Abstract
Objectives
School-based interventions can establish positive behaviours that reduce the likelihood of oral diseases later in life. The Brush Day & Night (BDN) programme is a 21-day school-based educational programme to promote good oral health behaviours. This study aims to evaluate the effect of the BDN programme on oral health knowledge and behaviour outcomes in children after the intervention as compared to a control group over 24 weeks.
Methods
This was a superiority cluster randomised trial of children aged 6-12 years from Indonesia (N = 2021) and Nigeria (N = 750). All children were provided with toothpaste and a toothbrush, and the intervention groups (N = 1107 and 439, respectively) received the 21-day BDN programme. Children were followed up at Weeks 3, 8, and 24 after the programme start date and completed a questionnaire addressing the objectives at all timepoints. Improvement in oral health knowledge and behaviour was calculated based on the percentage of positive change in answers and analysed based on a conditional logistic approach for each evaluation timepoint, compared with control, with a 95% CI.
Results
After 24 weeks, Indonesian children following the BDN programme presented with a 30% and 60% additional probability, respectively, of adequate timing of toothbrushing and of being aware of the importance of adequate toothbrushing frequency compared with control. In Nigeria, after 24 weeks, children following the BDN programme had a 92% and 73% higher probability of adequate toothbrushing frequency and of using fluoride toothpaste, respectively, compared with control.
Conclusions
The BDN programme is effective at improving children's knowledge and behaviour compared with a control population.
Key words: Dental caries, Brush Day & Night, Quality of life, Oral hygiene
Introduction
The FDI World Dental Federation defines oral health as “the ability to speak, smile, smell, taste, touch, chew, swallow, and convey a range of emotions through facial expressions with confidence and without pain, discomfort, and disease of the craniofacial complex,” highlighting disease and condition status as 1 element of oral health but also emphasising its relationship to physiological and psychosocial function and its influence on overall well-being.1
Dental caries is the most common noncommunicable disease worldwide and remains a significant public health issue, affecting the primary teeth of more than 530 million children.2 Children's dental caries experience can lead to poor oral health, which has been shown to affect children's ability to sleep, eat, and socialise,3,4 affect school performance,5,6 and result in absence from school with 50 million school hours lost per year.4,7
Limiting sugar intake and brushing twice daily with a fluoride toothpaste (1000-1500 ppm) to remove plaque are widely recommended for all age groups8,9 and are effective in improving gingival health and preventing caries.10,11 School-based interventions represent an ideal approach to improve knowledge around issues such as sugar intake and regular toothbrushing and improve good oral health behaviour at the most influential stages of a child's life; schools offer an inclusive environment in which to reach children whilst also permitting the involvement of teachers and parents.8,12,13 Promoting, repeating, and reinforcing good oral health behaviours during childhood can reduce caries risk in childhood, and once established, these behaviours are sustained throughout adulthood, reducing the likelihood of caries in later life.8,9,14
Improving oral health at both local and population levels is now a common practice worldwide, but a 2013 Cochrane Review of school-based interventions identified the need for interventions that utilise behavioural theory in their design and highlighted the effectiveness of oral health interventions for improving children's oral health knowledge and plaque outcomes.14 As part of a 15-year partnership, the FDI World Dental Federation and Unilever have developed a 21-day, school-based educational programme called Brush Day & Night (BDN), which is based on behavioural change theories.12 The BDN programme is designed to establish the habit of brushing day and night with fluoride toothpaste.11 It involves engaging messages and instructions on daily brushing, and participants are given free toothpaste and toothbrushes.11 It aims to educate children and improve oral health, whilst encouraging the dissemination of oral health messages from children to their parents and wider family members.15 The effectiveness of the 21-day BDN intervention has been previously reported.15 In a study conducted in 10 countries with 7991 children aged 2-12 years, there was an improvement in knowledge and behaviour, with a 25% increase in the number of schoolchildren who brushed their teeth twice daily at completion of the 21-day intervention.15 The programme was found to be most effective in children aged 7-9 years.15
To strengthen the evidence of the programme's effectiveness, this study aims to determine the impact of the 21-day BDN intervention on children's oral health knowledge and behaviour in a randomised sample group 3, 8, and 24 weeks after the start of the programme compared with baseline and a control group. The impact of the programme on plaque levels, caries experience, and well-being is reported in a separate article in this supplement.16
