Abstract
Objectives
Poor oral hygiene can have an adverse effect on quality of life. School-based interventions can establish positive behaviours that reduce the likelihood of dental caries later in life. The Brush Day & Night programme aims to encourage good oral health behaviour and improve oral health and quality-of-life outcomes. In this article, we report the effect of the programme on well-being and oral hygiene measured by plaque levels at 3, 8, and 24 weeks and dental caries at 24 weeks after programme start date.
Methods
This was a superiority cluster randomised trial of children 6-12 years of age from Indonesia (N = 2021) and Nigeria (N = 2104). All children were provided with toothpaste and a toothbrush. Children in the intervention group received the 21-day Brush Day & Night programme, whereas those in the control group did not. Children completed a questionnaire addressing the objectives at all time points. Their oral hygiene was assessed using the Oral Hygiene Index-Simplified (OHI-S). Additionally, at baseline and 24 weeks their caries status was recorded using the decayed, missing, and filled teeth (DMFT) index.
Results
In Indonesia, after participation in the programme children demonstrated a 45% increased probability of no worsening in the occurrence of decayed, missing, or filled teeth. In Nigeria, children had a 71% higher probability of having confidence in their smile and the proportion of children with good oral hygiene doubled from 40% to 80% at 24 weeks.
Conclusions
The Brush Day & Night programme was successful in improving well-being and oral hygiene in children in Nigeria and reduced the likelihood of worsening in the occurrence of decayed, missing, or filled teeth in children in Indonesia.
Key words: Dental caries, Brush Day & Night, Quality of life, Oral hygiene
Introduction
Oral health has an impact on overall health and well-being of children.1 Dental caries is the most prevalent oral disease and, despite decreases in caries prevalence over the last decades, it remains a significant problem in developing countries2, 3, 4, 5, 6, 7, 8, 9, 10 and disproportionately affects people of lower socioeconomic status.11 Previous studies in both adults and children have demonstrated that the impact on quality of life (QoL) correlates with the severity of dental caries, with the greatest effect associated with the most severe dental caries.12,13 Untreated, it can lead to pain and infection and result in the need for tooth extraction.14
From the patient's perspective, dental caries can significantly affect QoL by impacting social functioning, including chewing, appetite, sleep, and absenteeism.15,16 In children, dental caries is associated with significant pain, poor general health and well-being, and lower body weight and growth.15 It is estimated that children miss 50 million school hours per year due to oral health problems, which can ultimately affect a child's success later in life.17
Dental caries is almost entirely preventable. Prevention is achieved through inexpensive methods such as limiting sugar intake and brushing teeth twice daily with a fluoride toothpaste.14,18,19 The prevention of dental caries could also significantly reduce the financial burden on health services.20 Establishing regular toothbrushing habits during childhood can help reduce the likelihood of caries in later life.21 Microbial dental plaque is one of the most important aetiological factors for dental caries,22 and toothbrushing is considered the simplest individual preventive measure for plaque control, and it is effective in the long-term preservation of oral health.23,24 Considering that a healthy mouth and teeth can be achieved with education and properly acquired habits during childhood,25 school-based interventions are ideal to establish these behaviours.17Evidence suggests that informing children about the best behaviours leads to a better knowledge of the link between plaque removal and reduction in risk for dental caries, ultimately improving oral hygiene and well-being.1,5,20,26, 27, 28, 29
A 2013 Cochrane review of school-based interventions found that interventions that utilise behavioural theory in their design improved children's oral health knowledge and plaque outcomes.15 To this end, FDI World Dental Federation (FDI) and Unilever have developed a 21-day school-based educational programme called Brush Day & Night (BDN). The BDN programme was designed based on the theories of behaviour change30 and aims to establish the habit of brushing day and night with a fluoride toothpaste. Participants are instructed on daily brushing and given free toothpaste and toothbrushes. In a previous study conducted in 10 countries with 7991 children aged 2-12 years, the 21-day BDN intervention led to a 25% increase in the number of schoolchildren brushing their teeth twice daily at the conclusion of the programme.31 However, as well-being and oral health status were not assessed in that study, it is not known whether the behaviour change prompted by the 21-day BDN intervention translates into health benefits.
The main aim of the present study (NCT04001296) is to determine the impact of the 21-day BDN intervention on children's well-being and oral hygiene in a randomised sample 3, 8, and 24 weeks after the start of the study, and decayed, missing and filled teeth after 24 weeks, compared with baseline and a control group in two countries, Nigeria and Indonesia.
Materials and methods
Study design
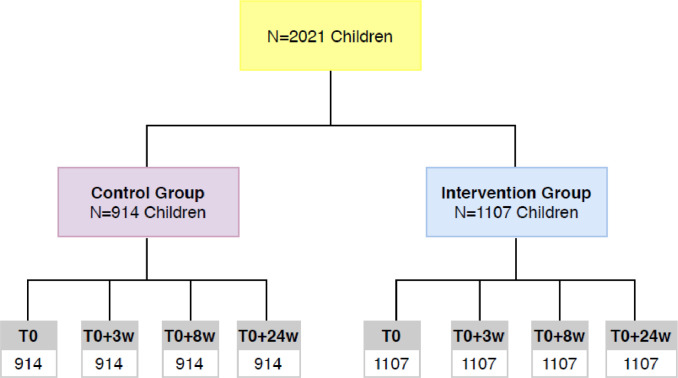
The methodology for this study has been described in detail previously.30 In brief, this was a two-arm, superiority, randomised controlled trial involving infant and junior schoolchildren aged 6-12 years from Indonesia and Nigeria. A total of 2021 children from Indonesia were included, 914 in the control group and 1107 in the intervention group. From Nigeria, a total of 1947 children were included, 915 in the control group and 1032 in the intervention group. Schools were matched into pairs by location (rural vs urban) and socioeconomic status and randomised to intervention and control groups using a randomisation table. The Nigerian study recruited children from 20 schools (10 in the control group and 10 in the intervention group, of which five were from rural locations and five from urban locations). The Indonesian study recruited children from 22 schools (10 in the control group, of which six were from rural locations and four were from urban locations, and 12 in the intervention group, of which eight were from rural locations and four from urban locations). Teachers were responsible for implementing the programme and were trained by local study coordinators. Schools in Indonesia were located in low- and middle-income areas, and schools in Nigeria were located in low- middle- and high-income settings.
Inclusion and exclusion criteria
The study included healthy children in grades 1, 2, and 3, in which most children are within the target age range of 6 to 12 years. Although the standard age range for these grades is 6-9 years, some children repeat school years, resulting in a broader age range being included in the study. Children needed to be willing and able to participate in the programme and planning to attend their school for the next 12 months. Children and families had no affiliation with FDI or Unilever.
The study excluded children who did not have a signed consent form, those scheduled for medical or dental procedures, those with allergies to toothpaste ingredients, those with obvious untreated caries or significant periodontal disease, and those whose well-being would be affected by the study.
Study endpoints
The primary endpoint of the study was to measure the impact of the 21-day school programme on oral hygiene via plaque levels and number of decayed, missing, and filled teeth in schoolchildren at different timepoints compared with baseline and with a control group. Plaque levels were measured by the short-form Oral Hygiene Index-Simplified (OHI-S) at all timepoints: baseline (T0), after 3 weeks (T0+21), 8 weeks (T1), and 24 weeks (T2). Decayed, missing and filled teeth were assessed by the Decayed Missing and Filled Teeth (DMFT) index at T0 and T2.
The secondary endpoint was to measure the impact of the 21-day BDN programme on well-being. This endpoint was measured using the percentage of positive change in answers to questions related to well-being in the children's questionnaire at all timepoints T0, T1, and T2. At baseline (T0), children answered a questionnaire consisting of eight main questions, of which three were related to well-being (Supplementary Figure 1, available online) and five were related to oral health knowledge and toothbrushing behaviour. The latter aspects are analysed and reported in a separate article in this supplement.32 Adverse events were also monitored.
Intervention
Children in the intervention schools took part in the structured 21-day Brush Day & Night programme and were each provided with toothpaste and a toothbrush at T0. Children were supervised when brushing and sang songs to facilitate learning the importance of brushing day and night, with stickers and calendars to track progress. A celebration was held at the end of the programme with certificates and rewards. The programme was supported by colourful materials with cartoon characters. Parents were provided with educational leaflets. Children in the control schools were provided with free toothpaste and toothbrushes at T0 but did not receive the 21-day intervention.
Statistical analysis
Baseline (T0) characteristics in the control and intervention groups were compared. Proportions and continuous variables were compared using the χ2 and Mann-Whitney tests, respectively. The frequency of each outcome (original and transformed variables) was estimated separately for the control and intervention groups and at each timepoint. The comparison of variables within the same group and across evaluation moments was performed for dependent groups, using McNemar's test for proportions and the Wilcoxon signed-rank test for continuous variables.
The variables “Mouth Pain,” “Smile Confidence,” and “Bullying because of teeth” were related to well-being. Improvement in well-being was calculated based on the percentage of positive change. Positive change was considered when a child moved from selecting a negative or neutral answer (ie, inadequate) to selecting a positive answer (ie, adequate) in any of the variables.
Particular outcome variables observed before and after the intervention/control period were categorised as adequate or inadequate using binary responses, where “1” represents adequacy and “0” represents inadequacy, as follows: Mouth Pain experience, "No pain" (1) vs “any reported level of pain” (0); Smile Confidence "Yes" (1) vs "No" or “Do not know” (0); Bullying because of teeth "No" (1) vs “Yes” or “Do not know” (0).
