Abstract
Objectives
The aim of this cross-sectional study was to apply a novel software to measure and compare levels of nonverbal synchrony, as a potential indicator of communication quality, in video recordings of racially-concordant and racially-discordant oncology interactions. Predictions include that the levels of nonverbal synchrony will be greater during racially-concordant interactions than racially-discordant interactions, and that levels of nonverbal synchrony will be associated with traditional measures of communication quality in both racially-concordant and racially-discordant interactions.
Design
This is a secondary observational analysis of video-recorded oncology treatment discussions collected from 2 previous studies.
Setting
Two National Cancer Institute-designated Comprehensive Cancer Centers and another large urban cancer center.
Participants
Participants from Study 1 include 161 White patients with cancer and 11 White medical oncologists. Participants from Study 2 include 66 Black/African-American patients with cancer and 17 non-Black medical oncologists. In both studies inclusion criteria for patients was a recent cancer diagnosis; in Study 2 inclusion criteria was identifying as Black/African American.
Main outcome measures
Nonverbal synchrony and communication quality.
Results
Greater levels of nonverbal synchrony were observed in racially-discordant interactions than in racially-concordant interactions. Levels of nonverbal synchrony were associated with indicators of communication quality, and these associations were more consistently found in racially-discordant interactions.
Conclusion
This study advances clinical communication and disparities research by successfully applying a novel approach capturing the unconscious nature of communication, and revealing differences in communication in racially-discordant and racially-concordant oncology interactions. This study highlights the need for further exploration of nonverbal aspects relevant to patient-physician interactions.
Keywords: nonverbal synchrony, racial disparities, communication quality, oncology, video-recorded, motion energy analysis
Introduction
High-quality patient-physician communication is associated with better patient psychosocial and medical outcomes, as well as greater treatment adherence across many care settings, including in oncology.1-4 Conversely, poor patient-physician communication can lead to poorer outcomes, including discontinuity of care, problems with patient safety, patient dissatisfaction, and higher individual, organizational, and societal costs. 4 Unfortunately, the quality of clinical communication is also associated with patient race, such that Black patients more often experience lower-quality communication than White patients.5-9 For example, research shows that physicians (including oncologists) tend to be less patient-centered, 6 more verbally dominant, 10 more contentious, 8 and provide less information 11 during interactions with Black patients; and Black patients tend to ask fewer questions 5 and are less likely to participate in decision making than their White counterparts.7,12,13 These communication disparities likely contribute to the well-documented racial inequities at every level of healthcare, including in oncology care, and the poorer health and greater mortality rates among Black relative to White patients.5,11,14
Researchers have focused on Black-White disparities in communication during clinical interactions with the goal of providing important information for training and interventions that would improve the quality of communication in racially-discordant, dyadic medical interactions.15-17 However, there are several limitations to prior research which we summarize throughout this section. First, researchers generally use global assessments of clinical interactions, such as affect (eg, warm/friendly), or patient-centeredness, but rarely examine important discrete nonverbal behaviors, such as eye gaze and leaning.8,18 While global assessments are important for assessing communication quality, they provide little information about specific behaviors that could be modified through interventions. Second, with a few exceptions,19-21 researchers who have studied the content of medical interactions have generally studied verbal communication (eg, patient active participation, physicians’ patient-centeredness), ignoring nonverbal communication, despite its critical role in creating, defining, and managing interpersonal relationships, including patient-physician relationships. 22
Research has consistently shown associations between patient-physician nonverbal communication and patient outcomes including relational rapport, trust, satisfaction, recall, adherence, symptom resolution, understanding, and long-term health improvements. 23 Further, research has demonstrated the influence of physician eye contact/gaze on physicians’ patient-centeredness, 24 rapport with patients, 25 patients’ perceptions of empathy, 26 and awareness of patients’ psychological problems. 27 Our study team recently observed that in an oncology setting, patients and oncologists smile, orient themselves to 1 another, and lean in toward 1 another at similar rates of frequency, but oncologists are more likely than patients to display an open posture. 21 Oncologists tend to interrupt patients more than patients interrupt oncologists, and oncologists spend more time speaking compared to patients. We also see that patients exhibit continuer behaviors (eg, head nods) to a greater extent than oncologists. 21
A third limitation of prior research in this area is that researchers have largely treated behaviors of each individual as if they occur independently, even though medical interactions are, by definition, dynamic and interdependent. Again with a few exceptions,21,28,29 this is mainly because researchers lack the tools to analyze the dynamic nature of communication by assessing how behaviors change and influence 1 another over time. 23 Finally, although there is general agreement that racial concordance and discordance play a significant role in physician-patient communication, there is a relative dearth of studies that compare racially-concordant and discordant medical interactions, using the same objective communication measures of what transpires during these interactions. 9
The current study extends prior research and fills important gaps in the clinical communication literature by investigating the dynamic, interdependent, unconscious nature of nonverbal interpersonal communication, during oncology interactions with Black patients in racially-discordant interactions and White patients in racially-concordant interactions. We employed a novel software that allowed comparisons between patient-physician nonverbal synchrony during oncology interactions that involved Black patients in racially-discordant interactions and White patients in racially-concordant interactions. Nonverbal synchrony is the coordination of movement between individuals during an interaction. 30 Nonverbal synchrony involves behavioral motion and is a dynamic and jointly determined phenomenon. It represents a form of matching on nonverbal behaviors between 2 individuals. For example, eye gaze by patients toward physicians is matched by eye gaze and/or postural shifts by physicians toward patients. This matching is not necessarily simultaneous or the same behavior, but it involves a meaningful temporal association between similar kinds of motion and exhibits a pattern of coordinated back-and-forth behaviors.31-33 For example, if 1 individual in an interaction shakes their head while another individual waves their hand, they are, together, exhibiting nonverbal synchrony. 32 Further, because human communication rarely occurs perfectly in time (as if looking in a mirror), as part of investigating nonverbal synchrony, use of this software also allowed us to identify the leader and follower in the interactions, or whether an individual is behaviorally leading or responding. This is akin to ballroom dancing where 1 partner leads while the other follows.
