Abstract
Objective:
To determine whether the transverse dimensions of the maxillary arch of 5-year-old children with unilateral cleft lip and palate (UCLP) have changed following centralization of cleft services in the United Kingdom.
Design:
Retrospective cross-sectional study.
Setting:
Digital analysis of UCLP maxillary dental casts.
Participants:
All available maxillary dental casts from 5-year-old participants of the Clinical Standards Advisory Group (CSAG, N = 114) and Cleft Care UK (CCUK, N = 175) studies.
Interventions:
Quantitative measurements of the intercanine width (ICW), intermolar width (IMW), and the distance from the midline to the greater and lesser side canine (GC/LC) and greater side and lesser side second primary molar (GE/LE). Degree measurements of the greater and lesser arch form angles, arch length, anterior palatal depth (APD), and posterior palatal depth were also measured.
Main outcome:
Differences between the transverse dimensions of the maxillary arch for the CSAG and CCUK cohorts.
Results:
In 5 (ICW, IMW, LC, LE, and APD) of the 11 measurements, there was a statistically significant difference between the CSAG and CCUK cohorts. In all of these, the CCUK values were greater than CSAG.
Conclusions:
There have been small but positive improvements for the transverse maxillary dimensions since centralization of the UK cleft service.
Keywords: cleft lip and palate, CSAG, CCUK, transverse, maxillary
Introduction
In the United Kingdom, children born with clefts of the lip and/or palate (CL/P) comprise about 1 in 700 live births (Coupland & Coupland 1988; Bellis & Wohlgemuth 1999; Gregg et al., 2008), and it is one of the most common congenital craniofacial abnormalities seen in humans worldwide (World Health Organization, 2003). The etiology is multifactorial and includes both genetic syndromes and specific phenotypes (Carson et al., 2017) as well as environmental factors such as maternal exposure to tobacco smoke, alcohol, poor nutrition, viral infection, medicinal drugs, and teratogens in early pregnancy (Little et al., 2002; Mossey et al., 2009). Disturbance of these two etiologies at specific time points during embryogenesis is likely to affect the development of the face. Affected children require considerable care from birth through to adulthood, from a multidisciplinary team providing highly specialized care to reach a successful outcome (Colbert et al., 2015).
The surgical goal in treating this dentofacial anomaly is to produce a harmonious facial appearance, with minimal residual asymmetry (Bell et al., 2014) and a successful reconstruction of the palate, lip, and alveolus that promotes functional development. Many surgical techniques have been described for closure of clefts (Agrawal, 2009). All involve incisions along the margin of the extra- and intraoral tissues of the cleft to create flaps of skin, muscle, and mucosa. These are then brought together in various patterns and sutured closed to recreate typical palatal, labial, and nasal anatomy. Irrespective of which technique is used, there will always be an element of scarring. The extent and severity of iatrogenic scarring will influence facial and maxillary growth and development (Williams et al., 2001; Gundlach & Maus, 2006) in the transverse as well as sagittal and vertical dimensions. There often remains a degree of asymmetry between the lesser and greater sides of the maxilla following repair. This influence on facial growth and development can lead to functional, cosmetic, and psychological problems (Gundlach & Maus 2006) as well as maxillary hypoplasia, and also explains why up to 70% of the cleft population may have a class III skeletal relationship (Williams et al., 2001). A narrow maxillary arch can result in crossbites, crowding, and delayed eruption of teeth which all effect dental health and smile aesthetics. A study comparing individuals with unilateral cleft lip and palate (UCLP) to unaffected norms postulated that a reduced palatal volume could result in anterior open bite, mouth breathing, backward growth rotations, and a low tongue position that increased the mandibular intermolar width (IMW) resulting in crossbites (Generali et al., 2017).
Prior to 1998, cleft care in the United Kingdom was fragmented, with 57 centers and 78 surgeons providing care for approximately 1000 children/year (Colbert et al., 2015). In 1996, the Clinical Standards Advisory Group (CSAG) was commissioned by the UK government to examine the care provided for people born with CL/P, together with the training of those delivering that care. The key conclusions of the subsequent CSAG report published in 1998 (CSAG, 1998) on clinical outcomes and service infrastructure were as follows (Bearn et al., 2001):
High volume of surgery was associated with better outcomes.
Sufficient volume of patients, with appropriate records, is required to verify the quality of care.
Some services lacked a comprehensive range of specialists and resources.
The final recommendations, which were accepted in full by the UK government and subsequently implemented, were wide ranging and included:
Centralization of expertise and resources to reduce the number of treatment centers from 57, down to between 8 and 15.
Centers providing cleft care should ensure the full range of skills are available.
Clinicians should agree on a common nationwide database for all patients with a cleft.
Training programs for all specialist cleft clinicians should only be provided in cleft centers.
The surgical specialties involved must develop a common training pathway for the small number of trainees required to specialize in cleft care.
