Abstract
Background
Homelessness has been associated with multiple detrimental health outcomes across observational studies. However, relatively few randomized controlled trials (RCTs) have been conducted on people who experience homelessness (PEH). Thus, this umbrella review ranked the credibility of evidence derived from systematic reviews (SRs) and meta-analyses (MAs) of observational studies investigating the associations between homelessness and any health outcome as well as RCTs targeting health needs in this population.
Methods
Several databases were systematically searched from inception through April 28, 2021. Any SR and/or MA reporting quantitative data and providing a control group were eligible for inclusion. The credibility of the evidence derived from observational studies was appraised by considering the significance level of the association and the largest study, the degree of heterogeneity, the presence of small-study effects as well as excess significance bias. The credibility of evidence was then ranked in five classes. For SRs and/or MAs of RCTs, we considered the level of significance and whether the prediction interval crossed the null. The AMSTAR-2 and AMSTAR-plus instruments were adopted to further assess the methodological quality of SRs and/or MAs. The Newcastle-Ottawa Scale (NOS) was employed to further appraise the methodological quality of prospective cohort studies only; a sensitivity analysis limited to higher quality studies was conducted.
Results
Out of 1549 references, 8 MAs and 2 SRs were included. Among those considering observational studies, 23 unique associations were appraised. Twelve of them were statistically significant at the p≤0.005 level. Included cases had worst health-related outcomes than controls, but only two associations reached a priori-defined criteria for convincing (class I) evidence namely hospitalization due to any cause among PEH diagnosed with HIV infection, and the occurrence of falls within the past year among PEH. According to the AMSTAR-2 instrument, the methodological quality of all included SRs and/or MAs was “critically low.” Interventional studies were scant.
Conclusion
While homelessness has been repeatedly associated with detrimental health outcomes, only two associations met the criteria for convincing evidence. Furthermore, few RCTs were appraised by SRs and/or MAs. Our umbrella review also highlights the need to standardize definitions of homelessness to be incorporated by forthcoming studies to improve the external validity of the findings in this vulnerable population.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12916-022-02423-z.
Keywords: Homeless, Health outcomes, Severe mental illness, Umbrella review
Background
Homelessness is an important social, public health, and human rights issue worldwide. The prevalence of homelessness varies among diverse countries and cultures around the world. Lifetime prevalence estimates from representative samples are 4.2% in the USA [1] to 4.9% in Europe [2]. However, high-quality data on the prevalence of homelessness in low- and middle-income countries (LMICs) is scant.
The operational definitions for homelessness likewise vary across different literature sources and settings [3] although a commonly accepted and implemented definition of homelessness globally comes from the European Typology of Homeless and Housing Exclusion study [4].
People experiencing homelessness (PEH) may face social and economic challenges that may lead to poor health, such as poverty, poor nutrition, and social exclusion. People who lack stable and appropriate housing appear to be at relatively high risk for a broad range of acute and chronic illnesses, especially infectious diseases, heart diseases, substance use disorders, and severe mental disorders [5]. However, it is unclear whether homelessness causes these disorders or otherwise these illnesses per se contribute to homelessness. Finally, evidence indicates that PEH has a lower probability of receiving proper care for their health conditions compared to the general population [6].
Data about differences in the prevalence of multiple health conditions between PEH and the general population is substantially unreliable, as exemplified by current knowledge about mental health [7] and infectious diseases among PEH [8]. Cohort and case-control studies have reported various health outcomes associated with homelessness, and several health outcomes have been the subject of a multitude of systematic reviews (SRs) and meta-analyses (MAs). While informative, this latter knowledge synthesis is usually restricted to a single outcome, and some of their results may be affected by biases, which are often poorly appraised [9]. Furthermore, randomized controlled trials (RCTs) targeting health-related outcomes in homeless populations are few, thus providing limited evidence to inform health policies [10]. Specifically, significant associations claimed by the original observational studies, or their pooled synthesis may be susceptible to biases such as excess significance [11], publication bias, reporting bias, and residual confounding, leading to misleading or inflated estimates of these associations [12].
Umbrella reviews (URs)—a systematic collection and appraisal of SRs and MAs performed on a specific topic [13]—can disentangle the aforementioned biases through appraising the quality and comprehensiveness of the data, and hence, assess which associations derived from observational studies are supported by the most credible evidence. Likewise, URs can provide a methodological appraisal of RCTs targeting a specific population or condition. Thus, in the current report, we aimed to conduct an umbrella review of the evidence from observational studies and RCTs considering multiple health outcomes involving PEH. In particular, we aimed at (i) assessing the reported association measures between homelessness and any health outcome and (ii) appraising the interventions targeting any health outcome among PEH.
Methods
Search strategy
We performed an umbrella review that included observational or RCTs that investigated the association between homelessness and any health outcome. The PubMed/MEDLINE, EMBASE, and SCOPUS databases were systematically searched from inception up to April 28, 2021. The following string was adopted for PubMed: (((“homeless persons”[MeSH Terms]) OR (“homeless youth”[MeSH Terms])) OR (“vulnerable populations”[MeSH Terms]) OR (homeless*[Title/Abstract])) AND (((((“meta analysis as topic”[MeSH Terms]) OR (“systematic reviews as topic”[MeSH Terms])) OR (“meta analysis”[Title/Abstract])) OR (“systematic review”[Title/Abstract]))). Please see Additional file 1: material 1. The definition of homelessness and related phenomena were independently recorded by two investigators.
Eligibility criteria
For the synthesis of evidence from SRs and MAs of observational studies, we included those studies reporting any health outcome among PEH compared to the general population or otherwise provided controls (i.e., people who are not experiencing homelessness, PEH without a particular exposure). We excluded those SRs or MAs of observational studies that only provided prevalence estimates of a given health condition in PEH without providing a measure of association. Specifically, those studies reporting interventions just targeting housing, but not the related health status, were likewise excluded. The SRs and MAs of RCTs suitable for inclusion were those documenting interventions targeting any health outcome among PEH; controls were PEH exposed to a health-targeting intervention different from the health-outcome intervention delivered to PEH cases. Eligible quantitative SRs and MAs of observational studies had to include at least 3 studies; eligible SRs and MAs of intervention studies had to include at least 5 studies. The rationale for this inclusion criterion is explained in detail elsewhere [14]. In the case of multiple MAs reporting on the same topic (i.e., overlapping with the same type of intervention or exposure), we considered only the one that included the largest number of studies as it is a standard procedure in previously conducted umbrella reviews [15, 16]. In cases there were two or more MAs pooling the same number of studies, we retained the most recent one. Qualitative reports were excluded. There were no language restrictions for the inclusion of studies for this umbrella review.
The protocol for this study was registered in PROSPERO with the following numbers: CRD42021252185, for the protocol investigating observational studies, and CRD42021252191 for the protocol that assessed evidence from intervention studies, respectively. Complete versions of each protocol are fully available online at https://osf.io/am67d/ and https://osf.io/58mhu/.
Data extraction
Three investigators (MDP, MB, MF) independently searched title/abstracts of retrieved references for eligibility, and when a consensus could not be achieved, additional authors with considerable expertise in umbrella reviews (AFC, MS, LS) and the study of homelessness (LS, JGF, SH, MK) were consulted. The same procedure was followed at the full-text level. The reference lists of included studies were also searched for the identification of additional eligible references. Among other variables, we recorded the following: publication year, considered health outcome, study design, number of the included studies, total sample size, homelessness definition, and disclosure of sponsorship. For each primary study included in the SRs or MAs, we additionally recorded the first author, year of publication, study design (i.e., cohort, case-control, cross-sectional, RCT), setting of the study (i.e., inpatients, outpatients, population-based), number of subjects included in the study (total sample, cases, and controls), sex, ethnicity, both adjusted and unadjusted effect sizes (ES), and 95% confidence interval (CI). Intervention and mean duration of RCT studies were likewise extracted.
Data analysis and assessment of the credibility of evidence
We re-analyzed each eligible MA using the extracted individual study estimates to compute the summary effect estimates and the exact p-value under the random-effects model with DerSimonian and Laird method if included studies were equal or more than 10, and Hartung, Knapp, Sidik, and Jonkman (HKSJ) if less than 10 [17, 18]. Cochran’s Q test and the I2 statistics were computed for the evaluation of heterogeneity across studies (I2>50% indicated high heterogeneity) [19, 20]. To further account for heterogeneity between studies, we computed 95% prediction intervals for the summary random-effect estimates [21]. We evaluated the presence of small-study effects (i.e., large studies fetching significantly more conservative results than smaller studies) by adopting the Egger’s regression asymmetry test (p≤0.10) [22]. For statistically significant MAs, we assessed the presence of excess significance bias by evaluating whether the number of observed studies with nominally statistically significant results was different from the expected number of studies with statistically significant results [23]. The expected number of statistically significant studies in each association was calculated from the sum of the statistical power estimates for each component study using an algorithm from a non-central t distribution [24–26]. The power estimates of each component study depended on the plausible effect size of the tested association, which was assumed to be the effect size of the largest study in each MA [27]. The presence of excess significance bias for individual MAs was considered at p≤0.10. The credibility of the evidence of each association provided by MAs of observational studies was assessed using the criteria previously applied in various medical fields [26, 28, 29], waiving the “number of cases” criterion since some health outcomes of PEH represent infrequent events. Briefly, the associations that presented nominally significant random-effect summary estimates were considered as “convincing” (Class I), “highly suggestive” (Class II), “suggestive” (Class III), “weak evidence” (Class IV), or “non-significant” (NS). Please, see the credibility box in Additional file 1: Table S1. For MAs of intervention studies, we assessed the significance of the pooled effect size as P<0.005, P=0.005–0.005, and P≥0.05 [30], the 95% prediction interval (excluding the null or not), the significance of the effect size of the largest study, and the presence of large heterogeneity (i.e., I2>50%) [31]. In addition, the methodological quality of those SRs and/or MAs was further appraised with the Assessment of Multiple Systematic Reviews Plus (AMSTAR-Plus) instrument [32]. All statistical tests were two-tailed. The data abstraction was performed using pre-defined Microsoft Excel® forms, while the statistical computations were carried out by an expert senior author (ED) using the STATA/SE, version 17.0 (StataCorp LLC) software. For each eligible quantitative report, two investigators (MDP and MB) independently rated the methodological quality using the AMSTAR-2 (Assessment of multiple SRs) tool [33] for quantitative SRs or MAs of observational studies. The prospective cohort studies included in the quantitative SRs or MAs of observational studies were rated for quality using the Newcastle-Ottawa scale (NOS) [34]. Finally, we adopted the following thresholds for the NOS scores: “good quality” (3-4 stars in the “selection domain” AND 1-2 stars in the “comparability” domain AND 2-3 stars in the “outcome” domain), “fair quality” (2 stars in the “selection domain” AND 1-2 stars in the “comparability” domain AND 2-3 stars in the “outcome” domain), and “poor quality” (0-1 stars in the “selection domain” OR 0 stars in the “comparability” domain OR 0-1 star in the “outcome” domain) [35].
Results
The search returned 1549 potentially eligible records, of which 11 records were manually retrieved. Upon title and abstract screening, 189 records were further assessed at the full-text level, of which 179 were excluded with reasons as detailed in Additional file 1: Table S2 [7, 8, 36–210]. Nine SRs or MAs of observational studies [211–219] were included, which yielded 23 comparisons. One MA of interventional studies [220] fetched two comparisons. Figure 1 provides a flowchart for study selection.
Fig. 1.
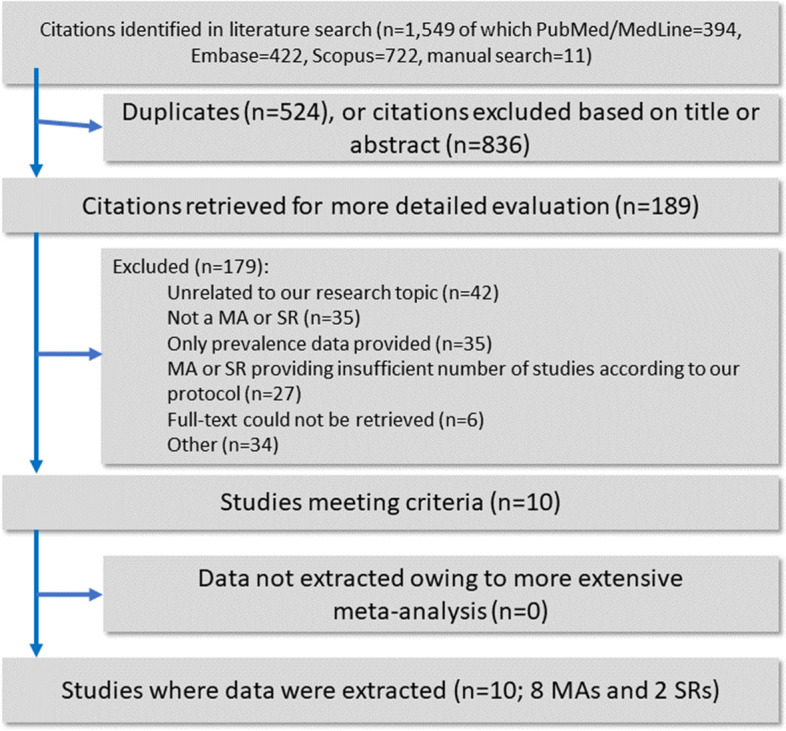
Flowchart of the literature search and evaluation process returning 10 systematic reviews and meta-analyses
Given the scant evidence for intervention studies, we decided to combine the reporting of both registration protocols into a single publication.
