Abstract
The climate crisis provides a critical new lens through which health and health behaviors need to be viewed. This paper has three goals. First, it provides background on the climate crisis, the role of human behavior in creating this crisis, and the health impacts of climate change. Second, it proposes a multilevel, translational approach to investigating health behavior change in the context of the climate crisis. Third, it identifies specific challenges and opportunities for increasing the rigor of behavioral medicine research in the context of the climate crisis. The paper closes with a call for behavioral medicine to be responsive to the climate crisis.
Keywords: Behavioral medicine, Climate change, Global warming, Anthropocene, Mitigation, Adaptation, Health co-benefits
Climate change is transforming the planet and, consequently, exacerbating threats to human health. This paper offers a framework for remaking behavioral medicine research to address climate change and its impacts.
Implications.
Practice: Instilling a sense of connection, promoting empathy, and developing a vision for humankind as interdependent must be a priority if we are to foster the kinds of behaviors—individually and collectively—that will promote planetary health.
Policy: Ultimately, the goals of our work as behavioral medicine researchers, practitioners, and policy makers, in response to the crises resulting from climate change, must be to redefine individual health and health behaviors as part of planetary health, with a priority on identifying how to motivate individuals to see themselves as part of humankind and take collective action.
Research: Priorities for a behavioral medicine research agenda include (1) promoting behavior changes to facilitate planetary health, (2) identifying and developing behavioral interventions at multiple levels—from the individual to systems-level—to facilitate climate-resilient health behaviors, and (3) preparing ourselves and our patients for future shocks to physical, social, and health systems that will feel uncanny and alien.
The Climate Crisis
The climate crisis (and its attendant mass extinctions and ecological breakdown) is the most complex and consequential challenge humans have ever faced [1]. For the past 10,000 years, Earth has experienced an incredibly stable temperature, which yielded predictable seasons, favorable conditions for agriculture and complex social systems, and enough consistency in the frequency and intensity of “natural” threats to allow for reliable infrastructure development. Because nature was predictable, we were able to develop technologies, cities, economies, and other markers of civilization that allowed many of us to ignore it. That period, because it was so odd in geographical terms, was given a name: the Holocene. We had long assumed that this stability was the only and natural state of Earth’s systems, but we now know that burning fossil fuels for energy has caused many of Earth’s systems to change radically [2–5].
We now live in the Anthropocene, an era of hotter temperatures and more variable weather conditions (as well as other human-caused changes to natural systems) that threaten human lives and the continuity of human civilizations. The past 7 years were the hottest ever recorded globally, and we are unlikely to enjoy such cool conditions again, because most or all of the years in the next decade will continue to shatter record high temperatures [6]. Indeed, paleoclimatologists have consulted the geologic record for past eras that could serve as analogs for Earth’s near-future state, and found that, by the 2030s, the mid-Pliocene (3.3–3 million years ago) was the closest match [7]. The mid-Pliocene era is the most recent period with atmospheric CO2 comparable with the present (ca. 400 ppm), with mean annual surface temperatures approximately 1.8°C–3.6°C warmer than preindustrial temperatures (i.e., 1,850–1,900), reduced ice sheet extents, and increased sea levels. Just as pre-Holocene Earth was inhospitable to human life, we now face accelerating risk of a rapid, irreversible return to a state of extreme instability and unpredictability across many Earth systems simultaneously [8]. Although every living species has an ancestor that survived the mid-Pliocene, past global warming/cooling took place over millennia. No species has faced the unprecedented speed at which anthropogenic warming is occurring [9]. Scientific estimates of the year in which mean local climate conditions will fall outside of the range to which its human infrastructure and plants/animals have adapted (e.g., mean annual temperature exceed the highest previously observed temperature for the area, and do not return) fall between 2036 (for tropical regions with very low prior variance) and 2080 (for more variable areas, under optimistic emissions scenarios), with a global (optimistic emissions) date of 2069 [4].
The popular term for the thresholds in Earth’s dynamic climate and ecological systems, past which rapid, consequential changes would make them inhospitable to humans, is “tipping points” [10]. These tipping points are terrifying, because they signify shifts from the current, steadily worsening conditions according to well understood causal associations between human activity and environmental consequence, to nonlinear (runaway, cascading) changes of unknown speed and upper bound. Such changes could be locked in, and represent a transformative shift from a state in which human activity functions as a crucial protector of human civilization to one in which such activity instead contributes to destabilizing the planetary conditions on which we depend.
The Role of Humans in the Climate Crisis
The first and most pressing example of human contributors to destabilizing the Earth systems that sustain our civilizations is global heating. Currently, the defining feature of modern civilizations is that they require massive energy use to maintain the unprecedented productivity and annual growth that wealthy nations have come to expect [11, 12]. This expectation is itself a new development in human history, which grew out of the widespread availability of cheap, dense energy in the form of fossil fuels, and is inseparable from it [13]. By burning coal, oil, methane (marketed as “natural gas”), and other fossil fuels, some societies have become incredibly wealthy, but burning these fuels releases carbon dioxide, methane, and other greenhouse gases (GHG) into the atmosphere [14]. These GHG slow the natural release of heat from the Earth’s atmosphere into space, trapping heat from the sun that would otherwise radiate off the planet, which results in a steadily warming atmosphere. As the atmosphere heats up, melting of ice at Earth’s poles reduces the reflective surface area that would otherwise deflect much of the Sun’s energy away from Earth, further increasing global heating.
Many such positive feedback loops (vicious cycles) in environmental systems are operating at an accelerating pace [15]. As the Earth becomes hotter, some areas become drier, which increases the risk of wildfires [16]. Since trees are among the most important means for capturing and storing carbon dioxide so that it does not contribute to further warming, when trees burn, not only are those carbon sinks lost but also the carbon they held is immediately released into the atmosphere. For just one prominent example, the Amazon rainforest is crucial as a carbon sink (i.e., captures CO2 that would otherwise join existing CO2 in the atmosphere and accelerate global heating), and it contributes to the predictability of the water cycle and ocean currents [17, 18]. It also contains much of the planet’s biomass and biodiversity. Till date, 20% of the Amazon rainforest has been lost, due to corporate beef and soy production, as well as local ranching and farming. With higher temperatures and less rain, fires have also increased. Whereas 25% of all GHG since 1960 have been trapped by global trees and plants (with the Amazon accounting for much of that sink), researchers recently found that the Brazilian Amazon now emits more CO2 than it captures [19]. In the past decade, the discrepancy between the CO2 emitted during fires and the smaller amount captured by remaining trees was equivalent to the annual GHG emissions of Japan (one of the world’s largest emitters).
Similarly, Earth’s oceans capture 25% of anthropogenic GHG emissions annually (41% of all human GHG till date) [20], but their effectiveness has decreased by almost 1% per year since 1959 [21]. As the oceans trap more CO2, they become more acidic and less hospitable to marine life that aids CO2 capture (and serves as a foundational component of planetary food cycles), and as the Earth warms, water temperature increases also reduce oceans’ capacity to trap CO2 [22].
Human Health Consequences of Climate Change
Although large scale, systemic failures that threaten human civilizations are difficult to predict, because we have no experience with nonlinear catastrophic changes, we have already begun to see impacts of climate change and related environmental devastation for human health [23]. In a 2018 literature review, 27 dimensions of human health were impacted by climate change or its impacts between 1980 and 2014, with death, mental health, and disease the most commonly identified [24]. In the most vulnerable regions of the planet, water and resource scarcity have exacerbated political conflict and migration pressures [25]. Throughout the world, warming temperatures have increased the number and geographic range of insects that spread vector-borne diseases [26]. Drought and heatwaves have intensified, with concurrent increases in heat-related deaths [27, 28]. Extreme weather events have become more frequent and intense, and their range has increased [29]. As with any threat to human health and safety, wealthier nations are better able to adapt to these new and accelerating risks, even as they continue to emit GHG that worsen the threats [30, 31].
