Abstract
Objective: To clarify the influence of obstructive sleep apnea (OSA) on postoperative cognitive dysfunction (POCD) in elderly patients undergoing joint replacement. Methods: This study retrospectively enrolled130 patients who underwent joint replacement in the Department of Orthopaedics of Taizhou Municipal Hospital between January 2019 and March 2021 for analysis. According to polysomnography (PSG) results, 80 patients without OSA were included in group A and 50 with OSA were assigned to group B. The two groups were compared with respect to the following items: surgical indications (length of stay (LOS), intraoperative blood loss (IBL) and operation time (OT), incidence of postoperative delirium (POD), postoperative cognitive function (Mini-mental State Examination, MMSE), neurological function recovery (National Institutes of Health Stroke Scale, NIHSS) and (Scandinavian Stroke Scale, SSS)), mental health (Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS)), compliance, overall response rate (ORR), complications and patient satisfaction. Results: The LOS and OT were shorter, and the IBL was less in group A compared with those in group B. Group A also showed reduced NIHSS and SSS scores as well as SAS and SDS scores when compared with group B. In addition, lower incidence of POD, and higher compliance, ORR and satisfaction were observed in group A than in group B. In terms of cognitive function, although the MMSE score in both groups decreased after surgery, patients in group B had a lower MMSE score and a milder form of POCD. Conclusions: OSA may affect the postoperative cognitive function and adversely influence the treatment outcome of elderly patients undergoing joint replacement.
Keywords: Obstructive sleep apnea, joint replacement, cognitive dysfunction, NIHSS, SSS, psychology, delirium
Introduction
Joint replacement is one of the most successful orthopedic procedures in the world, frequently used for primary and secondary osteoarthritis, osteonecrosis and intractable hip pain caused by rheumatoid arthritis [1]. With the progression of population aging, the number of patients undergoing the procedure is increasing at an accelerating rate [2,3]. Among all kinds of orthopedic inflammation, joint replacement can effectively relieve pain and improve patient mobility [4]. However, this technique requires highly professional skills, and improper operations will bring a series of postoperative complications or even cause death in serious cases [5,6]. Besides, orthopedic surgeries not only predispose patients to postoperative infections, but also adversely influence their postoperative mental state [7,8]. Before surgery, are there any other factors affecting surgery outcomes? In this study, we explored the effect of obstructive sleep apnea (OSA) in patients undergoing joint replacement surgery.
OSA, commonly seen in the elderly, increases with age in adults [9,10]. OSA is defined as repetitive cycles of upper airway collapse and sleep arousals that directly result in excessive daytime sleepiness [11]. In addition to excessive daytime sleepiness, hypertension [12], coronary heart disease [13], congestive heart failure [14] and stroke [15] are all closely related to OSA. Further research has found a strong association between OSA and impaired cognitive function, with significant impacts on attention, memory and executive function of patients [16]. For joint replacement that also brings cognitive dysfunction, what impact will it bring if the patient has OSA before surgery? The purpose of this study was to elucidate the influence of OSA in elderly patients undergoing joint replacement by analyzing indicators such as cognitive dysfunction.
Materials and methods
General data
The clinical data of 130 patients who underwent joint replacement in the Orthopedics Department of Taizhou Municipal Hospital from January 2019 to March 2021 were retrospectively analyzed. After polysomnography (PSG), patients were assigned to group A (without OSA; n=80) and group B (with OSA; n=50) according to relevant test results. Inclusion criteria: All patients were confirmed with rheumatoid arthritis [17] and received joint replacement treatment in our hospital; treatment-naive patients with relatively normal mental state and ability to effectively reflect their pain were enrolled. Exclusion criteria: Patients with disease or organ damage corresponding to this treatment, or with preoperative delirium, preoperative abnormal liver and kidney function, mental disorders, depression or Alzheimer’s disease. The patients’ families gave their consent for patients’ participation in this study and signed an informed consent. This study has obtained approval from the Medical Ethics Committee of Taizhou Municipal Hospital.
