Abstract
Objective:
The purpose of this study is to assess for any associations between individual and social factors and late-stage melanoma in Kentucky from 1995 to 2013.
Methods:
The study combines three datasets: individual level data from the Kentucky Cancer Registry (KCR), census tract level data from the United States (US) Census and county level physician licensure data from the Kentucky Department of Public Health. The study population is described by all cases, early-stage and late-stage. Logistic regression was used to evaluate the unadjusted associations between each covariate and early-stage and late-stage disease groups. All significant variables were assessed for interaction effect and the significant interaction terms were used in the final model. Multiple logistic regression provided the final model of late-stage disease.
Results:
In this study population, a dramatic increase in melanoma incidence is seen from 1995 to 2013 with a three-fold increase in the number of cases per year. Of the 10,109 cases reported, 13.6% have late-stage disease with a mean age for all cases at 56.9 years and the majority male. Late-stage cases are more commonly uninsured or insured with Medicaid or Medicare compared to early-stage lesions. Having a spouse or partner is clearly protective from being diagnosed with late-stage melanoma while being uninsured or having Medicaid increases the odds of late-stage melanoma.
Conclusion:
The incidence of melanoma is dramatically increasing. With no screening recommendation for the general population from the US Preventative Task Force, clinicians should focus on those at increased risk of late-stage melanoma; unmarried men who are uninsured or on Medicaid. 12
Keywords: Malignant melanoma, stage of diagnosis, marriage, insurance status, socioeconomic status
Introduction
Malignant melanoma is the deadliest form of skin cancer, yet it still has a good prognosis with a 90% survival rate. 1 This high survival rate is due to 85% of melanoma lesions being diagnosed at an early-stage. Unlike other forms of cancer, melanoma is most likely to occur in those with a higher socioeconomic status (SES) and generally is considered a disease of wealthy white individuals. 2 Despite this, it is known that people with lower SES, regardless of race, are more commonly diagnosed with an advanced disease stage. 3 Several studies have found an association with both low education levels and high poverty levels and late-stage melanoma lesions. 2,4–6 Other studies have indicated that late-stage melanoma is associated with being uninsured and unmarried or widowed with the highest risk among males. 7,8
Earlier detection of melanoma lesions has also been associated with physician density of both family physicians and dermatologists. 9 In 2015 the American Academy of Medical Colleges reported that the demand for physicians continues to grow faster than the supply leading to a projected deficit of up to 90,400 physicians by 2025. 10 Also, the dermatologist shortage is expected to continue, especially in rural areas, as the incidence of skin cancer increases and the capacity for training programs remains constant. 11
With no screening recommendation for melanoma in the general population from the US Preventative Task Force and a rising incidence rate, it is important for health care providers to know which segments of the population are of greatest risk for developing melanoma and failing to be detected early.1,12 The purpose of this study is to assess associations between individual and social factors and late-stage melanoma. We hypothesize that late-stage diagnosis is associated with an increased poverty level, decreased education level and decreased physician density.
Methods
The study combines data from three sources: individual level data from the Kentucky Cancer Registry (KCR), demographic census data from the United States (US) Census and county physician licensure data from the Kentucky Department of Public Health.13–15 The KCR, a statewide, population-based registry maintains a 99% complete case ascertainment rate and has received gold certification from the North America Association of Central Cancer Registries each year since formal certification was established in 1997. 15 Data for all reported melanoma cases among Kentucky residences from non-Hispanic whites, 18 years or older from 1995 to 2013 were provided by the KCR. Cases that were in situ lesions or non-primary tumors were excluded. Data on stage at diagnosis, age, gender, marital status, year of diagnosis, anatomic site of lesion, health insurance status, rural/urban residence, and Appalachian/non-Appalachian residence were obtained for each melanoma case.
