Abstract
Background: The use of retrograde intramedullary headless compression screw fixation for metacarpal neck and shaft fractures has been described in the literature. The purpose of this study was to perform a computed tomography (CT)-based morphological analysis of metacarpal size to help surgeons anticipate expected hardware needs. Methods: In all, 108 consecutive hand CT scans were evaluated for the medullary diameter in the volar-dorsal and radial-ulnar planes at the narrowest point of the canal, as well as for the distance from the articular surface to this point. Results were then analyzed by finger and by sex. Results: The ring finger had the smallest average medullary canal diameter for both men and women (2.7 and 2.6 mm, respectively); the small finger had the largest average diameter (3.9 mm) for men and the middle finger (3.6 mm) for women. Radial-ulnar was the rate-limiting dimension in the index, middle, and ring fingers, whereas volar-dorsal was the smallest dimension in the small finger, regardless of sex. Medullary diameter tended to be larger in patients aged more than 50 years. More than 50% of fingers have diameters >3.0 mm, and at least 40% of index, middle, and small fingers have diameters >3.5 mm, which are common diameters of commercially available headless compression screws. Conclusions: When preparing to perform open reduction internal fixation of a metacarpal using retrograde intramedullary headless compression screws, the surgeon needs to be prepared with screws of larger diameters to optimize fixation. Screws of larger diameters are needed to achieve endosteal purchase, regardless of sex.
Keywords: metacarpal, intramedullary, headless, compression, screw, fracture, computed, tomography, dimensions
Introduction
Metacarpal fractures are common, accounting for approximately 33% of all hand fractures. 1 Despite the relative prevalence of this injury, there is debate in the hand literature about the optimal treatment strategy. 2 Most agree that nonoperative management in the form of an orthosis or early protected mobilization is appropriate for closed, extra-articular, and minimally displaced fractures, but it can lead to weakness, extensor lag, palmar prominence, and poor cosmesis when used in the wrong settings. 3 Open reduction internal fixation with a plate and screws provides a rigid construct and allows for earlier range of motion (ROM) and return to work, but requires a more extensive exposure, with increased risk of infection, hardware complications, and formation of extensor tendon adhesions. 4 Furthermore, gaining purchase distally in the periarticular cancellous bone of the metacarpal head can be challenging when attempting to achieve anatomical reduction in metacarpal neck fractures. 5 Doing so may require placing the hardware in a very distal position, increasing the likelihood of symptomatic hardware requiring removal. Kirschner wire (K-wire) fixation can be done percutaneously or with a limited open approach, either antegrade or retrograde, but is less stable, limits ROM until pin removal, and is accompanied by the risk of pin site infections, osteomyelitis, tendon rupture, and nerve injury. Complication rates have been reported at more than 16%. 6
Intramedullary headless screws (IMHSs) have been proven effective in a variety of upper extremity injuries.7-10 More recently, promising results have been observed when using them to treat metacarpal neck and axially stable metacarpal shaft fractures11-14 (Figure 1). This technique minimizes soft tissue and periosteal disruption at the fracture site, allows for rapid mobilization postoperatively, and obviates the need for hardware removal. 14 The dorsal starting point and headless design ensure minimal violation of the articular cartilage. 15 Furthermore, excellent ROM and grip strength, along with high union rates, have been demonstrated in multiple studies.11,13,14
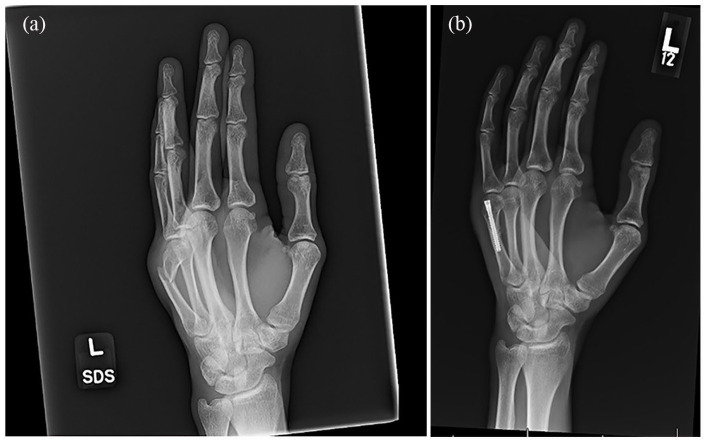
Figure 1.
