Abstract
Background
Assessing perceived needs for dental treatment is important in understanding and predicting people's health behaviours. The purpose of this study is to examine older men's perceptions regarding dental treatment needs, and to investigate the disparity between perceived needs and the actual oral health of a population of community-dwelling older Australians.
Methods
Using cross-sectional data from the 4th wave of the Concord Health and Ageing in Men Project, logistic regression analysis of perceived needs for dental treatment was conducted for 596 men aged 78 and over, with functional tooth units (FTUs), number of decayed tooth surfaces, and periodontitis as independent variables.
Results
Thirty-six percent (n = 216) of the participants believed they required some form of dental treatment. The remaining participants did not perceive a need for treatment, yet 65.3% objectively required prosthodontic or restorative care. The regression model showed men with lower FTUs were significantly more likely to report a perceived need for dental treatment than those with 12 FTUs [0–6 FTUs: adjusted odds ratio (OR) 2.58, 95% CI 1.28–5.20; 7–11 FTUs: adjusted OR 2.43, 95% CI 1.16–5.10]. However, neither the number of decayed tooth surfaces nor the existence of periodontitis was associated with perceived dental treatment needs.
Conclusions
Most older men viewed their oral health positively, and the majority of those with objectively assessed needs, did not perceive themselves as requiring dental treatment. Loss of FTUs appears to alert participants to seek treatment, but not the presence of dental caries or periodontitis.
Key words: Perceived dental treatment needs, Functional tooth unit, Dental caries, Periodontitis, Community-dwelling older men, Australia
Introduction
Older people are now retaining more natural teeth than previous generations.1 Although this is an ideal trend, they may be more vulnerable or susceptible to oral diseases, such as dental caries or periodontitis.2,3 Routine dental visits have been associated with better oral health with lower cases of active dental caries and tooth loss.4 As exposure to the risk factors of periodontitis and dental caries changes with age, it is prudent to promote regular dental visits as a continuing preventive measure. It has been established in the past that personal capacity for preventive care decreases in older people, thus increasing the progression of existing dental diseases.2 The National Survey of Adult Oral Health (NSAOH) 2004–2006 provides the most recent published analysis of oral health status of adult and community-dwelling older people in Australia.5 Gender differences were observed over a broad range of generations. Prevalence of edentulism was higher among older women than older men, but older men had higher rates of untreated tooth decay, lower rates of filled teeth, and a higher prevalence of periodontitis than older women.
Adding to the above factors, older people also have been characterised as utilising dental services less frequently compared to younger people.4 The lack of perceived need for dental treatment is one of the barriers deterring their visits to a dental practitioner.6 Numerous studies have reported on this issue focusing on older people.7, 8, 9 Socioeconomic factors, such as education and income, significantly influence the utilisation of dental services, especially among older people, yet the primary reason for seeking dental health services is due to the perception that they require dental treatment, or a desire for reassurance that they do not require further dental treatment.10
The concept of social needs is defined by Bradshaw.11 His taxonomy of need outlines different types of need, which is often referenced by administrators and researchers.11 It includes ‘felt need’, ‘normative need’, and ‘expressed need’. ‘Felt need’, which is the equivalent to ‘perceived need’, is the typical need where an individual would emotionally sense a requirement. This ‘perceived need’ is crucial, as it is the main determinant for people in proactively seeking dental service. However, their limited awareness and knowledge of dental health may factor into an improper decision with respect to their ‘perceived dental needs’. ‘Normative need’, which professionals define as an ‘objective need’ in any given situation, is not absolute. ‘Expressed need’, also known as ‘demanded need’, is defined as a perceived need turned into action. In the area of preventive medicine, ‘normative need’ is sometimes postulated by professionals whereas lay people may not recognise any perceived need.
Several studies have reported on the relationship between perceived dental treatment needs and the objective oral health condition of either younger adults only or across generations.12, 13, 14, 15, 16 There are few studies solely focused on older populations.17, 18, 19 Some, such as Åstrøm et al., have reported that perception of dental treatment needs can be a major determinant for individuals in seeking dental treatment.17 There has been no past study which has assessed the perceived dental treatment needs of older people by taking general health comorbidities into consideration. In this study, we focused on perceived needs, and examined their association with objective oral health status determined by professionals using Concord Health and Ageing in Men Project (CHAMP) data.
Australia is a nation with considerable ethnic diversity, where one third of the Australian population are born in other countries.20 Thus, socioeconomic factors and people's ethnicity are important determinants of their health status.21 The CHAMP study was initiated to estimate the range of general health conditions among the older male population representing Australia. It is mainly concerned with causes and consequences of major geriatric syndromes including falls, bone strength and fractures, cognitive impairment and dementia, poor mobility and functional dependence. Oral health assessment was included from the 8-year follow-up, from which the data of this study were obtained.22 The purpose of this study is to examine how older men perceived their dental treatment needs, and investigate the gap between perceived treatment needs and actual state of oral health [decayed tooth, functional tooth units (FTUs), and periodontitis] among CHAMP participants, taking into account comorbidities, oral health-related behaviour, and socioeconomic factors.