The effect of the intervention was analysed comparing the effect at each timepoint against baseline, with changes from adequate to inadequate categorised as “worse,” changes from inadequate to adequate categorised as “improved” and no change categorised as “equal.”
The effect of the intervention was analysed based on a conditional logistic approach for each of the three evaluation timepoints: T0 + 21, T1, and T2 and reported as odds ratio (OR) with 95% CI.
OHI-S score before and after the intervention/control was categorised as “poor,” “moderate,” or “good,” and change in plaque levels was categorised as “equal,” “improved,” or “worse.” The effect of the intervention on the DMFT Index was assessed using a standard logistic regression, where the response variable stated "Not worse" (no change in the index treated as a continuous variable) or "Worse" from T0 to T2 evaluation.
Crude estimates of the effect of the intervention on particular outcomes were adjusted for variables showing relevant relation with both assignment group and given outcome. Significant variables identified through a univariate analysis (P value ≤ .05) were selected from the grouped set of covariates: (i) basic children's data (age, grade, gender), (ii) children's other characteristics at baseline evaluation (their opinion on the importance of everyday brushing, usage of fluoride toothpaste, feeling of pain in mouth while eating), and (iii) location of school (rural or urban), and subsequently added to a model. As a result, each outcome was adjusted for a different combination of controlling variables.
Ethics
This study was conducted in accordance with the Declaration of Helsinki. Ethical approval was received from the Nigerian State Universal Basic Education Board and the Health Research Ethics Commission at the Faculty of Dental Teaching, Trisakti University, Indonesia. All parents or legal guardians of the participating children signed an informed consent form.
Results
Nigeria
Distribution of study participants
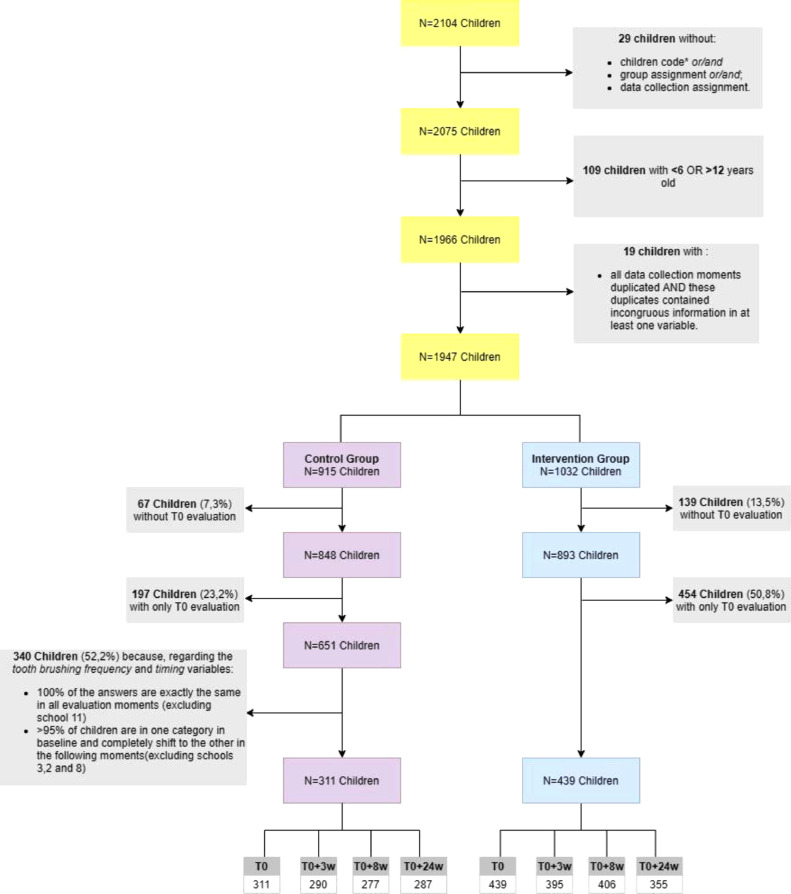
The recruitment of children is presented in Figure 1. A total of 5436 observations were made on 2104 children. Of these, 157 children were excluded before randomisation to give a total of 1947 (1032 in the intervention group and 915 in the control group). During the study, a further 593 children were excluded from the intervention group and 604 children from the control group, leaving 439 and 311, respectively.
Fig. 1.
Study flowchart for the Nigeria study.
*Number of children code incomplete (without identification of school and grade).
Baseline characteristics
Baseline characteristics are presented in Table 1. Median (25th–75th percentiles) ages of children were similar across intervention and control groups (9.0 [8.0–10.0] vs 8.0 [7.0–10] years, respectively). The distribution of male and female children was likewise similar (approximately 50%). The intervention group included significantly more children from rural or semirural areas than the control group (61.7% vs 53.4%; P = .027). Smile confidence was significantly lower in the intervention group compared with the control group (P = .005). The intervention group showed significant differences in oral hygiene, with 39.6%, 52.4%, and 8.0% of children presenting good, moderate, or poor oral hygiene, respectively, compared with 50.8%, 40.1%, and 9.1% in the control group (P = .01). Almost all children (approximately 92%) across both groups presented with no decayed, missing, or filled teeth.
Table 1.
Childrens' baseline characteristics by assigned group in the Nigeria study.
| Control 311 N (%)* |
Intervention 439 N (%)* |
P value† | |
|---|---|---|---|
| Age | |||
| Median (P25, P75) | 8.0 (7.0, 10.0) | 9.0 (8.0, 10.0) | .453 |
| Gender | |||
| Male | 161 (51.8) | 212 (48.8) | .305 |
| Female | 143 (46.0) | 222 (51.2) | |
| Schools | |||
| Rural | 166 (53.4) | 271 (61.7) | .027 |
| Urban | 145 (46.6) | 168 (38.3) | |
| Do not use | 16 (5.2) | 39 (8.9) | |
| Not sure | 21 (6.8) | 154 (35.2) | |
| Mouth Pain | |||
| Do not hurt | 244 (78.5) | 347 (79.4) | .989 |
| It hurts a little bit/sometimes | 29 (9.3) | 45 (10.3) | |
| It hurts | 15 (4.8) | 24 (5.5) | |
| It makes me cry | 8 (2.6) | 13 (3.0) | |
| Do not know | 6 (1.9) | 8 (1.8) | |
| Smile Confidence | |||
| Confident | 290 (94.2) | 393 (89.7) | .005 |
| Not confident | 13 (4.2) | 43 (9.8) | |
| Do not know | 3 (0.0) | 2 (0.5) | |
| Bullying | |||
| Do not feel bullied | 266 (88.4) | 373 (86.5) | .184 |
| Feel bullied and it's okay | 17 (5.6) | 22 (5.1) | |
| Feel bullied and feel sad | 13 (4.3) | 19 (4.4) | |
| Feel bullied and makes me cry | 4 (1.3) | 5 (1.2) | |
| Do not know | 1 (0.3) | 12 (2.8) | |
| OHI-S Scores | |||
| Good oral hygiene | 123 (50.8) | 158 (39.6) | .010 |
| Moderate oral hygiene | 67 (40.1) | 209 (52.4) | |
| Poor oral hygiene | 22 (9.1) | 32 (8.0) | |
| DMFT | |||
| 0 | 238 (94.4) | 364 (90.5) | .111 |
| 1 | 8 (3.2) | 24 (6.0) | |
| 2 | 5 (2.0) | 9 (2.2) | |
| 3-5 | 0 (0.0) | 5 (1.2) | |
| >5 | 1 (0.4) | 0 (0.0) | |
DMFT = decayed, missing, or filled teeth; OHI-S = Oral Hygiene Index-Simplified.
Percentage of non-missing responses within the study group.
Wilcoxon test for continuous variable; chi-square test for all other variables.
