Abstract
Background/Aims
We evaluated the clinical significance and prognostic power of functional luminal imaging probe (FLIP) panometry in patients with achalasia treated with peroral endoscopic myotomy (POEM), and examined the clinical parameters associated with symptomatic improvement and the presence of contractility (POC) following POEM.
Methods
We reviewed the electronic medical records of patients with achalasia treated with FLIP panometry and POEM at a tertiary teaching hospital in Seoul, Republic of Korea. Follow-up examination was composed of esophageal manometry and questionnaires on symptoms. We analyzed the FLIP data by interpolating using the cubic spline method in MATLAB.
Results
We retrospectively analyzed 33 men and 35 women (mean age 52 ± 17 years), of whom 14, 39, and 15 patients were diagnosed with achalasia types I, II, and III, respectively. The FLIP panometry diagnoses were reduced esophagogastric junction opening (REO) with a retrograde contractile response (n = 43); REO with an absent contractile response (n = 5); REO with a normal contractile response (n = 11); and a retrograde contractile response (n = 9). Overall, the patients showed improvements in Eckardt scores following POEM from 6.48 ± 2.20 to 1.16 ± 1.15 (P < 0.01). Post-POEM symptomatic improvement was not significantly associated with any of the clinical parameters, including panometry diagnosis. Conversely, post-POEM POC was significantly associated with the presence of repetitive antegrade contractions and achalasia subtypes (both P < 0.01).
Conclusion
While FLIP panometry was not significantly associated with the clinical course of achalasia, FLIP panometry was associated with POC following POEM and may complement manometry in the functional evaluation of esophageal motility disorders.
Keywords: Esophageal achalasia, Manometry, Myotomy
Introduction
Achalasia is an esophageal motility disorder characterized by the inability of the lower esophageal sphincter (LES) to relax and a lack of esophageal body peristalsis. Treatment methods include medication, endoscopic treatment, and surgical treatment. Among them, peroral endoscopic myotomy (POEM) has become the mainstay of endoscopic treatment for achalasia.1-3 POEM is currently being highlighted as a new treatment.
High-resolution manometry (HRM) based on a spatiotemporal plot can help diagnose esophageal motor disorders; the Chicago classification based on HRM showed a higher diagnostic yield than the previously used conventional criteria based on linear waves.4-7 However, the Chicago classification has its limitations, including inconsistent measurements of the adequacy of the esophagogastric junction (EGJ) with integrated relaxation pressure (IRP).
As research on achalasia has increased, interest in the functional luminal imaging probe (FLIP) has also increased.8-10 The FLIP showed a higher diagnostic yield compared to the previously used IRP in the measurement of the function of EGJ using the EGJ-distensibility index (EGJ-DI).11-13 Moreover, FLIP panometry can mimic secondary peristalsis, and new diagnostic criteria based on panometry showed a better diagnostic yield compared to the Chicago classification.14 However, its usefulness before POEM treatment is yet unproven, except in a small number of cases.15 Moreover, it is unclear which parameters can predict symptomatic improvement and the presence of esophageal peristalsis after POEM treatment.16,17 The aim of this study is to investigate the clinical significance of panometry before POEM and determine the predictive parameters of symptomatic improvement and presence of esophageal peristalsis after POEM.
Materials and Methods
Patients
We reviewed the clinical records of adult patients (age >18 years) with achalasia who had undergone FLIP panometry after induction of general anesthesia and POEM at a tertiary referral center in Seoul, South Korea, from October 2017 to March 2020. The following clinical data were collected: age, sex, HRM, FLIP data, and pre- and post-POEM Eckardt scores. This study was approved by the institutional review board of the treating institute (Approval No. S2019-1634).
Peroral Endoscopic Myotomy Operative Technique
POEM was performed by 3 expert endoscopists (H.Y.J., K.D.C., and D.H.K.) while the patient was under general anesthesia. All of the procedures were performed using an upper gastrointestinal endoscope with a plastic cap and carbon dioxide insufflation. Landmarks, such as the LES, gastroesophageal junction, and site of incision in the mid-esophagus, were identified by endoscopy before POEM. After injecting a starch-based or saline solution into the submucosal layer to create a submucosal bleb, a mucosal incision of approximately 3 cm was made using a hook knife (Olympus, Tokyo, Japan) using the dry cut mode at 60 W with effect 5 (ERBE, Tübingen, Germany). Myotomy was performed in the posterior (5 o’clock) position with an insulated-tip knife nano (Olympus, Tokyo, Japan) using the mode at 80 W with effect 7 at the discretion of the endoscopist; the myotomy was intended to be of selective/partial thickness in all of the cases. Following the completion of myotomy, the mucosal incision site was closed with endoclips.3
High-resolution Manometry With Esophageal Pressure Topography
Esophageal pressure topography studies of all patients were performed using a solid-state, high-resolution impedance manometry (HRIM) catheter with 32 circumferential sensors and 16 impedance sensors (InSight Ultima; Diversatek, Highlands Ranch, CO, USA). Manometry profiles were analyzed using the Zvu Advanced GI Diagnostic Software (Diversatek).
