Abstract
Objectives:
Lung cancer continues to be the leading cause of cancer-related deathworldwide. Have been reported high mortality rates from lung cancer in Latin America, but the disparities within the regions of Peru and under-reporting death certification reported prevent the inclusion of Peru in analysis of the mortality trends for lung cancer. We evaluated lung cancer mortality trends and smoking prevalence in Peru and its geographical areas.
Materials and Methods:
We obtained the data from the registry of the Peruvian Ministry of Health between 2008 and 2017. Mortality rates per 100,000 person-years were computed using the world’s SEGI population and trends were analyzed using the Joinpoint regression Program Version 4.7.0. Smoking prevalence was estimated from the Demographic and Family Health Survey.
Results:
In Peru, mortality rates were roughly 1.3 times higher in males than in females. The coast region had significant downward trends among males, whereas the highlands region had significant upward trends among females. According to provinces, Apurimac showed an annually significant rise in both sexes (+10.6% in males, and +11.6% in females). In general, smoking prevalence was higher in males compared to females, principally among young adults.
Conclusions:
Peru showed downward mortality trends in the last decade with variability across regions. Males had a higher smoking prevalence, principally among young adults. Public health interventions for smoking reduction should be implemented to reduce lung cancer mortality.
Key Words: Lung cancer, mortality, smoking, Peru
Introduction
With more than 1.7 million deaths, lung cancer continues to be the leading cause of cancer-related death worldwide . Lung cancer is strongly related to smoking, being one of the preventable risk factors of this disease. Although mortality is typically higher in males than in females, the male-to-female ratio varies widely across regions (Sung and Ferlay et al., 2021). In Latin America the late 1990s, smoking prevalence started to increase rapidly among males, whereas females began to increase a few decades later (Costa e Silva and Koifman 1998; Islami and Torre et al., 2015). Moreover, the prevalence of other recognized risk factors also modifies the burden of this disease (air pollution, occupational exposures, and radiation) (Mao and Yang et al., 2016).
In Latin America, lung cancer has the highest mortality rate along with breast, stomach, and prostate cancers in these region (Bray and Piñeros 2016; Bray and Ferlay et al., 2018; Carioli and Bertuccio et al., 2020), and represents a public health problem (Raez and Cardona et al., 2018). These lung cancer mortality rates are also strong related to smoking. In recent years, tobacco consumption has increased in women, and decreased in male (Islami and Torre 2015). Furthermore, Latin America reported a high smoking prevalence, only behind the Asian and European countries (Islami and Torre 2015), and in the first decade of XXI century, smoking has affected life expectancy, especially but not exclusively in men of the region (Palloni and Novak et al., 2015).
Although previous research have identified lung cancer as a public health problem in the Latin American population (Carioli and Bertuccio 2020; Carioli and La Vecchia et al., 2017), in Peru represents 11% of deaths from cancer, behind gastric cancer (Zafra-Tanaka and Tenorio-Mucha et al., 2020), there is scarce literature about the distribution of lung cancer within a specific country. The disparities between and within the regions of Peru might have generated a disproportionally epidemiological transition (Programa de las Naciones Unidas para el Desarrollo 2019), affecting the distribution of smoking prevalence and lung cancer mortality. As a result, it is crucial to perform a comprehensive analysis of the mortality trends for lung cancer to understand on its temporal pattern by gender and region within Peru. This outcomes could improve the understanding of lung cancer distribution and provide insights for the development of public health interventions in the most affected regions. Therefore, we estimate the mortality trends for lung cancer by sex in Peru and its geographical areas. Also, we evaluate the smoking prevalence in Peru and its provinces.
Materials and Methods
Study Design
We performed an ecological study using the Peruvian Ministry of Health database for the period 2008-2017. The database contains the death certificates from health centers across the 25 provinces of Peru. The information is available through its online platform: http://www.minsa.gob.pe/portada/transparencia/solicitud/, and provides the number of deaths aggregated into five age groups and by sex. Deaths from lung cancer were identified by the codes C33 and C34 of the International Classification of Diseases (ICD), 10th revision (1992).
The smoking prevalence from 2013 to 2017 was estimated using the databases from the Demographic and Family Health Survey (ENDES in Spanish), population-based annual survey ejecuted 25 administrative provinces of Peru, and conducted under model and methodology of the Demographic and Health Surveys Program (DHS Program) by the National Institute of Statistics and Information (INEI in Spanish). Information of smoking habits are extraacted from individuals aged 15 years or older . The complete details of the survey design and data can be found in the following website: http://iinei.inei.gob.pe/microdatos.
Setting
Peru is in the Andean region of South America, south of the equator line and on the coast of the Pacific Ocean. It is divided into 25 administrative provinces which are located across three major geographical regions: coast, highlands, and rainforest. The coast region only covers 11.7 % of the national territory, but it is the most populated region with approximately 56.3% of the total population of Peru. The highlands cover approximately 27.9% of the national territory, including 29.7% of the population. The rainforest is the largest region of the country, accounting for 60.3% of the national territory, but only contains 14% of the total population.