Materials and methods
Study participants
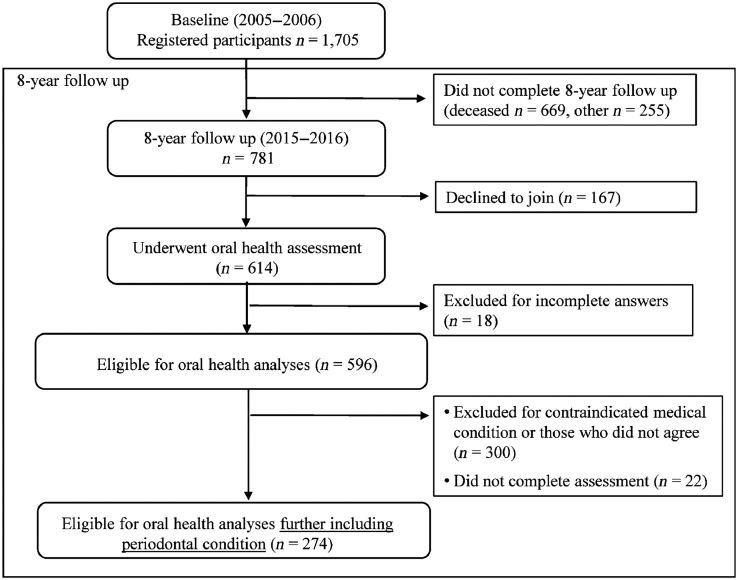
Cross-sectional data were collected as part of the fourth wave (between 2015 and 2016) of CHAMP, which is a longitudinal epidemiologic study of older men in New South Wales (NSW), Australia. Participants were males aged 78 years and over at the time of the 8-year follow-up study, living in a defined geographical region (Local Government Areas of Burwood, Canada Bay and Strathfield).22 The three defined regions in Sydney around Concord Hospital were selected for geographical reasons. The sampling frame of the NSW Electoral Roll was utilised, where registration is compulsory for all citizens of Australia. All eligible men in the study area were invited to join the study excluding men living in residential aged care facilities in the original cohort conducted in 2005–2006. In the 8-year follow-up study, all eligible men were invited again, and 781 participants from the original cohort of 1,705 men were available for re-examination for their general health (Figure 1). All participants were given a verbal explanation of the study purpose and methods involved, as well as having signed consent forms.
Fig. 1.
Flowchart of the 8-year follow-up population, remaining participants and reasons for loss.
Oral health assessment
Functional tooth units and decayed tooth surfaces
Standard intra-oral assessments were conducted by two calibrated oral health therapists using protocols consistent with Australian dental data collection standards.21 Calibration procedure and examiners’ reliability were reported previously by Wight et al.21 Tooth loss, replacement teeth and number of teeth present including third molars were recorded for each participant. Functional tooth units (FTUs) were calculated as described by Kayser and Ueno et al.23,24 The number of FTUs was defined as pairs of opposing posterior natural and artificial teeth on implant-supported, fixed, and removable prosthesis. Two opposing premolars were defined as one FTU and two opposing molars were defined as two FTUs; a full set of complete dentition consists of 12 FTUs (third molars were excluded). The maximum number of FTUs is thus 12 units. FTU scores were later clustered into three groups for analyses: 0–6 FTUs, 7–11 FTUs, and 12 FTUs.23 FTUs measure the contact of opposing posterior teeth and are therefore used as an estimate of masticatory efficiency.23,24 The number of natural teeth was categorised as 0, 1–9, 10–19, and 20 or more.23
Coronal and root surface dental decay were assessed and recorded for each tooth surface present. For coronal caries of molars and premolars, each of the five coronal surfaces (occlusal, mesial, buccal, distal, and lingual) was assessed. For coronal caries of incisors and canines, each of the five coronal surfaces (incisal, mesial, buccal, distal, and lingual) was assessed. As for root caries experience, the four root surfaces (mesial, buccal, distal, and lingual) were assessed. Presence of active coronal and root surface caries was later combined into a single decayed tooth surface (DS) measurement. Details of the intra-oral assessment have been described previously.21
A variable of normative treatment needs for prosthodontics or restoration was created based on numbers of FTUs and decayed tooth surfaces. People with ‘10–12 FTUs’ and ‘no decayed tooth surface’ were categorised as without normative treatment needs.23
Periodontal disease
Periodontal disease was measured only in those men without any previous medical history, including rheumatic fever, renal dialysis, haemophilia, having pacemaker or automatic defibrillator, artificial material in their heart, transplanted organ, and bacterial endocarditis.21 Periodontal disease was assessed on each tooth at three sites (mesio-buccal, buccal and distobuccal) and categorised using Centers for Disease Control (CDC) and Prevention/American Academy of Periodontology (AAP) case definitions for severe, moderate, mild or no-disease.3,25,26 Severe periodontal disease was defined as ≥2 interproximal sites for Clinical Attachment Loss (CAL) ≥6 mm, and as ≥1 interproximal site for periodontal Pocket Depth (PD) ≥4 mm.27
A variable of normative treatment needs for prosthodontics, restoration or periodontitis was created. People with ‘10–12 FTUs’, ‘no decayed tooth surface’ and ‘no evidence of periodontitis’ were categorised as without normative treatment needs.