The 2000 US Census Bureau provided county level data on percentage of residents having graduated high school and percentage below the poverty level.13 The Kentucky Department of Public Health provided 2006 physician licensure data with number of all-physicians, family practice physicians and dermatologists, in each county.14 To determine the physician density the number of all-physicians, family physicians and dermatologists, per 10,000 population by county was then calculated using the 2006 US Census Bureau intercensal population estimates.17
The outcome variable of interest is cancer stage: early versus late, with early-stage defined as stage I and II lesions and late-stage defined as stage III and IV lesions per the classification system of the American Joint Committee on Cancer.18 The independent variables of interest are poverty level, education level and physician density. The percentage of the county below the poverty level and percentage with a high school education are provided as continuous variables. Physician density is assessed with the continuous variables of all-physicians, family practice physicians and dermatologists. The number of total physicians was used as melanoma is diagnosed by many types of physicians not only family practice physicians or dermatologists.
Descriptive statistics were used to characterize the distribution of variables for all cases, early-stage and late-stage cases. Logistic regression was used to evaluate the unadjusted associations between each covariate and early-stage and late-stage disease groups. All significant variables were assessed for interaction effect and significant interaction terms were described and utilized in the final model analysis. Multiple logistic regression was then used to formulate the final model of late-stage disease. The model was first run with all covariates and then variables were removed using backward elimination to arrive at the model of best fit. All reported P-values are two-tailed with statistical significance set at an alpha level of 0.05 and 95% confidence intervals. All analyses were conducted using SPSS version 23. Institutional Review Board approval was obtained prior to undertaking this study.
Results
The demographic characteristics of the study population: all cases, early-stage and late-stage disease are described in Table 1. There were 10,109 cases reported between 1995 and 2013, with 13.6% late-stage. Comparing early and late-stage disease groups, both have similar age distributions with the mean age of all cases at 56.9 years, while 63% of late-stage cases are found in males. Almost half of all cases, early and late-stage occurred among married individuals.
Table 1:
Characteristics of Melanoma Cases by Disease Stage in Kentucky from 1995–2013
| Variable | All Stages | Early Stage | Late Stage |
|---|---|---|---|
|
| |||
| n (%) | n (%) | n (%) | |
|
| |||
| Cases | 10,109 | 8,735 (86.4) | 1,374 (13.6) |
|
| |||
| Age | |||
| 18–34 | 957 (9.5) | 836 (9.6) | 121 (8.8) |
| 35–64 | 5,732 (56.7) | 4,951 (56.7) | 781 (56.8) |
| >64 | 3,420 (33.8) | 2,948 (33.7) | 472 (34.4) |
|
| |||
| Gender | |||
| Male* | 5,433 (53.7) | 4,567 (52.3) | 866 (63.0) |
| Female* | 4,676 (46.3) | 4,168 (47.7) | 508 (37.0) |
|
| |||
| Marital Status | |||
| Married/Partner* | 4,450 (44) | 3,803 (43.5) | 647 (47.1) |
| Single* | 723 (7.2) | 568 (6.5) | 155 (11.3) |
| Widowed* | 578 (5.7) | 495 (5.7) | 117 (8.5) |
| Separated/Divorced* | 612 (6.1) | 463 (5.3) | 115 (8.4) |
| Unknown* | 3746 (37.1) | 3,406 (39) | 340 (24.7) |