Descriptive characteristics of the 10 included eligible SRs and MAs of observational and intervention studies are outlined in Table 1. The observational studies had the following control groups: PEH without SUD [211], PEH who did not inject drugs [212], people not experiencing homelessness [213–215, 218, 219], or the general population [216, 217]. Although substantially overlapping, we nonetheless recorded “people not experiencing homelessness” and “general population” controls, as documented by the original study at review. The included MA of RCTs controlled for various treatment exposures [220].
Table 1.
Characteristics of the included SRs or MAs of observational and interventional studies
| Author, year (type of study) | Type of studies included | Health outcome examined | Exposures/active treatment | Control group | No. of studies included in the MA or SR (No. of studies included in the present UR) | Population | Homelessness adopted definition | AMSTAR-2 or AMSTAR-plus |
|---|---|---|---|---|---|---|---|---|
| Tweed et al., 2021 (MA) [215] | Cross-sectional, case-control, cohort studies, and baseline data from interventional studies | Mortality, morbidity, health-related quality of life, self-rated health | Homelessness, imprisonment, substance use (other than alcohol, cannabis, or performance-enhancing drugs), sex working, SMI | Absence of homelessness, imprisonment, substance use, sex working, or SMI | 237 (5) | People experiencing homelessness, imprisonment, substance use, sex working, or SMI | People who are rough sleeping or unstably/marginally housed | Critically low |
| Arum et al., 2021 (MA) [216] | Cross-sectional, case-control, cohort studies | HIV and HCV diagnosis | Homelessness, unstable housing | Absence of homelessness or unstable housing | 37 (24) | People who use injective drugs | Lacking access to adequate housing, according to the Institute of Global Homelessness | Critically low |
| Suh et al., 2020 (MA) [217] | Cross-sectional, cohort studies | Geriatric syndrome outcomes | Homelessness | Absence of homelessness | 5 (4) | People experiencing homelessness | People lacking a fixed, regular, and adequate nighttime residence, including those utilizing temporary shelters, being homeless, living in an abandoned building or vehicle, or any other unstable or nonpermanent situation, according to the US Department of Health and Human Services | Critically low |
| Al-Shakarchi et al., 2020 (MA) [218] | Case-control, cohort studies | Cardiovascular disease | Homelessness | Absence of homelessness | 17 (9) | People experiencing homelessness | Not provided | Critically low |
| van Draanen et al., 2020 (SR) [219] | Cross-sectional, case-control, cohort studies | Opioid-related fatal and non-fatal overdose | Any measure of socioeconomic marginalization | Different levels of socio-economic marginalization | 37 (4) | People who use opioids in North America, Europe, the United Kingdom, Australia, and New Zealand | Not provided | Critically low |
| Lin et al., 2019 (MA) [220] | Cross-sectional, cohort studies | Antiretroviral therapy adherence | Homelessness, sex working, or drug use | Absence of homelessness, sex working, or drug use | 29 (4) | People with HIV infection | Not provided | Critically low |
| Aldridge et al., 2017 (MA) | SRs, MAs, cross-sectional, cohort studies | Mortality, morbidity | Homelessness, imprisonment, sex working, substance use disorder | Absence of homelessness, imprisonment, sex working, or substance use disorder | 337 (3) | People experiencing homelessness, imprisonment, substance use, or sex working | Not provided | Critically low |
| Bassuk et al., 2015 (MA) [222] | Cross-sectional, case-control, cohort studies | Mental health disorders, behavioral disorders | Homelessness | Absence of homelessness | 7 (7) | Children/adolescents experiencing homelessness aged less than 18 years, enrolled in the United States and accompanied by a parent | The literal definition of homelessness includes emergency shelter, transitional housing, residing in places not meant for human habitation, fleeing domestic violence, or not having an identified residence | Critically low |
| Aidala et al. 2016 (SR) [223] | Cross-sectional, case-control, cohort studies, RCT | HIV health care access and utilization, adherence to antiretroviral treatments, HIV clinical health outcomes, other health outcomes, emergency department, and inpatient use, HIV risk behaviors | Homelessness, unstable housing | Absence of homelessness or unstable housing | 152 (19) | People with HIV infection who live in high-income countries | Not provided | Critically low |
| Hyun et al., 2020 (MA) [224] | RCT, cluster RCT | Depression, anxiety, mental health status, PTSD symptoms, psychological distress, self-efficacy, quality of life | Psychosocial interventions | Control condition | 11 (6) | People experiencing homelessness | Living situation of rooflessness without a shelter of any kind and houselessness with a temporary institution or shelter to sleep, according to the European typology on homelessness and housing exclusion | 10 |
MA meta-analysis, PTSD post-traumatic stress disorder, RCT randomized controlled trial, SMI severe mental illness, SR systematic review, UR umbrella review
Description and summary of associations
Observational studies
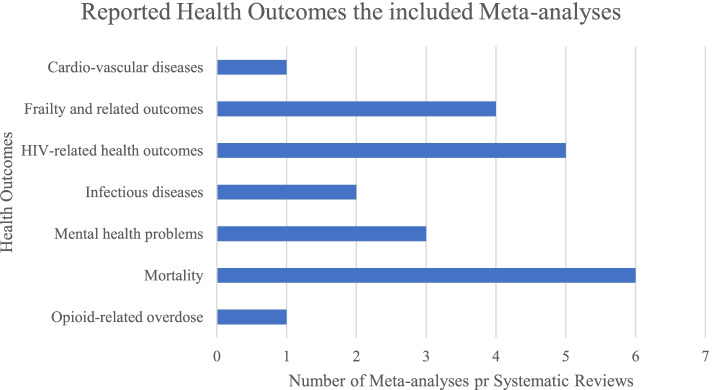
Nine eligible SRs and/or MAs of observational studies assessed 23 associations, evaluated by 122 individual studies from 73 original reports, estimating adverse health outcomes associated with homelessness. Six (26.1%) associations concerned various causes of mortality among PEH, five (21.7%) associations regarded health outcomes related to HIV infection, and four (17.4%) associations inquired about premature geriatric syndromes (e.g., falls, functional limitations). Please refer to Fig. 2 for additional details. Twelve out of 23 (52.2%) associations were nominally statistically significant at a p≤0.005 level based on the random-effects model, and 7 (30.4%) reached p≤1×10−6. Fifteen associations (65.2%) had large heterogeneity, and the 95% prediction interval excluded the null value for only five associations (21.7%). In twenty associations (86.9%), the effect of the largest study was statistically significant at p≤0.05. A small-study effect was detected in one association (4.3%), and excess significance bias occurred in one out of ten studies suitable for such estimation (10%). Please refer to Table 2 for details.
Fig. 2.
Number of systematic reviews or meta-analyses of observational studies reporting health outcomes among PEH by category of health outcome
Table 2.
Evidence from SRs or MAs of observational studies for the association between homelessness and any health outcome
| Criteria for Level-of-Evidence Classification | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author, year | Adverse health outcomes | Exposed/unexposed | Prevalence (%) based on cohort studies | No. of included studies per association | Random-effects measure, ES (95% CIs) | Results | p value random effects | I2 (p value) | PIs (95 % CIs) | SSE/ESB | LS | CE | AMSTAR-2 quality |
| Aidala et al., 2016 [223] | Hospitalization due to any cause | PEH with HIV/Non-homeless with HIV | 21.8% | 4 | OR: 2.05 (1.7–2.46) | Increased odds for PEH with HIV | 4.6×10−15 | 4.5% (0.85) | 1.31–3.19 | No/no | Yes | I | Critically low |
| Suh et al., 2020 [217] | Falls in the previous year | PEH/Non-homeless | NA | 3 | RR: 3.42 (3.15–3.70) | Increased chances for PEH | 1.07×10−199 | 0.08% (0.969) | 2.03–5.73 | No/No | Yes | I | Critically low |
| Aldridge et al., 2017 | Mortality due to any cause | PEH/General population | NA | 5 | SMR: 6.22 (4.2–9.2) | Increased chances for PEH | 6.8×10−20 | 98.16% (0.0001) | 1.53–25.33 | No/NA | Yes | II | Critically low |
| Aldridge et al., 2017 | Mortality due to external causes, as defined by ICD-10 | PEH/General population | NA | 6 | SMR: 15.75 (10.58–23.44) | Increased chances for PEH | 5.2×10−42 | 97.43% (0.0001) | 3.63–68.17) | No/NA | Yes | II | Critically low |
| Arum et al., 2021 [216] | HCV infection | PEH who inject drugs/PEH who did not inject drugs | NA | 19 | RR: 1.66 (1.37−2) | Increased chances for PEH who inject drugs | 1.4×10−7 | 55.4% (0.0019) | 0.88–3.12 | No/NA | Yes | II | Critically low |
| Suh et al., 2020 [217] | Limitations in activities of daily living | PEH/Non-homeless | NA | 4 | RR: 1.46 (1.27–1.68) | Increased chances for PEH | 8.7×10−8 | 53.2% (0.057) | 0.85–2.49 | No/No | Yes | II | Critically low |
| Suh et al., 2020 [217] | Limitations in instrumental activities of daily living | PEH/Non-homeless | NA | 4 | RR: 1.36 (1.25–1.48) | Increased chances for PEH | 7.4×10−13 | 44.9% (0.199) | 0.99–1.85 | No/No | Yes | II | Critically low |
| Aidala et al., 2016 [223] | Emergency department use due to any cause | PEH with HIV/Non-homeless with HIV | 21.6% | 6 | OR: 1.73 (1.31–2.28) | Increased chances for PEH with HIV | 1×10−4 | 67.2% (0.22) | 0.75–3.97 | No/No | Yes | III | Critically low |
| Aidala et al., 2016 [223] | Nonadherence to antiretroviral therapy | PEH/Non-homeless | 8.5% | 5 | OR: 1.55 (1.29–1.86) | Increased chances for PEH | 2.3×10−6 | 16.5% (0.689) | 1.04–2.31 | No/Yes | Yes | III | Critically low |
| Al-Shakarchi et al., 2020 [218] | Diagnosis of cardiovascular disease, as defined by ICD-10 | PEH/Non-homeless | 26.8% | 9 | OR: 2.59 (1.61–4.18) | Increased chances for PEH | 9.6×10−5 | 98.4% (0.0001) | 0.44–15.23 | No/NA | Yes | III | Critically low |
| Arum et al., 2021 [216] | HIV infection | PEH who inject drugs/PEH who did not inject drugs | NA | 12 | RR: 1.43 (1.12–1.83) | Increased chances for PEH who inject drugs | 0.0037 | 52.9% (0.015) | 0.72–2.85 | No/NA | Yes | III | Critically low |
| van Draanen et al., 2020 [219] | Opioid-related overdose | PEH/Non-homeless | NA | 4 | OR: 2.10 (1.43–3.10) | Increased chances for PEH | 1.5×10−4 | 59.8% (0.032) | 0.45–9.75 | No/NP | Yes | III | Critically low |
| Bassuk et al., 2015 [222] | Mental Health problems, assessed by the Child Behavior Checklist | Homeless schoolchildren/non-homeless school children | NA | 3 | OR: 1.77 (1.13–2.76) | Increased chances for Homeless school children | 0.012 | 17.9% (0.518) | 0.05–64.4 | No/NP | Yes | IV | Critically low |
| Lin et al., 2019 [220] | Adherence to antiretroviral therapy | PEH/General population | NA | 4 | OR: 0.5 (0.32–0.77) | Better adherence in the general population | 0.002 | 72.4% (0.064) | 0.08–3.16 | No/No | Yes | IV | Critically low |
| Suh et al., 2020 [217] | Frailty | PEH/Non-homeless | NA | 3 | RR: 2.59 (1.05–6.39) | Increased chances for PEH | 0.0388 | 97.8% (0.0001) | 0.001–2.8×105 | Yes/NA | Yes | IV | Critically low |
| Tweed et al., 2021 [215] | Mortality due to external causes, as defined in ICD-10 | PEH with SUD/PEH without SUD | NA | 4 | HR: 2.3 (1.26–4.2) | Increased chances for PEH with SUD | 0.0069 | 78.5% (0.093) | 0.17–31.02 | No/NA | Yes | IV | Critically low |
| Aidala et al., 2016 [223] | Mortality due to any cause | PEH with HIV/Non-homeless with HIV | 32.8% | 7 | HR: 1.43 (0.74–2.77) | Increased chances for PEH with HIV | 0.286 | 90.5% (0.001) | 0.15–13.69 | No/No | Yes | NS | Critically low |
| Aidala et al., 2016 [223] | Viral load non-suppression | PEH with HIV/Non-homeless with HIV | 5.6% | 3 | OR: 1.23 (0.89–1.71) | Increased chances for PEH with HIV | 0.215 | 70% (0.083) | 0.03–51.48 | No/No | No | NS | Critically low |
| Bassuk et al., 2015 [222] | Mental Health problems, assessed by the Child Behavior Checklist | Homeless pre-school children/non-homeless pre-school children | 4.6% | 3 | OR: 1.47 (0.93–2.35) | Increased chances for Homeless pre-school children | 0.101 | 13.9% (0.544) | 0.04–53.39 | No/NP | Yes | NS | Critically low |
| Bassuk et al., 2015 [222] | Mental Health problems, assessed by the Child Depression Inventory | Homeless school children/non-homeless school children | NA | 3 | OR: 1.45 (0.77–2.73) | Increased chances for Homeless school children | 0.248 | 31.6% (0.35) | 0.01–453.76 | No/NP | No | NS | Critically low |
| Tweed et al., 2021 [215] | Mortality due to any cause | PEH with SUD/PEH without SUD | 45.5% | 5 | HR: 1.6 (0.99–2.57) | Increased chances for PEH with SUD | 0.0536 | 96.1% (1×10−4) | 0.26–9.61 | No/No | Yes | NS | Critically low |
| Tweed et al., 2021 [215] | Mortality due to any cause | PEH with SMI/PEH without SMI | 8.4% | 3 | HR: 0.89 (0.69–1.15) | Increased chances for PEH without SMI | 0.382 | 19.9% (0.473) | 0.1–7.64 | No/NP | No | NS | Critically low |
| Tweed et al., 2021 [215] | Mortality due to external causes, as defined by ICD-10 | PEH with SMI/Homeless without SMI | NA | 3 | HR: 3.13 (0.78–12.51) | Increased chances for PEH with SMI | 0.106 | 93.4% (0.003) | 0.001–9.6×107 | No/NA | Yes | NS | Critically low |
CE credibility evidence, CI confidence interval, ES effect size, ESB excess significance bias, HR hazard ratio, ICD-10 International Classification of Diseases, 10th revision, LS largest study with significant effect, MA meta-analysis, NA not applicable, NP not pertinent because of fewer than expected number of observed studies, NS not significant, OR odds ratio, PEH people experiencing homelessness, PI prediction interval, RR risk ratio, SMI severe mental illness, SMR standardized mortality ratio, SR systematic review, SSE small study effect, SUD substance use disorder
Intervention studies
One eligible MA of intervention studies documented two therapeutic interventions, evaluated by 10 unique RCTs from 10 original reports, estimating interventions associated with mental health status among PEH [220]. One association concerned the psychological interventions among PEH diagnosed with depression, while the remaining one dealt with psychological interventions for anxiety. None of the assessed associations reached a statistically significant value at p≤0.005 based on the random-effects model [30]. The degree of heterogeneity of the documented associations was quantified in I2=42.5% for depression and 39.9% for anxiety. The 95% prediction intervals crossed the null for the outcomes of both interventions. Neither of the largest studies of the two associations was statistically significant at p≤0.05. Please refer to Table 3 for details.