Manometry sensors were positioned to record data from the terminal portion of the proximal esophageal segment through the distal esophagus and into the proximal stomach. The HRIM assembly was fixed in place by taping it to the patient’s nose. Esophageal HRM was performed before and after POEM. The esophageal HRM protocol included a 30-second interval without swallowing to assess the basal EGJ pressure and morphology, followed by ten 5-mL swallows of normal saline solution in the supine position.18 Manometric data were analyzed using Zvu Advanced GI Diagnostic Software by 1 investigator (K.W.J.).19 Achalasia subtypes were determined based on the Chicago classification. IRP and LES resting pressure data were analyzed. The presence of contractility (POC) using esophageal HRM after POEM was defined by 2 investigators (K.W.J. and L.C.H.) after discussion.16
Functional Luminal Imaging Probe Measurement Protocol
The FLIP assembly was 240 cm long, with a 16-cm-long cylindrical bag mounted on the distal end of the catheter (EndoFLIP; Crospon, Galway, Ireland). The infinitely compliant bag housed 16 impedance planimetry electrodes spaced at 1-cm intervals and a solid-state pressure transducer positioned at the distal end. Impedance planimetry electrodes were used to generate cross-sectional areas (CSAs), and the intra-bag pressure was extracted from the solid-state pressure transducer.
Patients underwent general anesthesia during endoscopic intervention in the left lateral decubitus position. The FLIP catheter was inserted trans-orally and positioned under the direct endoscopic view, with 1 or 2 sensors placed distal to the EGJ. The proper placement was confirmed based on a visualized hourglass-like shape on the FLIP display; the narrowed area of the hourglass indicated the EGJ. The bag was gradually filled with normal saline from 30 mL to 70 mL with 10-mL intervals, with pauses for approximately 30 seconds to 60 seconds at each volume. FLIP measurements were gathered before POEM during general anesthesia.
Interpretation of Functional Luminal Imaging Probe Panometry
Continuous data measured using the FLIP obtained through the 16 sensors were extracted as ASCII files and analyzed using MATLAB (The Math Works, Natick, MA, USA). The customized program for data analysis was used to construct a topography plot based on the ASCII data extracted from each sensor. For better resolution, topography plot data were interpolated with 2-mm accuracy, and volume and pressure changes were displayed to aid in the intuitive understanding of the correlation between topography plots over time. The color in the topography plot indicates the diameter.
When evaluating FLIP motility, the volume was increased by 10 mL. We evaluated each data point from 30 mL to 70 mL using the EGJ-DI. To obtain the EGJ-DI, the median narrowest CSA was divided by the median intra-balloon pressure. The radius was obtained using the minimum diameter for each volume, and each CSA was derived using the radius. To evaluate the EGJ-DI, the median CSA for each volume was used.20
Each patient’s FLIP panometry data were evaluated by 2 investigators (K.W.J. and L.C.H.). The contraction that was induced by the distension pattern was evaluated for all patients in the study. Esophageal contractions were defined when an esophageal body diameter decreased by ≥ 5 mm in 2 or more adjacent impedance planimetry channels.
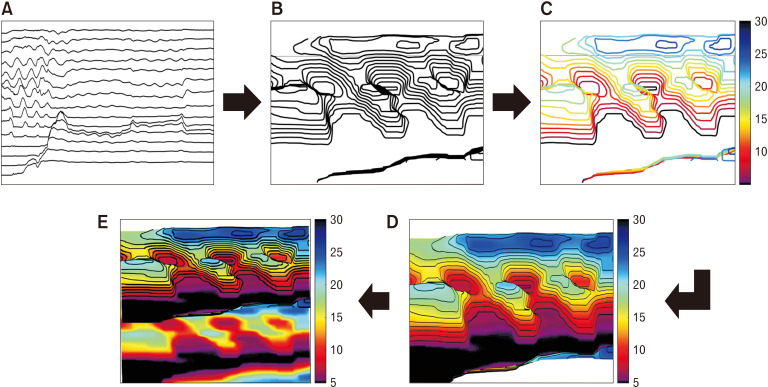
FLIP data were converted to 3-dimensional panometry data. We measured the diameter from the probe. Three-dimensional contour plots were constructed based on the measured diameter to which the color contour was applied. We painted the surface with color according to the colored 3-dimensional contour plots. Finally, 3-dimensional panometry was compared with 2-dimensional panometry (Fig. 1).
