Abstract
We sought to evaluate the sagittal plane knee joint loading patterns during a double-leg landing task among young athletes who passed or failed return-to-sport (RTS) criteria following ACL reconstruction (ACLR), and in uninjured athletes. Participants completed quadriceps strength testing, a hop test battery, and the International Knee Documentation Committee subjective form following medical RTS clearance. ACLR participants ‘passed’ RTS criteria (RTS-PASS) if they met ≥90 limb symmetry (%) or score on all measures and were categorized as ‘failing’ (RTS-FAIL) if not. All participants completed three-dimensional motion analysis testing. Sagittal plane kinematic and kinetic variables were calculated during a double-leg drop vertical jump task. Mean limb values and limb symmetry indices (LSI; %) were calculated and compared using a one-way ANOVA (for LSI) and mixed between-within ANOVA (for group x limb differences). 205 participants were included, with 39 in the RTS-PASS group, 109 in the RTS-FAIL group, and 57 CTRLs. The RTS-FAIL group demonstrated lower symmetry values for peak vertical ground reaction force, peak internal knee extension moment, and peak knee flexion angle. Group x limb interactions were observed for peak vertical ground reaction force and peak internal knee extension moment. Involved limb values were reduced in the RTS-PASS and RTS-FAIL groups compared to CTRLs, while the RTS-PASS groups had lower uninvolved limb values compared to the RTS-FAIL and CTRLs.
Clinical Significance:
Young athletes who pass RTS criteria after ACLR land symmetrically during a double-leg task, but symmetry was achieved by reducing loading on both limbs.
Keywords: ACL reconstruction, biomechanics, kinetics, kinematics, joint loading, return-to-sport criteria
INTRODUCTION
Young athletes following anterior cruciate ligament reconstruction (ACLR) commonly demonstrate altered movement mechanics compared to uninjured athletes during daily and sports-related tasks.1 Altered movement patterns and between-limb asymmetries in joint loading strategies are observed at the time of return-to-sport (RTS) clearance and for up to 2-years following ACLR2–5 during gait,6 running,7 and landing tasks.4,5,8–10 Previous work demonstrates between-limb asymmetries in limb loading strategies during performance of bilateral landing tasks at the time of RTS clearance after ACLR.2,11 However, it is not understood if passing commonly used RTS criteria coincides with symmetrical joint loading strategies during sports-related tasks. Further, the focus on between-limb symmetry in evaluating movement mechanics limits understanding of each limb’s contribution to the observed movement pattern or joint loading strategy.
Persistent alterations in movement mechanics after ACLR are important to address in rehabilitation given the association with worse longitudinal outcomes. At the time of release to RTS, asymmetry in knee moments at the time of initial contact during a double-limb landing were one of four variables that predicted second ACL injury within the subsequent 12-months.8 In the long-term, altered sagittal plane knee movement patterns and limb loading strategies are associated with reduced knee-related function and markers of tibiofemoral cartilage degeneration in individuals after ACLR.5,9,12 In young individuals after ACLR, asymmetries (reduced in the involved limb) in knee flexion motion during landing at the time of RTS was associated with worse knee-related function two years later.10 Further, reduced involved limb loading (via reduced vertical ground reaction force and internal knee extension moments) during a bilateral drop landing task at 6-months post-ACLR were associated with worsening knee cartilage structural composition three years later.13 Vertical ground reaction force offers an indication of between-limb distribution of overall limb loading during a double limb task, which is commonly reduced on the involved limb, and shifted to the uninvolved limb, following ACLR.11,13 Reduced internal knee extension moments during landing are commonly observed in young individuals at the time of RTS following ACLR, and are associated with asymmetries in quadriceps femoris strength.1,2
Young athletes following ACLR also demonstrate persistent deficits in clinical measures, namely deficits in thigh muscle strength2–4,14,15 and reduced knee-related function.16 Adequate strength, knee-related function, and performance on functional tests through RTS test batteries are recommended to evaluate readiness to resume sporting activities after ACLR.17–19 Despite young athletes struggling to meet the most common RTS test batteries;20,21 the utility of current RTS criteria to reduce risk of second ACL injuries remains unclear.18,22 Missing from published RTS criteria are aspects of movement quality and joint loading,17,18,23 despite multiple reviews encouraging the inclusion of biomechanical assessment in RTS decision-making.18,19,24 However, it remains unknown if passing commonly used RTS criteria coincides with both symmetrical and normalized movement patterns and knee joint loading strategies during sports-related tasks. Previous work has focused on alterations in movement mechanics with respect to between-limb symmetry,2,4–6 which limits understanding of each limb’s contribution to the observed movement pattern or joint loading strategy. Understanding the contribution of each limb to joint loading strategies based on an athletes RTS test performance (i.e. pass or fail) will provide critical knowledge regarding if current RTS criteria could serve as a sufficient proxy, indicating normalized movement patterns and knee joint loading in preparation for RTS.
Therefore, the purpose of this study was to assess if performance (pass or fail) on a battery of commonly used RTS criteria, in young athletes following ACLR, coincides with restoration of lower limb (both involved and uninvolved limb) movement mechanics during a bilateral landing task, with respect to uninjured individuals. Based on previous work reporting that individuals after ACLR who did not pass RTS criteria demonstrated reduced knee joint loading during gait,6 we hypothesized that 1) young athletes who passed commonly used RTS criteria, inclusive of strength and functional performance symmetry, would demonstrate similar sagittal plane movement patterns and limb loading strategies compared to uninjured individuals on both limbs and 2) young athletes who fail RTS criteria would demonstrate sagittal plane movement patterns and limb loading strategies that underload the involved limb compared to the uninvolved limb, and compared to those who pass RTS criteria and uninjured controls.
METHODS (Secondary Analysis of a Prospective Cohort Study, Level of Evidence 1b)
Participants
Two hundred and five individuals in the ACL REconstruction Long-term outcomes in Adolescents and Young adults (ACL-RELAY) Study were analyzed as part of this secondary analysis. The ACL-RELAY Study, a collaboration between Ohio State University and Cincinnati Children’s Hospital Medical Center, is an ongoing, prospective cohort study examining outcomes after ACLR, collecting injury, clinical, and biomechanical data beginning at the time of medical clearance for full sports participation. Participants in the ACL-RELAY Study are recruited from local orthopaedic practices and physical therapy clinics in the greater Cincinnati and Northern Kentucky areas at the time of medical RTS clearance after primary, unilateral ACLR.