Table 3.
Evidence from SRs or MAs of intervention studies for the association between different interventions for PEH and any health outcome
| Author, year | Considered health outcome | Active treatment/control treatment | Number of patients allocated to each treatment | No. of included studies per association | Random-effects measure, ES (95% CIs) |
Results | p value random effects | I2 (p value) | PIs (95 % CIs) | LS | AMSTAR-plus |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hyun et al., 2020 [224] | Depression | Psychological interventions/treatment as usual | 236/224 | 5 | SMD: − 0.24 (− 0.49–0.02) | Psychological interventions are more effectiver than treatment as usual | 0.07 | 42.6% (0.2) | − 0.964–0.491 | No | 10 |
| Hyun et al., 2020 [224] | Anxiety | Psychological interventions/treatment as usual | 229/215 | 5 | SMD: − 0.25 (− 0.51–0) | Psychological interventions are moe effective than treatment as usual | 0.05 | 39.9% (0.28) | − 0.967–0.459 | No | 10 |
CI confidence interval, ES effect size, LS largest study with significant effect, MA meta-analysis, PI prediction interval, RR risk ratio, SMD standardized mean difference, SR systematic review
Grading of systematic reviews and meta-analyses of observational studies
Concerning the SRs and/or MAs of observational studies, none of them concurrently reached a “convincing evidence” threshold, according to the adapted credibility box, and a “high quality” score based on the AMSTAR-2 tool. According to the latter, every SR and/or MA included in the present study was rated as having “critically low” methodological quality. Please refer to Additional file 1: Table S3 [211–219].
Convincing evidence
Among the 23 associations, two (8.7%) were supported by “convincing evidence”: hospitalization due to any cause among PEH diagnosed with HIV infection and the occurrence of falls within the past year among PEH. Both health outcomes were more common among PEH compared to non-homeless controls.
Highly suggestive evidence
Five (21.7%) associations were rated “highly suggestive evidence”: (1) mortality due to any cause; (2) mortality due to external causes (i.e., intentional injury, unintentional injury, poisoning) among PEH compared to the general population; (3) HCV-infection among PEH using injection drugs compared to those who did not; (4) the presence of limitations in activities of daily living (ADL, e.g., dressing, eating, toileting); and (5) instrumental activities of daily living (IADL, e.g., using telephone, using transportations, taking medications) among PEH compared to non-homeless controls. These above-mentioned health outcomes were more common among PEH compared to their respective controls. Mortality due to any cause and mortality due to external causes had high standardized mortality ratios=6.22 (95% C.I.=4.2–9.2), and SMR=15.75 (95% C.I.=10.58–23.44), respectively.
Suggestive, weak, and no evidence
Five (21.7%) associations were rated “suggestive evidence,” four (17.4%) were “weak evidence,” while “no significant evidence” was found in seven (30.5%) associations.
Grading of systematic reviews and meta-analyses of intervention studies
Concerning intervention studies, the sole MA retrieved obtained a score of “10” at the AMSTAR-plus. Please refer to Table 3 for details.
Sensitivity analysis
A sensitivity analysis limited to high-quality prospective cohort studies included eleven (47.8%) associations, rated according to the NOS. Upon sensitivity analysis, two associations worsen, and one association improved in terms of credibility evidence. Hospitalization due to any cause among PEH with HIV infection shifted from “convincing evidence” to “highly suggestive evidence”, non-adherence to antiretroviral therapy (ART) among PEH with HIV infection shifted from “suggestive evidence” to “weak evidence”, and mortality due to any cause among PEH with SUD up-graded from “no significant evidence” to “highly suggestive evidence”. Please refer to Additional file 1: Table S4 [211, 214, 217, 219].
Discussion
Statement of principal findings
We found convincing evidence that all-cause hospitalization in people with HIV infection and the occurrence of falls within the past year were more common among PEH compared to comparison populations. We also found highly suggestive evidence that mortality due to any cause; mortality due to external causes; hepatitis C infection among PEH using injection drugs; limitations in activities of daily living; and limitations in instrumental activities of daily living were significantly more common in PEH compared to their comparison populations. Mortality due to any cause and mortality due to external causes had high standardized mortality ratios such that PEH had a mortality rate six times their comparison groups and they were about 15 times more likely to die from either accidents or intentional self-harm.
Strengths and limitations
To our knowledge, this study is the first umbrella review that systematically inquired about any health-related outcomes and interventions among PEH, grading the evidence by using previously adopted and widely accepted criteria of credibility [14, 16, 29, 31, 221]. All SRs/or MAs of observational studies were graded as having “critically low” methodological quality according to the AMSTAR-2 instrument. Among the associations rated with “highly suggestive evidence”, two were not deemed as “convincing” due to high heterogeneity. Overall, 65.2% of the associations covered by the present umbrella review were hampered by high heterogeneity, which held upon controlling for high-quality prospective studies (seven out of eleven associations—63.6%—had an I2>50%).
The differences in definitions of “homelessness” and thus categories of homelessness (for example individuals without permanent housing who may live on the streets; stay in a shelter, mission, single room occupancy facilities, abandoned building or vehicle; or in any other unstable or non-permanent situation) adopted by the authors of the included SRs or MAs could likewise account for the high rates of heterogeneity. Half of the appraised studies lacked a “homelessness” definition, and the remaining half provided a broad definition, as detailed in Table 1. The timeframe for the homelessness definition, or its related labels, varied across the individual studies included by the appraised SRs or MAs, often merging people who were currently homeless with people who were experiencing this condition within varying timeframes (i.e., 30-day, 6-month, or 12-month intervals, as usually documented by the authors of the original studies). Future research should, therefore, rely on consistent operational definitions, or otherwise stratify their results accordingly, especially considering that substantial variability of the adopted definitions exists across different world regions [222].
The limitations of this review include the exclusion of RCTs on the impact of housing interventions (Housing First) on PEH. However, such interventions were not deemed eligible for inclusion according to our a priori criteria since we focused on those interventions directly targeting health outcomes in PEH rather than on interventions aimed at reducing the burden of homelessness. Sensitivity analyses were restricted to high-quality prospective studies. Because of the lack of relevant SRs or MAs, we could not appraise otherwise relevant associations between homelessness and health outcomes such as alcohol-related issues, cancer, or infectious diseases other than HIV or HCV. Mental illness-related issues were only accounted for by three comparisons focusing on children experiencing homelessness [223].
Comparison with previous studies
Considering the two associations reaching “convincing evidence” before sensitivity analysis, the documented hospitalization trend due to any cause in people with HIV is consistent with a recent retrospective cohort study [224]. A significant increase in “falls during the previous year” may be the result of high rates of concurrent geriatric syndromes, alcohol use disorders, and drug abuse as described elsewhere [225].
Hence, upstream (e.g., poverty, poor nutrition, barriers to healthcare, and HIV treatment) and downstream factors (i.e., comorbidities and multimorbidity) significantly affect PEH [5], jeopardize their healthcare, and inflate their hospitalization rates compared to the general population [222].
Although we were unable to include any SR and MA reporting on the relationship between the COVID-19 pandemic and homelessness, PEH could be at higher risk also at developing hospitalization or fatalities due to COVID-19 according to recent evidence [226] although this finding deserves replication, providing evidence for the need of well-designed interventions targeting this vulnerable population.
Conclusions and implications for further research
This review adds weight to arguments about why reducing homelessness should be a priority beyond human rights justification. The evidence that experiencing homelessness leads to worse health outcomes is only a secondary consideration for providing affordable housing albeit an important one. Housing reduces hospitalization rates according to RCTs involving PEH with chronic illnesses [227, 228]. This study demonstrates that a readily treatable illness such as HIV is not adequately managed in PEH resulting in significant downstream healthcare costs in addition to preventable patient suffering. A recent SR identified that housing PEH (in the short term) improves some aspects of health in this population with HIV, anxiety, and depression [229].
However, focusing just on providing housing for this population does not mean that an individual’s health needs are automatically solved. We know from Housing First studies that just providing housing does not result in improvements in mental health or addictions after a year, especially in people who have experienced significant trauma [55]. This umbrella review suggests that the health effects of homelessness are serious, longstanding, and involve all parts of the health system. Finally, while psychological interventions are expected to be more effective than TAU in reducing the burden of the associated health condition among clinical and non-clinical populations [230], the herein reviewed MA focusing on PEH on the matter [220] failed to reach a statistically significant threshold according to our conservative p value set at p=.005, though it could not be excluded the condition of homelessness itself could attenuate the effects of such psychological interventions.
What is needed now are studies that look at better coordination of care for this population that may involve hospitals and community partners as well as programs to address health issues in people recently housed after experiencing homelessness. In addition, it should be reiterated that there is an urgent need for international standardization of housing status to improve research rigor that could improve the external generalizability of this field and hence direct policy. Furthermore, more studies should be conducted in low- and middle-income countries as the vast majority of studies to date on this topic have been performed in developed nations. Such bias related to the geographical region may depend on a variety of issues, including, but not necessarily limited to, public health policies as well as the limited funding in LMICs. Lastly, more SRs and MAs with enhanced methodological quality are an unmet need in this field.
Supplementary Information
Additional file 1: Material 1. adopted search strings. Table S1. criteria for the evaluation of the credibility of the evidence of observational studies. Please note that criterion n.1 (sample size of cases) was purposely waived as outlined in the main-text, methods section. Table S2. List of the 179 excluded records, with the reason(s). Note: duplicate records may appear multiple times for consistency issues. Table S3. Included SRs or MAs of observational studies; quality rating according to the AMSTAR-2. Table S4. Sensitivity analysis of evidence from SRs or MAs of observational studies for the association between homelessness and any health outcome.
Acknowledgments
None.
Abbreviations
- ADL
Activities of daily living
- AMSTAR-2
Assessment of Multiple Systematic Reviews 2
- AMSTAR-plus
Assessment of Multiple Systematic Reviews Plus
- ART
Antiretroviral therapy
- CI
Confidence interval
- COVID-19
Coronavirus disease 2019
- ES
Effect size
- HCV
Hepatitis C virus
- HIV
Human immunodeficiency virus
- IADL
Instrumental activities of daily living
- LMICs
Low- and middle-income countries
- MA
Meta-analysis
- NOS
Newcastle-Ottawa Scale
- PEH
People experiencing homelessness
- RCT
Randomized controlled trial
- SMR
Standardized mortality ratio
- SR
Systematic review
- SUD
Substance use disorder
Authors’ contributions
MF and AFC conceived the study together with MS. MS and AFC provided input over the study process. MDP, MB, and AM extracted the data, assisting in manuscript drafting under MF guidance. ED performed the analyses. AdB, LS, RC, SH, JGF, ED, and MK provided expert input over the review process and final drafting. The authors read and approved the final manuscript.
Funding
Open access funding provided by Linköping University. This study received no funding.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and are available online at https://osf.io/am67d/ and https://osf.io/58mhu/.
The additional file includes the following: material 1 – [search strings]; table S1 - [criteria for the evaluation of the credibility of the evidence of observational studies]; table S2 – [excluded studies with reasons]; table S3 – [quality rating of the included SRs or MAs of observational studies, according to the AMSTAR-2]; table S4 – [sensitivity analysis].