A parallel pattern of vulnerability exists within nations, with poorer regions within even the wealthiest nations bearing disproportionate exposure to climate change impacts [32], relative to their GHG contributions or the generational benefits of those emissions (i.e., even though many wealthy citizens of the US have been able to adopt “greener” lifestyles, their consumption of goods and services keeps their cumulative GHG footprint high, and they have received outsized public and private benefit from historical GHG emissions through familial wealth, national infrastructure, and artificially low prices for energy-intensive goods). Indeed, even at the state level, the share of state wealth held by the top 10% is positively associated with GHG emissions [33]. Across the United States, areas with greater concentration of capital have more resources to devote to climate adaptation (e.g., NYCs infrastructure for sea level rise), whereas poorer areas have been decimated by hurricanes and wildfires (e.g., New Orleans, parts of California). We have seen that, even during the same extreme weather event or wildfire, wealthy areas and their inhabitants are protected by governmental resource allocation or private deployment of firefighting and related services, so disasters increase wealth inequality locally [34]. Within US cities, wealthier neighborhoods are often significantly cooler than poorer neighborhoods due to tree cover, less asphalt and concrete to trap heat throughout the day and radiate heat at night. Furthermore, wealthier individuals are less likely to work outdoors, and more likely to have air conditioning during dangerous heatwaves [35]. In a 2009 study of 30 homes of older adults in Detroit, the average maximum indoor temperature was 95°F [36]. And since poverty in the United States is concentrated in Black, Indigenous, Latino/a, and other marginalized communities due to structural racism, the health consequences of climate change are disproportionately borne by racial and ethnic groups that have been minoritized. For example, the average BIPOC lives in a census tract with higher urban heat island intensity than non-Hispanic Whites in all but 6 of the 175 largest urbanized areas in the continental US [37]. The same historical, structural, and policy realities mean that BIPOC are at greater risk of chronic disease and are most vulnerable to—and least able to cope with—the dire health effects of climate change, thus widening existing disparities in health.
Human Behavior and Its Relationship to Health and Climate Change
Health-related behaviors, such as engaging in physical activity, eating a healthy diet, and maintaining an appropriate weight, are critically important in preventing or delaying chronic diseases and promoting optimal health and well-being (Nudelman and Shiloh, 2015). These behaviors also play an important role in adaptation to and mitigation of climate change, since promoting behaviors and policies that encourage healthy lifestyles—for example, adopting plant-based diets and engaging in more active transportation such as walking while reducing driving—can benefit both the prevention of chronic diseases and at the same time promote a healthy environment [38]. Thus, an important area of research is identifying how best to promote changes in individuals’ behaviors that both improve their health and reduce GHG emissions [39]. Can we find ways to meaningfully improve the behaviors that are linked to both human health and climate change, and thus simultaneously address these multiple, synergistic threats to human health?
With respect to individual behaviors that contribute GHG emissions, diet and transportation are the most important [38, 40]. Because of land use and carbon emissions associated with raising animals for human consumption, as well as methane produced by bovine digestive processes (in particular), diets low in meat and dairy produce the fewest emissions [41–43]. The other major behavioral determinant of GHG is transportation, with air travel producing the most emissions, and the cumulative emissions of gas-powered vehicles an important contributor [44, 45]. These two changes: adopting a vegan or vegetarian diet, and foregoing owning fossil-fuel powered cars, air travel and increasing active transportation (walking, bicycling) for daily commutes, would result in substantial individual GHG emissions reduction. Those same changes, framed as eating a healthier plant-based diet and increasing exercise, are also two of the most important behavioral contributors to healthy aging, reducing chronic disease risk, and improving quality of life. In addition, mitigating our use of energy sources (using fewer appliances and machines that produce substantial GHG) is a behavior change that can produce fewer GHG and thus should be targeted [46]. Thus, changing behaviors to improve health outcomes can have the co-benefit of improving the environment, and vice versa. A major focus of future research should involve the extent to which focusing on these co-benefits can stimulate effective behavioral changes that have larger, synergistic effects than attention to either of them alone [47, 48].
Human behaviors are not only directly linked to adverse changes in climate and the environment, and thus a critical target for reducing the threats to human health posed by climate change, but also these behaviors are themselves threatened by climate impacts [49–51]. We have already begun to see how climate change impacts the health behaviors that are crucial for individual health and well-being. Physical activity, and outdoor labor and exercise in particular, becomes dangerous at high temperatures [52]. We have seen sedentary behavior increase, and exercise decrease, for years, and extreme temperatures are associated with less activity [53, 54]. Indeed, some areas of the planet have already recorded heat index values above the threshold for human survivability [50]. We know that temperatures will continue to increase, but a rapid shift away from fossil fuels will cap the upper limit of that increase. Some research suggests that food availability and nutritional value will be impacted by climate change, even in wealthy nations, due to the impact of atmospheric carbon and harsh conditions on the nutritional content of vegetables [55–57]. Recent large-scale international studies of the effect of temperature increases on sleep (using actigraphy) and mood (using social media data) show large, consistent reduction in sleep [58] and worsened mood on hotter days [59].
Recognizing that many of the behaviors that improve individual and planetary health are identical is crucial to a comprehensive understanding of health itself [60]. Whereas many of the social trends of the past century have yielded an atomized view of self and other, and our technological developments have created physical and psychological distance between our daily experience and the natural systems that make life possible [61], the established scientific perspective (across multiple disciplines) is that our physical and psychological health are inseparable from the health of our planetary and local environmental systems [62]. A few conceptual models of the underlying unity of individual and planetary health have been offered, including the CDCs One Health initiative, and the Planetary Health concept in the environmental health literature [63]. By shifting our collective focus from individual and population health to planetary health, the implications for every aspect of our daily lives are profound. Changing individual diets and transportation patterns becomes only the first step in a radical reordering of priorities focused on protecting the natural and human systems that sustain us—as individuals, family members, community members, citizens, and as scientists.
Indeed, we cannot isolate the health effects of health behaviors from the contexts in which they occur. In this regard, it is clear that the importance of health behaviors for human survival increases as the atmosphere gets hotter and wetter. However, maintaining a healthy lifestyle throughout the lifespan, eating a healthy diet and engaging in physical activity, avoiding risky behaviors and engaging in self-care activities to maximize health and well-being (e.g., adherence to medication and health-promoting regimens) all become more challenging in a world characterized by climate and infrastructure instability in the places in which we live [64]. These threats have the potential to affect our health and health-related behaviors both directly and indirectly (see Chevance et al., 2021 for a first proposition of a conceptual model presenting the bi-directional associations between climate change outcomes and health behaviors).
For example, climate change can render our health systems more fragile and vulnerable to breakdowns, as when wildfires, extreme weather events and other climate-related crises cause the shutdown or reduced functioning of hospitals and clinics [26, 65, 66]. Our food systems are similarly vulnerable, with the availability, nutritional value, and supply chains on which our nutritional systems rely all affected by climate change, leading to more food insecurity, under-nutrition, malnutrition, and obesity (given a tendency to eat more low-quality but calorie-dense food). Hotter days make physical activity unsafe and impact sleep, resulting in circadian disruption (hotter nights can result in poorer sleep, especially in urban heat islands) and the adverse health effects of poor sleep. Extreme weather and weather disasters can exacerbate many risks and create societal conflict and instability, with resulting adverse health effects due to migration, increases in refugee crises, and struggles for resources in environments characterized by scarcity, conflict, and strife. These physical health threats imposed by climate change also threaten psychological and social well-being, with likely increases in depression, suicidality, violence, addictive behaviors and other psychosocial detriments [67]. As with all global harms, these impacts arrive earliest and cause the greatest harm in communities that have been historically marginalized and continue to experience the consequences of systemic racism, disinvestment, and discrimination.
