Abstract
Background:
There is no comprehensive study addressing all the epidemiological aspects of Lung cancer (LC) in Iran, therefore this systematic review investigated the epidemiological aspects of lung cancer in Iran.
Methods:
The search was performed until the Aug. 2020 on the in international databases based on PRISMA protocol by Pulmonary Neoplasms, Lung Neoplasm, Neoplasm, Lung, Lung Cancer, Cancer, Pulmonary Cancer, Cancer, Pulmonary, Cancers, Cancer of the Lung, Iran, incidence, death, risk factors keywords and different combinations of them. Articles that evaluated epidemiological aspects of lung cancer were included in the analysis.
Results:
Of 1420 articles, 82 cases were entered the analysis. Based on studies, in Iran, lung cancer has been the most common cancer and its prevalence is increasing. Squamous cell carcinoma and adenocarcinoma is the most common type of lung cancer in men and women, respectively. Cigarette smoking, human papilloma virus (HPV) infection, mustard gas, occupational risk factors and genetic factors considered as the major reported risk factors for lung cancer and vegetarian diet as a protective factor.
Conclusion:
In according to the increasing trend of incidence and mortality of lung cancer in Iran, elimination of the major risk factors can decrease this issue and national comprehensive planning should be considered in health promotion plans.
Keywords: Lung cancer, Epidemiology, Risk factor, Survival, Iran
Introduction
Lung cancer (LC) is second most common cancer in both genders and most common and dead-liest cancer worldwide, with a 5-year survival rate of 19% and estimated that 13% of cancer incidence and 24% of cancer mortality causes related to lung cancer (1).
LC incidence strongly dependent on the geographic region, therefore, in developed countries is higher than the undeveloped and is raising in Asian countries (2). LC morbidity and mortality is more prevalent among men (1).
In Iran, LC is one of the most common cancers with increasing trend, great economic burden and various pattern in different geographical areas (3). Several risk factors associated with LC may had synergistic effects; smoking, diet, occupational and environmental risk factors, family history and gender, but smoking is the most important risk factor (4).
Therefore, investigating the causes of increased incidence and mortality of LC and associated risk factors is essential for comprehensive health planning for reducing the burden of disease. Since there is no comprehensive study addressing all the epidemiological aspects of this cancer in Iran, therefore, the present study aimed to investigate the epidemiological aspects of LC in Iran.
Methods
This systematic review was based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol (5).
Search strategy
The search was performed until the Aug. 2020 on the in international databases (PubMed, web of science, Scopus, Google Scholar, Science Direct, Springer and ProQuest) and national databases (SID: Scientific Information Database, Magiran, Irandoc, IranMedex and MedLib) without time limitation. Search was performed by Pulmonary Neoplasms, Lung Neoplasm, Neoplasm, Lung, Lung Cancer, Cancer, Pulmonary Cancer, Cancer, Pulmonary, Cancers, Cancer of the Lung, Iran, incidence, death, risk factors keywords and different combinations of them with AND, OR operators.
Inclusion and exclusion criteria
Articles, which revealed different epidemiological aspects including, incidence, mortality, prevalence and risk factors of LC in Iran were included. Studies that did not have access to the full text, editorial letters, case reports and review articles were excluded.
Articles selection
After an initial search and examination of the articles title and abstract, articles full text that were in line with the study, entered in the reading phase and finally the studies matched with the aims of the study were analyzed.
Data Extraction
A table including related variables, sample size, risk factors and severity of relationship was designed (Table 1).
Table 1:
Risk factors associated with lung cancer in Iran
| Author | publication Year | Location | Sample size | Related factor | Risk index | |
|---|---|---|---|---|---|---|
| Nadji SA. (58) | 2007 | Mazandaran | Case:141 control: 92 |
active smoking, HPV infection | NA | |
| Hosseini-Khalili A. (53) | 2009 | Tehran | 20 male | mustard gas | NA | |
| Hosseini M. (45) | 2009 | Tehran | Case:242 Control: 242 |
Smoking | OR(CI): 5.4(3.2–8.9) | |
| Occupational exposures to inorganic dusts | OR(CI): 4.2(2.8–6.7) | |||||