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Michele Fornaro, Email: dott.fornaro@gmail.com.
Elena Dragioti, Email: elena.dragioti@liu.se.
Michele De Prisco, Email: deprisco.michele@gmail.com.
Martina Billeci, Email: martina.bi@hotmail.it.
Anna Maria Mondin, Email: annamondin90@gmail.com.
Raffaella Calati, Email: raffaella.calati@unimib.it.
Lee Smith, Email: Lee.Smith@aru.ac.uk.
Simon Hatcher, Email: shatcher@toh.ca.
Mark Kaluzienski, Email: mkaluzienski@toh.ca.
Jess G. Fiedorowicz, Email: jess-fiedorowicz@uiowa.edu
Marco Solmi, Email: marco.solmi83@gmail.com.
Andrea de Bartolomeis, Email: adebarto@unina.it.
André F. Carvalho, Email: andrefc7@hotmail.com
References
- 1.Tsai J. Lifetime and 1-year prevalence of homelessness in the US population: results from the National Epidemiologic Survey on Alcohol and Related Conditions-III. J Public Health. 2018;40(1):65–74. doi: 10.1093/pubmed/fdx034. [DOI] [PubMed] [Google Scholar]
- 2.Taylor O, Loubiere S, Tinland A, Vargas-Moniz M, Spinnewijn F, Manning R, Gaboardi M, Wolf JR, Bokszczanin A, Bernad R. Lifetime, 5-year and past-year prevalence of homelessness in Europe: a cross-national survey in eight European nations. BMJ Open. 2019;9(11):e033237. doi: 10.1136/bmjopen-2019-033237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bensken WP. How do we define homelessness in large health care data? Identifying variation in composition and comorbidities. Health Serv Outcomes Res Methodol. 2021;21(1):145–166. doi: 10.1007/s10742-020-00225-5. [DOI] [Google Scholar]
- 4.EUROPEAN TYPOLOGY OF HOMELESSNESS AND HOUSING EXCLUSION (ETHOS) [https://www.feantsa.org/download/ethos2484215748748239888.pdf]
- 5.Liu M, Hwang SW. Health care for homeless people. Nat Rev Dis Prim. 2021;7(1):1–2. doi: 10.1038/s41572-020-00234-1. [DOI] [PubMed] [Google Scholar]
- 6.Gilmer C, Buccieri K. Homeless patients associate clinician bias with suboptimal care for mental illness, addictions, and chronic pain. J Prim Care Commun Health. 2020;11:2150132720910289. doi: 10.1177/2150132720910289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fazel S, Khosla V, Doll H, Geddes J. The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Med. 2008;5(12):e225. doi: 10.1371/journal.pmed.0050225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beijer U, Wolf A, Fazel S. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(11):859–870. doi: 10.1016/S1473-3099(12)70177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ioannidis JP. Why most published research findings are false. PLoS Med. 2005;2(8):e124. doi: 10.1371/journal.pmed.0020124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ojo-Fati O, Joseph AM, Ig-Izevbekhai J, Thomas JL, Everson-Rose SA, Pratt R, Raymond N, Cooney NL, Luo X, Okuyemi KS. Practical issues regarding implementing a randomized clinical trial in a homeless population: strategies and lessons learned. Trials. 2017;18(1):1–10. doi: 10.1186/s13063-017-2046-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ioannidis JP, Munafo MR, Fusar-Poli P, Nosek BA, David SP. Publication and other reporting biases in cognitive sciences: detection, prevalence, and prevention. Trends Cognit Sci. 2014;18(5):235–241. doi: 10.1016/j.tics.2014.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ioannidis JP. Why most discovered true associations are inflated. Epidemiology. 2008;19(5):640–8. 10.1097/EDE.0b013e31818131e7. [DOI] [PubMed]
- 13.Ioannidis JP. Integration of evidence from multiple meta-analyses: a primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. Cmaj. 2009;181(8):488–493. doi: 10.1503/cmaj.081086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dragioti E, Evangelou E, Larsson B, Gerdle B. Effectiveness of multidisciplinary programmes for clinical pain conditions: An umbrella review. J Rehabil Med. 2018;50(9):779–791. doi: 10.2340/16501977-2377. [DOI] [PubMed] [Google Scholar]
- 15.Tsilidis KK, Kasimis JC, Lopez DS, Ntzani EE, Ioannidis JP. Type 2 diabetes and cancer: umbrella review of meta-analyses of observational studies. BMJ. 2015;350:g7607. [DOI] [PubMed]
- 16.Theodoratou E, Tzoulaki I, Zgaga L, Ioannidis JP. Vitamin D and multiple health outcomes: umbrella review of systematic reviews and meta-analyses of observational studies and randomised trials. BMJ. 2014;348:g2035. 10.1136/bmj.g2035. [DOI] [PMC free article] [PubMed]
- 17.DerSimonian R, Laird N. Meta-analysis in clinical trials. Contr Clin Trials. 1986;7(3):177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 18.IntHout J, Ioannidis JP, Borm GF. The Hartung-Knapp-Sidik-Jonkman method for random effects meta-analysis is straightforward and considerably outperforms the standard DerSimonian-Laird method. BMC Med Res Methodol. 2014;14(1):1–12. doi: 10.1186/1471-2288-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cochran WG. The combination of estimates from different experiments. Biometrics. 1954;10(1):101–129. doi: 10.2307/3001666. [DOI] [Google Scholar]
- 20.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011;342:d549. 10.1136/bmj.d549. [DOI] [PubMed]
- 22.Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002. 10.1136/bmj.d4002. [DOI] [PubMed]
- 23.Ioannidis JP, Trikalinos TA. An exploratory test for an excess of significant findings. Clin Trials. 2007;4(3):245–253. doi: 10.1177/1740774507079441. [DOI] [PubMed] [Google Scholar]
- 24.Tsilidis KK, Papatheodorou SI, Evangelou E, Ioannidis JP. Evaluation of excess statistical significance in meta-analyses of 98 biomarker associations with cancer risk. J Natl Cancer Inst. 2012;104(24):1867–1878. doi: 10.1093/jnci/djs437. [DOI] [PubMed] [Google Scholar]
- 25.Tsilidis KK, Panagiotou OA, Sena ES, Aretouli E, Evangelou E, Howells DW. Salman RA-S, Macleod MR, Ioannidis JP: Evaluation of excess significance bias in animal studies of neurological diseases. PLoS Biol. 2013;11(7):e1001609. doi: 10.1371/journal.pbio.1001609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dragioti E, Karathanos V, Gerdle B, Evangelou E. Does psychotherapy work? An umbrella review of meta-analyses of randomized controlled trials. Acta Psychiatrica Scandinavica. 2017;136(3):236–246. doi: 10.1111/acps.12713. [DOI] [PubMed] [Google Scholar]
- 27.Ioannidis JP. Clarifications on the application and interpretation of the test for excess significance and its extensions. J Math Psychol. 2013;57(5):184–187. doi: 10.1016/j.jmp.2013.03.002. [DOI] [Google Scholar]
- 28.Bellou V, Belbasis L, Tzoulaki I, Evangelou E, Ioannidis JP. Environmental risk factors and Parkinson's disease: an umbrella review of meta-analyses. Parkinson Relat Disord. 2016;23:1–9. doi: 10.1016/j.parkreldis.2015.12.008. [DOI] [PubMed] [Google Scholar]
- 29.Bortolato B, Köhler CA, Evangelou E, León-Caballero J, Solmi M, Stubbs B, Belbasis L, Pacchiarotti I, Kessing LV, Berk M. Systematic assessment of environmental risk factors for bipolar disorder: an umbrella review of systematic reviews and meta-analyses. Bipolar Disord. 2017;19(2):84–96. doi: 10.1111/bdi.12490. [DOI] [PubMed] [Google Scholar]
- 30.Koletsi D, Solmi M, Pandis N, Fleming PS, Correll CU, Ioannidis JP. Most recommended medical interventions reach P< 0.005 for their primary outcomes in meta-analyses. Int J Epidemiol. 2020;49(3):885–893. doi: 10.1093/ije/dyz241. [DOI] [PubMed] [Google Scholar]
- 31.Li X, Meng X, Timofeeva M, Tzoulaki I, Tsilidis KK, Ioannidis JP, Campbell H, Theodoratou E. Serum uric acid levels and multiple health outcomes: umbrella review of evidence from observational studies, randomised controlled trials, and Mendelian randomisation studies. Bmj. 2017;357:j2376. doi: 10.1136/bmj.j2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Correll CU, Rubio JM, Inczedy-Farkas G, Birnbaum ML, Kane JM, Leucht S. Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiatr. 2017;74(7):675–684. doi: 10.1001/jamapsychiatry.2017.0624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, Moher D, Tugwell P, Welch V, Kristjansson E. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. Bmj. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Oxford: 2000.
- 35.Sharmin S, Kypri K, Khanam M, Wadolowski M, Bruno R, Mattick RP. Parental supply of alcohol in childhood and risky drinking in adolescence: systematic review and meta-analysis. Int J Environ Res Public Health. 2017;14(3):287. doi: 10.3390/ijerph14030287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ontario HQ. Interventions to Improve Access to Primary Care for People Who Are Homeless: A Systematic Review. Ont Health Technol Assess Ser. 2016;16(9):1–50. [PMC free article] [PubMed] [Google Scholar]
- 37.Abad N, Baack B, O'Leary A, Lyles C. A review of HIV/STD behavioral prevention interventions for female sex workers in the United States. Sexual Transmit Dis. 2014;41:S114. doi: 10.1097/OLQ.0000000000000078. [DOI] [Google Scholar]
- 38.Adams-Guppy JR, Guppy A. A systematic review of interventions for homeless alcohol-abusing adults. Drugs. 2016;23(1):15–30. [Google Scholar]
- 39.Alividza V, Mariano V, Ahmad R, Charani E, Rawson TM, Holmes AH, Castro-Sánchez E. Investigating the impact of poverty on colonization and infection with drug-resistant organisms in humans: a systematic review. Infect Dis Poverty. 2018;7(1):76. doi: 10.1186/s40249-018-0459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Altena AM, Brilleslijper-Kater SN, Wolf JL. Effective interventions for homeless youth: a systematic review. Am J Prev Med. 2010;38(6):637–645. doi: 10.1016/j.amepre.2010.02.017. [DOI] [PubMed] [Google Scholar]
- 41.Altena AM, Brilleslijper-Kater SN, Wolf JLM. Effective Interventions for Homeless Youth. A Systematic Review. Am J Prevent Med. 2010;38(6):637–645. doi: 10.1016/j.amepre.2010.02.017. [DOI] [PubMed] [Google Scholar]
- 42.Andrade FMR, Figueiredo AS, Capelas ML, Charepe Z, Deodato S. Experiences of homeless families in parenthood: a systematic review and synthesis of qualitative evidence. Int J Environ Res Public Health. 2020;17(8):2712. 10.3390/ijerph17082712. [DOI] [PMC free article] [PubMed]
- 43.Aubry T, Bloch G, Brcic V, Saad A, Magwood O, Abdalla T, Alkhateeb Q, Xie E, Mathew C, Hannigan T, et al. Effectiveness of permanent supportive housing and income assistance interventions for homeless individuals in high-income countries: a systematic review. Lancet Public Health. 2020;5(6):e342–e360. doi: 10.1016/S2468-2667(20)30055-4. [DOI] [PubMed] [Google Scholar]
- 44.Auerswald C, Woan J, Lin J. The health status of street children in low-and middle-income countries: A systematic review. Turk Pediatri Arsivi. 2013;48:75. doi: 10.1016/j.jadohealth.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 45.Ayano G, Shumet S, Tesfaw G, et al. A systematic review and meta-analysis of the prevalence of bipolar disorder among homeless people. BMC Public Health. 2020;20:731. 10.1186/s12889-020-08819-x. [DOI] [PMC free article] [PubMed]
- 46.Ayano G, Belete A, Duko B, Tsegay L, Dachew BA. Systematic review and meta-analysis of the prevalence of depressive symptoms, dysthymia and major depressive disorders among homeless people. BMJ Open. 2021;11(2):e040061. doi: 10.1136/bmjopen-2020-040061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ayano G, Shumet S, Tesfaw G, Tsegay L. A systematic review and meta-analysis of the prevalence of bipolar disorder among homeless people. BMC Public Health. 2020;20(1):731. doi: 10.1186/s12889-020-08819-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ayano G, Solomon M, Tsegay L, Yohannes K, Abraha M. A Systematic Review and Meta-Analysis of the Prevalence of Post-Traumatic Stress Disorder among Homeless People. Psychiatr Q. 2020;91(4):949–963. doi: 10.1007/s11126-020-09746-1. [DOI] [PubMed] [Google Scholar]
- 49.Ayano G, Tesfaw G, Shumet S. The prevalence of schizophrenia and other psychotic disorders among homeless people: a systematic review and meta-analysis. BMC Psychiatry. 2019;19(1):370. doi: 10.1186/s12888-019-2361-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ayano G, Tsegay L, Abraha M, Yohannes K. Suicidal Ideation and Attempt among Homeless People: a Systematic Review and Meta-Analysis. Psychiatr Q. 2019;90(4):829–842. doi: 10.1007/s11126-019-09667-8. [DOI] [PubMed] [Google Scholar]