(a) Anteroposterior radiograph of a left hand of a 31-year-old male patient demonstrating a left fifth metacarpal distal shaft fracture with approximately 60° of apex dorsal angulation, and (b) postoperative image of the same patient following open reduction internal fixation using a standard 4.0-mm Acutrack 2 headless compression screw (Acumed, Hillsboro, Oregon)
By minimizing soft tissue disruption and requiring less immobilization, IMHS can be an ideal treatment in the proper setting. Recent studies, however, have been conflicting regarding the biomechanical stability of the construct. Melamed et al demonstrated an inferior load to failure (LTF) and stiffness of IMHS compared with dorsal plate fixation. Further examination of the study, however, reveals that they used only a 2.4-mm-diameter screw in their analysis. 16
The purpose of our study was to evaluate the dimensions of the intramedullary (IM) canal in a series of metacarpals using computed tomographic (CT) analysis. To date, there has been only 1 previous study on using CT analysis to evaluate metacarpal dimensions, but the authors only recorded the shaft lengths, shaft bending angles, and capital-axis angles and did not examine the IM canal. 17 We hypothesize that in many cases the diameter of the IM canal is much wider than the screws used in the biomechanical studies, and that to obtain the necessary cortical purchase in the isthmus and subsequently improve the biomechanical stability of the construct, larger diameter screws are required.
Materials and Methods
Data Collection
We conducted a database search including all patients who had undergone a CT scan of the hand from January 1, 2006, to October 31, 2016, yielding a total of 111 CT scans. Inclusion criteria included age ≥18 years, atraumatic metacarpals, and adequate visualization on sagittal, axial, and coronal cuts. Three patients under the age of 18 were identified in the search and subsequently excluded; therefore, CT scans of 108 hands were included in the final analysis and reviewed using Philips IntelliSpace PACS Enterprise (Phillips IntelliSpace PACS, Forest City, California). The measurement accuracy of this imaging software has been validated by a previous study. 18 Multiple data points were recorded, including the diameter of the narrowest point of the metacarpal shaft in the volar-dorsal and radial-ulnar directions, and the length from the metacarpal head to the narrowest point of the metacarpal shaft (Figure 2). Each data point was obtained by 2 independent investigators and averaged. In any case of disagreement, the final value was assigned by the senior investigator (M.D.). Descriptive analyses were then performed for age, sex, laterality, and digit.
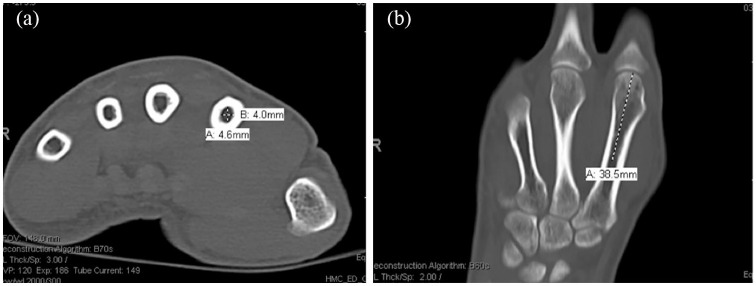
Figure 2.
Computed tomographic measurements of the metacarpal using Philips IntelliSpace PACS Enterprise. Image (a) represents an axial cut depicting the measurement performed to determine the (A) volar-dorsal and (B) radial-ulnar measurement at the narrowest part of the metacarpal shaft. Image (b) represents a coronal cut depicting the measurement performed to determine the (A) length from the metacarpal head to the narrowest point of the metacarpal shaft.
Statistical Analysis
We used the intraclass correlation coefficient (ICC) to determine the level of agreement between observers. A value between 0.50 and 0.75 was considered moderate agreement; 0.75 and 0.90, good; and 0.90 and 1.00, excellent. 19 In addition, the percentages of IM canals with diameters of <2.4, ≥2.4, ≥3.0, ≥3.5, and ≥4.0 mm were determined to allow for a comparison with the dimensions of the leading threads of common commercially available headless compression screws (HCSs).
