Abstract
Background
Traumatic peripheral nerve injuries cause chronic pain, disability, and long-term reductions in quality of life. However, their incidence after extremity trauma remains poorly understood.
Methods
The IBM® MarketScan® Commercial Database from 2010 to 2015 was used to identify patients aged 18 to 64 who presented to emergency departments for upper and/or lower extremity traumas. Cumulative incidences were calculated for nerve injuries diagnosed within 2 years of trauma. Cox regression models were developed to evaluate the associations between upper extremity nerve injury and chronic pain, disability, and use of physical therapy or occupational therapy.
Results
The final cohort consisted of 1 230 362 patients with employer-sponsored health plans. Nerve injuries were diagnosed in 2.6% of upper extremity trauma patients and 1.2% of lower extremity trauma patients. Only 9% and 38% of nerve injuries were diagnosed by the time of emergency department and hospital discharge, respectively. Patients with nerve injuries were more likely to be diagnosed with chronic pain (hazard ratio [HR]: 5.9, 95% confidence interval [CI], 4.3-8.2), use physical therapy services (HR: 10.7, 95% CI, 8.8-13.1), and use occupational therapy services (HR: 19.2, 95% CI, 15.4-24.0) more than 90 days after injury.
Conclusions
The incidence of nerve injury in this national cohort was higher than previously reported. A minority of injuries were diagnosed by emergency department or hospital discharge. These findings may improve practitioner awareness and inform public health interventions for injury prevention.
Keywords: epidemiology, research & health outcomes, surgery, specialty, outcomes, nerve injury, nerve, diagnosis, incidence, administrative database
Introduction
Peripheral nerve injuries cause chronic pain, disability, and long-term disruptions in daily living, leisure, professional development, and education.1-7 Moreover, traumatic nerve injuries commonly affect relatively young individuals at their peak economic productivity, resulting in incalculable losses to personal income and lifelong reductions in quality of life.8-11 Understanding the epidemiology of traumatic nerve injuries is important for improving their management and for developing prevention strategies. Unfortunately, the incidence of these injuries in the United States remains unclear.
An estimated 3.4 million upper extremity traumas are evaluated in emergency departments across the United States each year.12,13 Depending on trauma location and severity, 1% to 3% of these patients are diagnosed with nerve injuries during the first few months after trauma.11,14,15 Establishing the long-term prevalence and burden of nerve injuries has proven difficult, however, because they are often diagnosed months to years after trauma and in a variety of care settings. 16 Patients may be referred to pain medicine, physical medicine and rehabilitation, occupational and physical therapy, and/or psychiatry for management of unspecified chronic pain or dysfunction before their nerve injuries are recognized. Delays in diagnosis limit surgical options and may lead to suboptimal recovery.17-19
A common reference for the incidence of traumatic nerve injuries in the United States is based on insurance claims from 1998. 11 Since then, advances in our understanding of nerve topography, injury pathophysiology, and nerve regeneration have led to a paradigm shift in the treatment of nerve injuries.20,21 New treatment options, such as nerve transfers, are available that necessitate prompt diagnosis and management.21-24 To improve recognition of nerve injuries and guide allocation of medical resources, modern estimates for the incidences of these injuries must be established. Additionally, an understanding of injury causes, such as falls or motorcycle crashes, is necessary to inform public health interventions for injury prevention.
In this study, we use a national database of commercial insurance claims to document nerve injuries diagnosed up to 2 years following extremity trauma. In addition to reporting the incidence of these injuries, we identify high-risk injury mechanisms and evaluate delays between extremity trauma and diagnosis of nerve injury. We also examine the associations between nerve injuries and chronic pain, disability, use of physical therapy, and use of occupational therapy.
Materials and Methods
Data Source and Cohort Selection
Patient information was collected from the IBM® MarketScan® Commercial Database (Ann Arbor, MI from January 1, 2010 until September 30, 2015). The MarketScan database consists of inpatient and outpatient medical claims of individuals insured by employer-sponsored health plans and their dependents. The initial cohort was assembled from adults aged 18 to 64 who presented to an emergency department for extremity trauma between January 1, 2010 and December 31, 2013, allowing for a 2-year follow-up for most patients. Inclusion in the final cohort required: (1) at least one International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis code for upper or lower extremity injury (Supplemental Table S1); (2) at least one known injury location; and (3) continuous enrollment in the MarketScan database for at least 90 days prior to and 90 days following extremity trauma. The study was determined to be exempt from human subjects’ regulation by our Institutional Review Board (IRB). Findings were reported in accordance to RECORD recommendations. 25
Outcome Variables
Study outcomes were defined by ICD-9-CM diagnosis codes and Common Procedural Terminology (CPT-4) codes. The primary outcomes were upper or lower extremity nerve injury diagnoses, and patients could receive multiple nerve injury diagnoses during follow-up (Supplemental Table S2). To improve the attributability of nerve injuries to traumas, each nerve injury was linked to plausible anatomic areas. For example, a digital nerve injury was only included if the patient had a documented trauma involving the hand or wrist (Supplemental Table S3). Secondary outcomes were long-term sequelae of traumatic injuries. These included chronic pain (ICD-9-CM 337.20—337.22, 337.29, 338.0, 338.21, 338.29, 338.4, 354.4, 355.71), disability (ICD-9-CM V49.0—V49.3), use of occupational therapy services (ICD-9-CM V57.2; CPT-4 97003, 97004, 97112, 97533, 97535, 97537, 97755), and use of physical therapy services (ICD-9-CM V57.1; CPT-4 97001, 97002, 97110, 97116, 97542, 97750). The time-to-diagnosis, or the number of calendar days from the index trauma until first coding of an outcome, was calculated for all primary and secondary outcomes. Maximum follow-up time was 2 years after trauma.