Effect of the BDN programme
Well-being
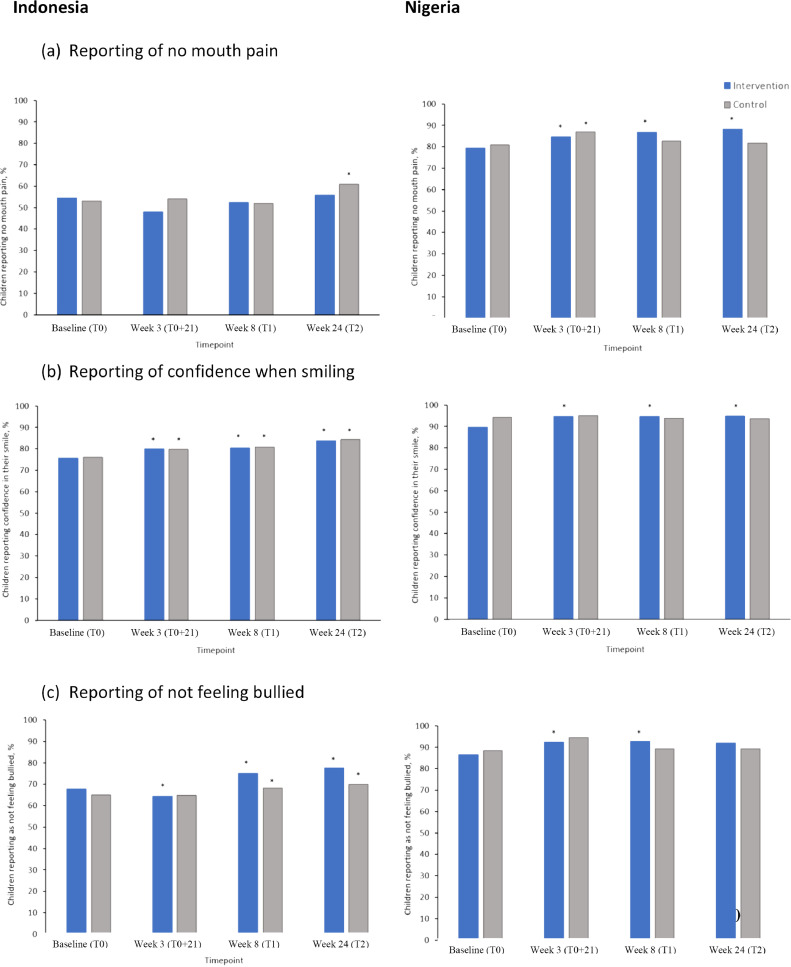
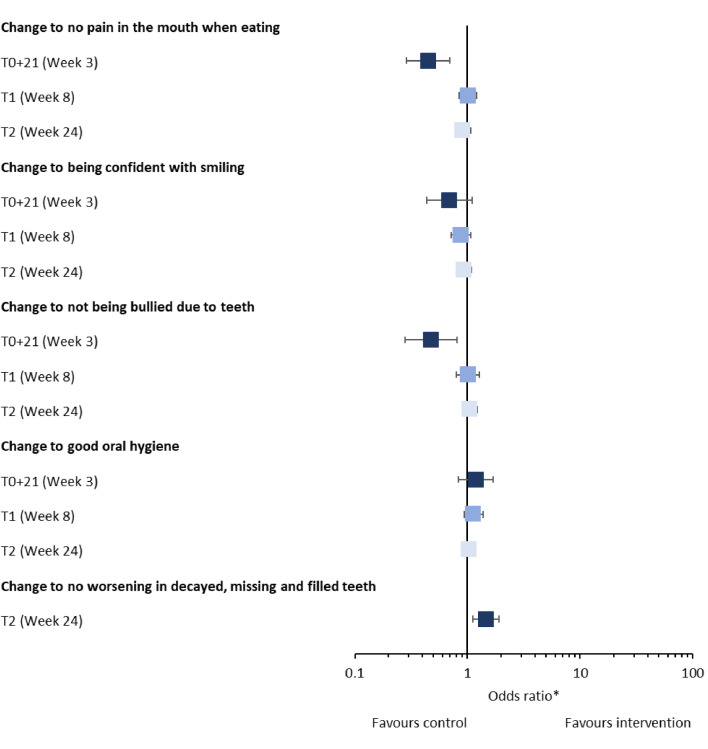
At Week 3 (T0 + 21), both control and intervention groups showed a significant decrease in mouth pain versus baseline (P < .05) (Figure 2A), but by Weeks 8 and 24 (T1 and T2), this was only seen in the intervention group. When adjusted for children and school characteristics, there were significantly more children reporting mouth pain in the intervention group at Week 3 (T0 + 21) compared with the control group (Table 2, Figure 3). There were no differences between groups at Weeks 8 or 24 (T1 and T2). In children reporting pain or unsure of pain at baseline, similar levels of improvement were seen for both groups across all timepoints.
Fig. 2.
Effect of Brush Day & Night programme or control on change in quality of life, well-being, and social measures of schoolchildren from Indonesia and Nigeria at Weeks 3, 8. and 24 compared with baseline (FAS). (A) Reporting of confidence when smiling. (B) Reporting of not feeling bullied. BDN = Brush Day & Night FAS = full analysis set; QoL = quality of life.
Table 2.
Effect of intervention on oral health, covariate analysis in the Nigeria study.
|
T0+3W |
T0+8W |
T0+24W |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | OR | 95% CI | N | OR | 95% CI | n | OR | 95% CI | ||
| Change to no pain in the mouth when eating | ||||||||||
| Crude effect of the intervention | 662 | 0.764 | 0.365-1.600 | 656 | 1.246 | 0.880-1.765 | 622 | 1.360 | 1.063-1.739 | |
| + children's age and grade | 275/387 | 0.646 | 0.293-1.425 | 263/393 | 1.311 | 0.908-1.893 | 277/345 | 1.387 | 1.066-1.803 | |
| + children's other characteristics*† | 0.367 | 0.145-0.926 | 1.058 | 0.709-1.577 | 1.229 | 0.921-1.640 | ||||
| + school location (rural vs urban) | 0.318 | 0.123-0.823 | 0.941 | 0.619-1.432 | 1.205 | 0.896-1.619 | ||||
| Change to being confident with the smile | ||||||||||
| Crude effect of the intervention | 662 | 1.948 | 0.671-5.655 | 662 | 1.433 | 0.886-2.317 | 621 | 1.471 | 1.059-2.043 | |
| + children´s other characteristics*‡ | 275/387 | 1.587 | 0.511-4.932 | 266/396 | 1.205 | 0.719-2.020 | 276/345 | 1.521 | 1.059-2.184 | |
| + school location (rural vs urban) | 2.938 | 0.743-11.616 | 1.308 | 0.764-2.238 | 1.709 | 1.132-2.581 | ||||
| Change to not being bullied due to teeth | ||||||||||
| Crude effect of the intervention | 660 | 0.640 | 0.241-1.700 | 651 | 1.451 | 0.948-2.221 | 620 | 1.088 | 0.919-1.454 | |
| + children's grade | 276/384 | 0.599 | 0.206-1.742 | 260/391 | 1.868 | 1.129-3.092 | 277/343 | 1.100 | 0.789-1.533 | |
| + children's other characteristics†§ | 0.640 | 0.208-1.966 | 2.222 | 1.275-3.875 | 1.114 | 0.788-1.573 | ||||
| + school location (rural vs urban) | 0.633 | 0.206-1.942 | 2.381 | 1.340-4.231 | 1.147 | 0.802-1.642 | ||||
| Change to "Good" OHI-S category | ||||||||||
| Crude effect of the intervention | 507 | 9.707 | 4.270-22.670 | 537 | 5.066 | 3.230-7.947 | 479 | 3.515 | 2.594-4.843 | |
| + children's age | 169/338 | 10.451 | 4.502-24.264 | 186/351 | 5.738 | 3.503-9.399 | 194/285 | 3.504 | 2.561-4.793 | |
| + school location (rural vs urban) | 10.906 | 4.631-25.685 | 5.741 | 3.504-9.406 | 3.769 | 2.675-5.311 | ||||
| No worsening in DMFT Index | ||||||||||
| Crude effect of the intervention | 519 | 0.143 | 0.018-1.126 | |||||||
| + children's age | 210/309 | 0.139 | 0.017-1.102 | |||||||
| + school location (rural vs urban) | 0.120 | 0.014-0.932 | ||||||||
CI = confidence intervals; DMFT = decayed, missing, or filled teeth; n, number of children (control/intervention); OHI-S = Oral Hygiene Index-Simplified; OR = odds ratio.
Usage of fluoride toothpaste at baseline child's adequacy of brushing timing at baseline.
Child's adequacy of brushing frequency at baseline.
Experience of being laughed at because of teeth.
Confidence when smiling.
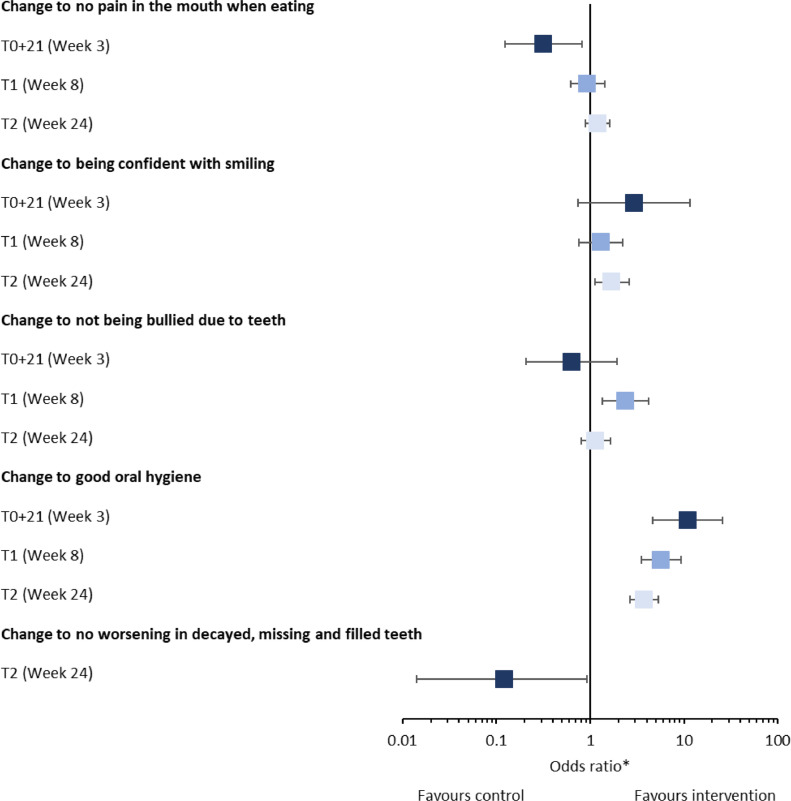
Fig. 3.
Effect of Brush Day & Night programme on well-being and oral health in schoolchildren from Nigeria at Weeks 3, 8, and 24 compared with control (FAS). BDN = Brush Day & Night; FAS = full analysis set.
*Adjusted for child's age and school location.
