Abstract
Objective The jugular foramen is one of the most challenging surgical regions in skull base surgery. With the development of endoscopic techniques, the endoscopic endonasal approach (EEA) has been undertaken to treat some lesions in this area independently or combined with open approaches. The purpose of the current study is to describe the anatomical steps and landmarks for the EEA to the jugular foramen and to compare it with the degree of exposure obtained with the lateral infratemporal fossa approach.
Materials and Methods A total of 15 osseous structures related to the jugular foramen were measured in 33 adult dry skulls. Three silicone-injected adult cadaveric heads (six sides) were dissected for EEA and three heads (six sides) were used for a lateral infratemporal fossa approach (Fisch type A). The jugular foramen was exposed, relevant landmarks were demonstrated, and the distances between relevant landmarks and the jugular foramen were obtained. High-quality pictures were obtained.
Results The jugular foramen was accessed in all dissections by using either approach. Important anatomical landmarks for EEA include internal carotid artery (ICA), petroclival fissure, inferior petrosal sinus, jugular tubercle, and hypoglossal canal. The EEA exposed the anterior and medial parts of the jugular foramen, while the lateral infratemporal fossa approach (Fisch type A) exposed the lateral and posterior parts of the jugular foramen. With EEA, dissection and transposition of the facial nerve was avoided, but the upper parapharyngeal and paraclival ICA may need to be mobilized to adequately expose the jugular foramen.
Conclusion The EEA to the jugular foramen is anatomically feasible but requires mobilization of the ICA to provide access to the anterior and medial aspects of the jugular foramen. The lateral infratemporal approach requires facial nerve transposition to provide access to the lateral and posterior parts of the jugular foramen. A deep understanding of the complex anatomy of this region is paramount for safe and effective surgery of the jugular foramen. Both techniques may be complementary considering the different regions of the jugular foramen accessed with each approach.
Keywords: jugular foramen, internal carotid artery, infratemporal fossa, endoscopic, endonasal, microscopic, skull base surgery
Introduction
The jugular fossa and foramen constitute one of the most challenging regions in skull base surgery. 1 2 3 Besides transmission of the internal jugular vein (IJV) and lower cranial nerves IX–XI, its deep location and vital surrounding structures contribute to the difficulties related to surgical approaches to this area. The internal carotid artery (ICA) anteriorly, the facial nerve laterally, the hypoglossal nerve medially, and the vertebral artery inferiorly are some of the important neurovascular structures surrounding the jugular foramen. 2 Tumors are the most common lesions involving the jugular foramen; the majority of which are paragangliomas, schwannoma, and meningiomas, with a small percentage of other tumors, such as chondrosarcomas and chordomas. 4
Multiple approaches, some combined, have been used to access the jugular foramen. Traditional approaches to the jugular foramen can be categorized into three groups: (1) lateral approaches directed through the mastoid bone, including Fisch's infratemporal fossa approach type A; (2) posterior approaches directed through the posterior cranial fossa, including retrosigmoid, far-lateral, and transcondylar variations; and (3) anterior approach directed through the tympanic bone, including preauricular subtemporal-infratemporal approach. 1 2 5
With the development of endoscopic techniques, the endoscopic endonasal approach (EEA) has been used to treat some lesions in the jugular foramen independently 6 7 8 9 10 or combined with open approaches. 11 12 However, description of the endoscopic endonasal anatomy of the jugular foramen is rare in the literature. 6 13 14 15 16 The purpose of this study is to describe the anatomical steps and landmarks for the EEA to the jugular foramen and to compare it with the degree of exposure obtained with the infratemporal fossa approach (Fisch type A), which is a classical microsurgical approach to the jugular foramen used by otolaryngologists.
Materials and Methods
Osseous Study
Thirty-three adult dry skulls were used to study the osseous structures related to the jugular foramen. Fifteen morphometric measurements were taken from the extracranial surface of the skull base with the help of a sliding Vernier caliper: eight from the anterior perspective, and seven from the lateral perspective. To secure the fidelity of data, Liu and Yang did the measurements, and the final values presented were averaged data. From the anterior perspective, MPP was define as the intersection point of an extended line of the conchal crest of the palatine bone and the posterior margin of the medial pterygoid plate, and MPP corresponds to the anterior margin of the pharyngeal orifice of the eustachian tube (ET) and was used as the starting point for measurements: A1, foramen ovale; A2, foramen spinosum; A3, sphenoid spine (SS); A4, carotid foramen; A5, jugular foramen; A6, foramen lacerum; A7, hypoglossal canal; A8, occipital condyle ( Fig. 1A ). Correspondently, SS was chosen as the lateral perspective start point, which was an important landmark in open lateral microsurgical approaches: L1, posterior margin of foramen spinosum; L2, posterior margin of foramen ovale; L3, lateral margin of foramen lacerum; L4, hypoglossal canal; L5, lateral margin of occipital condyle; L6, carotid foramen; L7, jugular foramen ( Fig. 1B ).
Fig. 1.