Results
A total of 108 hands were analyzed from 108 individuals above the age of 18 (range, 19-95; mean, 48.3) years. There were 76 men and 32 women, with 50 right hands and 58 left hands. Agreement between the 2 observers was considered moderate to excellent (ICC = 0.576-0.943).
Table 1 shows the mean dimensions stratified by both finger and sex. The radial-ulnar dimension of the ring finger was the narrowest digit in both men (2.7 mm) and women (2.6 mm). The digit with the largest diameter was found to be the small finger in the radial-ulnar direction for men (3.9 mm) and the middle finger in the volar-dorsal direction for women (3.6 mm). The radial-ulnar direction was the narrowest dimension for index, middle, and ring fingers, whereas the volar-dorsal direction was the narrowest in the small finger, regardless of sex (Figure 3). Although right-sided metacarpals had slightly larger diameters, there was no statistically significant difference (Supplemental Material). In all digits, men demonstrated larger distances to the narrowest point on the metacarpal shaft than women (P < .001) (Table 2). In men, 33 of 73 index fingers, 33 of 74 middle fingers, 3 of 75 ring fingers, and 0 of 74 small fingers demonstrated distances ≥40mm, whereas nearly no female digits met or exceeded this length.
Table 1.
Mean Diameters of the Metacarpal Canals at Their Narrowest Point Stratified by Finger and Sex in the Radial to Ulnar Direction and Volar to Dorsal Direction.
| Direction | Finger | Overall mean, mm | Sex | Mean by sex, mm | P value |
|---|---|---|---|---|---|
| Radial to ulnar | Index | 3.1 | F | 3.0 | 1.000 |
| M | 3.15 | ||||
| Middle | 3.1 | F | 3.2 | 1.000 | |
| M | 3.0 | ||||
| Ring | 2.6 | F | 2.6 | 1.000 | |
| M | 2.7 | ||||
| Small | 3.7 | F | 3.5 | .453 | |
| M | 3.9 | ||||
| Volar to dorsal | Index | 3.4 | F | 3.5 | 1.000 |
| M | 3.3 | ||||
| Middle | 3.6 | F | 3.6 | 1.000 | |
| M | 3.5 | ||||
| Ring | 3.05 | F | 3.0 | 1.000 | |
| M | 3.1 | ||||
| Small | 3.3 | F | 3.1 | .056 | |
| M | 3.5 |
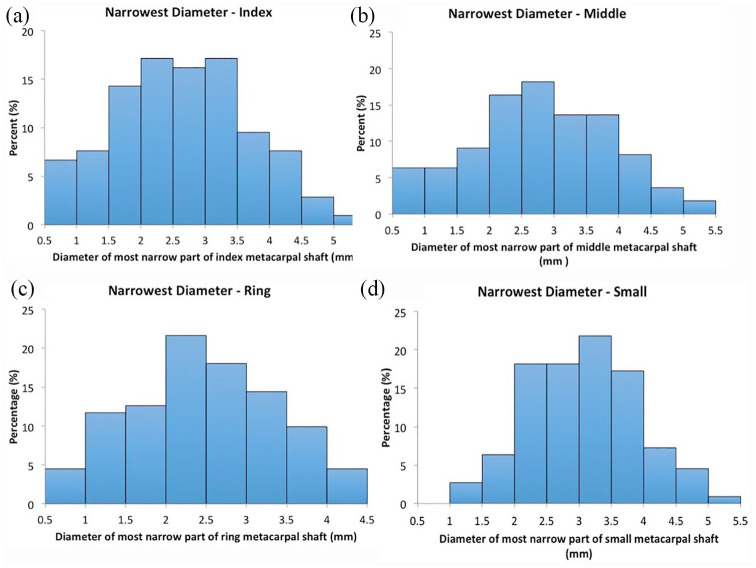
Figure 3.