| chemical compounds | OR(CI): 3.4 (2.1–5.6) | |||||
| heavy metals | OR(CI): 3.0(1.3–7.0) | |||||
| Razmkhah m. (59) | 2005 | Shiraz | Case: 72 Control: 262 |
AG genotypes of SDF-1 | p-value =0.008 | |
| Mosavi-Jarr Ahi A (60) | 2009 | Iran | 12,488,020 men, 677,469 women | occupational exposure | RR(CI):1.9 (1.7–2.1) for high exposure 1.3 (1.2–1.4)for low exposure | |
| Karimzadeh L. (61 | 2011 | Tehran | Case: 40 Control: 40 |
consumption of baked bread in traditional oven | OR(CI): 22.6(1.9–270) | |
| Mahaki B. (62) | 2011 | Iran | - | Smoking | Posterior Median : 1.067 | |
| Karimzadeh L. (56) | 2012 | Tehran | Case: 50 Control: 50 |
nitrate and nitrite | OR(CI): 2.7( 0.13–0.96) | |
| Masjedi MR. (49) | 2013 | Tehran | case: 242 Control: 484 | Smoking | OR(CI): 6.2 (3.3–11.6) | |
| Male/Female | OR(CI): 3.1 (1.2–8.1) | |||||
| Hosseini M. (47) | 2014 | Tehran | case: 242 Control: 484 | Bread | OR(CI): 1.54 (1.02–2.32) | |
| Rice | OR(CI): 1.84(1.17–2.89) | |||||
| beef (Upper third month) | OR(CI): 2.67 (1.39–5.10) | |||||
| Butter | Middle third month | OR(CI): 1.70(1.07–2.71) | ||||
| Upper third month | OR(CI): 2.94 (1.79–4.82) | |||||
| White cheese | Middle third month | OR(CI): 3.87 (2.52–2.93) | ||||
| Upper third month | OR(CI): 6.52 (3.49–12.18) | |||||
| Yogurt | Middle third month | OR(CI): 2.37 (1.46–3.83) | ||||
| Upper third month | OR(CI): 2.98 (1.77–5.00) | |||||
| vegetable ghee | OR(CI): 2.27 (1.17–4.40) | |||||
| animal ghee | OR(CI): 7.71 (3.17–18.74) | |||||
| Najafi F. (48) | 2016 | Iran | 413591 | -daily cigarette smoking -low consumption of vegetables |
NA | |
| Safari A. (63) | 2016 | Tehran | 490 | Opium consumption | NA | |
| Dehghani M. (64) | 2018 | Yasuj | Case:34 Control: 61 |
C allele rs2645429 in Farnesyl-Diphosphate Farnesyltransferase 1 |
OR(CI): C allele 2.71(1.12–6.59) CC : 3.02(1.09–8.39) |
|
| Motovali-Bashi M. (65) | 2012 | Isfahan | Case: 65 Control: 80 |
possessed heterozygous (*1/*2A) genotype | OR(CI): 2.79(1.01–7.65). | |
| Zafarghandi MR. (51) | 2013 | Iranian veterans | 7,570exposed and 7,595 unexposed with 25-year follow-up | Sulfur mustard exposure | Incidence rate ratio: 1.81 (95 % CI 1.27–2.56), Age adjusted incidence rate ratio 1.64 (95 % CI 1.15–2.34), HR of cancer: 2.02 (95 % CI 1.41–2.88). | |
| Keeley BR. (66) | 2014 | Golestan | Case: 78 Control: 81 |
G-CSF | OR: 27.7 | |
| GM-CSF | OR: 13.3 | |||||
| Nikseresht M. (67) | 2018 | Yasuj | Case: 34 Control: 50 |
C-allele of the rs2245214 ATG5 gene polymorphism | OR(CI): 3.52(1.33-9.26) | |
| Adibhesami G. (68) | 2018 | Tehran | Case: 120 Control: 120 |
T0M1 / T1M1 genotype was | OR(CI): 3.46(1.61–7.46) | |
| Rahmati A. (69) | 2016 | Golestan | 50,045 adults enrolled from 2004 to 2008, followed annually until June 2015 | Opium use | HRs (1.73 (95% CI: 0.99–3.03) | |
| Eydian Z. (70) | 2016 | Zabol | Case: 200 Control: 200 |
P53 codon 72 polymorphism | Non-significant | |
| Motovali-Bashi M. (71) | 2014 | Isfahan | Case: 288 Control: 352 |
Lys751Gln polymorphism | OR(CI):1.8(I 0.848–3.819) | |
| 751Gln/Gln genotype | OR(CI): 0.7(0.307–1.595). | |||||
| Karimzadeh L. (56) | 2012 | Tehran | Case: 40 Control: 40 |
Animal sources of nitrate and nitrite intake | OR(CI): 2.7(0.13–0.9) | |
| fruit intake | OR(CI): 0.26 (1.3–11) | |||||
| Rikhtegar S. (72) | 2018 | Tehran | Case: 50 Control: 50 |
KRAS | P-value :0.01 | |
| NRAS expression levels | P-value :0.001 | |||||
| Ahmadi M. ( 73 ) | 2018 | Yazd | Case: 96 Control: 100 |
CHRNA3 rs1051730 single nucleotide polymorphism | Non-significant | |
| Chitsaz M. ( 74 ) | 2018 | Tehran | Case: 50 Control: 50 |
Expression of EGFR And FGFR4 Genes | P-value :0.003 | |
| Amini F. (75) | 2017 | Isfahan | Case: 61 Control: 111 |
miR-214-binding site polymorphism in EGFR | Non-significant | |
| Motovali-Bashi M. ( 76 ) | 2012 | Isfahan | Case: 120 Control: 100 |
Distribution of C(−1562)T genotype in type IV collagenase promoter | OR(CI): 19.89 (3.21–120.60) in age group of < 60 yr | |
| Motovali-Bashi M. ( 35 ) | 2012 | Isfahan | Case: 172 Control: 123 |
gelatinase B genotype | OR(CI): 2.56(0.06–23.82) | |
| Motovali-Bashi M. ( 77 ) | 2012 | Isfahan | Case: 112 Control: 120 |
T/C single nucleotide polymorphism in CYP1A1 gene | P-value :0.001 | |
| C allele | P-value : 0.0001 | |||||
| Motovali-Bashi M. ( 78 ) | 2013 | Isfahan | Case: 120 Control: 110 |
−765G/C polymorphism of cyclooxygenase 2 genes | P-value : 0.06 | |
| Rashidi M. (55) | 2014 | Isfahan | - | Arsenic | - | |
| Mobasheri MR. ( 58 ) | 2014 | - | - | particulate matter <2.5 micrometers | R=0.65 | |