Prior research shows that although nonverbal synchrony is often largely unconscious, unintentional, and effortless, 34 it can be predicted by pre-interaction attitudes 35 and has post-interaction consequences. 36 People synchronize more with those with whom they have existing positive relationships, 37 those with whom they want to develop positive relationships, 38 and those whom they trust. 35 In a laboratory-based study, individuals with higher implicit bias favoring their own race synchronized more with an avatar of their own race than with an avatar of a different race. 34 Higher levels of nonverbal synchrony result in more subsequent positive affect and liking, 36 perceptions of similarity, closeness, rapport with the interaction partner, and collaborative problem solving.35,39,40 Relevant to clinical outcomes, nonverbal synchrony positively influences therapeutic processes, 41 cooperation, 42 adherence, 39 and memory of what transpired during an interaction.43,44 However, recent studies have challenged prior findings about the positive role of nonverbal synchrony in clinical interactions. 45 These studies suggest that nonverbal synchrony may not be exclusively associated with positive aspects of the relationship 46 ; rather, they may also indicate efforts to maintain or repair strained relationships.46,47
In this study, we examined the dynamics of nonverbal behaviors by applying a novel software to naturally-occurring racially-concordant oncology interactions with White patients and racially-discordant oncology interactions with Black patients all occurring in major urban cancer centers. First, we investigated whether nonverbal synchrony differs in either strength or valence in racially-discordant patient-physician interactions compared to racially-concordant patient-physician interactions. Our first hypothesis was that the levels of nonverbal synchrony will be greater during racially-concordant interactions than racially-discordant interactions. We also examined associations between nonverbal synchrony and other indicators of communication quality during these interactions. These included observers’ independent ratings of physicians’ patient-centered communication, physician and patient individual affect, and relational rapport between physicians and patients. This allowed us to examine the convergent validity of this new way of measuring clinical communication (ie, nonverbal synchrony) with more traditional measures of clinical communication quality. Our second hypothesis was that levels of nonverbal synchrony will be positively associated with the measures of physician patient-centered communication, patient and physician affect, and patient-physician relational rapport. This would be true in both racially-concordant and racially-discordant oncology interactions.
Method
Participants and Procedures of the Parent Studies
Data were taken from 2 National Cancer Institute (NCI)-funded studies. Study 1 was conducted at 2 urban NCI-designated comprehensive cancer centers between April 2002 and March 2006, was an investigation of how patient-physician communication influences patient treatment decisions, and largely included White patients and White oncologists (ie, racially-concordant interactions). 48 Study 2 was conducted at 1 of the same cancer centers as in Study 1 plus another large urban cancer center in the same city between April 2012 and December 2014. Study 2 investigated associations between communication and outcomes during racially-discordant oncology interactions, and specifically included Black patients and their non-Black oncologists (ie, racially-discordant interactions). 15 Patients of participating physicians were selected and recruited consecutively based on eligibility criteria. Both studies collected patient and physician self-report data (including self-identified race) and video-recordings of their clinical interactions. 49 Only the patients and physicians who provided written consent to allow their self-report and video-recorded data to be used in secondary analyses were included in the current study. All study procedures for the current cross-sectional secondary analysis were approved by Wayne State University’s Behavioral Institutional Review Board (IRB# 044716B3E). The reporting of this study conforms to STROBE guidelines. 50 All patient and physician data reported in this article are de-identified.
Current Study Procedures
For the video-recorded data, we used the complete video-recorded clinical interactions to assess physicians’ patient-centered communication, five-minute segments of the interactions to assess nonverbal synchrony, and one-minute segments of the interactions to assess patient and physician affect and relational report. To obtain the 5-minute segments (used to assess nonverbal synchrony), video-recordings were edited, regardless of the length of the interaction, into 5-minute segments. For example, if an interaction was 23 minutes long, it was edited to have four five-minute segments and one three-minute segment. To obtain the one-minute segments (used to assess affect and relational rapport), we divided the complete recorded interactions into 5 equal time segments. Then, we extracted the first minute from each segment that included the patient and the physician. This resulted in five one-minute segments per interaction, regardless of the length of the interaction. Physical exams during the interactions were excluded in selecting the five- and one-minute segments.
Assessing Nonverbal Synchrony
We assessed nonverbal synchrony using Motion Energy Analysis (MEA) 51 software. This provided time series data for the amount of motion observed. MEA is an automated method that continuously monitors the amount of change in pre-defined regions of interest, thus quantifying movement occurrence. We considered each individual in the interaction as 1 region of interest to capture full body movement. We quantified nonverbal synchrony by deriving scores using windowed cross-correlation matrices to obtain nonverbal synchrony scores for each interaction. 52 Because nonverbal synchrony tends to ebb and flow during conversations, we used windowed cross-correlation to measures the changing synchronization that occurs in the interaction by comparing small sections of time at different time lags. 53 By identifying multiple smaller sections at multiple different time lags, windowed cross-correlation provides an estimate of synchronization between systems which do not have a constant lag (in this instance, 2 people having a discussion). Figure 1 shows windowed cross-correlation results from the time series data. Nonverbal synchrony scores are jointly determined phenomena that represent amounts and direction of influence (ie, who is “leading” in the interaction, similar to leading and following in dancing) of synchronous movement within interactions.