Histogram plots depicting the distribution of diameters at the narrowest point of the intramedullary canal for the (a) index, (b) middle, (c) ring, and (d) small metacarpals.
Table 2.
Mean Length From the Metacarpal Head to the Narrowest Point of the Metacarpal Shaft Stratified by Finger and Sex.
| Finger | Overall mean | Sex | Mean by sex | P value |
|---|---|---|---|---|
| Index | 37.5 | F | 35.6 | <.001 |
| M | 39.2 | |||
| Middle | 37.4 | F | 35.4 | <.001 |
| M | 39.4 | |||
| Ring | 32.55 | F | 30.8 | <.001 |
| M | 34.3 | |||
| Small | 29.6 | F | 27.7 | <.001 |
| M | 31.6 |
With increasing age, the distance from the metacarpal head to the narrowest point of the metacarpal shaft did not meaningfully change; however, the diameter of the medullary canal increased, when both age >50 and >65 years were used as cutoff points (Table 3).
Table 3.
Mean Diameters of the Metacarpal Canals at Their Narrowest Point Regardless of Direction (Radial-Ulnar or Volar-Dorsal) Stratified Using Age 65 and Age 50 as Cutoff Points.
| Finger | Age, y | Mean by age | P value |
|---|---|---|---|
| Index | <65 | 2.4 | <.001 |
| ≥65 | 3.6 | ||
| Middle | <65 | 2.5 | <.001 |
| ≥65 | 3.8 | ||
| Ring | <65 | 2.3 | .002 |
| ≥65 | 3.0 | ||
| Small | <65 | 3.1 | 1.000 |
| ≥65 | 3.2 | ||
| Index | <50 | 2.4 | .006 |
| ≥50 | 3.1 | ||
| Middle | <50 | 2.6 | .004 |
| ≥50 | 3.3 | ||
| Ring | <50 | 2.4 | .206 |
| ≥50 | 2.7 | ||
| Small | <50 | 3.1 | 1.000 |
| ≥50 | 3.1 |
Table 4 shows the percentage of metacarpals that have dimensions based on commonly used HCSs. Overall, 70.1% of middle fingers are ≥2.4 mm and 20.6% are ≥4.0 mm at their narrowest point. Even for ring fingers, the narrowest digit observed in the study, 67% are ≥2.4 mm and 9.3% are ≥4.0 mm. Following stratification based on sex, the percentages between men and women were quite comparable. The only notable difference was in the ring finger, where the narrowest portion was ≥4.0 mm in 12% of men compared with only 3.0% of women, and the small finger, where the narrowest portion was ≥4.0 mm in 22.2% of men compared with only 3.0% of women.
Table 4.
Percentage of Diameters at the Narrowest Point of the Metacarpal Shaft Based on Commonly Used Headless Compression Screws, Stratified by Direction (Volar-Dorsal and Radial-Ulnar) With the Entire Study Population, Women, and Men.
| Sex | Finger | Measurement | % of fingers <2.4 mm | % of fingers ≥2.4 mm | % of fingers ≥3.0 mm | % of fingers ≥3.5 mm | % of fingers ≥4.0 mm |
|---|---|---|---|---|---|---|---|
| Overall | Index | Radial-ulnar | 28.3 | 71.7 | 54.7 | 39.6 | 19.8 |
| Volar-dorsal | 20.8 | 79.2 | 64.2 | 42.5 | 28.3 | ||
| Middle | Radial-ulnar | 29.9 | 70.1 | 51.4 | 40.2 | 20.6 | |
