Abstract
Objective
The main purpose of this study is to determine the presence of carotid artery calcification (CAC) detected on digital panoramic radiographs (DPRs) retrospectively and correlate the findings with cardiovascular risk factors including gender, age, smoking status, hypertension, diabetes, and hyperlipidemia, along with atherosclerotic cardiovascular disease and periodontal status.
Methods
This clinical study is registered at ClinicalTrials.gov as NCT04017078. DPRs, periodontal status and cardiovascular risk factors of 1,101 patients (576 males, 525 females) were evaluated. The patients were grouped based on whether CAC was detected in dental DPRs [CAC (+)] or not [CAC (–)]. Periodontal status was categorised as gingivitis, periodontitis, and gingivitis with reduced periodontium (periodontally stable patient).
Results
Out of 1,101 patients, whose mean age was 42.1 ± 15.5 years and 525 (47.7%) were female, 34 (3.1%) were diagnosed with CAC on DPRs. No significant difference was observed between groups considering gender, hypertension, diabetes, hyperlipidemia, smoking, and periodontal status. Patients aged 40–55 years (n = 398, 36.15%) and patients older than 55 years (n = 222, 20.16%) were associated with CAC (odds ratio = 4.49, 95% confidence interval = 1.65–12.17, P = 0.003; odds ratio = 4.41, 95% confidence interval = 1.33–14.61, P = 0.015, respectively).
Conclusion
Among all parameters, only age exhibited significant correlation with an increased risk of carotid calcification. Further studies with prospective designs and larger study populations are needed.
Key words: Carotid calcification, Panoramic radiography, Periodontitis, Periodontal disease, Systemic diseases
Introduction
Atherosclerosis is a highly prevalent chronic inflammatory vascular disease and the major cause of cardiovascular death. The earliest macroscopic signs of atherosclerosis are fatty streaks. Over time, these evolve into atheromatous plaques, and the vessels may become partially or fully occluded. Clinical manifestations vary based on the rate, degree and location of the vascular occlusion.1 Stroke, a major clinical consequence of this calcification, occurs as a result of partial or complete occlusion of the carotid arteries.
Since stroke is anticipated to be one of the primary causes of death by 2030, its early diagnosis is important in order to overcome mortality and morbidity.2,3 For this reason, panoramic radiographs, which are used routinely in dental practice, might be useful tools for the detection of carotid artery calcification (CAC), and their use might achieve early detection in asymptomatic patients.4 CAC can be detected when the bifurcation and proximal internal carotid areas of the carotid artery are observed in panoramic radiographs.5
Periodontal diseases are chronic inflammatory diseases that are triggered by bacteria. The two most common forms of periodontal disease are gingivitis and periodontitis. Periodontitis results in a loss of the alveolar bone support of the teeth, whereas gingivitis is localised to the gingiva.6,7 According to the Global Burden of Disease Study, severe periodontitis is the sixth most encountered disease worldwide with an overall prevalence of 11.2%, and it affects about 743 million people.8 Several epidemiological studies have shown that gingivitis9 and periodontitis10 may be associated with stroke by adversely affecting early atherosclerotic processes, increasing the risk of atheroma plaque development and plaque rupture.7,11
Several studies have pointed out the correlation between CAC detected on digital panoramic radiographs (DPRs) and periodontal status.3,12, 13, 14 Studies performed on specific populations, such as nonsmokers13 or individuals over 60 years of age,14 found that there may be a significant relationship between CAC and periodontal conditions,13,14 whereas no correlation was observed in studies conducted with general populations.3,12 Only one study used the definition of periodontitis together with clinical and radiographic data,14 whereas others used only radiographic bone loss3 or periodontal risk.12,13
As a result of the methodological differences and inconsistency of the findings in previous studies, additional studies are needed to comprehend the possible relationship between periodontitis and CAC. The main goal of this research is to retrospectively establish the presence of CAC detected by DPRs and then to correlate the findings with periodontal status, atherosclerotic cardiovascular disease, and cardiovascular risk factors such as age, gender, smoking status, hypertension, diabetes, and hyperlipidemia. The authors hypothesise that more CAC might be observed on DPRs of individuals with periodontitis, and CAC might correlate with various cardiovascular risk factors such as age, gender, smoking status, hypertension, hyperlipidemia, and diabetes.
