Abstract
Background
Neurological manifestations of COVID-19 are thought to be associated with the disease severity of COVID-19 and poor clinical outcomes. Dysregulated immune responses are considered to be mediating such complications. Our case illustrates multiple critical neurological complications simultaneously developed in a patient with non-severe COVID-19 and successful recovery with a multifaceted therapeutic approach. The cerebrospinal fluid (CSF) interleukin-6 (IL-6) level was temporally correlated with the clinical severity of the status epilepticus in our patient, suggesting a causal relationship.
Case presentation
A previously healthy 20-year-old female patient presented with a first-onset seizure. Concomitant non-severe COVID-19 pneumonia was diagnosed. CSF study showed lymphocytic pleocytosis with elevated IL-6 levels in CSF. During hospitalization under the diagnosis of autoimmune encephalitis, status epilepticus developed, and the seizure frequency was temporally correlated with the CSF IL-6 level. Furthermore, a new embolic stroke developed without a significant cardioembolic source. Contrary to the exacerbated COVID-19-associated neurological complications, COVID-19 pneumonia was cleared entirely. After treatment with antiseizure medications, antithrombotics, antiviral agents, and immunotherapy, the patient was discharged with near-complete recovery.
Conclusion
Active serological, and radiological evaluation can be helpful even in non-severe COVID-19, and multidimensional treatment strategies, including immunotherapy, can successfully reverse the neurological complication.
Keywords: COVID-19, Status epilepticus, Encephalitis, Stroke, Interleukin-6
Background
Neurological manifestations of coronavirus disease 2019 (COVID-19) can occur, which are known to be associated with disease severity of COVID-19 and poor clinical outcomes [1]. Various neurotropic properties of the SARS-CoV-2, including the hematogenous and neuronal transmission and other neurovirulent mechanisms such as hypoxia-related, inflammation-related, and angiotensin-converting enzyme-2 binding-related neuroinvasion have been previously suggested [2, 3]. Among many neurological syndromes of COVID-19, serious neurological complications such as seizures, encephalitis, and stroke have been previously reported. Seizures accounted for 0.5–1% of the neurological complications and were commonly associated with systemic derangements, suggesting acute symptomatic seizures [4]. Encephalitis showed an incidence rate of 0.25% among all COVID-19 and was associated with significant morbidity and mortality [5]. Ischemic strokes occurring in COVID-19 patients were usually associated with underlying cardiovascular risk factors [6]; however, thrombogenic vasculopathy of COVID-19 has also been suggested in young patients [7].
Herein, we describe a patient with multiple critical neurological complications with concomitant non-severe COVID-19 and successful recovery after a multifaceted treatment strategy.
Case presentation
Our patient was a previously healthy 20-year-old woman with unremarkable medical/neurological history. She presented with a first-onset focal tonic-clonic seizure on her left face and arm, followed by a drowsy mentality. The family reported that the patient experienced an unusual personality change from a week ago, exhibiting reckless and violent driving. The day before the hospital visit, the patient complained of dizziness and somnolence. She did not have a history of febrile seizures or any family history of seizure disorders. On presentation, she had an unnoticed fever, for which the polymerase chain reaction (PCR) for SARS-CoV-2 on nasal swab was tested and yielded a positive result. Vital signs were normal, with a respiratory rate of 18/min and SpO2 of 98% in room air. The arterial blood gas analysis was within the normal range, revealing pH 7.40, pCO2 37.6, pO2 84.6, and HCO3 23.4.