- 51.Bahji A, Bajaj N. Opioids on trial: a systematic review of interventions for the treatment and prevention of opioid overdose. Can J Addict. 2018;9(1):26–33. doi: 10.1097/CXA.0000000000000013. [DOI] [Google Scholar]
- 52.Banks S, McHugo GJ, Williams V, Drake RE, Shinn M. A prospective meta-analytic approach in a multisite study of homelessness prevention. New Direct Eval. 2002;2002(94):45–60. doi: 10.1002/ev.50. [DOI] [Google Scholar]
- 53.Barajas-Nava L. Oral substitution treatment of injecting opioid users for prevention of HIV infection. J Assoc Nurs AIDS Care. 2017;28(5):832–833. doi: 10.1016/j.jana.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 54.Batra K, Pharr J, Olawepo JO, Cruz P. Understanding the multidimensional trajectory of psychosocial maternal risk factors causing preterm birth: A systematic review. Asian J Psychiatr. 2020;54:102436. doi: 10.1016/j.ajp.2020.102436. [DOI] [PubMed] [Google Scholar]
- 55.Baxter AJ, Tweed EJ, Katikireddi SV, Thomson H. Effects of Housing First approaches on health and well-being of adults who are homeless or at risk of homelessness: systematic review and meta-analysis of randomised controlled trials. J Epidemiol Community Health. 2019;73(5):379–387. doi: 10.1136/jech-2018-210981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bazzi AR, Drainoni ML, Biancarelli DL, Hartman JJ, Mimiaga MJ, Mayer KH, Biello KB. Systematic review of HIV treatment adherence research among people who inject drugs in the United States and Canada: evidence to inform pre-exposure prophylaxis (PrEP) adherence interventions. BMC Public Health. 2019;19(1):31. doi: 10.1186/s12889-018-6314-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bazzi AR, Drainoni ML, Biancarelli DL, Hartman JJ, Mimiaga MJ, Mayer KH, Biello KB. Systematic review of HIV treatment adherence research among people who inject drugs in the United States and Canada: Evidence to inform pre-exposure prophylaxis (PrEP) adherence interventions 11 Medical and Health Sciences 1117 Public Health and Health Services. BMC Public Health. 2019;19(1):1. doi: 10.1186/s12889-018-6314-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Behzadifar M, Gorji HA, Rezapour A, Bragazzi NL. Prevalence of hepatitis C virus among street children in Iran. Infect Dis Poverty. 2018;7(1):88. doi: 10.1186/s40249-018-0469-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Benston EA. Housing Programs for Homeless Individuals With Mental Illness: Effects on Housing and Mental Health Outcomes. Psychiatr Serv. 2015;66(8):806–816. doi: 10.1176/appi.ps.201400294. [DOI] [PubMed] [Google Scholar]
- 60.Bernstein RS, Meurer LN, Plumb EJ, Jackson JL. Diabetes and hypertension prevalence in homeless adults in the United States: a systematic review and meta-analysis. Am J Public Health. 2015;105(2):e46–e60. doi: 10.2105/AJPH.2014.302330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Blanquet M, Legrand A, Pélissier A, Mourgues C. Socio-economics status and metabolic syndrome: A meta-analysis. Diab Metab Syndr. 2019;13(3):1805–1812. doi: 10.1016/j.dsx.2019.04.003. [DOI] [PubMed] [Google Scholar]
- 62.Bonner A, Luscombe C. Suicide and homelessness. J Public Mental Health. 2009;8(3):7–19. doi: 10.1108/17465729200900016. [DOI] [Google Scholar]
- 63.Borkhoff CM, Wieland ML, Myasoedova E, Ahmad Z, Welch V, Hawker GA, Li LC, Buchbinder R, Ueffing E, Beaton D, et al. Reaching those most in need: a scoping review of interventions to improve health care quality for disadvantaged populations with osteoarthritis. Arthritis Care Res (Hoboken) 2011;63(1):39–52. doi: 10.1002/acr.20349. [DOI] [PubMed] [Google Scholar]
- 64.Brownfield NR, Thielking M, Bates G, Morrison F. Does poverty impact student academic outcomes and wellbeing in australian universities? A systematic review. J Soc Inclusion. 2020;11(2):4–19. [Google Scholar]
- 65.Bryant J, Bonevski B, Paul C, McElduff P, Attia J. A systematic review and meta-analysis of the effectiveness of behavioural smoking cessation interventions in selected disadvantaged groups. Addiction. 2011;106(9):1568–1585. doi: 10.1111/j.1360-0443.2011.03467.x. [DOI] [PubMed] [Google Scholar]
- 66.Burra TA, Stergiopoulos V, Rourke SB. A systematic review of cognitive deficits in homeless adults: implications for service delivery. Can J Psychiatr. 2009;54(2):123–133. doi: 10.1177/070674370905400210. [DOI] [PubMed] [Google Scholar]
- 67.Byrne T, Montgomery AE, Dichter ME. Homelessness among female veterans: a systematic review of the literature. Women Health. 2013;53(6):572–596. doi: 10.1080/03630242.2013.817504. [DOI] [PubMed] [Google Scholar]
- 68.Campos-Matos I, Russo G, Perelman J. Connecting the dots on health inequalities - A systematic review on the social determinants of health in Portugal. Int J Equity Health. 2016;15(1):26. doi: 10.1186/s12939-016-0314-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Carver H, Ring N, Miler J, Parkes T. What constitutes effective problematic substance use treatment from the perspective of people who are homeless? A systematic review and meta-ethnography. Harm Reduct J. 2020;17(1):10. doi: 10.1186/s12954-020-0356-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cassone A. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Pathog Glob Health. 2012;106(7):377. doi: 10.1179/2047772412Z.00000000086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Chandler CE, Austin AE, Shanahan ME. Association of Housing Stress With Child Maltreatment: A Systematic Review. Trauma Violence Abuse. 2020;23:639–659. doi: 10.1177/1524838020939136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chant C, Smith O, Wang A, Burns K, Dos Santos CC, Friedrich JO, Hwang S. Critical illness in homeless persons: A systematic review of the literature. Intens Care Med. 2013;39:S512. doi: 10.1007/s00134-013-3124-4. [DOI] [PubMed] [Google Scholar]
- 73.Chant C, Smith O, Wang A, Hwang S, Friedrich JO, Burns KEA, et al. Homelessness and critical care: a systematic review of the literature. Intensive Care Med. 2014;40(1):123–5. 10.1007/s00134-013-3124-4. [DOI] [PubMed]
- 74.Chant C, Wang A, Burns KE, dos Santos CC, Hwang SW, Friedrich JO, Smith OM. Critical illness in homeless persons is poorly studied: a systematic review of the literature. Intensive Care Med. 2014;40(1):123–125. doi: 10.1007/s00134-013-3124-4. [DOI] [PubMed] [Google Scholar]
- 75.Charron CB, Hayes T, Pakhale S. A systematic review of interventions for smoking tobacco in low socio-economic populations. Am J Respir Crit Care Med. 2018;197. https://www.atsjournals.org/doi/abs/10.1164/ajrccm-conference.2018.197.1_MeetingAbstracts.A6253.
- 76.Clark NC, Lintzeris N, Gijsbers A, Whelan G, Dunlop A, Ritter A, Ling WW. LAAM maintenance vs methadone maintenance for heroin dependence. Cochrane Database Syst Rev. 2002;2:CD002210. doi: 10.1002/14651858.CD002210. [DOI] [PubMed] [Google Scholar]
- 77.Coldwell CM, Bender WS. The effectiveness of assertive community treatment for homeless populations with severe mental illness: a meta-analysis. Am J Psychiatry. 2007;164(3):393–399. doi: 10.1176/ajp.2007.164.3.393. [DOI] [PubMed] [Google Scholar]
- 78.Conn VS, Ruppar TM. Medication adherence outcomes of 771 intervention trials: Systematic review and meta-analysis. Prev Med. 2017;99:269–276. doi: 10.1016/j.ypmed.2017.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Constance J, Lusher JM. Diabetes management interventions for homeless adults: a systematic review. Int J Public Health. 2020;65(9):1773–1783. doi: 10.1007/s00038-020-01513-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Coren E, Hossain R, Pardo JP, Veras MM, Chakraborty K, Harris H, Martin AJ. Interventions for promoting reintegration and reducing harmful behaviour and lifestyles in street-connected children and young people. Evid Based Child Health. 2013;8(4):1140–1272. doi: 10.1002/ebch.1923. [DOI] [PubMed] [Google Scholar]
- 81.Costa F, Hagan JE, Calcagno J, Kane M, Torgerson P, Martinez-Silveira MS, Stein C, Abela-Ridder B, Ko AI. Global Morbidity and Mortality of Leptospirosis: A Systematic Review. PLoS Negl Trop Dis. 2015;9(9):e0003898. doi: 10.1371/journal.pntd.0003898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Coufopoulos A, McDowell G, Roe B, Maden M. Interventions to improve nutrition and nutrition related health amongst homeless mothers and their children: a systematic review. Proceed Nutr Soc. 2012;71(OCE2):E161. 10.1017/S0029665112002182.
- 83.Cumber SN, Tsoka-Gwegweni JM. The Health Profile of Street Children in Africa: A Literature Review. J Public Health Afr. 2015;6(2):566. doi: 10.4081/jphia.2015.566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Curtis J. Impact of x-ray screening programmes for active tuberculosis in homeless populations: a systematic review of original studies. J Public Health (Oxf) 2016;38(1):106–114. doi: 10.1093/pubmed/fdv014. [DOI] [PubMed] [Google Scholar]
- 85.da Silva TFC, Lovisi GM, Verdolin LD, Cavalcanti MT. Adherence to drug treatment among schizophrenic spectrum patients: A systematic review of the literature. Jornal Brasileiro de Psiquiatria. 2012;61(4):242–251. doi: 10.1590/S0047-20852012000400008. [DOI] [Google Scholar]
- 86.Dalton-Locke C, Marston L, McPherson P, Killaspy H. The Effectiveness of Mental Health Rehabilitation Services: A Systematic Review and Narrative Synthesis. Front Psychiatry. 2020;11:607933. doi: 10.3389/fpsyt.2020.607933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.de Vet R, van Luijtelaar MJ, Brilleslijper-Kater SN, Vanderplasschen W, Beijersbergen MD, Wolf JR. Effectiveness of case management for homeless persons: a systematic review. Am J Public Health. 2013;103(10):e13–e26. doi: 10.2105/AJPH.2013.301491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.De Vet R, Van Luijtelaar MJA, Brilleslijper-Kater SN, Vanderplasschen W, Beijersbergen MD, Wolf JRLM. Effectiveness of case management for homeless persons: A systematic review. Am J Public Health. 2013;103(10):e13–e26. doi: 10.2105/AJPH.2013.301491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Degenhardt L, Peacock A, Colledge S, Leung J, Grebely J, Vickerman P, Stone J, Cunningham EB, Trickey A, Dumchev K, et al. Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health. 2017;5(12):e1192–e1207. doi: 10.1016/S2214-109X(17)30375-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Doran KM, Ragins KT, Gross CP, Zerger S. Medical respite programs for homeless patients: a systematic review. J Health Care Poor Underserved. 2013;24(2):499–524. doi: 10.1353/hpu.2013.0053. [DOI] [PubMed] [Google Scholar]
- 91.Dorney-Smith S, Thomson E, Hewett N, Burridge S, Khan Z. Homeless medical respite service provision in the UK. House Care Support. 2019;22(1):40–53. doi: 10.1108/HCS-08-2018-0021. [DOI] [Google Scholar]
- 92.Edlin BR, Eckhardt BJ, Shu MA, Holmberg SD, Swan T. Toward a more accurate estimate of the prevalence of hepatitis C in the United States. Hepatology. 2015;62(5):1353–1363. doi: 10.1002/hep.27978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.El Baba R, Colucci E. Post-traumatic stress disorders, depression, and anxiety in unaccompanied refugee minors exposed to war-related trauma: a systematic review. Int J Cult Mental Health. 2018;11(2):194–207. doi: 10.1080/17542863.2017.1355929. [DOI] [Google Scholar]
- 94.Embleton L, Mwangi A, Vreeman R, Ayuku D, Braitstein P. The epidemiology of substance use among street children in resource-constrained settings: a systematic review and meta-analysis. Addiction. 2013;108(10):1722–1733. doi: 10.1111/add.12252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ennis N, Roy S, Topolovec-Vranic J. Memory impairment among people who are homeless: a systematic review. Memory. 2015;23(5):695–713. doi: 10.1080/09658211.2014.921714. [DOI] [PubMed] [Google Scholar]
- 96.Fitzpatrick-Lewis D, Ganann R, Krishnaratne S, Ciliska D, Kouyoumdjian F, Hwang SW. Effectiveness of interventions to improve the health and housing status of homeless people: a rapid systematic review. BMC Public Health. 2011;11:638. doi: 10.1186/1471-2458-11-638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Flach Y, Razza TS. Suicidality in homeless children and adolescent: a systematic review. Aggress Violent Behav. 2022;64:101575.