Self-completed questionnaire
Data on age, income, country of birth, smoking history, and education attainment were collected through self-completed questionnaires. Country of birth was categorised into three groups: Australia; Greece or Italy; and other countries. Italy and Greece were categorised in the same group because they were of similar Mediterranean backgrounds, but individually comprised small groups for analysis. An income-based assessment was used to characterise income levels where the lowest income category was categorised as ‘all income from the aged pension only’; the middle category was income received from the ‘age pension plus other income’; and the highest category was ‘income from any possible combinations of superannuation, private income, own business/farm/partnership, wage or salary income, repatriation or veteran's pension, or other income’, but ineligible for any age pension due to high income. Post-school qualification was categorised as having post-secondary school qualification or not. Smoking status was classified into two categories, ‘never smoked’ or ‘current/previous smoker’.
Comorbidities were assessed using a standardised questionnaire, in which participants indicated whether they had been told by a physician if they had one or more of the following health conditions: diabetes, thyroid dysfunction, osteoporosis, Paget's disease, stroke, Parkinson's disease, kidney stones, dementia, depression, epilepsy, hypertension, heart attack, myocardial infarction, angina, congestive heart failure, intermittent claudication, chronic obstructive lung disease, liver disease, chronic kidney disease, cancer, osteoarthritis or gout.22 The number of comorbidities of each participant was categorised into either ‘0–3’ or ‘≥4’ comorbidities.
Oral health behaviour, perceived needs for dental treatment, and symptom
Information about dental health behaviour was obtained through a self-completed questionnaire, and then dichotomised as: (i) frequency of visiting dental professionals (‘once a year or more’ vs. ‘less than once a year’) and (ii) self-rated oral health (excellent/very good/good vs. fair/poor). The usual reasons for dental visits were categorised into ‘check-up’, ‘dental problem’, or ‘cannot recall’. Perceived dental treatment needs were assessed by inquiring ‘Do you think you need dental treatment NOW?’ to which participants were asked to reply ‘Yes’ or ‘No’.19 Participants were also inquired about dento-facial pain in the past month before the survey. Their last visit to a dental professional was inquired and they were asked to reply as ‘Less than 12 months ago’, ‘1 year to less than 2 years ago’, ‘2–5 years ago’, ‘5–10 years ago’, and ’10 years ago or more’. The responses were dichotomised as ‘less than 12 months ago’ or ‘1 year ago or more’.
Ethics statement
The study was performed in accordance with the World Medical Association Declaration of Helsinki, and the study protocol and consent procedures were approved by the Sydney Local Health District Human Ethics Research Committee (Approval No. HERC/14/CRGH/17).
Statistical analysis
Chi-squared tests were utilised to examine the bivariate associations between perceived dental treatment needs and categorical variables such as income, country of birth, comorbidities, smoking history, post-school qualification, utilisation of dental services, and oral health conditions. Average age by perceived dental treatment needs was analysed using Student's t-test. Chi-squared tests were also performed to examine the relationship between treatment need with the self-rated oral health, demographic, and clinical categorical variables. Logistic regression analysis by forced-entry methods was consummated with FTUs, decayed tooth surfaces, and periodontitis as independent variables, whereas perceived dental treatment needs was utilised as a dependent variable. Unadjusted and adjusted odds ratios (OR) and their 95% confidence intervals (CI) were calculated. In the adjusted analyses, country of birth, age (as a continuous variable), post-school qualification, income, smoking, the number of comorbidities, frequency of visiting dental professionals, edentulism, and dento-facial pain were included in each model simultaneously. Calculating variance inflation factors in each model allowed the detection of any presence of multi-collinearity.28 A two-sided P-value < 0.05 was used as a level of statistical significance. Statistical analyses were performed using Statistical Package for Social Sciences (SPSS) for Windows, version 11.5 (SPSS, Inc., Chicago, IL, USA). The reporting of this study conforms to the STROBE statement.29
Results
There were 781 participants who submitted the self-completed questionnaire, and 614 men (524 dentate and 90 edentate) who completed the oral health assessment (Figure 1). Matched data for comparison of perceived dental and objective oral needs were available for only 596 participants. Their average age was 83.8 ± 4.1 years and 307 (51.5%) were born in Australia, 144 (24.2%) were born in Greece or Italy, and 145 (24.3%) were born in other countries. The average number of natural teeth present was 15.6 ± 9.4. Two hundred and eighty-nine (56.3%) participants were available for analyses involving periodontal disease.
Of the 596 participants, 216 (36.2%) believed they required dental treatment at the time of answering the questionnaire. Table 1 summarises the distribution of participants by perceived dental treatment needs. Chi-squared analysis showed that perceived dental treatment needs were associated with country of birth (P = 0.04) as well as income (P = 0.01). No association was observed between perceived dental treatment needs and age, comorbidities, smoking behaviour, or post-school qualification.
Table 1.