Materials and methods
This study was approved by the Baskent University Institutional Review Board (D-KA18/24) and supported by the Baskent University Research Fund. All study procedures were performed in accordance with the Declaration of Helsinki and the Baskent University Research Committee Regulations. This clinical study is registered at ClinicalTrials.gov as NCT04017078.
This cross-sectional study evaluated DPRs, periodontal status, cardiovascular risk factors and atherosclerotic cardiovascular disease of 1,101 patients (576 males, 525 females) who were referred to Baskent University, Faculty of Dentistry, Department of Periodontology, during 2016–2018. Subjects with no medical records and DPRs not showing vertebra C3 and C4 were excluded.
Medical histories
Along with gender and age, data on hypertension, diabetes, hyperlipidemia, atherosclerotic cardiovascular disease (coronary heart disease, carotid artery stenosis, peripheral artery disease, and abdominal aortic aneurysm), and smoking status were recorded. All data were obtained from the hospital records of the patients. Subjects were classified into three age subgroups (<40 years, 40–55 years, >55 years). Patients were also grouped according to their smoking status, as never smoked, current smokers, and former smokers.
Periodontal clinical examination
Each participant was examined for periodontal status. On periodontal examination, plaque index (PI),15 gingival index (GI),15 bleeding on probing (BOP), probing pocket depth (PPD = distance between gingival margin and bottom of the periodontal pocket), and clinical attachment level (CAL = distance between the cemeno-enamel junction and the bottom of the periodontal pocket) were evaluated. All periodontal measurements were recorded at six sites around each tooth using a periodontal probe (‘O’ probe with the Williams probe, the University of Michigan), excluding the third molar, by two experienced periodontists (MBC, YS). Interobserver agreement of the trained periodontists blinded for CAC was at a substantial level (κ = 0.80). The periodontal status was categorised as gingivitis, reduced periodontium with gingivitis or periodontitis. When probing depths were 3 mm or less, BOP values were ≥10% of sites and no clinical attachment loss and/or recession occurred, the diagnosis has been made as gingivitis. If gingival inflammation was accompanied with clinical attachment loss and/or recession, probing depths were ≤3 mm and BOP values were ≥10% of sites, diagnosis was reduced periodontium with gingivitis (stable periodontitis patient with history of treated periodontitis).16 Finally, the patients who had interdental CAL at ≥2 non-adjacent teeth, or buccal or oral CAL ≥3 mm with probing depths >3 mm at ≥2 teeth were diagnosed with periodontitis.17
Radiographic evaluation
All digital panoramic images were obtained with the same device (Veraviewpocs 2D; Morita, Kyoto, Japan), with the following exposure parameters: 64–66 kVp, 6–9 mA, and 10 s. An observer with seven years’ experience in the Dentomaxillofacial Radiology Department of our university analysed each of the images twice with 30 days between analyses, using ClearCanvas (Synaptive Medical, Toronto, ON, Canada) software on an LED monitor under low light (HP Prodisplay P221 21.5” LED Backlit LED monitor; HP Inc., Toronto, Canada). Intraobserver agreement was calculated (κ = 0.89). The CAC findings were characterised as one or more radiopaque masses close to the cervical vertebrae at or below the level of the intervertebral space between C3 and C4 on the DPR18 (Fig. 1, Fig. 2). The CACs were defined as present (+) or absent (–) by the dentomaxillofacial radiologist. According to the CAC scores, the study population was divided into two groups as CAC (+) and CAC (–).
Fig. 1.
Image of a digital panoramic radiograph (DPR) showing a unilateral radiopacity of suspected carotid calcification on the left side (arrow).
Fig. 2.
Image of a digital panoramic radiograph (DPR) showing a unilateral radiopacity of suspected carotid calcification on the right side (arrow).
Statistical analysis
We used the Kolmogorov-Smirnov Test to assess whether the continuous variables have normal distributions. Levene's Test was performed to understand the homogeneity of variances. Categorical data were represented in terms of number of cases and percentages, whereas descriptive statistics for continuous variables were demonstrated as mean ± SD or median (min-max) percentiles where applicable.