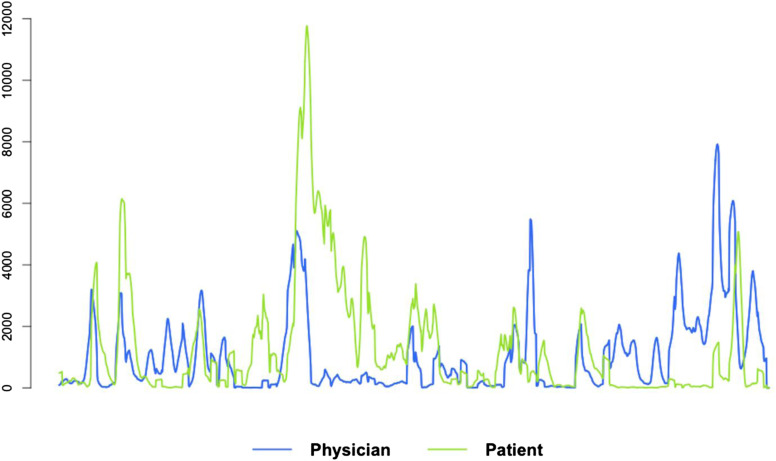
Figure 1.
Example of time-series of movement extracted with motion energy analysis.
Observed Indicators of Communication Quality
Patient-Centered Communication. Trained observers observed and rated full video-recorded interactions for physicians’ patient-centered communication. Observers had a minimum of a bachelor’s degree in social or behavioral science, self-identified as either Black or White, and were employed research assistants in our research lab. They were trained to observe and rate videos using rigorous training methods.15,21,54,55 Observers applied a global scale of physicians’ patient-centered communication to measure informativeness (eg, “the doctor thoroughly explained everything to the patient”); supportiveness (eg, “the doctor made the patient feel completely at ease during the consultation”); and partnership building (eg, “the doctor encouraged the patient to express concerns and worries”).8,15 At least 2 observers rated patient-centered communication (3 observers rated 15% of interactions to ensure continued reliability); inter-rater reliability was acceptable (intra-class correlation coefficient = .57-.74, P’s<.05). Each physician’s patient-centered communication score was the average of observers’ ratings.
Individual Affect and Relational Rapport. The 1-minute segments were observed in random order and rated by naïve observers who were instructed to provide their ratings for individual patient and physician affect and joint relational rapport. Naïve observers were racially-diverse research volunteers and were mainly students from Wayne State University. Ratings were divided into positive (warm, attentive, cheerful) and negative (tense, disagreeable, upset, sad) affect, and positive (liking, attentive, coordinated, trusting) and negative (cold, distant, disconnected) relational rapport.18,56
Data Analysis
We used linear mixed-effects models to analyze the influence of interaction-level racial concordance and discordance on nonverbal synchrony values. 57 Patient and physician nonverbal synchrony values from each five-minute video-recorded segment were nested within the interaction, with an additional random effect by physician to account for variation between interactions and individual physicians. MEA output was used to obtain bivariate time series of motion (1 time series for the patient and 1 for the physician; see Figure 1). Flat lines indicate no movement; spikes and peaks represent movement. We assessed nonverbal synchrony occurring within a 4-second time frame (ie, patient leading/lagging up to 2 s or physician leading/lagging up to 2 s). Because nonverbal synchrony between 2 individuals is a complex phenomenon, we employed 7 metrics to quantify different aspects of nonverbal synchrony between patients and physicians.
First, we examined global synchrony (mean absolute Fisher’s Z) to estimate average strength in synchronized movement across the interaction. Nonverbal synchrony scores were obtained for the segments of the interaction when the patient was leading (patient’s mean absolute Fisher’s Z) and when the physician was leading (physician’s mean absolute Fisher’s Z). We also measured peak synchrony (how synchronous the physician and patient were during their highest moments of time-lagged synchronous behavior) and peak lag (the extent to which the interaction was led by the patient vs the physician). Lastly, we assessed variability of peak synchrony and peak lag, which are estimates of varying strength of synchrony and turn taking behaviors, respectively.