Additional Variables
Available patient demographic information included age, gender, and location of home residence. Available trauma information included date of emergency department presentation, inpatient admission, injury location and type (eg, shoulder dislocation), external cause of injury (E-code) assigned at the time of trauma (Supplemental Table S4), and date of emergency department or hospital discharge. Location of residence was categorized by geographic region and metropolitan statistical area (MSA) using home ZIP codes. The 2000 United States census defined 366 MSAs, which included the majority of the United States population. Each MSA consisted of at least one urbanized center with 50 000 or more inhabitants as well as its surrounding counties. To examine the association between nerve injury and urbanization, population density (population size divided by land area in square miles) of each MSA was retrieved from the 2010 United States census.
Statistical Analysis
The cumulative incidences of nerve injuries were calculated over the 2-year follow-up period after extremity trauma. Because identifying factors associated with upper extremity nerve injuries may aid in their diagnosis and management, a multivariable Cox regression model was developed for upper extremity nerve injury. Additionally, factors associated with delays in diagnosis were evaluated via multivariable logistic regression models for brachial plexus, median nerve, ulnar nerve, radial nerve, and digital nerve injuries; the outcome of these models was nerve injury diagnosis within 365 days of trauma. Each logistic regression model only included patients with the nerve injury of interest, and models were not developed for isolated axillary or musculocutaneous nerve injuries because these diagnoses were very uncommon in our cohort. Multivariable Cox regression models were also developed for chronic pain, disability, occupational therapy use, and physical therapy use. To allow time for diagnosis of chronic pain (at least 90 days) and to examine the use of occupational and physical therapy in the chronic period, follow-up time for secondary outcome models began on day 91.
Each of the 10 multivariable regression models developed in this study included age, sex, inpatient admission, population density quartile, and type of injury. The secondary outcome models also included the presence of upper extremity nerve injury. Variables in each Cox regression model were screened for interactions with follow-up time; interaction terms with P-values less than .05 were included in the final models. For interpretation of the 10 models, Bonferroni adjustment was used to set the significance level to .005 (.05/10). Variables with P-values less than .005 were considered statistically significant. All analyses were performed using SAS, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
The final cohort consisted of 1 230 362 patients with employer-sponsored health plans, including 891 996 patients with upper extremity traumas and 365 466 patients with lower extremity traumas; 2.2% of patients experienced both upper and lower extremity traumas. The median patient age was 43 years, and median follow-up time after trauma was 1.8 years (Supplemental Table S5). The hands and feet were the most commonly injured areas, and fractures (n = 732 793) and open wounds (n = 671 838) were the most common injury types (Table 1). A total of 24 000 upper extremity nerve injuries and 3750 lower extremity nerve injury diagnoses were included. Of these, 90.8% of patients had a single nerve injury, 8.2% had 2 distinct nerve injuries, and 1% had more than 2 nerve injuries. The median nerve was the most commonly injured peripheral nerve (Table 2). Brachial plexus injuries comprised 5.1% of the diagnoses.
Table 1.
Locations and Types of Extremity Traumas.
| Location | Proportion of patients with each injury type (%)
a
|
||||||
|---|---|---|---|---|---|---|---|
| Amputation | Open wound | Crush | Fracture | Dislocation | Unspecified | Any b | |
| Shoulder | — | 0.47 | 0.01 | 2.74 | 3.55 | 4.73 | 9.94 |
| Arm | — | 0.57 | 0.01 | 3.04 | — | — | 3.60 |
| Elbow | — | 1.21 | 0.01 | — | 0.46 | — | 1.67 |
| Forearm | — | 3.77 | 0.03 | 8.45 | — | — | 12.17 |
| Wrist | — | 1.96 | 0.02 | 2.05 | 0.23 | — | 4.18 |
| Hand | 0.89 | 35.1 | 1.28 | 9.36 | 1.42 | 9.27 | 46.79 |
| Hip | — | 1.47 | 0.01 | 0.95 | 0.27 | 1.75 | 4.01 |
| Thigh | — | 1.47 | 0.02 | 1.69 | — | 1.75 | 4.46 |
| Knee | — | — | 0.02 | 3.81 | 0.72 | — | 1.48 |
| Leg | — | — | 0.06 | 3.81 | — | — | 3.86 |
| Ankle | — | — | 0.03 | 7.76 | 0.64 | — | 7.90 |
| Foot | 0.07 | 6.07 | 0.35 | 8.71 | 0.36 | — | 14.81 |
Patients could have multiple injury types at each location and injuries to multiple locations. The proportion of patients with each injury type-location pair is reported as a percentage.
Patients with at least one injury type in the corresponding location.
Table 2.