Methods
The Philips Alice 5 Polysomnography Sleep System (USA) was used to monitor the sleep status of patients. PSG is currently the gold standard for diagnosing OSA/hypopnea syndrome. Alice 5 was used to monitor the electroencephalogram (EEG), electrocardiogram (ECG), electromyography (EMG) of jaw and eye muscles, blood oxygen saturation, nasal and oral respiratory airflow and posture change of patients during sleep for at least 7 hours a night, and simultaneously monitored patients’ sleep condition throughout the night. All participants were prohibited from drinking alcohol, strong tea, coffee and other drinks that affect sleep 24 hours prior to the examination, nor were they allowed to take sleeping drugs. Instead, they were asked to drink as little water as possible after dinner. In addition, excessive facial grease was cleaned, and men had their beards shaved while women had their nail polish removed. The participants were grouped after the test results were obtained. After adequate preoperative preparation, patients in both groups received joint replacement.
Outcome measures
Surgical indications
The length of stay (LOS), intraoperative blood loss (IBL) and operation time (OT) were observed in both groups.
Incidence of postoperative delirium (POD)
The occurrence of postoperative POD in both groups was evaluated using the Confusion Assessment Method (CAM) [18]. The number of patients with POD at one hour, one day and two days after operation was recorded.
Cognitive function
The cognitive function of patients before and after treatment was evaluated by the Mini-mental State Examination (MMSE) [19].
Neurological function and mental health
The National Institute of Health stroke scale (NIHSS) [20] and Scandinavian Stroke Scale (SSS) [21] were adopted to evaluate the neurological function recovery of the patients. The degree of neurological recovery was inversely proportional to the score. The Self-Rating Anxiety Scale (SAS) and Self-Rating Depression Scale (SDS) [22,23], both containing 20 items with a full score of 100 points, were used to evaluate the mental health of patients in the two groups before and one month after treatment. The mental health of patients was negatively associated with the score.
Compliance
Patient compliance was compared between the two groups. If the patient took the initiative to strictly implement the doctor’s advice, actively cooperated with the clinical examination and investigation, and consciously adhered to the long-term standardized treatment, it was regarded as complete compliance. Partial compliance was indicated if the patient occasionally did not comply with the standard behavior during treatment, but was able to follow the doctor’s advice after being reminded or explained. If the patient did not follow the doctor’s advice for a long time during the treatment, or refused or discontinued the treatment midway, it was considered as non-compliance.
Overall response rate (ORR)
The clinical effects of the two groups were observed. Markedly effective is translated in successful operation, with no complications, postoperative bleeding, secondary injury or other adverse events. Effective corresponds to basically successful operation with minor complications. Ineffective is indicated if the operation was unsuccessful with complications and other adverse events. ORR = (markedly effective + effective) cases/total cases * 100%.
Complications
Postoperative complications, including nausea and vomiting, nerve injury, and POD were recorded and compared between the two groups.
Patient satisfaction
Patients’ satisfaction with the treatment was assessed using the treatment satisfaction questionnaire designed by our hospital, and the scores were compared between the two groups. On the 100-point scale, a score of 85-100, ≥60 and <60 points indicated satisfied, basically satisfied and dissatisfied, respectively.
Statistical methods
The sample size of this study was calculated using PASS 15.0 (NCSS Statistical Software, Kaysville, Utah) through the normal approximation method. Bilateral test level α=0.05 was used to conduct preliminary analysis of the data. Assuming that the overall response rate of the treatment group (Group A) was 97%, and that of the control group was 76%, and 80% power was required, the sample size of each group should be at least 38 cases in each group, with 76 cases in total. Based on a 20% dropout rate, at least 48 cases should be included in each group, a total of 96 cases.