| Ghayyoumi M. ( 79 ) | 2015 | Shiraz | Case: 50 Control: 38 |
Serum level of Triose Phosphate Isomerase | P-value: 0.76 | |
| Hamedi F. ( 80 ) | 2017 | Fars | Case: 100 Control: 100 |
Gln/Gln in male. | P-value: 0,044 | |
| Keshvary Ravan H. (81) | 2017 | Shahrekord | Case: 50 Control: 77 |
All c | In: Case 90%, control 82% | |
| Alle t | In: Case 10% control 16.2% | |||||
| Sazgar H. (82) | 2017 | Shahrekord | Case: 100 Control: 100 |
CT genotype | OR(CI): 3.59(2.04–6.69) | |
Results
Description of studies
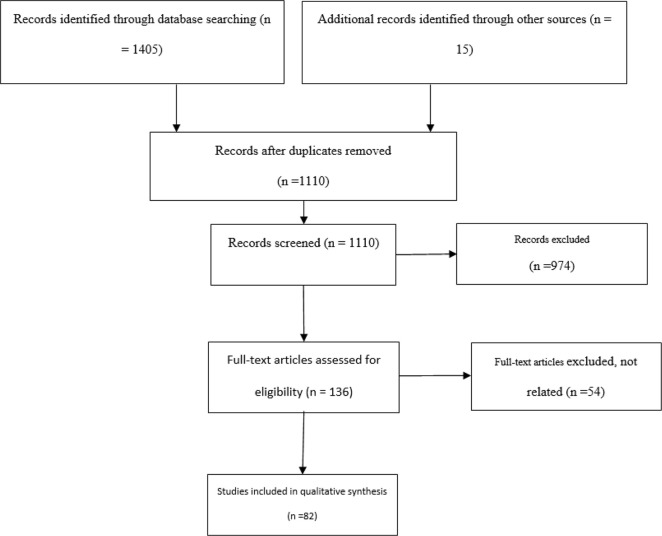
Details are listed in Figure 1.
Fig. 1:
Flow chart of included study
Incidence
LC in Iran was in low rate in 2002, so it was not among the five most common cancers in Iran, although its important mortality rate (6), but the incidence of lung cancer is rising in all parts of Iran (7–9) with an estimation of 5829 cases in 2010 (10).
According to the studies, LC has different rank as a most common cancer in various part of Iran, so that, in 2003, in northwest of Iran was the third most common cancer in men (ASR= 7.9) and the fifth most common cancer in women (ASR= 3.6) (11), the second place among men in Kerman in 2007 (ASR= 7.1) (12), the fourth place in men from 2004 to 2006 in Ardabil province (13), the third place in Golestan Province and in Khuzestan Province (15.4%) (14), the third place in men and the fifth place in women (15), the third place among men in Kerman (ASR= 14.6) (16) and the fifth place in east Azerbaijan (ASR=15.4) (17). In Birjand it reported as one of the ten most common cancers (18). In Tehran, the incidence of LC was 10.4% in men and 5% in women (19) and in another one, as the third most common cancer in men (ASR= 14.9) and women (ASR=7) (20). Lung and bronchus are the third most common cancers in women (2.9 per 100,000) and men (6.3 per 100,000) (21). In addition, it is the fourth most common cancer in both gender (22). In Tehran, LC was one of the ten most common cancers in both gender for elders (23).
Incidence of LC among men in Kerman is 5.85, 4.47, 3.93, 5.35, 7.92, 10.11 in 2004, 2005, 2006, 2007, 2008, 2009 respectively (24). In Kermanshah Province, LC accounts for 17.6% of men’s cancer and 7.3% of women’s (25). In north of Iran, 14% of diagnosed cancers are LC (26).
Prevalence and mortality
The 5-year prevalence of LC in Iran has been reported as 4.21 per 100,000 population, and with a male to female sex ratio of 2.01 (27), in Isfahan, period prevalence of Lung and bronchial cancer were estimated as 9.7% (28).
Based on Global Burden of Disease LC is ranked 28th among the causes of DALYs in Iran (29). Therefore, 120,022 deaths occurred due to LC from 1990 to 2015 in the entire population (36,729 deaths in females and 83 293 in males) (30), with the highest percentage among the 60–79-aged individuals (31).
According to the estimations in 2012, 4,361 deaths from LC and 4,888 new cases were registered in Iran, more incidence and deaths have been reported for men (7). Overall, 9,071 number of deaths from LC occurred in Iran in 2020 and accounted as the second leading cause of cancer death in Iran (32).
Gender and Age
In Iran, the incidence of the LC is higher in men than women (25); approximately 3 times higher and the highest incidence is in the age group of 80–84 (33, 34).
In Shiraz, 74.2% (35); Ardabil more than 80% (36); Sari, 74.2% and western Iran 83% of LC patients were men (37). For the age group over 65, lung and bronchial cancer are the fifth most common cancer in male (69.54) (15). The mean age of patients reported in a study 58.96 yr (38) in Isfahan, 65.8 yr (28), in chaharmahal Bakhtiari, 60.89 yr (39) and in western of Iran, 61.11 yr (37). In Ardabil in 2011 to 2016, mean age of patients was 65.51± 13.8 (40). In Isfahan 94% of LC occurred between the 40 to 90 ages (28).
In Iran the highest incidence was in the sixth decade of life and in men (7) and in Sari was more observed among older patients (25%) (37).
Histology
The squamous cell carcinoma (SCC) and adenocarcinoma (AC) are the most common type of LC in men and women in Iran, respectively (27, 34) and 85.3% of the patients had advanced stages of disease (38). In south of Iran, SCC is the most common type of LC (17). SCC, AC, and small cell carcinoma (SC) were the most common types of LC in Qazvin, respectively (41). In west of Iran, SCC was reported as the most common malignancy (37) from (22.5%) (42) to (61.3%) (36) in different studies and AC (23.5%) (42). In south of Iran, 78.6% of patients were non-small cell and most patients were diagnosed with advanced or metastatic disease (43).