Statistical analysis
Age-standardized mortality rate (ASMR) per 100,000 person-years were analyzed using the direct method based on the world’s standard SEGI population (National Cancer Institute). Joinpoint mortality trends were estimated using the Joinpoint regression Program Version 4.7.0 (Magnani and Bianchi et al., 2015; Kim and Fay et al., 2000). We used the variable “ever smoking in the last 12 months” to estimate the smoking prevalence from 2013 to 2017. First, we aggregated the individual-level data into nine age groups (15-24, …, and 95-100). Then, an average weighted smoking prevalence was estimated for each province by sex and by age group.
Results
Between 2008 and 2017, Peru had an average of 2,728 deaths with mortality rates (per 100,000 person-years) of 11.63 among males and 9.22 among females (male-to-female ratio of 1.3). According to regions, the highest mortality rate was in the coast (13.15 for males and 10.32 for females). The highlands had a rate of 8.42 for males and 7.23 for females and the rainforest a rate of 8.75 for males and 5.32 for females (Table 1).
Table 1.
Lung Cancer Deaths and Mortality Rates in Peru and Its Geographical Areas from 2008 to 2017
| Geographical areas | Males | Females | Ratio (Male to Female) | ||
|---|---|---|---|---|---|
| Deaths | Rates | Deaths | Rates | ||
| Peru | 1444 | 11.63 | 1284 | 9.22 | 1.3 |
| Coastal region | 1092 | 13.15 | 982 | 10.32 | 1.3 |
| Ancash | 49 | 9.88 | 49 | 9.03 | 1.1 |
| Arequipa | 69 | 11.76 | 74 | 11.53 | 1 |
| Callao | 75 | 17.3 | 61 | 12.19 | 1.4 |
| Ica | 40 | 11.73 | 35 | 9.35 | 1.3 |
| La Libertad | 80 | 10.61 | 74 | 8.77 | 1.2 |
| Lambayeque | 58 | 10.82 | 50 | 8.32 | 1.3 |
| Lima | 622 | 14.97 | 564 | 11.32 | 1.3 |
| Moquegua | 7 | 7.4 | 9 | 11.04 | 0.7 |
| Piura | 65 | 9.25 | 47 | 6.21 | 1.5 |
| Tacna | 17 | 12.68 | 14 | 11.06 | 1.1 |
| Tumbes | 10 | 12.93 | 6 | 8.24 | 1.6 |
| Highlands region | 262 | 8.42 | 253 | 7.23 | 1.2 |
| Apurimac | 13 | 7.78 | 13 | 6.65 | 1.2 |
| Ayacucho | 20 | 9.17 | 23 | 8.42 | 1.1 |
| Cajamarca | 36 | 6.67 | 27 | 4.24 | 1.6 |
| Cusco | 33 | 6.09 | 38 | 6.48 | 0.9 |
| Huancavelica | 17 | 11.87 | 16 | 9.64 | 1.2 |
| Huanuco | 35 | 11.22 | 33 | 9.67 | 1.2 |
| Junin | 60 | 11.75 | 58 | 10.37 | 1.1 |
| Pasco | 12 | 11.22 | 10 | 9.74 | 1.2 |
| Puno | 35 | 6.3 | 35 | 5.51 | 1.1 |
| Rainforest region | 90 | 8.75 | 49 | 5.32 | 1.6 |
| Amazonas | 11 | 7.12 | 10 | 6.46 | 1.1 |
| Loreto | 36 | 11.13 | 16 | 5.38 | 2.1 |
| Madre de Dios | 3 | 6.21 | 2 | 5.44 | 1.1 |
| San Martin | 29 | 9.36 | 15 | 5.63 | 1.7 |
| Ucayali | 11 | 5.75 | 6 | 3.91 | 1.5 |
a, Annual average of deaths for a 10-year period (2008–2017); b, Age-standardized rates per 100,000 person-years.