This study used SPSS 22.0 (Asia Analytics Formerly SPSS China) for comprehensive data statistical analysis. Categorical materials were analyzed by the χ2 test. Quantitative materials were given (x̅ ± s), and the inter-group comparison adopted the independent samples t-test, paired t-test for comparison at different time periods within groups, expressed as t. GraphPad Prism 8 software was used for plotting the experimental images. P<0.05 suggests the difference is statistically significant.
Results
General data
The comparison of patient general information revealed no significant difference in sex, age, body mass index, smoking history and drinking history between the two groups (P>0.05, Table 1).
Table 1.
General information of patients in the two groups
| Classification | Group A (n=80) | Group B (n=50) | t/χ2 | P |
|---|---|---|---|---|
| Sex | 0.11 | 0.739 | ||
| Male | 44 (55.00) | 26 (52.00) | ||
| Female | 36 (45.00) | 24 (48.00) | ||
| Age (years) | 68.90±4.79 | 69.29±3.49 | 0.50 | 0.619 |
| BMI (kg/m2) | 24.97±3.56 | 25.09±3.43 | 0.19 | 0.850 |
| Mean course of disease (months) | 31.55±3.76 | 30.87±4.13 | 0.97 | 0.336 |
| Smoking | 0.09 | 0.765 | ||
| Yes | 54 (67.50) | 35 (70.00) | ||
| No | 26 (32.50) | 15 (30.00) | ||
| Drinking | 0.69 | 0.492 | ||
| Yes | 48 (60.00) | 33 (66.00) | ||
| No | 32 (40.00) | 17 (34.00) | ||
| Hypertension | 0.26 | 0.612 | ||
| Yes | 46 (57.50) | 31 (62.00) | ||
| No | 34 (42.50) | 19 (38.00) | ||
| Diabetes mellitus | 0.20 | 0.657 | ||
| Yes | 40 (50.00) | 27 (54.00) | ||
| No | 40 (50.00) | 23 (46.00) |
BMI: body mass index.
Surgical indications
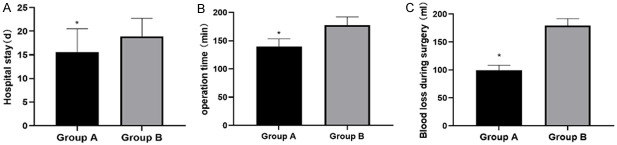
Comparing the surgical indications between the two groups, it was found that the LOS and OT were shorter and the IBL was less in group A compared with those group B (all P<0.05, Figure 1).
Figure 1.
Surgical indications of patients in two groups. A. Hospital stay: the hospital stay of patients in group A was significantly shorter than that in group B (P<0.05). B. Operation time: The operation time in group A was significantly shorter than that in group B (P<0.05). C. Intraoperative blood loss: the amount of intraoperative blood loss in group A was significantly lower than that in group B (P<0.05). Note: *P<0.05 vs. group B.
Group A had a lower incidence of POD
The incidence of POD in group A was significantly lower than that in group B (P<0.05, Table 2). The results indicate group A had better mental state, neurological function and mental function of after treatment than group B.
Table 2.
Incidence of postoperative delirium in the two groups
| Classification | Group A (n=80) | Group B (n=50) | χ2 | P |
|---|---|---|---|---|
| One hour after operation | 0 | 1 | - | - |
| One day after operation | 2 | 4 | - | - |
| Two days after operation | 2 | 5 | - | - |
| Incidence of postoperative delirium | 4 (5.00) | 10 (20.00) | 7.20 | 0.007 |
Group A had better cognitive function after surgery
The MMSE score, which showed no significant difference between groups A and B before operation (P>0.05), was reduced in both groups after operation, with a lower score in group A (P<0.05, Figure 2). This indicates that group A had better postoperative cognitive function recovery than group B.
Figure 2.