Figure 1.
Process for the conversion of functional luminal imaging probe (FLIP) data to 3-dimensional panometry data. (A) Based on FLIP data obtained from each channel of the probe, the values of each channel are shown in a 2-dimensional plot. The x-axis shows the procedure time (second), and the y-axis shows the diameter (mm) of each channel. (B) The measured diameter data were used to convert FLIP data to 3-dimensional panometry data, and the diameter between each channel was interpolated by the spline method. The spline interpolation method performs interpolation by making interpolation functions of neighboring regions match not only the functional but also the differential value. The 3-dimensional contour plot was created using diameter values obtained through interpolation. (C) The 3-dimensional contour plot is colored according to the diameter. Depending on the diameter, the color changes from red to blue, and a few of the measured diameters less than 5 mm is set to black. (D) Creating 3-dimensional panometry data using the colored 3-dimensional contour plot from Figure 2A. (E) Dimension reduction of 3-dimensional panometry data into the 2-dimensional plot helps check the patient’s condition. (B to E) In each 3-dimensional plot, the x-axis represents the procedure time (second), the y-axis represents the probe channel, and the z-axis represents the diameter (mm) measured at the probe.
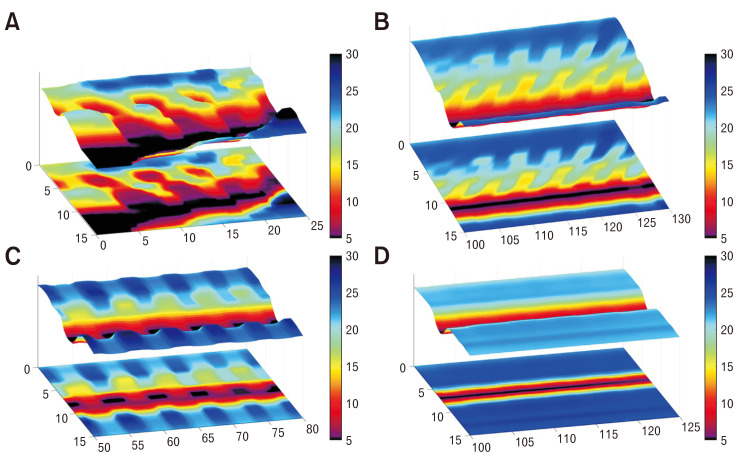
Contractions were assessed based on 3-dimensional panometry plots according to the diameter or direction of repetitive contractions. Occluding or non-occluding contractions were defined as those that were > 6 or ≤ 6 mm from the nadir diameter, respectively. A repetitive contraction was defined when 3 or more contractions occurred in a single direction (Fig. 2).8,21
Figure 2.
An example of the contraction types in functional luminal imaging probe (FLIP) panometry produced using the algorithm used to convert FLIP data to 3-dimensional panometry data developed in this study. The x-axis represents the procedure time (second), the y-axis represents the probe channel, and the z-axis represents the diameter (mm) measured at the probe. (A) Repetitive antegrade contraction 3-dimensional panometry data. (B) Repetitive retrograde contraction 3-dimensional panometry data. (C) Other contractility 3-dimensional panometry data. (D) Contractility-absent 3-dimensional panometry data.
Flip tomography motility classification was based on the study by Carlson et al.8 Reduced EGJ opening (REO) was defined as EGJ-DI < 3.0 mm2/mmHg.
Outcomes
The primary outcome was treatment success defined as a post-POEM symptom score (Eckardt symptom score) ≤ 3 (reference Eckardt score).22
Secondary outcomes assessed before and after POEM included the following: the gastroesophageal reflux disease questionnaire (GerdQ), basal LES pressure, IRP, POC based on HRM findings, procedure time, length of myotomy, EGJ-DI, and follow-up panometry.16
Definition of Presence of Contractility After Peroral Endoscopic Myotomy
Post-POEM peristalsis was classified as a weak contractility, premature contractility, or failed contractility according to a previous study based on the Chicago classification.7,16 POC was defined when weak and premature contractility were observed in follow-up HRM. The definition of a failed contractility was minimal (< 3 cm) integrity of the 20-mmHg isobaric contour distal to the proximal pressure trough; a weak contractility was defined based on a large (> 5 cm in length) or small (2-5 cm in length) break in the 20-mmHg isobaric contour. A premature contractility was defined as weak peristalsis with a small break and distal latency < 4.5 seconds (Supplementary Figure).