To be enrolled, ACLR participants are required to have completed a formal rehabilitation program, have been cleared for return to any-level of athletic activities by their respective orthopaedic surgeon and treating rehabilitation specialist, and whose goal is to return to cutting and pivoting sports on a regular basis of at least 50 hours/year. Neither the rehabilitation program, nor the decision for clearance to participate in sports, are controlled by the ACL-RELAY Study. Participants may, or may not, have undergone any formal or objective RTS testing prior to being medically cleared for sports participation by their respective medical team. Individuals with bone-patellar tendon-bone autograft, hamstring tendon autograft, or allograft are included, as well as those with and without meniscus repair or partial meniscectomy at the time of ACLR. Individuals are excluded from testing if they have a history of: 1) low back pain or 2) a lower extremity injury or surgery (besides the primary ACL injury) requiring the medical management by a physician within the past year, 3) a concomitant knee ligament injury (beyond grade 1 medial collateral ligament injury) in the involved limb. For these analyses, participants who underwent a modified ACLR procedure due to open epiphyseal plates in the tibia and/or femur were also excluded.
Uninjured and active individuals between 14 and 25 years of age were previously recruited from the community to serve as the control group (CTRL). Individuals were included in this group if they had no history of low back surgery, surgery to either lower extremity, and no history of injury requiring the care of a physician in the past year to either the low back or lower extremities. They also must have reported regular participation (≥ 50 hours/year) in cutting and pivoting sports. The study protocol was approved by the Institutional Review Board of Cincinnati Children’s Hospital Medical Center, and all participants and guardians, when required, provided written, informed consent/assent.
Study Testing
For the current analyses, all participants completed one laboratory testing session. For the ACLR group, study testing occurred within 4 weeks of medical RTS clearance. The involved limb was identified as the surgically reconstructed knee in the ACLR group and the “test” limb of the CTRL group was identified as the non-preferred landing limb.25
Return to Sport Criteria
The battery of tests included quadriceps strength assessment, single-leg hop tests (single, triple, and cross-over hops for distance and 6-meter timed hop), and the International Knee Documentation Committee subjective knee form (IKDC) score.18
Isometric quadriceps strength was assessed using an electromechanical dynamometer (Biodex Medical Systems, Inc, Shirley, NY) at 60° of knee flexion.11 Participants were secured in the dynamometer with the trunk supported, the hips flexed to 90°, the knee joint aligned with the dynamometer axis, and the dynamometer resistance pad secured to the distal shank. Real-time visual feedback and verbal encouragement was provided during the test to encourage maximal effort by the participant. Three recorded maximal-effort trials were completed for each knee (5 seconds in duration, separated by 15 seconds of rest). The average of the peak torque values from all 3 test trials was used to calculate quadriceps strength limb symmetry index (LSI, ratio of the performance of the involved/test and uninvolved/non-test limbs x 100%), with a LSI<100% in the ACLR group indicating involved limb strength deficits.
The single-leg hop test battery consisted of four tests (single, triple, cross-over hops for distance and 6-m timed hop) that are commonly used clinically, with good reliability in those following ACLR.26 Hop testing was performed in random order with each participant completing 2 practice trials and then 2 measurement trials on each limb. The average of the 2 test trials was used to calculate a LSI for each hop test, with a LSI<100% in the ACLR group indicating deficits in involved limb performance.
The IKDC score evaluated patient-reported knee function27,28 and is scored on a 0-to-100 scale, with 100 representing higher knee function.29,30 The IKDC score has been shown to be a reliable and valid measure of knee function in those following ACL injury.27,28
We established objective criterion cutoffs to determine which ACLR participants passed RTS criteria based on recommendations in the literature.19 ACLR participants were categorized as passing RTS criteria (RTS-PASS group) if they met ≥90% LSI on quadriceps strength and each of the hop tests, as well as scored ≥90 on the IKDC. Failing RTS criteria (RTS-FAIL group) occurred if at least one criterion was not met.20,31
3-Dimensional Motion Analysis
Testing.
At the same testing session, participants completed 3-dimensional motion analysis during a bilateral drop vertical jump (DVJ) task. Kinematic data were collected using a 12-camera motion capture system (Eagle cameras, Motion Analysis Corporation Santa Rosa, California) sampled at 240 Hz. Each participant was first instrumented with 37 retro-reflective markers secured to the bilateral upper extremities, trunk, pelvis, and lower extremities which were used to calculate joint centers and track segment motion during each task. For the DVJ task, participants were positioned on top of a 31-cm box, placed adjacent to the force plates, and executed practice trials followed by 3 measurement trials. Participants were instructed to drop off the box with both limbs simultaneously and upon landing, immediately execute a maximal-effort vertical jump toward an overhead target. Participants were positioned to land with each foot on separate force platforms (AMTI, Watertown, Massachusetts) to collect ground reaction force data (sampled at 1200 Hz and synchronized with the motion capture system). Variables of interest were calculated during initial contact and weight-acceptance portions of the landing phase. Initial contact was defined as the point in time where the vertical ground reaction force >10 N. Weight acceptance was the time from initial contact on the force plate until the body’s center of mass was at its lowest position. Similar methods have been published previously in individuals following ACLR.4,5,8,32
Variables of Interest.
Variables were established a priori and based on previous work linking these variables to longitudinal outcomes.2,5,8,24 Kinematic variables included knee flexion angle at initial contact (degrees) and peak knee flexion angle (degrees) during weight acceptance.10 Kinetic variables included peak vertical ground reaction force during weight acceptance (N/kg), internal knee moment at initial contact (Nm/kg), and peak internal knee extension moment (Nm/kg) during weight acceptance.2,5,8,24
Data Processing.
Biomechanical variables were calculated using Visual3D (v 5.0; C-Motion Inc) and custom-written MATLAB scripts (v 8.4; The MathWorks Inc). Marker trajectories and force plate data were low-pass filtered using a zero-lag, fourth-order Butterworth digital filter at 12 Hz and 50 Hz, respectively. Joint moments were calculated using inverse dynamics from the filtered marker trajectories and force plate data (12 Hz). Previous work with identical data processing methodology demonstrated high reliability in obtaining variables identified for this analysis.2,4,5,32 Limb values were calculated for each group and measures of between-limb symmetry were evaluated with LSI values (involved/test limb value/uninvolved/test limb value*100%).
Statistical Analysis
Statistical analyses were performed using SPSS (v21.0; IBM SPSS Statistics). Descriptive analysis of demographic data consisted of calculating frequencies and percentages for categorical data and means and standard deviations for continuous data. Categorical variables were evaluated with Pearson Chi-Square tests. Participant demographic and symmetry data were compared among the RTS-PASS, RTS-FAIL, and CTRL groups using a one-way analysis of variance (ANOVA), with multiple comparison analysis via Bonferroni post-hoc comparisons to identify between group differences (p≤ 0.05). A mixed between-within subjects (3×2) ANOVA analyzed group (RTS-PASS vs. RTS-FAIL vs. CTRL) by limb (involved/test limb vs. uninvolved/non-test limb) differences in each biomechanical variable (p≤ 0.05). Additional analyses were used to examine group and limb interactions consisting of one-way ANOVA, with Tukey’s multiple comparison tests (p≤ 0.05), and paired t-tests with a Bonferroni-corrected p-value (p≤ 0.0167).