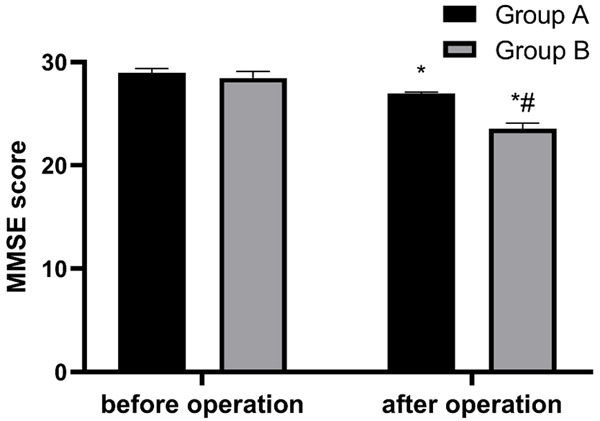
MMSE score of cognitive function of patients in two groups. There was no significant difference in cognitive function between the two groups before operation (P>0.05). After operation, the MMSE score decreased significantly in both groups, and the score in group A was significantly lower than that in group B (P<0.05). Note: *P<0.05 vs. after treatment; #P<0.05 vs. group A. MMSE, Mini-mental State Examination.
Group A had better postoperative neurological function and mental state recovery
The NIHSS, SSS, SAS and SDS scores were investigated in both groups. It was found that these scores were not significantly different between the two groups before operation (P>0.05); After operation, the scores decreased statistically in both groups and were lower in group A compared with those in group B (P<0.05, Figure 3).
Figure 3.
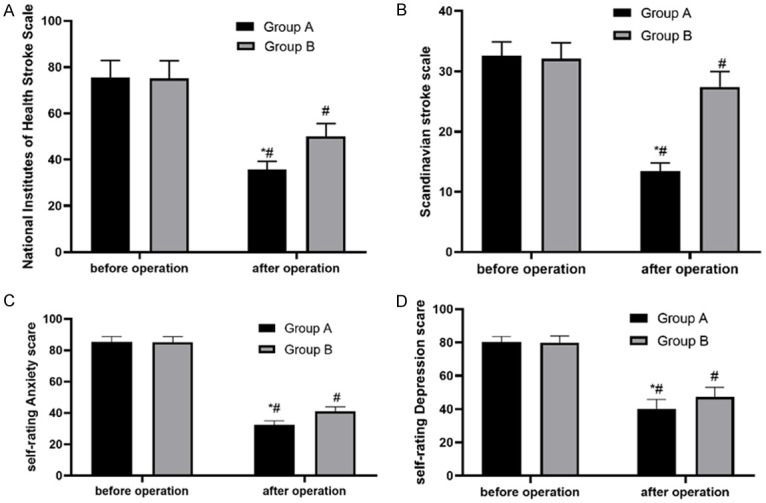
Neurological function and mental health of patients in two groups. A. NIHSS score: There were significant changes in NIHSS scores between the two groups after operation, and the score in group A was significantly lower than that in group B (P<0.05). B. SSS score: There were significant changes in SSS scores between the two groups after operation, and the score in group A was significantly lower than that in group B (P<0.05). C. SAS score: There were significant changes in SAS scores between the two groups after operation, and the score in group A was significantly lower than that in group B (P<0.05). D. SDS score: There were significant changes in SDS scores between the two groups after operation, and the score in group A was significantly lower than that in group B (P<0.05). Note: #P<0.05 vs. after operation; *P<0.05 vs. group B. NIHSS: National Institutes of Health Stroke Scale; SSS: Scandinavian Stroke Scale; SAS: Self-Rating Anxiety Scale; SDS: Self-Rating Depression Scale.
Group A had higher compliance during treatment
After statistically comparing the total compliance rate between the two groups, it was found that the total compliance rate was significantly higher in group A compared with that in group B (P<0.05, Table 3). This suggests that group A cooperated better during the treatment than group B.
Table 3.