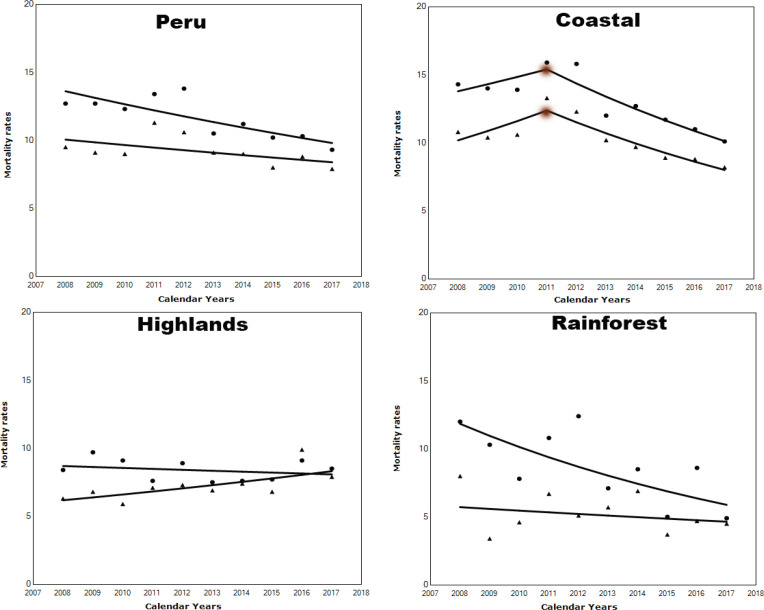
Figure 1 displays the mortality trends for lung cancer from Peru and its regions. Peruvian males had mortality rates above 10 per 100,000 person-years in most years, whereas females had rates above 8 per 100,000 person-years. Peru experienced a significant downward mortality trend in males (APC: −3.6% annually, 95%CI: −5.5, −1.6, p<0.05), whereas females had a downward trend, but not significant. The coast region experienced a downward trend since 2011 among males (APC: −6.8 annually, 95%CI: −10.4, −2.9, p<0.05) and females (APC: −7.0 annually, 95%CI: −9.6, −4.3, p=0.001). The highlands region had an upward trend among females since 2008 (APC: +3.4 annually, 95%CI: 0.7, 6.1, p<0.05), whereas males did not have significant changes. On the contrary, the rainforest region had a downward trend among males since 2008 (APC: −7.5 annually, 95%CI: −13.1, −1.5, p<0.05), whereas females did not have significant changes.
Figure 1.
Temporal Trends for Lung Cancer Mortality in Peru and Its Regions between 2008 and 2017 (● Males, and ▲ Females)
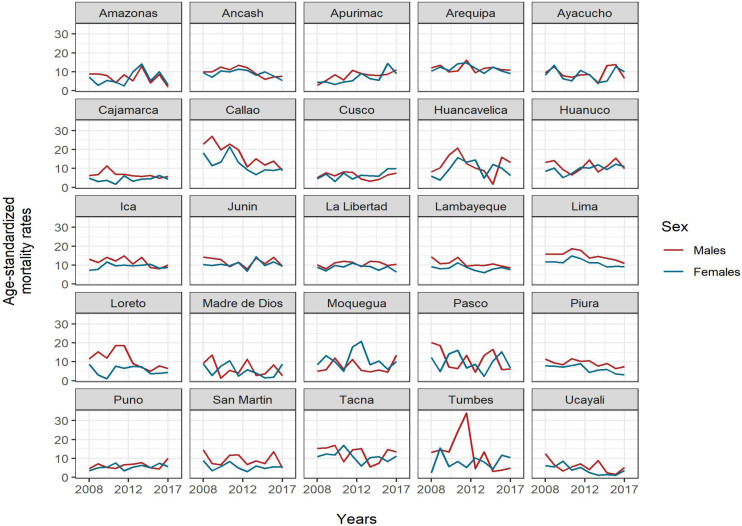
Table 2 shows the mortality trends of lung cancer in the Peruvian provinces. Among males, five coastal provinces showed significant downward trends annually. Ancash declined by 5.4%, Callao by 10%, Lambayeque by 4%, Piura by 4.5%, and Tumbes by 16.3%, while Lima declined by 7.3% from 2011 up to 2017. Apurimac (highlands province) showed a significant rise of 10.6%, whereas Loreto (rainforest province) declined by 10.2% annually. Among females, there was an annually significant decrease in Callao by 7.6%, and in Piura by 9.5%, moreover, a significant decrease was reported in Lima by 7.3% from 2011 until 2017. In contrast, Apurimac (highlands province had a significant rise of 11.6% in the whole period (Figure 2).
Table 2.
Temporal Trends for Lung Cancer Mortality from Peruvian Provinces. 2008–2017
| Geographical areas | Men | Women | ||||||
|---|---|---|---|---|---|---|---|---|
| Trend 1 | Trend 2 | Trend 1 | Trend 2 | |||||
| Years | APC (95%CI) | Years | APC (95%CI) | Years | APC (95%CI) | Years | APC (95%CI) | |
| Coastal region | ||||||||
| Ancash | 2008−2017 | −5.4* (−10.5, −0.1) | 2008−2015 | 1.7 (−6.6, 10.8) | 2015−2017 | −27.0 (−61.4, 38.2) | ||
| Arequipa | 2008−2017 | −0.9 (−5.0, 3.4) | 2008−2017 | −1.8 (−5.9, 2.4) | ||||
| Callao | 2008−2017 | −10.0* (−14.3, −5.6) | 2008−2017 | −7.6* (−13.7, −1.0) | ||||
| Ica | 2008−2017 | −4.3 (−8.4, 0.1) | 2008−2010 | 25.2 (−4.8, 64.6) | 2010−2017 | −2.7 (−6.2, 0.9) | ||