RESULTS
Participant and Group Demographics
A total of 205 young athletes met inclusion for this analysis (n=148 ACLR, n=57 CTRL). The majority of participants were female (n=142, 69.3%). (TABLE 1) The RTS-PASS group (n=39) was 2.1 years younger than the RTS-FAIL group (n=109) (p=0.001) and 1.7 years younger than the CTRL group (p=0.017). The RTS-FAIL group was 6.5 kg heavier than the CTRL group (p= 0.017). The RTS-PASS group had a higher proportion of hamstring autografts (n=35, 90%) compared to the RTS-FAIL group (n=47, 43%) (p= 0.001), but the RTS-PASS group had a lower proportion of bone-patellar tendon-bone (BPTB) autografts (n=4, 10%) compared to the RTS-FAIL group (n=51, 47%) (p< 0.0001). No other demographic differences were found among groups (TABLE 1).
TABLE 1.
Athlete Demographics Between RTS-PASS, RTS-FAIL and Control Groups
| RTS Status | PASS | FAIL | CTRL | P-value (ANOVA) |
|---|---|---|---|---|
| n | 39 (19.0%) | 109 (53.2%) | 57 (27.8%) | - |
| Biologic sex, n (% female) | 22 (56.4%) | 78 (71.6%) | 42 (73.7%) | 0.15$ |
| Age (years) | 15.4 ± 2.4 | 17.5±3.4 | 17.2±2.5 | 0.001 a,b |
| Height (cm) | 165.1 ± 12.1 | 167.8±10.1 | 166.5±8.8 | 0.33 |
| Weight (kg) | 61.9 ± 14.6 | 67.9±15.1 | 61.4±11.9 | 0.007 c |
| Months from surgery to RTS | 7.4 ± 1.6 | 6.9±2.1 | - | 0.28 |
| Graft Type, n (%) | AL: 0 (0%) HS: 35 (90%) PT: 4 (10%) |
AL: 11 (10%) HS: 47 (43%) PT: 51 (47%) |
- | <0.0001 $ |
| Meniscus Injury, n (%) | 15 (38.5%) | 58 (53.2%) | - | 0.11$ |
| IKDC | 97.6 ± 2.5 | 85.3 ± 11.0 | 96.3 ± 8.0 | <0.0001 a,c |
| QF strength LSI (%) | 104.7 ± 11.0 | 87.2 ± 16.7 | 98.8 ± 9.1 | <0.0001 a,c |
| Single Hop LSI (%) | 100.0 ± 5.4 | 92.8 ± 6.5 | 100.6 ± 5.6 | <0.0001 a,c |
| Triple Hop LSI (%) | 99.7 ± 5.1 | 93.9 ± 6.7 | 100.7 ± 5.4 | <0.0001 a,c |
| Crossover Hop LSI (%) | 99.2 ± 4.5 | 93.7 ± 9.4 | 100.1 ± 5.6 | <0.0001 a,c |
| Timed Hop LSI (%) | 100.8 ± 5.1 | 95.2 ± 7.7 | 100.8 ± 7.2 | <0.0001 a,c |
data are reported as mean ± standard deviation, unless otherwise noted
ANOVA= Analysis of Variance
Compared with Pearson Chi-Square test
PT= patellar tendon, HS= hamstring, AL= allograft, RTS= Return-to-Sport, CTRL= control group, IKDC= International Knee Documentation Committee, QF=Quadriceps Femoris
Indicates a statistically significant (p≤ 0.05) post-hoc comparison between Pass and Fail groups
Indicates a statistically significant (p≤ 0.05) post-hoc comparison between Pass and Control groups
Indicates a statistically significant (p≤ 0.05) post-hoc comparison between Fail and Control groups
Performance on Return-to-Sport Test Items
Of the 148 participants after ACLR, 39 (26.4%) met all RTS test item cutoffs and 109 (73.6%) failed at least one RTS test item cutoff. There were 62 participants (41.9%) who failed to meet the 90% quadriceps strength LSI cutoff and 70 participants (47.3%) failed to score ≥90 on the IKDC. Only 36 (24.3%) did not meet the 90% single hop LSI cutoff, 26 (17.6%) did not meet the triple hop LSI cutoff, 34 (23%) did not meet cross-over hop LSI cutoff, and 28 (18.9%) did not meet timed hop LSI cutoff. Group mean values for each RTS test item are presented in TABLE 1.