Treatment compliance of patients in two groups
| Classification | Group A (n=80) | Group B (n=50) | χ2 | P |
|---|---|---|---|---|
| Complete compliance | 52 (65.00) | 23 (46.00) | - | - |
| Partial compliance | 24 (30.00) | 15 (30.00) | - | - |
| Non-compliance | 4 (5.00) | 12 (24.00) | - | - |
| Total compliance rate (%) | 76 (95.00) | 38 (76.00) | 10.29 | 0.001 |
Group A had a higher ORR
A statistically higher ORR was determined in group A compared with that in group B (P<0.05, Table 4). Suggesting that the condition of patients in group A made it easier to improve the treatment efficacy.
Table 4.
Overall response rate of two groups of patients
| Classification | Group A (n=80) | Group B (n=50) | χ2 | P |
|---|---|---|---|---|
| Markedly effective | 50 (62.50) | 22 (44.00) | - | - |
| Effective | 28 (35.00) | 17 (34.00) | - | - |
| Ineffective | 2 (2.50) | 11 (22.00) | - | - |
| Overall response rate (%) | 78 (97.50) | 39 (78.00) | 13.00 | <0.001 |
Group A had a lower incidence of complications
The incidence of complications in group A was significantly lower than that in group B (P<0.05, Table 5). This shows that the status of patients in group A made the same treatment method less prone to complications and was safer.
Table 5.
Incidence of complications in two groups
| Classification | Group A (n=80) | Group B (n=50) | χ2 | P |
|---|---|---|---|---|
| Nausea and vomiting (%) | 2 (2.50) | 4 (8.00) | ||
| Headache (%) | 0 (0.00) | 3 (6.00) | ||
| Nerve injury (%) | 0 (0.00) | 3 (6.00) | ||
| Postoperative delirium (%) | 0 (0.00) | 2 (4.00) | ||
| Incidence of complications | 2 (2.50) | 12 (24.00) | 14.80 | <0.001 |
Group A had higher treatment satisfaction
Comparing the satisfaction of the two groups, it was found that the satisfaction of patients in group A was significantly higher than that in group B (P<0.05, Table 6). This shows that patients in group A were more satisfied with the treatment process.
Table 6.
Patient satisfaction in two groups
| Classification | Group A (n=80) | Group B (n=50) | χ2 | P |
|---|---|---|---|---|
| Satisfied | 48 (60.00) | 20 (40.00) | - | - |
| Basically satisfied | 26 (32.50) | 16 (30.00) | - | - |
| Dissatisfied | 6 (7.50) | 14 (28.00) | - | - |
| Total satisfaction (%) | 74 (92.50) | 36 (72.00) | 9.93 | 0.002 |
Discussion
In patients undergoing orthopedic operations, mental diseases such as POD and common mental stress not only affect the recovery of patients directly leading to prolonged LOS, but also easily impact patients’ cognition [24]. Without proper treatment, OSA can cause cognitive impairment and increased risk of work-related accidents and motor vehicle accidents [25]. In this section, we will discuss the influence of OSA on joint replacement surgery based on the results obtained.
First, the incidence rates of POCD and POD were analyzed. A statistically lower incidence of POD was determined in group A. Despite the presence of certain POCD in both groups, the incidence was significantly lower in group A compared with that in group B. As aforementioned, 50 patients in group B had OSA, while 80 patients in group A had no such disease. OSA is characterized by repeated partial or complete collapse of the upper respiratory tract during sleep, which results in changes in alveolar ventilation, intermittent hypoxemia, increased breathing effort and fluctuations of negative pressure in the chest cavity, causing the patient to wake up during sleep and consequently leading to sleep disruption and fragmented sleep [26]. OSA is associated with an increased risk of developing a wide range of end-organ diseases, outbreaks of inflammation and cardiovascular or metabolic diseases, which can significantly affect patients’ cognition [27,28]. Delirium is a neurological disease with incomplete pathophysiological research. When it occurs, there will always be multi-factor syndromes similar to acute brain failure and acute heart failure. Hence, delirium is closely related to brain function and is also the primary culprit of dementia caused by the decline of patients’ cognitive ability [29]. Orthopedic surgery, however, inevitably brings these problems and leads to cognitive impairment [30]. Combined with the above, it is apparent that patients in group B would have higher cognitive impairment without joint replacement surgery. After knee replacement surgery, the cognitive function of patients in group B, which was already affected to some extent, would be further impaired, and the incidence of POD would be further increased with a series of effects brought by the existing OSA.