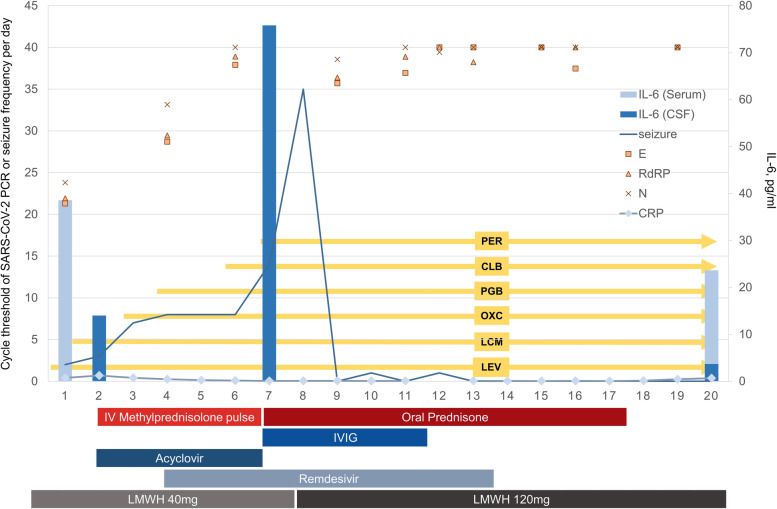
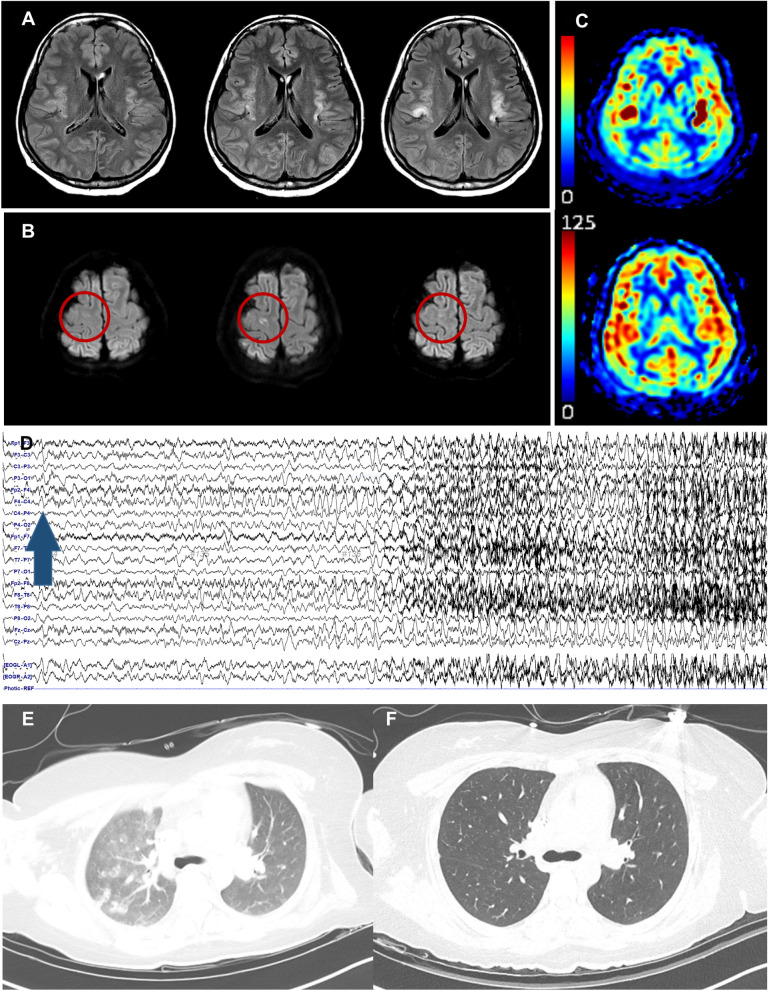
The progress of the patient is depicted in Fig. 1. Upon admission, focal seizures persisted, and continuous video-electroencephalogram (EEG) monitoring showed repeated high amplitude polymorphic delta activities from the right frontotemporal area evolving to generalized 1-2 Hz spike-wave discharges, suggesting an impending focal status epilepticus (Fig. 2). A cerebrospinal fluid (CSF) study showed lymphocytic pleocytosis (white blood cells 18 /ul, 93% lymphocyte) with CSF interleukin-6 (IL-6) level of 14.0 pg/ml, while a PCR test for SARS-CoV-2 in CSF was negative. Serum IL-6 was mildly elevated to 21.7 pg/ml, while serum C-reactive protein (CRP) was normal (0.70 mg/dl). Pathogen screening panels for serum and CSF included herpes simplex virus, varicella-zoster virus, enterovirus, tuberculosis, Ebstein-Barr virus, toxoplasmosis, and syphilis which came back negative. Brain magnetic resonance imaging (MRI) showed diffuse cortical high signal intensities, especially on bilateral insula with increased arterial spin labeling signals. Chest computed tomography (CT) showed patchy ground-glass opacities on bilateral lung fields, compatible with COVID-19 pneumonia. Serial images of brain MRI and chest CT are depicted in Fig. 2.