In children from the intervention group, the proportion reporting confidence in their smile significantly increased at all timepoints compared with baseline (Figure 2B) (P < .05). When adjusted for children and school characteristics, this increase was observed at Week 24 (T2) only when children had a 71% higher probability of having smile confidence (Table 2, Figure 3). In children with no confidence in their smile or no opinion at baseline, most declared an improvement at all timepoints compared with baseline in both the control and intervention groups (Supplementary Figure 2B, available online).
The proportion of children who were bullied due to their teeth decreased at all timepoints for all children but, particularly, for those in the intervention group. Significantly fewer children in the intervention group reported not feeling bullied at Weeks 3 (T0 + 21) and 8 (T1) compared with baseline (P < .05) (Figure 2C). When adjusted for children and school characteristics, at Week 8 (T1), significantly fewer children felt bullied in the intervention group compared with the control group (Table 2, Figure 3). In children who felt they were bullied due to their teeth at baseline, there was an improvement in all severity categories at all timepoints in children in both groups, although improvements appeared greater in children in the intervention groups (Supplementary Figure 2C, available online).
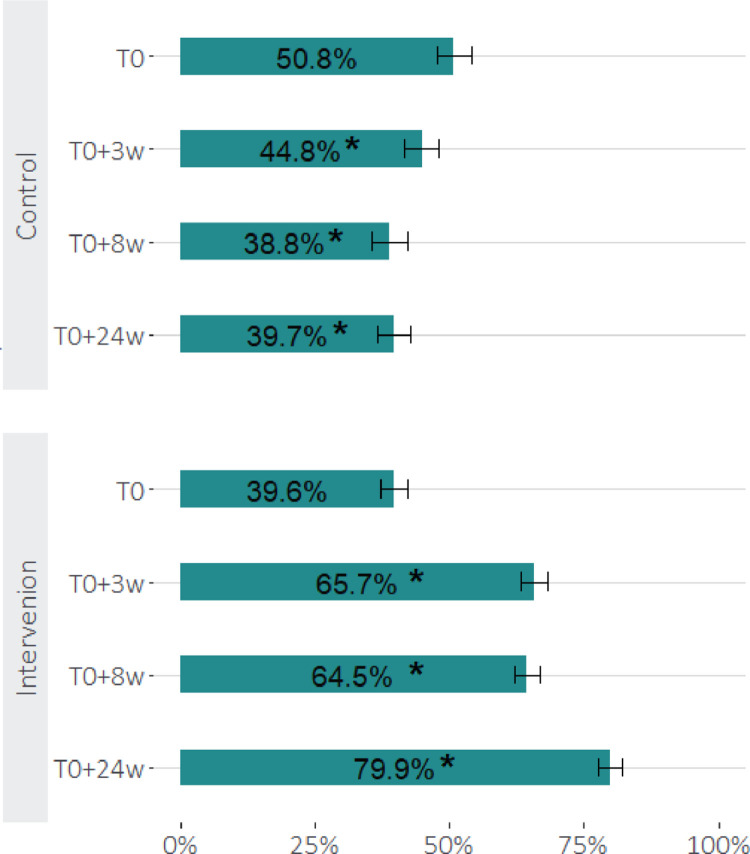
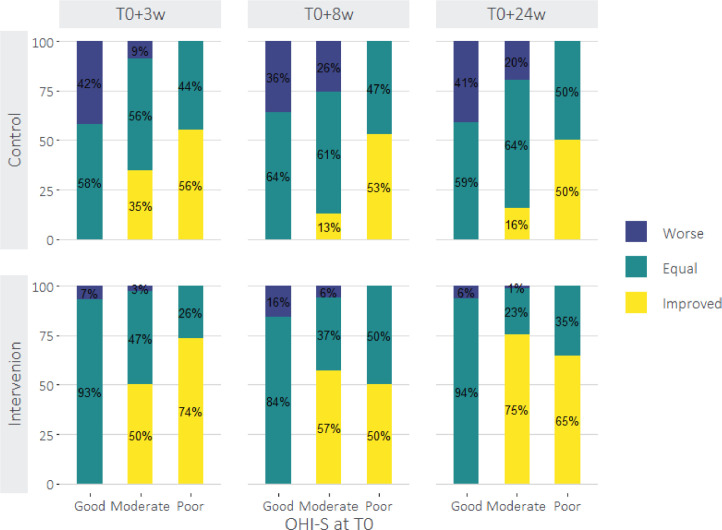
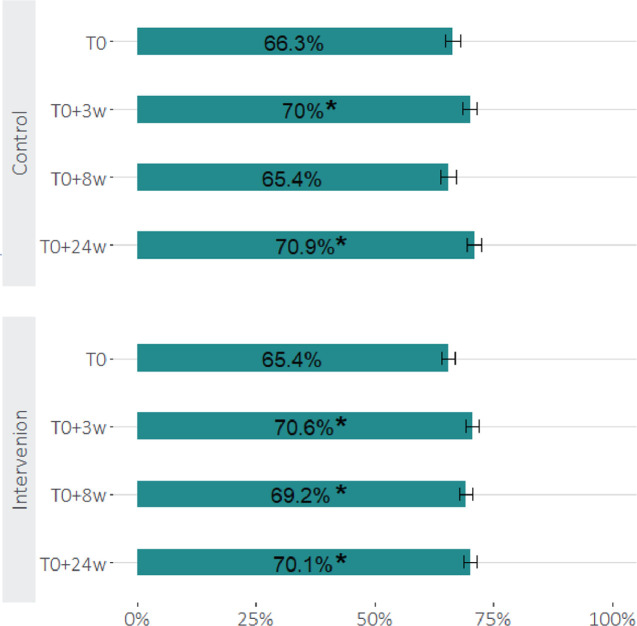
Oral hygiene
At baseline in Nigeria, 39.6% of children in the intervention group presented with good oral hygiene. There was an upward trend in oral hygiene over the duration of the programme, increasing to 65.7%, 64.5%, and 79.9% of children with good oral hygiene at 3, 8 and 24 weeks, respectively (P < .05 with respect to baseline) (Figure 4). In the control group, 50.8% of children presented with good oral hygiene at baseline. However, unlike the intervention group, there was a downward trend in oral hygiene over the 24-week period (44.8%, 38.8 %, and 39.7% of children with good oral hygiene at 3, 8, and 24 weeks, respectively; P < .05 with respect to baseline). When assessed by baseline status (Figure 5), oral hygiene did not improve in either the intervention or control group in children presenting good oral hygiene at baseline over the 24-week period. However, in children with moderate oral hygiene at baseline, improvement was observed over time in the intervention group compared with the control group (50%, 57%, and 75% of children with good oral hygiene at 3, 8, and 24 weeks, respectively, compared with 35%, 13%, and 16%, respectively; P < .001 for all timepoints). In children with poor oral hygiene at baseline, except for the 8-week timepoint, improvement was observed in the intervention group compared with the control group, but with no pattern over time (74%, 50%, and 65% of children with good oral hygiene at 3, 8, and 24 weeks, respectively, compared with 56%, 53%, and 50%, respectively; P < .001 for all timepoints). Covariate analysis revealed an odds ratio (OR) (95% CI), independent of age and school location, for change of OHI-S category to “good” at 3 weeks of 10.9 (4.631-25.685), which decreased over time to 3.8 (2.675-5.311) at 24 weeks (Table 2, Figure 3).
Fig. 4.
Proportion of children with good oral hygiene by OHI-S score in the Nigeria study. OHI-S = Oral Hygiene Index-Simplified.
*Statistically significant difference in proportions relative to baseline (P value < .05 from McNemar's test).
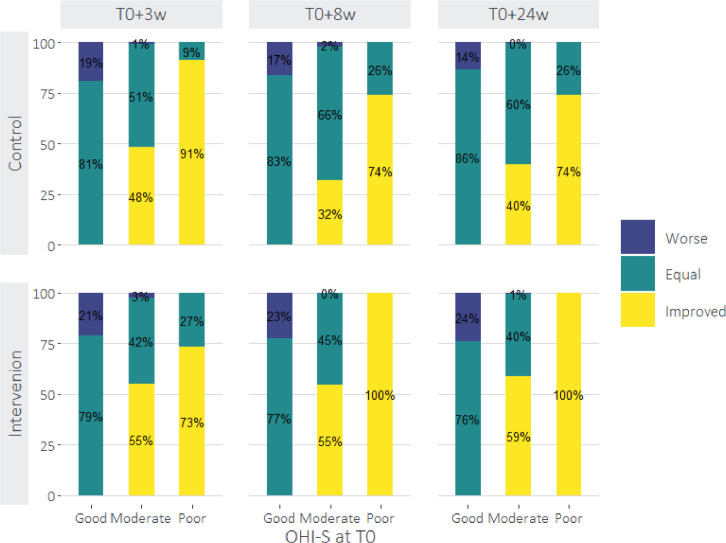
Fig. 5.
Change in OHI-S score category according to baseline status in the Nigeria study. OHI-S = Oral Hygiene Index-Simplified.
Decayed, missing, and filled teeth
At baseline, approximately 92% of children presented with a DMFT index of 0, indicating no decayed, missing, or filled teeth. At 24 weeks, 3% of children in the intervention group presented with a worse (increased) DMFT score, whereas all children in the control group continued to present with a DMFT score of 0 (Figure 6). However, covariate analysis revealed no impact of the programme on the OR of no worsening in the DMFT index at 24 weeks, either crude or adjusted for children's age and school location (Table 2, Figure 3).