From the perspective of neurological and psychological function, the scores of neurological function and depression and anxiety in group A were lower than those in group B. So, it is obvious that the neurological function of group B was worse than that of group A due to the damage caused by OSA to the patients’ nervous system and organs including the brain [27], and acute brain failure caused by delirium [29]. There is a close association between psychological conditions (such as anxiety and depression) and nervous system damage. Following the injury of the patient’s nervous system, there can be ischemic injury and the resulting inflammatory reaction, which could cause vasoconstriction and decreased blood flow, further damaging the nerve function and body function thereby leading to anxiety and depression in patients [31]. Without sound psychological counseling to channel the depressed mood of patients, these negative psychological emotions can form a vicious circle with various diseases [32]. In this study, the neurological function of patients in group B was significantly improved after joint replacement, but the recovery was far worse than that of patients in group A. As a result, the ORR in group B was lower and a series of surgical indications were inferior to those of group A. In short, for patients undergoing joint replacement, the postoperative cognitive function recovery and the therapeutic effect can be compromised in those with OSA.
Due to the limitations of time and equipment, some important indicators, such as inflammatory factors, patients’ quality of life and postoperative limb function, were not studied. In future clinical research, we will continue to detect and investigate these indicators, and constantly explore the harm of OSA to patients after operation to seek a solution.
In summary, OSA may affect the postoperative cognitive function and adversely affect the treatment outcome in elderly patients undergoing joint replacement. It is hoped that relevant solutions can be found in follow-up research in the future.
Disclosure of conflict of interest
None.
References
- 1.Guay J, Johnson RL, Kopp S. Nerve blocks or no nerve blocks for pain control after elective hip replacement (arthroplasty) surgery in adults. Cochrane Database Syst Rev. 2017;10:CD011608. doi: 10.1002/14651858.CD011608.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Molloy IB, Martin BI, Moschetti WE, Jevsevar DS. Effects of the length of stay on the cost of total knee and total hip arthroplasty from 2002 to 2013. J Bone Joint Surg Am. 2017;99:402–407. doi: 10.2106/JBJS.16.00019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stefl M, Lundergan W, Heckmann N, McKnight B, Ike H, Murgai R, Dorr LD. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J. 2017;99-B:37–45. doi: 10.1302/0301-620X.99B1.BJJ-2016-0415.R1. [DOI] [PubMed] [Google Scholar]
- 4.Lu Y, Xiao H, Xue F. Causes of and treatment options for dislocation following total hip arthroplasty. Exp Ther Med. 2019;18:1715–1722. doi: 10.3892/etm.2019.7733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lin D, Charalambous A, Hanna SA. Bilateral total hip arthroplasty in ankylosing spondylitis: a systematic review. EFORT Open Rev. 2019;4:476–481. doi: 10.1302/2058-5241.4.180047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.He C, He X, Tong W, Zheng W, Zhang T, Zhao J, Xu W. The effect of total hip replacement on employment in patients with ankylosing spondylitis. Clin Rheumatol. 2016;35:2975–2981. doi: 10.1007/s10067-016-3431-6. [DOI] [PubMed] [Google Scholar]