The average changes in groups were evaluated by Student's t-test. For comparisons of not normally distributed data, we performed the Mann-Whitney U test. Categorical data were analysed by Continuity Corrected Chi-square or Fisher's Exact test if needed.
In order to determine the best predictor(s) for the existence of CAC, multiple logistic regression analysis was performed. Any variable with a univariable test having a P-value of <0.25 was taken as a candidate for the multivariable model, together with all variables of known clinical importance. Odds ratios, 95% confidence intervals and Wald statistics for each independent variable were also analysed. Data analysis was executed using SPSS Statistics for Windows, Version 17.0 (SPSS Inc., Chicago, IL, USA). A P-value less than 0.05 was considered statistically significant.
Results
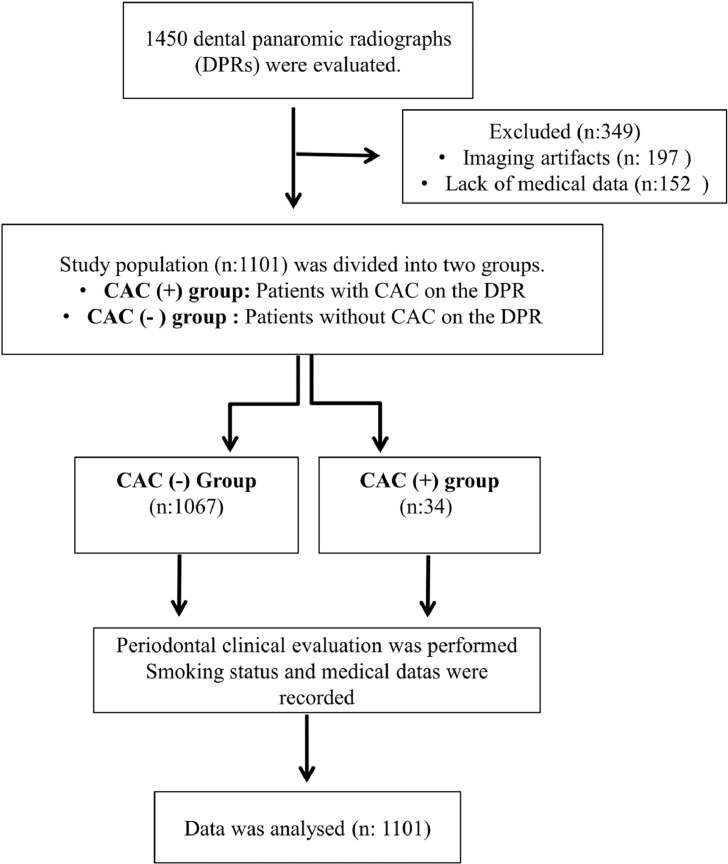
A total of 1,450 DPRs were evaluated. Of those, 197 radiographs having imaging artefacts and 152 patients with missing clinical data were not included in the study (Figure 3). The study analyses were thus performed on 1,101 DPRs. The mean age of the study population was 42.1 ± 15.5 years and 525 (47.7%) of all participants were female. Among those subjects, 34 (3.1%; 13 males, 21 females) had one or more radiopaque masses detected on the digital images. The most commonly recorded chronic disease was hypertension, which was followed by atherosclerotic cardiovascular disease. Of the study population, 43% were current smokers. In terms of periodontal status, 51% of the patients were diagnosed with gingivitis, 39% with periodontitis, and 9% with reduced periodontium with gingivitis.
Fig. 3.
Flow-chart of the study.
Characteristics of the patients with and without CAC are presented in Table 1. The mean ages of the two groups were 48.0 ± 11.0 and 41.9 ± 15.6 years for participants with and without CAC, respectively, and the difference was statistically significant (P = 0.003). In the CAC (+) group, the proportion of patients under 40 years of age was significantly lower, at 17.6% (P = 0.003), but increased for the 40- to 55-year range to become significantly higher, at 58.8% (P = 0.009), than for the CAC (–) group, while the proportions of patients over 55 for both groups were statistically similar (23.6% and 20.1%, P = 0.780). The percentage of female subjects was higher in CAC (+) than CAC (–) at 61.8% and 47.2%, respectively, but the difference was not significant (P = 0.135). No significant differences were detected in the presence of hypertension, hyperlipidemia, diabetes, and atherosclerotic cardiovascular disease (all P values > 0.1), and the profiles of CAC (+) and CAC (–) patients in terms of their smoking history were also comparable (all P values > 0.5). While the incidence of gingivitis was elevated in the CAC (–) group, and by contrast diagnoses for both periodontitis and reduced periodontium with gingivitis were higher in CAC (+) patients, none of these differences were statistically significant (all Ps > 0.1).