| Volar-dorsal | 16.8 | 83.2 | 68.2 | 51.4 | 33.6 | ||
| Ring | Radial-ulnar | 37.0 | 67.0 | 34.3 | 19.4 | 9.3 | |
| Volar-dorsal | 24.1 | 75.9 | 55.6 | 37.0 | 15.7 | ||
| Small | Radial-ulnar | 6.5 | 93.5 | 72.0 | 56.5 | 43.5 | |
| Volar-dorsal | 10.2 | 89.8 | 64.8 | 42.6 | 22.2 | ||
| Women | Index | Radial-ulnar | 30.3 | 69.7 | 54.5 | 39.3 | 18.2 |
| Volar-dorsal | 15.2 | 84.8 | 63.6 | 45.5 | 33.3 | ||
| Middle | Radial-ulnar | 18.2 | 81.8 | 51.5 | 48.5 | 21.2 | |
| Volar-dorsal | 18.2 | 81.8 | 66.7 | 60.6 | 39.4 | ||
| Ring | Radial-ulnar | 30.3 | 69.7 | 27.3 | 9.1 | 3.0 | |
| Volar-dorsal | 27.3 | 72.7 | 48.5 | 30.3 | 6.1 | ||
| Small | Radial-ulnar | 3.0 | 97.0 | 81.2 | 48.5 | 33.3 | |
| Volar-dorsal | 9.1 | 90.9 | 57.6 | 24.2 | 3.0 | ||
| Men | Index | Radial-ulnar | 27.4 | 73.6 | 54.8 | 39.7 | 20.5 |
| Volar-dorsal | 23.3 | 76.7 | 64.4 | 41.1 | 26.0 | ||
| Middle | Radial-ulnar | 35.1 | 64.9 | 51.4 | 36.5 | 20.3 | |
| Volar-dorsal | 17.6 | 82.4 | 68.9 | 47.3 | 31.1 | ||
| Ring | Radial-ulnar | 40.0 | 60.0 | 37.3 | 24.0 | 12.0 | |
| Volar-dorsal | 22.7 | 77.3 | 58.7 | 40.0 | 20.0 | ||
| Small | Radial-ulnar | 6.8 | 93.2 | 67.6 | 60.8 | 48.6 | |
| Volar-dorsal | 10.8 | 89.2 | 68.9 | 51.4 | 31.1 |
Discussion
Many techniques have been developed for the surgical management of metacarpal neck and shaft fractures, including antegrade (bouquet) 20 and retrograde (IM or crossed) K-wire fixation, 21 IM rods, 22 and plate and screw constructs. Boulton et al 5 first described the use of an HCS to treat a displaced comminuted subcapital fracture of the fifth metacarpal. Using a limited open approach and dorsal distal articular starting point, they inserted a 3.0-mm cannulated Synthes HCS (Synthes, Paoli, Pennsylvania) into the medullary canal in a retrograde fashion and buried it into the subchondral bone, achieving excellent results. Since then, the indications for this technique have been expanded to include both metacarpal neck and axially stable metacarpal shaft fractures. Ruchelsman et al 14 retrospectively reviewed 26 metacarpal neck/subcapital and 13 shaft fractures treated with limited open retrograde IMHSs. All patients achieved full composite flexion and resolution of any extensor lag by 3-week follow-up, and all patients demonstrated radiographic union by 6 weeks. Doarn et al 11 reviewed 9 fifth metacarpal neck and shaft fractures treated with a similar technique and demonstrated excellent postoperative ROM (0° of extension and 90° of flexion) and no residual grip weakness. Tobert et al 13 reviewed 16 patients with 18 metacarpal fractures (neck and shaft) treated with IMHSs and noted that all patients had a total active motion of over 240° and no complications.