Fig. 1.
A brief description of the progress of the patient. Note that CSF IL-6 (light blue bar graph) level is temporally correlated with the daily seizure frequency (line graph). SARS-CoV-2 PCR cycle threshold values for each gene (E, RdRP, N) are marked as square, triangle, and cross. Serum CRP level is shown in rhombus with connecting lines and was maintained below 1 mg/dl throughout the treatment period. CLB, clobazam; CRP, C-reactive protein; CSF, cerebrospinal fluid; IL-6, interleukin-6; IV, intravenous; IVIG, intravenous immunoglobulin G; LCM, lacosamide; LEV, levetiracetam; LMWH, low molecular weight heparin; OXC, oxcarbazepine; PCR, polymerase chain reaction; PER, perampanel; PGB, pregabalin
Fig. 2.
A-C are magnetic resonance imaging findings along the treatment period. A shows fluid-attenuated inversion recovery images at presentation, 7th day, and 15th day, from left to right. Note that high signal intensities involving bilateral insula intensify over time. B shows diffusion-weighted imaging at presentation, 7th day, and 15th day, from left to right. The red circle indicates the evolution of ischemic stroke lesion in the right frontal lobe, which developed on the 7th day and normalized on the 15th day. A and B show different aging stages of each lesion, supporting that the newly developed focal diffusion restriction in B is more likely due to an ischemic nature. C shows arterial spin labeling signals at presentation and two months after seizure resolution, from top to bottom. Note that the focal increase in bilateral insula, suggestive of ictal perfusion increase, is resolved. D shows the electroencephalogram findings of the patient. High amplitude polymorphic delta activities from the right frontotemporal area evolving to generalized 1-2 Hz spike-wave discharges were noted. The blue arrow indicates seizure onset from the right frontal and anterior temporal region. E is a chest computed tomography (CT) finding at presentation, which shows patchy ground-glass opacities in the right upper lung field, suggestive of COVID-19 pneumonia. F is a follow-up chest CT on day 10. Previously seen COVID-19 pneumonia is completely cleared
Given the subacute onset of neuropsychiatric symptoms with new-onset focal status epilepticus and CSF pleocytosis, a tentative diagnosis of probable autoimmune encephalitis was made. Antibodies against neuronal synaptic or intraneuronal antigens were negative in serum and CSF, and no solid tumor was found. Extensive screening tests for the autoimmune diseases came back negative as well, including thyroid panel, vasculitis lab, immunoglobulin G subclass, and anti-ganglioside antibodies. Clinical and EEG seizures progressively aggravated up to 35 per day during the first week. Despite the persistent seizures, intravenous (IV) anesthetic therapy was not considered because the seizures remained focal with only occasional generalization, and therefore the vital signs remained intact.
On day 7, a newly developed embolic stroke on the right frontal lobe was detected on a follow-up MRI. Considering the extensive seizure-related changes involving both insula areas, the new isolated focal lesion was thought of as evidence of an embolic stroke. Etiological evaluation of stroke revealed negative results, including transthoracic echocardiogram, electrocardiogram, Holter monitoring, and transcranial Doppler bubble study to rule out patent foramen ovale. Initially elevated D-dimer level (1.48 μg/ml) was decreased to 1.00 μg/ml. Routine thromboprophylaxis using low molecular weight heparin was increased to a therapeutic dose of secondary stroke prevention (2 mg/kg). The follow-up CSF study showed more increased IL-6 level of 75.8 pg/ml. Contrary to the exacerbated COVID-19-associated neurological complications, the follow-up chest CT revealed completely cleared bilateral lung fields. Daily followed serum CRP level was maintained under 1 mg/dl.
