Abstract
Background:
Arthroscopic treatment for labral tears includes debridement and repair. Long-term studies have failed to demonstrate a difference between these treatments in terms of conversion to total hip arthroplasty (THA).
Purpose:
To investigate 2 different labral treatments, debridement and repair, using an adjusted analysis to evaluate long-term conversion to THA.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
This was a retrospective cohort study of patients who underwent hip arthroscopy by a single surgeon between April 2007 and October 2014. Postoperative follow-up information included conversion to THA, patient satisfaction, and patient-reported outcome measures (modified Harris Hip Score; Hip Outcome Score, Activities of Daily Living and Sports Specific subscales; International Hip Outcome Tool; Nonarthritic Hip Score; and Lower Extremity Functional Scale).
Results:
Of the 204 hips included in the study, 99 (48.5%) underwent labral repair, and 105 (51.5%) underwent debridement. In total, 28 (13.7%) of the 204 patients underwent conversion to THA within 10 years after hip arthroscopy (labral repair: 5 [5.0%] vs labral debridement: 23 [21.9%]). Labral repair was associated with a significantly lower risk of conversion to THA compared with debridement (hazard ratio [HR] = 0.24; 95% CI, 0.07-0.74; P = .014). Additional factors associated with risk of conversion to THA included older age at the time of arthroscopy (HR = 1.06 per year; 95% CI, 1.02-1.11; P = .002) and Tönnis grade (HR = 2.39; CI, 1.14-5.41; P = .026). Abrasion chondroplasty, acetabuloplasty, body mass index, Outerbridge grade, and radiographic femoroacetabular impingement were not found to be significantly associated with risk of THA. No significant difference in patient satisfaction was found between treatment groups, and for patients who did not convert to THA, there was no difference in mean patient-reported outcome scores at final follow-up.
Conclusion:
Patients who underwent labral repair were less likely to convert to THA compared with patients who underwent labral debridement, despite adjustment for differences in baseline patient characteristics and preexisting pathology. Additional factors associated with a lower rate of hip survival were older age and osteoarthritis at the time of hip arthroscopy.
Keywords: hip arthroscopy, labral repair, labral debridement, labral tear, total hip arthroplasty, total hip conversion, femoroacetabular impingement
The acetabular labrum is a triangular-shaped, fibrocartilaginous structure that surrounds the hip. The labrum plays an integral part in maintaining proper hip stability and physiological function. 7 If the labrum becomes torn, the seal is disrupted, and health of the joint may be compromised. 4,6 One of the major risk factors for acetabular labral tears is femoroacetabular impingement (FAI), which entails asphericity of the femoral head (cam), excessive coverage of the anterior superior acetabular rim (pincer), or a retroverted acetabulum. 11,15 Injury from FAI and labral tears can extend into adjacent cartilage, which forecasts a poor prognosis for degenerative disease. 10,20,23,29 Therefore, clinical emphasis has been placed on treating labral tears and associated FAI.
Arthroscopic treatments for labral tears include debridement and repair. Labral debridement involves trimming and smoothing areas of torn or frayed labrum, whereas labral repair uses anchors and sutures to bundle tissue together and refix the labrum to its anatomic position. Although restoration of the labral seal provides a theoretical advantage, biomechanical studies have yielded mixed results when comparing the 2 surgical options and their effects on cartilage preservation. 1,30 Of relevance, Menge et al 21 found no significant difference in the hazard ratio (HR) between labral debridement and labral repair in terms of the risk of conversion to total hip arthroplasty (THA) when adjusted for independent contributors. However, Byrd and Jones 2 reported a high incidence of conversion to THA in patients who underwent labral debridement. Currently, hip arthroscopic surgeons emphasize conservation of the labrum using repair techniques whenever possible; labral repairs increased from 19% of all hip arthroscopy cases in 2009 to 81% in 2017. 28 Although the current literature has shown positive functional results with labral repair, comparative studies have not reported a significant difference in conversion to THA. 12,14,21
The purpose of this study was to investigate 2 different labral treatments, labral repair and labral debridement, using an adjusted analysis to evaluate the long-term conversion to THA. We hypothesized that labral repair would exhibit better hip survivorship than would labral debridement.