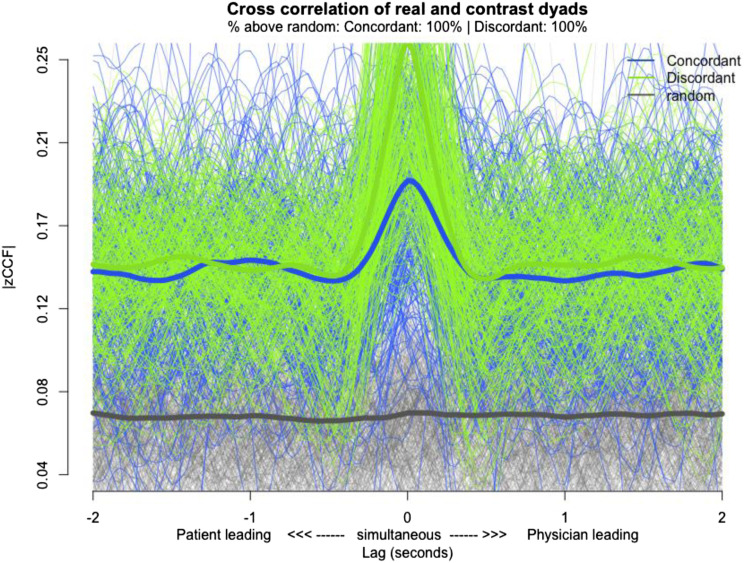
Humans often repeat behaviors across conversations (eg, smiling or head nodding), so time series data from human motion may show spurious nonverbal synchrony values even when no nonverbal synchrony is present. This pseudo-synchrony is problematic because hypothesis-testing of synchrony between any 2 times series assumes the time series are in synch with 1 another. Time series pairs that show pseudo-synchrony may lead to false conclusions. To avoid this, surrogate analysis may be used as a reliable measure for detecting real synchrony vs pseudo-synchrony. In a surrogate analysis framework, a large number of pseudo-pairs are generated by randomly matching patients’ data from 1 interaction with physicians’ data from a different interaction (ie, an interaction between a patient and physician that did not actually occur).53,58 Nonverbal synchrony metrics are then assessed on these pseudo pairs and compared to nonverbal synchrony metrics obtained from actual pairs. A significant difference indicates that observed nonverbal synchrony metrics in actual pairs are higher than expected by chance. Our surrogate analysis showed observed nonverbal synchrony metrics were significantly higher than chance; Δ|zCCF| = .08, z = 3.43, P < .001. This is displayed in the lagplot graph in Figure 2.
Figure 2.
Surrogate analysis lagplot graph.
Results
Sociodemographic characteristics of patients and physicians are reported in Table 1. Study 1 included only White patients in racially-concordant interactions (n = 161 patients; n = 17 physicians). Study 2 included only Black patients in racially-discordant interactions (n = 66 patients; n = 11 physicians).
Table 1.
Participant Demographics.
| Demographic | Racially-concordant interactions | Racially-discordant interactions | ||
|---|---|---|---|---|
| Patient | Physician | Patient | Physician | |
| N | 161 | 17 | 66 | 11 |
| Sex | ||||
| Female | 69 | 0 | 66 | 5 |
| Male | 92 | 17 | 0 | 6 |
| Mean age (SD) | 61.59 (12.92) | 44.69 (7.18) | 58.11 (10.62) | 48.03 (10.92) |
| Race | ||||
| Asian or Pacific Islander | 0 | 0 | 0 | 4 |
| Black or african-american | 0 | 0 | 66 | 0 |
| White | 161 | 17 | 0 | 5 |
| Other | 0 | 0 | 0 | 2 |
| Highest education | ||||
| Less than high school | 18 | 0 | 14 | 0 |
| Completed high school/Some college, technical, or trade school | 88 | 0 | 6 | 0 |
| Completed college, technical, or trade school | 39 | 0 | 37 | 0 |
| Completed graduate school | 11 | 17 | 9 | 11 |
| Patient household Income | ||||
| Less than $20,000 | 28 | — | 31 | — |
| $20,000 - 39 999 | 24 | — | 20 | — |
| $40,000 - $59,999 | 30 | — | 6 | — |
| $60,000 + | 58 | — | 10 | — |
| Patient employment status | — | |||
| Retired | 66 | — | 24 | — |
| Full-time | 28 | — | 14 | — |
| Part-time | 9 | — | 1 | — |
| On leave | 18 | — | 13 | — |
| Unemployed | 4 | — | 16 | — |
| Other (eg, student, homemaker, disability) | 36 | — | 0 | — |
| Physician years in practice | ||||
| Less than 1 Year | — | 0 | — | 6 |
| 1–2 Years | — | 1 | — | 0 |
| 3–5 Years | — | 2 | — | 1 |
| 6–10 Years | — | 1 | — | 1 |
| More than 10 Years | — | 12 | — | 3 |
For hypothesis 1, we predicted that the levels of nonverbal synchrony will be greater for racially-concordant interactions than for racially-discordant interactions. Findings (Table 2) showed the opposite, with greater levels of global synchrony and greater peak synchrony observed during the racially-discordant interactions than racially-concordant interactions. We also found that greater global synchrony occurred in the racially-discordant interactions when the patient rather than the physician was leading. However, global synchrony was the same in racially-concordant interactions regardless of who was leading (Table 2).
Table 2.
Nonverbal Synchrony Metrics by Interaction Type.
| Nonverbal synchrony metric | Racially-concordant interaction mean | Racially-discordant interaction mean | Diff | t | df | P | d |
|---|---|---|---|---|---|---|---|
| Global synchrony | .13 | .16 | .03 | 15.61 | 205.45 | <.001 | 2.18 |
| Global synchrony when the physician is leading | .13 | .15 | .03 | 15.00 | 201.43 | <.001 | 2.11 |
| Global synchrony when the patient is leading | .13 | .20 | .08 | 33.19 | 206.27 | <.001 | 4.71 |
| Mean peak synchrony | .24 | .27 | .03 | 7.46 | 171.5 | <.001 | 1.29 |
| SD peak synchrony | .11 | .14 | .03 | 13.05 | 159.08 | <.001 | 2.17 |
| Mean peak lag | .03 | .04 | .01 | .42 | 176.28 | .675 | .01 |
| SD peak lag | 5.27 | 6.18 | .91 | 3.47 | 178.54 | .006 | .69 |
| Leading-difference patient vs physician | .00 | .05 | .05 | 37.21 | 1158 | <.001 | 2.22 |
For hypothesis 2, we predicted that levels of nonverbal synchrony would be positively associated with indicators of communication quality including: levels of physicians’ patient-centered communication, patient and physician affect, and patient-physician relational rapport in both racially-discordant and racially-concordant interactions. As summarized in Table 3, these associations were more consistently found in the racially-discordant interactions.