- 7.Atesok K, Papavassiliou E, Heffernan MJ, Tunmire D, Sitnikov I, Tanaka N, Rajaram S, Pittman J, Gokaslan ZL, Vaccaro A, Theiss S. Current strategies in prevention of postoperative infections in spine surgery. Global Spine J. 2020;10:183–194. doi: 10.1177/2192568218819817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nazemi AK, Gowd AK, Carmouche JJ, Kates SL, Albert TJ, Behrend CJ. Prevention and management of postoperative delirium in elderly patients following elective spinal surgery. Clinical spine surgery. 2017;30:112–119. doi: 10.1097/BSD.0000000000000467. [DOI] [PubMed] [Google Scholar]
- 9.Senaratna CV, Perret JL, Lodge CJ, Lowe AJ, Campbell BE, Matheson MC, Hamilton GS, Dharmage SC. Prevalence of obstructive sleep apnea in the general population: a systematic review. Sleep Med Rev. 2017;34:70–81. doi: 10.1016/j.smrv.2016.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Imani MM, Sadeghi M, Farokhzadeh F, Khazaie H, Brand S, Dursteler KM, Bruhl A, Sadeghi-Bahmani D. Evaluation of blood levels of C-reactive protein marker in obstructive sleep apnea: a systematic review, meta-analysis and meta-regression. Life (Basel) 2021;11:362. doi: 10.3390/life11040362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: an american academy of sleep medicine systematic review, meta-analysis, and GRADE assessment. J Clin Sleep Med. 2019;15:301–334. doi: 10.5664/jcsm.7638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hla KM, Young T, Finn L, Peppard PE, Szklo-Coxe M, Stubbs M. Longitudinal association of sleep-disordered breathing and nondipping of nocturnal blood pressure in the Wisconsin sleep cohort study. Sleep. 2008;31:795–800. doi: 10.1093/sleep/31.6.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang J, Song Y, Ji Y, Song Y, Cai S, Yu Y, Liu S, Zhang W. Correlation between coronary artery disease and obstructive sleep apnea syndrome and analysis of risk factors. Exp Ther Med. 2018;15:4771–4776. doi: 10.3892/etm.2018.6070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang X, Ouyang Y, Wang Z, Zhao G, Liu L, Bi Y. Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Int J Cardiol. 2013;169:207–214. doi: 10.1016/j.ijcard.2013.08.088. [DOI] [PubMed] [Google Scholar]
- 15.Li M, Hou WS, Zhang XW, Tang ZY. Obstructive sleep apnea and risk of stroke: a meta-analysis of prospective studies. Int J Cardiol. 2014;172:466–469. doi: 10.1016/j.ijcard.2013.12.230. [DOI] [PubMed] [Google Scholar]
- 16.Bubu OM, Andrade AG, Umasabor-Bubu OQ, Hogan MM, Turner AD, de Leon MJ, Ogedegbe G, Ayappa I, Jean-Louis GG, Jackson ML, Varga AW, Osorio RS. Obstructive sleep apnea, cognition and Alzheimer’s disease: a systematic review integrating three decades of multidisciplinary research. Sleep Med Rev. 2020;50:101250. doi: 10.1016/j.smrv.2019.101250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lespasio MJ, Sodhi N, Mont MA. Osteonecrosis of the hip: a primer. Perm J. 2019;23:18–100. doi: 10.7812/TPP/18-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith HA, Gangopadhyay M, Goben CM, Jacobowski NL, Chestnut MH, Savage S, Rutherford MT, Denton D, Thompson JL, Chandrasekhar R, Acton M, Newman J, Noori HP, Terrell MK, Williams SR, Griffith K, Cooper TJ, Ely EW, Fuchs DC, Pandharipande PP. The preschool confusion assessment method for the ICU: valid and reliable delirium monitoring for critically III infants and children. Crit Care Med. 2016;44:592–600. doi: 10.1097/CCM.0000000000001428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pinto TCC, Machado L, Bulgacov TM, Rodrigues-Junior AL, Costa MLG, Ximenes RCC, Sougey EB. Is the montreal cognitive assessment (MoCA) screening superior to the mini-mental state examination (MMSE) in the detection of mild cognitive impairment (MCI) and alzheimer’s disease (AD) in the elderly? Int Psychogeriatr. 2019;31:491–504. doi: 10.1017/S1041610218001370. [DOI] [PubMed] [Google Scholar]