Distribution of participants by perceived dental treatment needs
| ALL (n = 596) | Perceived dental treatment needs |
|||
|---|---|---|---|---|
| Yes (n = 216) n (%) | No need (n = 380) n (%) | P-value⁎ | ||
| Age (mean ± SD) | 83.8 ± 4.1 | 83.9 ± 4.1 | 83.8 ± 4.1 | 0.91 |
| Country of birth | ||||
| Australia | 307 (51.5) | 97 (44.9) | 210 (55.3) | 0.04 |
| Greece/Italy | 144 (24.2) | 57 (26.4) | 87 (22.9) | |
| Others | 145 (24.3) | 62 (28.7) | 83 (21.8) | |
| Income† | ||||
| Low | 240 (40.3) | 104 (48.1) | 136 (35.8) | 0.01 |
| Middle | 135 (22.7) | 39 (18.1) | 96 (25.3) | |
| High | 221 (37.1) | 73 (33.8) | 148 (38.9) | |
| Comorbidities (4 or more) | 176 (29.5) | 66 (30.6) | 110 (28.9) | 0.71 |
| Ex/current smoker | 358 (60.1) | 130 (60.2) | 228 (60.0) | 0.97 |
| Having post-school qualification | 364 (61.1) | 130 (60.2) | 234 (61.6) | 0.79 |
The data were analysed for statistical significance using chi-squared test except for age. Age was analysed by Student's t-test.
The lowest income category was ‘all income from the aged pension only’; the middle was income received from the ‘age pension plus other income’; and the highest category was ‘income from any possible combinations of superannuation, private income, own business/farm/partnership, wage or salary income, repatriation or veteran's pension, or other income’.
Table 2 summarises the clinically observed oral health condition of participants by perceived dental treatment needs. Table 2a shows analysis for the total sample assessed from dental examination (n = 596), and Table 2b shows the sub-sample of participants (n = 289) who had completed periodontal examination. Chi-squared tests showed that perceived dental treatment needs were associated with: (i) the number of natural teeth present (P = 0.01); (ii) FTUs (P = 0.02), (iii) decayed tooth surface (P = 0.02); (iv) dento-facial pain in past month (P = 0.01); (v) self-rated oral health (P < 0.01); (vi) usual reason for dental visits (P = 0.01); (vii) last visit to a dental professional (P = 0.01); and (viii) periodontitis (P < 0.01).
Table 2.
Oral health of participants by perceived dental treatment needs
| ALL (n = 596) | Perceived dental treatment needs |
|||
|---|---|---|---|---|
| Yes (n = 216) n (%) | No need (n = 380) n (%) | P-value | ||
| (a) Dental condition, symptom, and oral health behaviours (n = 596) Objective oral health condition | ||||
| Number of natural teeth present | ||||
| 0 | 83 (13.9) | 20 (9.3) | 63 (16.6) | 0.01 |
| 1–9 | 88 (14.8) | 29 (13.4) | 59 (15.5) | |
| 10–19 | 163 (27.3) | 75 (34.7) | 88 (23.2) | |
| ≥20 | 262 (44.0) | 92 (42.6) | 170 (44.7) | |
| Functional Tooth Units (FTUs) | ||||
| 0–6 | 227 (38.1) | 95 (44.0) | 132 (34.7) | 0.02 |
| 7–11 | 204 (34.2) | 75 (34.7) | 129 (33.9) | |
| 12 | 165 (27.7) | 46 (21.3) | 119 (31.3) | |
| Decayed tooth surface | ||||
| 0 | 440 (73.8) | 151 (69.9) | 289 (76.1) | 0.02 |
| 1–2 | 67 (11.2) | 21 (9.7) | 46 (12.1) | |
| ≥3 | 89 (14.9) | 44 (20.4) | 45 (11.8) | |
| Edentate | 83 (13.9) | 20 (9.3) | 63 (16.6) | 0.01 |
| Normative treatment need for prosthodontics or restoration* | 405 (68.0) | 157 (72.7) | 248 (65.3) | 0.07 |
| Symptom and oral health behaviours | ||||
| Experienced pain in maxillofacial area in the past month† | 50 (8.4) | 27 (12.5) | 23 (6.1) | 0.01 |
| Self-rated oral health (excellent/very good/good) | 423 (71.0) | 107 (49.5) | 316 (83.2) | <0.01 |
| Frequency of visiting dental professionals (once a year or more) | 349 (58.6) | 119 (55.1) | 230 (60.5) | 0.23 |
| Usual reason for dental visits | ||||
| Check-up | 324 (54.4) | 100 (46.3) | 224 (58.9) | 0.01 |
| Dental problem | 236 (39.6) | 104 (48.1) | 132 (34.7) | |
| Can't recall | 36 (6.0) | 12 (5.6) | 24 (6.3) | |
| Last visit to a dental professional (less than 12 months ago) | 317 (53.2) | 108 (50.0) | 209 (55.0) | 0.01 |
| ALL (n = 289) | Perceived dental treatment needs |
|||
| Yes (n = 111) | No need (n = 178) | P-value | ||
| (b) Periodontal assessment (n = 289) Periodontitis | ||||
| No | 40 (13.8) | 12 (10.8) | 28 (15.7) | <0.01 |
| Mild/moderate | 167 (57.8) | 55 (49.5) | 112 (62.9) | |
| Severe | 82 (28.4) | 44 (39.6) | 38 (21.3) | |
| Normative treatment need for prosthodontics, restoration, or periodontitis | 277 (95.8) | 110 (99.1) | 167 (93.8) | 0.03 |
(a) Includes 596 participants who completed self-completed questionnaire and oral health assessment for FTU and decayed teeth. (b) Includes 289 participants who further underwent oral health assessment for periodontal disease.