Table 1.
Characteristics of the study population
| Variables | CAC (–) (n = 1,067) | CAC (+) (n = 34) | P-value |
|---|---|---|---|
| Cardiovascular risk factors | |||
| Mean age (years) | 41.9 ± 15.6 | 48.0 ± 11.0 | 0.003* |
| Age groups | |||
| <40 years | 475 (44.5%) | 6 (17.6%) | 0.003† |
| 40–55 years | 378 (35.4%) | 20 (58.8%) | 0.009† |
| >55 years | 214 (20.1%) | 8 (23.6%) | 0.780† |
| Gender | |||
| Female | 504 (47.2%) | 21 (61.8%) | 0.135† |
| Male | 563 (52.8%) | 13 (38.2%) | >0.999‡ |
| Hyperlipidemia | 9 (0.8%) | 0 (0.0%) | |
| Hypertension | 116 (10.9%) | 1 (2.9%) | 0.250‡ |
| Diabetes | 51 (4.8%) | 3 (8.8%) | 0.230‡ |
| Smoking status | |||
| Never smoked | 559 (52.4%) | 16 (47.1%) | 0.661† |
| Ex-smoker | 50 (4.7%) | 1 (2.9%) | >0.999‡ |
| Current smoker | 458 (42.9%) | 17 (50.0%) | 0.519† |
| Smoking free time of ex-smokers (years) | 8 (1–30) | 17 (17–17) | – |
| Number of cigarettes smoked per day (cigarettes/day) | 15 (1–60) | 20 (3–40) | 0.273§ |
| Duration of smoking (years) | 15 (1–50) | 15 (1–40) | 0.813§ |
| Atherosclerotic cardiovascular disease | 70 (6.6%) | 1 (2.9%) | 0.720‡ |
| Diagnosis | |||
| Gingivitis | 549 (51.5%) | 14 (41.2%) | 0.315§ |
| Periodontitis | 418 (39.1%) | 15 (44.1%) | 0.687§ |
| Reduced periodontium with gingivitis | 100 (9.4%) | 5 (14.7%) | 0.365‡ |
CAC, carotid artery calcification.
Statistical significant (P < 0.05).
Student's t-test.
Continuity corrected chi-square.
Fisher's exact test.
Mann-Whitney U test.
In order to differentiate between groups with and without CAC, the effects of the factors considered to be the most determinant were examined with multivariate logistic regression analysis, and the results are presented in Table 2. Variables determined as P < 0.25 as the outcome of univariate statistical analysis were included in the regression model as potential risk factors. The variable of diagnosis was also included in the multiple regression model as a candidate risk factor for clinical considerations, although its P-value from the univariate analysis was found to be greater than 0.25.
Table 2.
Multivariate logistic model for association of carotid calcification
| Variables | OR | CI 95% | Wald | P-value |
|---|---|---|---|---|
| Age groups | ||||
| <40 years | 1.000 | – | – | – |
| 40–55 years | 4.491 | 1.657–12.173 | 8.714 | 0.003 |
| >55 years | 4.408 | 1.330–14.615 | 5.885 | 0.015 |
| Gender female | 1.910 | 0.932–3.915 | 3.126 | 0.077 |
| Hypertension | 0.128 | 0.016–1.022 | 3.761 | 0.052 |
| Diabetes | 1.784 | 0.500–6.365 | 0.796 | 0.372 |
| Diagnosis | ||||
| Gingivitis | 1.000 | – | – | – |
| Periodontitis | 0.892 | 0.392–2.026 | 0.075 | 0.784 |
| Reduced periodontium with gingivitis | 1.286 | 0.424–3.903 | 0.197 | 0.657 |
CI, confidence interval; OR, odds ratio.
Statistical significant (P < 0.05).