| La Libertad | 2008−2017 | 0.9 (−2.4, 4.4) | 2008−2017 | −1.5 (−5.8, 3.0) | ||||
| Lambayeque | 2008−2017 | −4.0* (−6.9, −1.1) | 2008−2017 | −2.1 (−6.1, 2.0) | ||||
| Lima | 2008−2011 | 5.7 (−5.6, 18.3) | 2011−2017 | −7.3* (−10.8, −3.7) | 2008−2011 | 7.0 (−5.4, 21.2) | 2011−2017 | −7.3* (−11.1, −3.3) |
| Moquegua | 2008−2017 | 1.0 (−9.6, 12.9) | 2008−2017 | −1.0 (−12.1, 11.5) | ||||
| Piura | 2008−2017 | −4.5* (−8.0, −0.9) | 2008−2017 | −9.5* (−14.5, −4.1) | ||||
| Tacna | 2008−2017 | −4.1 (−13.2, 6.0) | 2008−2017 | −2.8 (−9.1, 3.9) | ||||
| Tumbes | 2008−2017 | −16.3* (−29.2, −1.0) | 2008−2017 | 6.7 (−7.1, 22.6) | ||||
| Highlands region | ||||||||
| Apurimac | 2008−2017 | 10.6* (2.6, 19.2) | 2008−2017 | 11.6* (3.6, 20.3) | ||||
| Ayacucho | 2008−2017 | −1.3 (−11.1, 9.6) | 2008−2017 | −0.4 (−10.7, 10.9) | ||||
| Cajamarca | 2008−2017 | −4.1 (−8.7, 0.8) | 2008−2017 | 4.6 (−5.0, 15.1) | ||||
| Cusco | 2008−2017 | −1.7 (−9.7, 7.0) | 2008−2017 | 7.9 (−0.3, 16.8) | ||||
| Huancavelica | 2008−2017 | −4.3 (−20.7, 15.6) | 2008−2017 | 3.1 (−9.5, 17.4) | ||||
| Huanuco | 2008−2011 | −16.1 (−47.7, 34.5) | 2011−2017 | 6.9 (−8.9, 25.4) | 2008−2017 | 5.1 (−0.9, 11.5) | ||
| Junin | 2008−2017 | −2.3 (−7.4, 3.1) | 2008−2017 | 0.4 (−4.6, 5.7) | ||||
| Pasco | 2008−2017 | −7.8 (−19.3, 5.3) | 2008−2017 | −2.9 (−17.7, 14.6) | ||||
| Puno | 2008−2017 | 3.2 (−3.5, 10.4) | 2008−2017 | 4.0 (−2.3, 10.6) | ||||
| Rainforest region | ||||||||
| Amazonas | 2008−2017 | −8.3 (−19.4, 4.3) | 2008−2017 | 3.4 (−11.6, 20.9) | ||||
| Loreto | 2008−2017 | −10.2* (−17.6, −2.3) | 2008−2017 | 1.3 (−14.9, 20.7) | ||||
| Madre de Dios | 2008−2017 | −6.5 (−22.7, 13.1) | 2008−2017 | −7.7 (−22.8, 10.4) | ||||
| San Martin | 2008−2017 | −3.8 (−12.2, 5.5) | 2008−2017 | −1.8 (−10.2, 7.5) | ||||
| Ucayali | 2008−2017 | −10.8 (−22.5, 2.6) | 2008−2017 | −16.1* (−26.9, −3.7) | ||||
Figure 2.
Temporal Trends for Lung Cancer Mortality in Peruvian Provinces between 2008 and 2017
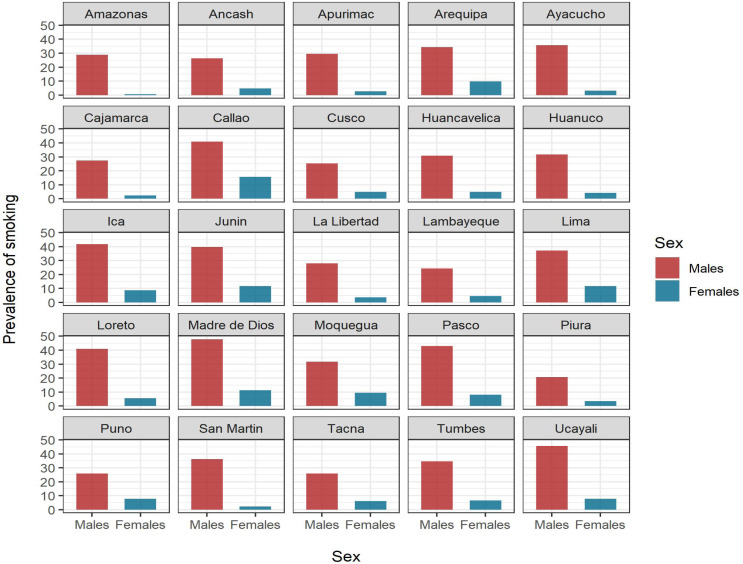
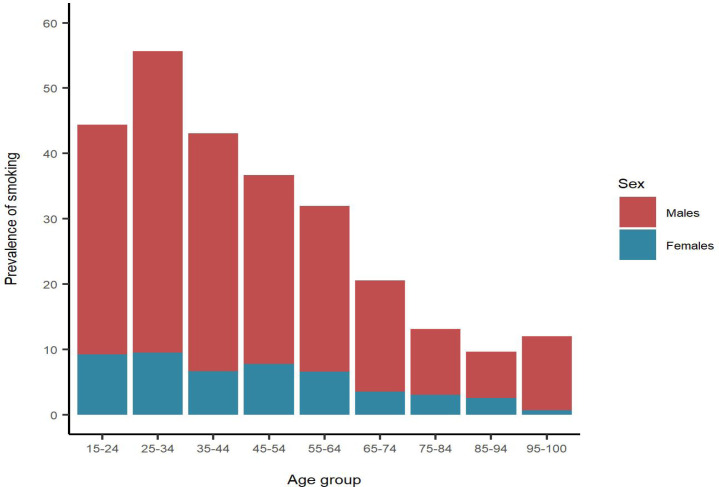
Smoking prevalence was higher in males than in females, ranging from 20–50% among males and 2–15% among females. Cajamarca, La Libertad, Piura, and San Martin had the lowest smoking prevalence in both genders. Rainforest provinces such as Madre de Dios and Ucayali had the highest prevalence among males (above 45%) and females (above 5%) (Figure 3). In addition, the 25-34 age group had the highest smoking prevalence (above 50% in males, and near 10% in females), followed by the 15-24 age group (above 40% in males, and near 10% in females) (Figure 4).