Methods
Study Design
This was a retrospective cohort study of patients undergoing hip arthroscopy by a single surgeon (S.D.M.) between April 2007 and October 2014. This time period was chosen to ensure that all patients had at least 5 years of clinical follow-up. Patients were included if they met the following criteria: acetabular labral tear that was treated with labral repair or labral debridement, minimum 5-year follow-up from the date of surgery to the date of survey response, completion of study surveys, and availability of preoperative radiographs. Patients were excluded if they met any of the following conditions: They had preoperative radiographs demonstrating a center-edge angle (CEA) of <20° indicating hip dysplasia, underwent hip arthroscopy for FAI without concomitant labral tear, underwent hip arthroscopy after previous ipsilateral hip surgery, or underwent hip arthroscopy for osteonecrosis. Consistent with indications found in prior studies that evaluated labral repair versus labral debridement, 21 labral debridement was performed if the labral tear was degenerative, hypoplastic, or isolated to a single plane involving <50% of the labrum. Labral repair was performed if there was adequate, healthy labral tissue for suture fixation or if the tear was complex with extension into the chondrolabral junction. For both labral repair and labral debridement, an attempt was made to restore the labral seal at the completion of the procedure. Institutional review board approval was obtained for the study protocol.
Data Collection
We invited patients to participate in the study after we filtered institutional data by operative year, followed by retrospective chart review, telephone surveys, and/or online surveys to attain applicable study data. Baseline patient characteristics included age, sex, laterality, body mass index (BMI), number of preoperative steroid injections, CEA, radiographic FAI, and Tönnis grade. 16 An alpha angle >50° was considered positive for cam FAI. 16 The presence of coxa profunda or crossover sign was considered positive for pincer FAI. 16 Intraoperative information included Outerbridge grade, traction time, and additional procedures performed. 18 Postoperative follow-up information included repeat hip arthroscopy on the ipsilateral side after surgery by the senior author (S.D.M.), conversion to THA, patient-reported outcome measures, and patient satisfaction. Prospectively collected patient-reported outcome measures were the modified Harris Hip Score (mHHS), Hip Outcome Score (HOS)–Activities of Daily Living subscale, HOS–Sports Specific subscale, 33-item International Hip Outcome Tool, Nonarthritic Hip Score, and Lower Extremity Functional Scale.
Preoperative Assessment
All patients initially presenting to the senior author’s clinic with hip pain underwent hip and pelvis radiography and a thorough physical examination, including provocation testing of the labrum and evaluation for FAI. 8 Patients with positive findings on physical examination (ie, pain and/or limited range of motion with flexion, adduction, and internal rotation or flexion, abduction, and external rotation) underwent magnetic resonance arthrography, diagnostic or therapeutic intra-articular injection of anesthetic or corticosteroid, and a trial of at least 3 months of nonoperative therapy including core strengthening physical therapy. Patients with persistent hip pain despite nonoperative therapy were offered hip arthroscopy.
Abbreviated Surgical Technique
Arthroscopic surgery on all patients was performed by a single surgeon. Anterolateral, anterior, midanterior, and Dienst portals were established. Puncture capsulotomy was performed to gain access to the joint, 3 and intermittent traction was used throughout the procedure. 31 To be consistent with indications found in previously published studies that evaluated labral repair versus labral debridement, 21 the surgeon performed labral debridement if the labral tear was degenerative, hypoplastic, or isolated to a single plane involving <50% of the labrum. Labral repair was performed if the remaining healthy labral tissue was adequate for suture fixation or if the tear was complex with extension into the chondrolabral junction. If the patient had concomitant FAI, the surgeon performed acetabular recession using a chondrolabral junction–preserving technique 32 and/or femoroplasty using an arthroscopic bur. 24 After treatment for labral tears and potentially concurrent FAI, the hip was dynamically tested to confirm range of motion. This was performed to ensure labral stability and absence of FAI.
Postoperative Rehabilitation
All patients included in this study underwent a strict postoperative rehabilitation protocol. After operative treatment, patients were allowed immediate weightbearing as tolerated using a flat-footed gait with crutches for 6 weeks. The decision to limit the patients’ activity during the first 6 weeks was secondary to the operating surgeon’s preference. A flat-footed gait with crutches prevented tilting of the pelvis and limited stress on the labral repair in the early postoperative period. At 6 weeks postoperatively, patients could start using a stationary bicycle to slowly regain motion in a manner that limited inflammation of healing tissue. At 10 weeks, patients were allowed to swim or use an elliptical trainer with light resistance. At 4 months, strengthening exercises including hamstring curls and short-arc leg press with low weight and high repetitions were encouraged. At 6 months, patients were permitted to gradually resume impact-loading exercises as tolerated. 22
Statistical Analysis
Statistical analysis was performed using SPSS Statistical Software Version 27 (IBM, Armonk, NY, USA). Categorical variables were analyzed using the chi-square test or Fisher exact test, as appropriate, and continuous variables were compared using Student t tests. Unadjusted survival analysis was performed using Kaplan-Meier curves, and comparisons were calculated using the log-rank test. We performed adjusted survival analysis with Cox proportional hazard models, adjusting for all variables that were significantly different between treatment groups at baseline (abrasion chondroplasty, acetabuloplasty, age, BMI, radiographic FAI) or those presumed to be predictive of conversion to THA (Tönnis grade and Outerbridge grade). All reported P values were 2-tailed, with the level of significance set at α = .05.