Statistical Methods
Descriptive statistics were expressed as mean ± standard deviation for continuous variables and as number (proportion) for categorical variables. The Kruskal–Wallis test was used to compare continuous variables between the subtypes of achalasia or the FLIP topography classification. Fisher’s exact test was used to compare categorical variables between the subtypes of achalasia or the FLIP topography classification. The t test was used to compare variables between the “with POC” and “without POC” groups. A P-value < 0.05 (two-tailed) was considered to be statistically significant.
All statistical analyses were performed using SPSS version 21.0 (IBM Corp, Armonk, NY, USA).
Results
General Characteristics of Patients
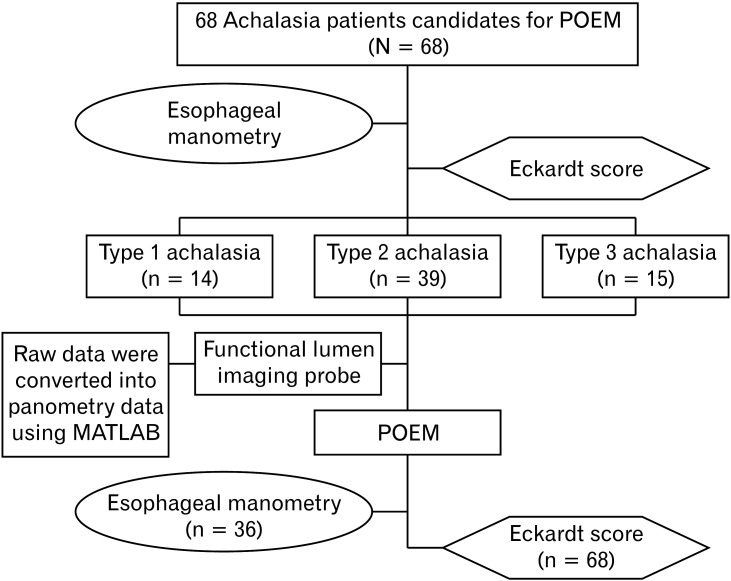
A total of 68 patients, including 33 men and 35 women, with a mean age of 52 ± 17 years, who had undergone POEM and had follow-up Eckardt score data were included in the analysis. Table 1 summarizes the patient characteristics at baseline. Table 2 summarizes FLIP topography and the motility classification as per the manometric motility diagnosis. Thirty-six of 68 patients attended follow-up HRM after POEM (Fig. 3). The median follow-up length of HRM and surveys after POEM was 205 days (interquartile range: 25th-75th percentile, 34-304 days).
Table 1.
General Characteristics According to the High-resolution Manometry Motility Diagnosis
| Variables | Type I achalasia | Type II achalasia | Type III achalasia | P-value |
|---|---|---|---|---|
| Number | 14 | 39 | 15 | |
| Age (yr) | 50.0 ± 14.8 | 49.8 ± 17.5 | 61.8 ± 13.1 | 0.045 |
| Male | 6 (43) | 21 (55) | 6 (40) | 0.594 |
| BMI (kg/m2) | 21.2 ± 4.3 | 22.2 ± 3.5 | 21.4 ± 3.1 | 0.355 |
| Median IRP (mmHg) | 20.0 ± 0.0 | 34.2 ± 13.9 | 33.2 ± 10.9 | 0.011 |
| Basal EGJ pressure (mmHg) | 14.0 ± 1.0 | 42.0 ± 19.4 | 53.1 ± 32.9 | 0.008 |
| Eckardt score | 6.4 ± 1.9 | 6.8 ± 2.4 | 5.8 ± 2.0 | 0.369 |
| EGJ-DI (mm2/mmHg) | 2.3 ± 1.6 | 1.4 ± 0.9 | 1.6 ± 1.1 | 0.278 |
| Myotomy length (cm) | 11.6 ± 2.5 | 11.5 ± 2.8 | 12 ± 2.2 | 0.811 |
| Procedure time (min) | 78.3 ± 22.9 | 75.4 ± 26.1 | 75 ± 20.5 | 0.804 |
BMI, body mass index; IRP, integrated relaxation pressure; EGJ, esophagogastric junction; EGJ-DI, EGJ-distensibility index.
Data are presented as mean ± SD or n (%).
Table 2.
Functional Luminal Imaging Probe Topography Motility Classification According to the Manometric Motility Diagnosis
| HRM motility diagnosis | No. of cases | FLIP topography motility classification | |||
|---|---|---|---|---|---|
| REO with retrograde contractile response | REO with absent contractile response | REO with normal contractile response | Retrograde contractile response | ||
| Type I achalasia | 14 | 7 (50.0) | 0 (0.0) | 2 (14.3) | 5 (35.7) |
| Type II achalasia | 39 | 28 (71.8) | 2 (5.1) | 6 (15.4) | 3 (7.7) |
| Type III achalasia | 15 | 8 (53.3) | 3 (20.0) | 3 (20.0) | 1 (6.7) |
HRM, high-resolution manometry; FLIP, functional luminal imaging probe; REO, reduced esophagogastric junction opening.