Cost
The estimated cost of LC in Iran in 2014 was reported 3,225,998,555,090 Iranian Rial and its annual cost is estimated as 76,617,943 US $ (3), In other investigation, the average cost of treating LC for one visit was reported 183 US Dollar for patients (44).
Risk factors
Cigarettes
Smoking is reported as the main cause of LC in Iran (36, 45, 46) and Odds Ratio of LC in smokers were reported 5.4 (95% CI: 3.2–8.9) (47) with a significant relationship with LC in smoker women (48). Smoking and opioid use simultaneously, are a serious risk factors for LC progression (49). Smoking increases the cost of LC, and men have higher risk than women (46). In another research, in current and former smokers, hospitalization and hospital costs increased in LC patients by 48 and 35%, respectively, compared to patients who never smoked (50).
Opium use
Opium use, with a relative risk adjusted for other variables in the cohort study in north of Iran for those who had consumed opium, at 1.73 for LC.
The risk elevates with increasing duration of use, so that, the relative risk of opioid consuming less than 10 yr reported a relative risk of 2.42 (51).
HPV infection
HPV infection has been implicated as a risk factor in LC progression (52).
Mustard gas
Findings show that the LC in persons who have exposed to mustard gas started in lower ages (53) and the mean age among them is decreased to 48±12 (6).
Occupational exposure
Recent studies have reported strong associations between LC and occupation and the environment in Iran with a chance of 4.2, (95% CI 2.8–6.7) (45). Reported associated workplace exposure are smoke and steam and number of metals, including arsenic, chromium, and nickel (54). Significantly increased risk of LC was observed in patients who exposed with inorganic dusts, heavy metals 3.0 (95% CI 1.3–7.0) and chemical compounds 3.4 (95% CI 2.1–5.6) (45). Arsenic in fertilizers has been reported as LC risk factor (55).
Nitrites
Positive relationship between animal sources of nitrite and LC has observed (OR = 2.7 95% CI: 0.13–0.96) (56).
Diet
Bread, rice, beef, liver, dairy products, animal and vegetable oils are known as risk factors for lung cancer in Iran (47). Fruit consumption significantly reduces LC risk (OR=0.26) (56), whereas low vegetable consumption regarded as a risk factor for LC (48).
Environmental factors
According to a study in Tehran, air pollution, dust and the presence of pollutants in the environment are associated with an increased risk of LC mortality (57) and suspended particles below 2.5 micron has been identified as a risk factor for LC with a coefficient of 0.43 (58).
Genetic Factors
Genetic polymorphisms and genetic defects can increase the risk of LC, details of factors associated with LC are presented in Table 1.
Discussion
This systematic review investigated the epidemiological aspects of LC in Iran. In general, LC is one of the most common cancers in Iran and has high mortality. Its incidence is rising in all parts of Iran (8, 9, 33) with an estimation of 5829 cases in 2010 (10). Moreover, the number of LC deaths increased from 4,361 in 2012 (7) to 6,124 in 2018, so LC is the second leading cause of cancer death in Iran, with accounting 11% of cancer deaths (32).
Some of the most significant risk factors for LC incidence are smoking, unhealthy diet, alcoholic drinks, the chemical quality of drinking water, vegetables, fruits and micro-nutrients, occupational exposures, air pollution, benignant lung disease such as asthma and tuberculosis, gender and race (4). In Iran, the main cause of LC is smoking (45, 46) and due to smoking, men have higher risk than women (46).
While increasing trend of LC incidence and mortality in Asian and African countries (83); in Denmark, UK and USA the mortality rate has been decreased due to implementation preventive programs for decreasing the smoking habit and lifestyle changing (84). Asian countries observed a sharp increase in the incidence and mortality rate of LC, due to increasing smoking trend in recent decades (85).
Initiation of preventive programs in recent years may lead to lower smoking in one or two decade, and if would be implemented appropriately, can reduce the increasing trend of LC in less than two decades (86). Thus, decreased smoking or quitting it, as a most effective approach, must be the focus of the public, policy makers, and planners worldwide (87).
Consumption vegetables and fruits is recommended as one of the key strategies in lowering down LC cases and increased consumption of high fat and fried food are considered as a risk factor and according to the prevalence of this risk factor in contemporary society, it became more significant than in the past and needs to proper planning (4, 48).
Mustard gas is one of the causes of LC that many people were exposed to it during the Iran-Iraq war (51). Some studies have reported strong associations between LC and occupation and the environment in Iran (36) such as exposure to smoke and steam and number of metals, including arsenic, chromium, and nickel (59). Therefore, it’s necessary to plan effectively for reducing the exposure time and increasing the safety equipment usage by workers and employers (45, 54, 55).
Environmental pollutions are considered as possible risk factors of LC. Thus, policy making for controlling and reduction of them, seems to be necessary to future control of LC (55, 58).
Conclusion
The incidence and mortality of LC in Iran is rising, while many of its risk factors can be modified; so planning to inform and reduce the risk factors is suggested .Smoking is the most important risk factor for LC, so reducing smoking is the most efficient action.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Financial support
No.
Footnotes
Conflicts of interest
There are no conflicts of interest.