Landing Mechanics
Kinematic Variables
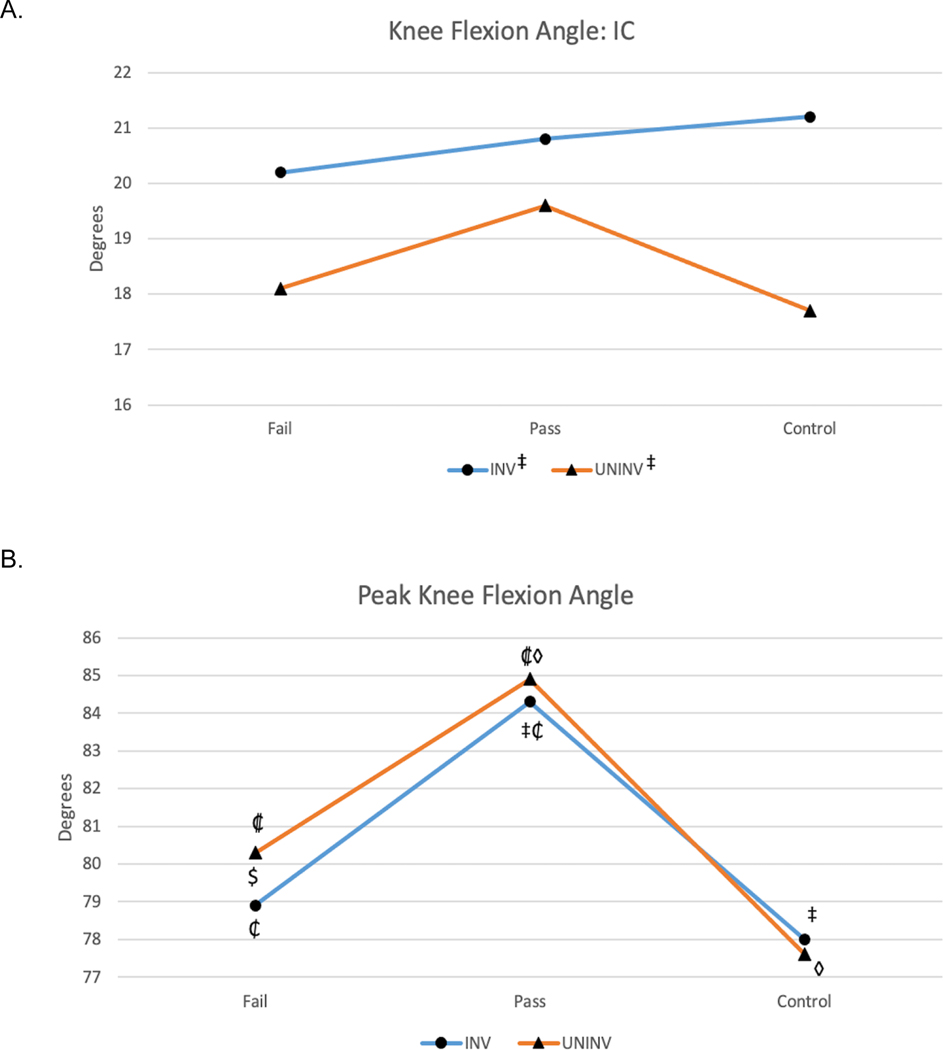
At initial contact, there were no differences in knee flexion angle LSI among the groups (TABLE 2) (p=0.66). Group x limb analysis showed a main effect for limb, with the involved/test limb landing with more knee flexion (FIGURE 1, TABLE 3) (p<0.001). During weight acceptance, peak knee flexion angle LSI was lower in the RTS-FAIL group compared to the CTRL group (TABLE 2) (p<0.001). A statistically significant group x limb interaction was observed for peak knee flexion angle (p=0.038), with both limbs in the RTS-PASS group demonstrating with greater peak knee flexion compared to the RTS-FAIL and CTRL groups (FIGURE 1, TABLE 3) (p<0.05). The RTS-FAIL group demonstrated reduced involved limb peak knee flexion angle compared to the uninvolved limb (FIGURE 1, TABLE 3) (p<0.001).
TABLE 2.
Limb Symmetry Values for Landing Variables among Groups
| RTS-PASS | RTS-FAIL | CTRL | P-value | Post-hoc comparisons | |
|---|---|---|---|---|---|
| Peak vGRF LSI (%) | 91.0 ± 16.7 | *83.2 ± 19.8 | *96.6 ± 19.2 | <0.001 | *p<0.0001 |
| IC KFA LSI (%) | 114.5 ± 41.1 | 107.9 ± 13.8 | 123.4 ± 36.9 | 0.66 | - |
| Peak KFA LSI (%) | 99.5 ± 5.6 | *98.4 ± 5.4 | *100.7 ± 5.0 | 0.03 | *p<0.001 |
| Peak KEM LSI (%) | †89.5 ± 19.6 | *†77.1 ± 23.8 | *96.5 ± 13.9 | <0.001 |
*p<0.001
†p=0.004 |
Data are reported as mean ± standard deviation
RTS-PASS=ACLR cohort that passed return to sport criteria, RTS-FAIL=ACLR cohort that failed return to sport criteria, CTRL=uninjured control group, LSI=limb symmetry index, vGRF=vertical ground reaction force, IC=initial contact, KFA=knee flexion angle, KEM=internal knee extension moment
Figure 1. Group x Limb Comparisons for Kinematic Variables during Landing.
INV=Involved Limb, UNINV=Uninvolved Limb, Fail=ACLR cohort that failed RTS criteria, Pass=ACLR cohort that passed RTS criteria
Panel A:
‡, main effect for limb: INV>UNINV, p<0.001
Panel B:
‡, INV: CTRL<Pass, p=.001
₡, INV: Fail<Pass, p=.002
◊, UNINV: CTRL<Pass, p<0.001
₵, UNINV: Fail<Pass, p=0.021
$, Fail: INV<UNINV, p<0.001
Table 3.
Raw Involved and Uninvolved Limb Values per Landing Variable with comparisons Between RTS-PASS, RTS-FAIL and Controls
| Variable | Involved Limb | Uninvolved Limb | P-value | |
|---|---|---|---|---|
| KFA (IC, deg) | RTS-PASS | 20.76 (18.74–22.78) | 19.64 (17.29–22.00) | ap<0.001 |
| RTS-FAIL | 20.16 (18.97–21.36) | 18.11(16.93–19.30) | ||
| CTRL | 21.22 (19.13–23.31) | 17.74 (16.16–19.32) | ||
| peak KFA (WA, deg) | RTS-PASS | 84.30 (81.78–86.81) | 84.90 (82.23–87.57) | bp=0.038 |
| RTS-FAIL | 78.91 (77.24–80.58) | 80.34 (78.55–82.13) | ||
| CTRL | 77.98 (75.98–79.99) | 77.62 (75.38–79.87) | ||
| peak vGRF (N/kg) | RTS-PASS | 1.46 (1.40–1.52) | 1.63 (1.56–1.70) | bp<0.001 |
| RTS-FAIL | 1.45 (1.40–1.50) | 1.80 (1.74–1.86) | ||
| CTRL | 1.70 (1.61–1.78) | 1.80 (1.70–1.87) | ||
| KEM (IC, Nm/kg) | RTS-PASS | 0.07 (0.01–0.13) | 0.05 (0.0–0.09) | ap=0.043 |
| RTS-FAIL | 0.10 (0.06–0.13) | 0.05 (0.01–0.08) | ||
| CTRL | 0.02 (−0.02–0.06) | 0.02 (−0.02–0.06) | ||
| peak KEM (WA, Nm/kg) | RTS-PASS | 1.60 (1.49–1.72) | 1.82 (1.71–1.92) | bp<0.001 |
| RTS-FAIL | 1.56 (1.43–1.69) | 2.05 (1.96–2.15) | ||