Results
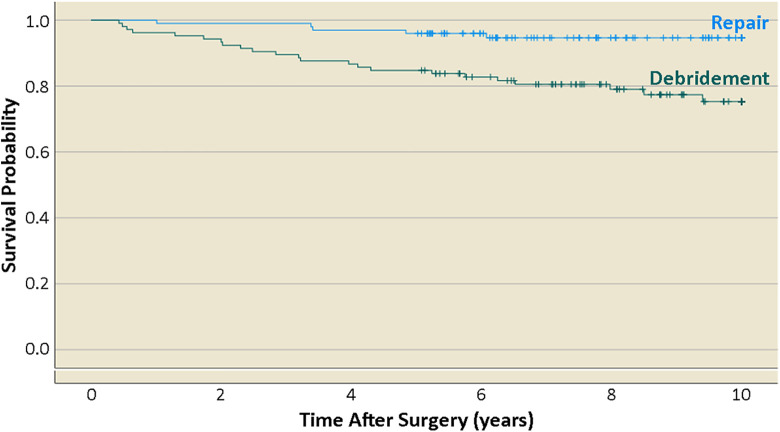
Of the 204 hips included in the study, 99 (48.5%) and 105 (51.5%) underwent labral repair and labral debridement, respectively (Figure 1). The debridement cohort was significantly older (P < .001), had a greater BMI (P = .012), and had a higher percentage of isolated cam lesions (P < .001). We found no significant difference between cohorts regarding sex, laterality, number of preoperative corticosteroid injections, CEA, or Tönnis grade (Table 1).
Figure 1.
Flowchart detailing patient enrollment.
Table 1.
Baseline Characteristics of Patients Undergoing Hip Arthroscopy for Acetabular Labral Tear a
| Labral Repair (n = 99) |
Labral Debridement (n = 105) |
P | |
|---|---|---|---|
| Age, y | 34.1 ± 1.9 | 40.4 ± 2.3 | <.001 |
| Body mass index | 25.8 ± 0.7 | 27.5 ± 1.0 | .012 |
| Sex | .589 | ||
| Male | 49 (49.5) | 48 (45.7) | |
| Female | 50 (50.5) | 57 (54.3) | |
| Laterality | .875 | ||
| Right | 52 (52.5) | 54 (51.4) | |
| Left | 47 (47.5) | 51 (48.6) | |
| No. of preoperative steroid injections | 1.23 ± 0.2 | 1.08 ± 0.2 | .422 |
| Center-edge angle, deg | 34.8 ± 1.1 | 35.4 ± 1.2 | .472 |
| Radiographic femoroacetabular impingement | <.001 | ||
| Isolated pincer | 36 (36.4) | 5 (4.8) | |
| Isolated cam | 8 (8.1) | 47 (44.8) | |
| Combined | 43 (43.4) | 16 (15.2) | |
| None | 12 (12.1) | 37 (35.2) | |
| Tönnis | .113 | ||
| Grade 0 | 24 (24.2) | 30 (28.6) | |
| Grade 1 | 67 (67.7) | 57 (54.3) | |
| Grade 2 | 8 (8.1) | 16 (15.2) | |
| Grade 3 | 0 (0.0) | 2 (1.9) |
a Data are reported as mean ± SD or No. of hips (%). Boldface P values indicate statistical significance (P < .05).
A significantly greater percentage of acetabuloplasty (P < .001) was performed in the labral repair cohort, whereas the debridement group had a greater percentage of abrasion chondroplasty (P < .001). No significant difference was found for Outerbridge grade, femoroplasty, microfracture, os acetabuli removal or fixation, chondrocalcinosis debridement, ligamentum teres debridement, or iliopsoas tendon debridement (Table 2).
Table 2.