This centralization of services took time, with the final number of centers reduced down to 10 by 2005 (Hodgkinson et al., 2005).
In 2013, the Cleft Care UK (CCUK) study undertook to investigate the clinical impacts (ie, patient outcomes) of the reconfigured cleft services in the United Kingdom. Similar to the original CSAG study, CCUK was a UK wide, multicenter cross-sectional study of 5-year-olds (n = 268) with nonsyndromic UCLP (Persson et al., 2015). It was found that while some outcomes such as facial growth, speech, and parental report of self-confidence had improved (Al-Ghatam et al., 2015; Waylen et al., 2015; Ness et al., 2017), others, such as dental health and hearing, had not (Smallridge et al., 2015).
Within the CCUK study, the 5-year-olds index was used to assess the dentoalveolar outcomes (Atack et al., 1997) rather than true anatomical change of the maxilla. Previous studies have examined true geometric changes in the maxillary dimensions but have compared the presence versus the absence of a UCLP (Generali et al., 2017); UCLP versus bilateral cleft lip and palate (BCLP; Monga et al., 2020); the effect of a specific surgical procedure, for example, early gingivoplasty (Wojtaszek-Slominska et al., 2010); or a nonsurgical intervention, for example, a presurgical infant orthopedic appliance for cleft lip and palate (Mishima et al., 1996; Papadopoulos et al., 2012) rather than the effect of service centralization.
The aim of the present study was therefore to examine the effect of national cleft service centralization on the maxillary arch dimensions of 5-year-old children born with UCLP. The null hypothesis tested was: There are no significant differences in any of the linear or angular measurements between the CSAG and CCUK cohorts.
Materials and Methods
The inclusion criteria for this study is taken from the CSAG and CCUK projects; 5-year-olds with UCLP in the United Kingdom. A total of 289 UCLP maxillary arch dental casts (114 from CSAG and 175 from CCUK) were identified for use in this study. Permission to conduct the study was granted by the Audit Steering Commitee of University Hospitals Bristol NHS Foundation Trust and it was registered as service evaluation (SE: 180). Access to the CCUK dental casts was approved by the CCUK Study Team. The CSAG dental casts were accessed from the CSAG archive at Bristol Dental School.
All 289 maxillary arch plaster dental casts, previously anonymized for patient data, were scanned using a 3Shape R700 (3 Shape) laser scanner, calibrated to ensure 0.02 mm accuracy. Each dental cast was assigned a unique identifier number by a maxillofacial technician outside of the research team, using a random number generator. This concealed the cohort to which each dental cast belonged (CSAG or CCUK). The digital dental casts were then measured by a single researcher (CM).
On the anonymized digital dental casts, a reference occlusal plane was constructed using the lowest point on the palatal gingival margin of the teeth 55 and 65 and the upper central incisor of the greater side. A reference sagittal plane was also constructed perpendicular to a line connecting the distal surfaces of 55 and 65 (Figures 1 –3) and passing through the gingival contact point of 51 and 61, or where these were not present the midpoint of the incisive papilla. Where neither were clear, as was the case with 15 of the dental casts, these were assessed independently by a second, also blinded researcher (AI), discussed, and a consensus reached as to the line which best represented this reference sagittal plane. The construction of the sagittal plane enabled independent measurement of the lesser and greater sides. Each measurement was considered independently for each dental cast, thus where landmarks were not identifiable (ie, missing 51), the measurements associated were not possible for that cast.
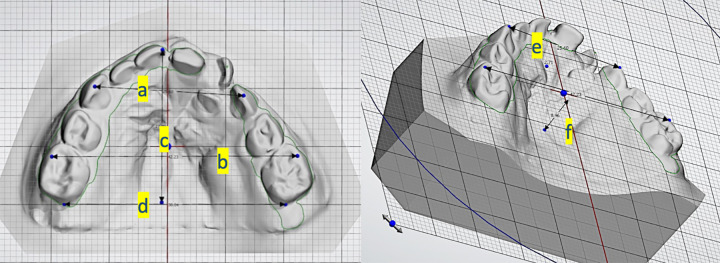
Figure 1.
Image to show linear measurements. A, Intercanine width (ICW), (B) intermolar width (IMW), (C) arch length (AL) which is perpendicular to the (D) distopalatal line, (E) anterior palatal depth (APD), and (F) posterior palatal depth (PPD).
Figure 2.