References
- 1.Siegel RL, Miller KD, Jemal A. (2019). Cancer statistics. CA Cancer J Clin, 69 (1): 7–34. [DOI] [PubMed] [Google Scholar]
- 2.Wong MCS, Lao XQ, Ho K-F, et al. (2017). Incidence and mortality of lung cancer: global trends and association with socioeconomic status. Sci Rep, 7 (1): 14300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roshandel G, Ghanbari-Motlagh A, Partovipour E, et al. (2019). Cancer incidence in Iran in 2014: Results of the Iranian National Population-based Cancer Registry. Cancer Epidemiol, 61: 50–8. [DOI] [PubMed] [Google Scholar]
- 4.Sadeghi-Gandomani H, Asgari-Tarazoj A, Ghoncheh M, et al. (2017). Lung cancer in the world: the incidence, mortality rate and risk factors. WCRJ, 4: e911. [Google Scholar]
- 5.Moher D, Liberati A, Tetzlaff J, et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ, 339: b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sadjadi A, Nouraie M, Mohagheghi MA, et al. (2005). Cancer occurrence in Iran in 2002, an international perspective. Asian Pac J Cancer Prev, 6 (3): 359–63. [PubMed] [Google Scholar]
- 7.Almasi Z, Mohammadian-Hafshejani A, Sale-hiniya H. (2016). Incidence, mortality, and epidemiological aspects of cancers in Iran; differences with the world data. J BUON, 21 (4):994–1004. [PubMed] [Google Scholar]
- 8.Bab S, Abdifard E, Moradi Y, et al. (2016). Lung cancer incidence trends in Iran and in six geographical regions of the country (2000 – 2005). Shiraz E Medical Journal, 17 (6): e38237. [Google Scholar]
- 9.Enayatrad M, Mirzaei M, Salehiniya H, et al. (2016). Trends in Incidence of Common Cancers in Iran. Asian Pac J Cancer Prev, 17 (S3):39–42. [DOI] [PubMed] [Google Scholar]
- 10.Mohagheghi MA, Mousavi-Jarrahi Y, Mosavi-Jarrahi A. (2011). Cost of care for lung cancer in the first year after diagnosis in Iran. Asian Pac J Cancer Prev, 12 (4):1013–5. [PubMed] [Google Scholar]
- 11.Sadjadi A, Malekzadeh R, Derakhshan M, et al. (2003). Cancer occurrence in Ardabil: Results of a population-based Cancer Registry from Iran. Int J Cancer, 107: 113–8. [DOI] [PubMed] [Google Scholar]
- 12.Sajadi A, Zahedi MJ, Moghadam SD, et al. (2007). The First Population-Based Cancer Survey in Kerman Province of Iran. Iran J Public Health, 36 (4): 26–34. [Google Scholar]
- 13.Babaei M, Jaafarzadeh H, Sadjadi AR, et al. (2009). Cancer Incidence and Mortality in Ardabil: Report of an Ongoing Population-Based Cancer Registry in Iran, 2004–2006. Iran J Public Health, 38 (4): 25–35. [Google Scholar]
- 14.Roshandel G, Sadjadi A, Aarabi M, et al. (2012). Cancer incidence in golestan province: report of an ongoing population-based cancer registry in Iran between 2004 and 2008. Arch Iran Med, 15 (4): 196–200. [PubMed] [Google Scholar]
- 15.Amoori N, Mirzaei M, Cheraghi M. (2014). Incidence of Cancers in Kuzestan Province of Iran: Trend from 2004 to 2008. Asian Pac J Cancer Prev, 15 (19): 8345–9. [DOI] [PubMed] [Google Scholar]
- 16.Shahesmaeili A, Afshar R.M, Sadeghi A, et al. (2018). Cancer incidence in Kerman Province, Southeast of Iran: Report of an ongoing population-based cancer registry, 2014. Asian Pac J Cancer Prev, 19 (6): 1533–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Somi Mh, Mousavi Sm, Rezaeifar P, et al. (2009). Cancer incidence among the elderly population in the northwest of Iran: a population based study. Int J Cancer, 2 (3): 117–26. [Google Scholar]
- 18.Mezginejad F, Haghighi F, Behravan M, et al. (2016). Cancer Types in Pathological Samples Referred to Educational Hospitals in Birjand During the Past Three Years (2011 – 2013). Int J Cancer Manag, 9 (5): e4075. [Google Scholar]
- 19.Kolahi AA, Mosavi-Jarrahi A. (2007). Incidence of occupational lung cancer in Tehran-Iran. Journal of Thoracic Oncology, 2 (8):S343–S4. [Google Scholar]
- 20.Mohagheghi Sma, Sar Mousavi Jarahi, Malekzadeh R, et al. (2009). Cancer incidence in Tehran metropolis: the first report from the tehran population-based cancer registry, 1998 – 2001. Arch Iran Med, 12 (1): 15–23. [PubMed] [Google Scholar]
- 21.Masoompour SM, Yarmohammadi H, Rezaianzadeh A, et al. (2011). Cancer incidence in southern Iran, 1998–2002: Results of population-based cancer registry. Cancer Epidemiol, 35 (5):e42–7. [DOI] [PubMed] [Google Scholar]
- 22.Karami K, Cheraghi M, Amori N, et al. (2014). Common Cancers in Khuzestan Province, South West of Iran, during 2005–2011. Asian Pac J Cancer Prev, 15 (21):9475–8. [DOI] [PubMed] [Google Scholar]
- 23.Rohani-Rasaf M, Rohani-Rasaf MR, Hashemi Nazari SS, et al. (2017). Cancer Incidence Rate in the Elderly Inhabitants of Tehran: Is there really any Cluster? Int J Cancer Manag, 10 (7):e5753. [Google Scholar]