People with one or more decayed tooth surface or FTU < 10 were categorised as having normative need.
People were asked about pain or discomfort from their face, mouth, jaw, or teeth limited from doing activities.
‡ People with one or more decayed tooth surface, FTU < 10, or periodontitis were categorised as having normative need.
As for normative treatment needs for prosthodontics or restoration in Table 2a, there were 405 (68.0%) participants identified as requiring actual treatment by dental examinations. Among 216 people with perceived treatment needs, 157 (72.7%) people had normative needs. Similarly, among 380 people without perceived treatment needs, 248 (65.3%) people had normative treatment needs. As for normative treatment needs for prosthodontics, restoration or periodontitis in Table 2b, 277 (95.8%) people were identified as requiring actual treatment. There were 111 people with perceived treatment needs, and 110 (99.1%) had normative treatment needs for prosthodontics, restoration, or periodontitis. Similarly, 167 people did not perceive need, yet most of them (93.8%) had normative treatment needs.
Among the 50 men who had experienced dento-facial pain in the previous month, 14 had three or more decayed tooth surfaces, and two had 1 or 2 decayed tooth surfaces. Chi-squared test analysis showed that people who experienced pain had significantly higher numbesr of decayed tooth surfaces compared with those who did not (P < 0.01). However, severity of periodontitis did not have any association with pain.
Table 3 presents the findings from logistic regression analyses where perceived dental treatment needs was a dependent variable, and the two oral health-related variables (FTUs and decayed tooth surfaces) were entered as independent variables (model 1). Compared to participants with an FTU score of 12, those with 0–6 FTUs were significantly more likely to believe they needed dental treatment (unadjusted OR 1.82, CI 1.17–2.81; adjusted OR 1.73, CI 1.07–2.80). Existence of three or more decayed tooth surfaces was also associated with perceived dental treatment needs, but was attenuated and no longer statistically significant after adjustment for confounders (unadjusted OR 1.77, CI 1.11–2.81; adjusted OR 1.39, CI 0.85–2.28).
Table 3.
Odds ratios for having perceived treatment needs by logistic regression analyses (reference: no need)
| Variables | Model 1 (n = 596) |
Model 2 (n = 289) |
||
|---|---|---|---|---|
| Crude OR (95% CI) | Adjusted OR* (95% CI) | Crude OR (95% CI) | Adjusted OR* (95% CI) | |
| FTU (reference: 12) | ||||
| 7–11 | 1.46 (0.94–2.27) | 1.45 (0.89–2.36) | 2.01 (0.99–4.09) | 2.43 (1.16–5.10) |
| 0–6 | 1.82 (1.17–2.81) | 1.73 (1.07–2.80) | 2.15 (1.09–4.27) | 2.58 (1.28–5.20) |
| Decayed surface (reference: 0) | ||||
| 1–2 | 0.82 (0.47–1.41) | 0.70 (0.40–1.23) | 0.79 (0.38–1.64) | 0.72 (0.35–1.51) |
| ≥3 | 1.77 (1.11–2.81) | 1.39 (0.85–2.28) | 1.59 (0.81–3.09) | 1.47 (0.69–3.13) |
| Periodontitis (reference: no) | ||||
| Mild/moderate | 1.09 (0.51–2.37) | 1.45 (0.55–2.40) | ||
| Severe | 2.61 (1.16–5.87) | 2.22 (0.97–5.04) | ||
FTU, functional tooth unit.
Adjusted by country of birth, age, post-school qualification, income, smoking, the number of comorbidities, frequency of visiting dental professionals, edentate and any pains in maxillofacial area in the past month.
A logistic regression analysis was also conducted which included FTUs, decayed tooth surfaces, and periodontitis as independent variables. Results for the 289 men who had an assessment of periodontal disease are shown in model 2. FTUs were associated with perceived treatment needs. Men with 7–11 FTUs were significantly more likely to perceive need for dental treatment (adjusted OR 2.43; CI 1.16–5.10) compared to those with 12 FTUs after adjustment. Similarly, those with 0–6 FTUs were significantly more likely to perceive needs for dental treatment (crude OR 2.15, CI 1.09–4.27; adjusted OR 2.58, CI 1.28–5.20) compared to those with 12 FTUs. Existence of severe periodontitis was associated with perceived needs for dental treatment in unadjusted analyses but was attenuated and no longer statistically significant after adjustment for confounders (crude OR 2.61, CI 1.16–5.87; adjusted OR 2.22, CI 0.97–5.04), compared to those without periodontitis in model 2.
Discussion
This is the first study reporting the number of functional tooth units being associated with perceived dental treatment needs among older men by taking: (i) socioeconomic factors; (ii) comorbidities; (iii) frequency of visiting dental professionals; and (iv) dento-facial pain into consideration. This study examined the oral health status of community-dwelling older Australian men from diverse cultural backgrounds, and how they perceived their oral health and their dental treatment needs. The findings indicate that fewer functional teeth in CHAMP men were associated with their perception of needing some form of dental treatment; however, dental decay and severity of periodontitis were not associated with their perception of dental treatment needs when we look at major oral diseases: (i) tooth loss, (ii) caries, and (iii) periodontitis.