Proportion of Individual Nerve Injuries.
| Injured nerve | Total nerve injuries (27 750) a | Proportion of total nerve injuries (%) |
|---|---|---|
| Upper extremity | ||
| Brachial plexus | 1413 | 5.09 |
| Axillary | 265 | 0.95 |
| Musculocutaneous | 30 | 0.11 |
| Radial | 1850 | 6.67 |
| Median | 10 401 | 37.48 |
| Ulnar | 3783 | 13.63 |
| Digital | 6258 | 22.55 |
| Lower extremity | ||
| Lumbosacral plexus | 122 | 0.44 |
| Femoral | 165 | 0.59 |
| Sciatic | 361 | 1.30 |
| Tibial | 41 | 0.15 |
| Peroneal | 658 | 2.37 |
| Tarsal | 651 | 2.35 |
| Plantar | 1752 | 6.31 |
A total of 25 171 patients were diagnosed with 27 750 nerve injuries; 90.8% of patients had a single nerve injury, 8.2% had 2 injuries, and 1% had more than 2 nerve injuries.
The overall cumulative incidence of nerve injury was 2.3% by 2 years, occurring in 2.6% of upper extremity traumas and 1.2% of lower extremity traumas (Table 3). Among patients who required hospitalization, the 2-year incidence of nerve injury was 5.5%, occurring in 9.2% of upper extremity traumas and 2.0% of lower extremity traumas. Upper extremity nerve injuries were particularly common after crush injuries and joint dislocations (Supplemental Table S6).
Table 3.
Cumulative Incidences of Nerve Injuries by Hospital or Emergency Department Discharge and by 2 Years After Trauma.
| Nerve injury | Patients (n) | Cumulative incidence (%) |
||||
|---|---|---|---|---|---|---|
| No inpatient admission |
Inpatient admission |
Overall |
||||
| Discharge | 2 years | Discharge | 2 years | 2 years | ||
| Any nerve | 1 230 362 | 0.18 | 2.03 | 2.09 | 5.46 | 2.26 |
| Any upper extremity nerve | 891 996 | 0.23 | 2.35 | 3.97 | 9.18 | 2.64 |
| Brachial plexus | 155 851 | 0.050 | 0.90 | 0.73 | 2.47 | 0.99 |
| Axillary nerve | 155 851 | 0.019 | 0.15 | 0.075 | 0.41 | 0.18 |
| Musculocutaneous nerve | 155 851 | 0.0007 | 0.014 | 0.012 | 0.083 | 0.021 |
| Radial nerve | 235 551 | 0.078 | 0.62 | 1.37 | 3.03 | 0.84 |
| Median nerve | 235 551 | 0.17 | 4.73 | 2.62 | 7.88 | 5.03 |
| Ulnar nerve | 235 551 | 0.093 | 1.53 | 1.68 | 4.88 | 1.84 |
| Digital nerve | 618 677 | 0.19 | 0.99 | 1.88 | 2.38 | 1.03 |
| Any lower extremity nerve | 365 466 | 0.022 | 1.04 | 0.45 | 2.02 | 1.2 |
| Lumbosacral plexus | 63 761 | 0.003 | 0.12 | 0.065 | 0.38 | 0.23 |
| Femoral nerve | 63 761 | 0.005 | 0.22 | 0.050 | 0.48 | 0.32 |
| Sciatic nerve | 80 436 | 0.019 | 0.28 | 0.29 | 0.97 | 0.53 |
| Tibial nerve | 81 880 | 0 | 0.016 | 0.042 | 0.11 | 0.054 |
| Peroneal nerve | 81 880 | 0.053 | 0.56 | 0.40 | 1.36 | 0.88 |
| Tarsal nerve | 271 199 | 0.004 | 0.29 | 0.03 | 0.48 | 0.31 |
| Plantar nerve | 271 199 | 0.009 | 0.85 | 0.008 | 0.62 | 0.83 |
When adjusting for trauma type, nerve injuries were more common among older individuals (hazard ratio [HR]: 1.08 per 10 years, 95% confidence interval [CI], 1.05-1.10), women (HR: 1.44, 95% CI, 1.34-1.54), and those requiring inpatient admission for trauma (HR: 1.83, 95% CI, 1.64-2.0). Population density quartile was not significantly associated with nerve injury diagnosis (P = .062).
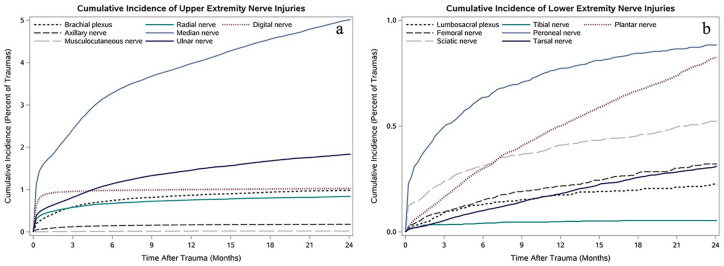
Only 9% of nerve injuries were identified by emergency department discharge, and only 38% of injuries were diagnosed by hospital discharge (Table 3). In general, upper extremity injuries were diagnosed earlier than lower extremity injuries (Figure 1). In the multivariable logistic regression models for brachial plexus injury and median nerve injury, patients requiring inpatient admission were more likely to be diagnosed within 1 year of trauma (brachial plexus injury model OR: 2.70, 95% CI, 1.54-4.76; median nerve injury model OR: 1.49, 95% CI, 1.23-1.82). Nonetheless, 12.2% of brachial plexus injuries and 21.3% of median nerve injuries were identified more than 1 year after extremity trauma (Table 4).