|
| |||
| Year Diagnosed | |||
| 1995–1998* | 1,343 (13.3) | 1,165 (13.3) | 178 (13.0) |
| 1999–2002 | 1,638 (16.2) | 1,324 (15.2) | 314 (22.9) |
| 2003–2006 | 2,094 (20.7) | 1,845 (21.1) | 249 (18.1) |
| 2007–2009 | 1,998 (19.8) | 1,745 (20.0) | 253 (18.4) |
| 2010–2013 | 3,036 (30.0) | 2,656 (30.4) | 380 (27.7) |
|
| |||
| Anatomic Site | |||
| Face, Head, Neck | 1,898 (18.8) | 1,666 (19.1) | 232 (16.9) |
| Trunk | 3,542 (35) | 3,157 (36.1) | 385 (28) |
| Limbs, Shoulder, Hips | 4,328 (42.8) | 3,886 (44.5) | 442 (32.2) |
| Overlapping, NOS* | 341 (3.4) | 26 (0.3) | 315 (22.9) |
|
| |||
| Insurance | |||
| Private insurance* | 4,820 (47.7) | 4,175 (47.8) | 645 (46.9) |
| Uninsured* | 364 (3.6) | 260 (3.0) | 104 (7.6) |
| Medicaid* | 334 (3.3) | 233 (2.7) | 101 (7.4) |
| Medicare* | 2,997 (29.6) | 2,506 (28.7) | 491 (35.7) |
| Unknown* | 1,594 (15.8) | 1,561 (17.9) | 33 (2.4) |
|
| |||
| Geography | |||
| Urban | 5,504 (54.4) | 4,776 (54.7) | 728 (53.0) |
| Rural | 4,605 (45.6) | 3,959 (45.3) | 646 (47.0) |
|
| |||
| Geography | |||
| Non-Appalachian | 7,326 (72.5) | 6,359 (72.8) | 967 (70.4) |
| Appalachian | 2,783 (27.5) | 2,376 (27.2) | 407 (29.6) |
|
| |||
| Mean (SD) | Mean (SD) | Mean (SD) | |
|
| |||
| Poverty level * | 15.5% (6.6%) | 15.4% (6.5%) | 16.0% (7.1%) |
|
| |||
| Education level * | 74.5% (9.2%) | 74.6% (9.2%) | 73.8% (9.5%) |
|
| |||
| All MD per 10,000 | 21.6 (14.7) | 21.7 (14.8) | 20.9 (14.3) |
|
| |||
| FP MD per 10,000 | 3.03 (1.32) | 3.03 (1.32) | 3.00 (1.33) |
|
| |||
| Derm per 10,000 * | 0.29 (0.30) | 0.29 (0.30) | 0.27 (0.30) |
MD, medical doctor, includes all physicians including doctors of osteopathic medicine
FP, family practice; Derm, dermatologists
indicates p <0.05
The majority of all cases and early-stage cases were on the trunk and shoulders, hips, or limbs. Whereas almost a quarter of late-stage cases were recorded as overlapping (C44.8, ICD-O-3) or as skin, not otherwise specified (NOS) (C44.9, ICD-O-3). Late-stage cases are more commonly uninsured or insured with Medicaid or Medicare compared to early-stage lesions. Those residing in urban areas and non-Appalachian counties accounted for the majority of all cases, early and late-stage. The mean percentage of those living below the poverty level by county was 15.5% with a range of 4.1– 45.0%. The mean percentage of those with a high school education level by county was 74.5%, with a range of 49 – 87%.
The entire state of Kentucky has 9,109 physicians, 1,361 family practice physicians and 121 dermatologists with the majority of counties without a dermatologist. There is a mean 20.9 all-physicians per 10,000 population for late-stage cases, compared to the early cases at 21.7. The number of family physicians and dermatologists is similar for early and late-stage groups.
Figure 1 demonstrates the dramatic increase in early-stage melanoma cases diagnosed in this population between 1995 and 2013 from 286 to 682 cases per year. The number of early-stage melanoma cases steadily increased but with a particularly large increase in cases from 2003 to 2006 and the largest number of cases reported from 2010 to 2013. Further analysis of year groups 1995 to 2002 and 2003 to 2013 did not reveal a significant difference among these groups to explain the rise in early-stage cases. The number of late-stage melanomas also steadily increased between 1995 and 2013 from 29 to 97 cases per year with a bump in the number of cases reported in 1999 to 2002 and the largest number of cases reported from 2010 to 2013.