Multivariate logistic regression analysis revealed that age was an independent risk factor for CAC (Table 2). Considering other potential risk factors, for subjects who were between 40 to 55 years old the risk of CAC increased 4.491 times (95% CI: 1.657–12.173) compared to subjects who were younger than 40 years (P = 0.003). In addition, a 4.408-fold (95% CI: 1.330–14.615) increase was observed in individuals who were older than 55 years (P = 0.015).
Discussion
The goals of the current study were: (i) to investigate the prevalence of CAC on DPRs; (ii) to correlate the findings with periodontal status, atherosclerotic cardiovascular disease, and cardiovascular risk factors. A total of 1,101 DPRs were examined and the prevalence of CAC was 3.1 %. Our findings are in accordance with previous studies, which found the prevalence of CAC in DPRs between 0.4% and 4.0%.19, 20, 21 On the other hand, higher prevalence rates were found in some previous studies,13,18,22, 23, 24 and these higher values attributed to ethnic dietary and geographic differences, along with sample size, sample type, imaging methods (analogue versus digital imaging), and diagnostic errors.12,22,25
The average age of the study population was 42.1 ± 15.5 years, which is lower than that of previous studies.13,14,26 This difference occurred because age-related exclusion criteria were not used in the present study; although the prevalence of CAC in young patients is lower, the process of atherosclerotic lesion formation begins in infancy.27 Thus, panoramic radiographs should be evaluated considering the fact that CAC may occur at any age.28
Three groups were formed based on the age of the participants. It was found that the number of patients aged 40–55 years in the CAC (+) group was significantly higher than that of the CAC (–) group (P = 0.009), and the rate of patients under the age of 40 was significantly lower in CAC (+) (P = 0.003). These results are consistent with the literature19,23 and confirm that with older age, there is an increase in suspected cases of carotid calcification and thus an age-dependent risk for this condition.
In the present study, out of 34 patients with CAC, 21 (61.8%) were female and 13 (38.2%) were male; this difference was not statistically significant. This result is consistent with numerous earlier studies,12,21,26,29,30 whereas Tamura et al.31 reported that the CAC incidence in female subjects was almost three times that of males. This discrepancy between the studies might be due to the sample size of the study.
Diabetes, hypertension, and hyperlipidemia are well-defined risk factors for atherosclerosis; however, previous studies reported different results about the relationship between these risk factors and CAC. For instance, Ertas et al.32 found that CAC was correlated with hypertension and hyperlipidemia but not with diabetes, whereas Ramesh et al.3 reported a correlation between diabetes and CAC as well. In addition, there are many studies in the literature that did not find a relationship between diabetes,33 hypertension,29,34,35 hyperlipidemia,34,35 and CAC. In this study, no significant differences were found between groups with or without CAC with respect to diabetes, hypertension, and hyperlipidemia. This may be due to the fact that our sample consisted of relatively younger individuals as compared to previous studies.
In this study, we classified patients according to their smoking habits. No difference was observed in smoking behaviour between groups with or without CAC. In contrast to our study, many studies have observed a significant relationship between smoking status and CAC.29,32,36 However, consistent with our results, Monteiro et al.33 and Atalay et al.37 reported that smoking is not associated with prevalence of CAC. These disparate results may be due to the use of different populations across studies.
According to a recent consensus report, periodontitis is regarded as an important risk factor for developing carotid atherosclerosis. There are several proposed mechanisms that may link periodontitis and atherosclerosis. One such mechanism is based on the direct participation of oral bacteria in the pathogenesis of the atherosclerotic plaque. Another potential mechanism is the activation of the host inflammatory response that leads to increased serum levels of mediators such as C-reactive protein, interleukin-1β and 6, and tumour necrosis factor-alpha38.
Studies of the relationship between periodontal disease and CAC detected by DPRs used different assessment methods to define periodontal condition. For instance, some studies used an association between periodontal bone loss and CAC,3,39,40 whereas others evaluated the correlation between CAC and periodontal risk.12,13 Periodontitis was diagnosed using pocket depth, bone loss, and BOP values in only one study.14 In the present study, periodontal disease was categorised into three groups using the latest World Workshop classification system.17 To the best of our knowledge, the present study is the first published report to correlate the findings of such calcifications with age, gender, diabetes, hypertension, hyperlipidemia, smoking, and periodontal status in the general population. In this study, we found no correlation between periodontal disease and CAC. This result is in agreement with the two studies performed with general population samples3,12 but inconsistent with the results of the others conducted in older populations.3,14 The relatively younger population of our study may explain the absence of an effect of periodontitis on CAC.