| CTRL | 2.01 (1.89–2.14) | 2.10 (1.98–2.22) | ||
All data reported as mean (95% Confidence Interval)
RTS-PASS=ACLR cohort that passed return to sport criteria, RTS-FAIL=ACLR cohort that failed return to sport criteria, CTRL=uninjured control group, IC= Initial Contact, WA= Weight Acceptance, KFA= Knee Flexion Angle, vGRF= Vertical Ground Reaction Force, KEM= Internal Knee Extension Moment,
Indicates a statistically significant main effect for limb
Indicates a statistically significant group x limb interaction, see Figure 1 for additional comparisons
Kinetic Variables
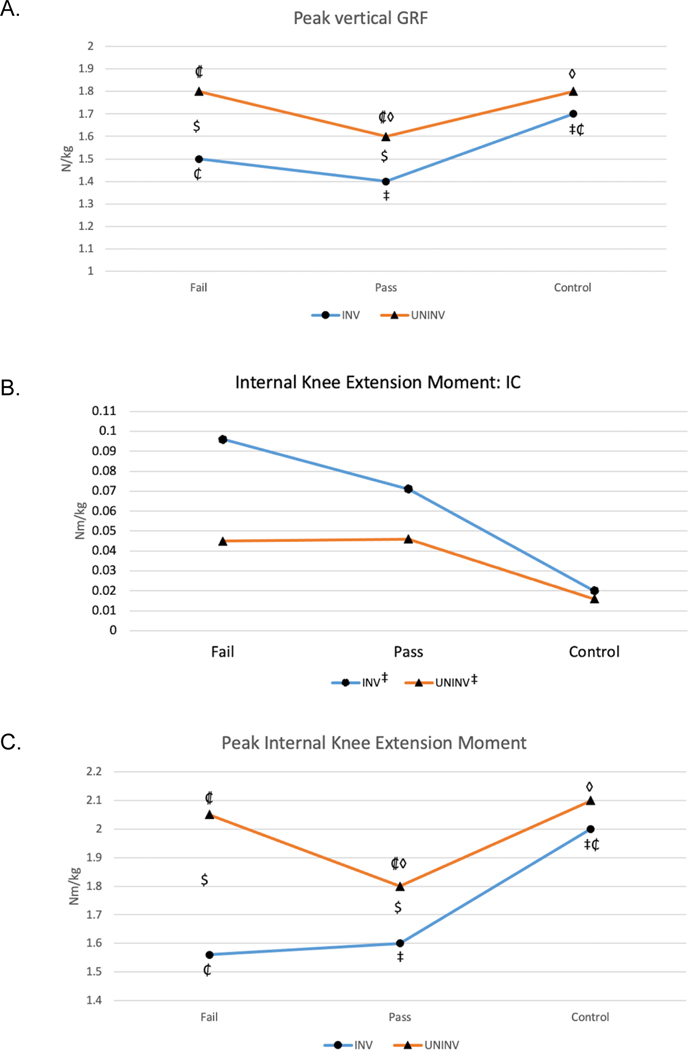
The RTS-FAIL group had lower LSI values for peak vertical ground reaction force and peak internal knee extension moment compared to the RTS-PASS and CTRL groups (TABLE 2) (p<0.05). Group x limb comparisons showed a main effect for limb at initial contact, with the internal knee extension moment being higher in the involved/test limb compared to the uninvolved/non-test limb (FIGURE 2, TABLE 3) (p=0.043). Statistically significant group x limb interactions were observed for peak vertical ground reaction force (p<0.001) and peak internal knee extension moment (p<0.001) (FIGURE 2, TABLE 3). On the involved limb, the RTS-FAIL and RTS-PASS groups demonstrated reduced peak vertical ground reaction force and peak internal knee extension moment compared to the CTRL group (FIGURE 2, TABLE 3) (p<0.05). On the uninvolved limb, the RTS-PASS group demonstrated reduced peak vertical ground reaction force and peak internal knee extension moments compared to both the RTS-FAIL and CTRL groups (FIGURE 2, TABLE 3) (p<0.05). Within group comparisons showed lower peak vertical ground reaction force and peak internal knee extension moment on the involved limb compared to the uninvolved limb for both the RTS-PASS and RTS-FAIL groups (FIGURE 2, TABLE 3) (p<0.0167).
Figure 2. Group x Limb Comparisons for Kinetic Variables during Landing.
Limb, UNINV=Uninvolved Limb, Fail=ACLR cohort that failed RTS criteria, Pass=ACLR cohort that passed RTS criteria, GRF= Ground Reaction Force, IC=initial contact
Panel A:
‡, INV: CTRL>Pass, p<0.001
₡, INV: CTRL>Fail, p<0.001
◊, UNINV: Pass<CTRL, p=0.044
₵, UNINV: Pass<Fail, p=0.010
$, Fail: INV<UNINV, p<0.001
Panel B:
‡, main effect for limb: INV>UNINV, p=0.043
Panel C:
‡, INV: CTRL>Pass, p=0.002
₡, INV: CTRL>Fail, p<0.001
◊, UNINV: Pass<CTRL, p=0.008
₵, UNINV: Pass<Fail, p=0.015
$, Fail: INV<UNINV, p<0.001
DISCUSSION
The purpose of this study was to assess if performance (pass or fail) on RTS criteria coincides with restoration of lower limb (both involved and uninvolved limb) movement mechanics during a bilateral landing task, with respect to uninjured individuals. Our findings indicate that young athletes following ACLR, regardless of RTS test performance, do not appear to have normalized sagittal plane landing biomechanics compared to uninjured controls at the time of medical RTS clearance. While the RTS-PASS group appears to achieve symmetrical knee loading (with values at or above 90% LSI) during the double limb landing task, symmetry during weight acceptance was achieved by reducing values on the uninvolved limb, rather than achieving normalized values on both limbs.