Detailed oral health status of CHAMP men and comparison with other populations was already reported by Wright et al.21 In short, the prevalence of edentulism was 13.9% among CHAMP men aged 78 years and over. This is relatively low in contrast with other reports from the UK, New Zealand, and the USA. Prevalence ratios of edentulism were 58% in data collected from the UK in 1998 among those aged 75 years and over, 52.2% in data from New Zealand collected in 2012 among people aged 65 years and over, and 31.3% in data from the USA collected in 2003–2004 among those aged 75 and over.21 Differences in the prevalence of edentulism could be attributed to various factors including gender difference, socioeconomic factors, health care system, and accessibility of dental services.21 As for the number of natural teeth present, 56% of CHAMP men had fewer than 20 natural teeth, which is identical to the 56% of Australian men in general aged 75 years and over who had fewer than 21 natural teeth.5
Most CHAMP men (71.0%) evaluated their own oral health favourably. Those who evaluated their oral health favourably were less likely to have perceived dental treatment needs. The prevalence of a positive perception of oral health is consistent with previous studies: the Florida Dental Care Study where nearly 80% of community-dwelling adults aged 45 and over evaluated their oral health favourably, and the Australian national survey where 82% of those aged 75 years or more (men and women) evaluated their oral health favourably.5,13 As for CHAMP men's behaviour for dental care, 349 men (58.6%) visited a dental professional once or more per year, and 317 men (53.2%) had visited dental professionals within the previous 12 months. As for their usual reason for dental visits, 324 men (54.4%) of those visited for check-ups, and 236 men (39.6%) were for dental problems. These patterns of behaviour are similar to the results of the Australian national survey, where 59% of people (men and women) aged 75 years and over visited for check-ups, and around 50% of the adult population visited a dental professional within the previous 12 months.30
Some studies have reported an incongruity between perceived treatment needs and the actual state of oral health among an adult or general population.12, 13, 14, 15, 16 Only a few studies, however, have previously reported the perceived dental treatment needs of older persons.17,19 Åstrøm et al.17 examined perceived dental treatment needs among Tanzanian older people. In their study, nearly half of the participants (47.8%) reported a perceived need for immediate dental treatment that differed from clinically assessed treatment needs. They concluded that people with a reduced number of occluding natural tooth units were more likely to have a perceived need for dental treatment. Reduced numbers of occluding natural tooth units can have a direct effect on chewing ability, and thus may be more easily recognised by an individual for its evident functional impact.31 These findings are consistent with our study. Locker et al.19 examined the perceived needs and oral health status among people aged 50 and over living in Ontario. They concluded that most participants underestimated their treatment needs, which is also consistent with other previous studies and our study.14,16,17
Several studies in the past have categorised different types of needs, with some focusing on specific types of treatment need.13, 14, 15,19 Instead of focusing on specific types, this study examined perceived treatment needs as a ’need for broad range of dental care’.32,33 Perception of dental treatment needs is reported to be generally lower than needs based on actual oral condition assessed by dental professionals. These data confirm the notion that older people tend to underestimate their dental treatment needs as compared to younger generations.34 As health literacy is generally lower in older people, it is important for elderly people to recognise the existence of any dental problem, rather than identifying a particular type of dental problem, due to fact that older people are more susceptible to oral diseases.2,3,35 This may nullify the requirement of detailing the types of oral treatment needed; hence, for our study purposes, we have defined perceived dental treatment need as the broader perceived need without detailing the specific treatments such as cleaning, fillings, extractions or prosthetic need.
As for the experience of pain, forty-four (8.6%) older men in our study had experienced dento-facial pain in the past month, which was associated with a perceived need for dental treatment in our bivariate analysis. We should note that the presence of dental caries itself was also associated with pain experience. However, the presence of active dental caries did not have any association with perceived dental treatment needs after taking confounding factors into account. Such factors included socioeconomic factors, oral health behaviours, and comorbidities.
Finally, sociodemographic characteristics of CHAMP participants were similar to the older population living in New South Wales in terms of income, education and country of birth, and thus they tend to represent the older male population of Australia's most populous metropolitan city, Sydney.21 Careful judgement is necessary when generalising these study results to older males of other state populations, and to those of the entire Australian population, especially considering ethnic diversity and socioeconomic factors. However, we believe that there would be no single epidemiological study which completely represents all of Australia except for national surveys. A few limitations to the present study merit consideration. First, a large number of participants were excluded from the periodontal assessment for specific medical reasons.21 This may have resulted in some selection bias. The smaller number of participants also reduced the power of statistical tests to demonstrate associations with periodontal disease. A second limitation was the loss of follow-up of participants, as this study excluded older men living in residential care. Many of them were likely edentate or with higher numbers of missing teeth. The study may also be subject to survival bias, where the health status of the surviving participants is better compared with those who had deceased or withdrew. Third, CHAMP participants are men and the results may not apply to older women.