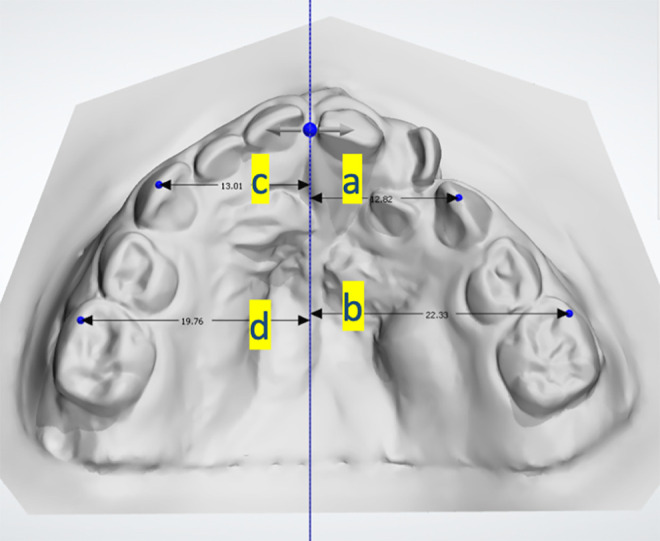
Image to show linear measurements to the sagittal plane midline. A, Lesser side canine to midline (LC), (B) lesser side E to midline (LE), (C) greater side canine to midline (GC), (D) greater side E to midline (GE).
Figure 3.
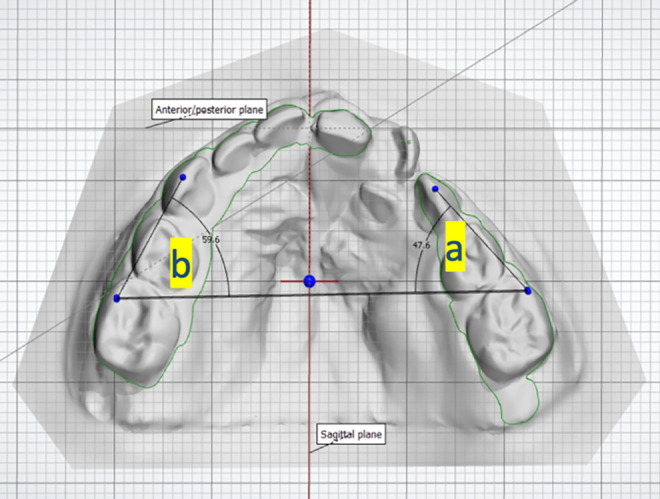
Image showing angular measurements. A, Lesser side angle (LA) and (B) greater side angle (GA).
The following measurements were made using OrthoAnalyzer software (ESM Digital Solutions Ltd; Figures 1 –3) by a single operator who was blinded to their allocation (CM), and the data transferred onto a Microsoft Excel spreadsheet:
Intercanine width (ICW)—cusp tip of 53 to cusp tip of 63.
Anterior palatal depth (APD)—vertical perpendicular distance between the midpoint of the line from 53 to 63 and the palate.
Lesser side canine (LC)—distance from the constructed midline to the lesser side 53 or 63 tip.
Greater side canine (GC)—distance from the constructed midline to the greater side 53 or 63 tip.
IMW—mesiobuccal cusp of 55 to mesiobuccal cusp of 65.
Posterior palatal depth (PPD)—vertical perpendicular distance between the midpoint of the posterior width line (line distal of 55-65) and the palate.
Lesser side second primary molar (LE)—distance from the constructed midline to the lesser side mesiobuccal cusp of the 55 or 65.
Greater side second primary molar (GE)—distance from the constructed midline to the greater side mesiobuccal cusp of the 55 or 65.
Arch length (AL)—mesial incisal edge of the upper central incisor (greater side) to line constructed distal to 55 to 65.
Lesser side angle (LA)—angle created between the IMW line and line between lesser side primary molar mesiobuccal cusp (LE) and lesser side canine cusp tip (LC).
Greater side angle (GA)—angle created between the IMW line and line between greater side primary molar mesiobuccal cusp (GE) and greater side canine cusp tip (GC).
In order to assess intraoperator reliability, a random selection of 30 dental casts were remeasured by the same operator (CM), a minimum of 2 weeks following the initial measurements. The technician deleted any previous measurements within the software prior to remeasurement.
Statistical Analysis
The data were analyzed using Stata version 16 (Stata Corp) statistics package, with a predetermined significance level of α = 0.05. The data were considered to follow a normal distribution. Table 1 illustrates the means, standard deviations, and 95% CIs of the means for each of the 11 measurements. Differences were explored using 2 sample t tests. When comparing sides with respect to cohort (CSAG vs CCUK), a linear mixed dental cast analysis was performed and the results presented as margin plots to illustrate any interaction between the cohort and the lesser or greater side of each maxillary dental cast. Intraoperator reliability was estimated with intraclass correlation coefficients and Lin concordance correlation coefficient (Lin, 1989, 2000).
Table 1.