Along with IV acyclovir and remdesivir, IV methylprednisolone pulse therapy was given to treat autoimmune encephalitis. Because the seizures persisted after the methylprednisolone, IV immunoglobulin G was administrated next, to which the patient started to respond. The seizures finally halted on the 12th day, and her neurological deficits gradually resolved thereafter. During the course of the treatment, her otherwise vital signs remained stable and intact oxygenation was maintained. A Follow-up study revealed normalized CSF IL-6 level to 3.7 pg/ml and decreased serum IL-6 level to 13.3 pg/ml. After 39 days of hospitalization, the patient successfully recovered from COVID-19 pneumonia, encephalitis, status epilepticus, and stroke, and she was discharged home at a modified Rankin scale of 1.
Discussion and conclusions
Our case illustrates multiple critical neurological complications simultaneously developed in a patient with non-severe COVID-19 and successful recovery with a multifaceted therapeutic approach. The commonality in the development of the neurological complications observed in our patient can be characterized as dysregulated immune response, which led to thromboinflammation and neuroinflammation [8]. This alteration of immune homeostasis and subsequent pro-inflammatory conditions occurring in COVID-19 were previously thought to be positively correlated with the severity of the infection. However, our case distinctively shows multiple critical neurological manifestations precipitated by non-severe and even resolving state of pulmonary COVID-19.
The CSF IL-6 level was temporally correlated with the clinical severity of the status epilepticus in our patient, and the immunotherapies improved the patient’s condition, suggesting a causal relationship. This association with IL-6 and status epilepticus in our patient also raises the possibility of new-onset refractory status epilepticus (NORSE) diagnosis [9, 10]. However, we postulate that this specific case did not fall under the typical diagnosis of NORSE because of the course of the status epilepticus, which was characterized by rapid cessation without the use of IV anesthetic therapy and focal semiology or electrographic seizures without coma. The serological association between the disease severity of COVID-19 and serum IL-6 level as a key cytokine has been widely studied [11]. What is noteworthy about this particular case is that the dysregulated host response to SARS-CoV-2, represented by elevated CSF IL-6 and clinical manifestations, was confined to the extrapulmonary system, especially to the central nervous system (CNS). Although serum IL-6 level was not measured at the time of the most severe seizures, we speculate that the IL-6-mediated inflammatory response provoked by COVID-19 infection was limited to the CNS, considering the only mildly elevated initial serum IL-6 level while the pulmonary involvement was evident, and constantly normal-ranged other inflammatory markers, such as CRP.
Although we cannot confirm the exact immune mechanism by which the neuroinvasion occurred in this patient, the clear implication of our case is that multiple critical neurological complications by the immune response can occur in non-severe COVID-19. Also, a multidimensional therapeutic approach, especially with immunotherapy despite COVID-19, successfully reversed the neurological complications of COVID-19.
In conclusion, our case exemplifies a variety of severe neurological syndrome occurring in a non-severe COVID-19 patient and signifies an immunological aspect of neurovirulence in COVID-19. Our case thereby suggests that active neurological evaluation and multifaceted treatment can be helpful in COVID-19 patients, despite mild pulmonary manifestation.
Acknowledgments
Not applicable.
Abbreviations
- CNS
Central nervous system
- CRP
C-reactive protein
- CSF
Cerebrospinal fluid
- CT
Computed tomography
- EEG
Electroencephalogram
- IL-6
Interleukin-6
- IV
Intravenous
- MRI
Magnetic resonance imaging
- NORSE
New-onset refractory status epilepticus
- PCR
Polymerase chain reaction
Authors’ contributions
SK: data interpretation, drafted the work and approved the final version of the paper. YK, MK, and YC: data interpretation, revised the draft critically for important intellectual content, and approved the final version of the paper. JYC: conceptualization, substantial revision of the manuscript, and approved the final version of the manuscript. T-KJ: conceptualization and supervision of the study, data interpretation, revised the draft critically for important intellectual content, and approved the final version of the paper. All authors have seen and approved the manuscript being submitted.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The data supporting this study’s findings are available on request from the corresponding author [TJ Kim]. The data are not publicly available due [to them containing information that could compromise research participant privacy.]