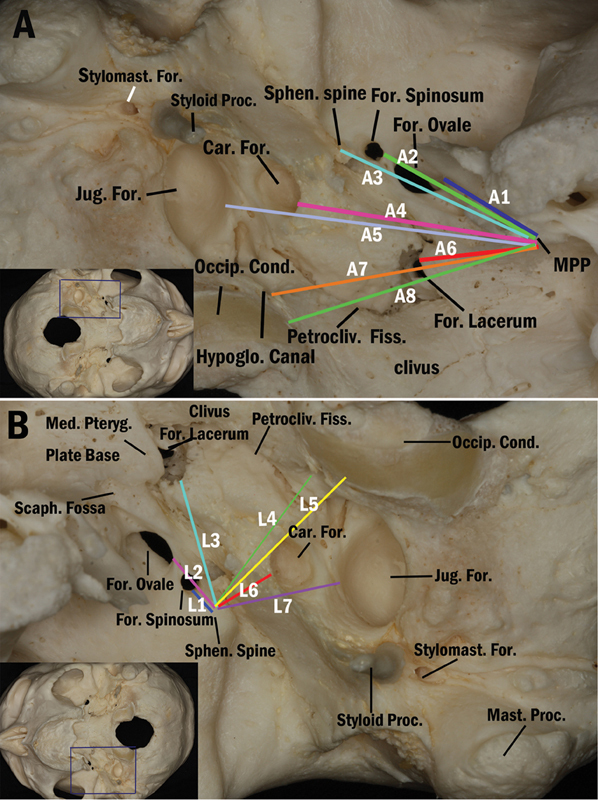
Dry skull photographs showing the measurements of the landmarks related to the jugular foramen. ( A ) From the anterior perspective, the posterior margin of the MPP was used as the starting point for the measurements. This point corresponds to the pharyngeal orifice of the eustachian tube, and the distances measured were as follows: A1, distance from the MPP to the foramen ovale; A2, distance from the MPP to the foramen spinosum; A3, distance from the MPP to the sphenoid spine; A4, distance from the MPP to the carotid foramen; A5, distance from the MPP to the jugular foramen; A6, distance from the MPP to the foramen lacerum; A7, distance from the MPP to the hypoglossal canal; A8, distance from the MPP to the occipital condyle. ( B ) From the lateral perspective, the sphenoid spine was used as the starting point for the measurements: L1, the posterior margin of the foramen spinosum; L2, the posterior margin of the foramen ovale; L3, the lateral margin of the foramen lacerum; L4, the hypoglossal canal; L5, the lateral margin of the occipital condyle; L6, the carotid foramen; L7, the jugular foramen. Car., carotid; Cond., condyle; For., foramen; Jug., jugular; MPP, medial pterygoid plate; Mast., mastoid; Med., medial; Occip., occipital; Petrocliv., petroclival; Proc., process; Pteryg., pterygoid; Sphen., sphenoid; Stylomast., stylomastoid; Hypoglo. hypoglossal.
Anatomical Dissection
Six lightly embalmed human-head specimens (12 sides) were injected with colored silicone and scanned for computed tomography imaging guidance before dissection. In three heads (six sides), an infratemporal approach (Fisch type A) was performed. In the remaining three heads (six sides), an EEA to the jugular foramen was completed. The jugular foramen was exposed, and relevant landmarks were demonstrated.
Endoscopic Endonasal Approach
Three heads (six sides) were used for endoscopic dissection with rod-lens endoscopes, 4 mm in diameter and 18 cm in length, with 0 and 45 degrees lenses (Storz Endoscopy, Tuttlingen, Germany). Video images of the endoscopic anatomy were recorded with Image 1 system (Storz Endoscopy, Tuttlingen, Germany) with HD video camera. Endoscopic skull base surgical instruments (Storz Endoscopy, Tuttlingen, Germany), skull base surgical drills, and navigation (Stryker Corp, Kalamazoo, Michigan, United States) were used to complete the dissection. EEA dissections to the jugular foramen were performed through combined trasnasal and endoscopic sublabial transmaxillary approaches. The sublabial transmaxillary approach was added to augment lateral dissection within the infratemporal fossa. Under visualization with a 0 degrees endoscope, the dissection started with ipsilateral resection of the middle turbinate and a complete spheno-ethmoidectomy. The floor of the sphenoid sinus was drilled to the level of its posterior wall providing broad communication between the sphenoid sinus and the nasopharynx. The nasopharyngeal orifice of the ET was well appreciated. A medial maxillectomy was performed on the same side to widely expose the posterior wall of the maxillary sinus from the nasal floor to the orbit. A complete transpterygoid approach was performed. The dissection progressed from the pterygosphenoidal fissure to foramen lacerum, from foramen lacerum to petroclival fissure, and from petroclival fissure to jugular foramen.
At this point, a sublabial transmaxillary approach was added to facilitate dissection in the infratemporal fossa. Using both routes (transnasal and transmaxillary), the dissection progressed within the infratemporal fossa contents. The internal maxillary artery and its branches were identified and ligated. The V2 and V3 branches of the trigeminal nerve were identified and preserved or sectioned if necessary to facilitate further dissection within the infratemporal fossa. In most cases, it is not necessary to cut V2 and V3 during the endonasal exposure of the jugular foramen. In our six dissections, just one need cut V2 and V3 for better visualization and measurement. And in an actual clinical scenario, V2 and V3 should be preserved. The upper parapharyngeal space was dissected. The medial ET was mobilized inferiorly and laterally after disconnecting it from the pterygoid-sphenoidal fissure, and resected partially or completely 17 18 to allow further dissection of the petrous part of the temporal bone and the petroclival fissure. The petrous part of the temporal bone was drilled to expose the petrous segment of the ICA. 17 The inferior wall of the carotid canal, and the middle and inferior clival bone were drilled to identify the hypoglossal canal, jugular tubercle, and inferior petrous sinus. 6 The ICA from the parapharyngeal segment to the paraclival segment was dissected, mobilized, and displaced medially to maximize direct access to the jugular foramen for measurements. In a clinical setting, dissection is usually medial to the ICA. The medial mobilization was only for measurements in this study. For the surgical approach, medial or lateral mobilization of the ICA may be required. For example, a lesion expanding inferiorly to the occipital condyle may not require mobilization of the ICA.
The posterior wall of the carotid canal in the temporal bone, vaginal process of the tympanic part of the temporal bone, as well as infralabyrinthine air cells were drilled. Then the jugular foramen region was fully exposed. In cases of infectious process or biopsies, a full exposure of the foramen is not required.
Infratemporal Fossa Approach (Fisch Type A)
A postauricular C-shaped skin incision was performed. Transection with closure of the external auditory canal was completed. A wide mastoidectomy was performed. The facial nerve was skeletonized from the geniculate ganglion to stylomastoid foramen. In the upper cervical dissection, the jugular vein, ICA, and lower cranial nerves IX–XII were identified. The facial nerve was identified as it exited the stylomastoid foramen. The facial nerve was then transposed anteriorly from the geniculate ganglion to the stylomastoid foramen. The tympanic membrane, malleus, and incus were removed, and the tympanic bone in the anterior hypotympanum was drilled to expose the lateral aspect of the jugular bulb. The infralabyrinthine bone overlying the jugular bulb, ICA, and sigmoid sinus were removed. The sigmoid sinus was occluded and ligated. The medial wall of the ET was removed to identify the petrous carotid artery. 19 The upper cervical IJV, the jugular bulb, and the sigmoid sinus were exposed, ligated and resected to identify the lower cranial nerves in the jugular foramen region.