Angiography is the most accurate method to assess atherosclerotic disease, but it is an invasive procedure. Therefore, Doppler ultrasonographic examination is used as a gold standard for diagnosis of atherosclerosis because similar results to angiography can be obtained with this non-invasive method. CAC can also be detected via DPR, which is an imaging tool mostly used in dental practice. However, a recent review reported wide variation in the specificity of CAC detection by DPR compared to the gold standard of carotid artery ultrasound examination.41 Because of its retrospective design, Doppler ultrasonographic examination could not be used in the present study, which is a main limitation of the study. Other limitations include the fact that it was a retrospective study and had only a single radiologist. Lastly, in the advanced stages of periodontitis, teeth are frequently extracted because of the loss of supporting structure. In light of this, the lack of the evaluation of tooth loss may be regarded as a limitation of this study.
In conclusion, using DPRs, CAC was detected in 3.1% of the patients, and the results of the current study showed no correlation between periodontal status and CAC. The cause of these results was likely particular elements of the study design and study population. It is important to clarify the possible relationship between periodontitis and CAC with additional studies and to draw attention to this issue. Clinicians should conduct routine DPRs in more detail to detect the presence of CAC since broad use of DPRs may lead to early diagnosis and can be life-saving for patients who are asymptomatic. In addition, early detection of CACs by DPRs may allow for faster referral to a physician for further medical evaluation.
REFERENCES
- 1.Herrington W, Lacey B, Sherliker P, et al. Epidemiology of atherosclerosis and the potential to reduce the global burden of atherothrombotic disease. Circ Res. 2016;118:535–546. doi: 10.1161/CIRCRESAHA.115.307611. [DOI] [PubMed] [Google Scholar]
- 2.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramesh A, Soroushian S, Ganguly R. Coincidence of calcified carotid atheromatous plaque, osteoporosis, and periodontal bone loss in dental panoramic radiographs. Imaging Sci Dent. 2013;43:235–243. doi: 10.5624/isd.2013.43.4.235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zeng XT, Leng WD, Lam YY, et al. Periodontal disease and carotid atherosclerosis: a meta-analysis of 17,330 participants. Int J Clin Cardiol. 2016;203:1044–1051. doi: 10.1016/j.ijcard.2015.11.092. [DOI] [PubMed] [Google Scholar]
- 5.Bengtsson VW, Persson GR, Berglund J, et al. Carotid calcifications in panoramic radiographs are associated with future stroke or ischemic heart diseases: a long-term follow-up study. Clin Oral Investig. 2019;23:1171–1179. doi: 10.1007/s00784-018-2533-8. [DOI] [PubMed] [Google Scholar]
- 6.Tonetti MS, Jepsen S, Jin L, et al. Impact of the global burden of periodontal diseases on health, nutrition and wellbeing of mankind: a call for global action. J Clin Periodontol. 2017;44:456–462. doi: 10.1111/jcpe.12732. [DOI] [PubMed] [Google Scholar]
- 7.Hamilton JA, Hasturk H, Kantarci A, et al. Atherosclerosis, periodontal disease, and treatment with resolvins. Curr Atheroscler Rep. 2017;19:57. doi: 10.1007/s11883-017-0696-4. [DOI] [PubMed] [Google Scholar]
- 8.Kassebaum NJ, Bernabe E, Dahiya M, et al. Global burden of severe periodontitis in 1990–2010: a systematic review and meta-regression. J Dent Res. 2014;93:1045–1053. doi: 10.1177/0022034514552491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dorfer CE, Becher H, Ziegler CM, et al. The association of gingivitis and periodontitis with ischemic stroke. J Clin Periodontol. 2004;31:396–401. doi: 10.1111/j.1600-051x.2004.00579.x. [DOI] [PubMed] [Google Scholar]
- 10.Grau AJ, Becher H, Ziegler CM, et al. Periodontal disease as a risk factor for ischemic stroke. Stroke. 2004;35:496–501. doi: 10.1161/01.STR.0000110789.20526.9D. [DOI] [PubMed] [Google Scholar]