Intraoperative Characteristics of Patients Undergoing Hip Arthroscopy for Acetabular Labral Tear a
| Labral Repair (n = 99) |
Labral Debridement (n = 105) |
P | |
|---|---|---|---|
| Outerbridge | .176 | ||
| Grade 0 | 1 (1.0) | 3 (2.8) | |
| Grade 1 | 17 (17.2) | 17 (16.2) | |
| Grade 2 | 46 (46.5) | 35 (33.3) | |
| Grade 3 | 26 (26.3) | 31 (29.5) | |
| Grade 4 | 9 (9.1) | 19 (18.1) | |
| Procedures | |||
| Femoroplasty | 52 (52.5) | 62 (59.0) | .348 |
| Acetabuloplasty | 81 (81.8) | 19 (18.1) | <.001 |
| Microfracture | 4 (4.0) | 9 (8.6) | .185 |
| Abrasion chondroplasty | 5 (5.1) | 23 (21.9) | <.001 |
| Os acetabuli removal/fixation | 3 (3.0) | 1 (1.0) | .285 |
| Chondrocalcinosis debridement | 0 (0.0) | 1 (1.0) | .330 |
| Ligamentum teres debridement | 3 (3.0) | 3 (2.8) | .942 |
| Iliopsoas tendon debridement | 3 (3.0) | 4 (3.8) | .760 |
a Data are reported as No. of hips (%). Boldface P values indicate statistical significance (P < .05).
A total of 4 (2.0%) of the 204 hips underwent subsequent hip arthroscopy for recurrence of pain. Of these hips, 2 were in the repair cohort, and subsequent arthroscopy at 3 years and 4 years after initial surgery. The other 2 hips were in the debridement cohort, and subsequent arthroscopy at 5 years and 6 years after initial surgery. None of these 4 hips underwent future THA within the study period.
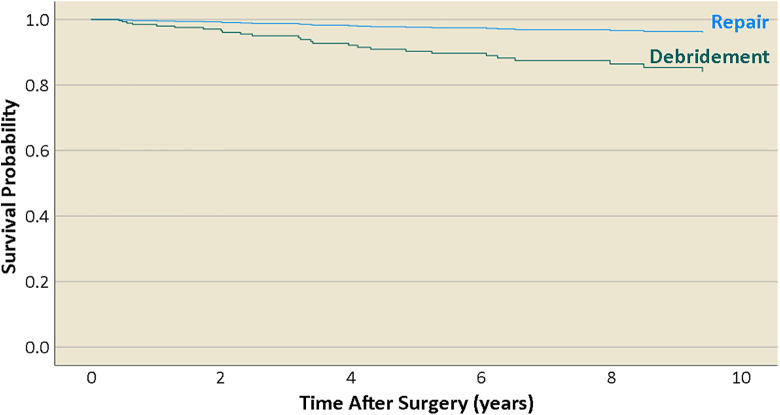
Of the 204 patients, 28 patients (13.7%) underwent conversion to THA within 10 years after hip arthroscopy. Of the 99 patients who underwent labral repair, 5 patients (5.1%) converted to THA at a mean ± standard deviation of 3.74 ± 1.90 years. Of the 105 patients who underwent labral debridement, 23 patients (21.9%) converted to THA at a mean of 3.70 ± 2.66 years. Unadjusted survival analysis yielded an estimated THA-free survival at 10 years of 94.9% for labral repair and 75.3% for labral debridement (P < .001) (Figure 2).
Figure 2.
Unadjusted survival curves for labral repair versus labral debridement.
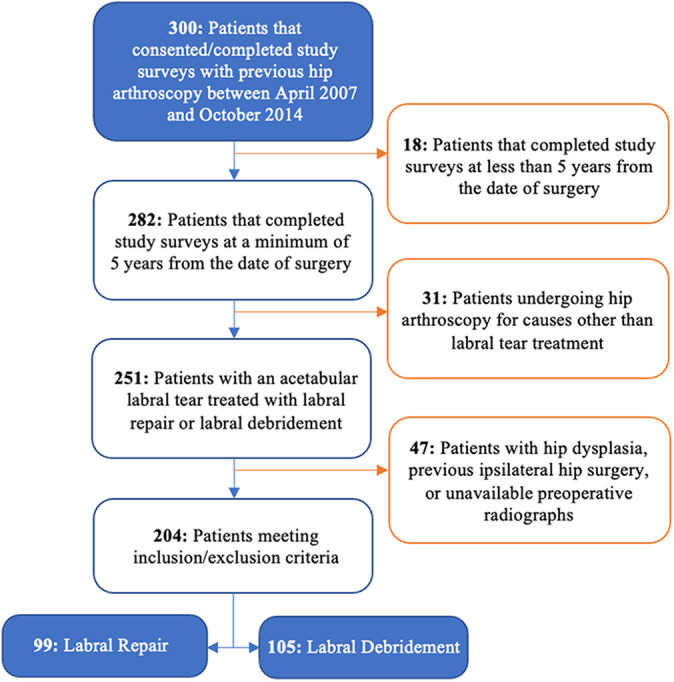
In the multivariable Cox model, which adjusted for all variables that were significantly different between treatment groups at baseline or those presumed to be predictive of conversion of THA, labral repair remained associated with a significantly lower risk of conversion to THA compared with labral debridement (HR = 0.24; 95% CI, 0.07-0.74; P = .014). Additional factors associated with risk of conversion to THA included older age at the time of arthroscopy (HR = 1.06 per year; 95% CI, 1.02-1.11; P = .002) and Tönnis grade (HR = 2.39; 95% CI, 1.14-5.41; P = .026). We found no significant associations between risk of THA and abrasion chondroplasty, acetabuloplasty, BMI, Outerbridge grade, or radiographic FAI (Table 3). Adjusted survival curves plotted at the means of covariates for labral repair versus labral debridement are shown in Figure 3.