Results
Osseous Study
Jugular Foramen and Its Related Osseous Structures
The jugular foramen is located between the temporal bone and the occipital bone ( Fig. 2A , B ). The jugular foramen is divided into three compartments: two venous compartments and a neural compartment. 2 The venous compartments consist of a larger posterolateral venous channel, the sigmoid part, and a smaller anteromedial venous channel, the petrosal part ( Fig. 2B – D and F ). The neural part, through which the glossopharyngeal, vagus, and accessory nerves course, is located between the sigmoid and petrosal parts at the site of the intrajugular processes of the temporal and occipital bones.
Fig. 2.
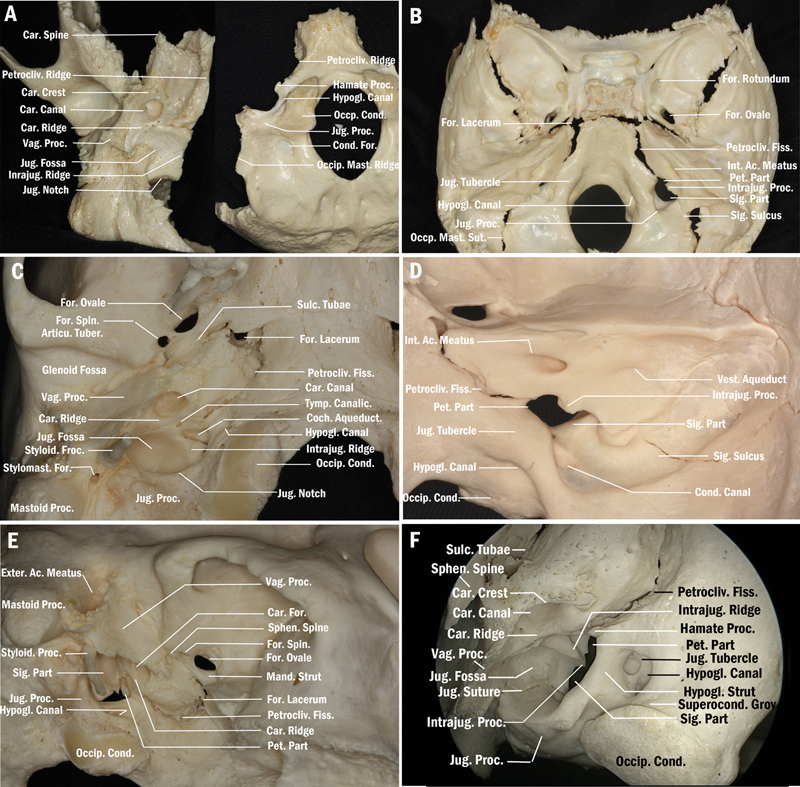
Views of the related osseous landmarks around the JF. Exocranial ( A ) and endocranial ( B ) views of the osseous landmarks around the JF. The jugular foramen is formed by the temporal bone medially and the occipital bone laterally. ( C ) Close view of the ventral surface of the JF related osseous landmarks in right side from anteroinferior perspective. The carotid foramen is anterior to the JF. The vaginal process of the tympanic part of the temporal bone, the styloid process, and the stylomastoid foramen are anterolateral, lateral, and posterolateral to the JF, respectively. The sulcus tubae is anterior to the carotid foramen. The anterior end of the sulcus tubae is close to the foramen lacerum medially. Lateral to the sulcus tubae are the sphenoid spine, the foramen spinosum, and the foramen ovale, respectively, from posterior to anterior. The occipital condyle and the hypoglossal canal are located medial to the JF. ( D ) Posterolateral view of the intracranial surface of the osseous landmarks around the JF. The JF is divided into three compartments from anterior to posterior: petrosal part, neural part, and sigmoid part. Anteromedial is the petroclival fissure and posterolateral is the sigmoid sulcus. The jugular tubercle is situated medial to the JF. The intracranial orifice of the hypoglossal canal is located inferior to the jugular tubercle. The condylar canal is posterior to the JF. ( E ) Anterolateral view of the intracranial surface of the osseous landmarks around the JF. ( F ) Endoscopic anterolateral view of the ventral osseous landmarks around the JF. The carotid ridge separates the jugular fossa from the carotid foramen. The hypoglossal canal is separated from the JF by the hypoglossal strut. Ac., acoustic; Car., carotid; Cond., condyle; Exter., external; Fiss., fissure; For., foramen; Hypogl., hypoglossal; Intrajug., intrajugular; Int. internal; JF, jugular foramen; Jug., jugular; Mand., mandibular; Mast., mastoid; Occip., occipital; Pet., petrosal; Proc., process; Petrocliv., petroclival; Sphen., sphenoid; Sut., suture; Sulc., sulcus; Sig., sigmoid; Styloid., styloidal; Stylomast., stylomastoid; Vag., vaginal; Vest., vestibular.
The jugular tubercle is situated medial to the medial edge of the jugular foramen ( Fig. 2B , D , and F ). The occipital condyle is located along the lateral margin of the anterior half of foramen magnum in the area below and medial to the jugular foramen ( Fig. 2A , C , and D–F ). The hypoglossal canals are located medial to the jugular foramina between the jugular tubercle and occipital condyle ( Fig. 2A – F ). The anterior margin of the jugular foramen, namely the carotid ridge, separates the foramen, and the carotid canal ( Fig. 2C ). The styloid process and the stylomastoid foramen are located lateral to the outer orifice of the jugular foramen ( Fig. 1A , B , and 2C ). The facial nerve exits the stylomastoid foramen lateral to the lateral edge of the jugular foramen. The anterior margin of the jugular foramen is located just behind the part of the tympanic bone that forms the posterior wall of the glenoid fossa and the anterior and inferior walls of the bony part of the external auditory canal ( Fig. 1A , B and 2C , E ). The vaginal process of the tympanic part of the temporal bone separates both the carotid canal and sigmoid part of the foramen from the glenoid fossa ( Fig. 2C , E ). The styloid process projects downward from the vaginal process of the tympanic part of the temporal bone, lateral to the jugular foramen ( Fig. 1A , B and 2C, E ).