Developing Strategies and Solutions to the Climate Crisis: A Multilevel, Translational Approach
Given the potentially broad-based impacts on health and health behaviors from climate change, mitigating climate change requires us to focus not just on individual behaviors, but to take a multilevel and translational approach. We must address multiple levels of influence from the individual’s behavior on GHG emissions, to family/household behaviors, to broader environmental and policy approaches (encouraging focus on the collective good, changing social norms, facilitating advocacy by individuals and groups). Till date, most work has estimated only how behavior can impact individual health and GHG emissions. Research should now begin to estimate how multilevel behavioral changes—from individual to policy change—can affect planetary health [including individual health; [68]].
Identifying Co-Occurring Climate Change and Health-Related Behaviors
Developing effective behavior changes that make a meaningful impact on climate change and the resulting threats to human health requires taking a solutions-oriented or strategic science approach: first specifying the goals, soliciting ideas from end-users, then identifying “drivers” of the relevant behaviors by individuals and groups, and developing and testing/evaluating strategies to engage the drivers and ultimately change the behavior. Use of behavior change frameworks such as the Science of Behavior Change (SOBC) experimental medicine approach and the Obesity-Related Behavioral Intervention Trials (ORBIT) model can be helpful in identifying underlying drivers of behavior that can be used as intervention targets, but these frameworks must be extended to address multiple levels of analysis, not just individual behavior change (Czajkowski et al., 2015; Powell et al., 2022; Nielsen et al., 2018). Methods can range from novel approaches to individual behavior change based on motivations unique to achieving co-benefits, to changing social norms via social marketing/social media, to natural experiments to evaluate how best to motivate individuals and groups to advocate policy solutions. Testing localized models of excess health and behavioral risk due to climate will allow for targeted interventions. Future risk prediction models should be tailored for vulnerable populations, including historically marginalized/racialized groups, recently hospitalized patients with chronic disease, etc.
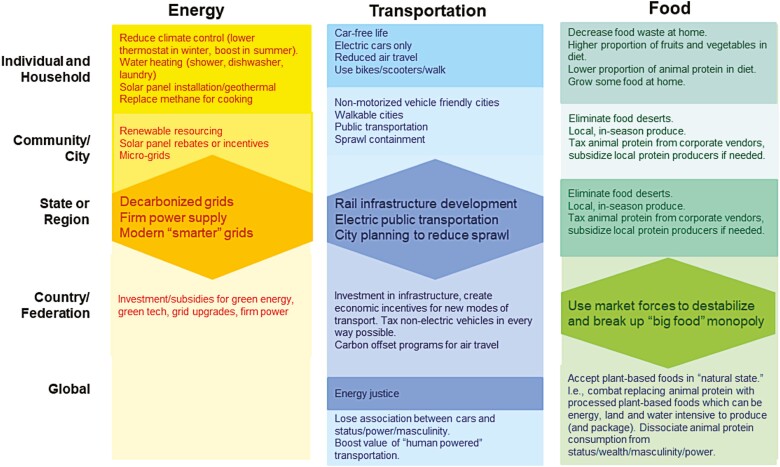
One approach for pursuing this ambitious new goal is to first identify high-impact climate change behaviors and define health behaviors that further these goals within these categories. As an example of this approach, our subcommittee of the SBM Presidential Working Group on Climate Change and Health first reviewed existing reports from advocacy groups and papers (e.g., Project Drawdown) that have estimated the climate change mitigation potential of individual and household behavior changes, where climate mitigation potential was typically measured as CO2 or other GHG emissions reductions. We then identified behaviors in the three “high potential impact” domains that also have high impact on human health (food/nutrition/agriculture, transportation and energy use); organized these behaviors according to how they might be addressed at multiple levels of analyses (individual level, family or household level, community/neighborhood level, government policy (City, State, Regional) level, country/federation level, and global/”human culture” level); and finally, identified mechanisms (“drivers”) of these behaviors at various levels of analysis that could be potential intervention targets.
Figure 1 provides examples of behaviors or actions that are useful for addressing the three “high impact” behavioral domains.
Fig 1.
Actions to mitigate climate change for three “high impact” behavioral domains at multiple levels.
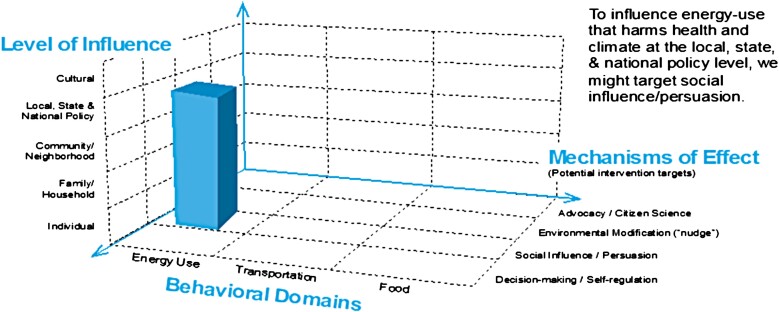
Figure 2 provides a potential framework that illustrates the potential of this approach and can be used to identify mechanisms or “drivers” of these behaviors at various levels of analysis that could be potential intervention targets.
Fig 2.
A framework that can be used to identify mechanisms or “drivers” of climate change-related behaviors at various levels of analysis.
Research on the topics that emerge from this conceptual matrix could take on many forms, for example:
Confirming the links between health-related benefits and individual climate change mitigation actions;
Modeling/estimating the magnitude of the impacts of climate change on health-related behaviors; and
Developing interventions that target the specific drivers of behaviors within domains, and evaluating their effects on climate change mitigation.
In addition to traditional definitions of “health behavior,” we must begin to focus on how climate change will impact behaviors relevant to mental and physical health. Parameters will include climate change estimates (i.e., local temperature, humidity, precipitation changes, extreme weather), behavioral sensitivity to climate parameters, and any moderation of the health behavior—mental/physical health association by climate parameters.
Given the inevitability of climate change, and the likely irreversible environmental changes that are already taking place we must also focus on behavioral adaptation to existing or future climate and environmental impacts. To do this, we will need to reimagine health behaviors/infrastructure for behaviors in a hotter/wetter context globally, with hyperlocal variation in climate impacts. Adaptive behaviors will be necessary to cope with: the fragility of the healthcare system (adapting health systems to boost resilience/access); fragility of the nutrition/food system (local microproduction, greening cities); impediments to physical activity (how to adapt without increasing GHG); and impacts on sleep (methods for cooling besides air conditioning, perhaps with emphasis on planting more trees to accelerate the greening of cities?). In addition, we will need to address risk exacerbation by investing in equitable resilience-building approaches, bolster individuals’ and populations’ capacity to cope with detriments to well-being due to stress, trauma, depression/anxiety and substance abuse brought on by climate-related crises, and identifying ways to deal with increased migration, refugee crises, and the stress, trauma and conflict that could potentially result from these effects. It is important to note that this is not an exhaustive list of changes that will require adaptation. Indeed, adapting to a changing climate and world will require maximal flexibility and the adoption of new behavioral strategies, along with the ability to reimagine wellbeing for a future in which our current complex systems fail to deliver security/stability. We will need to redefine individual well-being as contingent on our collective well-being, and individual behavior change will need to co-exist with engagement in collective action.
Transportation
The transportation sector accounts for 29% of all GHG emissions in the United States [69]. Transportation over land, and notably the use of individual cars, represents an important proportion of GHG emissions worldwide (e.g., 12% of total EU emissions and 59% of the transportation sector emissions in the United States). Estimates of GHG emissions reductions from interventions that promote replacing short trips by car with physically active modes (walking, bicycling; i.e., active transport) vary extensively from one study to another. For example, a quasi-experimental study conducted in New Zealand reported only a 1% reduction in CO2 emissions after 3 years of an intervention that combined walking and cycling infrastructure development and behavior change promotion at the scale of a city [70]. A recent systematic review of the GHG reductions and health co-benefits associated with active transport interventions found, unsurprisingly, that the intensity of the intervention was associated with its impact [39].