Fig. 6.
Change in DMFT score by assigned group in the Nigeria study. DMFT = decayed, missing, or filled teeth.
Indonesia
Distribution of study participants
The recruitment of children is presented in Figure 7. A total of 8084 observations were made in 2021 children (1107 in the intervention group and 914 in the control group). All evaluation timepoints were available for all children and none were excluded.
Fig. 7.
Study flowchart for the Indonesia study.
Baseline characteristics
Baseline characteristics are presented in Table 3. Children in the intervention group were older by 1 year compared with the control group (median [25th–75th percentiles] 10 [9–10] vs 9 [7–10], respectively). The distribution of male and female children was similar across intervention and control groups (approximately 50%). The intervention group included more children from rural or semirural areas than the control (67.4% vs 60.5%). There was a significant difference in mouth pain between the intervention and control groups. Approximately 66% of children across both groups presented with good oral hygiene, and approximately 32% presented with moderate oral hygiene. However, only approximately 10% of children presented with no decayed, missing, or filled teeth, with a median DMFT score of 6.
Table 3.
Childrens' baseline characteristics by assigned group in the Indonesia study.
| Control914 N (%)* | Intervention1107 N (%)* | P value† | |
|---|---|---|---|
| Age | |||
| Median (P25, P75) | 9 (7, 10) | 10 (9, 10) | .008 |
| Gender | |||
| Male | 449 (49.1) | 559 (50.5) | .569 |
| Female | 465(50.9) | 548 (49.5) | |
| Schools | |||
| Rural | 553 (60.5) | 746 (67.4) | .001 |
| Urban | 361 (39.5) | 361 (32.6) | |
| Mouth Pain | |||
| Do not hurt | 484 (53.1) | 603 (54.6) | .001 |
| It hurts a little bit/sometimes | 212 (23.2) | 225 (20.4) | |
| It hurts | 88 (9.6) | 163 (14.8) | |
| It makes me cry | 84 (9.2) | 77 (7.0) | |
| Do not know | 44 (4.8) | 37 (3.2) | |
| Smile Confidence | |||
| Confident | 693 (76.0) | 834 (75.6) | .978 |
| Not confident | 190 (20.8) | 234 (21.2) | |
| Do not know | 29 (3.2) | 35 (3.2) | |
| Bullying | |||
| Do not feel bullied | 593 (65.0) | 741 (67.7) | .120 |
| Feel bullied and it's okay | 228 (25.0) | 222 (20.3) | |
| Feel bullied and feel sad | 51 (5.6) | 74 (6.8) | |
| Feel bullied and makes me cry | 10 (1.1) | 13 (1.2) | |
| Do not know | 30 (3.3) | 44 (4.0) | |
| OHI-S scores | |||
| Good oral hygiene | 606 (66.4) | 724 (65.4) | .112 |
| Moderate oral hygiene | 284 (31.1) | 368 (33.2) | |
| Poor oral hygiene | 23 (2.5) | 15 (1.4) | |
| DMFT | |||
| Median (P25, P75) | 6 (3, 10) | 6 (3, 9) | .086 |
| Categories | |||
| 0 | 81 (8,9) | 113 (10,2) | .625 |
| 1 | 52 (5,7) | 58 (5,2) | |
| 2 | 63 (6,9) | 90 (8,1) | |
| 3-5 | 217 (23,8) | 265 (23,9) | |
| >5 | 500 (54,8) | 581 (52,5) | |
DMFT = decayed, missing, or filled teeth; OHI-S = Oral Hygiene Index-Simplified.
Percentage of non-missing responses within the study group.
Wilcoxon test for continuous variable; chi-square test for all other variables.
Effect of the BDN programme
Well-being
At baseline, more than 40% of children from both groups in Indonesia reported mouth pain when eating. There were no significant differences in the proportion of children from either the intervention or control group reporting mouth pain at baseline or Weeks 3 and 8 (T0, T0 + 21, and T1) (Figure 2A). At Week 24 (T2), there were significantly fewer children reporting mouth pain in the control group compared with baseline (P < .05), but there was no significant difference from baseline in children in the intervention group.
When adjusted for children and school characteristics, there were significantly fewer children reporting mouth pain in the control group at Week 3 (T0 + 21) compared with the intervention group (P < .05) (Table 4, Figure 8). In children who reported pain at baseline, there was a similar improvement in reduction in pain severity at all timepoints in both the control and intervention group (Supplementary Figure 2A, available online).
Table 4.
Effect of intervention on oral health, covariate analysis in the Indonesia study.
|
T0+3W |
T0+8W |
T0+24W |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | OR | 95% CI | n | OR | 95% CI | n | OR | 95% CI | ||
| Change to no pain in the mouth when eating | ||||||||||
| Crude effect of the intervention | 2010 | 0.516 | 0.358-0.743 | 2001 | 0.974 | 0.826-1.147 | 1998 | 0.855 | 0.766-0.956 | |
| + children's sex and grade | 2010 | 0.521 | 0.361-0.753 | 2001 | 0.973 | 0.830-1.156 | 1998 | 0.859 | 0.767-0.961 | |
| + children's other characteristics* | 2010 | 0.492 | 0.333-0.726 | 2001 | 0.959 | 0.811-1.134 | 1998 | 0.852 | 0.760-0.955 | |
| + school location (rural vs urban) | 2010 | 0.445 | 0.286-0.694 | 2001 | 1.010 | 0.841-1.213 | 1998 | 0.902 | 0.793-1.065 | |
| Change to being confident with the smile | ||||||||||
| Crude effect of the intervention | 1997 | 1.018 | 0.693-1.496 | 2007 | 0.918 | 0.763-1.106 | 2000 | 1.005 | 0.884-1.142 | |
| + children's sex and grade | 1997 | 1.024 | 0.696-1.507 | 2007 | 0.917 | 0.761-1.104 | 2000 | 1.001 | 0.880-1.138 | |
| + children's other characteristics* | 1997 | 1.069 | 0.711-1.607 | 2007 | 0.918 | 0.760-1.110 | 2000 | 0.995 | 0.871-1.137 | |
| + school location (rural vs urban) | 1997 | 0.690 | 0.434-1.095 | 2007 | 0.874 | 0.718-1.064 | 2000 | 0.935 | 0.806-1.084 | |
| Change to not being bullied due to teeth | ||||||||||
| Crude effect of the intervention | 2001 | 0.752 | 0.508-1.130 | 1998 | 1.080 | 0.879-1.326 | 1997 | 1.107 | 0.969-1.265 | |
| + children's sex and grade | 2001 | 0.749 | 0.489-1.126 | 1998 | 1.081 | 0.879-1.330 | 1997 | 1.114 | 0.974-1.273 | |
| + children's other characteristics* | 2001 | 0.847 | 0.550-1.304 | 1998 | 1.029 | 0.822-1.289 | 1997 | 1.076 | 0.933-1.242 | |
| + school location (rural vs urban) | 2001 | 0.475 | 0.281-0.803 | 1998 | 1.014 | 0.799-1.286 | 1997 | 1.047 | 0.892-1.228 | |
| Change to "Good" OHI-S category | ||||||||||
| Crude effect of the intervention | 2015 | 1.054 | 0.765-1.453 | 2015 | 1.169 | 0.981-1.392 | 2015 | 0.950 | 0.848-1.065 | |
| + children's sex and grade | 2015 | 1.044 | 0.756-1.442 | 2015 | 1.173 | 0.853-1.398 | 2015 | 0.942 | 0.840-1.057 | |
| + children's other characteristics* | 2015 | 1.136 | 0.812-1.590 | 2015 | 1.182 | 0.988-1.415 | 2015 | 0.940 | 0.834-1.058 | |
| + school location (rural vs urban) | 2015 | 1.191 | 0.835-1.702 | 2015 | 1.131 | 0.933-1.372 | 2015 | 1.027 | 0.902-1.170 | |
| No worsening in DMFT Index | ||||||||||
| Crude effect of the intervention | 2015 | 0.786 | 0.624-0.990 | |||||||
| + baseline DMFT Index | 2015 | 0.801 | 0.635-1.011 | |||||||
| + children's sex and grade | 2015 | 0.805 | 0.638-1.016 | |||||||
| + children's other characteristics a | 2015 | 0.794 | 0.628-1.004 | |||||||
| + school location (rural vs urban) | 2015 | 1.454 | 1.115-1.891 | |||||||
CI = confidence interval; DMFT = decayed, missing, or filled teeth; n, number of children; OHI-S = Oral Hygiene Index- Simplified; OR, odds ratio.
Child´s opinion on the importance of everyday brushing (at baseline), usage of fluoride toothpaste (at baseline), feeling of pain in the mouth while eating (at baseline).
Fig. 8.
Effect of BDN programme on well-being and oral health in schoolchildren from Indonesia at Weeks 3, 8, and 24 compared with control (FAS). BDN = Brush Day & Night; FAS = full analysis set.
*Adjusted for child's age and school location.
The proportion of children reporting confidence in their smile significantly increased in both the intervention and control group at all timepoints compared with baseline (Figure 2B). When adjusted for children and school characteristics, there was no significant difference between the intervention and control groups in the proportion of children reporting confidence in their smile (Table 4, Figure 8). In children with no confidence in their smile or no opinion at baseline, except for the control group at Week 3, most declared an improvement at all timepoints compared with baseline in both the control and intervention groups (Supplementary Figure 2B, available online).