- 98.Folsom D, Jeste DV. Schizophrenia in homeless persons: a systematic review of the literature. Acta Psychiatr Scand. 2002;105(6):404–413. doi: 10.1034/j.1600-0447.2002.02209.x. [DOI] [PubMed] [Google Scholar]
- 99.Formosa EA, Kishimoto V, Orchanian-Cheff A, Hayman K. Emergency department interventions for homelessness: a systematic review. Cjem. 2021;23(1):111–122. doi: 10.1007/s43678-020-00008-4. [DOI] [PubMed] [Google Scholar]
- 100.Formosa EA, Kishimoto V, Orchanian-Cheff A, Hayman KG. 302 Emergency Department Interventions for Homelessness: A Systematic Review. Ann Emerg Med. 2019;74(4):S119. doi: 10.1016/j.annemergmed.2019.08.261. [DOI] [PubMed] [Google Scholar]
- 101.Fry CE, Langley K, Shelton KH. A systematic review of cognitive functioning among young people who have experienced homelessness, foster care, or poverty. Child Neuropsychol. 2017;23(8):907–934. doi: 10.1080/09297049.2016.1207758. [DOI] [PubMed] [Google Scholar]
- 102.Gentry S, Forouhi NG, Notley C. Are Electronic Cigarettes an Effective Aid to Smoking Cessation or Reduction Among Vulnerable Groups? A Systematic Review of Quantitative and Qualitative Evidence. Nicotine Tob Res. 2019;21(5):602–616. doi: 10.1093/ntr/nty054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Getty CA, Morande A, Lynskey M, Weaver T, Metrebian N. Mobile telephone-delivered contingency management interventions promoting behaviour change in individuals with substance use disorders: a meta-analysis. Addiction. 2019;114(11):1915–1925. doi: 10.1111/add.14725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Gulati G, Keating N, O'Neill A, Delaunois I, Meagher D, Dunne CP. The prevalence of major mental illness, substance misuse and homelessness in Irish prisoners: systematic review and meta-analyses. Ir J Psychol Med. 2019;36(1):35–45. doi: 10.1017/ipm.2018.15. [DOI] [PubMed] [Google Scholar]
- 105.Hamilton K, Tolfree R, Mytton J. A systematic review of active case-finding strategies for tuberculosis in homeless populations. Int J Tuberc Lung Dis. 2018;22(10):1135–1144. doi: 10.5588/ijtld.17.0784. [DOI] [PubMed] [Google Scholar]
- 106.Hamilton K, Tolfree R, Mytton J. Impact and implementation of active case finding for tuberculosis in homeless populations: a systematic review. Lancet. 2019;394:S48. doi: 10.1016/S0140-6736(19)32845-4. [DOI] [PubMed] [Google Scholar]
- 107.Hanlon P, Yeoman L, Gibson L, Esiovwa R, Williamson AE, Mair FS, Lowrie R. A systematic review of interventions by healthcare professionals to improve management of non-communicable diseases and communicable diseases requiring long-term care in adults who are homeless. BMJ Open. 2018;8(4):e020161. doi: 10.1136/bmjopen-2017-020161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Heerde JA, Hemphill SA. A systematic review of associations between perpetration of physically violent behaviors and property offenses, victimization and use of substances among homeless youth. Children Youth Serv Rev. 2014;44:265–277. doi: 10.1016/j.childyouth.2014.06.020. [DOI] [Google Scholar]
- 109.Heerde JA, Hemphill SA. Is Substance Use Associated with Perpetration and Victimization of Physically Violent Behavior and Property Offences Among Homeless Youth? A Systematic Review of International Studies. Child Youth Care Forum. 2015;44(2):277–307. doi: 10.1007/s10566-014-9282-x. [DOI] [Google Scholar]
- 110.Heerde JA, Hemphill SA. The role of risk and protective factors in the modification of risk for sexual victimization, sexual risk behaviors, and survival sex among homeless youth: A meta-analysis. J Investig Psychol Offend Profil. 2017;14(2):150–174. doi: 10.1002/jip.1473. [DOI] [Google Scholar]
- 111.Heerde JA, Hemphill SA. Associations between individual-level characteristics and exposure to physically violent behavior among young people experiencing homelessness: A meta-analysis. Aggress Violent Behav. 2019;47:46–57. doi: 10.1016/j.avb.2019.03.002. [DOI] [Google Scholar]
- 112.Heerde JA, Scholes-Balog KE, Hemphill SA. Associations between youth homelessness, sexual offenses, sexual victimization, and sexual risk behaviors: a systematic literature review. Arch Sex Behav. 2015;44(1):181–212. doi: 10.1007/s10508-014-0375-2. [DOI] [PubMed] [Google Scholar]
- 113.Herrman H. Mental disorders among homeless people in western countries. PLoS Med. 2008;5(12):e237. doi: 10.1371/journal.pmed.0050237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Heuvelings CC, de Vries SG, Greve PF, Visser BJ, Bélard S, Janssen S, Cremers AL, Spijker R, Shaw B, Hill RA, et al. Effectiveness of interventions for diagnosis and treatment of tuberculosis in hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review. Lancet Infect Dis. 2017;17(5):e144–e158. doi: 10.1016/S1473-3099(16)30532-1. [DOI] [PubMed] [Google Scholar]
- 115.Heuvelings CC, Greve PF, de Vries SG, Visser BJ, Bélard S, Janssen S, Cremers AL, Spijker R, Shaw E, Hill RA, et al. Effectiveness of service models and organisational structures supporting tuberculosis identification and management in hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review. BMJ Open. 2018;8(9):e019642. doi: 10.1136/bmjopen-2017-019642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Hino P, Yamamoto TT, Bastos SH, Beraldo AA, Figueiredo T, Bertolozzi MR. Tuberculosis in the street population: a systematic review. Rev Esc Enferm USP. 2021;55:e03688. doi: 10.1590/s1980-220x2019039603688. [DOI] [PubMed] [Google Scholar]
- 117.Hino P, Yamamoto TT, Bastos SH, Beraldo AA, Figueiredo TMRM, Bertolozzi MR. Tuberculosis in the street population: a systematic review. Revista da Escola de Enfermagem da U S P. 2021;55:e03688. doi: 10.1590/s1980-220x2019039603688. [DOI] [PubMed] [Google Scholar]
- 118.Hodgson KJ, Shelton KH, van den Bree MB, Los FJ. Psychopathology in young people experiencing homelessness: a systematic review. Am J Public Health. 2013;103(6):e24–e37. doi: 10.2105/AJPH.2013.301318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Hodgson KJ, Shelton KH, Van Den Bree MBM, Los FJ. Psychopathology in young people experiencing homelessness: A systematic review. Am J Public Health. 2013;103(6):e24–e37. doi: 10.2105/AJPH.2013.301318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Hoell A, Franz M, Salize HJ. Healthcare for homeless people with mental illness-A review of results of current interventions. Psychiatrie. 2017;14(2):75–85. [Google Scholar]
- 121.Hoffberg AS, Spitzer E, Mackelprang JL, Farro SA, Brenner LA. Suicidal Self-Directed Violence Among Homeless US Veterans: A Systematic Review. Suicide Life Threat Behav. 2018;48(4):481–498. doi: 10.1111/sltb.12369. [DOI] [PubMed] [Google Scholar]
- 122.Hossain MM, Purohit N, Sultana A, Ma P, McKyer ELJ, Ahmed HU. Prevalence of mental disorders in South Asia: An umbrella review of systematic reviews and meta-analyses. Asian J Psychiatr. 2020;51:102041. doi: 10.1016/j.ajp.2020.102041. [DOI] [PubMed] [Google Scholar]
- 123.Hwang SW, Tolomiczenko G, Kouyoumdjian FG, Garner RE. Interventions to improve the health of the homeless: a systematic review. Am J Prev Med. 2005;29(4):311–319. doi: 10.1016/j.amepre.2005.06.017. [DOI] [PubMed] [Google Scholar]
- 124.Ijaz S, Jackson J, Thorley H, Porter K, Fleming C, Richards A, Bonner A, Savović J. Nutritional deficiencies in homeless persons with problematic drinking: a systematic review. Int J Equity Health. 2017;16(1):71. doi: 10.1186/s12939-017-0564-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Ijaz S, Thorley H, Porter K, Fleming C, Jones T, Kesten J, Mamluk L, Richards A, Marques EMR, Savović J. Interventions for preventing or treating malnutrition in homeless problem-drinkers: a systematic review. Int J Equity Health. 2018;17(1):8. doi: 10.1186/s12939-018-0722-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Karki P, Shrestha R, Huedo-Medina TB, Copenhaver M. The impact of methadone maintenance treatment on HIV risk behaviors among high-risk injection drug users: a systematic review. Evid Based Med Public Health. 2016;2:e1229. [PMC free article] [PubMed] [Google Scholar]
- 127.Kenworthy J, Ayyub R, Rtveladze K, Wright D, Xia A, Fordham R. A systematic literature review of the societal costs and consequences of heroin addiction. Value Health. 2017;20(9):A497. doi: 10.1016/j.jval.2017.08.560. [DOI] [Google Scholar]
- 128.Klop HT, de Veer AJE, van Dongen SI, Francke AL, Rietjens JAC, Onwuteaka-Philipsen BD. Palliative care for homeless people: a systematic review of the concerns, care needs and preferences, and the barriers and facilitators for providing palliative care. BMC Palliat Care. 2018;17(1):67. doi: 10.1186/s12904-018-0320-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Krahn J, Caine V, Chaw-Kant J, Singh AE. Housing interventions for homeless, pregnant/parenting women with addictions: a systematic review. J Soc Distress Homeless. 2018;27(1):75–88. doi: 10.1080/10530789.2018.1442186. [DOI] [Google Scholar]
- 130.Kyle T, Dunn JR. Effects of housing circumstances on health, quality of life and healthcare use for people with severe mental illness: a review. Health Soc Care Community. 2008;16(1):1–15. doi: 10.1111/j.1365-2524.2007.00723.x. [DOI] [PubMed] [Google Scholar]
- 131.Leaver CA, Bargh G, Dunn JR, Hwang SW. The effects of housing status on health-related outcomes in people living with HIV: a systematic review of the literature. AIDS Behav. 2007;11(6 Suppl):85–100. doi: 10.1007/s10461-007-9246-3. [DOI] [PubMed] [Google Scholar]
- 132.Leibler JH, Zakhour CM, Gadhoke P, Gaeta JM. Zoonotic and Vector-Borne Infections Among Urban Homeless and Marginalized People in the United States and Europe, 1990-2014. Vector Borne Zoonotic Dis. 2016;16(7):435–444. doi: 10.1089/vbz.2015.1863. [DOI] [PubMed] [Google Scholar]
- 133.Lowrie R, Stock K, Lucey S, Knapp M, Williamson A, Montgomery M, Lombard C, Maguire D, Allan R, Blair R, et al. Pharmacist led homeless outreach engagement and non-medical independent prescribing (Rx) (PHOENIx) intervention for people experiencing homelessness: a non- randomised feasibility study. Int J Equity Health. 2021;20(1):19. doi: 10.1186/s12939-020-01337-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Luong CT, Rew L, Banner M. Suicidality in Young Men Who Have Sex with Men: A Systematic Review of the Literature. Issues Ment Health Nurs. 2018;39(1):37–45. doi: 10.1080/01612840.2017.1390020. [DOI] [PubMed] [Google Scholar]
- 135.Ly A, Latimer E. Housing First Impact on Costs and Associated Cost Offsets: A Review of the Literature. Can J Psychiatry. 2015;60(11):475–487. doi: 10.1177/070674371506001103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ly TDA, Castaneda S, Hoang VT, Dao TL, Gautret P. Vaccine-preventable diseases other than tuberculosis, and homelessness: A scoping review of the published literature, 1980 to 2020. Vaccine. 2021;39(8):1205–1224. doi: 10.1016/j.vaccine.2021.01.035. [DOI] [PubMed] [Google Scholar]
- 137.Maglione MA, Raaen L, Chen C, Azhar G, Shahidinia N, Shen M, Maksabedian E, Shanman RM, Newberry S, Hempel S. Effects of medication assisted treatment (MAT) for opioid use disorder on functional outcomes: a systematic review. J Subst Abuse Treatment. 2018;89:28–51. doi: 10.1016/j.jsat.2018.03.001. [DOI] [PubMed] [Google Scholar]
- 138.Magwood O, Salvalaggio G, Beder M, Kendall C, Kpade V, Daghmach W, Habonimana G, Marshall Z, Snyder E, O'Shea T, et al. The effectiveness of substance use interventions for homeless and vulnerably housed persons: A systematic review of systematic reviews on supervised consumption facilities, managed alcohol programs, and pharmacological agents for opioid use disorder. PLoS One. 2020;15(1):e0227298. doi: 10.1371/journal.pone.0227298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Martinez O, Wu E, Sandfort T, Dodge B, Carballo-Dieguez A, Pinto R, Rhodes S, Moya E, Chavez-Baray S. Evaluating the Impact of Immigration Policies on Health Status Among Undocumented Immigrants: A Systematic Review. J Immigrant Minor Health. 2015;17(3):947–970. doi: 10.1007/s10903-013-9968-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Mattick RP, Breen C, Kimber J, Davoli M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev. 2009;3:CD002209. doi: 10.1002/14651858.CD002209.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Mattick RP, Breen C, Kimber J, Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev. 2014;2:CD002207. doi: 10.1002/14651858.CD002207.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.McInnes DK, Li AE, Hogan TP. Opportunities for engaging low-income, vulnerable populations in health care: a systematic review of homeless persons' access to and use of information technologies. Am J Public Health. 2013;103(Suppl 2):e11–e24. doi: 10.2105/AJPH.2013.301623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.McPherson P, Krotofil J, Killaspy H. Mental health supported accommodation services: a systematic review of mental health and psychosocial outcomes. BMC Psychiatry. 2018;18(1):128. doi: 10.1186/s12888-018-1725-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Mendes KT, Ronzani TM, de Paiva FS. Homeless population, vulnerabilities and drugs: a systematic review. Psicol Soc. 2019;31:e169056. 10.1590/1807-0310/2019v31169056.