The excellent clinical and radiographic results demonstrated by these studies suggest that the use of IMHS is a safe and effective option to treat transverse or short oblique metacarpal neck and shaft fractures in skeletally mature patients without infection. Benefits of this technique include rapid mobilization, minimal soft tissue disruption, and no need for hardware removal. Concerns include cartilage damage due to the intracapsular starting point, but a recent 3-dimensional CT analysis by ten Berg et al 15 revealed that only 4% of the articular surface was involved in the clinically relevant sagittal arc of motion when using the recommended dorsal starting point. Furthermore, significantly more cartilage damage can be incurred when using the retrograde percutaneous K-wire technique, as multiple attempts to achieve an adequate starting position can repeatedly violate the articular surface. 14
Several biomechanical studies have called the stability of the IMHS construct into question. Melamed et al 16 compared a 2.4-mm IMHS with 1.5- to 2.0-mm locking and nonlocking plates in human cadaveric metacarpals and found that the IMHS demonstrated significantly lower LTF and stiffness than plates. Similarly, Beutel et al 23 compared a 3.0-mm IMHS and crossed K-wires in cadaveric metacarpals and found a significantly lower stiffness and maximum displacement in the IMHS. Jones et al 24 compared a 3.0-mm IMHS versus crossed K-wires versus locking plate fixation in 30 sawbone metacarpals and found that the IMHS mechanical properties were comparable with those of the crossed K-wires, but both were weaker than the locking plate construct. On the contrary, Avery et al 25 determined that IMHS was the biomechanically superior construct, but they compared a 3.5-mm IMHS with IM K-wires in fresh frozen cadaveric specimens. To our knowledge, the necessary stiffness and LTF for metacarpal fractures to withstand immediate protected motion are unknown; however, the average bending moment during metacarpal joint flexion has been estimated to be 0.35 N m. 26
In these biomechanical studies, the size of the IMHSs used must be taken into consideration. Melamed et al used only a 2.4-mm IMHS, whereas Beutel et al and Jones et al used a 3.0-mm IMHS16,23,24. In our study, we find that these implants would frequently be too small to gain adequate purchase in the medullary canal. For example, despite the ring finger being the narrowest digit observed in the study (mean of 2.7 mm in men and 2.6 mm in women), 19.4% of them were greater than or equal to 3.5 mm at the narrowest point, suggesting that using a 2.4- or 3.0-mm screw in these patients would lead to an unstable construct. That number increases to 39.6% in the index, 40.2% in the middle, and 42.6% in the small fingers.
Interestingly, the diameter of the small digit metacarpal at its narrowest point was quite large, with an average radial-ulnar measurement greater than any of the other digits. This is in contrast to the dimensions of the distal phalanx of the small digit, which were shown in a recent radiographic study at our institution to consistently measure smaller than any of the other digits. 18 Following stratification based on sex, there was not a dramatic difference observed between them, apart from the number of ring and small fingers measuring greater than 4.0 mm. The narrowest portion of the ring finger was ≥4.0 mm in 12% of men compared with only 3.0% of women, and the narrowest portion of the small finger was ≥4.0 mm in 22.2% of men compared with only 3.0% of women. This should be taken into consideration during preoperative planning, as larger diameter IMHSs may be necessary when treating the ring and small digits in men.
The length to the narrowest part of the medullary canal did vary based on sex. In men, 45.2% of index fingers and 44.6% of middle fingers demonstrated distances ≥40 mm to the narrowest point on the metacarpal shaft, whereas nearly no female digits met or exceeded this length. This is important because 40 mm is the longest available length of many commercially available HCSs, the diameters of which would be required for this application. Therefore, alternative means of fixation may need to be pursued if the available screws are too short to achieve cortical fixation within the medullary canal.
In addition, we found that increased patient age was associated with increased medullary canal diameters. This is consistent with the findings in femoral shaft diameters.27,28 Expansion of the medullary canal over time may be the result of cortical thinning or may be due to cortical remodeling, placing more bone at the periphery, thus increasing bending stiffness.
We are unable to comment on any influence that hand dominance may have on metacarpal dimensions. Because hand CT scans were obtained for multiple reasons by different providers, hand dominance was not consistently documented. Although it is conceivable that metacarpal morphology may be altered by load during skeletal growth or by chronic stresses, as previously described by Roy et al, 29 we cannot speak of this in our current study. Previous anthropological studies have demonstrated that right hand second metacarpals tend to be larger than left regardless of hand dominance 30 ; although our right-sided measurements were larger than the left, these differences did not rise to the level of significance.
The importance of preoperative planning and proper screw selection cannot be overstated. To achieve adequate stability, solid purchase must be obtained by the leading threads proximally in the cortical bone and by the trailing threads distally in the subchondral bone. Use of an undersized IMHS would lead to a mechanically weaker and less stable construct. In addition, when treating metacarpal shaft fractures in particular, the chosen implant must be long enough to ensure that the leading threads extend proximal to the fracture line. In the senior author’s clinical experience, the measurements on radiographs are accurate for surgical planning. We elected to use CT scans, however, to allow more accurate volar-dorsal and radial-ulnar measurements as the overlap of the metacarpals on a lateral radiograph hinders precise measurements.