Figure 1:
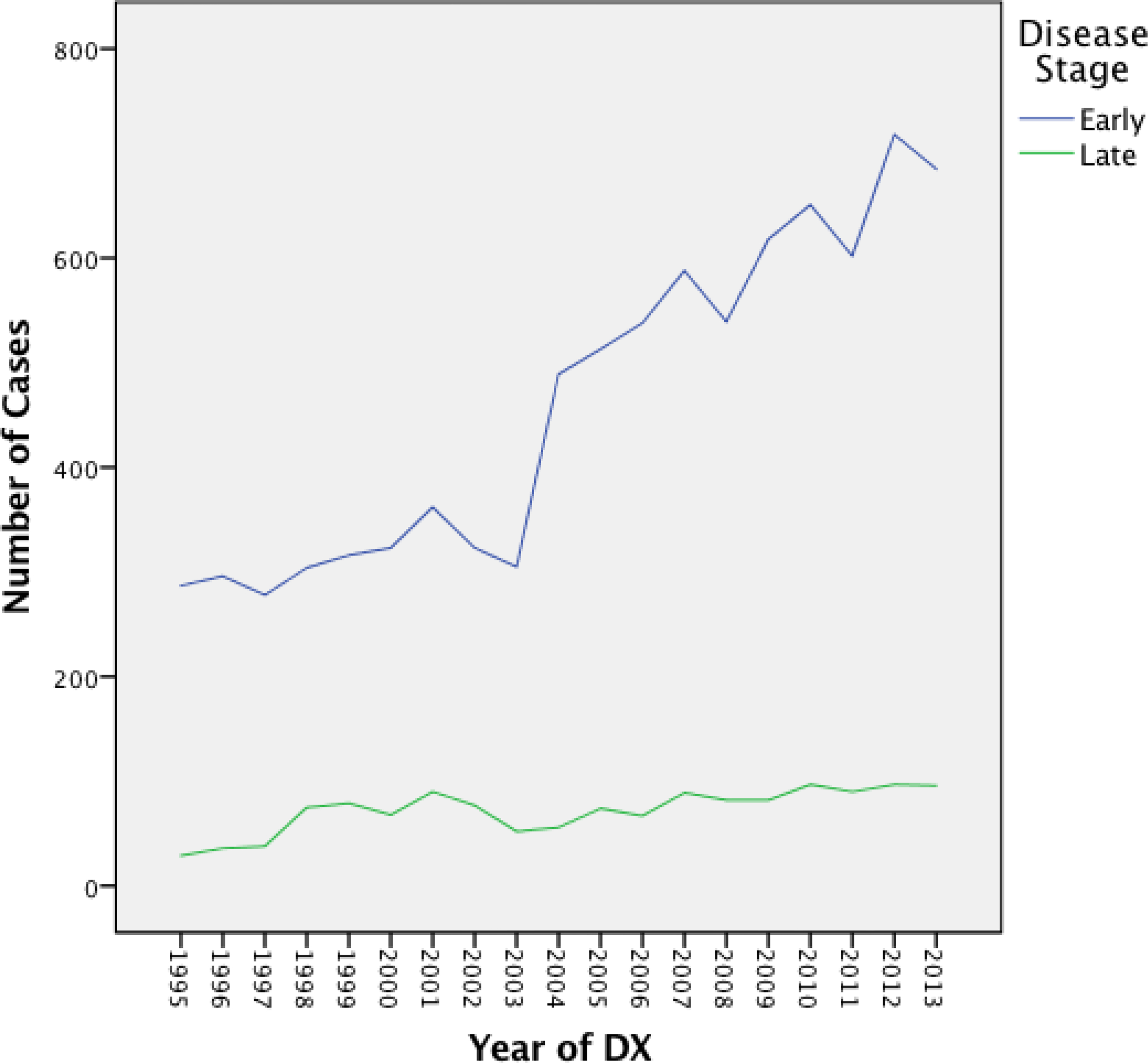
Early and Late-Stage Melanoma by Year of Diagnosis in Kentucky from 1995–2013
Analysis for interaction effect revealed interaction between age and gender and insurance and gender to be significant. Females 35–64 years old and greater than 64 have 40% (CI 0.44–0.79) and 32% (CI 0.57–0.81) decreased odds of late-stage melanoma compared to females 18–34 years old. At the same time, males 35–64 years old have a 42% (CI 1.05–1.93) increased odds compared to females 18–34 years old.
The final model is provided in Table 2 and demonstrates that marital status, year diagnosed, anatomic site and the insurance-gender interaction are associated with late-stage melanoma. The final model explains 14.4% (Cox and Snell R square) and 26.3% (Nagelkerke R squared) of the variance in late-stage of diagnosis.