- 145.Moe J, Kirkland SW, Rawe E, Ospina MB, Vandermeer B, Campbell S, Rowe BH. Effectiveness of Interventions to Decrease Emergency Department Visits by Adult Frequent Users: A Systematic Review. Acad Emerg Med. 2017;24(1):40–52. doi: 10.1111/acem.13060. [DOI] [PubMed] [Google Scholar]
- 146.Momsen AM, Rasmussen JO, Nielsen CV, Iversen MD, Lund H. Multidisciplinary team care in rehabilitation: An overview of reviews. J Rehabil Med. 2012;44(11):901–912. doi: 10.2340/16501977-1040. [DOI] [PubMed] [Google Scholar]
- 147.Moniruzzaman A, Kazanjian A, Wong H, Chowdhury MM, Elwood RK, Fitzgerald JM. A systematic review on risk factors of mortality among Tb patients. Am J Respir Crit Care Med. 2010;181. 10.1164/ajrccm-conference.2010.181.1_MeetingAbstracts.A5460.
- 148.Morton MH, Kugley S, Epstein R, Farrell A. Interventions for youth homelessness: A systematic review of effectiveness studies. Child Youth Serv Rev. 2020;116:105096. doi: 10.1016/j.childyouth.2020.105096. [DOI] [Google Scholar]
- 149.Murray RL, Bauld L, Hackshaw LE, McNeill A. Improving access to smoking cessation services for disadvantaged groups: a systematic review. J Public Health (Oxf) 2009;31(2):258–277. doi: 10.1093/pubmed/fdp008. [DOI] [PubMed] [Google Scholar]
- 150.Muzzey FK, Fortenberry JD, Maas MK, Holtrop K, McCauley H. 169. Sexual and Gender Minority Homeless Youth and Their Sexual Relationships: A Systematic Review of Recent Literature. J Adolesc Health. 2020;66(2):S86. doi: 10.1016/j.jadohealth.2019.11.172. [DOI] [Google Scholar]
- 151.Nevard I, Green C, Bell V, Gellatly J, Brooks H, Bee P. Conceptualising the social networks of vulnerable children and young people: a systematic review and narrative synthesis. Soc Psychiatry Psychiatr Epidemiol. 2021;56(2):169–182. doi: 10.1007/s00127-020-01968-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Nilsson S, Nordentoft M, Hjorthoj C. Psychiatric predictors for becoming homeless and exiting homelessness: A systematic review and meta-analysis. Schizophrenia Bull. 2020;46:S278. doi: 10.1093/schbul/sbaa029.686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Noh D. Psychological Interventions for Runaway and Homeless Youth. J Nurs Scholar. 2018;50(5):465–472. doi: 10.1111/jnu.12402. [DOI] [PubMed] [Google Scholar]
- 154.Omerov P, Craftman Å, Mattsson E, Klarare A. Homeless persons' experiences of health- and social care: A systematic integrative review. Health Soc Care Community. 2020;28(1):1–11. doi: 10.1111/hsc.12857. [DOI] [PubMed] [Google Scholar]
- 155.Paisi M, March-McDonald J, Burns L, Snelgrove-Clarke E, Withers L, Shawe J. Perceived barriers and facilitators to accessing and utilising sexual and reproductive healthcare for people who experience homelessness: a systematic review. BMJ Sex Reprod Health. 2020;47:211–220. doi: 10.1136/bmjsrh-2020-200799. [DOI] [PubMed] [Google Scholar]
- 156.Paisi MD, March-Mcdonald J, Burns L, Snelgrove-Clarke E, Withers L, Shawe J. Perceived barriers and facilitators to accessing and utilising sexual and reproductive healthcare for people who experience homelessness: A systematic review. BMJ Sex Reprod Health. 2020;47:211–220. doi: 10.1136/bmjsrh-2020-200799. [DOI] [PubMed] [Google Scholar]
- 157.Paquette K, Cheng MP, Kadatz MJ, Cook VJ, Chen W, Johnston JC. Chest radiography for active tuberculosis case finding in the homeless: a systematic review and meta-analysis. Int J Tuberc Lung Dis. 2014;18(10):1231–1236. doi: 10.5588/ijtld.14.0105. [DOI] [PubMed] [Google Scholar]
- 158.Parks RW, Stevens RJ, Spence SA. A systematic review of cognition in homeless children and adolescents. J R Soc Med. 2007;100(1):46–50. doi: 10.1177/014107680710000116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Parriott A, Malekinejad M, Miller AP, Marks SM, Horvath H, Kahn JG. Care Cascade for targeted tuberculosis testing and linkage to Care in Homeless Populations in the United States: a meta-analysis. BMC Public Health. 2018;18(1):485. doi: 10.1186/s12889-018-5393-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Peng Y, Hahn RA, Finnie RKC, Cobb J, Williams SP, Fielding JE, Johnson RL, Montgomery AE, Schwartz AF, Muntaner C, et al. Permanent Supportive Housing With Housing First to Reduce Homelessness and Promote Health Among Homeless Populations With Disability: A Community Guide Systematic Review. J Public Health Manag Pract. 2020;26(5):404–411. doi: 10.1097/PHH.0000000000001219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Polcin DL. Co-occurring substance abuse and mental health problems among homeless persons: Suggestions for research and practice. J Soc Distress Homeless. 2016;26(1):1–10. doi: 10.1179/1573658X15Y.0000000004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Polillo A, Gran-Ruaz S, Sylvestre J, Kerman N. The use of eHealth interventions among persons experiencing homelessness: A systematic review. Digit Health. 2021;7:2055207620987066. doi: 10.1177/2055207620987066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Ponka D, Agbata E, Kendall C, Stergiopoulos V, Mendonca O, Magwood O, Saad A, Larson B, Sun AH, Arya N, et al. The effectiveness of case management interventions for the homeless, vulnerably housed and persons with lived experience: A systematic review. PLoS One. 2020;15(4):e0230896. doi: 10.1371/journal.pone.0230896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Rajendran M, Zaki RA, Aghamohammadi N. Contributing risk factors towards the prevalence of multidrug-resistant tuberculosis in Malaysia: A systematic review. Tuberculosis (Edinb) 2020;122:101925. doi: 10.1016/j.tube.2020.101925. [DOI] [PubMed] [Google Scholar]
- 165.Rezaei O, Ghiasvand H, Higgs P, Noroozi A, Noroozi M, Rezaei F, Armoon B, Bayani A. Factors associated with injecting-related risk behaviors among people who inject drugs: a systematic review and meta-analysis study. J Addict Dis. 2020;38(4):420–437. doi: 10.1080/10550887.2020.1781346. [DOI] [PubMed] [Google Scholar]
- 166.Richter D, Hoffmann H. Independent housing and support for people with severe mental illness: systematic review. Acta Psychiatr Scand. 2017;136(3):269–279. doi: 10.1111/acps.12765. [DOI] [PubMed] [Google Scholar]
- 167.Riquelme-Miralles D, Palazón-Bru A, Sepehri A, Gil-Guillén VF. A systematic review of non-pharmacological interventions to improve therapeutic adherence in tuberculosis. Heart Lung. 2019;48(5):452–461. doi: 10.1016/j.hrtlng.2019.05.001. [DOI] [PubMed] [Google Scholar]
- 168.Roy L. Criminal behavior and victimization among homeless individuals with severe mental illness: A systematic review (Psychiatric Services (2014)) Psychiatr Serv. 2014;65(7):896. doi: 10.1176/appi.ps.657erratum. [DOI] [PubMed] [Google Scholar]
- 169.Roy L, Crocker AG, Nicholls TL, Latimer EA, Ayllon AR. Criminal behavior and victimization among homeless individuals with severe mental illness: a systematic review. Psychiatr Serv. 2014;65(6):739–750. doi: 10.1176/appi.ps.201200515. [DOI] [PubMed] [Google Scholar]
- 170.Sandgren A, Vonk Noordegraaf-Schouten M, van Kessel F, Stuurman A, Oordt-Speets A, van der Werf MJ. Initiation and completion rates for latent tuberculosis infection treatment: a systematic review. BMC Infect Dis. 2016;16:204. doi: 10.1186/s12879-016-1550-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Saulle R, Vecchi S, Gowing L. Supervised dosing with a long-acting opioid medication in the management of opioid dependence. Cochrane Database Syst Rev. 2017;4:CD011983. doi: 10.1002/14651858.CD011983.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Sayal AP, Slomovic J, Bhambra NS, Popovic MM, Lichter M. Visual impairment and the prevalence of ocular pathology in homeless children and adults globally: a systematic review. Can J Ophthalmol. 2020;56:158–165. doi: 10.1016/j.jcjo.2020.09.023. [DOI] [PubMed] [Google Scholar]
- 173.Scappaticci ALSS, Blay SL. Homeless adolescent mothers: A systematic review of the literature. Revista de Psiquiatria do Rio Grande do Sul. 2010;32(1):3–15. doi: 10.1590/S0101-81082010000100002. [DOI] [Google Scholar]
- 174.Schneider JA, Skaathun B, Michaels S, Young L, Green K, Morgan E, Coombs RW, Friedman S, Laumann E. Drivers of HIV treatment success among a population-based sample of younger black MSM. Top Antiviral Med. 2015;23:494–495. [Google Scholar]
- 175.Schreiter S, Bermpohl F, Krausz M, Leucht S, Rössler W, Schouler-Ocak M, Gutwinski S. The Prevalence of Mental Illness in Homeless People in Germany. Dtsch Arztebl Int. 2017;114(40):665–672. doi: 10.3238/arztebl.2017.0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Schreiter S, Bermpohl F, Krausz M, Leucht S, Rössler W, Schouler-Ocak M, Gutwinski S. The prevalence of mental illness in homeless people in Germany - A systematic review and meta-analysis. Deutsches Arzteblatt Int. 2017;114(40):665–672. doi: 10.3238/arztebl.2017.0665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Schumacher JE, Milby JB, Wallace D, Meehan DC, Kertesz S, Vuchinich R, Dunning J, Usdan S. Meta-analysis of day treatment and contingency-management dismantling research: Birmingham Homeless Cocaine Studies (1990-2006) J Consult Clin Psychol. 2007;75(5):823–828. doi: 10.1037/0022-006X.75.5.823. [DOI] [PubMed] [Google Scholar]
- 178.Shortt SE, Hwang S, Stuart H, Bedore M, Zurba N, Darling M. Delivering primary care to homeless persons: a policy analysis approach to evaluating the options. Healthc Policy. 2008;4(1):108–122. [PMC free article] [PubMed] [Google Scholar]
- 179.Silva EN, da Silva Pereira ACE, de Araújo WN, Elias FTS. A systematic review of economic evaluations of interventions to tackle tuberculosis in homeless people. Revista Panamericana de Salud Publica/Pan Am J Public Health. 2018;42:e40. doi: 10.26633/RPSP.2018.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Silva EN, Pereira A, de Araújo WN, Elias FTS. A systematic review of economic evaluations of interventions to tackle tuberculosis in homeless people. Rev Panam Salud Publica. 2018;42:e40. doi: 10.26633/RPSP.2018.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Simmonds M, Simmonds K, Weleff J. Prevalence and problems of pain in the homeless: A systematic review. J Pain. 2016;17(4):S12–S13. doi: 10.1016/j.jpain.2016.01.050. [DOI] [Google Scholar]
- 182.Simoens S, Matheson C, Bond C, Inkster K, Ludbrook A. The effectiveness of community maintenance with methadone or buprenorphine for treating opiate dependence. Br J Gen Pract. 2005;55(511):139–146. [PMC free article] [PubMed] [Google Scholar]
- 183.Soar K, Dawkins L, Robson D, Cox S. Smoking amongst adults experiencing homelessness: A systematic review of prevalence rates, interventions and the barriers and facilitators to quitting and staying quit. J Smok Cessation. 2020;15:94–108. doi: 10.1017/jsc.2020.11. [DOI] [Google Scholar]
- 184.Speirs V, Johnson M, Jirojwong S. A systematic review of interventions for homeless women. J Clin Nurs. 2013;22(7-8):1080–1093. doi: 10.1111/jocn.12056. [DOI] [PubMed] [Google Scholar]
- 185.Spence S, Stevens R, Parks R. Cognitive dysfunction in homeless adults: a systematic review. J R Soc Med. 2004;97(8):375–379. doi: 10.1177/014107680409700804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Strang J, Groshkova T, Uchtenhagen A, Van Den Brink W, Haasen C, Schechter MT, Lintzeris N, Bell J, Pirona A, Oviedo-Joekes E. Heroin on trial: systematic review and meta-analysis of randomised trials of diamorphine-prescribing as treatment for refractory heroin addiction. Br J Psychiatr. 2015;207(1):5–14. doi: 10.1192/bjp.bp.114.149195. [DOI] [PubMed] [Google Scholar]
- 187.Stubbs JL, Thornton AE, Sevick JM, Silverberg ND, Barr AM, Honer WG, Panenka WJ. Traumatic brain injury in homeless and marginally housed individuals: a systematic review and meta-analysis. Lancet Public Health. 2020;5(1):e19–e32. doi: 10.1016/S2468-2667(19)30188-4. [DOI] [PubMed] [Google Scholar]
- 188.Sudarsanam TD, Tharyan P. Rifampicin compared to isoniazid for preventing active TB in HIV-negative people at risk of developing active TB: Implications for public health. Clin Epidemiol Global Health. 2014;2(1):28–36. doi: 10.1016/j.cegh.2013.11.003. [DOI] [Google Scholar]
- 189.Sumalinog R, Harrington K, Dosani N, Hwang SW. Advance care planning, palliative care, and end-of-life care interventions for homeless people: A systematic review. Palliat Med. 2017;31(2):109–119. doi: 10.1177/0269216316649334. [DOI] [PubMed] [Google Scholar]