Figure 3.
Smoking Prevalence by Sexes for Peruvian Provinces in 2017
Figure 4.
Smoking Prevalence According Age Group in Peru
Discussion
Our study provides a temporal analysis of lung cancer mortality rates as well as the smoking prevalence for Peru and its geographical areas. Mortality trends varied according to geographical regions and sex, e.g. Highlands region females had a significant upward mortality trend, but a downward trend in coast region. In contrast, males experienced downward mortality trends in coast and rainforest region. Moreover, males still have higher lung cancer mortality rates than females, except in Moquegua and Cusco. Smoking prevalence is high among young adults.
We found lower mortality rates than European and some Latin American countries. Malvezzi et al., (2017) found that European males had a mortality rate above 30 per 100,000 males, whereas females had a mortality rate above 10 per 100,000 females. In Latin America, only Argentina and Cuba had similar mortality rates to European countries (Carioli and Bertuccio 2020; Carioli and La Vecchia, 2017), while Colombia and Mexico reported lower mortality rates than our study (Carioli and Bertuccio, 2020; Carioli and La Vecchia 2017). These studies did not include Peru (Carioli and Bertuccio, 2020; Carioli and La Vecchia, 2017), probably because of the under-reporting death certification reported (Torres-Roman and Gomez-Rubio et al., 2020; Ruiz and Torres-Roman et al., 2019). In this study, we corrected the under-reporting, providing the first large study of lung cancer mortality from Peru.
The reasons for the downward mortality trends for lung cancer in our population could be related to the implementation of public health programs and policies, the rise of the human development index (HDI), and the different levels of exposure to established risk factors for lung cancer. Peru has made pivotal public health achievements towards controlling tobacco consumption in the last three decades. The government enacted several laws from 1991 to 1998 that prohibited smoking in public places and prevent exposure to tobacco (Congreso de la República, 1991; Congreso de la República ,1997; Congreso de la República, 1997; Congreso de la República 1998). Subsequently, the implementation of the Plan Esperanza in 2012 provided funding for the development of health promotion and prevention campaigns, as well as to provide resources to increase diagnosis and access to treatment cost for several neoplasms, including lung cancer, reducing the out-of-pocket expenditure for vulnerable populations in low-economic settings (Vidaurre and Santos et al., 2017). The combination of these efforts has made improvements in the delivery of healthcare services that could explain the downward trends found in our analysis. Of these interventions, the smoking restriction efforts have probably had the highest impact (Jemal and Thun et al., 2008; Feuer and Levy et al., 2012), and can explain the changes observed around 2005. Another explanation is the relationship between the HDI and mortality trends for lung cancer (Wong and Lao et al., 2017). Wong et al., (2017) identified that the countries with a high HDI reported decreases in the mortality rates, while countries with low HDI have not shown favorable trends. Peru’s HDI shifted from a medium category during the 90s to a high category in the early 2000s (United Nations Development Programme 2019); hence, it is plausible that the increase in HDI may have influenced the mortality reduction over time.
Despite declining mortality trends, males still have higher rates compared to females. But the male-to-female ratio found in Peru was 1.33, probably due to the reduction in the prevalence of smoking in men, but not in women. This ratio is lower than in other Latin American countries. In the last 10 years, Argentina tripled the mortality rates in males compared to females, whereas Brazil, Chile, Cuba, and Mexico doubled this ratio. These findings are consistent in previous studies (Hernández-Garduño and Ocaña-Servín, 2018; Ruoyi and Baosen, 2014; Aareleid and Zimmermann et al., 2017). The difference in lung cancer mortality by sex reflects the variable degree of exposure to risk factors such as tobacco use or smoking habits between males and females (Thun and Carter et al., 2013). The latest report of the American Cancer Society and Vital Strategies identified that the daily use of tobacco remains higher in Peruvian males than females (11.9% vs. 4.2%) (Drope and Schluger et al., 2018), which explains the higher mortality rates seen in males. Moreover, the observed lung cancer mortality trends in our study reflect the prevalence of past tobacco use. Another highlights of our study was that the young population had a higher smoking prevalence compared to older population. Which means that the young population with concurrent smoking habits are at risk of developing lung cancer in the coming decades. In a study focused on the young population of Lima, it stands out that among the tumors with the highest mortality in men is lung cancer. A segment where this diagnosis is not so common (Luna-Abanto and Ruiz et al., 2020)
Although Latin America has implemented effective control measures against tobacco (Burki, 2017), there is still room for improvement, especially in the provinces with smoking prevalence as high as 50%. For this reason, Peru should implement public health programs to lower smoking prevalence, with the final aim to reduce the morbidity and mortality of lung cancer (Pichon-Riviere and Bardach et al., 2016), and reduce the financial impact of smoking on the health system in Peru (Pichon-Riviere and Bardach, 2016).