Data are presented as n (%).
Figure 3.
Flow diagram of the patient allocation process. POEM, peroral endoscopic myotomy.
Primary Outcome
Of the 68 patients with achalasia, 14 (20.6%) had type I, 39 (57.4%) had type II, and 15 (22.1%) had type III. However, the mean baseline Eckardt score was 6.48 ± 2.20. Two of the 68 patients showed improvement of symptoms in terms of the Eckardt score, although the scores did not fall below a cutoff value of 3 despite POEM. There was no statistically significant difference between the pre- and post-Eckardt scores according to the achalasia subtypes (P = 0.605, Table 3). Moreover, there was no statistical significance between the Eckardt score and types of FLIP panometry diagnoses (P = 0.854, Table 3). There were significant differences between pre- and post-POEM EGJ-DI values (1.6 ± 1.1 vs 8.8 ± 5.0, P < 0.01).
Table 3.
Functional Luminal Imaging Probe Panometry, Achalasia Subtypes, and Eckardt Scores Before and After Peroral Endoscopic Myotomy
| Variables | No. of cases | Pre-POEM Eckardt score | Post-POEM Eckardt score | P-value |
|---|---|---|---|---|
| Achalasia subtypes | 0.605 | |||
| Type I achalasia | 14 | 6.43 ± 1.95 | 1.57 ± 1.28 | |
| Type II achalasia | 39 | 6.77 ± 2.34 | 1.21 ± 1.17 | |
| Type III achalasia | 15 | 5.80 ± 1.97 | 0.67 ± 0.82 | |
| FLIP topography classification | 0.854 | |||
| REO with retrograde contractile response | 43 | 6.32 ± 2.37 | 0.90 ± 1.01 | |
| REO with absent contractile response | 5 | 6.80 ± 2.86 | 1.60 ± 1.14 | |
| REO with normal contractile response | 11 | 6.82 ± 2.13 | 1.36 ± 1.57 | |
| Retrograde contractile response | 9 | 6.67 ± 1.00 | 1.89 ± 0.92 |
POEM, peroral endoscopic myotomy; FLIP, functional luminal imaging probe; REO, reduced esophagogastric junction opening.
Data are presented as mean ± SD.
Secondary Outcome
Presence of contractility after peroral endoscopic myotomy
A total of 36 patients, comprised of 18 men and 18 women, with a mean age of 53 ± 15 years, underwent follow-up HRM to determine the presence/absence of contractility after POEM. Twenty-four patients showed contractility after POEM, whereas 12 patients did not.
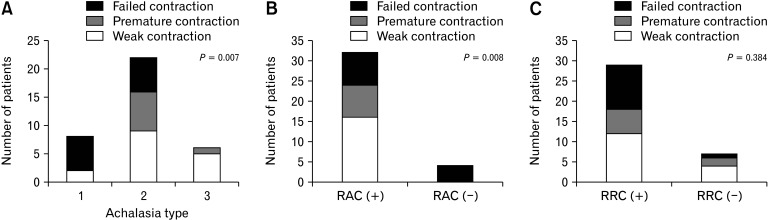
Supplementary Figure illustrates the patterns of POC after POEM. A total of 24 patients who had POC after POEM also had repetitive antegrade contractions (RACs). However, among the 12 patients without POC after POEM, 8 patients showed RACs. The prevalence of POC was significantly higher in patients with RAC than in those without RAC (with POC group: 24/24 patients showed RACs; without POC group: 8/12 patients showed RACs, P = 0.008, Table 4 and Fig. 4). Repetitive retrograde contractions (RRCs) were observed in 18 of 24 patients with POC and in 11 of 12 patients without POC. There was no significant relationship between RRCs and contractility (with POC group: 18/24 patients with RRCs; without POC group: 11/12 patients with RRCs, P = 0.384, Table 4 and Fig. 4).
Table 4.