Declarations
Ethics approval and consent to participate
Ethics approval was obtained from the Ajou University Hospital Institutional Review Board, and the board waived the need for patient consent. (AJIRB-MED-EXP-21-359).
Consent for publication
Written informed consent was obtained from the case patient for publication of this report and any accompanying images. A copy of the written consent is available for review by the Editor of this journal.
Competing interests
All authors report no disclosures of financial relationships (and those of their “immediate family members”) from the past two years.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chen X, Laurent S, Onur OA, et al. A systematic review of neurological symptoms and complications of COVID-19. J Neurol. 2021;268(2):392–402. doi: 10.1007/s00415-020-10067-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roy D, Ghosh R, Dubey S, Dubey MJ, Benito-Leon J, Kanti RB. Neurological and neuropsychiatric impacts of COVID-19 pandemic. Can J Neurol Sci. 2021;48(1):9–24. doi: 10.1017/cjn.2020.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bodro M, Compta Y, Sanchez-Valle R. Presentations and mechanisms of CNS disorders related to COVID-19. Neurol Neuroimmunol Neuroinflamm. 2020;8(1):e923. [DOI] [PMC free article] [PubMed]
- 4.Asadi-Pooya AA. Seizures associated with coronavirus infections. Seizure. 2020;79:49–52. doi: 10.1016/j.seizure.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siow I, Lee KS, Zhang JJY, Saffari SE, Ng A. Encephalitis as a neurological complication of COVID-19: a systematic review and meta-analysis of incidence, outcomes, and predictors. Eur J Neurol. 2021;28(10):3491–3502. doi: 10.1111/ene.14913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Qureshi AI, Baskett WI, Huang W, et al. Acute ischemic stroke and COVID-19: an analysis of 27 676 patients. Stroke. 2021;52(3):905–912. doi: 10.1161/STROKEAHA.120.031786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rahmawati PL, Tini K, Susilawathi NM, Wijayanti IAS, Samatra DP. Pathomechanism and Management of Stroke in COVID-19: review of Immunopathogenesis, coagulopathy, endothelial dysfunction, and downregulation of ACE2. J Clin Neurol. 2021;17(2):155–163. doi: 10.3988/jcn.2021.17.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gupta A, Madhavan MV, Sehgal K, et al. Extrapulmonary manifestations of COVID-19. Nat Med. 2020;26(7):1017–1032. doi: 10.1038/s41591-020-0968-3. [DOI] [PubMed] [Google Scholar]
- 9.Jun JS, Lee ST, Kim R, Chu K, Lee SK. Tocilizumab treatment for new onset refractory status epilepticus. Ann Neurol. 2018;84(6):940–945. doi: 10.1002/ana.25374. [DOI] [PubMed] [Google Scholar]
- 10.Sakuma H, Tanuma N, Kuki I, Takahashi Y, Shiomi M, Hayashi M. Intrathecal overproduction of pro-inflammatory cytokines and chemokines in febrile infection-related refractory status epilepticus. J Neurol Neurosurg Psychiatry. 2015;86(7):820–822. doi: 10.1136/jnnp-2014-309388. [DOI] [PubMed] [Google Scholar]
- 11.Jones SA, Hunter CA. Is IL-6 a key cytokine target for therapy in COVID-19? Nat Rev Immunol. 2021;21(6):337–339. doi: 10.1038/s41577-021-00553-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting this study’s findings are available on request from the corresponding author [TJ Kim]. The data are not publicly available due [to them containing information that could compromise research participant privacy.]