Energy
Household energy use accounts for 20% of individual GHG emissions in the United States (25% for wealthy individuals, due to larger home size). The energy used to heat and cool homes, power appliances and devices, and increasingly to charge vehicles, is often produced by burning fossil fuels. A recent study of 93 million US homes [71] found that completely decarbonizing the US electrical grid would achieve the Paris Agreement’s target of a 28% reduction in GHG by 2025 (to stay below 2°C warming); however, decarbonizing the grid is not enough to meet 2050 targets, due to the growth of housing stock. Both decarbonizing the grid and changing carbon-intensive behavior (by wealthy individuals, in particular) are necessary.
Food
The food industry has a large GHG footprint. Climate and environmental advocates have tried to promote plant-based diets as good for the environment. Many health scholars also seek to promote greater consumption of vegetables and fruits, and significantly less animal protein consumption because of the links of the latter with long-term health problems. In theory, shifting one’s diet to include less meat should produce health benefits and, in the aggregate, a change in societal/cultural practices that would lead to reduction in GHG emissions—provided people do not substitute animal protein with “innovative foods” that have a high impact on the environment due to the land use and water use. Changes in food consumption will require some changes to cultural practices that are held dear, and of which people are protective.
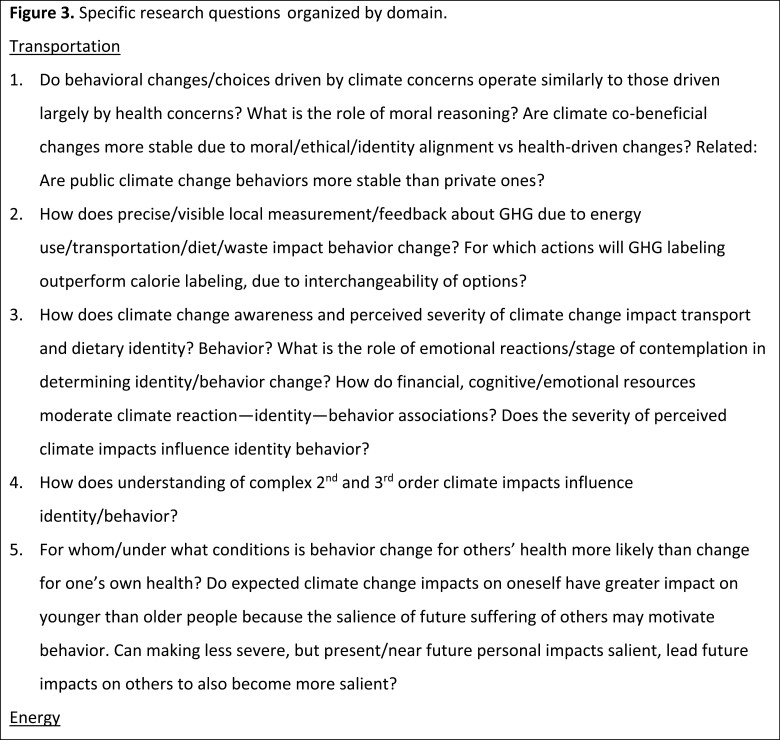
Much of the food industry’s GHG footprint is due to production methods. Climate scientists have modeled some of the benefits of reducing that GHG footprint, under the assumption that if the population changed its demand for foods, companies would respond by changing their supply and their production methods. But, is this realistic given the reality of how the food industry operates? An interdisciplinary team of behavioral health scientists, economists, and climate scientists could build a model that would show the magnitude of population dietary shift needed to yield the supply-side production shifts that are necessary. Specifically, they could identify what messaging/reframing/interventions would shift people to eat more plant-based diets, model the corresponding change in “demand” signal and what the food industry is likely to do in response. For example, if they are likely to devote money and resources to energy, land and water-use intensive food substitutes, is that really an environmental benefit (or a health one)? (Fig. 3).
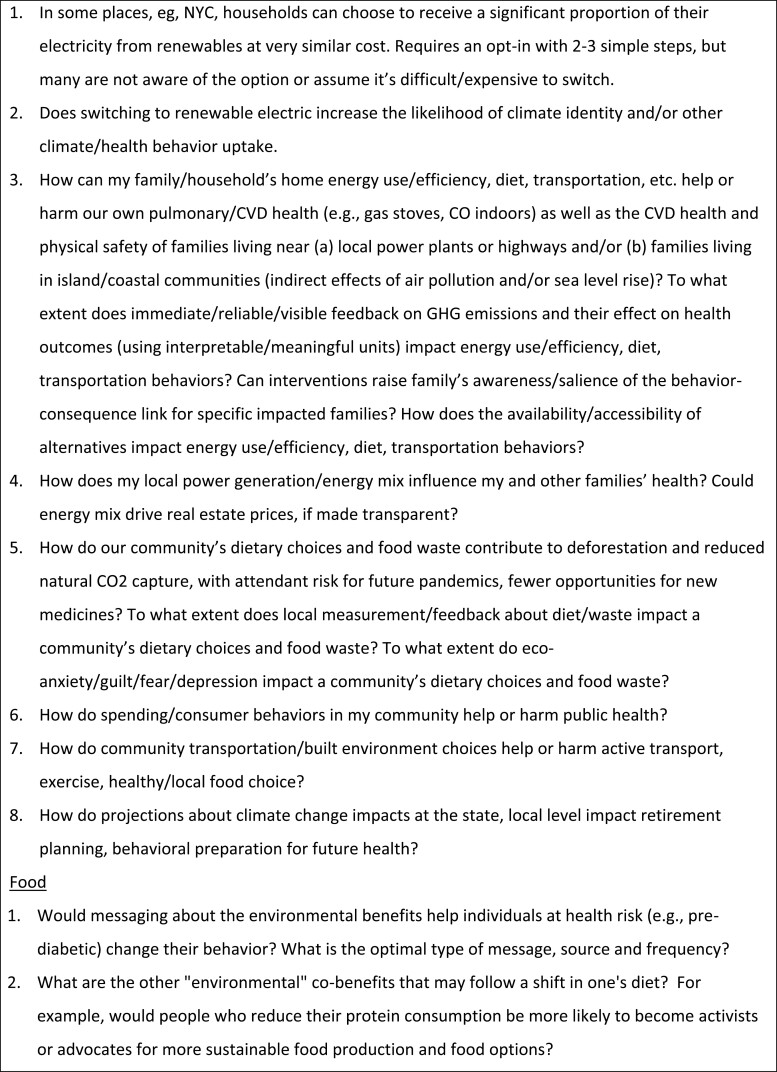
Fig 3.
Specific research questions and hypotheses organized by domain.
Challenges and Opportunities in Climate Change Research for Behavioral Medicine Researchers
Answering these questions and addressing the health impacts of the climate crisis requires scientific adaptations in the field of behavioral medicine. Specifically, we will need to broaden the lens through which we view, understand, and solve problems to encompass the scope of this challenge. These adaptations will require us to expand the data and methods, theory, and interventions that are currently familiar to our field.
Data and Methods
Behavioral medicine research has increasingly availed itself of innovative methods to capture intensive longitudinal data, from wearable devices to self-reports via ecological momentary assessments. Addressing climate will accelerate these trends as we home in on how extreme weather and health behaviors are coupled. But the nature of weather phenomena presents interesting challenges and will benefit from close collaboration between behavioral and environmental scientists.
Weather data are multidimensional. Extreme weather events are often described in terms of a single characteristic (e.g., heatwave, drought) but, in reality, many are compound events with multiple interconnected, interacting, or cascading components [26, 72]. The natural environment can be characterized in terms of many physical and perceptual characteristics [73, 74]. Weather stations often have many sensors to capture a variety of these dimensions. Those stations are typically in fixed locations, but people are mobile. Networks of spatially-distributed weather stations can be paired with location data from smartphones or other wearable devices to identify weather conditions that create the context for a person’s health behavior. Privacy concerns arise when tracking location data; however, these concerns can be managed ethically [75]. Extreme precision is not needed, so geofences can be created to limit the frequency of location tracking. Data aggregation can also be managed to keep location data segregated from other personal information, using it only to look up environmental conditions and only aggregating the environmental conditions with other participant data.