- 11.Leira Y, Seoane J, Blanco M, et al. Association between periodontitis and ischemic stroke: a systematic review and meta-analysis. Eur J Epidemiol. 2017;32:43–53. doi: 10.1007/s10654-016-0170-6. [DOI] [PubMed] [Google Scholar]
- 12.Tiller R, Bengel W, Rinke S, et al. Association between carotid area calcifications and periodontal risk: a cross sectional study of panoramic radiographic findings. BMC Cardiovasc Disord. 2011;11:67. doi: 10.1186/1471-2261-11-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kamak G, Yildirim E, Rencber E. Evaluation of the relationship between periodontal risk and carotid artery calcifications on panoramic radiographs. Eur J Dent. 2015;9:483–489. doi: 10.4103/1305-7456.172614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bengtsson VW, Persson GR, Berglund J, et al. A cross-sectional study of the associations between periodontitis and carotid arterial calcifications in an elderly population. Acta Odontol Scand. 2016;74:115–120. doi: 10.3109/00016357.2015.1050603. [DOI] [PubMed] [Google Scholar]
- 15.Loe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38(Suppl):610–616. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 16.Trombelli L, Farina R, Silva CO, et al. Plaque-induced gingivitis: case definition and diagnostic considerations. J Clin Periodontol. 2018;45(Suppl 20):S44–S67. doi: 10.1111/jcpe.12939. [DOI] [PubMed] [Google Scholar]
- 17.Papapanou PN, Sanz M, Buduneli N, et al. Periodontitis: consensus report of workgroup 2 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol. 2018;89(Suppl 1):S173–S182. doi: 10.1002/JPER.17-0721. [DOI] [PubMed] [Google Scholar]
- 18.Maia PRL, Medeiros AMC, Pereira HSG, et al. Presence and associated factors of carotid artery calcification detected by digital panoramic radiography in patients with chronic kidney disease undergoing hemodialysis. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;126:198–204. doi: 10.1016/j.oooo.2018.04.005. [DOI] [PubMed] [Google Scholar]
- 19.Santos JM, Soares GC, Alves AP, et al. Prevalence of carotid artery calcifications among 2,500 digital panoramic radiographs of an adult Brazilian population. Med Oral Patol Oral Cir Bucal. 2018;23:e256–e261. doi: 10.4317/medoral.22350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Friedlander AH, Lande A. Panoramic radiographic identification of carotid arterial plaques. Oral Surg Oral Med Oral Pathol. 1981;52:102–104. doi: 10.1016/0030-4220(81)90181-x. [DOI] [PubMed] [Google Scholar]
- 21.Pornprasertsuk-Damrongsri S, Thanakun S. Carotid artery calcification detected on panoramic radiographs in a group of Thai population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:110–115. doi: 10.1016/j.tripleo.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 22.Barona-Dorado C, Gutierrez-Bonet C, Leco-Berrocal I, et al. Relation between diagnosis of atheromatous plaque from orthopantomographs and cardiovascular risk factors. A study of cases and control subjects. Med Oral Patol Oral Cir Bucal. 2016;21:e66–e71. doi: 10.4317/medoral.20183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee JS, Kim OS, Chung HJ, et al. The prevalence and correlation of carotid artery calcification on panoramic radiographs and peripheral arterial disease in a population from the Republic of Korea: the Dong-gu study. Dentomaxillofac Radiol. 2013;42 doi: 10.1259/dmfr/29725099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gustafsson N, Ahlqvist JB, Naslund U, et al. Calcified carotid artery atheromas in panoramic radiographs are associated with a first myocardial infarction: a case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018;125:199–204. doi: 10.1016/j.oooo.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 25.Nasseh I, Aoun G. Carotid artery calcification: a digital panoramic-based study. Diseases. 2018;6:5. doi: 10.3390/diseases6010015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bayram B, Uckan S, Acikgoz A, et al. Digital panoramic radiography: a reliable method to diagnose carotid artery atheromas? Dentomaxillofac Radiol. 2006;35:266–270. doi: 10.1259/dmfr/50195822. [DOI] [PubMed] [Google Scholar]