The results of eight measurements of the osseous landmarks related to the anterior approach to the jugular foramen are described in Table 1 . The results of seven measurements of osseous landmarks related to the lateral approach to the jugular foramen are available in Table 2 . Important measurements were obtained for the EEA approach. For example, the mean distance from the pharyngeal orifice of the ET to foramen lacerum is 15 mm, 29 mm to the carotid foramen, and 30 mm to the jugular foramen.
Table 1. Distances of osseous landmarks around the jugular foramen from anterior perspective.
| Measurements | Side | Mean (mm) |
Minimum (mm) |
Maximum (mm) |
|
|---|---|---|---|---|---|
| A1 | Distance from MPP to foramen ovale | L | 13.5 | 9.0 | 18.0 |
| R | 14.5 | 11.5 | 19.6 | ||
| A2 | Distance from MPP to foramen spinosum | L | 25.8 | 21.0 | 31.0 |
| R | 26.4 | 21.4 | 34.2 | ||
| A3 | Distance from MPP to sphenoid spine | L | 29.9 | 25.0 | 36.0 |
| R | 30.1 | 24.7 | 35.0 | ||
| A4 | Distance from MPP to carotid foramen | L | 29.0 | 23.0 | 33.0 |
| R | 29.2 | 24.5 | 34.0 | ||
| A5 | Distance from MPP to jugular foramen | L | 30.25 | 27.3 | 33.2 |
| R | 30.13 | 27.5 | 32.8 | ||
| A6 | Distance from MPP to foramen lacerum | L | 15.62 | 13.5 | 17.7 |
| R | 15.27 | 12.9 | 17.6 | ||
| A7 | Distance from MPP to hypoglossal canal | L | 25.7 | 22.0 | 30.0 |
| R | 26.0 | 21.0 | 32.0 | ||
| A8 | Distance from MPP to occipital condyle | L | 21.1 | 17.0 | 29.0 |
| R | 22.2 | 17.0 | 29.2 |
Note: The middle point of the posterior (MPP) margin of the medial pterygoid plate was used as the starting point for the measurements, which corresponds to the pharyngeal orifice of the eustachian tube.
Table 2. Distances of osseous landmarks around the jugular foramen from the lateral perspective.
| Measurements | Side | Mean (mm) | Minimum (mm) | Maximum (mm) | |
|---|---|---|---|---|---|
| L1 | Distance from SS to foramen spinosum | L | 4.4 | 1.0 | 9.0 |
| R | 4.5 | 1.0 | 8.0 | ||
| L2 | Distance from SS to foramen ovale | L | 9.5 | 5.0 | 12.0 |
| R | 9.6 | 5.8 | 13.0 | ||
| L3 | Distance from SS to foramen lacerum | L | 18.2 | 7.0 | 22.0 |
| R | 18.6 | 7.1 | 24.0 | ||
| L4 | Distance from SS to hypoglossal canal | L | 11.8 | 8.3 | 17.0 |
| R | 12.0 | 8.3 | 15.5 | ||
| L5 | Distance from SS to occipital condyle | L | 19.4 | 17.0 | 23.0 |
| R | 20.0 | 16.0 | 27.0 | ||
| L6 | Distance from SS to carotid foramen | L | 7.6 | 5.0 | 11.0 |
| R | 7.8 | 5.5 | 10.5 | ||
| L7 | Distance from SS to jugular foramen | L | 20.8 | 17.0 | 26.0 |
| R | 21.0 | 16.8 | 28.0 |
Abbreviation: SS, sphenoid spine.
Anatomical Dissection
Endoscopic Endonasal Approach to the Jugular Foramen
In the EEA to the jugular foramen, identification of the petrous segment of the ICA was one of the most important steps. The landmarks for the petrous segment of the ICA (anterior genu or lacerum, horizontal part, and posterior genu of the petrous ICA) were the vidian canal, pterygosphenoidal fissure, foramen lacerum, ET, V3, SS and levator veli palatine muscle ( Fig. 3A ). The pterygosphenoidal fissure, foramen lacerum contents, and fibrocartilaginous tissue of the petroclival fissure were continuous with the cartilaginous part of the ET ( Fig. 3B ). The inferior petrosal sinus, the hypoglossal canal and the jugular tubercle were important landmarks in the petroclival region and jugular foramen region ( Fig. 3C ).
Fig. 3.