Figure 1.
Cumulative incidence curves for peripheral nerve injury diagnoses. (a) Cumulative incidences of upper extremity nerve injury diagnoses within 2 years of upper extremity trauma. (b) Cumulative incidence of lower extremity nerve injury diagnoses within 2 years of lower extremity trauma.
Table 4.
Cumulative Incidences of Individual Nerve Injuries at 90 days, 180 days, 1 Year, and 2 Years.
| Injured nerve | Patients (n) a | Cumulative incidence (%) |
|||
|---|---|---|---|---|---|
| 90 days | 180 days | 1 year | 2 years | ||
| Brachial plexus | 155 851 | 0.59 | 0.74 | 0.865 | 0.985 |
| Axillary nerve | 155 851 | 0.12 | 0.145 | 0.17 | 0.18 |
| Musculocutaneous nerve | 155 851 | 0.009 | 0.013 | 0.018 | 0.021 |
| Radial nerve | 235 551 | 0.58 | 0.67 | 0.75 | 0.84 |
| Median nerve | 235 551 | 2.41 | 3.27 | 3.96 | 5.03 |
| Ulnar nerve | 235 551 | 0.81 | 1.13 | 1.45 | 1.84 |
| Digital nerves | 618 677 | 0.96 | 0.98 | 1.00 | 1.03 |
| Lumbosacral plexus | 63 761 | 0.088 | 0.13 | 0.17 | 0.23 |
| Femoral nerve | 63 761 | 0.093 | 0.15 | 0.22 | 0.32 |
| Sciatic nerve | 80 436 | 0.235 | 0.31 | 0.41 | 0.53 |
| Tibial nerve | 81 880 | 0.034 | 0.041 | 0.048 | 0.054 |
| Peroneal nerve | 81 880 | 0.49 | 0.63 | 0.77 | 0.88 |
| Tarsal nerve | 271 199 | 0.053 | 0.099 | 0.18 | 0.31 |
| Plantar nerves | 271 199 | 0.16 | 0.30 | 0.50 | 0.83 |
Patients with at least one trauma in the anatomical group corresponding to each nerve injury. A total of 891 996 patients had at least one upper extremity trauma. A total of 365 466 patients had at least one lower extremity trauma.
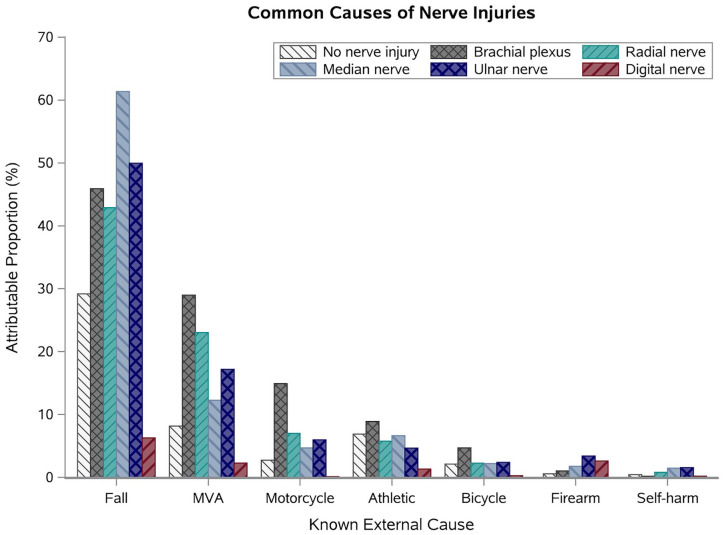
A relatively large proportion of brachial plexus injuries were diagnosed after motorcycle and motorized vehicle crashes (Figure 2). Indeed, the brachial plexus was the most common nerve injury among patients involved in motorcycle crashes, occurring in 0.7% of crashes. However, the majority of brachial plexus, median nerve, ulnar nerve, and radial nerve injuries were associated with falls.
Figure 2.
Among patients with known mechanisms of traumatic injury (E-codes), proportions of upper extremity nerve injuries that were associated with 7 common mechanisms.
Note. MVA represents motorized vehicle accidents. Fifty percent of ulnar nerve injuries (dark blue, cross pattern) were associated with falls. In comparison, falls were experienced by 29% of patients who were not diagnosed with any upper extremity nerve injury (light gray, thin diagonal pattern).
Individuals with upper extremity nerve injuries were significantly more likely to be diagnosed with chronic pain (P < .0001), use occupational therapy (P < .0001), and use physical therapy (P < .0001) more than 90 days after the index trauma (Table 5). Notably, patients who resided in more urbanized areas were more likely to use occupational and physical therapy and were less likely to be diagnosed with chronic pain than patients in less urbanized areas. Nerve injury was not significantly associated with disability diagnosis, although this diagnosis was only present in 831 patients (0.07%) in this cohort.
Table 5.