The proportion of children who were bullied due to their teeth decreased significantly at Weeks 8 and 24 (T1 and T2) for all children, but particularly for those in the intervention group (P < .05) (Figure 2C). When adjusted for children and school characteristics, there was no significant difference between groups at all timepoints, apart from Week 3, when there was a significant increase in the number of children in the intervention group who felt they were bullied due to their teeth compared with those in the control group (Table 4, Figure 8). In children who felt they were bullied due to their teeth at baseline, there was an improvement in all severity categories at all timepoints in both groups, although improvements appeared greater in children in the intervention group (Supplementary Figure 2C, available online).
Oral hygiene
At baseline in Indonesia, 65.4% of children in the intervention group presented with good oral hygiene. There was a slight upwards trend in oral hygiene over 3, 8 and 24 weeks, increasing to 70.6%, 69.2%, and 70.1% of children with good oral hygiene, respectively (P < .05 with respect to baseline) (Figure 9). In the control group, 66.4% of children presented with good oral hygiene at baseline. As with the intervention group, there was a slight upwards trend in oral hygiene over the 24-week period (70.0%, 65.4 %, and 70.9% of children with good oral hygiene, P < .05 with respect to baseline). When assessed by baseline status (Figure 10), oral hygiene did not improve in either the intervention or control group in children presenting with good oral hygiene at baseline over the 24-week period. However, in children with moderate oral hygiene at baseline, improvement was observed in the intervention group compared with the control group (55%, 55%, and 59% of children with good oral hygiene at 3, 8, and 24 weeks, respectively, compared with 48%, 32%, and 40%, respectively; P < .001). In children with poor oral hygiene at baseline, except for the 3-week time point, a marked improvement in oral hygiene was observed in the intervention group compared with the control group (73%, 100%, and 100% of children with good oral hygiene at 3, 8, and 24 weeks, respectively, compared with 91%, 74%, and 74%, respectively; P < .001). Covariate analysis revealed no increased likelihood of changing category to “good” at any time point over 24 weeks (Table 4, Figure 8).
Fig. 9.
Proportion of children with good oral hygiene by OHI-S score in the Indonesia study. OHI-S = Oral Hygiene Index-Simplified.
*Statistically significant difference in proportions relative to baseline (P value < .05 from McNemar's test).
Fig. 10.
Change in OHI-S score category according to baseline status in the Indonesia study. OHI-S = Oral Hygiene Index-Simplified.
Decayed, missing and filled teeth
At baseline, only approximately 10% of children presented with a DMFT index of 0, indicating the presence of decayed, missing, or filled teeth in approximately 90% of children, with a mean DMFT index of 6 (Table 3). At 24 weeks, the score remained unchanged (Figure 11), and approximately 22% of children in both groups showed worsening (Figure 12). However, covariate analysis revealed an OR (95% CI) of no worsening in DMFT index at 24 weeks of 1.45 (1.115-1.891) and 0.79 (0.624-0.990 when adjusted for baseline DMFT Index, sex, school grade, baseline opinion on importance of everyday brushing, use of fluoride toothpaste, and feeling of pain in the mouth while eating [Table 4, Figure 8]).
Fig. 11.
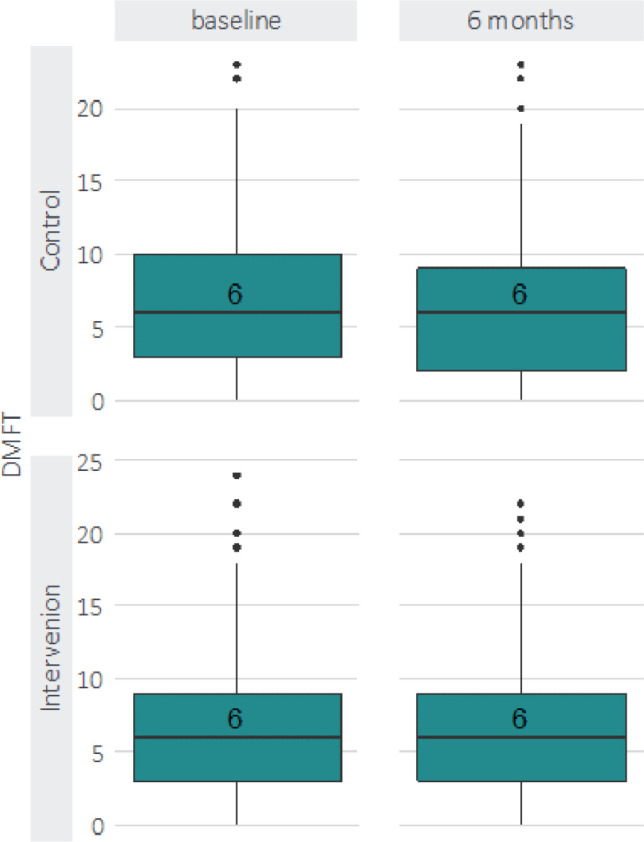
Distribution of DMFT by evaluation moment and assigned group in the Indonesia study. DMFT = decayed, missing, or filled teeth.
Fig. 12.

Change in DMFT by assigned group in the Indonesia study. DMFT = decayed, missing, or filled teeth.
Discussion
Childhood is a good time to introduce new toothbrushing habits because children seem to be receptive, and it is when their personality starts to develop together with mental maturation, increasing the likelihood for these habits to be maintained for life.25,33 The BDN programme developed by FDI and Unilever aims to instigate behavioural change leading to twice-daily brushing with a fluoride toothpaste in countries of low socioeconomic status. A previous study showed that the 21-day BDN intervention led to a 25% increase in the number of schoolchildren brushing their teeth twice daily and a further 8% improvement after 6-12 months.31 The main aim of the present study is to determine the impact of the 21-day BDN intervention on the well-being and oral health of children in Nigeria and Indonesia.
This study focuses on three key areas that may be burdensome to schoolchildren in terms of well-being: mouth pain, confidence in their smile, and feeling bullied because of their teeth. Oral health-related QoL is an outcome that has garnered increasing interest due to the growing focus on patient-centered care, and the recognition that health extends beyond disease, encompassing a state of physical, mental, and social well-being.16 In this study, we attempted to measure well-being through three questions addressing symptomatic, psychological, and social interaction domains. The oral health-related to quality of life (OHIP-14) questionnaire could have been introduced, but children at this age require either a simpler format or an interviewer to supervise/administer the questionnaire,34 which would have made the questionnaire too time-consuming to implement.
In the Nigerian study, baseline characteristics showed some significant differences in terms of happiness with smile and good oral hygiene being more prevalent in the control group.
After participation in the BDN programme, when adjusted for children's and school characteristics, the intervention group children showed a 71% higher probability of smile confidence after 24 weeks.
This is one of the expected outcomes of an intervention because children feel that they are taking care of their teeth, making them cleaner and brighter.35 On the other hand, six months may not be a long enough period to observe if this intervention can modify mouth pain and bullying, although an overall improvement in both groups was measured.
In the Nigerian study, poor oral hygiene was rare, and prevalence was similar across both groups, as was occurrence of dental caries. After 24 weeks, the proportion of children achieving good oral hygiene doubled in the intervention group and decreased in the control group. Analysis of baseline oral hygiene revealed that this effect of the programme was seen in children presenting with moderate or poor oral hygiene. Covariate analysis revealed that children in the intervention group were almost 11 times more likely to change OHI-S category to “good” at 3 weeks, independently of age and school location, but this effect declined to 3.8 times more likely at 24 weeks. These findings are in accordance with studies that include regularly conducted interactive education25,36,37 and where significant reduction in plaque index scores was reported after intervention.38,39 This study shows that the 21-day programme can maintain good oral hygiene in children for 6 months without the need of any additional intervention during this period.
Almost all children in Nigeria presented no decayed, missing, or filled teeth at baseline. However, after 24 weeks, 3% of the children in the intervention group had a worse DMFT score, whereas those in the control group maintained a DMFT score of 0. Covariate analysis revealed a likelihood of DMFT worsening by more than 8-fold. It is challenging to explain this because there is no reason for worsening of the DMFT score, mainly because in a low-caries-prevalence population one would not expect to observe a significant change in this short period of time.
In the Indonesia study, the intervention group had significantly more mouth pain at baseline. Baseline caries were similar across groups with the majority having good oral hygiene, but with high caries prevalence and severity. However, unlike what was seen in Nigeria, there seems to be a negative correlation between good oral hygiene and high incidence of dental caries. In Indonesian children, the high caries prevalence cannot be due to bad oral hygiene habits, as reported in a separate article in this supplement.32 This negative correlation might be explained by the fact that dental caries is a multifactorial disease where different factors may play a role in the disease manifestation and not only oral hygiene.40,41 Behavioural factors such as regular toothbrushing, use of dental floss and mouthwashes, a balanced diet, and regular visits to oral-health professionals are all associated with a decreased risk of dental caries.16,17
After the BDN programme, changes in mouth pain, smile confidence, and bullying were similar in both the intervention and control groups, in both the crude and adjusted analyses. As with the Nigerian study, six months may be too short a period to observe changes to the bully experience and pain. The high level of caries experienced at baseline may explain the lack of effect on smiling confidence as decay of anterior teeth can cause embarrassment that would not be negated by the positive feeling of participating in the programme and taking care of one's own oral health. However, children who were bullied at baseline showed a greater improvement in severity in the intervention group than the control group. As children in the control group were also supplied with a toothbrush and toothpaste and were aware of their participation in the study, this could suggest that a greater awareness of oral health and hygiene at baseline is associated with a greater improvement in well-being outcomes. After the BDN programme, a moderate upwards trend of similar magnitude (∼5%) in oral hygiene in both the intervention and control groups was observed.