Some environmental influences may be more perceptual than physical. The heat index is one such example [74]. The same temperature can be perceived as more or less amenable to behaviors like physical activity. Some of those perceptual characteristics can be calculated from physical indices; others may require self-reports from human actors themselves. In some cases, fusing physical and perceptual data may be important for understanding how the natural environment impacts behavior.
Weather is also dynamic. It can vary dramatically within a single day as well as across seasons. Momentary weather data will be needed to determine which features are most relevant for predicting health behaviors. Sampling rates for physical and perceptual features of the environment will vary. In the United States, most weather stations record hourly observations and intermediate points can be interpolated. Self-reports of weather conditions can be done as often as desired, with the caveat that every self-report increases response burden and may induce measurement fatigue. Decisions about data aggregation will need to be made carefully to preserve the rich information about weather dynamics.
The dynamic nature of weather and behavior raises analytic challenges. Intensive longitudinal data have dependencies that violate assumptions of common statistical tests [76]. Multilevel modeling and dynamic systems modeling have become more common in behavioral medicine. Further innovation will be required if the field is to leverage the full potential of these data. For example, some weather indices may have very proximal or even immediate effects on behavior; others may have delayed or lagged effects. Some may have cumulative effects on behavior. Intensive longitudinal data raise new questions about the specific features and timing of data that should be used to characterize weather phenomena. Answering these questions will also accelerate theory development.
Theory to Frame, Name, and Explain
Human behavior has contributed to the climate crisis and increased the frequency and power of extreme weather events. These extreme weather events are also influencing a range of human behaviors, including health behaviors. Behavioral medicine theories can be applied and expanded to improve solutions for mitigation and adaptation in the climate crisis. Social–ecological models have become quite pervasive as the field has recognized that behavior unfolds in context. These models specify that the environment influences behavior. Such environmental influences on health behavior have often been defined in terms of the built or social environments. The natural environment has received less attention. The natural environment is generally less modifiable than either the built or social environment. Yet features of the natural environment (i.e., weather indices or features of their distributions over time) can either create or constrain opportunities for different health behaviors. Three broad questions arise that require theoretical attention.
Mitigation
First, what factors explain people’s attraction to behaviors that contribute to the greenhouse gas emissions that are changing our climate? Agriculture and transportation are two of the economic sectors that contribute most to the greenhouse gas emissions [77]. Behavioral medicine has a rich history of investigating diet and physical activity behaviors.
Project Drawdown, a nonprofit organization devoted to halting the increase in harmful greenhouse gas emissions, has proposed solutions that call for experts in behavioral medicine [78]. On the agriculture front, they have identified reducing food waste and promoting and promoting plant-rich diets as important solutions.
Some food waste occurs in production and transportation but others waste occurs in meal preparation and consumption. Experts in behavioral medicine and nutritional sciences can contribute to this solution by developing, testing, and applying insights from theories that explain why consumers accept food waste. Others have begun to apply theories we know well, such as the theory of planned behavior [79]. This work has yet to avail itself of the most significant advances in behavioral science. The roles of beliefs (e.g., knowledge, values, identity), emotions (e.g., rewards, regrets), social influences (e.g., comparisons, support), and automatic processes (e.g., habits, automatic affective evaluations) will need to be explained to create solutions [80, 81].
Promoting plant-rich diets provides a second opportunity for developing theory that can inform solutions. Cattle are a major source of global greenhouse gas emissions [77]. Meat is a staple in Western diets and production has increased dramatically over the past half century despite the environmental threat it presents [82]. The EAT-Lancet Commission has recommended dramatically decreasing red meat consumption to create a more sustainable food system and reduce greenhouse gas emissions [83]. Meat-based dietary patterns appear to be more stable than plant-based dietary patterns [84]. Behavioral medicine has contributed to understanding of energy intake broadly. This expertise can be leveraged to identify targets for shifting people toward more plant-rich diets. One of the immediate opportunities for advancing this work involves elaborating on the motivational targets that underpin specific consumption patterns, including both full vegetarianism and reduced meat consumption patterns [85].
Similar questions exist in the transportation sector. Physical activity is a long-standing area of emphasis in behavioral medicine. This work has typically emphasized volume or intensity over the domain of activity. Recent findings suggest that activity from different domains may have different health consequences but this work has focused on occupational rather than transportation-related physical activity [86]. Active transportation would be a valuable target for physical activity promotion, but little is known about the unique drivers of active transportation beyond urban design [87]. Theory that integrates the person within their environment, to identify shared and unique drivers of active transportation relative to other domains of physical activity, would be valuable.
Adaptation
Second, what factors make it difficult to adopt more environmentally sensitive behaviors? Extreme weather is increasing in frequency and creating new challenges for health. As one example, extreme heat has become more common and is a leading cause of weather-related mortality [26, 72]. Heat stress increases physical and mental health problems as well as mortality. Behaviors can be modified to reduce health threats (e.g., clothing selection, fan use, self-dousing, increasing fluid intake), but these behaviors are often not even viewed as health behaviors unless they are linked with well-defined clinical conditions (e.g., fluid intake for patients with kidney stones). More critically, little is known about the factors influencing uptake and use of these health behaviors. Adapting and refining existing behavioral theories for these unique behaviors would identify key targets for behavioral interventions (illustrated in the conceptual matrix of Fig. 2).
Intervention
Behavioral medicine is a solutions-focused field and there is a great need for solutions to support mitigation and adaptation during the climate crisis. Systems change will be required to avert an environmental catastrophe, but individual level efforts should not be overlooked. Some health behaviors have climate co-benefits and provide a person-level targets for supporting mitigation. Other behaviors will need to be modified to adapt to the health threats arising from increasing extreme environmental conditions. Building on the examples described above, experts in behavioral medicine are called to develop interventions to reduce food waste, promote plant-based diets, increase active transportation, and support informed thermoregulation strategies. These examples are not exhaustive and cross-talk with environmental scientists and clinicians will undoubtedly reveal additional targets for behavioral interventions.
Existing trends in behavioral intervention development position the field well to meet the need for climate-informed solutions. The Obesity-Related Behavioral Intervention Trials (ORBIT) framework [88, 89] and the Multiphase Optimization Strategy (MOST); [90] have both drawn attention to the importance of early-phase intervention development activities. These activities involve preparation of a conceptual model, identifying candidate intervention components to engage each target, determining the mode of delivery and dose for each component, adapting content to target specific populations, evaluating safety and acceptability, evaluating proof-of-concept for modifying a behavioral target. Using MOST, candidate intervention components would also be screened to determine which should be included in an optimized treatment package. The treatment package could then be evaluated for efficacy and effectiveness in modifying the behavioral outcome and reducing health risks. Climate informed intervention development should take care not to skip the critical early-phase activities.
A second advance in behavioral intervention development that has appeal for climate-informed solutions involves progress on just-in-time adaptive interventions (JITAIs) [91, 92]. The premise of JITAIs is that intervention delivery can be more effective and less burdensome if it is timed to coincide with moments of availability, receptivity, opportunity, and vulnerability (or some combination thereof). Thus, the microintervention doses in a JITAI are tailored to contextual conditions. Those conditions can be defined quite broadly. Weather conditions are not acutely modifiable but can be used to tailor intervention delivery to moments of particular vulnerability when people are challenged to adapt. For example, during moments of extreme heat, text messages could be triggered to engage targets that would modify behaviors and support efficient thermoregulation. These messages could be as simple as reminders that the forecast calls for hot temperatures, so lighter clothing and more exposed skin would be more comfortable. In ongoing work, we are tailoring messages for physical activity promotion based on current temperatures; this approach could be extended to promote active transportation [93]. Likewise, just-in-time fluid intake interventions developed to support patients with kidney stones could be adapted to support hydration in regions with extreme temperatures [94].