Table 2:
Final Model of Adjusted Odds Ratio of Late-Stage Melanoma in Kentucky from 1995–2013
| Variable | Late-Stage | Late-Stage |
|---|---|---|
|
| ||
| OR (95% CI) | P value | |
|
| ||
| Marital Status | ||
| Married/Partner | Referent | |
| Single | 1.39 (1.11–1.75) | 0.005 |
| Widowed | 1.44 (1.11–1.89) | 0.007 |
| Separated/Divorced | 1.36 (1.06–1.75) | 0.015 |
| Unknown | 0.73 (0.58–0.93) | 0.008 |
|
| ||
| Year Diagnosed | ||
| 1995–1998 | Referent | |
| 1999–2002 | 1.30 (1.00–1.68) | 0.051 |
| 2003–2006 | 0.66 (0.48–0.90) | 0.009 |
| 2007–2009 | 0.69 (0.50–0.94) | 0.019 |
| 2010–2013 | 0.69 (0.51–0.93) | 0.019 |
|
| ||
| Anatomic Site | ||
| Face, Head, Neck | Referent | |
| Trunk | 0.92 (0.76–1.10) | 0.343 |
| Limbs, Shoulder, Hips | 0.90 (0.75–1.07) | 0.231 |
| Overlapping, NOS | 82.90 (53.84–127.84) | <0.005 |
|
| ||
| Insurance*Gender | ||
| Female Private insurance | Referent | |
| Female Uninsured | 3.26 (1.93–5.51) | <0.005 |
| Female Medicaid | 7.64 (4.08–14.31) | <0.005 |
| Female Medicare | 4.66 (2.40–9.06) | <0.005 |
| Female Unknown | 4.08 (2.38–7.00) | <0.005 |
| Male Private insurance | 0.67 (0.31–1.44) | 0.302 |
| Male Uninsured | 4.76 (2.83– 8.00) | <0.005 |
| Male Medicaid | 11.72 (6.36– 21.59) | <0.005 |
| Male Medicare | 19.2 (10.35–35.63) | <0.005 |
| Male Unknown | 5.03 (2.98–8.48) | <0.005 |
In the final model, single individuals have a 39% (CI 1.11–1.75) increased odds of late-stage disease, widowed a 44% (CI 1.11–1.89) increased odds and divorced a 36% (CI 1.06–1.75) increased odds compared to those who are married. As the incidence rate of melanoma increases from 1995 to 2013 the odds of late-stage diagnosis are significantly less from 2003 to 2013. Having a lesion that is overlapping or NOS increases the odds of late-stage disease 82 (CI 53.84–127.84) fold. Meanwhile, compared to privately insured females, uninsured females experienced a greater than 3-fold increased odds of late-stage disease (CI 1.93–5.51) and being a female on Medicaid increased the odds over 7-fold (CI 4.08–14.31). Simultaneously, males are at greater odds of late-stage melanoma compared to insured females with uninsured males at almost a 5-fold increased odds (CI 2.83–8.00), males on Medicaid with almost a 12-fold increased odds (CI 6.36–21.59) and males on Medicare with a 19-fold increased odds (CI 10.35–35.63) of late-stage disease compared to insured females. While the univariate analysis showed a significant impact of poverty, education and physician density on late-stage disease the adjusted regression did not show these outcome factors to be significant.
Discussion
Kentucky is a rural state with high poverty, low high school education levels and low physician density that has high melanoma incidence and mortality rates. Despite these factors, this analysis did not find strong evidence to conclude that the stage at which melanoma is diagnosed is impacted by poverty, education or physician density. Instead, this analysis supports previous research that demonstrates that gender, marital status and health insurance status affect stage of diagnosis. 19–21
Having a spouse or partner was clearly protective from being diagnosed with late-stage melanoma. This supports previous research by Mandala et al that marriage is protective against later stage melanoma with those who are widowed at particularly increased risk. 20 The analysis did determine that a diagnosis of overlapping lesion or NOS increased the odds of late stage melanoma by dramatically. Yet, it must be noted that the diagnosis code of NOS is often used when the known diagnosis code is not clear. Therefore, the authors feel that this finding is inexact and needs further investigation and clarification.