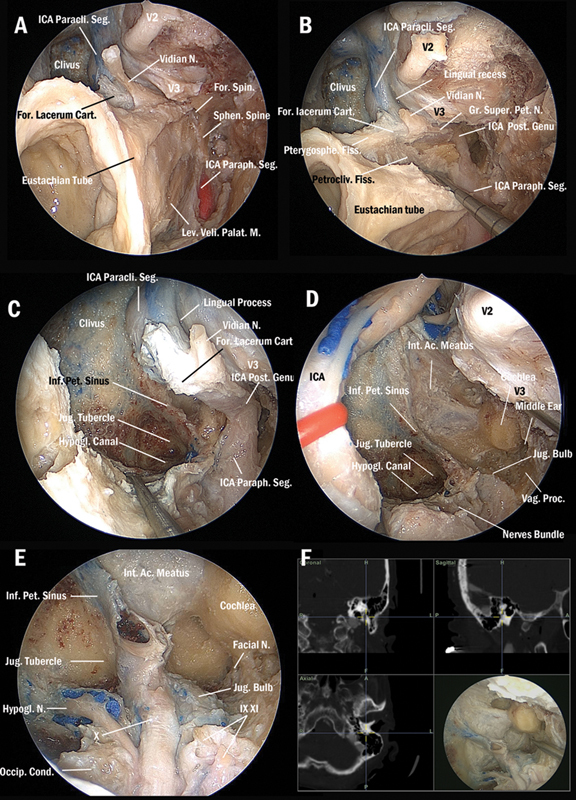
Endoscopic endonasal approach to the jugular foramen. ( A ) After dissection of the infratemporal fossa and drilling of the pterygoid part of the sphenoid bone to identify following landmarks: the vidian nerve, the foramen lacerum cartilage, the anterior genu of ICA, the V2, the V3, the eustachian tube, the sphenoid spine, and the parapharyngeal segment of the ICA. ( B ) After resection of the tensor veli palatini muscle and drilling the sphenoid spine, the tubal process of the tympanic part of the temporal bone was identified as well as the anteromedial portion of the tympanic part of the temporal bone to expose the bony part of the ET; the vertical ICA; the posterior genu of the ICA; and the hypotympanum. After cutting the cartilaginous ET from the foramen lacerum fibrocartilage below the level of the vidian nerve and drilling the petrous bone following the vidian nerve and the greater superficial petrosal nerve, the anterior genu of the ICA and the horizontal segment of the petrous ICA were exposed. ( C ) After cutting the pharyngobasilar fascia from the foramen lacerum, drilling the inferior wall of the carotid canal, and removing the middle and inferior clival bone to identify the hypoglossal canal and the jugular tubercle. The fibrocartilage of the petroclival fissure was removed to expose the whole course of the ICA from the parapharyngeal to the paraclival segments. ( D ) The ICA was displaced medially to get full access to the jugular foramen region. The hypoglossal canal was open to identify the hypoglossal nerve. The inferior petrous sinus was dissected and the jugular tubercle was drilled. The posterior wall of the carotid canal, the vaginal process of the tympanic part of the temporal bone, and a portion of the mastoid cells (the retrofacial cells and infralabyrinthine cells) were drilled to expose the posterior cranial nerves bundle. ( E ) After dissection of the nerves bundle to identify the cranial nerves IX–XII (the cranial nerves IX and XI were sectioned). The jugular bulb is situated posterolateral to the nerves bundle. ( F ) Image guidance confirmed the fallopian portion of the facial nerve, the jugular bulb and the cochlea. Ac., acoustic; Car., carotid; Cart., cartilage; Cond., condyle; Fiss., fissure; For., foramen; Gr., greater; Hori., horizontal; Hypogl. hypoglossal; Int. internal; Jug., jugular; Lev., levator; M., muscle; N., nerve; Occip., occipital; Paracli., paraclival; Paraph., parapharyngeal; Palat., palatine; Pet., petrous; Petrocliv., petroclival; Post., posterior; Proc., process; Spterygosph., Pterygosphenoidal; Sphen., sphenoid; Seg., segment; Sphen., sphenoid; Super., superficial; Vag., vaginal; ICA, internal carotid artery.
The entire course of the ICA from the parapharyngeal to paraclival segments was dissected and displaced medially for full exposure of the jugular foramen region ( Fig. 3C ). Although this provides maximal access, it does not represent typical intraoperative dissection. After medial displacement of the ICA, the jugular foramen was fully accessed. Besides the medial and anterior parts of the jugular foramen, the lateral and superior parts of the jugular foramen were also well accessed. The lower cranial nerves were identified in the center of the jugular foramen region. The hypoglossal canal was situated medial to the nerve bundle. The inferior petrous sinus coursed medio-superiorly. Between the inferior petrous sinus and the hypoglossal canal was the jugular tubercle. The occipital condyle was located medio-inferiorly to the nerve bundle. The sigmoid sinus coursed latero-superiorly. The cochlea was located superiorly. The vaginal process of the tympanic part of the temporal bone was situated lateral to the nerve bundle ( Fig. 3D – F ).
Infratemporal Fossa Approach Type A to the Jugular Foramen
In the subtotal petrosectomy, important landmarks were identified and skeletonized, such as petrous segment of the ICA, sigmoid sinus, jugular bulb, semicircular canals, middle cranial fossa, facial nerve in the fallopian canal, digastric ridge, and stylomastoid foramen ( Fig. 4A ). The facial nerve was identified and freed from the temporal bone from the stylomastoid foramen to the geniculate ganglion and then transposed anteriorly to fully expose the jugular foramen region. The ICA was identified from the parapharyngeal segment to the petrous segment. The IJV was identified from upper neck and jugular bulb to the sigmoid sinus. The carotid ridge separates the ICA from the IJV ( Fig. 4B ). To provide full access to the lower cranial nerves, the IJV, jugular bulb, as well as sigmoid sinus were ligated and resected ( Fig. 4C , D ). Microscopic dissection allowed visualization of the three compartments of the jugular foramen: petrous part anteriorly, neural part medially, and sigmoid part posteriorly ( Fig. 4D ). The petrous segment of the ICA was situated anterior to the jugular foramen separated by the carotid ridge. The hypoglossal canal was located posteroinferior to the jugular foramen separated by the jugular tubercle. The occipital condyle was situated inferior to the hypoglossal canal ( Fig. 4C , D ).
Fig. 4.