Table 3.
Relationships between Individual Affect, Relational Rapport and Nonverbal Synchrony Metrics.
| Nonverbal Synchrony Metric | Racially-Concordant Interactions | |||||
|---|---|---|---|---|---|---|
| Patient | Physician | Dyad | ||||
| Positive Affect | Negative Affect | Positive Affect | Negative Affect | Positive Rapport | Negative Rapport | |
| Global synchrony | β = −.001 t (1163.8) = −2.3, P = .03 | |||||
| Global synchrony when the physician is leading | β = −.001 t (1141.6) = −2.4 P = .02 | |||||
| Global synchrony when the patient is leading | β = −.002 t (1149.0) = −2.2, P = .03 | β = −.004 t (1106.4) = −2.0, P =. 04 | ||||
| Racially-discordant interactions | ||||||
| Global synchrony | β = .003 t (935.5) = 4.2, P < .001 | β = − .002 t (1046.9) = −3.0, P = .003 | β = .002 t (742.7) = 4.1, P < .001 | β = − .004 t (981.4) = −4.1, P < .001 | ||
| Global synchrony when the physician is leading | β = .003 t (995.1) = 4.8, P < .001 | β = − .003 t (1073.2) = −3.7, P < .001 | β = .003 t (852.0) = 4.4, P < .001 | β = − .005 t (1045.6) = −4.4, P < .001 | ||
| Global synchrony when the patient is leading | β = .004 t (959.7) = 4.0, P < .001 | β = − .003 t (1043.9) = −2.5, P = .01 | β = .006 t (59.5) = 2.7, P = .01 | β = .003 t (795.4) = 3.9, P < .001 | β = − .007 t (1000.9) = −4.3, P < .001 | |
Bold = positive association.
Underline = negative association.
Regarding the association between nonverbal synchrony and physicians’ patient-centered communication, findings showed a significant association between peak synchrony and physicians’ patient-centered communication in racially-discordant interactions (β = −.004, t (272.8) = 2.04, P =.04). However, no significant associations were found between any of the nonverbal synchrony metrics and physicians’ patient-centered communication in the racially-concordant interactions.
Further, findings showed that in racially-discordant interactions, global synchrony was positively associated with patients’ positive affect and positive patient-physician rapport, and negatively associated with patients’ negative affect and negative patient-physician rapport. When the physician was leading in these interactions, global synchrony was positively associated with patients’ positive affect and positive patient-physician rapport and negatively associated with patients’ negative affect and negative patient-physician rapport. When the patient was leading, global synchrony was also positively associated with both patients’ and physicians’ positive affect and positive patient-physician rapport, and negatively associated with patients’ negative affect and negative patient-physician rapport.
In the racially-concordant interactions, however, global synchrony was only associated with ratings of negative affect and relational rapport. Global synchrony was negatively associated with negative affect, overall and irrespective of who was leading. When the patient was leading, global synchrony was negatively associated with negative patient-physician rapport.
Discussion
This study extends prior research on racial disparities in clinical communication by using a novel approach that captures the dynamic, interdependent, unconscious nature of nonverbal interpersonal communication, and revealing previously undiscovered differences in patient-physician communication during oncology interactions with Black patients in racially-discordant interactions and White patients in racially-concordant interactions. Measuring nonverbal synchrony in medical interactions represents a markedly different way of studying communication from more traditional methods, and we show that the substantial amount of convergence in this and traditional assessments of the quality of this naturally occurring medical interactions. This speaks to the convergent validity of these very different levels of measurement and opens the door for more ways of objectively determining how well physician and patients are communicating.
Considerable research has shown that unconscious processes affect the outcome of human interactions in logical and theoretically coherent ways.56,59,60 Our findings may suggest that among Black patients and non-Black physicians unconscious processes were operating to overcome potential race and cultural barriers by “matching” their behaviors, and thus creating greater nonverbal synchrony. Such motivations may have been absent in racially-concordant interactions, where these barriers do not exist. Bergsieker and colleagues 61 (2010) found that patients from different racial groups have divergent goals in the impressions they aim to make in clinical interactions. They concluded that patients who are racial minorities tend to seek to be respected and be seen as competent by their providers, compared to patients who are White who tend to seek to be liked and viewed as moral by their providers. They also observed divergent behavioral strategies undertaken by patients to achieve the desired impression. There is also evidence that individuals with higher levels of implicit racial bias may work harder at controlling their bias during inter-racial interactions, and, although we did not assess that influence of implicit bias in this study, may explain the differences observed. 62 Our study team’s previous research on verbal clinical communication showed Black patients with higher levels of group-based medical mistrust in physicians had more negative evaluations of their non-Black physicians. We have also reported that Black patients with higher levels of previous discrimination were more verbally active while communicating with their non-Black physicians, which taken with the findings presented here, may suggest that Black patients may use verbal and nonverbal strategies to gain control in their interactions with non-Black physicians. 54