When comparing oral hygiene measured at T0 with later timepoints, the improvement observed in the intervention group was limited to children presenting moderate to poor oral hygiene, and the improvement was more pronounced than in the control group in these populations. In addition, covariate analysis revealed no increased likelihood of changing category to “good” at any timepoint of the programme, which is in line with the results of other studies.42,43 This may be because the control group became self-motivated to improve their oral hygiene habits due to their participation in the study and the frequent oral examinations, known as the Hawthorne effect.43
Only 10% of children presented no decayed, missing, or filled teeth at baseline, with a high DMFT index. This remained unchanged after 24 weeks, while overall decayed, missing, or filled teeth worsened in approximately 22% of children. However, covariate analysis adjusting for baseline DMFT Index, gender, school grade, baseline opinion on importance of everyday brushing, use of fluoride toothpaste, and feeling of pain in the mouth while eating revealed a 45% increase in the likelihood of no further worsening of DMFT score. Other school-based oral health studies have found no changes in the DMFT scores after 6 months43, 44, 45 and some found DMFT scores to be higher in control group but not significantly different.42,43,46
Although it is not possible to statistically compare both countries' results due to the sample differences, it is interesting to analyse the common outcomes and the differences found. The improvement in well-being of children from both countries is an important outcome because it is related to less absenteeism at school, better learning and better productivity.47 The children in Nigeria and Indonesia showed some important differences at baseline that can be explained by differing habits and knowledge. The high percentage of Indonesian children with good oral hygiene habits and dental caries contrasts with Nigerian children at baseline.
Indonesian children seem to be affected by other factors that lead to high dental caries prevalence and severity. Oral hygiene improvement could not be seen within the intervention group in Indonesia, mostly due to the high percentage of children with good oral hygiene at baseline, making an improvement difficult. Dietary habits may play an important role with regard to caries experience because good oral hygiene is not enough to offset other cariogenic factors.48
However, the BDN programme proved effective in preventing additional caries over 24 weeks. This finding makes a strong case for implementing the programme to achieve sustained oral hygiene habits, while trying to reduce aetiologic factors for dental caries.
On the other hand, Nigerian children showed a very low caries prevalence, and it was expected that good oral hygiene habits would help maintain these levels. Given the significant improvement in oral hygiene at 24 weeks compared to baseline in Nigeria, the BDN programme can play an important role in caries prevention.
Certain results from the present study are consistent with previous research. Significant reduction in intervention children's plaque levels versus control groups were reported in a 2017 meta-analysis49 and in all four studies included in the 2013 Cochrane Review.15 Short follow-up periods highlight the need for further research into the sustainability of programme outcomes. Previous research results related to caries incidence show mixed results, with some studies reporting reduced DMFT or decayed, missing, or filled surfaces (DMFS) scores following school-based education programmes,20,50 while others have found no effect.44,51, 52, 53 Short evaluation periods in certain studies may hinder the detection of programme effects on caries incidence.49,52,53
This study has some limitations. Many exclusions in the Nigeria study resulted in a small study population, reducing the interpretability of the results. In addition, the socioeconomic status of the children was not comparable. Parent's educational level was used as a proxy measure for children's socioeconomic status; however, limited responses to the questionnaire administered to parents meant that this variable was not included in the data analysis. The data obtained did show socioeconomic differences between the two countries, with children in Nigeria overall having a higher socioeconomic status than those in Indonesia. As mentioned, schools were paired according to the socioeconomic status of the area in which they were located and divided between intervention and control groups.
Another limitation is that the effect of the interventions beyond 24 weeks on oral hygiene and caries is unknown. It would therefore be of interest to extend the observation period to determine whether, and when, the programme should be repeated.
Conclusion
The BDN programme proved successful in improving the well-being of the children taking part in both Indonesia and Nigeria. In Indonesia, the BDN programme increased the likelihood of no further worsening in decayed, missing, or filled teeth by 45%. In Nigeria, the programme led to a 71% higher probability of having confidence in their smile and doubled the proportion of children presenting with good oral hygiene.
Acknowledgments
Acknowledgements
The authors would like to thank the following study leads: Dr Tri Erri Astoeti, National Liaison Officer, Indonesian Dental Association, and Dr Olabode Adeyemi Ijarogbe, President, Nigerian Dental Association. They also thank Dr Sofia Correia, University of Porto, for her contribution to the data analysis. Medical writing assistance was provided by Alice Kirby and Lee Kempster at MediTech Media, under the authors’ conceptual direction and based on feedback from the authors.
Funding
This article is published as part of a supplement sponsored by Unilever. Medical writing assistance, in the form of preparation and revision of the manuscript, as well as support of the conduct of the research, was supported financially by Unilever.
Conflict of interest
P.M., C.F., and S.T. report no conflicts of interest regarding the work under consideration for publication, no relevant financial activities outside the submitted work, and no patents or copyrights. S.M. is an employee of Unilever Oral Care.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.identj.2021.01.018.
Appendix. Supplementary materials
References
- 1.Tai B, Du M, Peng B, Fan M, Bian Z. Experiences from a school-based oral health promotion programme in Wuhan City, PR China. Int J Paediatr Dent. 2001;11(4):286–291. doi: 10.1046/j.1365-263x.2001.00281.x. [DOI] [PubMed] [Google Scholar]
- 2.Adair PM, Burnside G, Pine CM. Analysis of health behaviour change interventions for preventing dental caries delivered in primary schools. Caries Res. 2013;47(Suppl 1):2–12. doi: 10.1159/000351829. [DOI] [PubMed] [Google Scholar]
- 3.American Academy on Pediatric Dentistry; American Academy of Pediatrics Policy on early childhood caries (ECC): classifications, consequences, and preventive strategies. Pediatr Dent. 2008;30(7 Suppl):40–43. [PubMed] [Google Scholar]
- 4.Cruz RKS, Freitas YNL, Mendes TCO, et al. Spatial inequality of dental caries in the Brazilian territory. Braz Oral Res. 2020;33:e122. doi: 10.1590/1807-3107bor-2019.vol33.0122. [DOI] [PubMed] [Google Scholar]
- 5.Chapman A, Copestake SJ, Duncan K. An oral health education programme based on the National Curriculum. Int J Paediatr Dent. 2006;16(1):40–44. doi: 10.1111/j.1365-263X.2006.00677.x. [DOI] [PubMed] [Google Scholar]
- 6.Mouradian WE, Wehr E, Crall JJ. Disparities in children's oral health and access to dental care. JAMA. 2000;284(20):2625–2631. doi: 10.1001/jama.284.20.2625. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention (CDC). Children's oral health. Available from: https://www.cdc.gov/oralhealth/basics/childrens-oral-health/index.html. Accessed 3 December 2020.
- 8.Drummond BK, Meldrum AM, Boyd D. Influence of dental care on children's oral health and wellbeing. Br Dent J. 2013;214(11):E27. doi: 10.1038/sj.bdj.2013.533. [DOI] [PubMed] [Google Scholar]
- 9.Jurgensen N, Petersen PE. Promoting oral health of children through schools–results from a WHO global survey 2012. Community Dent Health. 2013;30(4):204–218. [PubMed] [Google Scholar]
- 10.World Health Organization. World Conference on Social Determinants of Health. Available from: https://www.who.int/sdhconference/en/. Accessed 3 December 2020.
- 11.FDI World Dental Federation. Brush Day & Night 12 years of improving oral health worldwide. Available from: https://www.fdiworlddental.org/sites/default/files/media/resources/fdi-bdn_12_years_oral_health.pdf. Accessed 3 December 2020.
- 12.Bukhari OM. Dental caries experience and oral health related quality of life in working adults. Saudi Dent J. 2020;32(8):382–389. doi: 10.1016/j.sdentj.2019.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramos-Jorge J, Alencar BM, Pordeus IA, et al. Impact of dental caries on quality of life among preschool children: emphasis on the type of tooth and stages of progression. Eur J Oral Sci. 2015;123(2):88–95. doi: 10.1111/eos.12166. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization. Sugars and dental caries factsheet. Available from: https://www.who.int/news-room/fact-sheets/detail/sugars-and-dental-caries. Accessed 3 December 2020.
- 15.Cooper AM, O'Malley LA, Elison SN, et al. Primary school-based behavioural interventions for preventing caries. Cochrane Database Syst Rev. 2013;(5) doi: 10.1002/14651858.CD009378.pub2. [DOI] [PubMed] [Google Scholar]
- 16.FDI World Dental Federation. Oral health and quality of life. Available from: https://www.fdiworlddental.org/resources/policy-statements-and-resolutions/oral-health-and-quality-of-life. Accessed 3 December 2020.