The marked geographic variability of the mortality rates of lung cancer in Peru probably highlights the different prevalence of well-known risk factors (asbestos, radon, fumes from biomass fuels, air pollution), besides tobacco (Barone-Adesi and Chapman et al., 2012; Grosche and Kreuzer et al., 2006; Barcenas and Delclos et al., 2005; Raaschou-Nielsen and Andersen et al., 2013). To date, Peru continues to use chrysotile asbestos (Torres-Roman and Gomez-Rubio 2020), which hampers the reduction of mortality rates of lung cancer, diminishing the benefits of the enacted health policies against smoking tobacco. Less attention, but with probable greater impact, is the outdoor environmental pollution with air quality levels among the worst in Latin America (50 µg / m3 PM2.5 in Lima 2005-2011) (Gonzales and Steenland, 2014). On the other hand, indoor pollution derived from the use of biomass fuels for cooking or heating rooms still occurs in a third of the population (Gonzales and Steenland, 2014). The Pan American Health Organization, the World Health Organization, and the German Development Cooperation Agreement found that pollution using biomass fuel is a risk factor for the development of lung cancer (Kim and Jahan et al., 2011). There are multiple reports that point to wood or charcoal smoke indoors exposure as a risk factor for lung cancer (Arrieta and Campos-Parra et al., 2012; Hernandez-Garduno and Brauer et al., 2004; Arrieta and Cardona et al., 2015; Arrieta and Cardona et al., 2011; Corrales and Rosell et al., 2020). In this populations, it has been associated with EGFR gene alterations, specifical mutations in exon 21 or deletions of exon 19, associated with non-smokers, females, and adenocarcinoma histology (Arrieta and Cardona, 2015; Arrieta and Cardona, 2011). In Latin America, several studies have reported an intermediate range of EGFR gen alterations between Asia and Caucasian populations, with frequencies between 19% (Argentina) and 60% (Peru) (Arrieta and Cardona, 2011). In fact, studies with a greater number of cases have consistently reported elevated frequencies in Peru (between 51.1 and 32% of EGFR gene alterations) (Arrieta and Cardona, 2015; Mas and Piscocha et al., 2017). In the Peruvian region of the highlands, families use biomass fuels for cooking, which is a more common task for the female population. This scenario places females, who are directly in contact with food cooking, at a high level of exposure to smoke, dust, and gases, which has a negative impact on their health. Therefore, this risk factor could be responsible for the increase in the mortality rates in females in the highlands regions reported here. More epidemiological data is required to establish this possible relationship in our population between exposure to wood smoke and this high frequency of alterations in the EGFR gene, which is not the objective of the current work.
Future directions
Improved cancer mortality registration in various geographic areas of Peru remains a requirement for monitoring its trends. Tobacco control and eventual elimination is the key issue for reducing lung cancer mortality. Moreover, the control of biomass fuels and prohibition of the use of chrysotile asbestos.
Limitations
Our study has some limitations. The lack of information on new cases of lung cancer limits the estimation or other parameters like incidence or mortality-to-incidence ratio. Moreover, we used a secondary database, which is subject to underreporting. However, we applied data correction as previous studies (Torres-Roman and Gomez-Rubio 2020,Ruiz and Torres-Roman 2019), which reduces the bias of sub-registry. In addition, we do not have information on smoking prevalence in previous decades, which did not allow us to evaluate the temporal trend of this habit in the Peruvian population.
In conclusion, our study shows that Peru had downward mortality trends for lung cancer, mainly in males. In addition, some regions and provinces are increasing their mortality rates. Peru had a high smoking prevalence, principally among young adults. Primary care interventions are important to reduce the smoking prevalence, which will decrease lung cancer mortality rates.
Author Contribution Statement
J. Smith Torres-Roman: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing - original draft, Writing - review & editing. Bryan Valcarcel: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing - original draft, Writing - review & editing. Jose F. Martinez-Herrera: Investigation, Writing - original draft, Writing - review & editing. Janina Bazalar-Palacios: Investigation, Writing - original draft, Writing - review & editing. Carlo La Vecchia: Supervision, Writing - original draft, Writing - review & editing. Luis E. Raez: Supervision, Writing - original draft, Writing - review & editing.
Acknowledgments
Not applicable.