Linear and Angular Measurements Mean, Standard Deviation, 95% Confidence Intervals Along With the Corresponding P Values for Each Cohort.
| Measurement | Cohort | No. of models | Mean/mm or degrees | SD | 95% Confidence interval | P value |
|---|---|---|---|---|---|---|
| Intercanine width (ICW) | CSAG | 104 | 24.69 | 3.12 | 24.08-25.29 | .044 |
| CCUK | 166 | 25.45 | 2.96 | 25.00-25.91 | ||
| Anterior palatal depth (APD) | CSAG | 95 | 2.1 | 1.63 | 1.77-2.43 | .029 |
| CCUK | 160 | 2.52 | 1.36 | 2.30-2.73 | ||
| Lesser side canine (LC) | CSAG | 100 | 10.05 | 2.9 | 9.48-10.63 | .004 |
| CCUK | 161 | 11.09 | 2.75 | 10.66-11.52 | ||
| Greater side canine (GC) | CSAG | 100 | 14.47 | 1.65 | 14.14-14.80 | .084 |
| CCUK | 162 | 14.23 | 1.28 | 14.03-14.43 | ||
| Intermolar width (IMW) | CSAG | 104 | 39.96 | 3.39 | 39.30-40.61 | .003 |
| CCUK | 166 | 41.19 | 3.15 | 40.71-41.67 | ||
| Posterior palatal depth (PPD) | CSAG | 101 | 9.71 | 2.4 | 9.24-10.19 | .073 |
| CCUK | 162 | 10.26 | 2.41 | 9.89-10.64 | ||
| Lesser side second primary molar (LE) | CSAG | 104 | 19.5 | 2.74 | 18.97-20.04 | .002 |
| CCUK | 163 | 20.53 | 2.61 | 20.12-20.93 | ||
| Greater side second primary molar (GE) | CSAG | 104 | 20.42 | 2.2 | 20.00-20.85 | .599 |
| CCUK | 163 | 20.56 | 1.87 | 20.26-20.85 | ||
| Arch length (AL) | CSAG | 101 | 25.09 | 2.33 | 24.63-5.55 | .485 |
| CCUK | 161 | 24.9 | 1.97 | 24.59-25.21 | ||
| Lesser side angle (LA) | CSAG | 100 | 47.35 | 7.52 | 45.86-48.84 | .749 |
| CCUK | 161 | 47.65 | 7.26 | 46.52-48.78 | ||
| Greater side angle (GA) | CSAG | 101 | 62.7 | 6.19 | 61.48-63.92 | .082 |
| CCUK | 162 | 61.54 | 4.52 | 60.84-62.25 |
Abbreviations: CCUK, Cleft Care UK; CSAG, Clinical Standards Advisory Group; SD, standard deviation.
Results
Using intraclass correlation coefficients, intraexaminer reliability was found to be good for each of the 11 measurements in this study, with values over 0.95 and narrow 95% CIs for all measurements except for the GC (0.822; 0.660-0.911) and GE (0.916; 0.830-0.959) measurements. This is reiterated by Lin concordance correlation coefficient (Lin, 1989, 2000) where all measurements values were above 0.95 except GC (0.80) and GE (0.92).
Considering each of the measurements in turn and comparing CSAG with CCUK (Table 1), statistically significant differences were observed between the cohorts for the ICW (P =.044), APD (P =.029), LC (P =.004), IMW (P =.003), and LE (P = .002) measurements. In each case, the mean values of the CCUK cohort were greater than those observed in the CSAG cohort. There were no statistically significant differences between the 2 cohorts for the GC (P = .084), PPD (P = .073), GE (P = .599), AL (P = .485), the LA (P = .749), or GA (P = .082) measurements.
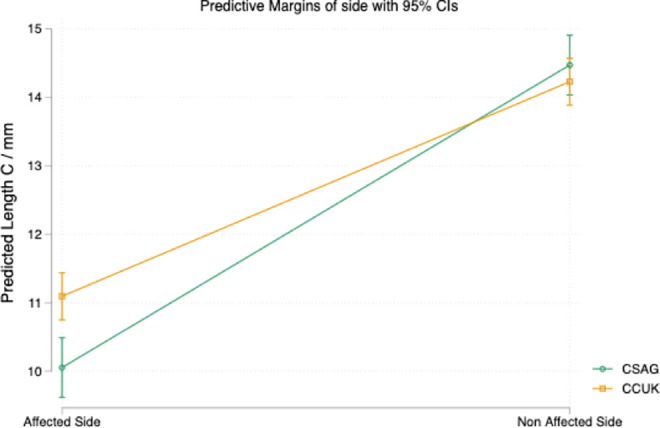
With the lesser and greater side canine measurements for each cohort, it can be seen that the difference between the mean values for LC was 1.04 mm, which was statistically significantly different, with the CCUK value being larger. The difference between the means for the GC was only 0.24 mm, which was not statistically significant, and in this case the mean was slightly larger for the CSAG cohort. The mean LC values for both CSAG and CCUK (10.05 and 11.09 mm, respectively) were smaller than the GC values (14.47 and 14.23 mm, respectively). This is also illustrated in the margin plot (Figure 4) along with the associated interaction between the cohorts.