In addition to these scientific adaptations, behavioral medicine researchers and practitioners will need to prioritize solutions-focused work with populations most impacted as a means of promoting health equity, moving from the universal to the hyperlocal. The timescale for research must also be adjusted: we have never before had to consider how rapid, all-encompassing changes to the environment in which our variables of interest or interventions operate will influence the validity of conclusions drawn from research in today’s climate conditions. Modern climate modeling can now “tell the future” with greater precision than ever before, because physics are increasingly determining future conditions. We must leverage these insights, or we will lose all credibility/utility.
We will also need to work in transdisciplinary/cross-disciplinary groups across environmental/climate science, behavioral medicine, clinical medicine/public health, sociologists, anthropologists, computer scientists, and others. The scientists we will need to collaborate with are not those we typically are familiar with—we need also to identify funding sources for the large, cross-disciplinary efforts needed.
Envisioning the Future: A Call for Crisis-Responsive Behavioral Medicine
Behavioral medicine has slowly broadened its focus from the individual, to the family, community, healthcare system, and cultural context. More recently, we have begun to appreciate how environmental exposures shape health and behavior, but most of the “environment” we have considered has been the built and social environments. It is now clear that behavioral medicine experts have neglected the impacts of the rapid, unprecedented, and deadly changes that our reliance on fossil fuels has ignited in the natural environment [95]. However, the radical perspective shift required to appreciate the trembling shake in every foundational assumption on which our science is built, is of a magnitude akin to any previous paradigm shift [24].
Priorities for a behavioral medicine research agenda include (1) promoting behavior changes to facilitate planetary health, (2) identifying and developing behavioral interventions at multiple levels—from the individual to systems-level—to facilitate climate-resilient health behaviors, and (3) preparing ourselves and our patients for future shocks to physical, social, and health systems that will feel uncanny and alien. One way to begin preparing for the climate impacts that are now unavoidable is to integrate climate and health prediction models (e.g., [96]). The scope and nature of health behaviors we consider needs to be broadened to encompass the range of behaviors relevant in the Anthropocene.
Ultimately, the goals of our work as behavioral medicine researchers and practitioners in response to the crises resulting from climate change require us to redefine individual health and health behaviors as part of One Health/ Planetary health, with a priority on identifying how to motivate individuals to see themselves as part of humankind and to take collective action. A major challenge—and a potential transformative opportunity as well—is the ability to realize our connectedness as human beings and with the planet: that how each of us behaves has implications for others of us. Encouraging empathic, collective thinking and action is essential to securing livable conditions for ourselves and others, though the ability to foster this kind of perspective has eluded us, especially during this hyper-polarized time. But instilling a sense of connection, empathy and a vision for humankind as interdependent must be a priority if we are to foster the kinds of behaviors—individually and collectively—that will promote environmental health.
If we approach our mission in this way and become fluent in forecasting and targeted resilience interventions, in collaboration with scientists from relevant fields, we have the potential to become a uniquely important field in terms of our societal impact. We believe everyone will eventually adopt a One Health/Planetary Health perspective but, if we are early adopters, we will draw the most talented young people to our field. This shift can give rise to a different way of promoting optimal health behaviors: rather than framing health behavior change as important only for individual health and well-being, we can emphasize the importance of health behaviors for preparing us to confront the greatest challenge humanity has ever faced. Behavioral medicine has long aspired to greater impacts; the climate crisis is our call to adapt our approach and deliver tangible benefit to the societies that have given us the training and opportunity to be useful.
Acknowledgments
The authors wish to thank Luis Blanco, Guillaume Chevance, and Lorraine Whitmarsh for their contributions to this manuscript. Dr. Edmondson’s work on this manuscript was supported by U24 AG052175.
Compliance with Ethical Standards
Conflict of Interest: None declared.
Primary Data: Findings reported have not been previously published and this manuscript is not being simultaneously submitted elsewhere. Data have not been previously reported elsewhere. The authors have full control of all primary data and agree to allow the Journal to review data if requested.
Ethical Approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Transparency Statement: This commentary does not include or reflect any original data collection, analysis, code, or materials, nor does it include tests of hypotheses that would require pre-registration.
REFERENCES
- 1. McNutt M. Climate change impacts. Science. 2013; 341( 6145): 435. [DOI] [PubMed] [Google Scholar]
- 2. Abram NJ, McGregor HV, Tierney JE, Evans MN, McKay NP, Kaufman DS; PAGES 2k Consortium. Early onset of industrial-era warming across the oceans and continents. Nature. 2016; 536( 7617): 411– 418. [DOI] [PubMed] [Google Scholar]
- 3. Mahony CR, MacKenzie WH, Aitken SN.. Novel climates: trajectories of climate change beyond the boundaries of British Columbia’s forest management knowledge system. For Ecol Manag. 2018; 410: 35– 47. [Google Scholar]
- 4. Mora C, Frazier AG, Longman RJ, et al. The projected timing of climate departure from recent variability. Nature. 2013; 502( 7470): 183– 187. [DOI] [PubMed] [Google Scholar]
- 5. Urban MC. Climate change. Accelerating extinction risk from climate change. Science. 2015; 348( 6234): 571– 573. [DOI] [PubMed] [Google Scholar]
- 6. Arguez A, et al. Should we expect each year in the next decade (2019–28) to be ranked among the top 10 warmest years globally? Bull Am Meteorol Soc. 2020; 101( 5): E655– E663. [Google Scholar]
- 7. Burke KD, Williams JW, Chandler MA, Haywood AM, Lunt DJ, Otto-Bliesner BL.. Pliocene and Eocene provide best analogs for near-future climates. Proc Natl Acad Sci U S A. 2018; 115( 52): 13288– 13293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Steffen W, Rockström J, Richardson K, et al. Trajectories of the Earth system in the anthropocene. Proc Natl Acad Sci U S A. 2018; 115( 33): 8252– 8259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Zhongming Z, Linong L, Xiaona Y, et al. AR6 Climate Change 2021: The Physical Science Basis. 2021. [Google Scholar]
- 10. Lenton TM. Environmental tipping points. Ann Rev Environ Resour. 2013; 38( 1): 1– 29. [Google Scholar]
- 11. Wang L, Wang H, Dong Z, Wang S, Cao Z.. The air pollution effect of government economic growth expectations: evidence from China’s cities based on green technology. Environ Sci Pollut Res Int. 2021; 28( 22): 27639– 27654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Blanford GJ, Richels RG, Rutherford TF.. Feasible climate targets: the roles of economic growth, coalition development and expectations. Energy Econ. 2009; 31: S82– S93. [Google Scholar]
- 13. Malm A. Fossil Capital: The Rise of Steam Power and The Roots of Global Warming. Brooklyn, NY: Verso Books; 2016. [Google Scholar]
- 14. Peters GP, Marland G, Le Quéré C, et al. Rapid growth in CO2 emissions after the 2008–2009 global financial crisis. Nat Clim Change. 2012; 2( 1): 2– 4. [Google Scholar]