Comparison of Variables Between the “Without Presence of Contractility” and “With Presence of Contractility” Groups
| Variables | Without POC group (n = 12) | With POC group(n = 24) | P-value |
|---|---|---|---|
| LES pressure (mmHg) | 38.2 ± 16.6 | 40.7 ± 14.0 | 0.638 |
| IRP pressure (mmHg) | 29.1 ± 14.0 | 32.3 ± 10.5 | 0.446 |
| Myotomy length (cm) | 10.7 ± 4.5 | 15.8 ± 9.0 | 0.281 |
| Procedure time (min) | 84.7 ±32.4 | 71.8 ± 21.5 | 0.165 |
| Achalasia type | 0.007 | ||
| Type I achalasia | 6 | 2 | |
| Type II achalasia | 6 | 16 | |
| Type III achalasia | 0 | 6 | |
| RAC | 0.008 | ||
| RAC (–) | 4 | 0 | |
| RAC (+) | 8 | 24 | |
| RRC | 0.384 | ||
| RRC (–) | 1 | 6 | |
| RRC (+) | 11 | 18 | |
| FLIP topography classification | 0.128 | ||
| REO with retrograde contractile response | 7 | 17 | |
| REO with absent contractile response | 0 | 2 | |
| REO with normal contractile response | 1 | 4 | |
| Retrograde contractile response | 4 | 1 | |
| Pre-POEM Eckardt score | 6.00 ± 2.30 | 6.88 ± 2.58 | 0.327 |
| Post-POEM Eckardt score | 1.08 ± 0.10 | 1.29 ± 1.43 | 0.654 |
POC, presence of contractility; LES, lower esophageal sphincter; IRP, integrated relaxation pressure; RAC, repetitive antegrade contraction; RRC, repetitive retrograde contraction; FLIP, functional luminal imaging probe; EGJ-DI, esophagogastric junction–distensibility index; POEM, peroral endoscopic myotomy.
Data are presented as mean ± SD or n.
Figure 4.
(A) Number of patients with the presence of contractility after peroral endoscopic myotomy (POEM) in achalasia subtypes. (B) The number of patients with presence of contractility (POC) after POEM in the repetitive antegrade contractions (RACs) group. (C) The number of patients with POC after POEM in the repetitive retrograde contractions group.
Among the patients who had POC after POEM, 2 (8.0%) had type I, 16 (67.0%) had type II, and 6 (25.0%) had type III. Among those without POC after POEM, 6 (50.0%) had type I and 6 (50.0%) had type II. There were significant differences among the types of achalasia in POC (P = 0.007, Table 4 and Fig. 4). The panometry analysis based on the 2019 criteria did not show clinical significance with respect to POC (P = 0.128, Table 4).
After POEM, FLIP panometry was measured. However, no significant repetitive pattern of contraction was observed.
Peroral endoscopic myotomy procedure-related parameters
We investigated the relationship between clinical outcomes and procedure-related parameters (myotomy length and procedure time). There was no significant association between Eckardt scores and myotomy length (11.6 ± 2.6 cm with symptomatic improvement vs 11.5 ± 2.1 cm without symptomatic improvement; P = 0.897) or between Eckardt scores and procedure time (75.9 ± 24.1 minutes with symptomatic improvement vs 81.2 ± 31.7 minutes without symptomatic improvement; P = 0.401).
As for POC, there was no significant association between POC and the myotomy length (15.8 ± 9.0 cm with POC vs 10.7 ± 4.5 cm without POC; P = 0.281) or between POC and procedure time (84.7 ± 32.4 vs 71.8 ± 21.5 minutes; P = 0.165).
Gastroesophageal reflux disease questionnaire
The follow-up GerdQ was completed by 32 patients. Most patients scored less than 8, and 1 patient scored 8. There were no significant differences among achalasia subtypes in the number of patients who completed the GerdQ (7 in type I, 19 in type II, and 6 in type III; P = 0.878). Moreover, there were no significant differences between the panometry pattern and GerdQ (20 in REO with retrograde contractile response, 2 in REO with absent contractile response, 5 in REO with normal contractile response, and 5 in retrograde contractile response; P = 0.599).
Discussion
All of the patients with achalasia who had undergone POEM showed significant symptomatic improvement. POC was significantly higher in those with RAC and achalasia type II.
All manometric subtypes of achalasia in our study showed symptomatic improvement, in line with a previous report by Kim et al.3 In previous studies, achalasia was effectively identified using real-time FLIP panometry to evaluate esophageal motility.8,14,21 However, the predictive value of FLIP panometry had no statistical significance.21 In contrast, our results showed an association with FLIP panometry pattern in the clinical course after POEM in patients with achalasia.
RACs obtained using panometry showed a predictive value for the presence of contractility after POEM in patients with achalasia. RAC is a normal physiological secondary peristalsis of the esophagus, and its presence in achalasia indicates remaining esophageal function in patients with achalasia.
In patients with achalasia, functional recovery was observed in the distal esophagus after POEM; this suggests that impaired neuronal function limited to the LES may be prominent in some patients with achalasia.16 In our study, the presence of RAC, and achalasia subtypes had an association with POC after POEM in patients with achalasia.