Figure 4.
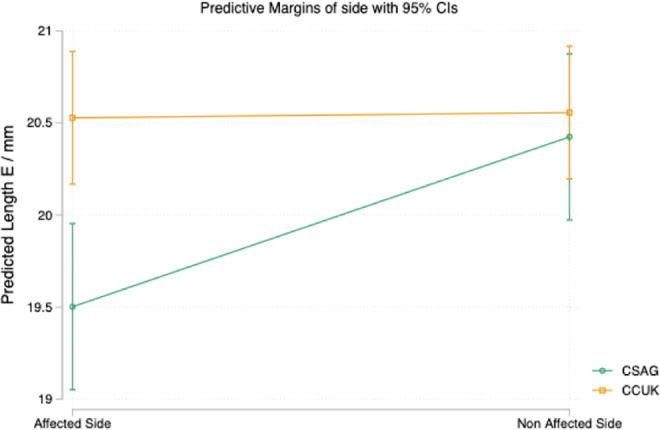
Margin plot illustrating the interaction between the CSAG and CCUK cohorts on the lesser side C measurement (LC) and greater side C measurement (GC). CCUK indicates Cleft Care UK; CSAG, Clinical Standards Advisory Group.
Considering both the LE and GE measurements for each cohort in more detail, it can be seen that the difference between the mean values for the measurement LE was 1.03 mm and was statistically significantly different, being greater in the case of CCUK. The difference for the GE was not statistically significant with 0.14 mm as the difference between the mean values. The mean LE values for both CSAG and CCUK (19.50 and 20.53 mm, respectively) were smaller than GE values (20.42 and 20.56 mm, respectively) although to a lesser amount. This is also illustrated in the margin plot (Figure 5) along with the associated interaction between the cohorts. It can be seen that the line between LE and GE for the CCUK cohort is almost horizontal indicating similar values for the 2 sides, whereas the slope of the line for the CSAG cohort illustrates a greater difference between LE and GE in this cohort.
Figure 5.
Margin plot illustrating the interaction between the CSAG and CCUK cohorts on the lesser side E measurement (LE) and greater side E measurement (GE).
With respect to AL, there were no clinically or statistically significant differences between the cohorts (P = .485). For the angular measurements, the angles were larger in the case of the greater side, irrespective of cohort (Table 1). However, when comparing the CSAG and CCUK cohorts, there was no statistically significant difference between them, for either the LA (P = .749) or GA (P = .082).
Discussion
In the present study, children with UCLP were chosen as this phenotype reflects many of the problems seen in all cleft forms, while providing a relatively unaffected side for comparison. Five-year-old children were selected as any effects of surgery on the transverse arch dimensions will be unaffected by other inventions such as orthodontic treatment, which would normally occur at a later age.
In determining the effect of service centralization, we consider the anterior, posterior, and archform angles in turn.
The Anterior Segment
Previously reported values for intercanine width of a noncleft population at the age of 5 years are 28.4 mm for girls and 30.3 mm for boys (Bishara et al., 1997). In the mixed male and female sample from the current study, the mean ICW was 24.7 mm for CSAG and 25.5 mm for CCUK. Although both values are still below the average for the noncleft child of either gender, the mean ICW for the CCUK cohort was closer to the norm for the unaffected child. It can also be seen that if the unaffected GC measurement for either the CSAG or CCUK sample was doubled, this value would sit between the male and female average values for a noncleft population. Therefore, the observed reduction in the ICW value is likely to be due to the collapse toward the midline of the lesser segment as a result of the surgical scarring at the cleft repair site. Therefore, the CCUK value being greater than the CSAG indicates improvement in the anterior segment outcome for the CCUK cohort.
The APD measurement was found to be statistically significantly different with the CCUK cohort value being greater than CSAG, although the difference in the means was only 0.42 mm. This is in line with previously published work (Wojtaszek-Slominska et al., 2010).
The Posterior Segment
Reported values of a noncleft population for posterior arch width are 40.8 mm for girls and 43.5 mm for boys (Bishara et al., 1997). In the present study, using combined male and female data, the CSAG IMW mean was 40 mm, whereas the CCUK mean was greater at 41.2 mm. This would indicate that IMW is normalizing from the CSAG to the CCUK cohort, with greater symmetry of the lesser and greater segments. This is in-keeping with 2 previous studies where posterior width of cleft and noncleft cohorts were studied over time (Generali et al., 2017; Mazaheri et al., 1971). Historically, Mazaheri et al. (1971) found that at 5 years of age, the upper posterior arch width and intercanine width are reduced in a CLP compared to noncleft children, whereas almost half a century later, Generali et al. (2017) reported no statistically significant difference in the posterior width between a cleft and noncleft cohort. The difference in IMW in the current study appears to originate from the smaller LE measurement for the CSAG cohort in a similar way to that seen anteriorly.