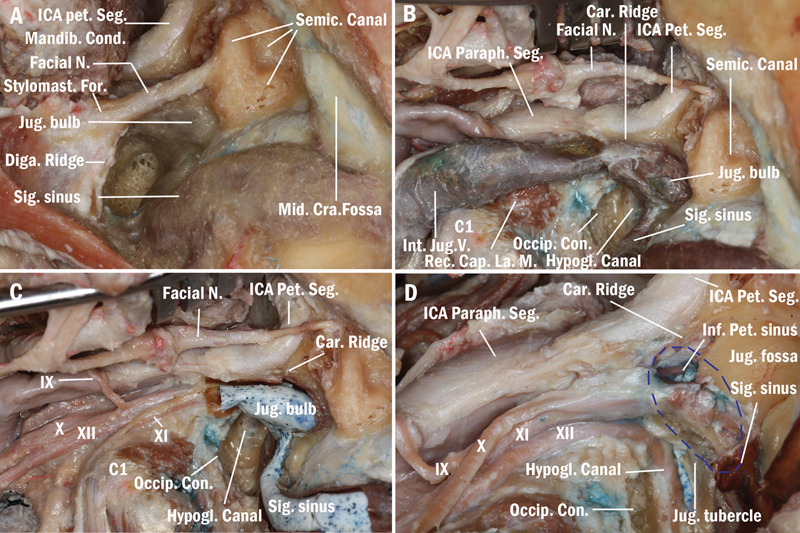
Lateral microscopic infratemporal fossa type A approach to the jugular foramen. ( A ) Subtotal petrosectomy was performed to identify the petrous segment of the ICA, the facial nerve in fallopian canal, the jugular bulb, and the sigmoid sinus. ( B ) The facial nerve was identified and freed from the temporal bone from the stylomastoid foramen to the geniculate ganglion and then transposed anteriorly to fully expose the jugular foramen region. The ICA was identified from the parapharyngeal segment to the petrous segment. The internal jugular vein was identified from upper neck through the jugular bulb to the sigmoid sinus. ( C ) The cranial nerves IX–XII were identified from the upper neck to the jugular foramen region. The internal jugular vein in upper neck was ligated and resected to view the relationship of the posterior cranial nerves, the internal jugular vein, and the jugular bulb. ( D ) The jugular bulb and the sigmoid sinus were ligated and removed, and the hypoglossal canal was drilled to identify the hypoglossal nerve. Microscopic lateral view of the three compartments of the jugular foramen (the blue dashed circle): the petrous part anteriorly, the neural part medially, and the sigmoid part posteriorly. Car., carotid; Cap., capitis; Cra., cranial; Cond., condyle; Diga., digastrics; Lat., lateralis; Hypogl., hypoglossal; Int., internal; Jug., jugular; M., muscle; Mandib., mandibular; Mid., middle; N., nerve; Occip., occipital; Paraph., parapharyngeal; Pet., petrous; Seg., segment; Rec., rectus; Semic., semicircular; Sig., sigmoid; Stylomast., stylomastoid; ICA, internal carotid artery.
Discussion
Microsurgical anatomy of jugular foramen was well reported previously. 2 However, description of the endoscopic endonasal anatomy of the jugular foramen is rare in the English literature. 13 14 15 16 20 The JF could be exposed in different extent, namely intracranially, foraminal, and extracranially. The report by Dallan et al 14 was the first endoscopic endonasal anatomic study on the jugular foramen. This report focused on anatomy of the infratemporal fossa and described the endoscopic endonasal route to the upper parapharyngeal portion of the internal jugular vein (extracranially JF) and ICA. However, the anatomy of the jugular foramen (intracranially and foraminal JF) was not described. Investigations by Lee et al 13 in 2012, and Komune et al 15 in 2015 were confined in the upper parapharyngeal portion of the internal jugular vein (extracranially JF). Another report by Zhang et al 16 combined endoscopic transoral and endonasal approach to the jugular foramen in cadaver. The JF was exposed intracranially, foraminal, and extracranially. Last but not least in 2017, we 6 described the anatomical basis, surgical technique, and outcomes of a group of 18 patients who underwent the endoscopic endonasal approach to the JF. This article emphasized the application of endoscopic endonasal approach to the JF. Therefore, this article did not focus detailed anatomy of the jugular foramen. Thus, our current article completed the detailed anatomic description.
Our current study describes the anatomical steps and landmarks for the EEA to the jugular foramen (foraminal and extracranially) and to compare it with the degree of exposure obtained with the lateral infratemporal fossa approach. This study presented both osseous anatomy of the JF in detailed and well-illustrated endoscopic endonasal anatomy of the JF and proximity. In addition, comparison of anterior endoscopic endonasal approach and the open lateral microsurgical approach was performed in cadavers. As far as we knew, these will add some new knowledge in literature.
Several osseous landmarks were measured in dry skulls for each approach and then compared with the respective approach during cadaveric dissections. During EEA, the mean distance from the pharyngeal orifice of the ET to foramen lacerum is 15 mm , 29 mm to the carotid foramen, and 30 mm to the jugular foramen. These are important measurements of the depth of the dissection that the surgeon should keep in mind when working in this region. During the EEA to the petrous segment of the ICA, the foramen lacerum is the most anterior landmark, and the jugular foramen is located immediately posterior to the carotid foramen.
In the present investigation, landmarks for the endoscopic approach to the jugular foramen are identified as follows: ET, levator veli palatine muscle, mandibular branch of the trigeminal nerve, foramen ovale, middle meningeal artery, foramen spinosum, SS, stylopharyngeal fascia, parapharyngeal and petrous segments of ICA, foramen lacerum, vidian canal, and inferior petrosal sinus, pterygosphenoidal fissure, as well as petroclival fissure. Some of these landmarks, such as the mandibular branch of the trigeminal nerve, levator veli palatine muscle, ET, and stylopharyngeal fascia have been reported. 13 Of aforementioned landmarks, the ET and petrous ICA are of paramount importance. We previously proposed a surgically oriented classification of the ET in five segments from anterior to posterior (medial to lateral): nasopharyngeal, pterygoid, lacerum, petrous, and osseous segments. 17 The EEA to the jugular foramen requires mobilization or transection of the cartilaginous portion of the ET. 6 21 We previously explored the anatomical relationship of the ET and petrous ICA. 17 The ICA from the upper parapharyngeal segment to paraclival segment may need to be dissected and displaced to adequately expose the jugular foramen. In addition, the foramen lacerum is a key structure in skull base surgery. We have described the foramen lacerum by defining anterior (vidian canal and pterygosphenoidal fissure), medial (pterygosphenoidal and petroclival fissures), lateral (lingual process and petrolingual ligament), and inferior walls (ET). 18
Landmarks for the infratemporal fossa Fisch type A approach to the jugular foramen include: the mastoid process of the temporal bone, styloid process, SS, transverse process of atlas, mandibular fossa, vaginal process of the tympanic part of the temporal bone, ET, facial nerve, ICA, IJV, jugular bulb, lower cranial nerves, sigmoid sinus, inferior petrosal sinus, hypoglossal canal, and occipital condyle. These landmarks have been reported in previous publications. 15 22 23 24
The EEA allows access to the jugular foramen from an anterior and medial trajectory via transnasal, transmaxillary, transpterygoid, transparapharyngeal, transpetrous, transcondylar, and transclival routes. Therefore, the anterior and medial aspect of the jugular foramen can be well exposed. 6 15 16 25 This approach also provides a good visualization of the parapharyngeal, petrous, paraclival, and cavernous sinus segments of the ICA, if necessary. 13 The ICA can be identified, protected, as well as retracted for further exposure of the lower cranial nerves. It is important to note that the ICA is a limiting factor and dissection usually proceeds medial to the petrous and parapharyngeal ICA. Medial access to the jugular bulb and foramen is enhanced with mobilization of the ICA at foramen lacerum and a contralateral transmaxillary approach. 24 26 The lower cranial nerves IX–XI are situated between the ICA and IJV at the level of the jugular foramen. This may facilitate early identification of these nerves but also poses a risk of injury. In this approach, the hypoglossal canal and the hypoglossal nerve can be identified and protected, which is one of the most adjacent structures of the jugular foramen. Compared with the open lateral microsurgical infratemporal fossa Fisch Type A approach, EEA does not require identification and transposition of the facial nerve. With the EEA, the sigmoid sinus cannot be exposed and ligated to control distal venous bleeding. Even though the EEA has the advantage of avoiding manipulation of the facial nerve compared with the lateral approach, working within the jugular foramen is more challenging because of the difficulty of controlling the lower cranial nerves and jugular vein through this approach. Also, the jugular vein is located deep to the nerves. Overclosing the ear canal results in maximum conductive hearing loss that is avoided from an anterior approach.