Ideally, racial discordance or concordance should not affect the quality of communication in oncology interactions. The reality is, of course, quite different; and this study has shown that differences exist even when the communication involves nonverbal behaviors that almost certainly exist outside conscious or intentional control. While these behaviors are nonverbal and unconscious, they converge with other aspects of physician-patient communication, especially in racially-discordant medical interactions. Thus, the possibility exists for multi-level interventions that address ways to improve the quality of medical interactions. This could help mitigate the well-documented racial disparities in clinical communication, and perhaps in tandem with other efforts, help reduce disparities in cancer treatment and mortality.29,54
Findings from this study must be considered within its limitations. First, because this dynamic analysis of medical interactions was the first of its kind, we focused our analyses exclusively on nonverbal synchrony. Future research should also include predictors of nonverbal synchrony (eg, demo- and psycho-graphics, racial attitudes), expand upon its consequences (eg, treatment decisions), and integrate nonverbal synchrony with the topics being discussed in medical interactions (eg, diagnosis, prognosis, treatment). Second, our data were all based on patients’ initial appointments with an oncologist. Future research should expand on what we have established here by investigating any changes over time for Black and White patients and their physicians.41,45 This does not, however, diminish the importance of nonverbal synchrony in the early stages of potentially difficult clinical interactions, as they may well set the template and tone for subsequent interactions. Third, although these data allowed us to observe an important behavioral pattern that few researchers have been able to observe, the data are somewhat dated and may have prevented us from observing any influence of more recent race-focused medical communication training. Fourth, due to the fact that this was a secondary analysis, we had an imbalance in gender of patients and physicians both within and between studies. Similarly, although we were able to make direct comparison between racially-concordant and racially-discordant patient-physician interactions (something few studies have been able to do) 29 we were unable to examine the behaviors of Black patients and Black physicians in racially-concordant interactions; or racially-discordant interactions between White patients and Black physicians. This limitation reflects the fact that so few physicians in the United States self-identify as Black or African American, especially in oncology where less than 3% of practicing oncologists identify as Black or African American. 9
One very important part of future efforts would be to see if the differences found in nonverbal synchrony across racially-discordant and concordant interactions and the associations between the ways we assessed the quality of clinical communication replicate in other kinds of medical interactions, and in more recent datasets. If they do, then research can proceed on why these differences occur and perhaps ways to remediate them. If, for example, physicians adapting their nonverbal behavior to the behavior of their Black patients does produce better communication in racially-discordant medical interactions, this may lead to interventions designed to improve the quality of clinical communication. We also encourage future researchers to investigate concordance and discordance of other important factors such as gender, and how the intersection of multiple factors may influence nonverbal synchrony and associated outcomes.
Conclusions
This study highlights the need for further exploration of nonverbal aspects relevant to patient-physician interactions. Although medical interactions by their nature involve interdependent behaviors that change over the course of these interactions, there is a dearth of research assessing this process. This study demonstrated that it is possible to capture such behaviors in the form of nonverbal synchrony. Nonverbal synchrony may operate largely outside of the awareness of individuals, but our data indicate that it may have an adaptive function in clinical encounters involving patients and physicians whose initial meeting is marred by a healthcare system fraught with an abhorrent history of racism. 63
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute of Minority Health and Health Disparities grant R21MD011766-01 (LMH), National Cancer Institute grant R01CA75003 (TLA), National Cancer Institute grant U54CA153606 (TLA).
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author’s Note: A preliminary version of this paper was presented as a podium presentation to the American Society of Clinical Oncology’s Quality Care Symposium in San Diego, California in September 2019.
ORCID iD
Lauren M. Hamel https://orcid.org/0000-0002-8910-7079
References
- 1.Epstein RM, Street RL. Patient-Centered Communication in Cancer Care. Bethsda, Md: U.S. Department of Health and Human and Services National Institutes of Health; 2007. [Google Scholar]
- 2.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359-364. [DOI] [PubMed] [Google Scholar]
- 3.Zachariae R, Pedersen CG, Jensen AB, Ehrnrooth E, Rossen PB, von der Maase H. Association of perceived physician communication style with patient satisfaction, distress, cancer-related self-efficacy, and perceived control over the disease. Br J Cancer. 2003;88(5):658-665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vermeir P, Vandijck D, Degroote S, et al. Communication in healthcare: A narrative review of the literature and practical recommendations. Int J Clin Pract. 2015;69(11):1257-1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eggly S, Harper FW, Penner LA, Gleason MJ, Foster T, Albrecht TL. Variation in question asking during cancer clinical interactions: A potential source of disparities in access to information. Patient Educ Counsel. 2011;82(1):63-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cooper LA, Roter DL, Johnson RL, Ford DE, Steinwachs DM, Powe NR. Patient-centered communication, ratings of care, and concordance of patient and physician race. Ann Intern Med. 2003;139(11):907-915. [DOI] [PubMed] [Google Scholar]