Archform Angles
When considering the angular measurements LA and GA, the results were similar for both cohorts, and there was no statistically significant difference between the CSAG and CCUK dental casts in the greater side measurements (GC and GE). However, a lack of difference for the LA value might be explained by the clinically and statistically significant effect of service centralization on both the LC and LE dimensions, both of which were greater in the CCUK cohort, thereby keeping LA largely unaffected.
Limitations
As the dental casts were previously anonymized, it was not possible to consider patient gender as a variable in this study.
There were occasional issues with the recording of measurements due to dental cast artifacts, and so the results should be interpreted with some caution. Sagittal plane identification could be subjective, which would be reflected as measurement bias for the lesser and greater side measurements. This potential issue was not, however, noted in the intraexaminer reliability results.
Consideration was given to including a palatal volume measurement in the current study but discounted as being inaccurate and liable to misinterpretation. Palatal volume has previously been investigated by Generali et al. (2017) and Monga et al. (2020) who compared individuals with UCLP or BCLP and found that the palatal volumes in UCLP and BCLP were significantly smaller than those of unaffected controls. However, boundary identification to enclose a volume where the arch is sometimes incomplete is subjective. Furthermore, in the current study, it was occasionally evident that the observed palate on the dental cast did not comprise true anatomical morphology. Examples of this included an imprint of gauze in the palatal vault or alveolar ridge and an abnormally smooth palatal surface. This may infer that an oronasal fistula was present at the time the original impression was taken and has obvious implications for landmark identification and volumetric measurement. It is the same reason why not all of the dental casts in both cohorts could be used to determine all 11 measurements. Measurements could not always be performed as landmark identification and construction of the occlusal plane was sometimes not possible. Each measurement was considered independently, and in 4 casts for each cohort, no measurements were possible (proportionally 3.4% in CSAG and 2.3% in CCUK). The range of missing values for the measurements was 5.1% (IMW) to 12.9% (APD). There were also less casts as part of the CSAG cohort. It is understood these had be loaned for previous research and not returned, thus an element of selection bias is present. Despite these limitations, the sample sizes for each measurement in each cohort were still large and provided good evidence for a positive effect of service centralization on patient outcomes.
Clinical Impact
An improvement in transverse outcomes at this stage may reduce the need for prealveolar bone graft orthodontics as surgical access will already be acceptable. This would reduce the burden on the patient as well as the cleft service which operates within limitations of the UK National Health Service.
The reasons for these small but positive improvements in cleft outcomes following service centralization are most likely due to changes in surgical protocol, experience, and technique. It has previously been reported that improved surgical outcomes for cleft-affected children are associated with surgeons performing a higher number of surgical repairs (Al-Ghatam et al., 2015). Following centralization of services, Scott et al. (2015) found that of the 18 primary cleft surgeons in the United Kingdom, 16 were reaching the target of 40 cases annually. This is considerably different from the CSAG findings where only 17 of the 83 surgeons operated on more than 5 babies over a 2-year period (Colbert et al., 2015). A further difference to the way these babies with UCLP were treated is with the widespread adoption in the United Kingdom of the Oslo surgical protocol for repair. This technique is associated with improved outcomes for craniofacial morphology and nasiolabial appearance (Brattström et al., 2005; Fudalej et al., 2015). This may also account for the strong homogeneity of the individual measurements. Finally, surgical training in the United Kingdom is now via a structured pathway, which provides relevant experience (Rautio et al., 2017) for both oral and maxillofacial and plastic surgeons, via craniofacial training fellowships. The introduction of centralization in the United Kingdom has meant that evidence-based changes, such as surgical protocol, can be implemented across the service and fewer cleft centers means increased surgical experience for those operating on these complex cases.
The results of this study suggest that recommendations following the initial CSAG investigation and report in 1998 leading to service centralization and improvements in training have had a small but positive influence on the surgical repair of clefts and therefore patient outcomes. The United Kingdom is one of the few countries in the world to have centralized cleft care which has led to meaningful improvements for this group of patients.
Conclusions
The following conclusions were made as a result of the effect of service centralization on cleft maxillary arch dimensions:
The null hypothesis was rejected as there was a statistically significant difference between the CSAG and CCUK cohorts for 5 of the 11 measurements.
With respect to noncleft norms, both the CSAG and CCUK cohorts were reduced for the anterior width, whereas the CCUK cohort was approaching normalization for the posterior width.
Clear differences remain between the lesser and greater sides of the maxilla for children with UCLP.