- 190.Sundin EC. Homelessness and experiences of psychological trauma in the western world: A research review and a qualitative study. Eur Psychiatry. 2011;26:1811. doi: 10.1016/S0924-9338(11)73515-5. [DOI] [Google Scholar]
- 191.Tankimovich M. Barriers to and interventions for improved tuberculosis detection and treatment among homeless and immigrant populations: a literature review. J Community Health Nurs. 2013;30(2):83–95. doi: 10.1080/07370016.2013.778723. [DOI] [PubMed] [Google Scholar]
- 192.Thomas CP, Fullerton CA, Kim M, Montejano L, Lyman DR, Dougherty RH, Daniels AS, Ghose SS, Delphin-Rittmon ME. Medication-assisted treatment with buprenorphine: assessing the evidence. Psychiatric Serv. 2014;65(2):158–170. doi: 10.1176/appi.ps.201300256. [DOI] [PubMed] [Google Scholar]
- 193.Thomas Y, Gray M, McGinty S. A systematic review of occupational therapy interventions with homeless people. Occup Ther Health Care. 2011;25(1):38–53. doi: 10.3109/07380577.2010.528554. [DOI] [PubMed] [Google Scholar]
- 194.Thorley H, Porter K, Fleming C, Jones T, Kesten J, Marques E, Richards A, Savović J. Interventions for preventing or treating malnutrition in problem drinkers who are homeless or vulnerably housed: protocol for a systematic review. Syst Rev. 2015;4:131. doi: 10.1186/s13643-015-0114-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.To MJ, Brothers TD, Van Zoost C. Foot Conditions among Homeless Persons: A Systematic Review. PLoS One. 2016;11(12):e0167463. doi: 10.1371/journal.pone.0167463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Topolovec-Vranic J, Ennis N, Colantonio A, Cusimano MD, Hwang SW, Kontos P, Ouchterlony D, Stergiopoulos V. Traumatic brain injury among people who are homeless: a systematic review. BMC Public Health. 2012;12:1059. doi: 10.1186/1471-2458-12-1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Tsai J, Rosenheck RA. Risk factors for homelessness among US veterans. Epidemiol Rev. 2015;37:177–195. doi: 10.1093/epirev/mxu004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Twyman L, Bonevski B, Paul C, Bryant J. Perceived barriers to smoking cessation in selected vulnerable groups: a systematic review of the qualitative and quantitative literature. BMJ Open. 2014;4(12):e006414. doi: 10.1136/bmjopen-2014-006414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Vijayaraghavan M, Elser H, Frazer K, Lindson N, Apollonio D. Interventions to reduce tobacco use in people experiencing homelessness. Cochrane Database Syst Rev. 2020;12:CD013413. doi: 10.1002/14651858.CD013413.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Wang JZ, Mott S, Magwood O, Mathew C, McLellan A, Kpade V, Gaba P, Kozloff N, Pottie K, Andermann A. The impact of interventions for youth experiencing homelessness on housing, mental health, substance use, and family cohesion: a systematic review. BMC Public Health. 2019;19(1):1528. doi: 10.1186/s12889-019-7856-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Weber JJ. A systematic review of nurse-led interventions with populations experiencing homelessness. Public Health Nurs. 2019;36(1):96–106. doi: 10.1111/phn.12552. [DOI] [PubMed] [Google Scholar]
- 202.White BM, Newman SD. Access to primary care services among the homeless: a synthesis of the literature using the equity of access to medical care framework. J Prim Care Community Health. 2015;6(2):77–87. doi: 10.1177/2150131914556122. [DOI] [PubMed] [Google Scholar]
- 203.Whitney B, Kruszka B, Lorvick J, Lucas GM, Wechsberg W, Kuo I, Cunningham WE, Clemenzi-Allen A, Franks J, Crane HM. Association between housing stability and new HIV diagnosis in seek and test studies. Topics Antiviral Med. 2017;25(1):362s–363s. [Google Scholar]
- 204.Wilson MG, Aidala A, Gogolishvili D, Shubert V, Rueda S, Bozack A, Chambers LA, Caban M, Rourke SB. Housing status and the health of people living with HIV/AIDS: A systematic review. Can J Infect Dis Med Microbiol. 2012;23:40A–41A. [Google Scholar]
- 205.Woan J, Lin J, Auerswald C. The health status of street children and youth in low- and middle-income countries: a systematic review of the literature. J Adolesc Health. 2013;53(3):314–321.e312. doi: 10.1016/j.jadohealth.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 206.Wright N, Walker J. Homelessness and drug use - A narrative systematic review of interventions to promote sexual health. AIDS Care Psycholog Socio Med Aspects AIDS/HIV. 2006;18(5):467–478. doi: 10.1080/09540120500220474. [DOI] [PubMed] [Google Scholar]
- 207.Wright NM, Walker J. Homelessness and drug use - a narrative systematic review of interventions to promote sexual health. AIDS Care. 2006;18(5):467–478. doi: 10.1080/09540120500220474. [DOI] [PubMed] [Google Scholar]
- 208.Xiang J, Kaminga AC, Wu XY, Lai Z, Yang J, Lian Y, Wang X, Wen SW, Liu A, Dai W. Lifetime prevalence of suicidal attempt among homeless individuals in North America: a meta-analysis. J Affect Disord. 2021;287:341–349. doi: 10.1016/j.jad.2021.03.052. [DOI] [PubMed] [Google Scholar]
- 209.Yadee J, Bangpan M, Thavorn K, Welch V, Tugwell P, Chaiyakunapruk N. Assessing evidence of interventions addressing inequity among migrant populations: A two-stage systematic review. Int J Equity Health. 2019;18(1):64. doi: 10.1186/s12939-019-0970-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Zlotnick C, Tam T, Zerger S. Common needs but divergent interventions for U.S. homeless and foster care children: results from a systematic review. Health Soc Care Community. 2012;20(5):449–476. doi: 10.1111/j.1365-2524.2011.01053.x. [DOI] [PubMed] [Google Scholar]
- 211.Tweed EJ, Thomson RM, Lewer D, Sumpter C, Kirolos A, Southworth PM, Purba AK, Aldridge RW, Hayward A, Story A, et al. Health of people experiencing co-occurring homelessness, imprisonment, substance use, sex work and/or severe mental illness in high-income countries: a systematic review and meta-analysis. J Epidemiol Community Health. 2021;75:1010–1018. doi: 10.1136/jech-2020-215975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Arum C, Fraser H, Artenie AA, Bivegete S, Trickey A, Alary M, Astemborski J, Iversen J, Lim AG, MacGregor L, et al. Homelessness, unstable housing, and risk of HIV and hepatitis C virus acquisition among people who inject drugs: a systematic review and meta-analysis. Lancet Public Health. 2021;6:e309–e323. doi: 10.1016/S2468-2667(21)00013-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Suh K, Beck J, Katzman W, Allen DD. Homelessness and rates of physical dysfunctions characteristic of premature geriatric syndromes: systematic review and meta-analysis. Physiother Theory Pract. 2020;38:1–10. doi: 10.1080/09593985.2020.1809045. [DOI] [PubMed] [Google Scholar]
- 214.Al-Shakarchi NJ, Evans H, Luchenski SA, Story A, Banerjee A. Cardiovascular disease in homeless versus housed individuals: a systematic review of observational and interventional studies. Heart. 2020;106(19):1483–1488. doi: 10.1136/heartjnl-2020-316706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.van Draanen J, Tsang C, Mitra S, Karamouzian M, Richardson L. Socioeconomic marginalization and opioid-related overdose: A systematic review. Drug Alcohol Depend. 2020;214:108127. doi: 10.1016/j.drugalcdep.2020.108127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Lin D, Zhang CY, He ZK, Zhao XD. How does hard-to-reach status affect antiretroviral therapy adherence in the HIV-infected population? Results from a meta-analysis of observational studies. BMC Public Health. 2019;19(1):789. doi: 10.1186/s12889-019-7135-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Aldridge RW, Story A, Hwang SW, Nordentoft M, Luchenski SA, Hartwell G, Tweed EJ, Lewer D, Vittal Katikireddi S, Hayward AC. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet. 2018;391(10117):241–250. doi: 10.1016/S0140-6736(17)31869-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Bassuk EL, Richard MK, Tsertsvadze A. The prevalence of mental illness in homeless children: a systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2015;54(2):86–96.e82. doi: 10.1016/j.jaac.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 219.Aidala AA, Wilson MG, Shubert V, Gogolishvili D, Globerman J, Rueda S, Bozack AK, Caban M, Rourke SB. Housing Status, Medical Care, and Health Outcomes Among People Living With HIV/AIDS: A Systematic Review. Am J Public Health. 2016;106(1):e1–e23. doi: 10.2105/AJPH.2015.302905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Hyun M, Bae SH, Noh D. Systematic review and meta-analyses of randomized control trials of the effectiveness of psychosocial interventions for homeless adults. J Adv Nurs. 2020;76(3):773–786. doi: 10.1111/jan.14275. [DOI] [PubMed] [Google Scholar]
- 221.Dragioti E, Solmi M, Favaro A, Fusar-Poli P, Dazzan P, Thompson T, Stubbs B, Firth J, Fornaro M, Tsartsalis D. Association of antidepressant use with adverse health outcomes: a systematic umbrella review. JAMA Psychiatry. 2019;76(12):1241–1255. doi: 10.1001/jamapsychiatry.2019.2859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Fazel S, Geddes JR, Kushel M. The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet. 2014;384(9953):1529–1540. doi: 10.1016/S0140-6736(14)61132-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Smartt C, Prince M, Frissa S, Eaton J, Fekadu A, Hanlon C. Homelessness and severe mental illness in low-and middle-income countries: scoping review. BJPsych Open. 2019;5(4):e57. doi: 10.1192/bjo.2019.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Clemenzi-Allen A, Neuhaus J, Geng E, Sachdev D, Buchbinder S, Havlir D, et al. Housing instability results in increased acute care utilization in an urban HIV clinic cohort. In: Open forum infectious diseases: Oxford University Press US; 2019. p. ofz148. [DOI] [PMC free article] [PubMed]
- 225.Brown RT, Kiely DK, Bharel M, Mitchell SL. Factors associated with geriatric syndromes in older homeless adults. J Health Care Poor Underserved. 2013;24:456–468. doi: 10.1353/hpu.2013.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Culhane D, Treglia D, Steif K, Kuhn R, Byrne T. Estimated emergency and observational/quarantine capacity need for the US homeless population related to COVID-19 exposure by county; projected hospitalizations, intensive care units and mortality. 2020. https://endhomelessness.org/wp-content/uploads/2020/03/COVID-paper_clean-636pm.pdf.
- 227.Buchanan D, Kee R, Sadowski LS, Garcia D. The health impact of supportive housing for HIV-positive homeless patients: a randomized controlled trial. Am J Public Health. 2009;99(S3):S675–S680. doi: 10.2105/AJPH.2008.137810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a housing and case management program on emergency department visits and hospitalizations among chronically ill homeless adults: a randomized trial. Jama. 2009;301(17):1771–1778. doi: 10.1001/jama.2009.561. [DOI] [PubMed] [Google Scholar]
- 229.Onapa H, Sharpley CF, Bitsika V, McMillan ME, MacLure K, Smith L, Agnew LL. The physical and mental health effects of housing homeless people: A systematic review. Health Soc Care Community. 2021;30:448–468. doi: 10.1111/hsc.13486. [DOI] [PubMed] [Google Scholar]
- 230.van Agteren J, Iasiello M, Lo L, Bartholomaeus J, Kopsaftis Z, Carey M, Kyrios M. A systematic review and meta-analysis of psychological interventions to improve mental wellbeing. Nat Human Behav. 2021;5(5):631–652. doi: 10.1038/s41562-021-01093-w. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Material 1. adopted search strings. Table S1. criteria for the evaluation of the credibility of the evidence of observational studies. Please note that criterion n.1 (sample size of cases) was purposely waived as outlined in the main-text, methods section. Table S2. List of the 179 excluded records, with the reason(s). Note: duplicate records may appear multiple times for consistency issues. Table S3. Included SRs or MAs of observational studies; quality rating according to the AMSTAR-2. Table S4. Sensitivity analysis of evidence from SRs or MAs of observational studies for the association between homelessness and any health outcome.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and are available online at https://osf.io/am67d/ and https://osf.io/58mhu/.
The additional file includes the following: material 1 – [search strings]; table S1 - [criteria for the evaluation of the credibility of the evidence of observational studies]; table S2 – [excluded studies with reasons]; table S3 – [quality rating of the included SRs or MAs of observational studies, according to the AMSTAR-2]; table S4 – [sensitivity analysis].