- 20.Majidi S, Luby M, Lynch JK, Hsia AW, Benson RT, Kalaria CP, Nadareishvili Z, Latour LL, Leigh R. MRI-based thrombolytic therapy in patients with acute ischemic stroke presenting with a low NIHSS. Neurology. 2019;93:e1507–e1513. doi: 10.1212/WNL.0000000000008312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stubbs PW, Mortensen J. Clinimetrics: the Scandinavian stroke scale. J Physiother. 2020;66:132. doi: 10.1016/j.jphys.2019.08.010. [DOI] [PubMed] [Google Scholar]
- 22.Dunstan DA, Scott N. Norms for Zung’s self-rating anxiety scale. BMC Psychiatry. 2020;20:90. doi: 10.1186/s12888-019-2427-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jokelainen J, Timonen M, Keinanen-Kiukaanniemi S, Harkonen P, Jurvelin H, Suija K. Validation of the Zung self-rating depression scale (SDS) in older adults. Scand J Prim Health Care. 2019;37:353–357. doi: 10.1080/02813432.2019.1639923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steiner LA. Postoperative delirium. Part 1: pathophysiology and risk factors. Eur J Anaesthesiol. 2011;28:628–36. doi: 10.1097/EJA.0b013e328349b7f5. [DOI] [PubMed] [Google Scholar]
- 25.Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, Harrod CG. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American academy of sleep medicine clinical practice Guideline. J Clin Sleep Med. 2017;13:479–504. doi: 10.5664/jcsm.6506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kheirandish-Gozal L, Gozal D. Obstructive sleep apnea and inflammation: proof of concept based on two illustrative cytokines. Int J Mol Sci. 2019;20:459. doi: 10.3390/ijms20030459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Almendros I, Gozal D. Intermittent hypoxia and cancer: undesirable bed partners? Respir Physiol Neurobiol. 2018;256:79–86. doi: 10.1016/j.resp.2017.08.008. [DOI] [PubMed] [Google Scholar]
- 28.Gozal D, Farre R, Nieto FJ. Obstructive sleep apnea and cancer: epidemiologic links and theoretical biological constructs. Sleep Med Rev. 2016;27:43–55. doi: 10.1016/j.smrv.2015.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Badrin S, Mohamad N, Yunus NA, Zulkifli MM. A brief psychotic episode with depressive symptoms in silent right frontal lobe infarct. Korean J Fam Med. 2017;38:380–382. doi: 10.4082/kjfm.2017.38.6.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhu C, Wang B, Yin J, Xue Q, Gao S, Xing L, Wang H, Liu W, Liu X. Risk factors for postoperative delirium after spinal surgery: a systematic review and meta-analysis. Aging Clin Exp Res. 2020;32:1417–1434. doi: 10.1007/s40520-019-01319-y. [DOI] [PubMed] [Google Scholar]
- 31.Ponirakis G, Al Hamad H, Sankaranarayanan A, Khan A, Chandran M, Ramadan M, Tosino R, Gawhale PV, Alobaidi M, AlSulaiti E, Elsotouhy A, Elorrabi M, Khan S, Nadukkandiyil N, Osman S, Thodi N, Almuhannadi H, Gad H, Mahfoud ZR, Al-Shibani F, Petropoulos IN, Own A, Al Kuwari M, Shuaib A, Malik RA. Association of corneal nerve fiber measures with cognitive function in dementia. Ann Clin Transl Neurol. 2019;6:689–697. doi: 10.1002/acn3.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu L, Zhang L. Effect of high-quality nursing on improvement of anxiety and depression of patients with acute stroke in MRI examination. Iran J Public Health. 2017;46:1646–1651. [PMC free article] [PubMed] [Google Scholar]