Availability of data
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. You can also request the raw data through the following form: https://www.minsa.gob.pe/portada/transparencia/solicitud/, placing your personal data and the information to be requested
Any conflict of interest
None.
References
- Aareleid T, Zimmermann M-L, Baburin A, et al. Divergent trends in lung cancer incidence by gender, age and histological type in Estonia: a nationwide population-based study. BMC Cancer. 2017;17:596. doi: 10.1186/s12885-017-3605-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arrieta O, Campos-Parra AD, Zuloaga C, et al. Clinical and pathological characteristics, outcome and mutational profiles regarding non–small-cell lung cancer related to wood-smoke exposure. J Thorac Oncol. 2012;7:1228–34. doi: 10.1097/JTO.0b013e3182582a93. [DOI] [PubMed] [Google Scholar]
- Arrieta O, Cardona AF, Bramuglia GF, et al. Genotyping non-small cell lung cancer (NSCLC) in Latin America. J Thorac Oncol. 2011;6:1955–9. doi: 10.1097/JTO.0b013e31822f655f. [DOI] [PubMed] [Google Scholar]
- Arrieta O, Cardona AF, Martín C, et al. Updated frequency of EGFR and KRAS mutations in nonsmall-cell lung cancer in Latin America: the Latin-American Consortium for the Investigation of Lung Cancer (CLICaP) J Thorac Oncol. 2015;10:838–43. doi: 10.1097/JTO.0000000000000481. [DOI] [PubMed] [Google Scholar]
- Barcenas CH, Delclos GL, El-Zein R, et al. Wood dust exposure and the association with lung cancer risk. Am J Ind Med. 2005;47:349–57. doi: 10.1002/ajim.20137. [DOI] [PubMed] [Google Scholar]
- Barone-Adesi F, Chapman RS, Silverman DT, et al. Risk of lung cancer associated with domestic use of coal in Xuanwei, China: retrospective cohort study. BMJ. 2012:345. doi: 10.1136/bmj.e5414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- Bray F, Piñeros M. Cancer patterns, trends and projections in Latin America and the Caribbean: a global context. Salud Publica Mex. 2016;58:104–17. doi: 10.21149/spm.v58i2.7779. [DOI] [PubMed] [Google Scholar]
- Burki TK. Latin America makes progress on tobacco control. Lancet Respiratory Med. 2017;5:470. doi: 10.1016/S2213-2600(17)30160-1. [DOI] [PubMed] [Google Scholar]
- Carioli G, Bertuccio P, Malvezzi M, et al. Cancer mortality predictions for 2019 in Latin America. Int J Cancer. 2020;147:619–32. doi: 10.1002/ijc.32749. [DOI] [PubMed] [Google Scholar]
- Carioli G, La Vecchia C, Bertuccio P, et al. Cancer mortality predictions for 2017 in Latin America. Ann J Eur Soc Med Oncol. 2017;28:2286–97. doi: 10.1093/annonc/mdx301. [DOI] [PubMed] [Google Scholar]
- Congreso de la República. Ley No. 26957. Ley que prohíbe la venta de productos elaborados con tabaco a menores de edad. El Peruano. 1998. [Google Scholar]
- Corrales L, Rosell R, Cardona AF, et al. Lung cancer in never smokers: The role of different risk factors other than tobacco smoking. Crit Rev Oncol Hematol. 2020;148:02895. doi: 10.1016/j.critrevonc.2020.102895. [DOI] [PubMed] [Google Scholar]
- Costa e Silva VLd, Koifman S. Smoking in Latin America: a major public health problem. Cad Saude Publica. 1998;14:S109–S15. [PubMed] [Google Scholar]
- Feuer EJ, Levy DT, McCarthy WJ. Chapter 1: the impact of the reduction in tobacco smoking on US Lung cancer mortality, 1975–2000: an introduction to the problem. Risk Anal. 2012;32:6–13. doi: 10.1111/j.1539-6924.2011.01745.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales GF, Steenland K. Environmental health in Peru: outdoor and indoor air contamination. Rev Panam Salud Publica. 2014;36:141. [PubMed] [Google Scholar]
- Grosche B, Kreuzer M, Kreisheimer M, et al. Lung cancer risk among German male uranium miners: a cohort study, 1946–1998. Br J Cancer. 2006;95:1280–7. doi: 10.1038/sj.bjc.6603403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez-Garduno E, Brauer M, Perez-Neria J, et al. Wood smoke exposure and lung adenocarcinoma in non-smoking Mexican women. Int J Tuberc Lung Dis. 2004;8:377–83. [PubMed] [Google Scholar]
- Hernández-Garduño E, Ocaña-Servín HL. Lung cancer mortality trends in Mexico, 1999-2014. Salud publica de Mexico. 2018;60:366–9. doi: 10.21149/8730. [DOI] [PubMed] [Google Scholar]