Acknowledgments
Many thanks must go to Chris Keating (Maxillofacial Technician) who provided advice and support with the software and gave up his time to blind all of the dental casts.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Charlotte Molyneaux https://orcid.org/0000-0001-9480-6651
Martyn Sherriff https://orcid.org/0000-0003-3737-1449
References
- Agrawal K. Cleft palate repair and variations. Indian J Plast Surg. 2009;42(suppl):102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Ghatam R, Jones TE, Ireland AJ, Atack NE, Chawla O, Deacon S, Albery L, Cobb AR, Cadogan J, Leary S, et al. Structural outcomes in the Cleft Care UK study. Part 2: dento-facial outcomes. Orthod Craniofac Res. 2015;18(suppl 2):14–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atack N, Hathorn I, Mars M, Sandy JR. Study dental casts of 5 year old children as predictors of surgical outcome in unilateral cleft lip and palate. Eur J Orthod. 1997;19(2):165–170. [DOI] [PubMed] [Google Scholar]
- Bearn D, Mildinhall S, Murphy T, Murray JJ, Sell D, Shaw WC, Williams AC, Sandy JR. Cleft lip and palate care in the United Kingdom--the clinical standards advisory group (CSAG) study. Part 4: outcome comparisons, training, and conclusions. Cleft Palate Craniofac J. 2001;38(1):38–43. [DOI] [PubMed] [Google Scholar]
- Bell A, Lo TWR, Brown D, Bowman AW, Siebert JP, Simmons DR, Millett DT, Ayoub AF. Three-dimensional assessment of facial appearance following surgical repair of unilateral cleft lip and palate. Cleft Palate Craniofac J. 2014;51(4):462–471. [DOI] [PubMed] [Google Scholar]
- Bellis TH, Wohlgemuth B. The incidence of cleft lip and palate deformities in the south-east of Scotland (1971-1990). Br J Orthod. 1999;26(2):121–125. [DOI] [PubMed] [Google Scholar]
- Bishara SE, Jakobsen JR, Treder J, Nowak A. Arch width changes from 6 weeks to 45 years of age. Am J Orthod Dentofacial Orthop. 1997;111(4):401–409. [DOI] [PubMed] [Google Scholar]
- Brattström V, Mølsted K, Prahl-Andersen B, Semb G, Shaw WC. The eurocleft study: intercenter study of treatment outcome in patients with complete cleft lip and palate. Part 2: craniofacial form and nasolabial appearance. Cleft Palate Craniofac J. 2005;42(1):69–77. [DOI] [PubMed] [Google Scholar]
- Carson JC, Standley J, Petrin A, Shaffer JR, Butali A, Buxo CJ, Castilla E, Christensen K, Deleyiannis FWD, Hecht JT, et al. Identification of 16q21 as a modifier of nonsyndromic orofacial cleft phenotypes. Genetic Epidem. 2017;41(8):887–897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colbert SD, Green B, Brennan PA, Mercer N. Contemporary management of cleft lip and palate in the United Kingdom. have we reached the turning point?. Br J Oral Maxillofac Surg. 2015;53(7):594–598. [DOI] [PubMed] [Google Scholar]
- Coupland MA, Coupland AI. Seasonality, incidence, and sex distribution of cleft lip and palate births in Trent region, 1973-1982. Cleft Palate J. 1988;25(1):33–37. [PubMed] [Google Scholar]
- CSAG. Cleft Lip and/or Palate, Report of a CSAG Committee. HMSO; 1998. [Google Scholar]
- Fudalej PS, Wegrodzka E, Semb G, Hortis-Dzierzbicka M. One-stage (Warsaw) and two-stage (Oslo) repair of unilateral cleft lip and palate: craniofacial outcomes. J Cranio-Maxillofac Surg. 2015;43(7):1224–1231. [DOI] [PubMed] [Google Scholar]
- Generali C, Primozic J, Richmond S, Bizzarro M, Flores-Mir C, Ovsenik M, Perillo L. Three-dimensional evaluation of the maxillary arch and palate in unilateral cleft lip and palate subjects using digital dental casts. Eur J Orthod. 2017;39(6):641–645. [DOI] [PubMed] [Google Scholar]
- Gregg TA, Leonard AG, Hayden C, Howard KE, Coyle CF. Birth prevalence of cleft lip and palate in Northern Ireland (1981 to 2000). Cleft Palate Craniofac J. 2008;45(2):141–147. [DOI] [PubMed] [Google Scholar]
- Gundlach KK, Maus C. Epidemiological studies on the frequency of clefts in Europe and world-wide. J Cranio maxillofac Surg. 2006;34(suppl 2):1–2. [DOI] [PubMed] [Google Scholar]
- Hodgkinson PD, Brown S, Duncan D, Grant C, McNauchton A, Thomas P, Rye Mattick C. Management of children with cleft lip and palate: a review describing the application of multidisaplinary team working in this condition based upon experiences of a regional cleft lip and palate centre in the united Kingdom. Fetal and Mat Med Review. 2005;16(1):1–27. [Google Scholar]