Table 3.
Results of Cox Multivariate Regression a
| Variable | Hazard Ratio (95% CI) | P |
|---|---|---|
| Treatment (repair vs debridement) | 0.24 (0.07-0.74) | .014 |
| Abrasion chondroplasty | 1.80 (0.65-5.00) | .257 |
| Acetabuloplasty | 2.39 (0.84-6.78) | .102 |
| Age | 1.06 (1.02-1.11) | .002 |
| Body mass index | 1.06 (0.98-1.14) | .176 |
| Outerbridge grade | 1.23 (0.68-2.21) | .490 |
| Radiographic femoroacetabular impingement | 0.84 (0.58-1.20) | .329 |
| Tönnis grade | 2.39 (1.14-5.41) | .026 |
a Results were adjusted for variables that were significantly different at baseline between treatment groups and those presumed to be predictive of conversion to total hip arthroplasty. Boldface P values indicate statistical significance (P < .05).
Figure 3.
Adjusted survival curves plotted at the means of covariates for labral repair versus labral debridement.
We found no significant difference between treatment groups in terms of postoperative pain relief within the first 6 months of surgery or patient satisfaction. Similarly, for patients who did not convert to THA, we found no difference in mean patient-reported outcome measures at final follow-up for modified Harris Hip Score (P = .38), HOS-Activities of Daily Living subscale (P = .60), HOS–Sport Specific subscale (P = .48), 33-item International Hip Outcome Tool (P = .31), Nonarthritic Hip Score (P = .69), or Lower Extremity Functional Scale (P = .40) (Table 4).
Table 4.
Comparison of Subjective Postoperative Pain Relief, Patient Satisfaction, and Patient-Reported Outcome Measures Between Treatments a
| Labral Repair (n = 99) |
Labral Debridement (n = 105) |
P | |
|---|---|---|---|
| Postoperative pain relief at 6 mo | .345 | ||
| Yes | 75 (75.8) | 84 (80.0) | |
| No | 24 (24.2) | 21 (20.0) | |
| Patient satisfaction | .629 | ||
| Yes | 87 (87.9) | 89 (84.8) | |
| No | 12 (12.1) | 16 (15.2) | |
| Patient-reported outcome measures | |||
| mHHS | 86.1 ± 3.1 | 84.1 ± 3.1 | .378 |
| HOS-ADL | 88.3 ± 3.0 | 87.2 ± 3.0 | .603 |
| HOS–Sport | 75.1 ± 5.0 | 72.4 ± 5.5 | .475 |
| iHOT-33 | 75.0 ± 4.9 | 71.2 ± 5.2 | .312 |
| NAHS | 84.1 ± 3.8 | 83.0 ± 3.1 | .690 |
| LEFS | 67.8 ± 3.0 | 66.0 ± 3.3 | .402 |
a Data are reported as No. of hips (%) or mean ± 95% CI. HOS-ADL, Hip Outcome Score–Activities of Daily Living subscale; HOS–Sport, Hip Outcome Score–Sports Specific subscale; iHOT-33, 33-item International Hip Outcome Tool; LEFS, Lower Extremity Functional Scale; mHHS, modified Harris Hip Score; NAHS, Nonarthritic Hip Score.