Multivariable Regression Models for Chronic Pain, Disability, Use of Occupational Therapy, and Use of Physical Therapy More Than 90 days After Upper Extremity Traumatic Injury.
| Variable | Chronic pain |
Disability |
Physical therapy |
Occupational therapy |
||||
|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Nerve injury a | 5.91* | 4.29-8.15 | 10.90 | 0.72-165 | 10.72* | 8.80-13.06 | 19.20* | 15.38-23.96 |
| Age (year) | 1.021* | 1.020-1.022 | 1.028* | 1.017-1.039 | 1.022* | 1.022-1.023 | 1.020* | 1.019-1.021 |
| Inpatient admission | 5.97* | 4.55-7.82 | 2.98* | 2.00-4.45 | 1.61* | 1.56-1.66 | 1.74* | 1.67-1.80 |
| Male | 0.53* | 0.45-0.62 | 0.67* | 0.51-0.87 | 0.75* | 0.74-0.76 | 0.75* | 0.73-0.76 |
| Population density | ||||||||
| Highest quartile | 0.69* | 0.67-0.71 | 0.98 | 0.69-1.39 | 1.20* | 1.18-1.22 | 1.62* | 1.57-1.66 |
| Third quartile | 0.82* | 0.79-0.86 | 0.67 | 0.42-1.07 | 1.14* | 1.12-1.17 | 1.38* | 1.34-1.43 |
| Second quartile | 0.90* | 0.86-0.95 | 0.77 | 0.44-1.34 | 1.13* | 1.10-1.16 | 1.26* | 1.21-1.31 |
| Lowest quartile | 0.94 | 0.90-0.99 | 0.40 | 0.18-0.88 | 1.04 | 1.01-1.07 | 1.05 | 1.00-1.10 |
| Not in an MSA | — | — | — | — | — | — | — | — |
| Injury type b | ||||||||
| Crush | 1.05 | 0.96-1.15 | 1.33 | 0.55-3.25 | 0.96 | 0.92-1.00 | 0.96 | 0.89-1.02 |
| Dislocation | 0.70* | 0.65-0.74 | 0.86 | 0.46-1.60 | 1.38* | 1.34-1.42 | 1.24* | 1.19-1.29 |
| Fracture | 1.16 | 0.98-1.38 | 1.18 | 0.79-1.77 | 0.97 | 0.95-0.99 | 1.04 | 1.01-1.07 |
| Open wound | 0.80* | 0.77-0.84 | 0.76 | 0.50-1.15 | 0.88* | 0.87-0.90 | 0.86* | 0.83-0.88 |
| Unspecified | 2.15* | 1.66-2.78 | 1.14 | 0.69-1.90 | 1.17* | 1.14-1.20 | 1.15* | 1.11-1.191 |
Note. HR = hazard ratios; CI = confidence interval; MSA = metropolitan statistical area.
Patients with any upper extremity injury, including brachial plexus injury, musculocutaneous nerve injury, axillary nerve injury, median nerve injury, ulnar nerve injury, radial nerve injury, and digital nerve injuries.
Injuries to the upper extremity. An individual patient could have multiple injury types.
Indicates P-values < .005.
Discussion
As the potential for restored function after nerve injury continues to improve,26-29 it is imperative that: (1) nerve injuries are identified early; and that (2) surgeons are provided with the training and resources to appropriately manage them. Achieving these goals requires an understanding of the epidemiology of traumatic nerve injury.
We demonstrate that peripheral nerve injuries are relatively common in patients with history of extremity trauma. The overall incidence of 2.3% is 38% higher than reported in an influential study by Taylor et al, 11 which only included nerve injuries identified within the first 90 days of injury using a dataset from 1998. Indeed, 36% of upper extremity nerve injuries and 71% of lower extremity nerve injuries in our cohort were diagnosed beyond 90 days. The overall incidence at 90 days was 1.3% (1.7% for upper extremity traumas and 0.3% for lower extremity traumas), suggesting that early identification of these injuries has not substantially improved since 1998.
We also report that 2.1% of hospitalized patients with extremity traumas (4% for upper extremity traumas and 0.5% for lower extremity traumas) were diagnosed with nerve injuries by the time of hospital discharge. This corroborates findings of a recent German study, which identified nerve injuries in 3.3% of hospitalized upper extremity trauma patients, 15 and a highly cited Canadian study, which reported peripheral nerve injuries in 2.8% of extremity trauma patients by hospital discharge. 14 However, the 2-year incidence of nerve injury among hospitalized trauma patients in our cohort was nearly double these previous estimates, suggesting that the true prevalence of nerve injury after severe trauma has been underestimated.
Given the time-sensitive nature of nerve reconstruction, nerve injuries more severe than neuropraxia should be identified as soon as possible after trauma. It is generally agreed that reconstruction should occur before 12 months after injury for optimal outcomes.16,21 However, the incidence curves for nerve injuries (Figure 1) varied widely in our cohort. Incidence likely depends on each nerve’s anatomic distribution and topography as well as the complex interplay between symptom severity, patient awareness, practitioner knowledge, and available treatments. A more readily apparent nerve injury is likely to be diagnosed sooner, and its incidence curve will reach an early plateau (eg, digital nerve injuries). For other nerve injuries, such as those in the lower extremity or those masked by concomitant injuries, identification may be more difficult and, thus, diagnosis more delayed. The etiology of a neuropathy, other than traumatic transection, is also often unknown. Scarring, inflammation, or compensatory changes in behavior after a trauma may lead to the development of compression neuropathies months to years later. Indeed, carpal tunnel syndrome may explain the relatively high incidence of median nerve injuries in this cohort as well as the continued rise in median nerve injury diagnoses 2 years after trauma.