- 24.Keyghobadi N, Rafiemanesh H, Mohammadian-Hafshejani A, et al. (2015). Epidemiology and trend of cancers in the province of Kerman: southeast of Iran. Asian Pac J Cancer Prev, 16 (4): 1409–13. [DOI] [PubMed] [Google Scholar]
- 25.Rahimi Z, Kasraei R, Najafi F, et al. (2015). Cancer notification at a referral hospital of Kermanshah, Western Iran (2006–2009). Asian Pac J Cancer Prev, 16 (1): 133–7. [DOI] [PubMed] [Google Scholar]
- 26.Bozorgi F, Hedayatizadeh-Omran A, Alizadeh-Navaei R, et al. (2017). Causes of Death of Cancer Patients in a Referral Hospital in Northern Iran between 2013 and 2016. WCRJ, 4 (3): e909. [Google Scholar]
- 27.Vardanjani HM, Zeinali M, Radmerikhi S, et al. (2017). Lung Cancer Prevalence in Iran by Histologic Subtypes. Adv Biomed Res, 6:111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tolou Ghamari Z. (2018). Prevalence of lung cancer in Isfahan Province, Iran. 2018. J Egypt Natl Canc Inst, 30 (2): 57–9. [DOI] [PubMed] [Google Scholar]
- 29.Modirian M, Rahimzadeh S, Cheraghi Z, et al. (2015). Burden of Cancers in Iran from 1990 to 2010: findings from the Global Burden of Disease study 2010. Arch Iran Med, 18 (10): 629–37. [PubMed] [Google Scholar]
- 30.Rajai N, Ghanbari A, Yoosefi M, et al. (2020). National and subnational trends in incidence and mortality of lung cancer in Iran from 1990 to 2016. Asia Pac J Clin Oncol, 16 (3): 129–36. [DOI] [PubMed] [Google Scholar]
- 31.Ghasemi S, Mahaki B, Dreassi E, et al. (2020). Spatial Variation in Lung Cancer Mortality and Related Men-Women Disparities in Iran from 2011 to 2014. Cancer Manag Res, 12: 4615–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Global Cancer Observatory (2021). Iran-islamic-republic-of-fact-sheets: The Global Cancer Observatory. International Agency for Research on Cancer, Lyon, France. Available from: https://gco.iarc.fr/today/data/factsheets/populations/364-iran-islamic-republic-of-fact-sheets.pdf. [Google Scholar]
- 33.Almasi Z, Salehiniya H, Amoori N, et al. (2016). Epidemiology Characteristics and Trends of Lung Cancer Incidence in Iran. Asian Pac J Cancer Prev, 17 (2): 557–62. [DOI] [PubMed] [Google Scholar]
- 34.Khazaei S, Mansori K, Soheylizad M, et al. (2017). Epidemiology of lung cancer in Iran: Sex difference and geographical distribution. Middle East Journal of Cancer, 8: 223–8. [Google Scholar]
- 35.Motovali-bashi M, Taghvaei S, Hemati S. (2012). The Association between Gelatinase B and Lung Cancer in Smokers and Non-Smokers. Journal of Isfahan Medical School, 30:1393–402. [Google Scholar]
- 36.Ghobadi H, Sharghi A, Sadat-Kermani J. (2013). Epidemiology and Risk Factors for Lung Cancer in Ardabil, Iran. JArUMS, 13 (2): 220–8. [Google Scholar]
- 37.Abbasi M, Moradi F, Esna-Ashari F, et al. (2019). Epidemiological and Pathological Study of Lung Cancer in Patients Referred to Ekbatan and Shahid Beheshti Hospitals in Hamadan during 2001 – 2016. Avicenna Journal of Clinical Medicine, 25 (4): 236–43. [Google Scholar]
- 38.Adnan K, Esfahani-Monfared Z, Sei S, et al. (2016). Clinicopathological Characteristics of Iranian Patients with Lung Cancer: a Single Institute Experience. Asian Pac J Cancer Prev, 17 (8): 3817–22. [PubMed] [Google Scholar]
- 39.Shahbazi-Gahrouei D, Danesh A. (2004). Investigation of cancers incidence relevant to radiation in Chaharmahal and Bakhtiari province during five years (1998–2002). J Shahrekord Univ Med Sci, 6 (1):7–13. [Google Scholar]
- 40.Adham D, Asl E, Abbasgholizadeh N, et al. (2019). Spatial Analysis and Epidemiology of Lung Cancer in the Northwest of Iran. P J M H S, (12): 20181851. [Google Scholar]
- 41.Hajmanoochehri F, Mohammadi N, Zohal MA, et al. (2014). Epidemiological and clinico-pathological characteristics of lung cancer in a teaching hospital in Iran. Asian Pac J Cancer Prev, 15 (6):2495–500. [DOI] [PubMed] [Google Scholar]
- 42.Salari A, Taghipour S, Moghimi M, et al. (2012). Evaluation of frequency of clinical and pathological findings in lung diseases in shahid Sadoughi University of medical sciences of yazd, during 2001–2006. Iranian Journal of Surgery, 20 (1): 27–33. [Google Scholar]
- 43.Abedi S, Janbabaee G, Moosazadeh M, et al. (2017). Epidemiology of Lung Cancer Patients Attending Tooba Clinic and Imam Khomeini Hospital, Sari, Iran 2010–2014. J Mazandaran Univ Med Sci, 27 (151): 86–93. [Google Scholar]
- 44.Akbarzadeh Ba, Esmaeili M, Kimiafar K. (2009). Medical information management and assessment of direct costs of treatment of lung cancer. Health Information Management, 5 (2):151–8. [Google Scholar]
- 45.Hosseini M, Naghan PA, Karimi S, et al. (2009). Environmental risk factors for lung cancer in Iran: a case–control study. Int J Epidemiol, 38 (4): 989–96. [DOI] [PubMed] [Google Scholar]