Other papers reported POC in some patients with achalasia after myotomy. Roman et al16 reported that weak peristalsis after myotomy was usually characterized by a large (> 5 cm in length) or small (2-5 cm in length) break in the 20-mmHg isobaric contour, and premature contractions were characterized as distal latency < 4.5 seconds.
As the presence of peristalsis was associated with improved symptomatic and radiographic outcomes,23 Carlson et al14 mentioned that patients with achalasia with RACs before POEM may be more likely to show presence of peristalsis. Our study concluded that RACs were associated with presence of contractility after POEM.
Other intraoperative EndoFLIP studies on panometry included fewer than 50 patients and were conducted in the same hospital that invented panometery.24-26 However, our study is meaningful as it included the largest number of patients among intraoperative EndoFLIP panometry studies to date.
This study had a limitation. We analyzed topography using specialized software, which is not widely available. However, the data and profile obtained from this panometry pattern are technically comparable to those from other studies.8,20
In conclusion, this study demonstrated that the presence of RACs and the panometry pattern have an association with POC after POEM. These parameters may reflect pathogenic features or the degree of neurodegeneration.
Supplementary Material
Note: To access the supplementary figure mentioned in this article, visit the online version of Journal of Neurogastroenterology and Motility at http://www.jnmjournal.org/, and at https://doi.org/10.5056/jnm21186.
Footnotes
Financial support: This study was financially supported by a grant of the Korean Society of Neurogastroenterology and Motility (KSNM-20-02).
Conflicts of interest: None.
Author contributions: Kee Wook Jung: conceptualization and methodology; Li-Chang Hsing and KyungMin Choi: data curation, formal analysis, and manuscript drafting; Segyeong Joo and KyungMin Choi: prepared the MALTLAB formula and analyzed the manometric data; Nayoung Kim: statistical analyses; and Ga Hee Kim, Hee Kyong Na, JeongHoon Lee, Ji Yong Ahn, Do Hoon Kim, Kee Don Choi, Ho June Song, Gin Hyug Lee, and Hwoon-Yong Jung: supervised the study and provided important intellectual contributions.
References
- 1.Werner YB, Hakanson B, Martinek J, et al. Endoscopic or surgical myotomy in patients with idiopathic achalasia. N Engl J Med. 2019;381:2219–2229. doi: 10.1056/NEJMoa1905380. [DOI] [PubMed] [Google Scholar]
- 2.Ponds FA, Fockens P, Lei A, et al. Effect of peroral endoscopic myotomy vs pneumatic dilation on symptom severity and treatment outcomes among treatment-naive patients with achalasia: a randomized clinical trial. JAMA. 2019;322:134–144. doi: 10.1001/jama.2019.8859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim GH, Jung KW, Jung HY, et al. Superior clinical outcomes of peroral endoscopic myotomy compared with balloon dilation in all achalasia subtypes. J Gastroenterol Hepatol. 2019;34:659–665. doi: 10.1111/jgh.14616. [DOI] [PubMed] [Google Scholar]
- 4.Ghosh SK, Pandolfino JE, Rice J, Clarke JO, Kwiatek M, Kahrilas PJ. Impaired deglutitive EGJ relaxation in clinical esophageal manometry: a quantitative analysis of 400 patients and 75 controls. Am J Physiol Gastrointest Liver Physiol. 2007;293:G878–G885. doi: 10.1152/ajpgi.00252.2007. [DOI] [PubMed] [Google Scholar]
- 5.Pandolfino JE, Ghosh SK, Rice J, Clarke JO, Kwiatek MA, Kahrilas PJ. Classifying esophageal motility by pressure topography characteristics: a study of 400 patients and 75 controls. Am J Gastroenterol. 2008;103:27–37. doi: 10.1111/j.1572-0241.2007.01532.x. [DOI] [PubMed] [Google Scholar]
- 6.Pandolfino JE, Kwiatek MA, Nealis T, Bulsiewicz W, Post J, Kahrilas PJ. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology. 2008;135:1526–1533. doi: 10.1053/j.gastro.2008.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ International High Resolution Monometry Working Group, author. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24(suppl 1):57–65. doi: 10.1111/j.1365-2982.2011.01834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carlson DA, Gyawali CP, Kahrilas PJ, et al. Esophageal motility classification can be established at the time of endoscopy: a study evaluating real-time functional luminal imaging probe panometry. Gastrointest Endosc. 2019;90:915–923. e1. doi: 10.1016/j.gie.2019.06.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carlson DA, Kou W, Lin Z, et al. Normal values of esophageal distensibility and distension-induced contractility measured by functional luminal imaging probe panometry. Clin Gastroenterol Hepatol. 2019;17:674–681. e1. doi: 10.1016/j.cgh.2018.07.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kwiatek MA, Pandolfino JE, Hirano I, Kahrilas PJ. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP) Gastrointest Endosc. 2010;72:272–278. doi: 10.1016/j.gie.2010.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rohof WO, Hirsch DP, Kessing BF, Boeckxstaens GE. Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology. 2012;143:328–335. doi: 10.1053/j.gastro.2012.04.048. [DOI] [PubMed] [Google Scholar]