Future Directions
Traumatic nerve injuries are predominantly managed at large, tertiary referral centers. However, the results of this study suggest that the risk of nerve injury per trauma does not depend on local population density. Therefore, there is a need to improve recognition of these injuries at both academic and community centers. There is also a need to understand where patients receive their first medical contact, from where and to whom they are referred for specialized evaluation, and who first diagnoses their nerve injury. The answers to these questions, unavailable in this dataset, would shed light on associations identified in this study and could be used to improve the overall treatment of nerve injuries through building capacity in rural settings.
In the months and years following traumatic injury, chronic pain and functional deficits may be inadequately managed by providers untrained in the identification and treatment of nerve injuries. Indeed, timely evaluation by a peripheral nerve specialist is often only possible if patients are referred by nonexperts who are aware of these injuries and their sequelae. Each medical contact after injury is an opportunity for referral to a nerve specialist. As the frequency of medical contacts decreases in the months to years after injury, the window of opportunity to treat a nerve injury narrows. Patients may be lost to follow-up or may seek evaluation years after injury, once their pain or functional recovery has plateaued.
Improving identification and timely referral of nerve injuries may involve increased funding for continuing medical education for general practitioners, trauma surgeons, and/or emergency department staff. Such activities can provide supplemental training on conducting a secondary survey, when to suspect a nerve injury, how to further investigate a potential injury, and where to refer a patient for additional evaluation. Improved public awareness of nerve injuries may also assist in injury prevention. For example, awareness of the association between motorcycle crashes and brachial plexus injuries may promote adherence to simple and inexpensive behaviors, such as wearing reflective clothing or using daytime headlights, that have been shown to significantly reduce motorcycle crashes.30,31 Additionally, an understanding of the types of traumas most associated with brachial plexus injury may help policymakers and companies improve performance specifications for motorcycle protective clothing.32,33
Multiple national databases were considered for this study, including the Healthcare Cost and Utilization Project (HCUP) family of databases; each database has advantages and limitations for answering specific questions. The MarketScan database was selected because it provided national, longitudinal information on insured patients across multiple practice settings. Therefore, we felt that this database maximized the chance of capturing traumatic nerve injuries. Other databases, such as HCUP Nationwide Emergency Department Sample, include all payers and offer more complete information on patient comorbidities, but in more focused treatment settings (eg, emergency department only). Having described the national incidence of nerve injuries after trauma, future studies may utilize other databases to examine the overall economic, and societal burden of nerve injuries.
Limitations
This study has several limitations inherent in retrospective reviews of administrative datasets. Trauma and nerve injury diagnoses were dependent on ICD-9-CM and CPT-4 coding rather than medical records. International Classification of Diseases coding may be inconsistent or unreliable, and it was impossible to ascertain the accuracy of diagnoses. Even in situations where they are properly entered, ICD codes often cannot capture the full clinical presentation, such as severity of soft tissue injury, concomitant injuries, or other complicating factors. While only nerve injuries corresponding to traumas in plausible anatomic areas were included, ICD-9-CM coding does not specify the location of individual nerve injuries or whether an injury was a consequence of the documented trauma. Additionally, a patient with a trauma coded to a specific area (eg, hand) may experience a second trauma (eg, a finger laceration) at a later date and not be evaluated in an emergency department. Even if this second trauma were the true cause of a digital nerve injury, the nerve injury would appear to be linked to the first, unrelated trauma. As such, we were unable to establish a causal relationship between traumas and nerve injuries; we report the incidence of nerve injuries in a trauma population rather than reporting the proportion of traumas causing nerve injury. Similarly, we identified a strong association between nerve injury and chronic pain, use of physical therapy, and occupational therapy, but we were not able to determine the specific reason for a chronic pain diagnosis or focus of therapy. It is possible that a polytrauma patient could experience chronic pain unrelated to the nerve injury, and the statistical relationships reported in our models should not be interpreted as casual. Polytrauma patients were not excluded from this cohort, as this would have removed the subset of patients experiencing highest impact energy and would have likely resulted in inappropriately low incidence estimates.
Nonetheless, the incidences reported in this study are likely underestimates. Nerve injuries may have been excluded simply because their associated traumas were not coded at the time of emergency department presentation or hospitalization. We also could not evaluate patients diagnosed with traumas outside of emergency departments, and we could not document undiagnosed nerve injuries. Moreover, our cohort only included patients with employer-based insurance, and insurance status may reflect important differences in environment, lifestyle, and high-risk behaviors that may influence risk of injury. On the other hand, patients with insurance may be more likely to receive medical evaluation in the event of an injury and more likely to be diagnosed with a nerve injury if present. Because only nerve injuries that were diagnosed could be included, the apparent incidence of nerve injuries in an uninsured trauma population would likely still underestimate the true incidence. The types of traumas sustained by an insured, working population are almost certainly different from those in the general trauma population, which tends to be younger and often uninsured. 13 However, we feel there is value in understanding the mechanisms of injury in this patient cohort, such as the association between motorcycle crashes and brachial plexus injury, even if the distribution of injuries differs from the overall trauma population.