In a nation that does not provide affordable health care without insurance it is not unexpected that being uninsured or having Medicaid increases the odds of being diagnosed with a late-stage melanoma. The effect of health insurance status on melanoma disease stage lends itself to further investigation. Of relevance would be the effect of the expanded health insurance access through the Affordable Care Act that has provided over 500,000 uninsured Kentucky residents with coverage. 22
Education and poverty level by county was utilized to measure the effect of SES on late-stage melanoma. Increased poverty and decreased education was noted to be associated with late-stage disease in the univariate analysis but this study did not find an association in the final model when controlling for all other variables. Since this analysis did not demonstrate any influence of poverty or education at the county level, further research needs to be conducted with individual level data.
In this study, we found a three-fold increase in cases per year for both early and late-stage disease. This mirrors previous literature that shows a dramatic rise in the incidence of melanoma over the last few decades. 19 Prevention should focus on those at increased risk for late-stage disease.
This study has several important limitations. First, poverty and education were used as surrogates for socioeconomic status and were measured at the county level, not the individual level. Secondly, physician density can only be considered an aggregate of patients’ use of medical services. The actual use of physician services by these patients may not be reflective of the physician density. Additionally, this study did not account for other medical providers including physician assistants and nurse practitioners. The analysis of poverty level, education level and physician density by county in a state with 120 counties may have been obscured by aggregating at the county level. Further research should consider analysis by larger geographic regions such as area development districts. Also, additional risk factor information was not available for the study participants. Lastly, this study was restricted to the state of Kentucky, which may not be representative of other parts of the country.
Conclusion
While the incidence of melanoma continues to rise, clinicians should focus on those at increased risk of late-stage melanoma; unmarried men who are uninsured or on Medicaid. 19
Brief Description:
As the incidence of malignant melanoma in the United States continues to rise the incidence and mortality rate in Kentucky remain higher than the national average. This paper provides an analysis of almost twenty years of late stage melanoma cases in Kentucky. With no national screening guidelines to guide providers, this paper offers recommendations on which patients physicians should consider screening.
Key Points:
There is a significant increase in the incidence of early and late-stage melanoma
Marriage is protective against late-stage melanoma
Late-stage melanoma is associated with lack of insurance or insurance with Medicaid
Acknowledgments
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors would like to thank Thomas Tucker, PhD and Phillip Westgate, PhD for their mentorship and contributions to this project.
Footnotes
The authors have no financial disclosures to declare and no conflicts of interest to report.
IRB approval obtained by the University of Kentucky IRB.
Contributor Information
Virginia L. Valentin, University of Utah, Department of Family and Preventive Medicine (previously at University of Kentucky College of Health Sciences).
Wayne Sanderson, University of Kentucky, College of Public Health.
Susan Westrom, University of Kentucky, College of Public Health.
Eric Durbin, University of Kentucky, Kentucky Cancer Registry.
References
- 1.Pollack LA, Li J, Berkowitz Z et al. Melanoma Survival in the United States, 1992–2005. J Am Acad Dermatol. 2011; 65(5 Suppl 1): S78–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh SD, Ajani UA, Johnson CJ et al. Association of cutaneous melanoma incidence with area-based socioeconomic indicators-United States, 2004–2006. J Am Acad Dermatol. 2011; 65:S58.e1–12. [DOI] [PubMed] [Google Scholar]