This study is based on a follow-up of the original participants of the longitudinal CHAMP study. In year 8 of the study (Wave 4), the first oral health data were collected. The data of our present study therefore provide the first opportunity in Australia to facilitate the investigation of inter-relationships among various age-related health problems, comorbidities and health-related behaviours with the oral health perceptions and outcomes of community-dwelling older Australian men. The CHAMP study focused exclusively on older men, who generally have a shorter life expectancy than females. Males are characterised as exhibiting less healthy life styles and less frequent utilisation of health service compared with older females, yet most of the epidemiological studies previously published tended to focus on females.22,36
In conclusion, the findings of this study indicate that the number of functional tooth units, and not the pathology of periodontitis or decayed teeth, is related to an individual's perception of dental treatment needs. Most older men viewed their oral health positively, but the majority of men with dental problems did not consider themselves as requiring dental treatment – in contrast to their objectively assessed oral health status. A better understanding of this perception in dental treatment needs is important in promoting changes in oral health behaviour, thus leading to better planning and prioritising of oral health care services for an ageing population.
Acknowledgments
Acknowledgements
The authors would like to thank all CHAMP's staff and participants for their contributions. The CHAMP study is funded by National Health and Medical Research Council (301916), Ageing and Alzheimer's Institute, and the Australian Research Council Centre of Excellence in Population Ageing Research (CEPAR). We also acknowledge the Australian government for granting the Endeavour Research Fellowship to Dr Sachiko Takehara to work at the Centre for Oral Health Strategy, The University of Sydney. We would also like to acknowledge Steven Chu, Kate Milledge, Melissa Casey and Garry Law for their assistance, data collection and advice on the study. All authors have reviewed and approved the final version of manuscript. All authors have primary responsibility for final content.
Author contributions
C.W., L.W., V.N., V.H., F.B., D.C., M.S., D.H., and R.C. designed the oral health and the principal Wave 5 CHAMP study. S.T. and F.W. designed this project. S.T. analysed data with support from F.W. and R.C. S.T. drafted the manuscript in consultation with C.W., L.W. and R.C. All authors discussed the results and contributed to the final manuscript.
Conflict of interest
None of authors have any conflict of interest to declare.
References
- 1.Petersen PE. The World Oral Health Report 2003: continuous improvement of oral health in the 21st century–the approach of the WHO Global Oral Health Programme. Community Dent Oral Epidemiol. 2003;31(Suppl 1):3–23. doi: 10.1046/j..2003.com122.x. [DOI] [PubMed] [Google Scholar]
- 2.Tonetti MS, Bottenberg P, Conrads G, et al. Dental caries and periodontal diseases in the ageing population: call to action to protect and enhance oral health and well-being as an essential component of healthy ageing – consensus report of group 4 of the joint EFP/ORCA workshop on the boundaries between caries and periodontal diseases. J Clin Periodontol. 2017;44(Suppl 18):S135–S144. doi: 10.1111/jcpe.12681. [DOI] [PubMed] [Google Scholar]
- 3.Wright FAC, Law GG, Milledge KL, et al. Chewing function, general health and the dentition of older Australian men: the Concord Health and Ageing in Men Project. Community Dent Oral Epidemiol. 2019;47:134–141. doi: 10.1111/cdoe.12435. [DOI] [PubMed] [Google Scholar]
- 4.Thomson WM, Williams SM, Broadbent JM, et al. Long-term dental visiting patterns and adult oral health. J Dent Res. 2010;89:307–311. doi: 10.1177/0022034509356779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Australian Institute of Health and Welfare . Australian Institute of Health and Welfare; Canberra, ACT: 2008. The national survey of adult oral health 2004-06. Dental statistics and research series; p. 39. [Google Scholar]
- 6.Borreani E, Wright D, Scambler S, et al. Minimising barriers to dental care in older people. BMC Oral Health. 2008;8:7. doi: 10.1186/1472-6831-8-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kiyak HA. An explanatory model of older persons’ use of dental services. Implications for health policy. Med Care. 1987;25:936–952. doi: 10.1097/00005650-198710000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Abrams RA, Ayers CS, Lloyd PM. Attitudes of older versus younger adults toward dentistry and dentists. Spec Care Dentist. 1992;12:67–70. doi: 10.1111/j.1754-4505.1992.tb00413.x. [DOI] [PubMed] [Google Scholar]
- 9.Gilbert GH, Duncan RP, Heft MW, et al. Dental health attitudesamong dentate black and white adults. Med Care. 1997;35:255–271. doi: 10.1097/00005650-199703000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Kiyak HA, Reichmuth M. Barriers to and enablers of older adults’ use of dental services. J Dent Educ. 2005;69:975–986. [PubMed] [Google Scholar]
- 11.Bradshaw J. In: Problems and progress in medical care: essays on current research. McLachlan G, editor. Oxford University Press; London: 1972. A taxonomy of social need; pp. 71–82. editor. [Google Scholar]