Our sample also only included patients under the age of 65, which further limits generalizability of our results. While patients in this cohort tended to be older than the average United States trauma population, 13 the fact that most traumas are experienced by relatively young men does not necessarily assist in identifying nerve injuries clinically. Indeed, our results suggest that older individuals are more likely to be diagnosed with nerve injury than younger individuals, when adjusting for trauma type. This corroborates findings from previous studies demonstrating that older individuals tend to sustain more severe injuries from the same impact energy. 34 Although the MarketScan database may not be representative of United States traumas, our incidences are reported as per trauma rather than per person in the general population.
Conclusion
Nerve injuries were relatively common in this cohort of over 1.2 million patients with employer-sponsored health plans. The overall incidence of upper extremity nerve injury was 2.6% by 2 years after trauma, and patients with these injuries were more likely to be diagnosed with chronic pain and to use physical therapy and occupational therapy services. Despite recent advancements in the treatment of nerve injuries, only a minority of injuries were diagnosed by the time of emergency department or hospital discharge. Our findings support the need for increased practitioner awareness of nerve injuries in both academic and community settings.
Supplemental Material
Supplemental material, Supplemental_material for Incidence of Nerve Injury After Extremity Trauma in the United States by William M. Padovano, Jana Dengler, Megan M. Patterson, Andrew Yee, Alison K. Snyder-Warwick, Matthew D. Wood, Amy M. Moore and Susan E. Mackinnon in HAND
Footnotes
Supplemental material is available in the online version of the article.
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: The study was determined to be exempt from human subjects’ regulation by our Institutional Review Board.
Statement of Informed Consent: This study involved analyses of the IBM® MarketScan® Commercial Database, in which patient data are de-identified in accordance to the Health Instance Portability and Accountability Act. Therefore, no informed consent for this study was feasible or necessary. IBM Watson Health and MarketScan are trademarks of IBM Corporation in the United States, other countries or both.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research reported in this publication involved services provided by the Center for Administrative Data Research, which is supported in part by the Washington University Institute of Clinical and Translational Sciences grant UL1 TR002345 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH) and Grant Number R24 HS19455 through the Agency for Healthcare Research and Quality (AHRQ). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH.
ORCID iDs: Megan M. Patterson  https://orcid.org/0000-0001-7748-7759
https://orcid.org/0000-0001-7748-7759
Matthew D. Wood  https://orcid.org/0000-0001-8132-6827
https://orcid.org/0000-0001-8132-6827
Susan E. Mackinnon  https://orcid.org/0000-0002-5561-6027
https://orcid.org/0000-0002-5561-6027
References
- 1. Chemnitz A, Dahlin LB, Carlsson IK. Consequences and adaptation in daily life–patients’ experiences three decades after a nerve injury sustained in adolescence. BMC Musculoskel Dis. 2013;14(1):252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Novak CB, Anastakis DJ, Beaton DE, et al. Relationships among pain disability, pain intensity, illness intrusiveness, and upper extremity disability in patients with traumatic peripheral nerve injury. J Hand Surg Am. 2010;35(10):1633-1639. [DOI] [PubMed] [Google Scholar]
- 3. Novak CB, Anastakis DJ, Beaton DE, et al. Biomedical and psychosocial factors associated with disability after peripheral nerve injury. J Bone Joint Surg Am. 2011;93(10):929-936. [DOI] [PubMed] [Google Scholar]
- 4. Bailey R, Kaskutas V, Fox I, et al. Effect of upper extremity nerve damage on activity participation, pain, depression, and quality of life. J Hand Surg Am. 2009;34(9):1682-1688. [DOI] [PubMed] [Google Scholar]
- 5. Dijkers M. Quality of life of individuals with spinal cord injury: a review of conceptualization, measurement, and research findings. J Rehabil Res Dev. 2005;42(3):87-110. [DOI] [PubMed] [Google Scholar]
- 6. Dolan R, Butler J, Murphy S, et al. Health-related quality of life and functional outcomes following nerve transfers for traumatic upper brachial plexus injuries. J Hand Surg Eur Vol. 2012;37(7):642-651. [DOI] [PubMed] [Google Scholar]
- 7. Domeshek LF, Krauss EM, Snyder-Warwick AK, et al. Surgical treatment of neuromas improves patient-reported pain, depression, and quality of life. Plast Reconstr Surg. 2017; 139(2):407-418. [DOI] [PubMed] [Google Scholar]
- 8. Ciaramitaro P, Mondelli M, Logullo F, et al. Traumatic peripheral nerve injuries: epidemiological findings, neuropathic pain and quality of life in 158 patients. J Peripher Nerv Syst. 2010;15(2):120-127. [DOI] [PubMed] [Google Scholar]