- 12.Pandolfino JE, de Ruigh A, Nicodème F, Xiao Y, Boris L, Kahrilas PJ. Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP™) in achalasia patients. Neurogastroenterol Motil. 2013;25:496–501. doi: 10.1111/nmo.12097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Smeets FG, Masclee AA, Keszthelyi D, Tjwa ET, Conchillo JM. Esophagogastric junction distensibility in the management of achalasia patients: relation to treatment outcome. Neurogastroenterol Motil. 2015;27:1495–1503. doi: 10.1111/nmo.12651. [DOI] [PubMed] [Google Scholar]
- 14.Carlson DA, Lin Z, Kahrilas PJ, et al. The functional lumen imaging probe detects esophageal contractility not observed with manometry in patients with achalasia. Gastroenterology. 2015;149:1742–1751. doi: 10.1053/j.gastro.2015.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Campagna RAJ, Carlson DA, Hungness ES, et al. Intraoperative assessment of esophageal motility using FLIP during myotomy for achalasia. Surg Endosc. 2020;34:2593–2600. doi: 10.1007/s00464-019-07028-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roman S, Kahrilas PJ, Mion F, et al. Partial recovery of peristalsis after myotomy for achalasia: more the rule than the exception. JAMA Surg. 2013;148:157–164. doi: 10.1001/2013.jamasurg.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Foisy H, Pioche M, Chabrun E, et al. Role of rapid drink challenge during esophageal high-resolution manometry in predicting outcome of peroral endoscopic myotomy in patients with achalasia. J Neurogastroenterol Motil. 2020;26:204–214. doi: 10.5056/jnm19135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pandolfino JE, Ghosh SK, Zhang Q, Jarosz A, Shah N, Kahrilas PJ. Quantifying EGJ morphology and relaxation with high-resolution manometry: a study of 75 asymptomatic volunteers. Am J Physiol Gastrointest Liver Physiol. 2006;290:G1033–G1040. doi: 10.1152/ajpgi.00444.2005. [DOI] [PubMed] [Google Scholar]
- 19.Jung KW, Jung HY, Myung SJ, et al. The effect of age on the key parameters in the Chicago classification: a study using high-resolution esophageal manometry in asymptomatic normal individuals. Neurogastroenterol Motil. 2015;27:246–257. doi: 10.1111/nmo.12482. [DOI] [PubMed] [Google Scholar]
- 20.Carlson DA, Hirano I. Application of the gunctional lumen imaging probe to esophageal disorders. Curr Treat Options Gastroenterol. 2017;15:10–25. doi: 10.1007/s11938-017-0116-4. [DOI] [PubMed] [Google Scholar]
- 21.Carlson DA, Kahrilas PJ, Lin Z, et al. Evaluation of esophageal motility utilizing the functional lumen imaging probe. Am J Gastroenterol. 2016;111:1726–1735. doi: 10.1038/ajg.2016.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eckardt VF, Aignherr C, Bernhard G. Predictors of outcome in patients with achalasia treated by pneumatic dilation. Gastroenterology. 1992;103:1732–1738. doi: 10.1016/0016-5085(92)91428-7. [DOI] [PubMed] [Google Scholar]
- 23.Nicodème F, de Ruigh A, Xiao Y, et al. A comparison of symptom severity and bolus retention with Chicago classification esophageal pressure topography metrics in patients with achalasia. Clin Gastroenterol Hepatol. 2013;11:131–137. doi: 10.1016/j.cgh.2012.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Attaar M, Su B, Wong HJ, et al. Intraoperative impedance planimetry (EndoFLIP™) results and development of esophagitis in patients undergoing peroral endoscopic myotomy (POEM) Surg Endosc. 2021;35:4555–4562. doi: 10.1007/s00464-020-07876-y. [DOI] [PubMed] [Google Scholar]
- 25.Holmstrom AL, Campagna RAJ, Cirera A, et al. Intraoperative use of FLIP is associated with clinical success following POEM for achalasia. Surg Endosc. 2021;35:3090–3096. doi: 10.1007/s00464-020-07739-6. [DOI] [PubMed] [Google Scholar]
- 26.Holmstrom AL, Campagna RAJ, Alhalel J, et al. Intraoperative FLIP distensibility during POEM varies according to achalasia subtype. Surg Endosc. 2021;35:3097–3103. doi: 10.1007/s00464-020-07740-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.