- 15. Field CB, Lobell DB, Peters HA, et al. Feedbacks of terrestrial ecosystems to climate change. Annu Rev Environ Resour. 2007; 32: 1– 29. [Google Scholar]
- 16. Loehman RA. Drivers of wildfire carbon emissions. Nat Clim Change. 2020; 10( 12): 1070– 1071. [Google Scholar]
- 17. Brienen RJ, Phillips OL, Feldpausch TR, et al. Long-term decline of the Amazon carbon sink. Nature. 2015; 519( 7543): 344– 348. [DOI] [PubMed] [Google Scholar]
- 18. Yang Y, Saatchi SS, Xu L, et al. Post-drought decline of the Amazon carbon sink. Nat Commun. 2018; 9( 1): 1– 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gatti LV, Basso LS, Miller JB, et al. Amazonia as a carbon source linked to deforestation and climate change. Nature. 2021; 595( 7867): 388– 393. [DOI] [PubMed] [Google Scholar]
- 20. Heinze C, Meyer S, Goris N, et al. The ocean carbon sink–impacts, vulnerabilities and challenges. Earth Syst Dyn. 2015; 6( 1): 327– 358. [Google Scholar]
- 21. Armstrong McKay DI, Cornell SE, Richardson K, et al. Resolving ecological feedbacks on the ocean carbon sink in Earth system models. Earth Syst Dyn. 2021; 12( 3): 797– 818. [Google Scholar]
- 22. Steinberg DK, Landry MR.. Zooplankton and the ocean carbon cycle. Ann Rev Mar Sci. 2017; 9: 413– 444. [DOI] [PubMed] [Google Scholar]
- 23. Lemery J, Knowlton K, Sorensen C.. Global Climate Change and Human Health: From Science to Practice. Hoboken, NJ: John Wiley & Sons; 2021. [Google Scholar]
- 24. Mora C, Spirandelli D, Franklin EC, et al. Broad threat to humanity from cumulative climate hazards intensified by greenhouse gas emissions. Nat Clim Change. 2018; 8( 12): 1062– 1071. [Google Scholar]
- 25. Kaczan DJ, Orgill-Meyer J.. The impact of climate change on migration: a synthesis of recent empirical insights. Clim Change. 2020; 158( 3): 281– 300. [Google Scholar]
- 26. Ebi KL, Vanos J, Baldwin JW, et al. Extreme weather and climate change: population health and health system implications. Annu Rev Public Health. 2021; 42: 293– 315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. GC WMO, C. Climate 2001–2010: A Decade of Climate Extremes—Summary Report. WMO no. 1119. Geneva, Switzerland: World Meteorological Organization; 2013. [Google Scholar]
- 28. Ebi KL, Capon A, Berry P, et al. Hot weather and heat extremes: health risks. Lancet. 2021; 398( 10301): 698– 708. [DOI] [PubMed] [Google Scholar]
- 29. Bellprat O, Guemas V, Doblas-Reyes F, Donat MG.. Towards reliable extreme weather and climate event attribution. Nat Commun. 2019; 10( 1): 1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Adger WN. Vulnerability. Glob Environ Change. 2006; 16( 3): 268– 281. [Google Scholar]
- 31. Knight KW, Schor JB, Jorgenson AK.. Wealth inequality and carbon emissions in high-income countries. Soc Curr. 2017; 4( 5): 403– 412. [Google Scholar]
- 32. McDermott-Levy R, Scolio M, Shakya KM, et al. Factors that influence climate change-related mortality in the United States: an integrative review. Int J Environ Res Public Health. 2021; 18( 15): 8220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Jorgenson A, Schor J, Huang X.. Income inequality and carbon emissions in the United States: a state-level analysis, 1997–2012. Ecol Econ. 2017; 134: 40– 48. [Google Scholar]
- 34. Howell J, Elliott JR.. Damages done: the longitudinal impacts of natural hazards on wealth inequality in the United States. Soc Probl. 2019; 66( 3): 448– 467. [Google Scholar]
- 35. Wilson B, Chakraborty A.. Mapping vulnerability to extreme heat events: lessons from metropolitan Chicago. J Environ Plan Manag. 2019; 62( 6): 1065– 1088. [Google Scholar]
- 36. White-Newsome JL, Sánchez BN, Jolliet O, et al. Climate change and health: indoor heat exposure in vulnerable populations. Environ Res. 2012; 112: 20– 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Hsu AI, Yttri EA.. B-SOiD, an open-source unsupervised algorithm for identification and fast prediction of behaviors. Nat Commun. 2021; 12( 1): 5188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Chevance G, Fresán U, Hekler EB, et al. Thinking health-related behaviors in a climate change context: a narrative review. Transl Behav Med. 2022. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Quam VG, Rocklöv J, Quam M, et al. Assessing greenhouse gas emissions and health co-benefits: a structured review of lifestyle-related climate change mitigation strategies. Int J Environ Res Public Health. 2017; 14( 5): 468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Bernard P. Health psychology at the age of Anthropocene. Health Psychol Behav Med. 2019; 7( 1): 193– 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Carlsson-Kanyama A, González AD.. Potential contributions of food consumption patterns to climate change. Am J Clin Nutr. 2009; 89( 5): 1704S– 1709S. [DOI] [PubMed] [Google Scholar]
- 42. McMichael AJ, Powles JW, Butler CD, Uauy R.. Food, livestock production, energy, climate change, and health. Lancet. 2007; 370( 9594): 1253– 1263. [DOI] [PubMed] [Google Scholar]
- 43. Macdiarmid JI, Whybrow S.. Nutrition from a climate change perspective. Proc Nutr Soc. 2019; 78( 3): 380– 387. [DOI] [PubMed] [Google Scholar]
- 44. Maibach E, Steg L, Anable J.. Promoting physical activity and reducing climate change: opportunities to replace short car trips with active transportation. Prev Med. 2009; 49( 4): 326– 327. [DOI] [PubMed] [Google Scholar]
- 45. Woodcock J, Banister D, Edwards P, Prentice AM, Roberts I.. Energy and transport. Lancet. 2007; 370( 9592): 1078– 1088. [DOI] [PubMed] [Google Scholar]
- 46. Gardner GT, Stern PC.. The short list: the most effective actions US households can take to curb climate change. Environment. 2008; 50( 5): 12– 25. [Google Scholar]
- 47. Robinson TN. Save the world, prevent obesity: piggybacking on existing social and ideological movements. Obesity. 2010; 18 Suppl 1: S17– S22. [DOI] [PubMed] [Google Scholar]
- 48. Whitley CT, Gunderson R, Charters M.. Public receptiveness to policies promoting plant-based diets: framing effects and social psychological and structural influences. J Environ Policy Plan. 2018; 20( 1): 45– 63. [Google Scholar]
- 49. Paavola J. Health impacts of climate change and health and social inequalities in the UK. Environ Health. 2017; 16( Suppl 1): 113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Raymond C, Matthews T, Horton RM.. The emergence of heat and humidity too severe for human tolerance. Sci Adv. 2020; 6( 19): eaaw1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Sherwood SC, Huber M.. An adaptability limit to climate change due to heat stress. Proc Natl Acad Sci U S A. 2010; 107( 21): 9552– 9555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Sheridan SC, Allen MJ.. Temporal trends in human vulnerability to excessive heat. Environ Res Lett. 2018; 13( 4): 043001. [Google Scholar]
- 53. Swinburn BA, Kraak VI, Allender S, et al. The Global Syndemic of Obesity, undernutrition, and climate change: the Lancet Commission report. Lancet. 2019; 393( 10173): 791– 846. [DOI] [PubMed] [Google Scholar]
- 54. Turrisi TB, Bittel KM, West AB, et al. Seasons, weather, and device-measured movement behaviors: a scoping review from 2006 to 2020. Int J Behav Nutr Phys Act. 2021; 18( 1): 1– 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Fanzo J, Davis C, McLaren R, et al. The effect of climate change across food systems: implications for nutrition outcomes. Glob Food Sec. 2018; 18: 12– 19. [Google Scholar]
- 56. Leisner CP. Review: climate change impacts on food security-focus on perennial cropping systems and nutritional value. Plant Sci. 2020; 293: 110412. [DOI] [PubMed] [Google Scholar]
- 57. Schnitter R, Berry P.. The climate change, food security and human health Nexus in Canada: a framework to protect population health. Int J Environ Res Public Health. 2019; 16( 14): 2531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Minor K, Bjerre Nielsen A, Jonasdottir S, et al. Ambient warming and human sleep duration and timing: a worldwide case-crossover study using big data from wearable devices. In ISEE Conference Abstracts; 2021.