Conclusion
Recent studies have shown the IMHS to be a viable option in the treatment of metacarpal neck and shaft fractures, with minimal soft tissue disruption, early mobilization, and good clinical outcomes. Our study was the first to use CT scans to characterize the dimensions of the IM canal of the metacarpals and show that a significant percentage are too capacious for some standard size HCSs. We also found that nearly half of the male index and middle metacarpals demonstrate a distance of ≥40mm to the narrowest portion of the endosteal isthmus. Extra attention must be paid during preoperative planning to ensure that appropriately sized implants are available during the procedure. Further studies including descriptive studies of screw sizes used clinically, use of radiographs for preoperative planning, and clinical outcomes, may be helpful.
Supplemental Material
Supplemental material, Supplementary_material for Morphological Analysis of Metacarpal Shafts With Respect to Retrograde Intramedullary Headless Screw Fixation by Mark L. Dunleavy, Xavier Candela and Michael Darowish in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: No informed consent was obtained; 200 consecutive deidentified hand radiographs were used.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Mark L. Dunleavy  https://orcid.org/0000-0002-6403-3229
https://orcid.org/0000-0002-6403-3229
References
- 1. Nakashian MN, Pointer L, Owens BD, et al. Incidence of metacarpal fractures in the US population. Hand (NY). 2012;7(4):426-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Friedrich JB, Vedder NB. An evidence-based approach to metacarpal fractures. Plast Reconstr Surg. 2010;126(6):2205-2209. [DOI] [PubMed] [Google Scholar]
- 3. Strub B, Schindele S, Sonderegger J, et al. Intramedullary splinting or conservative treatment for displaced fractures of the little finger metacarpal neck? A prospective study. J Hand Surg Eur Vol. 2010;35(9):725-729. [DOI] [PubMed] [Google Scholar]
- 4. Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg Am. 1998;23(5):827-832. [DOI] [PubMed] [Google Scholar]
- 5. Boulton CL, Salzler M, Mudgal CS. Intramedullary cannulated headless screw fixation of a comminuted subcapital metacarpal fracture: case report. J Hand Surg Am. 2010;35(8):1260-1263. [DOI] [PubMed] [Google Scholar]
- 6. Hsu LP, Schwartz EG, Kalainov DM, et al. Complications of K-wire fixation in procedures involving the hand and wrist. J Hand Surg Am. 2011;36(4):610-616. [DOI] [PubMed] [Google Scholar]
- 7. Geissler WB. Carpal fractures in athletes. Clin Sports Med. 2001;20:167-188. [DOI] [PubMed] [Google Scholar]
- 8. Rutgers M, Mudgal CS, Shin R. Combined fractures of the distal radius and scaphoid. J Hand Surg. 2008;33B:478-483. [DOI] [PubMed] [Google Scholar]
- 9. Slade JF, III, Taksali S, Safanda J. Combined fractures of the scaphoid and distal radius: a revised treatment rationale using percutaneous and arthroscopic techniques. Hand Clin. 2005;21:427-441. [DOI] [PubMed] [Google Scholar]
- 10. Hotchkiss RN. Displaced fractures of the radial head: internal fixation or excision? J Am Acad Orthop Surg. 1997;5:1-10. [DOI] [PubMed] [Google Scholar]
- 11. Doarn MC, Nydick JA, Williams BD, et al. Retrograde headless intramedullary screw fixation for displaced fifth metacarpal neck and shaft fractures: short term results. Hand (N.Y.). 2015;10(2):314-318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. del Piñal F, Moraleda E, Rúas JS, et al. Minimally invasive fixation of fractures of the phalanges and metacarpals with intramedullary cannulated headless compression screws. J Hand Surg Am. 2015;40(4):692-700. [DOI] [PubMed] [Google Scholar]