The infratemporal fossa Fisch Type A approach provides good visualization to the lateral aspect of the jugular foramen region. 15 25 The facial nerve is identified and transposed anteriorly to provide excellent exposure of the jugular foramen. Fallopian bridge technique 27 described by Pensak and Jackler in 1997 was a good choice for some tumors originated in JF in selected cases. The parapharyngeal segment of the ICA and IJV are identified and controlled. The sigmoid sinus is ligated to control major venous bleeding.
The EEA and lateral microsurgical approach to the jugular foramen each have distinct advantages and limitations ( Table 3 ). Therefore, the selection of the approach to the jugular foramen mainly depends on the location and extension of the pathology. EEA is a feasible alternative route for lesions involving anterior and medial aspects of the jugular foramen, particularly indicated for lesions that extend from the foramen lacerum to the jugular foramen, such as chondrosarcomas, or from the lower clivus to the jugular foramen, such as chordomas. The additional access provided by the contralateral transmaxillary approach has not been fully explored anatomically. 23 24
Table 3. Comparison of endoscopic endonasal approach and Infratemporal fossa approach Fisch type A.
| Exposure and manipulation of facial nerve | Exposure and manipulation of ICA | Exposure and manipulation of cranial nerves IX–XII | Exposure and manipulation of IJV | Anatomical relations of IJV and cranial nerves IX–XII | |
|---|---|---|---|---|---|
| EEA | No | Parapharyngeal, petrosal, paraclival segment | Difficult | Difficult | IJV is located deep to the cranial verves |
| IFTA | Yes, anterior transposition | Parapharyngeal, upper cervical, petrosal segment partially or completely | Yes | Yes, easy to ligation | Cranial nerves are located deep to the IJV |
Abbreviations: EEA, endoscopic endonasal approach; ICA, internal carotid artery; IFTA, infratemporal fossa approach Fisch type A; IJV, internal jugular vein.
Limitations
First, in current report, we did not operate any pathology with either approach and the type and extent of the tumor may significantly affect what we can safely do. Second, we did not calculate the time that each approach has taken, which would be helpful to the reader.
Conclusion
The EEA to the jugular foramen is anatomically feasible and requires mobilization of the ICA to provide access to the anterior and medial aspects of the jugular foramen. The lateral infratemporal approach requires facial nerve transposition to provide access to the lateral and posterior parts of the jugular foramen. A deep understanding of the complex anatomy of this region is paramount for safe and effective surgery of the jugular foramen. Both techniques may be complementary considering the different regions of the jugular foramen best accessed with each approach.
Funding Statement
Funding None.
Conflict of Interest None declared.
Note
This study has been presented at 26th Annual Meeting North American Skull Base Society at Fairmont Scottsdale Princess Scottsdale, Arizona, on February 12–14, 2016.
References
- 1.Griessenauer C J, McGrew B, Matusz P, De Caro R, Loukas M, Tubbs R S. Surgical approaches to the jugular foramen: a comprehensive review. J Neurol Surg B Skull Base. 2016;77(03):260–264. doi: 10.1055/s-0035-1567863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rhoton A L., JrJugular foramen Neurosurgery 200047(3, Suppl):S267–S285. [DOI] [PubMed] [Google Scholar]
- 3.Constanzo F, Coelho Neto M, Nogueira G F, Ramina R. Microsurgical anatomy of the jugular foramen applied to surgery of glomus jugulare via craniocervical approach. Front Surg. 2020;7:27. doi: 10.3389/fsurg.2020.00027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ramina R, Maniglia J J, Fernandes Y B, Paschoal J R, Pfeilsticker L N, Coelho Neto M.Tumors of the jugular foramen: diagnosis and management Neurosurgery 200557(1, Suppl):59–68. [DOI] [PubMed] [Google Scholar]
- 5.Luzzi S, Giotta Lucifero A, Del Maestro M et al. Anterolateral approach for retrostyloid superior parapharyngeal space schwannomas involving the jugular foramen area: a 20-year experience. World Neurosurg. 2019;132:e40–e52. doi: 10.1016/j.wneu.2019.09.006. [DOI] [PubMed] [Google Scholar]
- 6.Vaz-Guimaraes F, Nakassa A CI, Gardner P A, Wang E W, Snyderman C H, Fernandez-Miranda J C. Endoscopic endonasal approach to the ventral jugular foramen: anatomical basis, technical considerations, and clinical series. Oper Neurosurg (Hagerstown) 2017;13(04):482–491. doi: 10.1093/ons/opx014. [DOI] [PubMed] [Google Scholar]
- 7.de Lara D, Ditzel Filho L F, Prevedello D Met al. Endonasal endoscopic approaches to the paramedian skull base World Neurosurg 201482(6, Suppl):S121–S129. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Q, Lv H, Wang Z, Guo H, Li M. Endoscopic transoral approach for extracranial hypoglossal schwannoma. ORL J Otorhinolaryngol Relat Spec. 2011;73(05):282–286. doi: 10.1159/000330270. [DOI] [PubMed] [Google Scholar]