- Islami F, Torre LA, Jemal A. Global trends of lung cancer mortality and smoking prevalence. Transl Lung Cancer Res. 2015;4:327. doi: 10.3978/j.issn.2218-6751.2015.08.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemal A, Thun MJ, Ries LA, et al. Annual report to the nation on the status of cancer, 1975–2005, featuring trends in lung cancer, tobacco use, and tobacco control. J Natl Cancer Inst. 2008;100:1672–94. doi: 10.1093/jnci/djn389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim HJ, Fay MP, Feuer EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19:335–51. doi: 10.1002/(sici)1097-0258(20000215)19:3<335::aid-sim336>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- Kim K-H, Jahan SA, Kabir E. A review of diseases associated with household air pollution due to the use of biomass fuels. J Hazard Mater. 2011;192:425–31. doi: 10.1016/j.jhazmat.2011.05.087. [DOI] [PubMed] [Google Scholar]
- Luna-Abanto J, Ruiz LG, Laura-Martinez J, et al. Cancer incidence and mortality trends in young adults in Metropolitan Lima young adults, 1990–2012. Ecancermedicalscience. 2020:14. doi: 10.3332/ecancer.2020.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malvezzi M, Carioli G, Bertuccio P, et al. European cancer mortality predictions for the year 2017, with focus on lung cancer. Ann Oncol. 2017;28:1117–23. doi: 10.1093/annonc/mdx033. [DOI] [PubMed] [Google Scholar]
- Mao Y, Yang D, He J, et al. Epidemiology of lung cancer. Surg Oncol Clin. 2016;25:439–45. doi: 10.1016/j.soc.2016.02.001. [DOI] [PubMed] [Google Scholar]
- Mas L, Piscocha C, Landa J, et al. Prevalence of EGFR mutations in the Peruvian population: Study in a large cohort of patients with NSCLC. Am Soc Clin Oncol. 2017:2017. [Google Scholar]
- Palloni A, Novak B, Pinto-Aguirre G. The enduring effects of smoking in Latin America. Am J Public Health. 2015;105:1246–53. doi: 10.2105/AJPH.2014.302420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pichon-Riviere A, Bardach A, Augustovski F, et al. Impacto económico del tabaquismo en los sistemas de salud de América Latina: un estudio en siete países y su extrapolación a nivel regional. Rev Panam Salud Publica. 2016;40:213–21. [PubMed] [Google Scholar]
- Programa de las Naciones Unidas para el Desarrollo. El Reto de la Igualdad: Una lectura de las dinámicas territoriales en el Perú Lima: PNUD. 2019. [Google Scholar]
- Raaschou-Nielsen O, Andersen ZJ, Beelen R, et al. Air pollution and lung cancer incidence in 17 European cohorts: prospective analyses from the European Study of Cohorts for Air Pollution Effects (ESCAPE) Lancet Oncol. 2013;14:813–22. doi: 10.1016/S1470-2045(13)70279-1. [DOI] [PubMed] [Google Scholar]
- Raez LE, Cardona AF, Santos ES, et al. The burden of lung cancer in Latin-America and challenges in the access to genomic profiling, immunotherapy and targeted treatments. Lung Cancer. 2018;119:7–13. doi: 10.1016/j.lungcan.2018.02.014. [DOI] [PubMed] [Google Scholar]
- Ruiz EF, Torres-Roman JS, Servan SA, et al. Trends and geographic pattern of stomach cancer mortality in Peru. Cancer Epidemiol. 2019;58:193–8. doi: 10.1016/j.canep.2018.10.018. [DOI] [PubMed] [Google Scholar]
- Ruoyi Q, Baosen Z. Analysis of the distribution and trend of lung cancer mortality in China between 2004 and 2010. Chin J Health Statist. 2014;31:932–5. [Google Scholar]
- Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021 doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med. 2013;368:351–64. doi: 10.1056/NEJMsa1211127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres-Roman JS, Gomez-Rubio V, Sanchez-Trujillo L, et al. Geographic study of mortality due to mesothelioma in Peru and its evolution. Cancer Epidemiol. 2020;68:101791. doi: 10.1016/j.canep.2020.101791. [DOI] [PubMed] [Google Scholar]
- United Nations Development Programme. Human Development Report 2019. USA: UNDP; 2019. [Google Scholar]
- Vidaurre T, Santos C, Gómez H, et al. The implementation of the Plan Esperanza and response to the imPACT Review. Lancet Oncol. 2017;18:e595–e606. doi: 10.1016/S1470-2045(17)30598-3. [DOI] [PubMed] [Google Scholar]
- Wong MC, Lao XQ, Ho K-F, et al. Incidence and mortality of lung cancer: global trends and association with socioeconomic status. Sci Rep. 2017;7:1–9. doi: 10.1038/s41598-017-14513-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. International Classification of Disease and Related Health Problems: 10th Revision. Geneva: World Health Organization; 1992. [Google Scholar]
- Zafra-Tanaka JH, Tenorio-Mucha J, Villarreal-Zegarra D, et al. Cancer-related mortality in Peru: Trends from 2003 to 2016. PLoS One. 2020;15:e0228867. doi: 10.1371/journal.pone.0228867. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request. You can also request the raw data through the following form: https://www.minsa.gob.pe/portada/transparencia/solicitud/, placing your personal data and the information to be requested