- 59. Romanello M, McGushin A, Di Napoli C, et al. The 2021 report of the Lancet Countdown on health and climate change: code red for a healthy future. Lancet. 2021; 398( 10311): 1619– 1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Horton R, Beaglehole R, Bonita R, Raeburn J, McKee M, Wall S.. From public to planetary health: a manifesto. Lancet. 2014; 383( 9920): 847. [DOI] [PubMed] [Google Scholar]
- 61. Herzog L, Kellmeyer P, Wild V.. Digital behavioral technology, vulnerability and justice: towards an integrated approach. Rev Soc Econ. 2021;80: 1– 22. [Google Scholar]
- 62. Rabinowitz PM, Pappaioanou M, Bardosh KL, Conti L.. A planetary vision for one health. BMJ Glob Health. 2018; 3( 5): e001137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Whitmee S, Haines A, Beyrer C, et al. Safeguarding human health in the Anthropocene epoch: report of The Rockefeller Foundation-Lancet Commission on planetary health. Lancet. 2015; 386( 10007): 1973– 2028. [DOI] [PubMed] [Google Scholar]
- 64. Obradovich N, Fowler JH.. Climate change may alter human physical activity patterns. Nat Hum Behav. 2017; 1( 5): 1– 7. [Google Scholar]
- 65. Kotcher J, Maibach E, Miller J, et al. Views of health professionals on climate change and health: a multinational survey study. Lancet Planet Health. 2021; 5( 5): e316– e323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Watts N, Amann M, Arnell N, et al. The 2020 report of The Lancet Countdown on health and climate change: responding to converging crises. Lancet. 2021; 397( 10269): 129– 170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Hayes K, Poland B.. Addressing mental health in a changing climate: incorporating mental health indicators into climate change and health vulnerability and adaptation assessments. Int J Environ Res Public Health. 2018; 15( 9): 1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Schill C, Anderies JM, Lindahl T, et al. A more dynamic understanding of human behaviour for the Anthropocene. Nat Sustain. 2019; 2( 12): 1075– 1082. [Google Scholar]
- 69. Facts E. US Transportation Sector Greenhouse Gas Emissions, 1990–2019. Washington DC, USA: Office of Transportation and Air Quality; 2021. [Google Scholar]
- 70. Keall MD, Shaw C, Chapman R, et al. Reductions in carbon dioxide emissions from an intervention to promote cycling and walking: a case study from New Zealand. Transp Res D Transp Environ. 2018; 65: 687– 696. [Google Scholar]
- 71. Goldstein B, Gounaridis D, Newell JP.. The carbon footprint of household energy use in the United States. Proc Natl Acad Sci U S A. 2020; 117( 32): 19122– 19130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Seneviratne S, Nicholls N, Easterling D, et al. Changes in climate extremes and their impacts on the natural physical environment. In: Field CB, Barros V, Stocker TF, Qin D, Dokken DJ, Ebi KL, Mastrandrea MD, Mach KJ, Plattner G-K, Allen SK, Tignor M, Midgley PM, eds, IPCC. 582 pp. Cambridge, UK: Cambridge University Press. 2012. [Google Scholar]
- 73. Heim RR. An overview of weather and climate extremes—products and trends. Weather Clim Extremes. 2015; 10: 1– 9. [Google Scholar]
- 74. Steadman RG. The assessment of sultriness. Part I: A temperature-humidity index based on human physiology and clothing science. J Appl Meteorol Climatol. 1979; 18( 7): 861– 873. [Google Scholar]
- 75. Wang JL, Loui MC.. Privacy and ethical issues in location-based tracking systems. In 2009 IEEE International Symposium on Technology and Society. 2009.
- 76. Snijders TA, Bosker RJ.. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. Hoboken, NJ: Sage; 2011. [Google Scholar]
- 77. EPA. Inventory of U.S. Greenhouse Gas Emissions and Sinks: 1990-2019. In: Environmental Protection Agency, US Government printing office, ed. Washington, D.C; 2021. [Google Scholar]
- 78. Hawken P. Drawdown: The Most Comprehensive Plan Ever Proposed to Reverse Global Warming. NY, NY: Penguin; 2017. [Google Scholar]
- 79. van der Werf P, Seabrook JA, Gilliland JA.. Food for naught: using the theory of planned behaviour to better understand household food wasting behaviour. Can Geogr. 2019; 63( 3): 478– 493. [Google Scholar]
- 80. Neff RA, Spiker ML, Truant PL.. Wasted food: U.S. consumers’ reported awareness, attitudes, and behaviors. PLoS One. 2015; 10( 6): e0127881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Qi D, Roe BE.. Household food waste: multivariate regression and principal components analyses of awareness and attitudes among U.S. consumers. PLoS One. 2016; 11( 7): e0159250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Ritchie H, Roser M.. Meat and Dairy Production . 2019. Available at OurWorldInData.org. Last accessed November, 2021.
- 83. Willett W, Rockström J, Loken B, et al. Food in the Anthropocene: the EAT-Lancet Commission on healthy diets from sustainable food systems. Lancet. 2019; 393( 10170): 447– 492. [DOI] [PubMed] [Google Scholar]
- 84. Milfont TL, Satherley N, Osborne D, Wilson MS, Sibley CG.. To meat, or not to meat: a longitudinal investigation of transitioning to and from plant-based diets. Appetite. 2021; 166: 105584. [DOI] [PubMed] [Google Scholar]
- 85. Rosenfeld DL, Burrow AL.. Vegetarian on purpose: understanding the motivations of plant-based dieters. Appetite. 2017; 116: 456– 463. [DOI] [PubMed] [Google Scholar]
- 86. White RL, Babic MJ, Parker PD, Lubans DR, Astell-Burt T, Lonsdale C.. Domain-specific physical activity and mental health: a meta-analysis. Am J Prev Med. 2017; 52( 5): 653– 666. [DOI] [PubMed] [Google Scholar]
- 87. Sallis JF, Bull F, Burdett R, et al. Use of science to guide city planning policy and practice: how to achieve healthy and sustainable future cities. Lancet. 2016; 388( 10062): 2936– 2947. [DOI] [PubMed] [Google Scholar]
- 88. Czajkowski SM, Powell LH, Adler N, et al. From ideas to efficacy: the ORBIT model for developing behavioral treatments for chronic diseases. Health Psychol. 2015; 34( 10): 971– 982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Czajkowski SM, Hunter CM.. From ideas to interventions: a review and comparison of frameworks used in early phase behavioral translation research. Health Psychol. 2021; 40( 12): 829– 844. [DOI] [PubMed] [Google Scholar]
- 90. Collins LM, Murphy SA, Strecher V.. The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions. Am J Prev Med. 2007; 32( 5 Suppl): S112– S118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Nahum-Shani I, Smith SN, Spring BJ, et al. Just-in-time adaptive interventions (JITAIs) in mobile health: key components and design principles for ongoing health behavior support. Ann Behav Med. 2018; 52( 6): 446– 462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Nahum-Shani I, Hekler EB, Spruijt-Metz D.. Building health behavior models to guide the development of just-in-time adaptive interventions: a pragmatic framework. Health Psychol. 2015; 34S: 1209– 1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Hojjatinia S, Hojjatinia S, Lagoa CM, Brunke-Reese D, Conroy DE.. Person-specific dose-finding for a digital messaging intervention to promote physical activity. Health Psychol. 2021; 40( 8): 502– 512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Conroy DE, West AB, Brunke-Reese D, Thomaz E, Streeper NM.. Just-in-time adaptive intervention to promote fluid consumption in patients with kidney stones. Health Psychol. 2020; 39( 12): 1062– 1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Turner MG, Calder WJ, Cumming GS, et al. Climate change, ecosystems and abrupt change: science priorities. Philos Trans R Soc Lond B Biol Sci. 2020; 375( 1794): 20190105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Chen K, Vicedo-Cabrera AM, Dubrow R.. Projections of ambient temperature-and air pollution-related mortality burden under combined climate change and population aging scenarios: a review. Curr Environ Health Rep. 2020; 7: 1– 13. [DOI] [PubMed] [Google Scholar]