Landing on a stiffer knee (i.e. less knee flexion excursion) on the involved limb has been associated with worse knee related function.5,9 In our sample, the involved limb landed with more knee flexion compared to the uninvolved limb at initial contact across all groups. While statistically significant, the differences between limbs are likely too small to be noticed clinically (approximately 2–3o).33,34 However, the peak knee flexion motion achieved during weight acceptance was different among the groups. The RTS-PASS group demonstrated greater peak knee flexion compared to both RTS-FAIL and CTRLs on both limbs. This finding may be related to individual rehabilitation programs (more emphasis working on landing mechanics)35 or differences in function between RTS-PASS and RTS-FAIL groups.2,11 Despite all three group achieving symmetry (LSI≥90%) with respect to peak knee flexion angle, the peak knee flexion angle of the involved limb was lower than the uninvolved limb for the RTS-FAIL group. Reductions in involved limb knee flexion angle during landing at 6 months post-ACLR (between limb differences of 3.2º) have been associated with markers of tibiofemoral cartilage degeneration 3 years later.9 However, the between-limb difference in the RTS-FAIL group was less than 2º (on average), suggesting that these differences are likely too small to be observed clinically and are potentially not clinically meaningful. A single-leg landing task may be more sensitive to detecting sagittal plane kinematic differences among groups and between limbs.5
In terms of lower limb loading, symmetry (LSI) values between the RTS-PASS group and CTRL group were not statistically different for the peak vertical ground reaction force or peak internal knee extension moment achieved during landing. While the RTS-PASS group appeared to achieve joint loading symmetry, this did not indicate ‘normalized’ knee joint loading compared to the uninjured reference group. The RTS-PASS group demonstrated reduced peak vertical ground reaction force and peak internal knee extension moment on both the involved and uninvolved limbs. These data indicate that the RTS-PASS group achieved symmetry by unloading the uninvolved limb. However, between-limb asymmetry was noted in the RTS-FAIL group for both vertical ground reaction force and peak internal knee extension moment, which was driven by lower involved limb loading. It is important to note, that the involved limbs of both the RTS-PASS and RTS-FAIL groups were significantly lower compared to the CTRL group for both of these limb loading variables, which is in line with previous work.1,24 For both groups, these reductions indicate a reduced ability to load the knee, despite completing rehabilitation and being cleared for sports participation. An underloading pattern on the involved limb has been associated with subsequent indicators of joint degeneration in individuals after ACLR.9,12
This study adds to the growing evidence demonstrating the limitations of limb symmetry as an outcome measure for both RTS test items and biomechanical variables.18,36–39 With LSI values, the context of ‘sufficient’ is lost and any between group comparisons (i.e. RTS-FAIL vs. RTS-PASS) can be influenced by changes in either limb.36,38 Changes (generally worsening) in both biomechanics and strength are well-known to occur in the contralateral limb following ACLR,38,40 and limb symmetry values are unable to account for these changes.18,39 While our limb symmetry findings could be interpreted that landing is considered ‘normalized’ in the RTS-PASS group (i.e. no LSI differences with CTRLs), the comparisons of each limb’s mean value indicates that both ACLR groups (regardless of RTS testing performance) demonstrate limb and knee loading deficits during landing, compared to uninjured controls. This may seem counterintuitive, as the RTS-PASS group is assumed to have higher lower limb function as they met RTS criteria. These data indicate that additional considerations may be warranted in evaluating symmetry data, as it is also plausible the RTS-PASS group met RTS criteria because the uninvolved limb was detrained.38–40 Further work to establish the most optimal comparison metric(s) for both biomechanical variables and RTS test items remains a critical need.
Overall, our findings are in line with Di Stasi and colleagues,6 who compared the gait characteristics 6-months post-ACLR of individuals (mean age 29.3 years) who passed and failed RTS criteria.6 At 6-months post-ACLR, both of their defined pass and fail groups demonstrated reduced involved limb peak knee angles and knee moments compared to the uninvolved side, with a greater magnitude of asymmetry in the fail group.6 While the RTS criteria for classifying individuals were similar between Di Stasi and colleagues and the present study (both used quadriceps strength LSI, single-leg hop test LSI, and patient-reported outcome measures), key methodological differences (no control group) limit direct comparisons between gait mechanics and landing mechanics by RTS group after ACLR.6
Much of the previous research has examined the association of asymmetries (i.e. LSI) in limb loading and knee loading during landing tasks with asymmetries in quadriceps strength.2–5,41 However the present study is novel in that quadriceps strength was only one of the RTS test items used to categorize ACLR participants. We found 57% of RTS-FAIL group did not meet the quadriceps strength cutoff (≥90% LSI). While this is in line with previous work reporting that 44%−60% do not meet quadriceps strength symmetry criteria,20,41 it also indicates that 43% of the RTS-FAIL group had ≥90% quadriceps strength LSI and the reason they failed was due to a different factor. Thus any differences observed in the present study could be driven by any of the RTS test items or unmeasured factors, such as psychological recovery/fear of re-injury that were not evaluated in this analysis.42–44 While it was beyond the scope of this study, further investigation into which RTS test item (or interaction between RTS test items) impacts the identified biomechanical differences during double-limb landing may help inform future RTS decisions.
LIMITATIONS
The present study is not without limitations. Firstly, this study had low numbers in the RTS-PASS group. However, this frequency of athletes in the RTS-PASS group is consistent with previous findings in other studies.20,21 Secondly, we did not control for graft type, meniscus status (repair vs. meniscectomy), or the duration of rehabilitation in our analyses. We found that there were more BPTB autografts in the RTS-FAIL group, which is in line with previous research indicating those with BPTB ACLR may require more time (>12 months) to meet common RTS strength and function milestones.45 Our cohort was predominately female (69%). While this sex distribution is reflective of the incidence and risk of ACL injuries in females compared to males,46 the external validity of these results to a predominately male population may be limited. We used the most commonly-reported RTS test items (quadriceps strength, hop tests, self-reported knee function) and passing standards (≥90% LSI on each) to determine the RTS-PASS vs. RTS-FAIL groups.18 However, previous work has called for further research into the ability of these test items and the ≥90% LSI cutoff scores to evaluate risk of poor outcomes following ACLR, including reducing the risk of a second ACL injury.18 Lastly, we did not perform analyses to determine if any specific RTS test item (or the raw values themselves) were associated with kinematic and kinetic variables during the landing tasks. This study did not evaluate biomechanical variables, beyond sagittal plane knee-related variables and the ground reaction force, that may inform landing mechanics in this population. Future work in these areas is warranted.
CONCLUSIONS
Passing the RTS criteria used in this study did not indicate normalized double-limb landing mechanics in young athletes following ACLR at the time of RTS. Young athletes who passed RTS criteria demonstrated symmetrical lower limb loading; however, this symmetry was achieved by reducing load on both the involved and uninvolved limbs. Reduced involved limb loading, characterized by lower vertical ground reaction force and knee extension moments, were demonstrated by young athletes who both passed and failed RTS criteria, compared to the uninvolved limb and compared to young uninjured individuals.
ACKNOWLEDGEMENTS
Funding Source(s): This work was funded, in part, by support from the National Institutes of Health grant F32-AR055844 and the National Football League Charities Medical Research Grants 2007, 2008, 2009, 2011.
Institutional Review Board: This study was approved by the Cincinnati Children’s Hospital Intuitional Review Board (approval #: 2008-0514)
Public Trials Registry: N/A
Financial Disclosures: There are no disclosures.