- 17.Kwan SY, Petersen PE, Pine CM, Borutta A. Health-promoting schools: an opportunity for oral health promotion. Bull World Health Organ. 2005;83(9):677–685. [PMC free article] [PubMed] [Google Scholar]
- 18.Walsh T, Worthington HV, Glenny AM, Appelbe P, Marinho VC, Shi X. Fluoride toothpastes of different concentrations for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2010;(1) doi: 10.1002/14651858.CD007868.pub2. [DOI] [PubMed] [Google Scholar]
- 19.FDI World Dental Federation Promoting oral health through fluoride toothpaste. Int Dent J. 2019;69(1):17–18. doi: 10.1111/idj.12469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ekstrand KR, Kuzmina IN, Kuzmina E, Christiansen ME. Two and a half-year outcome of caries-preventive programs offered to groups of children in the Solntsevsky district of Moscow. Caries Res. 2000;34(1):8–19. doi: 10.1159/000016564. [DOI] [PubMed] [Google Scholar]
- 21.Curnow M, Burnside G, Pine C, editors. Sustained dental health benefits for adults from childhood toothbrushing intervention. Abstract 0549. IADR; San Francisco, CA: 2017. [Google Scholar]
- 22.Patil SP, Patil PB, Kashetty MV. Effectiveness of different tooth brushing techniques on the removal of dental plaque in 6-8 year old children of Gulbarga. J Int Soc Prev Community Dent. 2014;4(2):113–116. doi: 10.4103/2231-0762.138305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nassar PO, Bombardelli CG, Walker CS, et al. Periodontal evaluation of different toothbrushing techniques in patients with fixed orthodontic appliances. Dental Press J Orthod. 2013;18(1):76–80. doi: 10.1590/s2176-94512013000100017. [DOI] [PubMed] [Google Scholar]
- 24.Raviteja N, Prasad MG, Radhakrishna A, et al. Evaluation of mechanical plaque removal effectiveness of toothbrush and its modifications in intellectually disabled children. J Biomed Pharm Res. 2017;6 [Google Scholar]
- 25.Ceyhan D, Akdik C, Kirzioglu Z. An educational programme designed for the evaluation of effectiveness of two tooth brushing techniques in preschool children. Eur J Paediatr Dent. 2018;19(3):181–186. doi: 10.23804/ejpd.2018.19.03.3. [DOI] [PubMed] [Google Scholar]
- 26.Biesbrock AR, Walters PA, Bartizek RD. Short-term impact of a national dental education program on children's oral health and knowledge. J Clin Dent. 2004;15(4):93–97. [PubMed] [Google Scholar]
- 27.Worthington HV, Hill KB, Mooney J, Hamilton FA, Blinkhorn AS. A cluster randomized controlled trial of a dental health education program for 10-year-old children. J Public Health Dent. 2001;61(1):22–27. doi: 10.1111/j.1752-7325.2001.tb03351.x. [DOI] [PubMed] [Google Scholar]
- 28.Reinhardt CH, Lopker N, Noack MJ, Klein K, Rosen E. Peer tutoring pilot program for the improvement of oral health behavior in underprivileged and immigrant children. Pediatr Dent. 2009;31(7):481–485. [PubMed] [Google Scholar]
- 29.de Farias IA, de Araujo Souza GC, Ferreira MA. A health education program for Brazilian public schoolchildren: the effects on dental health practice and oral health awareness. J Public Health Dent. 2009;69(4):225–230. doi: 10.1111/j.1752-7325.2009.00127.x. [DOI] [PubMed] [Google Scholar]
- 30.Melo P, Malone S, Rao A, Fine C. A 21-day school-based toothbrushing intervention in children aged 6 to 9 years in Indonesia and Nigeria: protocol for a two-arm superiority randomized controlled trial. JMIR Res Protoc. 2020;9(2):e14156. doi: 10.2196/14156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Melo P, Fine C, Malone S, Frencken JE, Horn V. The effectiveness of the Brush Day and Night programme in improving children's toothbrushing knowledge and behaviour. Int Dent J. 2018;68(Suppl 1):7–16. doi: 10.1111/idj.12410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Melo P, Fine C, Malone S, Taylor S. Impact of the Brush Day & Night programme on oral health knowledge and behaviour in children. Int Dent J71 (Suppl 1), 2021. [DOI] [PMC free article] [PubMed]
- 33.WHO Global School Health Initiative & World Health Organization . World Health Organization; Geneva: 1996. Health Education and Promotion U. The status of school health. [Google Scholar]
- 34.McGrath C, Broder H, Wilson-Genderson M. Assessing the impact of oral health on the life quality of children: implications for research and practice. Community Dent Oral Epidemiol. 2004;32(2):81–85. doi: 10.1111/j.1600-0528.2004.00149.x. [DOI] [PubMed] [Google Scholar]
- 35.Carvalho JC, Rebelo MAB, Vettore MV. The relationship between oral health education and quality of life in adolescents. Int J Paediatr Dent. 2013;23(4):286–296. doi: 10.1111/ipd.12006. [DOI] [PubMed] [Google Scholar]
- 36.Joybell C, Krishnan R, Kumar V S. Comparison of two brushing methods- fone's vs modified bass method in visually impaired children using the audio tactile performance (ATP) technique. J Clin Diagn Res. 2015;9(3):ZC19–ZC22. doi: 10.7860/JCDR/2015/11307.5651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vangipuram S, Jha A, Raju R, Bashyam M. Effectiveness of peer group and conventional method (Dentist) of oral health education programme among 12-15 year old school children - a randomized controlled trial. J Clin Diagn Res. 2016;10(5):Zc125–Zc129. doi: 10.7860/JCDR/2016/17725.7844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reddy M, Lakshmi S, Kulkarni S, Doshi D, Reddy B, Shaheen S. Impact of oral health education on plaque scores with and without periodic reinforcement among 12-year-old school children. J Indian Assoc Public Health Dent. 2016;14(2):116–120. [Google Scholar]
- 39.Gauba A, Bal IS, Jain A, Mittal HC. School based oral health promotional intervention: effect on knowledge, practices and clinical oral health related parameters. Contemp Clin Dent. 2013;4(4):493–499. doi: 10.4103/0976-237X.123056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Melo P, Marques S, Silva OM. Portuguese self-reported oral-hygiene habits and oral status. Int Dent J. 2017;67(3):139–147. doi: 10.1111/idj.12273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ismail AI, Tellez M, Pitts NB, et al. Caries management pathways preserve dental tissues and promote oral health. Community Dent Oral Epidemiol. 2013;41(1):e12–e40. doi: 10.1111/cdoe.12024. [DOI] [PubMed] [Google Scholar]
- 42.Frencken JE, Borsum-Andersson K, Makoni F, Moyana F, Mwashaenyi S, Mulder J. Effectiveness of an oral health education programme in primary schools in Zimbabwe after 3.5 years. Community Dent Oral Epidemiol. 2001;29(4):253–259. doi: 10.1034/j.1600-0528.2001.290403.x. [DOI] [PubMed] [Google Scholar]
- 43.van Palenstein Helderman WH, Munck L, Mushendwa S, van't Hof MA, Mrema FG. Effect evaluation of an oral health education programme in primary schools in Tanzania. Community Dent Oral Epidemiol. 1997;25(4):296–300. doi: 10.1111/j.1600-0528.1997.tb00943.x. [DOI] [PubMed] [Google Scholar]
- 44.Damle SG, Patil A, Jain S, Damle D, Chopal N. Effectiveness of supervised toothbrushing and oral health education in improving oral hygiene status and practices of urban and rural school children: a comparative study. J Int Soc Prev Community Dent. 2014;4(3):175–181. doi: 10.4103/2231-0762.142021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ashley FP, Sainsbury RH. The effect of a school-based plaque control programme on caries and gingivitis. A 3-year study in 11 to 14-year-old girls. Br Dent J. 1981;150(2):41–45. doi: 10.1038/sj.bdj.4804533. [DOI] [PubMed] [Google Scholar]
- 46.Sharma G, Vashishth S. Effectiveness of dental health education program in improving the oral health status of 6-13 year old government residential school children of Mysore district. Global J Res Anal. 2017;6(7) [Google Scholar]
- 47.Peres MA, Macpherson LMD, Weyant RJ, et al. Oral diseases: a global public health challenge. Lancet. 2019;394(10194):249–260. doi: 10.1016/S0140-6736(19)31146-8. [DOI] [PubMed] [Google Scholar]
- 48.Maharani DA, Adiatman M, Rahardjo A, Burnside G, Pine C. An assessment of the impacts of child oral health in Indonesia and associations with self-esteem, school performance and perceived employability. BMC Oral Health. 2017;17(1):65. doi: 10.1186/s12903-017-0358-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stein C, Santos NML, Hilgert JB, Hugo FN. Effectiveness of oral health education on oral hygiene and dental caries in schoolchildren: systematic review and meta-analysis. Community Dent Oral Epidemiol. 2018;46(1):30–37. doi: 10.1111/cdoe.12325. [DOI] [PubMed] [Google Scholar]
- 50.Al-Jundi S, Hammad M, Alwaeli H. The efficacy of a school-based caries preventive program: a 4-year study. Int J Dent Hyg. 2006;4(1):30–34. doi: 10.1111/j.1601-5037.2006.00156.x. [DOI] [PubMed] [Google Scholar]
- 51.Chandrashekar B, Suma S, Sukhabogi J, Manjunath B, Kallury A. Oral health promotion among rural school children through teachers: an interventional study. Indian J Public Health. 2014;58(4):235–240. doi: 10.4103/0019-557X.146278. [DOI] [PubMed] [Google Scholar]
- 52.Zanin L, Meneghim M, Assaf A, Cortellazzi K, Pereira A. Evaluation of an educational program for children with high risk of caries. J Clin Pediatr Dent. 2008;31(4):246–250. doi: 10.17796/jcpd.31.4.e521842t26200h27. [DOI] [PubMed] [Google Scholar]
- 53.Jaime RA, Carvalho TS, Bonini GC, Imparato JCP, Mendes FM. Oral health education program on dental caries incidence for school children. J Clin Pediatr Dent. 2015;39(3):277–283. doi: 10.17796/1053-4628-39.3.277. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.