- Lin L. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45(1):255–268. [PubMed] [Google Scholar]
- Lin L. A note on the concordance correlation coefficient. Biometrics. 2000;56(1):324–325. [Google Scholar]
- Little J, Cardy A, Munger RG. Tobacco smoking and oral clefts: a meta-analysis. Bull World Health Organ. 2002;82(3):213–218. [PMC free article] [PubMed] [Google Scholar]
- Mazaheri M, Harding RL, Cooper JA, Meier JA, Jones TS. Changes in arch form and dimensions of cleft patients. American J Orthod. 1971;60(1):19–32. [DOI] [PubMed] [Google Scholar]
- Mishima K, Sugahara T, Mori Y, Sakuda M. Three dimensional comparison between the palatal forms in complete unilateral cleft lip and palate with and without Hotz Plate from cheiloplasty to palatoplasty. Cleft Palate Craniofac J. 1996;33(4):312–317. [DOI] [PubMed] [Google Scholar]
- Monga N, Kharbanda OP, Balachandran R, Neelapu BC. Palatal volume estimation in operated unilateral and bilateral cleft lip and palate subjects using digital study dental casts. Orthod Craniofac Res. 2020;23(3):1–7. [DOI] [PubMed] [Google Scholar]
- Mossey P, Little J, Munger RG, Dixon MJ, Shaw WC. Cleft lip and palate. Lancet. 2009;374(9703):1773–1785. [DOI] [PubMed] [Google Scholar]
- Ness AR, Wills AK, Mahmoud O, Hall A, Sell D, Smallridge J, Southby L, Stokes D, Toms S, Waylen A, et al. Centre-level variation in treatment and outcomes and predictors of outcomes in 5-year-old children with non-syndromic unilateral cleft lip treated within a centralized service: the cleft care UK study. part 6: summary and implications. Orthod Craniofac Res. 2017;20(suppl 2):48–51. [DOI] [PubMed] [Google Scholar]
- Papadopoulos M, Koumpridou E, Vakalis M, Papageorgiou SN. Effectiveness or pre-surgical orthopaedic treatment for cleft lip and palate patients: a systematic review and meta analysis. Orthod Craniofac Res. 2012;15(4):207–236. [DOI] [PubMed] [Google Scholar]
- Persson M, Sandy JR, Waylen A, Wills AK, Al-Ghatam R, Ireland AJ, Hall AJ, Hollingworth W, Jones T, Peters TJ, et al. A cross-sectional survey of 5-year-old children with non-syndromic unilateral cleft lip and palate: the cleft care UK study. Part 1: background and methodology. Orthod Craniofac Res. 2015;18(suppl 2):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rautio J, Andersen M, Bolund S, Hukki J, Vindenes H, Davenport P, Arctander K, Larson O, Berggren A, Åbyholm F, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 2. surgical results. J Plast Surg Hand Surg. 2017;51(1):14–20. [DOI] [PubMed] [Google Scholar]
- Scott JK, Leary SD, Ness AR, Sandy JR, Persson M, Kilpatrick N, Waylen AE. Perceptions of team members working in cleft services in the United Kingdom: a pilot study. Cleft Palate Craniofac J. 2015;52(1):1–7. [DOI] [PubMed] [Google Scholar]
- Smallridge J, Hall AJ, Chorbachi R, Parfect V, Persson M, Ireland AJ, Wills AK, Ness AR, Sandy JR. Functional outcomes in the cleft care UK study-part 3: oral health and audiology. Orthod Craniofac Res. 2015;18(suppl 2):25–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waylen A, Ness AR, Wills AK, Persson M, Rumsey N, Sandy JR. Cleft care UK study. Part 5: child psychosocial outcomes and satisfaction with cleft services. Orthod Craniofac Res. 2015;18(suppl 2):47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Human Genetics Programme. World Atlas of Birth Defects. 2nd ed. International Centre for Birth Defects of the International Clearinghouse for Birth Defects Monitoring Systems in collaboration with the Human Genetics Programme of the World Health Organization; 2003. [Google Scholar]
- Williams AC, Bearn D, Mildinhall S, Murphy T, Sell D, Shaw WC, Murray JJ, Sandy JR. Cleft lip and palate care in the United Kingdom—the clinical standards advisory group (CSAG) study. Part 2: dentofacial outcomes and patient satisfaction. Cleft Palate Craniofac J. 2001;38(1):24–29. [DOI] [PubMed] [Google Scholar]
- Wojtaszek-Slominska A, Renkielska A, Dobke M, Gosman A, Slominski W. Orthodontic characteristics of maxillary arch deficiency in 5-year-old patients undergoing unilateral cleft lip and palate repair with and without early gingivoplasty. J Cranio-Maxillofac Surg. 2010;38(3):155–159. [DOI] [PubMed] [Google Scholar]