- 7.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. JAMA. 1999;282(6):583-589. [DOI] [PubMed] [Google Scholar]
- 8.Street RL, Jr, Gordon H, Haidet P. Physicians’ communication and perceptions of patients: is it how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007;65(3):586-598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hamel LM, Chapman R, Malloy M, et al. Critical shortage of African American medical oncologists in the United States. J Clin Oncol. 2015;33(32):3697-3700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnson RL, Roter D, Powe NR, Cooper LA. Patient race/ethnicity and quality of patient-physician communication during medical visits. Am J Publ Health. 2004;94(12):2084-2090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eggly S, Barton E, Winckles A, Penner LA, Albrecht TL. A disparity of words: Racial differences in oncologist-patient communication about clinical trials. Health Expect. 2015;18(5):1316-1326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Williams DR. Miles to go before we sleep: Racial inequities in health. J Health Soc Behav. 2012;53(3):279-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ellis L, Canchola AJ, Spiegel D, Ladabaum U, Haile R, Gomez SL. Racial and ethnic disparities in cancer survival: The contribution of tumor, sociodemographic, institutional, and neighborhood characteristics. J Clin Oncol. 2018;36(1):25-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jean-Pierre P, Fiscella K, Griggs J, et al. Race/ethnicity-based concerns over understanding cancer diagnosis and treatment plan. J Natl Med Assoc. 2010;102(3):184-189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eggly S, Hamel LM, Foster TS, et al. Randomized trial of a question prompt list to increase patient active participation during interactions with black patients and their oncologists. Patient Educ Counsel. 2017;100(5):818-826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eggly S, Hamel LM, Heath E, et al. Partnering around cancer clinical trials (PACCT): Study protocol for a randomized trial of a patient and physician communication intervention to increase minority accrual to prostate cancer clinical trials. BMC Cancer. 2017;17(1):807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hamel LM, Dougherty DW, Kim S, et al. DISCO App: study protocol for a randomized controlled trial to test the effectiveness of a patient intervention to reduce the financial burden of cancer in a diverse patient population. Trials. 2021;22(1):636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Senft N, Hamel LM, Penner LA, et al. The influence of affective behavior on impression formation in interactions between black cancer patients and their oncologists. Soc Sci Med. 2018;211:243-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.D’Agostino TA, Bylund CL. Nonverbal accommodation in health care communication. Health Commun. 2014;29(6):563-573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall JA, Harrigan JA, Rosenthal R. Nonverbal behavior in clinician patient interaction. Appl Prev Psychol. 1995;4(1):21-37. [Google Scholar]
- 21.Hamel LM, Moulder R, Harper FWK, Penner LA, Albrecht TL, Eggly S. Examining the dynamic nature of nonverbal communication between Black patients with cancer and their oncologists. Cancer. 2021;127(7):1080-1090. [DOI] [PubMed] [Google Scholar]
- 22.Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Counsel. 2007;67(3):315-318. [DOI] [PubMed] [Google Scholar]
- 23.Henry SG, Fuhrel-Forbis A, Rogers MA, Eggly S. Association between nonverbal communication during clinical interactions and outcomes: A systematic review and meta-analysis. Patient Educ Counsel. 2012;86(3):297-315. [DOI] [PubMed] [Google Scholar]
- 24.Gorawara-Bhat R, Cook MA. Eye contact in patient-centered communication. Patient Educ Counsel. 2011;82(3):442-447. [DOI] [PubMed] [Google Scholar]
- 25.Harrigan JA, Oxman TE, Rosenthal R. Rapport expressed through nonverbal behavior. J Nonverbal Behav. 1985;9:95-110. [Google Scholar]
- 26.Montague E, Chen PY, Xu J, Chewning B, Barrett B. Nonverbal interpersonal interactions in clinical encounters and patient perceptions of empathy. J Participat Med. 2013;5:e33. [Google Scholar]
- 27.Zantinge EM, Verhaak PF, de Bakker DH, et al. The workload of general practitioners does not affect their awareness of patients’ psychological problems. Patient Educ Counsel. 2007;67(1-2):93-99. [DOI] [PubMed] [Google Scholar]
- 28.D’Agostino TA, Bylund CL. The Nonverbal Accommodation Analysis System (NAAS): Initial application and evaluation. Patient Educ Counsel. 2011;85(1):33-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shen MJ, Peterson EB, Costas-Muniz R, et al. The effects of race and racial concordance on patient-physician communication: A systematic review of the literature. J Racial Ethn Health Disparities. 2018;5(1):117-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kimura M, Daibo I. Interactional synchrony in conversations about emotional episodes: A measurement by “the between-participants pseudosynchrony experimental paradigm”. J Nonverbal Behav. 2006;30(3):115-126. [Google Scholar]
- 31.Ramseyer F, Tschacher W. Nonverbal synchrony or random coincidence? How to tell the difference. In: Development of multimodal interfaces: Active Listing and Synchrony. Berlin: Springer; 2010;5967:182-196. [Google Scholar]
- 32.Moulder RG, Boker SM, Ramseyer F, Tschacher W. Determining synchrony between behavioral time series: An application of surrogate data generation for establishing falsifiable null-hypotheses. Psychol Methods. 2018;23:757-773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramseyer F, Tschacher W. Synchrony: A core concept for a constructivist approach to psychotherapy. Constr Hum Sci. 2006;11:150-171. [Google Scholar]
