicle. The measure of private vehicle commuting minutes was chosen as a more consistent measure of distance to the hospital compared to walking or public transit routes.
While we have found that telehealth delivery of inpatient TUT is accepted by patients across the SVI and distance spectrums, this inpatient study did not evaluate outpatient telehealth access barriers. We acknowledge that additional research and policy efforts are needed to evaluate and improve access to telehealth tools and technology-literacy training to ensure equitable outpatient telehealth reach.
Future Work
This study among inpatients bolsters research showing that virtual TTP may increase access to treatment for marginalized and low-income outpatient populations.20 After discharge, it is essential that patients receive outpatient tobacco treatment to maximize quit rates. Evidence is accumulating in support of the feasibility, satisfaction, and notable quit rates associated with telehealth-delivered TUT.21,22 While we showed patients in all SVI categories were reached and receptive to telehealth-delivered TUT, future studies evaluating modes of care delivery (ie, in-person, telephone, and video) in relation to patient preferences, SDOH metrics, and treatment effectiveness are needed when in-person treatment is feasible post-pandemic. The promise of telehealth expanding care to marginalized communities can become a reality if concerted efforts are made to identify barriers and equalize access to required technology equipment, bandwidth, and training on tool use to close the digital divide.23
Future patient-centered surveys on access and barriers to TUT can enrich this data-driven SDOH analysis. Future analyses could also map TTP patient zip codes to broadband availability maps to increase understanding of potential technological barriers to access telehealth TUT. Expansion of SDOH analysis and use of geospatial mapping with use of full address or census tract data could facilitate more precise SDOH metric evaluation. Such metric evaluation could increase identification of environmental risk factors for smoking to improve tobacco use treatment, prevention, and policy efforts.24 It is imperative that ongoing analysis of care delivery continue to inform system and policy efforts to address SDOH to support equitable access to and delivery of healthcare, including tobacco treatment.
Supplementary Material
A Contributorship Form detailing each author’s specific involvement with this content, as well as any supplementary data, are available online at https://academic.oup.com/ntr.
Acknowledgments
We are grateful to the UNC Tobacco Treatment Program team for their provision and documentation of care.
Funding
This work was funded in part by the National Cancer Center, Comprehensive Cancer Center Initiative [grant number 3P30CA016086-43S1].
Declaration of Interests
All authors declare no conflicts of interest.
Data Availability
Data are not available for sharing due to privacy standards for protected health information contained in these data. Researchers may contact the corresponding author with any questions.
References
- 1. Centers for Disease Control and Prevention (CDC). Current Cigarette Smoking Among Adults in the United States. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking. Accessed November 16, 2020.
- 2. Creamer MR, Wang TW, Babb S, et al. . Tobacco product use and cessation indicators among adults—United States, 2018. MMWR. 2019;68(45):1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Garrett BE, Dube SR, Babb S, McAfee T. Addressing the social determinants of health to reduce tobacco-related disparities. Nicotine Tob Res. 2015;17(8):892–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Garrett BE, Martell BN, Caraballo RS, King BA. Socioeconomic differences in cigarette smoking among sociodemographic groups. Prev Chronic Dis. 2019;16:E74. doi: 10.5888/pcd16.180553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kingsbury JH, D’Silva J, O’Gara E, et al. . How much progress have we made? Trends in disparities in tobacco use. Prev Chronic Dis. 2020;17:E107. doi: 10.5888/pcd17.200090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cartmell KB, Dooley M, Mueller M, et al. . Effect of an evidence-based inpatient tobacco dependence treatment service on 30-, 90-, and 180-day hospital readmission rates. Med Care. 2018;56(4):358–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. U.S. Department of Health and Human Services. Smoking Cessation: A Report of the Surgeon General. 2020. https://www.hhs.gov/surgeongeneral/reports-and-publications/tobacco/2020-cessation-sgr-factsheet-key-findings/index.html. Accessed July 1, 2020.