- 9. Jaquet J-B, Luijsterburg AJ, Kalmijn S, et al. Median, ulnar, and combined median-ulnar nerve injuries: functional outcome and return to productivity. J Trauma. 2001;51(4):687-692. [DOI] [PubMed] [Google Scholar]
- 10. Lee B, Cripps R, Fitzharris M, et al. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 2014;52(2):110-116. [DOI] [PubMed] [Google Scholar]
- 11. Taylor CA, Braza D, Rice JB, et al. The incidence of peripheral nerve injury in extremity trauma. Am J Phys Med Rehabil. 2008;87(5):381-385. [DOI] [PubMed] [Google Scholar]
- 12. Ootes D, Lambers KT, Ring DC. The epidemiology of upper extremity injuries presenting to the emergency department in the United States. Hand. 2012;7(1):18-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wenzinger E, Rivera-Barrios A, Gonzalez G, et al. Trends in upper extremity injuries presenting to US emergency departments. Hand. 2017;14:408-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Noble J, Munro CA, Prasad VS, et al. Analysis of upper and lower extremity peripheral nerve injuries in a population of patients with multiple injuries. J Trauma. 1998;45(1):116-122. [DOI] [PubMed] [Google Scholar]
- 15. Huckhagel T, Nüchtern J, Regelsberger J, et al. Nerve injury in severe trauma with upper extremity involvement: evaluation of 49,382 patients from the TraumaRegister DGU® between 2002 and 2015. Scand J Trauma Resusc Emerg Med. 2018;26(1):76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dy CJ, Baty J, Saeed MJ, et al. A population-based analysis of time to surgery and travel distances for brachial plexus surgery. J Hand Surg Am. 2016;41(9):903-909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ray WZ, Mackinnon SE. Management of nerve gaps: autografts, allografts, nerve transfers, and end-to-side neurorrhaphy. Exp Neurol. 2010;223(1):77-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Griffin JW, Hogan MV, Chhabra AB, et al. Peripheral nerve repair and reconstruction. J Bone Joint Surg Am. 2013;95(23):2144-2151. [DOI] [PubMed] [Google Scholar]
- 19. Roganovic Z, Pavlicevic G. Difference in recovery potential of peripheral nerves after graft repairs. Neurosurgery. 2006; 59(3):621-633. [DOI] [PubMed] [Google Scholar]
- 20. Tung TH, Mackinnon SE. Nerve transfers: indications, techniques, and outcomes. J Hand Surg Am. 2010;35(2):332-341. [DOI] [PubMed] [Google Scholar]
- 21. Moore AM. Nerve transfers to restore upper extremity function: a paradigm shift. Front Neurol. 2014;5:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Giuffre JL, Kakar S, Bishop AT, et al. Current concepts of the treatment of adult brachial plexus injuries. J Hand Surg Am. 2010;35(4):678-688. [DOI] [PubMed] [Google Scholar]
- 23. Mackinnon SE. Future perspectives in the management of nerve injuries. J Reconstr Microsurg. 2018;34(9):672-674. [DOI] [PubMed] [Google Scholar]
- 24. Mackinnon SE. Discussion: state-of-the-art techniques in treating peripheral nerve injury. Plast Reconstr Surg. 2018;141(3):711-712. [DOI] [PubMed] [Google Scholar]
- 25. Benchimol EI, Smeeth L, Guttmann A, et al. The reporting of studies conducted using observational routinely-collected health data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Kubiak CA, Kung TA, Brown DL, et al. State-of-the-art techniques in treating peripheral nerve injury. Plast Reconstr Surg. 2018;141(3):702-710. [DOI] [PubMed] [Google Scholar]
- 27. Brennan MF, Debas HT. Surgical education in the United States: portents for change. Ann Surg. 2004;240(4):565-572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Demartines N, Mutter D, Vix M, et al. Assessment of telemedicine in surgical education and patient care. Ann Surg. 2000;231(2):282-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yee A, Padovano WM, Fox IK, et al. Video-based learning in surgery: establishing surgeon engagement and utilization of variable-duration videos. Ann Surg. 2019. [DOI] [PubMed] [Google Scholar]
- 30. Lin M-R, Kraus JF. A review of risk factors and patterns of motorcycle injuries. Acc Anal Prev. 2009;41(4):710-722. [DOI] [PubMed] [Google Scholar]
- 31. Wells S, Mullin B, Norton R, et al. Motorcycle rider conspicuity and crash related injury: case-control study. BMJ. 2004;328(7444):857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. de Rome L, Meredith L, Ivers R, et al. Validation of the principles of injury risk zones for motorcycle protective clothing. J Safety Res. 2014;50:83-87. [DOI] [PubMed] [Google Scholar]
- 33. de Rome L, Ivers R, Fitzharris M, et al. Effectiveness of motorcycle protective clothing: Riders’ health outcomes in the six months following a crash. Injury. 2012;43(12):2035-2045. [DOI] [PubMed] [Google Scholar]
- 34. Sterling DA, O’Connor JA, Bonadies J. Geriatric falls: injury severity is high and disproportionate to mechanism. J Trauma. 2001;50(1):116-119. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental_material for Incidence of Nerve Injury After Extremity Trauma in the United States by William M. Padovano, Jana Dengler, Megan M. Patterson, Andrew Yee, Alison K. Snyder-Warwick, Matthew D. Wood, Amy M. Moore and Susan E. Mackinnon in HAND