- 46.Ghobadi M, Farrokhi MR, Nakhaee N, et al. (2017). Estimation of the Cost of Smoking-Attributable Diseases (Five Selected Diseases): A Case in Kerman City, Iran, 2014. Addict Health, 9 (4): 190–8. [PMC free article] [PubMed] [Google Scholar]
- 47.Hosseini M, Naghan PA, Jafari AM, et al. (2014). Nutrition and lung cancer: a case control study in Iran. BMC Cancer, 14: 860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Najafi F, Moradinazar M, Barati M JT, et al. (2016). Correlation between risk factors for non-communicable diseases and common cancers in Iran: Ecological study. International Business Management, 10 (15):3015–9. [Google Scholar]
- 49.Masjedi MR, Naghan PA, Taslimi S, et al. (2013). Opium Could Be Considered an Independent Risk Factor for Lung Cancer: A Case-Control Study. Respiration, 85 (2):112–8. [DOI] [PubMed] [Google Scholar]
- 50.Akbari AB, Rezaei S, Arab M, et al. (2016). Effects of Smoking on Cost of Hospitalization and Length of Stay among Patients with Lung Cancer in Iran: a Hospital-Based Study. Asian Pac J Cancer Prev, 17 (9):4421–6. [PubMed] [Google Scholar]
- 51.Zafarghandi MR, Soroush MR, Mahmoodi M, et al. (2013). Incidence of cancer in Iranian sulfur mustard exposed veterans: a long-term follow-up cohort study. Cancer Causes Control, 24 (1): 99–105. [DOI] [PubMed] [Google Scholar]
- 52.Nadji SA, Mahmoodi M, Ziaee AA, et al. (2007). An increased lung cancer risk associated with codon 72 polymorphism in the TP53 gene and human papillomavirus infection in Mazandaran province, Iran. Lung Cancer, 56 (2): 145–51. [DOI] [PubMed] [Google Scholar]
- 53.Hosseini-khalili A, Haines DD, Modirian E, et al. (2009). Mustard gas exposure and carcinogenesis of lung. Mutat Res, 678 (1): 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alberg AJ, Yung RC, Strickland PT J. N. (2002). Respiratory cancer and exposure to arsenic, chromium, nickel, and polycyclic aromatic hydrocarbons. Clinics in Occupational and Environmental Medicine. Bloomberg School of Public Health, 2 (4): 779–801. [Google Scholar]
- 55.Rashidi M, Rameshat MH R. R. (2014). Geographic Health and Human Health; Using Space Technology and Remote Sensing in Monitoring Soil Pollution by Arsenic and the Related Lung Cancer in Isfahan, Iran: A Case Study. Journal of Isfahan Medical Sciences, 32 (287): 784–90. [Google Scholar]
- 56.Karimzadeh L, Koohdani F, Siassi F, et al. (2012). Relation between nitrate and nitrite food habits with lung cancer. J Exp Ther Oncol, 10 (2):107–12. [PubMed] [Google Scholar]
- 57.Hadei M, Hashemi Nazari SS, Yarahmadi M, et al. (2017). Estimation of Gender-Specific Lung Cancer Deaths due to Exposure to PM2.5 in 10 Cities of Iran during 2013 – 2016: A Modeling Approach. Int J Cancer Manag, 10 (8):e10235. [Google Scholar]
- 58.Mobasheri MRA. H. (2014). Using Satellite Images for Determination of Critical Points in Polluted Cities and their Relation to Lung Cancer Affection. Hakim Health Systems Research Journal, 17 (2):151–8. [Google Scholar]
- 59.Razmkhah M, Doroudchi M, Ghayumi SM, et al. (2005). Stromal cell-derived factor-1 (SDF-1) gene and susceptibility of Iranian patients with lung cancer. Lung Cancer, 49 (3):311–5. [DOI] [PubMed] [Google Scholar]
- 60.Mosavi-Jarrahi A, Mohagheghi M, Kalaghchi B, et al. (2009). Estimating the incidence of lung cancer attributable to occupational exposure in Iran. Popul Health Metr, 7:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Karimzadeh L, Koohdani F, Siassi F, et al. (2011). A case control study on the lung cancer risk factors in north of Iran. J Exp Ther Oncol, 9 (2): 153–8. [PubMed] [Google Scholar]
- 62.Mahaki B, Mehrabi Y, Kavousi A, et al. (2011). Multivariate disease mapping of seven prevalent cancers in Iran using a shared component model. Asian Pac J Cancer Prev, 12 (9): 2353–8. [PubMed] [Google Scholar]
- 63.Safari A, Reazai M, Tangestaninejad A, et al. (2016). Opium consumption: A potential risk factor for lung cancer and pulmonary tuberculosis. Indian J Cancer, 53 (4): 587–9. [DOI] [PubMed] [Google Scholar]
- 64.Dehghani M, Samani Z, Abidi H, et al. (2018). Relationship of SNP rs2645429 in Farnesyl-Diphosphate Farnesyltransferase 1 Gene Promoter with Susceptibility to Lung Cancer. Int J Genomics, 2018:4863757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Motovali-Bashi M, Biglari M, Hojati Z, et al. (2012). Role of CYP1A1 MspI polymorphism in CYP1A1 gene with susceptibility to lung cancer in Iranian patients. J Res Med Sci, 17 (5):1.23248650 [Google Scholar]