- 8. Centers for Disease Control and Prevention. BRFSS Prevalence & Trends Data. 2019. https://www.cdc.gov/brfss/brfssprevalence/. Accessed February 19, 2021.
- 9. Behavioral Risk Factor Surveillance System. Statistics and Reports: North Carolina. https://schs.dph.ncdhhs.gov/data/brfss/2018/nc/all/topics.htm#tu. Accessed May 19, 2021.
- 10. Patanavanich R, Glantz SA. Smoking is associated with COVID-19 progression: a meta-analysis. Nicotine Tob Res. 2020;22(9):1653–1656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kowitt SD, Cornacchione Ross J, Jarman KL, et al. . Tobacco quit intentions and behaviors among cigar smokers in the United States in response to COVID-19. Int J Environ Res Public Health. 2020;17(15):5368–5382. doi: 10.3390/ijerph17155368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Snowden LR, Graaf G. COVID-19, social determinants past, present, and future, and African Americans’ health. J Racial Ethn Health Disparities. 2021;8(1):12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Shoenbill KA, Newcomer E, Valcourt-Hall C, et al. . An analysis of inpatient tobacco use treatment transition to telehealth. Nicotine Tob Res. 2021:ntab233. doi: 10.1093/ntr/ntab233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry/Geospatial Research A, and Services Program. CDC Social Vulnerability Index 2018 Database. https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html. Accessed February 5, 2021.
- 15. Karmakar M, Lantz PM, Tipirneni R. Association of social and demographic factors with COVID-19 incidence and death rates in the US. JAMA Netw Open. 2021;4(1):e2036462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Bliss RL, Katz JN, Wright EA, Losina E. Estimating proximity to care: are straight line and zipcode centroid distances acceptable proxy measures? Med Care. 2012;50(1):99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Cantor JH, McBain RK, Pera MF, Bravata DM, Whaley CM. Who is (and is not) receiving telemedicine care during the COVID-19 pandemic. Am J Prev Med. 2021;61(3):434–438. doi: 10.1016/j.amepre.2021.01.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Talbot JA, Williamson ME, Pearson KB, et al. . Advancing Tobacco Prevention and Control in Rural America. Washington, DC: National Network of Public Health Institutes; 2019. https://nnphi.org/wp-content/uploads/2019/02/AdvancingTobaccoPreventionControlRuralAmerica.pdf. Accessed April 22, 2021. [Google Scholar]
- 19. Birkmeyer JD, Barnato A, Birkmeyer N, Bessler R, Skinner J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff (Millwood). 2020;39(11):2010–2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Slater JS, Nelson CL, Parks MJ, Ebbert JO. Connecting low-income smokers to tobacco treatment services. Addict Behav. 2016;52(Jan):108–114. doi: 10.1016/j.addbeh.2015.10.013. [DOI] [PubMed] [Google Scholar]
- 21. Richter KP, Shireman TI, Ellerbeck EF, et al. . Comparative and cost effectiveness of telemedicine versus telephone counseling for smoking cessation. JMIR. 2015;17(5):e113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kotsen C, Dilip D, Carter-Harris L, et al. . Rapid scaling up of telehealth treatment for tobacco-dependent cancer patients during the COVID-19 outbreak in New York City. Telemed J E Health. 2021;27(1):20–29. doi: 10.1089/tmj.2020.0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Federal Communications Commission. COVID-19 Telehealth Program. Federal Communications Commission. https://www.fcc.gov/covid-19-telehealth-program. Accessed April 5, 2021.
- 24. Siegel SD, Brooks MM, Gbadebo BM, Laughery JT. Using geospatial analyses of linked electronic health records and tobacco outlet data to address the social determinants of smoking. Prev Chronic Dis. 2019;16:E152. doi: 10.5888/pcd16.190186. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are not available for sharing due to privacy standards for protected health information contained in these data. Researchers may contact the corresponding author with any questions.