- 27.Francoso LA, Coates V. Anatomicopathological evidence of the beginning of atherosclerosis in infancy and adolescence. Arq Bras Cardiol. 2002;78:131–142. [PubMed] [Google Scholar]
- 28.Bayer S, Helfgen EH, Bos C, et al. Prevalence of findings compatible with carotid artery calcifications on dental panoramic radiographs. Clin Oral Investig. 2011;15:563–569. doi: 10.1007/s00784-010-0418-6. [DOI] [PubMed] [Google Scholar]
- 29.Brito AC, Nascimento HA, Argento R, et al. Prevalence of suggestive images of carotid artery calcifications on panoramic radiographs and its relationship with predisposing factors. Cien Saude Colet. 2016;21:2201–2208. doi: 10.1590/1413-81232015217.06622015. [DOI] [PubMed] [Google Scholar]
- 30.Carter LC, Haller AD, Nadarajah V, et al. Use of panoramic radiography among an ambulatory dental population to detect patients at risk of stroke. J Am Dent Assoc. 1997;128:977–984. doi: 10.14219/jada.archive.1997.0338. [DOI] [PubMed] [Google Scholar]
- 31.Tamura T, Inui M, Nakase M, et al. Clinicostatistical study of carotid calcification on panoramic radiographs. Oral Dis. 2005;11:314–317. doi: 10.1111/j.1601-0825.2005.01125.x. [DOI] [PubMed] [Google Scholar]
- 32.Ertas ET, Sisman Y. Detection of incidental carotid artery calcifications during dental examinations: panoramic radiography as an important aid in dentistry. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112:e11–e17. doi: 10.1016/j.tripleo.2011.02.048. [DOI] [PubMed] [Google Scholar]
- 33.Monteiro IA, Ibrahim C, Albuquerque R, et al. Assessment of carotid calcifications on digital panoramic radiographs: retrospective analysis and review of the literature. J Stomatol Oral Maxillofac Surg. 2018;119:102–106. doi: 10.1016/j.jormas.2017.11.009. [DOI] [PubMed] [Google Scholar]
- 34.Taheri JB, Moshfeghi M. Prevalence of calcified carotid artery on panoramic radiographs in postmenopausal women. J Dent Res Dent Clin Dent Prospects. 2009;3:46–51. doi: 10.5681/joddd.2009.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Imanimoghaddam M, Rah Rooh M, Mahmoudi Hashemi E, et al. Doppler sonography confirmation in patients showing calcified carotid artery atheroma in panoramic radiography and evaluation of related risk factors. J Dent Res Dent Clin Dent Prospects. 2012;6:6–11. doi: 10.5681/joddd.2012.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guimaraes Henriques JC, Kreich EM, Helena Baldani M, et al. Panoramic radiography in the diagnosis of carotid artery atheromas and the associated risk factors. Open Dent. 2011;5:79–83. doi: 10.2174/1874210601105010079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Atalay Y, Asutay F, Agacayak KS, et al. Evaluation of calcified carotid atheroma on panoramic radiographs and Doppler ultrasonography in an older population. Clin Interv Aging. 2015;10:1121–1129. doi: 10.2147/CIA.S84683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sanz M, Marco Del Castillo A, Jepsen S, et al. Periodontitis and cardiovascular diseases: consensus report. J Clin Periodontol. 2020;47:268–288. doi: 10.1111/jcpe.13189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beckstrom BW, Horsley SH, Scheetz JP, et al. Correlation between carotid area calcifications and periodontitis: a retrospective study of digital panoramic radiographic findings in pretreatment cancer patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:359–366. doi: 10.1016/j.tripleo.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 40.Persson RE, Hollender LG, Powell VL, et al. Assessment of periodontal conditions and systemic disease in older subjects. II. Focus on cardiovascular diseases. J Clin Periodontol. 2002;29:803–810. doi: 10.1034/j.1600-051x.2002.290903.x. [DOI] [PubMed] [Google Scholar]
- 41.Bengtsson VW, Persson GR, Renvert S. Assessment of carotid calcifications on panoramic radiographs in relation to other used methods and relationship to periodontitis and stroke: a literature review. Acta Odontol Scand. 2014;72:401–412. doi: 10.3109/00016357.2013.847489. [DOI] [PubMed] [Google Scholar]