Discussion
In this study, we found that patients with acetabular labral tears who underwent labral repair had a significantly lower conversion to THA when compared with patients who underwent labral debridement (HR = 0.24; 95% CI, 0.07-0.74; P = .014). These results held after adjustment for all observed differences in baseline factors. Age at the time of arthroscopy (HR = 1.06 per year; 95% CI, 1.02-1.11; P = .002) and Tönnis grade (HR = 2.39; 95% CI, 1.14-5.41; P = .026) were also associated with increased risk of conversion to THA. Among the hips that survived, both cohorts had patient-reported outcome scores at final follow-up that exceeded the threshold of the Patient Acceptable Symptom State for long-term follow-up. 25 We found no difference in patient-reported outcomes or patient satisfaction between groups.
The current study adds to the growing body of literature addressing functional outcomes and conversion to THA in patients undergoing hip arthroscopy for acetabular labral tears. In one of the first long-term studies comparing labral debridement and labral repair, Menge et al 21 reported that labral debridement and labral repair were both suitable treatments for labral tears, as both treatments resulted in significant improvements in patient-reported outcomes. However, those investigators found no significant difference in the HR between labral debridement and labral repair in terms of the risk of conversion to THA after accounting for independent contributors: older patients, hips with ≤2 mm of joint space preoperatively, and acetabular microfracture. Only when Menge et al adjusted their statistical analysis for microfracture alone (not for age or joint space) was labral debridement associated with a significantly higher risk of progression to THA. Thus, the results from the current study provide relevant evidence that patients who underwent labral repair were less likely to convert to THA when compared with patients who underwent labral debridement despite adjustment for differences in baseline characteristics and preexisting pathology. Furthermore, previous biomechanical studies demonstrated that restoration of the hip joint seal and reduction of contact pressures were associated with cartilage health in vitro. 6,27 Also, previous studies reported that loss of the seal mechanism was associated with alterations in synovial fluid and joint dynamics, which may lead to early osteoarthritis. 6,9,19 Thus, results of the current study reinforce the importance of labral conservation to preserve long-term health of the hip joint.
The findings of the current study support prior evidence that advanced age and osteoarthritis at the time of hip arthroscopy are predictive of poor postoperative outcomes and progression to THA. In 2009, Byrd and Jones 2 published a case series of patients after hip arthroscopy and reported that 88% of patients with osteoarthritis converted to THA within 10 years. Menge et al 21 reinforced these findings, reporting that older age, microfracture of the acetabulum, and joint space ≤2 mm were associated with a lower rate of hip survival. Similarly, Perets et al 26 reported that at minimum 5-year follow-up, hips that did not undergo THA had less radiographic and arthroscopic cartilage degeneration at the time of hip arthroscopy. In terms of functional outcomes, several studies have reported worse outcomes for patients with advanced osteoarthritis, with mixed results when considering age. 17,20,21,26 Martin et al 17 found that labral repair provided a benefit to patients older than 40 years without advanced osteoarthritis. In the context of the current study, hip arthroscopic surgeons should temper the expectations of patients who have cartilage wear, as there is ample evidence that such lesions are associated with a poor prognosis after hip arthroscopy and higher risk of conversion to THA.
Although uncomplicated labral tears may be addressed via standard repair techniques, complex tears and/or hypoplastic labrums may require advanced repair methods including the incorporation of grafted tissue to reestablish proper biomechanics. Notably, previous studies have reported successful outcomes for labral reconstruction using allografts or autografts from tensor fascia lata, semitendinosus, rectus femoris, gracilis, iliotibial band, and dermal tissue. Moreover, recent literature has demonstrated the utility of local capsular autograft as an effective approach to labral reconstruction that minimizes donor-site morbidity and preserves the chondrolabral junction. 13 As such, the senior author has expanded his repair indications to encompass labra that were previously deemed fit for debridement given the development of novel techniques and supporting evidence. 3,13,24,31 Overall, as the approaches to labral reconstruction advance, there is continued opportunity for joint preservation and increased survivorship.