References
- 1.Lepley AS, Kuenze CM. 2018. Hip and knee kinematics and kinetics during landing tasks after anterior cruciate ligament reconstruction: A systematic review and meta-analysis. J. Athl. Train 53(2):144–159 Available from: http://natajournals.org/doi/10.4085/1062-6050-334-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schmitt LC, Paterno MV, Ford MV, et al. 2016. Strength Asymmetry and Landing Mechanics at Return to Sport after ACL Reconstruction. Med. Sci. Sport. Exerc 47(7):1426–1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ithurburn MP, Altenburger AR, Thomas S, et al. 2018. Young athletes after ACL reconstruction with quadriceps strength asymmetry at the time of return-to-sport demonstrate decreased knee function 1 year later. Knee Surgery, Sport. Traumatol. Arthrosc 26(2):426–433. [DOI] [PubMed] [Google Scholar]
- 4.Ithurburn MP, Paterno MV, Ford KR, et al. 2015. Young athletes with quadriceps femoris strength asymmetry at return to sport after anterior cruciate ligament reconstruction demonstrate asymmetric single-leg drop-landing mechanics. Am. J. Sports Med 43(11):2727–2737. [DOI] [PubMed] [Google Scholar]
- 5.Ithurburn MP, Paterno MV, Ford KR, et al. 2017. Young Athletes after Anterior Cruciate Ligament Reconstruction with Single-Leg Landing Asymmetries at the Time of Return to Sport Demonstrate Decreased Knee Function 2 Years Later. Am. J. Sports Med 45(11):2604–2613. [DOI] [PubMed] [Google Scholar]
- 6.Di Stasi SL, Logerstedt D, Gardinier ES, Snyder-Mackler L. 2013. Gait patterns differ between ACL-reconstructed athletes who pass return-to-sport criteria and those who fail. Am. J. Sports Med 41(6):1310–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pairot-de-Fontenay B, Willy RW, Elias ARC, et al. 2019. Running Biomechanics in Individuals with Anterior Cruciate Ligament Reconstruction: A Systematic Review. Sport. Med 49(9):1411–1424 Available from: 10.1007/s40279-019-01120-x. [DOI] [PubMed] [Google Scholar]
- 8.Paterno M V, Schmitt LC, Ford KR, et al. 2010. Biomechanical measures during landing and postural stability predict second anterior cruciate ligament injury after anterior cruciate ligament reconstruction and return to sport. Am. J. Sports Med 38(10):1968–1978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shimizu T, Samaan MA, Tanaka MS, et al. 2019. Abnormal Biomechanics at 6 Months Are Associated With Cartilage Degeneration at 3 Years After Anterior Cruciate Ligament Reconstruction. Arthrosc. - J. Arthrosc. Relat. Surg 35(2):511–520 Available from: 10.1016/j.arthro.2018.07.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kotsifaki A, Korakakis V, Whiteley R, et al. 2019. Measuring only hop distance during single leg hop testing is insufficient to detect deficits in knee function after ACL reconstruction: A systematic review and meta-analysis. Br. J. Sports Med :1–16. [DOI] [PubMed]
- 11.Schmitt LC, Paterno MV, Hewett TE. 2012. The Impact of Quadriceps Femoris Strength Asymmetry on Functional Performance at Return to Sport Following Anterior Cruciate Ligament Reconstruction. J. Orthop. Sport. Phys. Ther 42(9):750–759 Available from: http://www.jospt.org/doi/10.2519/jospt.2012.4194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wellsandt E, Gardinier ES, Manal K, et al. 2016. Decreased Knee Joint Loading Associated with Early Knee Osteoarthritis after Anterior Cruciate Ligament Injury. Am. J. Sports Med 44(1):143–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hewett TE, Myer GD, Ford KR, et al. 2005. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: A prospective study. Am. J. Sports Med 33(4):492–501. [DOI] [PubMed] [Google Scholar]
- 14.Ithurburn MP, Longfellow MA, Thomas S, et al. 2019. Knee Function, Strength, and Resumption of Preinjury Sports Participation in Young Athletes Following Anterior Cruciate Ligament Reconstruction. J. Orthop. Sport. Phys. Ther 49(3):145–153. [DOI] [PubMed] [Google Scholar]
- 15.Thomeé R, Neeter C, Gustavsson A, et al. 2012. Variability in leg muscle power and hop performance after anterior cruciate ligament reconstruction. Knee Surgery, Sport. Traumatol. Arthrosc 20(6):1143–1151. [DOI] [PubMed] [Google Scholar]
- 16.Ithurburn MP, Zbojniewicz AM, Thomas S, et al. 2018. Lower patient-reported function at 2 years is associated with elevated knee cartilage T1rho and T2 relaxation times at 5 years in young athletes after ACL reconstruction. Knee Surgery, Sport. Traumatol. Arthrosc 0(0):0 Available from: 10.1007/s00167-018-5291-x. [DOI] [PubMed]
- 17.Burgi CR, Peters S, Ardern CL, et al. 2019. Which criteria are used to clear patients to return to sport after primary ACL reconstruction? A scoping review. Br. J. Sports Med :1–10. [DOI] [PubMed]
- 18.Losciale JM, Zdeb RM, Ledbetter L, et al. 2019. The association between passing return-to-sport criteria and second anterior cruciate ligament injury risk: A Systematic Review With Meta-analysis. J. Orthop. Sports Phys. Ther 49(2). [DOI] [PubMed] [Google Scholar]
- 19.Van Melick N, Van Cingel REH, Brooijmans F, et al. 2016. Evidence-based clinical practice update: Practice guidelines for anterior cruciate ligament rehabilitation based on a systematic review and multidisciplinary consensus. Br. J. Sports Med 50(24):1506–1515. [DOI] [PubMed] [Google Scholar]
- 20.Toole AR, Ithurburn MP, Rauh MJ, et al. 2017. Young Athletes After Anterior Cruciate Ligament Reconstruction Cleared for Sports Participation: How Many Actually Meet Recommended Return-to-Sport Criteria Cutoffs? J. Orthop. Sport. Phys. Ther 47(11):1–27 Available from: http://www.jospt.org/doi/10.2519/jospt.2017.7227. [DOI] [PubMed] [Google Scholar]
- 21.Welling W, Benjaminse A, Seil R, et al. 2018. Low rates of patients meeting return to sport criteria 9 months after anterior cruciate ligament reconstruction: a prospective longitudinal study. Knee Surgery, Sport. Traumatol. Arthrosc 26(12):3636–3644 Available from: 10.1007/s00167-018-4916-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Losciale JM, Bullock G, Cromwell C, et al. 2019. Hop Testing Lacks Strong Association With Key Outcome Variables After Primary Anterior Cruciate Ligament Reconstruction: A Systematic Review. Am. J. Sports Med :036354651983879 Available from: http://journals.sagepub.com/doi/10.1177/0363546519838794. [DOI] [PubMed]