- 12.Robinson PG, Nadanovsky P, Sheiham A. Can questionnaires replace clinical surveys to assess dental treatment needs of adults? J Public Health Dent. 1998;58:250–253. doi: 10.1111/j.1752-7325.1998.tb03002.x. [DOI] [PubMed] [Google Scholar]
- 13.Farmer J, Ramraj C, Azarpazhooh A, et al. Comparing self-reported and clinically diagnosed unmet dental treatment needs using a nationally representative survey. J Public Health Dent. 2017;77:295–301. doi: 10.1111/jphd.12205. [DOI] [PubMed] [Google Scholar]
- 14.Vered Y, Sgan-Cohen HD. Self-perceived and clinically diagnosed dental and periodontal health status among young adults and their implications for epidemiological surveys. BMC Oral Health. 2003;3:3. doi: 10.1186/1472-6831-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heft MW, Gilbert GH, Shelton BJ, et al. Relationship of dental status, sociodemographic status, and oral symptoms to perceived need for dental care. Community Dent Oral Epidemiol. 2003;31:351–360. doi: 10.1034/j.1600-0528.2003.00014.x. [DOI] [PubMed] [Google Scholar]
- 16.Gilbert AD, Nuttall NM. Self-reporting of periodontal health status. Br Dent J. 1999;186:241–244. doi: 10.1038/sj.bdj.4800075. [DOI] [PubMed] [Google Scholar]
- 17.Åstrøm A N, Kida IA. Perceived dental treatment need among older Tanzanian adults - a cross-sectional study. BMC Oral Health. 2007;7:9. doi: 10.1186/1472-6831-7-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gilbert GH, Heft MW, Duncan RP, et al. Perceived need for dental care in dentate older adults. Int Dent J. 1994;44:145–152. [PubMed] [Google Scholar]
- 19.Locker D, Jokovic A. Using subjective oral health status indicators to screen for dental care needs in older adults. Community Dent Oral Epidemiol. 1996;24:398–402. doi: 10.1111/j.1600-0528.1996.tb00887.x. [DOI] [PubMed] [Google Scholar]
- 20.The Australian Bureau of Statistics; Canberra, ACT: 2016. Cultural diversity in Australia [web]https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/by%20Subject/2007.0.55.001∼2021∼Main%20Features∼Cultural%20diversity∼17 [updated 27/03/2018 cited 2020 May 13] [Google Scholar]
- 21.Wright F, Chu SY, Milledge KL, et al. Oral health of community-dwelling older Australian men: the Concord Health and Ageing in Men Project (CHAMP) Aust Dent J. 2018;63:55–65. doi: 10.1111/adj.12564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cumming RG, Handelsman D, Seibel MJ, et al. Cohort profile: the Concord Health and Ageing in Men Project (CHAMP) Int J Epidemiol. 2009;38:374–378. doi: 10.1093/ije/dyn071. [DOI] [PubMed] [Google Scholar]
- 23.Ueno M, Yanagisawa T, Shinada K, et al. Masticatory ability and functional tooth units in Japanese adults. J Oral Rehabil. 2008;35:337–344. doi: 10.1111/j.1365-2842.2008.01847.x. [DOI] [PubMed] [Google Scholar]
- 24.Kayser AF. Shortened dental arches and oral function. J Oral Rehabil. 1981;8:457–462. doi: 10.1111/j.1365-2842.1981.tb00519.x. [DOI] [PubMed] [Google Scholar]
- 25.Loe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38(Suppl):610–616. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 26.Eke PI, Dye BA, Wei L, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol. 2015;86:611–622. doi: 10.1902/jop.2015.140520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Page RC, Eke PI. Case definitions for use in population-based surveillance of periodontitis. J Periodontol. 2007;78(Suppl 7S):1387–1399. doi: 10.1902/jop.2007.060264. [DOI] [PubMed] [Google Scholar]
- 28.Zhang J, Yu KF. What's the relative risk? A method of correcting the odds ratio in cohort studies of common outcomes. JAMA. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]
- 29.Erik von Elm DGA, Egger M, Pocock SJ, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;18:800–804. doi: 10.1097/EDE.0b013e3181577654. [DOI] [PubMed] [Google Scholar]
- 30.Spencer AJ, Harford J. In: Australia's dental generations: The National Survey of Adult Oral Health 2004–06. Slade GD, Spencer AJ, Roberts-Thomson K, editors. Australian Institute of Health and Welfare; Canberra, ACT: 2007. Dental care; pp. 143–172. [Google Scholar]
- 31.Naka O, Anastassiadou V, Pissiotis A. Association between functional tooth units and chewing ability in older adults: a systematic review. Gerodontology. 2014;31:166–177. doi: 10.1111/ger.12016. [DOI] [PubMed] [Google Scholar]
- 32.Pradeep Y, Chakravarty KK, Simhadri K, et al. Gaps in need, demand, and effective demand for dental care utilization among residents of Krishna district, AndhraPradesh, India. J Int Soc Prev Community Dent. 2016;6(Suppl 2):S116–S121. doi: 10.4103/2231-0762.189737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ekanayke L, Perera I. Factors associated with perceived oral health status in older individuals. Int Dent J. 2005;55:31–37. doi: 10.1111/j.1875-595x.2005.tb00029.x. [DOI] [PubMed] [Google Scholar]
- 34.Lim M, Crocombe LA, Do LG. Perceptions of dental treatment need in Australian-born and migrant populations. Eur J Oral Sci. 2017;125:479–486. doi: 10.1111/eos.12373. [DOI] [PubMed] [Google Scholar]
- 35.Baker DW, Gazmararian JA, Sudano J, et al. The association between age and health literacy among elderly persons. J Gerontol B Psychol Sci Soc Sci. 2000;55:S368–S374. doi: 10.1093/geronb/55.6.s368. [DOI] [PubMed] [Google Scholar]
- 36.Keene J, Li X. Age and gender differences in health service utilization. J Public Health (Oxf) 2005;27:74–79. doi: 10.1093/pubmed/fdh208. [DOI] [PubMed] [Google Scholar]