Limitations
Although this study used a large sample size with long-term follow-up to demonstrate a significant difference between survivorship in patients undergoing labral repair versus labral debridement, it is not without limitations. First, this was a retrospective analysis and was subject to the limitations therein; a randomized controlled trial would be needed to definitively determine causality. Second, the choice of treatment was based on preexisting labral pathology. However, indications for labral debridement featured pathology that was not necessarily more severe than that indicating labral repair, as patients with tears isolated to a single plane involving <50% of the labrum underwent debridement whereas patients with tears extending into the chondrolabral junction underwent repair. The analysis also adjusted for differences that are correlated with poor prognoses after hip arthroscopy, including cartilage damage, FAI, and osteoarthritis. Third, postoperative lateral CEAs were not recorded, and therefore the effect of iatrogenic overresection was not evaluated. 33 Fourth, with the publication of novel studies during this time period, 5 the senior author transitioned to performing predominantly labral repairs. Despite the associated learning curve for the surgeon, patients who underwent labral repair had significantly lower conversion to THA and no difference in patient-reported outcomes compared with patients who underwent labral debridement. Fifth, labral debridement is a less technically challenging procedure, whereas labral repair is complicated and requires an expert hip arthroscopic surgeon. Thus, results may differ for non–high volume hip arthroscopic surgeons.
Conclusion
Patients who underwent labral repair were less likely to convert to THA compared with patients who underwent labral debridement despite adjustment for differences in baseline characteristics and preexisting pathology. Additional factors associated with a lower rate of hip survival were older age and the presence of osteoarthritis at the time of hip arthroscopy.
Footnotes
Final revision submitted May 21, 2022; accepted May 26, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: Support was received from the Conine Family Fund for Joint Preservation. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Partners Human Research Committee (protocol No. 2011-P-000053/1).
References
- 1. Beaulé PE, Speirs AD, Anwander H, et al. Surgical correction of cam deformity in association with femoroacetabular impingement and its impact on the degenerative process within the hip joint. J Bone Joint Surg Am. 2017;99(16):1373–1381. [DOI] [PubMed] [Google Scholar]
- 2. Byrd JWT, Jones KS. Hip arthroscopy for labral pathology: prospective analysis with 10-year follow-up. Arthroscopy. 2009;25(4):365–368. [DOI] [PubMed] [Google Scholar]
- 3. Conaway WK, Martin SD. Puncture capsulotomy during hip arthroscopy for femoroacetabular impingement: preserving anatomy and biomechanics. Arthrosc Tech. 2017;6(6):e2265–e2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Crawford MJ, Dy CJ, Alexander JW, et al. The 2007 Frank Stinchfield Award: the biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res. 2007;465:16–22. [DOI] [PubMed] [Google Scholar]
- 5. Espinosa N, Rothenfluh D, Beck M, Ganz R, Leunig M. Treatment of femoro-acetabular impingement: preliminary results of labral refixation. J Bone Joint Surg Am. 2006;88(5):925–935. [DOI] [PubMed] [Google Scholar]
- 6. Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of the acetabular labral seal in hip joint mechanics. J Biomech. 2003;36(2):171–178. [DOI] [PubMed] [Google Scholar]
- 7. Ferguson SJ, Bryant JT, Ganz R, Ito K. The acetabular labrum seal: a poroelastic finite element model. Clin Biomech (Bristol, Avon). 2000;15(6):463–468. [DOI] [PubMed] [Google Scholar]
- 8. Griffin DR, Dickenson EJ, O’Donnell J, et al. The Warwick agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 2016;50(19):1169–1176. [DOI] [PubMed] [Google Scholar]
- 9. Henak CR, Ellis BJ, Harris MD, Anderson AE, Peters CL, Weiss JA. Role of the acetabular labrum in load support across the hip joint. J Biomech. 2011;44(12):2201–2206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Johnston TL, Schenker ML, Briggs KK, Philippon MJ. Relationship between offset angle alpha and hip chondral injury in femoroacetabular impingement. Arthroscopy. 2008;24(6):669–675. [DOI] [PubMed] [Google Scholar]
- 11. Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21(12):1496–1504. [DOI] [PubMed] [Google Scholar]
- 12. Krych AJ, Thompson M, Knutson Z, Scoon J, Coleman SH. Arthroscopic labral repair versus selective labral debridement in female patients with femoroacetabular impingement: a prospective randomized study. Arthroscopy. 2013;29(1):46–53. [DOI] [PubMed] [Google Scholar]