- 23.Graziano J, Chiaia T, De Mille P, et al. 2017. Return to sport for skeletally immature athletes after ACL reconstruction: Preventing a second injury using a quality of movement assessment and quantitative measures to address modifiable risk factors. Orthop. J. Sport. Med 5(4):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnston PT, McClelland JA, Webster KE. 2018. Lower Limb Biomechanics During Single-Leg Landings Following Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-Analysis. Sport. Med 48(9):2103–2126 Available from: 10.1007/s40279-018-0942-0. [DOI] [PubMed] [Google Scholar]
- 25.Ford KR, Schmitt LC, Hewett TE, Paterno MV. 2016. Identification of preferred landing leg in athletes previously injured and uninjured: A brief report. Clin. Biomech 31:113–116 Available from: 10.1016/j.clinbiomech.2015.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reid A, Birmingham TB, Stratford PW, et al. 2007. Hop Testing Provides a Reliable and Valid Outcome Measure During Rehabilitation After Anterior Cruciate Ligament Reconstruction. Phys. Ther 87(3):337–349 Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=01244666-200709000-00011. [DOI] [PubMed] [Google Scholar]
- 27.Irrgang JJ, Anderson AF, Boland AL, et al. 2006. Responsiveness of the International Knee Documentation Committee Subjective Knee Form. Am. J. Sports Med 34(10):1567–1573. [DOI] [PubMed] [Google Scholar]
- 28.Grevnerts HT, Terwee CB, Kvist J. 2015. The measurement properties of the IKDC-subjective knee form. Knee Surgery, Sport. Traumatol. Arthrosc 23(12):3698–3706. [DOI] [PubMed] [Google Scholar]
- 29.Taylor MK, Pietrobon R, Ghodra N, et al. 2005. Validation Of The International Knee Documentation Committee Subjective Knee Form. Med. Sci. Sport. Exerc 37(Supplement):S145 Available from: https://insights.ovid.com/crossref?an=00005768-200505001-00787. [Google Scholar]
- 30.Higgins LD, Taylor MK, Park D, et al. 2007. Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Jt. Bone Spine 74(6):594–599. [DOI] [PubMed] [Google Scholar]
- 31.Kyritsis P, Bahr R, Landreau P, et al. 2016. Likelihood of ACL graft rupture: Not meeting six clinical discharge criteria before return to sport is associated with a four times greater risk of rupture. Br. J. Sports Med 50(15):946–951. [DOI] [PubMed] [Google Scholar]
- 32.Ithurburn MP, Paterno MV, Thomas S, et al. 2019. Change in Drop-Landing Mechanics Over 2 Years in Young Athletes After Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med 47(11):2608–2616 Available from: http://journals.sagepub.com/doi/10.1177/0363546519864688. [DOI] [PubMed] [Google Scholar]
- 33.Maykut JN, Taylor-Haas JA, Paterno MV, et al. 2015. Concurrent validity and reliability of 2d kinematic analysis of frontal plane motion during running. Int. J. Sports Phys. Ther 10(2):136–46 Available from: http://www.ncbi.nlm.nih.gov/pubmed/25883862%0Ahttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4387721. [PMC free article] [PubMed] [Google Scholar]
- 34.Padua Michelle C Boling DA, DiStefano James A Onate Anthony I Beutler LJ. 2011. Reliability of the Landing Error Scoring System- Real Time, a Clinical Assessment Tool of Jump- Landing Biomechanics Recommended Citation "Reliability of the Landing Error Scoring System-Real Time, a Clinical Assessment Tool of Jump-Landing Biomechan. Available from: http://digitalcommons.unf.edu/hmov_facpub%0Ahttp://digitalcommons.unf.edu/hmov_facpub/2. [DOI] [PubMed]
- 35.Nagelli C V, Wordeman SC, Di Stasi S, et al. 2021. Neuromuscular Training Improves Biomechanical Deficits at the Knee in Anterior Cruciate Ligament-Reconstructed Athletes. Clin. J. Sport Med 31(2):113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wren TAL, Mueske NM, Brophy CH, et al. 2018. Hop Distance Symmetry Does Not Indicate Normal Landing Biomechanics in Adolescent Athletes With Recent Anterior Cruciate Ligament Reconstruction. J. Orthop. Sport. Phys. Ther 48(8):622–629 Available from: https://www.jospt.org/doi/10.2519/jospt.2018.7817. [DOI] [PubMed] [Google Scholar]
- 37.Losciale JM, Bullock G, Cromwell C, et al. 2020. Hop Testing Lacks Strong Association With Key Outcome Variables After Primary Anterior Cruciate Ligament Reconstruction: A Systematic Review. Am. J. Sports Med 48(2):511–522. [DOI] [PubMed] [Google Scholar]
- 38.Goerger BM, Marshall SW, Beutler AI, et al. 2015. Anterior cruciate ligament injury alters preinjury lower extremity biomechanics in the injured and uninjured leg: The JUMP-ACL study. Br. J. Sports Med 49(3):188–195. [DOI] [PubMed] [Google Scholar]
- 39.Wellsandt E, Failla MJ, Snyder-Mackler L. 2017. Limb Symmetry Indexes Can Overestimate Knee Function After Anterior Cruciate Ligament Injury. J. Orthop. Sport. Phys. Ther 47(5):334–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chung KS, Ha JK, Yeom CH, et al. 2015. Are muscle strength and function of the uninjured lower limb weakened after anterior cruciate ligament injury? Am. J. Sports Med 43(12):3013–3021. [DOI] [PubMed] [Google Scholar]
- 41.Palmieri-Smith RM, Lepley LK. 2015. Quadriceps strength asymmetry after anterior cruciate ligament reconstruction alters knee joint biomechanics and functional performance at time of return to activity. Am. J. Sports Med 43(7):1662–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McPherson AL, Feller JA, Hewett TE, Webster KE. 2019. Psychological Readiness to Return to Sport Is Associated With Second Anterior Cruciate Ligament Injuries. Am. J. Sports Med 47(4):857–862. [DOI] [PubMed] [Google Scholar]
- 43.Trigsted SM, Cook DB, Pickett KA, et al. 2018. Greater fear of reinjury is related to stiffened jump-landing biomechanics and muscle activation in women after ACL reconstruction. Knee Surgery, Sport. Traumatol. Arthrosc 26(12):3682–3689. [DOI] [PubMed] [Google Scholar]
- 44.Paterno M V, Flynn K, Thomas S, Schmitt LC. 2018. Self-Reported Fear Predicts Functional Performance and Second ACL Injury After ACL Reconstruction and Return to Sport: A Pilot Study. Sports Health 10(3):228–233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Smith AH, Capin JJ, Zarzycki R, Snyder-Mackler L. 2020. Athletes with bone-patellar tendon-bone autograft for anterior cruciate ligament reconstruction were slower to meet rehabilitation milestones and return-to-sport criteria than athletes with hamstring tendon autograft or soft tissue allograft : Secondary a. J. Orthop. Sports Phys. Ther 50(5):259–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Montalvo AM, Schneider DK, Webster KE, et al. 2019. Anterior Cruciate Ligament Injury Risk in Sport: A Systematic Review and Meta-Analysis of Injury Incidence by Sex and Sport Classification. J. Athl. Train 54(5):1062-6050-407-16 Available from: http://natajournals.org/doi/10.4085/1062-6050-407-16. [DOI] [PMC free article] [PubMed] [Google Scholar]