- 13. Tobert DG, Klausmeyer M, Mudgal CS. Intramedullary fixation of metacarpal fractures using headless compression screws. J Hand Microsurg. 2016;8(3):134-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ruchelsman DE, Puri S, Feinberg-Zadek N, et al. Clinical outcomes of limited-open retrograde intramedullary headless screw fixation of metacarpal fractures. J Hand Surg Am. 2014;39(12):2390-2395. [DOI] [PubMed] [Google Scholar]
- 15. ten Berg PW, Mudgal CS, Leibman MI, et al. Quantitative 3-dimensional CT analyses of intramedullary headless screw fixation for metacarpal neck fractures. J Hand Surg Am. 2013;38(2):322-330. [DOI] [PubMed] [Google Scholar]
- 16. Melamed E, Hinds RM, Gottschalk MB, et al. Comparison of dorsal plate fixation versus intramedullary headless screw fixation of unstable metacarpal shaft fractures: a biomechanical study. Hand (N.Y.). 2016;11(4):421-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rivlin M, Kim N, Lutsky KF, et al. Measurement of the radiographic anatomy of the small and ring metacarpals using computerized tomographic scans. Hand (N Y). 2015;10(4):756-761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Darowish M, Brenneman R, Bigger J. Dimensional analysis of the distal phalanx with consideration of distal interphalangeal joint arthrodesis using a headless compression screw. Hand (N.Y.). 2015;10(1):100-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Foucher G. “Bouquet” osteosynthesis in metacarpal neck fractures: a series of 66 patients. J Hand Surg Am. 1995;20(Suppl. 3):S86-S90. [DOI] [PubMed] [Google Scholar]
- 21. Schadel-Hopfner M, Wild M, Windolf J, et al. Antegrade intramedullary splinting or percutaneous retrograde crossed pinning for displaced neck fractures of the fifth metacarpal? Arch Orthop Trauma Surg. 2007;127(6):435-440. [DOI] [PubMed] [Google Scholar]
- 22. Gonzalez MH, Hall RF., Jr. Intramedullary fixation of metacarpal and proximal phalangeal fractures of the hand. Clin Orthop Relat Res. 1996;327:47-54. [DOI] [PubMed] [Google Scholar]
- 23. Beutel BG, Ayalon O, Kennedy OD, et al. Crossed K-wires versus intramedullary headless screw fixation of unstable metacarpal neck fractures: a biomechanical study. Iowa Orthop J. 2018;38:153-157. [PMC free article] [PubMed] [Google Scholar]
- 24. Jones CM, Padegimas EM, Weikert N, et al. Headless screw fixation of metacarpal neck fractures: a mechanical comparative analysis. Hand (N.Y.). 2019;14(2):187-192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Avery DM, III, Klinge S, Dyrna F, et al. Headless compression screw versus Kirschner wire fixation for metacarpal neck fractures: a biomechanical study. J Hand Surg Am. 2017;42(5):392. [DOI] [PubMed] [Google Scholar]
- 26. Vanik RK, Weber RC, Matloub HS, et al. The comparative strengths of internal fixation techniques. J Hand Surg Am. 1984;9(2):216-221. [DOI] [PubMed] [Google Scholar]
- 27. Milligan DJ, O’Brien S, Bennett D, et al. The effects of age and gender on the diameter of the femoral canal in patients who undergo total hip replacement. Bone Joint J. 2013;95-B(3):339-342. [DOI] [PubMed] [Google Scholar]
- 28. Casper DS, Kim GK, Parvizi J, et al. Morphology of the proximal femur differs widely with age and sex: relevance to design and selection of femoral prostheses. J Orthop Res. 2012;30(7):1162-1166. [DOI] [PubMed] [Google Scholar]
- 29. Roy TA, Ruff CB, Plato CC. Hand dominance and bilateral asymmetry in the structure of the second metacarpal. Am J Phys Anthropol. 1994;94(2):203-211. [DOI] [PubMed] [Google Scholar]
- 30. Plato CC, Wood JL, Norris AH. Bilateral asymmetry in bone measurements of the hand and lateral hand dominance. Am J Physl Anthropol. 1980;52(1):27-31. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_material for Morphological Analysis of Metacarpal Shafts With Respect to Retrograde Intramedullary Headless Screw Fixation by Mark L. Dunleavy, Xavier Candela and Michael Darowish in HAND