- 66.Keeley BR, Islami F, Pourshams A, et al. (2014). Prediagnostic serum levels of inflammatory biomarkers are correlated with future development of lung and esophageal cancer. Cancer Sci, 105 (9):1205–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nikseresht M, Shahverdi M, Dehghani M, et al. (2018). Association of single nucleotide autophagy-related protein 5 gene polymorphism rs2245214 with susceptibility to non-small cell lung cancer. J Cell Biochem, 120 (2):1924–31. [DOI] [PubMed] [Google Scholar]
- 68.Adibhesami G, Shahsavari GR, Amiri A, et al. (2018). Glutathione S-transferase M1 (GSTM1) and T1 (GSTT1) Polymorphisms and Lung Cancer Risk among a Select Group of Iranian People. Asian Pac J Cancer Prev, 19 (10): 2921–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rahmati A, Shakeri R, Khademi H, et al. (2017). Mortality from respiratory diseases associated with opium use: a population-based cohort study. Thorax, 72 (11): 1028–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Eydian Z, Asna’ashari AM, Behravan J, et al. (2016). Association of P53 codon 72 polymorphism and lung cancer in an ethnic Iranian population. Cell Mol Biol (Noisy-le-grand), 62 (9):34–8. [PubMed] [Google Scholar]
- 71.Motovali-Bashi M, Rezaei H, Dehghanian F, et al. (2014). Association between XPD (Lys751G1n) Polymorphism and Lung Cancer Risk: A Population-Based Study in Iran. Cell J, 16 (3): 309–14. [PMC free article] [PubMed] [Google Scholar]
- 72.Rikhtegar S, Hesampour A. (2018). Investigation of KRAS and NRAS expression levels in lung cancer patients compared to normal patients. Yafte, 20 (3): 19–27. [Google Scholar]
- 73.Ahmadi M, Moshtaghioun SM, Falahati A. (2018). Association of the CHRNA3 rs1051730 single nucleotide polymorphism with lung cancer risk in Iranian patients. JSSU, 26 (7): 599–606. [Google Scholar]
- 74.Chitsaz M, Hesampour A. (2018). Investigating the Expression of EGFR and FGFR4 Genes in Patients with Lung Cancer. JBUMS, 20 (4): 17–23. [Google Scholar]
- 75.Amini F, Motovalli Bashi M, Hemmati S. (2018). Study of egfr gene in relationship between polymorphism and mir-214 binding site in lung cancer. Pejouhesh dar Pezeshki (Research in Medicine), 41 (4): 268–274. [Google Scholar]
- 76.Motovali-bashi M, Taghvaei S, Hemati S. (2012). The association between the C (-1562)t polymorphism of type IV collagenase gene and reduced age of onset of lung cancer. Journal of Isfahan Medical School, 30 (203): 1–9 [Google Scholar]
- 77.Motovali-Bashi M, Bordbar M, Rezaei H. (2012). Study of association between T/C single nucleotide polymorphism in CYP1A1 gene and cancer initiation and smoking status in lung cancer patients. Pejouhesh dar Pezeshki (Research in Medicine), 36 (3): 151–6. [Google Scholar]
- 78.Motovali-Bashi M, Hojati Z. (2013). Investigation of correlation between −765G/C polymorphism of cyclooxygenase 2 genes and lung cancer in Isfahan population. Pejouhesh dar Pezeshki (Research in Medicine), 37 (1): 47–54. [Google Scholar]
- 79.Ghayyoumi M, Mansouri M. (2015). Determination of Serum level of Triose Phosphate Isomerase in lung Cancer Patients. Armaghane Danesh, 19 (11): 948–54. [Google Scholar]
- 80.Hamedi F, Tahmaseb MAG. (2016). Prognostic Importance of Polymorphisms in DNA-Repair Gene (XRCC1 Arg399Gln) in Patients with Lung Cancer in Fars Province, Iran. Journal of Isfahan Medical School, 34 (403): 1244–50. [Google Scholar]
- 81.Keshvary Ravan H, Kouhkan F, Sazgar H. (2017). Single Nucleotide Polymorphisms of MMP2 Gene Promoter on the Risk of Development and Metastasis of lung Cancer. Armaghane Danesh, 22 (1): 104–17. [Google Scholar]
- 82.Sazgar H. (2017). Evaluation of correlation between −1562 C/T in promoter single nucleotide polymorphisms of MMP-9 gene and lung cancer initiationand metastasis risk. Pars of Jahrom University of Medical Sciences, 15 (2): 9–16. [Google Scholar]
- 83.Pakzad R, Mohammadian-Hafshejani A, Ghoncheh M, et al. (2015). The incidence and mortality of lung cancer and their relationship to development in Asia. Transl Lung Cancer Res, 4 (6): 763–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jemal A, Center MM, DeSantis C, et al. (2010). Global patterns of cancer incidence and mortality rates and trends. Cancer Epidemiol Biomarkers Prev, 19 (8):1893–907. [DOI] [PubMed] [Google Scholar]
- 85.Bogos K, Kiss Z, Gálffy G, et al. (2019). Revising Incidence and Mortality of Lung Cancer in Central Europe: An Epidemiology Review from Hungary. Front Oncol, 9:1051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.de Groot P, Munden RF. (2012). Lung cancer epidemiology, risk factors, and prevention. Radiol Clin North Am, 50 (5): 863–76. [DOI] [PubMed] [Google Scholar]
- 87.Jazieh AR, AlGhamdi M, AlGhanem S, et al. (2018). Saudi lung cancer prevention and screening guidelines. Ann Thorac Med, 13 (4):198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]