- 9.Zimmer L A, Hirsch B E, Kassam A, Horowitz M, Snyderman C H. Resection of a recurrent paraganglioma via an endoscopic transnasal approach to the jugular fossa. Otology & neurotology: official publication of the American Otological Society, American Neurotology Society. European Academy of Otology and Neurotology. 2006;27:398–402. doi: 10.1097/00129492-200604000-00017. [DOI] [PubMed] [Google Scholar]
- 10.Fernandez-Miranda J C, Morera V A, Snyderman C H, Gardner P.Endoscopic endonasal transclival approach to the jugular tubercle Neurosurgery 201271(1, Suppl Operative):146–158. [DOI] [PubMed] [Google Scholar]
- 11.Taniguchi M, Kato A, Taki T et al. Endoscope assisted removal of jugular foramen schwannoma; report of 3 cases. Minim Invasive Neurosurg. 2005;48(06):365–368. doi: 10.1055/s-2005-915631. [DOI] [PubMed] [Google Scholar]
- 12.Samii M, Alimohamadi M, Gerganov V. Endoscope-assisted retrosigmoid infralabyrinthine approach to jugular foramen tumors. J Neurosurg. 2016;124(04):1061–1067. doi: 10.3171/2015.3.JNS142904. [DOI] [PubMed] [Google Scholar]
- 13.Lee D L, McCoul E D, Anand V K, Schwartz T H. Endoscopic endonasal access to the jugular foramen: defining the surgical approach. J Neurol Surg B Skull Base. 2012;73(05):342–351. doi: 10.1055/s-0032-1322796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dallan I, Bignami M, Battaglia P, Castelnuovo P, Tschabitscher M.Fully endoscopic transnasal approach to the jugular foramen: anatomic study and clinical considerations Neurosurgery 201067(3, Suppl Operative):ons1–ons7. [DOI] [PubMed] [Google Scholar]
- 15.Komune N, Komune S, Matsushima K, Rhoton A L., Jr Comparison of lateral microsurgical preauricular and anterior endoscopic approaches to the jugular foramen. J Laryngol Otol. 2015;129 02:S12–S20. doi: 10.1017/S0022215114002321. [DOI] [PubMed] [Google Scholar]
- 16.Zhang X, Tabani H, El-Sayed I et al. Combined endoscopic transoral and endonasal approach to the jugular foramen: a multiportal expanded access to the clivus. World Neurosurg. 2016;95:62–70. doi: 10.1016/j.wneu.2016.07.073. [DOI] [PubMed] [Google Scholar]
- 17.Liu J, Pinheiro-Neto C D, Fernandez-Miranda J C et al. Eustachian tube and internal carotid artery in skull base surgery: an anatomical study. Laryngoscope. 2014;124(12):2655–2664. doi: 10.1002/lary.24808. [DOI] [PubMed] [Google Scholar]
- 18.Wang W H, Lieber S, Mathias R N et al. The foramen lacerum: surgical anatomy and relevance for endoscopic endonasal approaches. J Neurosurg. 2018:1–12. doi: 10.3171/2018.6.JNS181117. [DOI] [PubMed] [Google Scholar]
- 19.Fisch U, Fagan P, Valavanis A. The infratemporal fossa approach for the lateral skull base. Otolaryngol Clin North Am. 1984;17(03):513–552. [PubMed] [Google Scholar]
- 20.Wang M, Chae R, Shehata Joseph et al. Comparative analysis of the subtonsillar, far-lateral, extreme-lateral, and endoscopic far-medial approaches to the lower clivus: an anatomical cadaver study. World Neurosurg. 2019;127:e1083–e1096. doi: 10.1016/j.wneu.2019.04.048. [DOI] [PubMed] [Google Scholar]
- 21.Simal-Julián J A, Miranda-Lloret P, Beltrán-Giner A, Plaza-Ramirez E, Botella-Asunción C. Full endoscopic endonasal extreme far-medial approach: eustachian tube transposition. J Neurosurg Pediatr. 2013;11(05):584–590. doi: 10.3171/2013.1.PEDS12462. [DOI] [PubMed] [Google Scholar]
- 22.Goldenberg R A.Surgeon's view of the skull base from the lateral approach Laryngoscope 198494(12 Pt 2):361–21. [DOI] [PubMed] [Google Scholar]
- 23.Roche P H, Mercier P, Sameshima T, Fournier H D. Surgical anatomy of the jugular foramen. Adv Tech Stand Neurosurg. 2008;33:233–263. doi: 10.1007/978-3-211-72283-1_6. [DOI] [PubMed] [Google Scholar]
- 24.Katsuta T, Rhoton A L, Jr, Matsushima T. The jugular foramen: microsurgical anatomy and operative approaches. Neurosurgery. 1997;41(01):149–201. doi: 10.1097/00006123-199707000-00030. [DOI] [PubMed] [Google Scholar]
- 25.Jacquesson T, Berhouma M, Tringali S, Simon E, Jouanneau E. Which routes for petroclival tumors? A comparison between the anterior expanded endoscopic endonasal approach and lateral or posterior routes. World Neurosurg. 2015;83(06):929–936. doi: 10.1016/j.wneu.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 26.Patel C R, Wang E W, Fernandez-Miranda J C, Gardner P A, Snyderman C H. Contralateral transmaxillary corridor: an augmented endoscopic approach to the petrous apex. J Neurosurg. 2018;129(01):211–219. doi: 10.3171/2017.4.JNS162483. [DOI] [PubMed] [Google Scholar]
- 27.Pensak M L, Jackler R K. Removal of jugular foramen tumors: the fallopian bridge technique. Otolaryngol Head Neck Surg. 1997;117(06):586–591. doi: 10.1016/S0194-59989770037-8. [DOI] [PubMed] [Google Scholar]