- 34.Sacheli LM, Christensen A, Giese MA, et al. Prejudiced interactions: Implicit racial bias reduces predictive simulation during joint action with an out-group avatar. Sci Rep. 2015;5:8507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vacharkulksemsuk T, Fredrickson BL. Strangers in sync: Achieving embodied rapport through shared movements. J Exp Soc Psychol. 2012;48(1):399-402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hove MJ, Risen JL. It’s All in the timing: Interpersonal synchrony increases affiliation. Soc Cognit. 2009;27(6):949-960. [Google Scholar]
- 37.Miles LK, Griffiths JL, Richardson MJ, Macrae CN. Too late to coordinate: Contextual influences on behavioral synchrony. Eur J Soc Psychol. 2010;40(1):52-60. [Google Scholar]
- 38.Miles LK, Lumsden J, Richardson MJ, Neil Macrae C. Do birds of a feather move together? Group membership and behavioral synchrony. Exp Brain Res. 2011;211(3-4):495-503. [DOI] [PubMed] [Google Scholar]
- 39.Wiltermuth S. Synchrony and destructive obedience. Soc Influ. 2012;7(2):78-89. [Google Scholar]
- 40.Wiltshire TJ, Steffensen SV, Fiore SM. Multiscale movement coordination dynamics in collaborative team problem solving. Appl Ergon. 2018;79:143-151. [DOI] [PubMed] [Google Scholar]
- 41.Ramseyer F, Tschacher W. Nonverbal synchrony in psychotherapy: coordinated body movement reflects relationship quality and outcome. J Consult Clin Psychol. 2011;79(3):284-295. [DOI] [PubMed] [Google Scholar]
- 42.Valdesolo P, Ouyang J, DeSteno D. The rhythm of joint action: Synchrony promotes cooperative ability. J Exp Soc Psychol. 2010;46(4):693-695. [Google Scholar]
- 43.Macrae CN, Duffy OK, Miles LK, Lawrence J. A case of hand waving: Action synchrony and person perception. Cognition. 2008;109(1):152-156. [DOI] [PubMed] [Google Scholar]
- 44.Miles LK, Nind LK, Henderson Z, Macrae CN. Moving memories: Behavioral synchrony and memory for self and others. J Exp Soc Psychol. 2010;46(2):457-460. [Google Scholar]
- 45.Ramseyer FT. Exploring the evolution of nonverbal synchrony in psychotherapy: The idiographic perspective provides a different picture. Psychother Res. 2020;30(5):622-634. [DOI] [PubMed] [Google Scholar]
- 46.Erdoes T, Ramseyer F. Change process in coaching: Interplay of movement synchrony, working alliance, self-regulation and goal attainment. Front Psychol. 2020;12:580351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Deres-Cohen K, Dolev-Amit T, Peysachov G, Ramseyer FT, Zilcha-Mano S. Nonverbal synchrony as a marker of alliance ruptures. Psychotherapy. 2021;58(4):499-509. [DOI] [PubMed] [Google Scholar]
- 48.Albrecht TL, Eggly SS, Gleason ME, et al. Influence of clinical communication on patients’ decision making on participation in clinical trials. J Clin Oncol. 2008;26(16):2666-2673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Penner LA, Orom H, Albrecht TL, Franks MM, Foster TS, Ruckdeschel JC. Camera-related behaviors during video recorded medical interactions. J Nonverbal Behav. 2007;31(2):99-117. [Google Scholar]
- 50.von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of Observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann Intern Med. 2007;147:573-577. [DOI] [PubMed] [Google Scholar]
- 51.Ramseyer FT. Motion energy analysis (MEA): A primer on the assessment of motion from video. J Counsel Psychol. 2020;67(4):536-549. [DOI] [PubMed] [Google Scholar]
- 52.Boker SM, Xu MQ, Rotondo JL, King K. Windowed cross-correlation and peak picking for the analysis of variability in the association between behavioral time series. Psychol Methods. 2002;7(3):338-355. [DOI] [PubMed] [Google Scholar]
- 53.Kleinbub JR, Ramseyer FT. rMEA: An R package to assess nonverbal synchronization in motion energy analysis time-series. Psychother Res. 2021;31(6):817-830. [DOI] [PubMed] [Google Scholar]
- 54.Penner LA, Harper FWK, Dovidio JF, et al. The impact of Black cancer patients’ race-related beliefs and attitudes on racially-discordant oncology interactions: A field study. Soc Sci Med. 2017;191:99-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Penner LA, Dovidio JF, Gonzalez R, et al. The effects of oncologist implicit racial bias in racially discordant oncology interactions. J Clin Oncol. 2016;34(24):2874-2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Richeson JA, Shelton JN. Brief report: Thin slices of racial bias. J Nonverbal Behav. 2005;29(1):75-86. [Google Scholar]
- 57.Gonzalez R, Griffin D. Dyadic data analysis. In: Cooper PMC H, Long DL, Panter AT, Rindskopf D, Sher KJ, eds. APA Handbook of Research Methods in Psychology, Vol. 3. Data Analysis and Research Publication. Washington. DC: American Psychological Association; 2012:439-450. [Google Scholar]
- 58.Moulder RG, Boker SM, Ramseyer F, Tschacher W. Determining synchrony between behavioral time series: An application of surrogate data generation for establishing falsifiable null-hypotheses. Psychol Methods. 2018;23(4):757-773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cooper LA, Roter DL, Carson KA, et al. The associations of clinicians’ implicit attitudes about race with medical visit communication and patient ratings of interpersonal care. Am J Publ Health. 2012;102(5):979-987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Dovidio JF, LaFrance M. Race, ethnicity, and nonverbal behavior. In: Hall JA, Knapp M, eds. Nonverbal Communication. The Hague, The Netherlands: DeGruyter-Mouton; 2013:671-696. [Google Scholar]
- 61.Bergsieker HB, Shelton JN, Richeson JA. To be liked versus respected: Divergent goals in interracial interactions. J Pers Soc Psychol. 2010;99(2):248-264. [DOI] [PubMed] [Google Scholar]
- 62.Shelton JN, Richeson JA, Salvatore J, Trawalter S. Ironic effects of racial bias during interracial interactions. Psychol Sci. 2005;16(5):397-402. [DOI] [PubMed] [Google Scholar]
- 63.Bailey ZD, Feldman JM, Bassett MT. How structural racism works - racist policies as a root cause of U.S. racial health inequities. N Engl J Med. 2021;384(8):768-773. [DOI] [PMC free article] [PubMed] [Google Scholar]