- 3.Reyes-Ortiz CA, Goodwin JS, Freeman JL. The effect of socioeconomic factors on incidence, stage at diagnosis and survival of cutaneous melanoma. Med Sci Monit. 2005; 11(5): 163–172. [PubMed] [Google Scholar]
- 4.Hu S, Sherman R, Arheart K et al. Predictors of Neighborhood Risk for Late-Stage Melanoma: Addressing Disparities Through Spatial Analysis and Area-Based Measures. J Invest Dermatol. 2014; 134: 937–945. [DOI] [PubMed] [Google Scholar]
- 5.Youl PH, Baade PD, Parekh S et al. Association between melanoma thickness, clinical skin examination and socioeconomic status: results of a large population-based study. Int J Cancer. 2011;128: 2158–2165. [DOI] [PubMed] [Google Scholar]
- 6.Eriksson H, Lyth J, Mansson-Brahme E et al. Low level of Education is Associated with Later Stage at Diagnosis and Reduced Survival in Cutaneous Malignant Melanoma: A nationwide Population-based study in Sweden. Eur J Cancer. 2013; 49: 2705–2716. [DOI] [PubMed] [Google Scholar]
- 7.Reyes-Ortiz CA, Freeman JL, Kuo Y, Goodwin JS. The Influence of Marital Status on Stage at Diagnosis and Survival of Older Persons with Melanoma. J Gerontol. 2007; 62A(8): 892–898. [DOI] [PubMed] [Google Scholar]
- 8.McLaughlin JM, Fisher JL, Paskett ED. Marital Status and Stage at Diagnosis of Cutaneous Melanoma. Cancer. 2011; 117: 1984–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roetzheim RG, Pal N, Van Durme DJ et al. Increasing supplies of dermatologists and family physicians are associated with earlier stage of melanoma detection. J Am Acad Dermatol. 2000; 43:211–218. [DOI] [PubMed] [Google Scholar]
- 10.Association of American Colleges. The Complexities of Physician Supply and Demand Projections from 2013 to 2025. March 2015.https://www.aamc.org/download/426242/data/ihsreportdownload.pdf?cm_mmc=AAMC-_-ScientificAffairs-_-PDF-_-ihsreport Accessed August 17, 2017. [Google Scholar]
- 11.Harris, Williams & Co. Dermatology Market Overview. August 2013. http://www.harriswilliams.com/system/files/industry_update/dermatology_market_overview.pdf Accessed August 17, 2017.
- 12.US Preventative Services Task Force. Screening for Skin Cancer Recommendation Statement. Website. https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/skin-cancer-screening2 Accessed February 5, 2018. [Google Scholar]
- 13.United States Census Bureau. Website. https://www.census.gov/topics.html Accessed August 23, 2017. [Google Scholar]
- 14.Surveillance and Health Data Branch. Department of Public Health. Kentucky Licensed Physicians by Specialty. August 2006. Website. http://chfs.ky.gov/nr/rdonlyres/307d34c5-e944-4ff4-ac55-3e96a3f96578/0/kentuckylicensedphysicians.pdf Accessed August 16, 2017. [Google Scholar]
- 15.Kentucky Cancer Registry. Website. http://cancer-rates.info/ky/index.php Accessed August 20, 2017. [Google Scholar]
- 16.Coker AL, DeSimone C, Eggleston KS et al. Smoking and survival among Kentucky Women diagnosed with invasive cervical cancer: 1995–2005. Gynecol Oncol. 2009; 112(2): 365–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.United States Census Bureau. Population Estimates. Intercensal Estimates of the Resident Population for Counties: April 1, 2000 to July 1, 2010. Website. https://www.census.gov/data/tables/time-series/demo/popest/intercensal-2000-2010-state.html Accessed August 18, 2017. [Google Scholar]
- 18.Edge S, Byrd DR, Compton CC et al. American Joint Committee on Cancer Staging Manual, 7th ed. Chicago, IL: Springer Science and Business Media LLC; 2011. [Google Scholar]
- 19.Seigel R, Ma J, Zou Z et al. Cancer Statistics. CA Cancer J Clin. 2014; 64:9–29. [DOI] [PubMed] [Google Scholar]
- 20.Mandala M, Imberti GL, Piazzalunga D et al. Association of Socioeconomic Status with Brelow Thickness and Disease-free and Overall Survival in Stage I-II Primary Cutaneous Melanoma. Mayo Clin Proc. Feb 2011; 86(2): 113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ward EM, Fedewa SA, Cokkinides et al. The Association of Insurance and Stage at Diagnosis Among Patients Aged 55 to 74 Years in the National Cancer Database. Cancer J. 2010; 16:614–621. [DOI] [PubMed] [Google Scholar]
- 22.Health Insurance.org. Website. https://www.healthinsurance.org/kentucky-state-health-insurance-exchange/ Accessed February 5, 2018. [Google Scholar]