- 13. Kucharik M, Abraham P, Nazal M, Varady N, Meek W, Martin S. Minimum 2-year functional outcomes of patients undergoing capsular autograft hip labral reconstruction. Am J Sports Med. 2021;49(10):2659–2667. [DOI] [PubMed] [Google Scholar]
- 14. Larson CM, Giveans MR, Stone RM. Arthroscopic debridement versus refixation of the acetabular labrum associated with femoroacetabular impingement: mean 3.5-year follow-up. Am J Sports Med. 2012;40(5):1015–1021. [DOI] [PubMed] [Google Scholar]
- 15. Leunig M, Beaulé PE, Ganz R. The concept of femoroacetabular impingement: current status and future perspectives. Clin Orthop Relat Res. 2009;467:616–622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mannava S, Geeslin AG, Frangiamore SJ, et al. Comprehensive clinical evaluation of femoroacetabular impingement, part 2: plain radiography. Arthrosc Tech. 2017;6(5):e2003–e2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Martin SD, Abraham PF, Varady NH, et al. Hip arthroscopy versus physical therapy for the treatment of symptomatic acetabular labral tears in patients older than 40 years: a randomized controlled trial. Am J Sports Med. 2021;49(5):1199–1208. [DOI] [PubMed] [Google Scholar]
- 18. Matles A. A microscopic study of the newborn fibrocartilagenous acetabular labrum. Clin Orthop Relat Res. 1967;54:197–206. [PubMed] [Google Scholar]
- 19. McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25–37. [DOI] [PubMed] [Google Scholar]
- 20. McCormick F, Nwachukwu BU, Alpaugh K, Martin SD. Predictors of hip arthroscopy outcomes for labral tears at minimum 2-year follow-up: the influence of age and arthritis. Arthroscopy. 2012;28(10):1359–1364. [DOI] [PubMed] [Google Scholar]
- 21. Menge TJ, Briggs KK, Dornan GJ, McNamara SC, Philippon MJ. Survivorship and outcomes 10 years following hip arthroscopy for femoroacetabular impingement labral debridement compared with labral repair. J Bone Joint Surg Am. 2017;99(12):997–1004. [DOI] [PubMed] [Google Scholar]
- 22. Naessig S, Kucharik M, Meek W, Eberlin C, Martin S. Prehabilitation and rehabilitation program for patients undergoing arthroscopic acetabular labral repair: a comprehensive 5-phase patient-guided program. Orthop J Sports Med. 2022;10(2):23259671211071073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nho SJ, Magennis EM, Singh CK, Kelly BT. Outcomes after the arthroscopic treatment of femoroacetabular impingement in a mixed group of high-level athletes. Am J Sports Med. 2011;39(1 suppl):14S–19S. [DOI] [PubMed] [Google Scholar]
- 24. Nwachukwu BU, Alpaugh K, McCormick F, Martin SD. All-arthroscopic reconstruction of the acetabular labrum by capsular augmentation. Arthrosc Tech. 2015;4(2):e127–e131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nwachukwu BU, Beck EC, Kunze KN, Chahla J, Rasio J, Nho SJ. Defining the clinically meaningful outcomes for arthroscopic treatment of femoroacetabular impingement syndrome at minimum 5-year follow-up. Am J Sports Med. 2020;48(4):901–907. [DOI] [PubMed] [Google Scholar]
- 26. Perets I, Chaharbakhshi EO, Mu B, et al. Hip arthroscopy in patients ages 50 years or older: minimum 5-year outcomes, survivorship, and risk factors for conversion to total hip replacement. Arthroscopy. 2018;34(11):3001–3009. [DOI] [PubMed] [Google Scholar]
- 27. Philippon MJ, Nepple JJ, Campbell KJ, et al. The hip fluid seal, part I: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):722–729. [DOI] [PubMed] [Google Scholar]
- 28. Riff AJ, Kunze KN, Movassaghi K, et al. Systematic review of hip arthroscopy for femoroacetabular impingement: the importance of labral repair and capsular closure. Arthroscopy. 2019;35(2):646–656.e3. [DOI] [PubMed] [Google Scholar]
- 29. Saadat E, Martin SD, Thornhill TS, Brownlee SA, Losina E, Katz JN. Factors associated with the failure of surgical treatment for femoroacetabular impingement: review of the literature. Am J Sports Med. 2014;42(6):1487–1495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Schmaranzer F, Haefeli PC, Hanke MS, et al. How does the dGEMRIC index change after surgical treatment for FAI? A prospective controlled study: preliminary results. Clin Orthop Relat Res. 2017;475(4):1080–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Skelley NW, Conaway WK, Martin SD. “In-round” labral repair after acetabular recession using intermittent traction. Arthrosc Tech. 2017;6(5):e1807–e1813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Syed H, Martin S. Arthroscopic acetabular recession with chondrolabral preservation. Am J Orthop. 2013;42(4):181–184. [PubMed] [Google Scholar]
- 33. Vesey RM, Bacon CJ, Brick MJ. Pre-existing osteoarthritis remains a key feature of arthroscopy patients who convert to total hip arthroplasty. J ISAKOS. 2021;6:199–203. [DOI] [PubMed] [Google Scholar]