Methods
Study design
This is a superiority cluster randomised trial conducted in Indonesia and Nigeria, involving 20primary and junior schools in Nigeria and 22 in Indonesia, including children aged 6-12 years. The schools in Indonesia were located in low- and middle-income areas, and schools in Nigeria were located in low- middle- and high-income settings. A total of 2021 children from Indonesia were included, 914 in the control group and 1107 in the intervention group. From Nigeria, a total of 1947 children were included, 915 in the control group and 1032 in the intervention group. Schools were matched into pairs by setting (urban or rural) and socioeconomic status and randomised to either intervention or control groups. Teachers were responsible for implementing the programme and were trained by local study coordinators. Further details on the methodology for this study, including the questionnaires and data management, have been previously described.12
Inclusion and exclusion criteria
To be considered for inclusion, children needed to be in school grade 1, 2, or 3, in which most children would be within the target age range of 6-12 years. Although the standard age range for these grades is 6-9 years, some children repeat school years, resulting in a slightly broader age range being included in the study. Children also needed to be in good general health, willing and able to participate in the programme (able to brush their teeth and understand and respond to questions), and planning on attending their currently registered school for at least the next 12 months.
Children were excluded from the study if they did not have written informed consent provided by a parent, were scheduled for medical or dental procedures during the study, had known allergies to any toothpaste ingredients, had obvious signs of gross or untreated caries or significant periodontal disease, or if the study could possibly affect their well-being.
Study endpoints
The primary endpoint was to measure the impact of the BDN programme on oral health knowledge and behaviour of school children over 24 weeks compared with baseline and a control group. This endpoint was measured using the percentage of positive change in answers to questions about oral health knowledge and behaviour on the children's questionnaire at all timepoints – baseline (T0), after 21 days (T0 + 21), after 8 weeks (T1) and 24 weeks (T2).
Outcome measures
At baseline (T0), children answered a questionnaire with 8 main questions, of which 5 addressed the primary objective of improvement in oral health knowledge and behaviour (Supplementary Figure 1, available online) and 3 addressed aspects related to oral health-associated well-being. Questionnaires were repeated for all children at T0 + 21, T1, and T2. Adverse events were also monitored.
Intervention
At T0, upon completion of the questionnaire, children in both groups were provided with toothpaste and a toothbrush. Those in the control group did not receive the BDN programme. Those in the intervention group received the 21-day BDN intervention, comprising brushing instructions, supervision when brushing, songs to facilitate learning about the importance of brushing day and night, and stickers and calendars to track their progress. The programme was supported by colourful materials with bespoke cartoon characters. Parents were provided with educational leaflets. At the end of the BDN programme, children in the intervention group took part in a celebration with certificates and rewards.12
Statistical analysis
Baseline characteristics of children in the intervention group were compared with those in the control group. Proportions and continuous variables were compared using the χ2 and the Mann–Whitney tests, respectively.
The frequency of each outcome (original and transformed variables) was estimated separately for control and intervention groups and at each timepoint. The comparison of variables within the same group and across evaluation timepoints was performed for dependent groups, using the McNemar's test for proportions and the Wilcoxon signed-rank test for continuous variables.
Variables “importance of everyday brushing,” “awareness of adequate frequency,” and “use of fluoride toothpaste” were related to oral health knowledge; variables “toothbrushing frequency” and “toothbrushing timing” were related to oral health behaviour.
Improvement in oral health knowledge and behaviour was calculated based on the percentage of positive change. Positive change is considered when a child moves from selecting a negative or neutral answer to selecting a positive one in any of the variables.
Most variables of interest regarding oral health knowledge and behaviour were categorised as adequate and inadequate. Outcome variables observed before and after the intervention/control were categorised into binary responses (1/0). Importance of everyday brushing was categorised as “Important” vs “Not important” or “Do not know.” Awareness of adequate frequency of toothbrushing in children who responded that it is important to brush teeth daily was categorised as “Adequate” vs “Inadequate.” Use of fluoride toothpaste was categorised as “Yes” vs “No” or “Do not know.” Toothbrushing frequency was categorised as “Adequate” vs “Inadequate, with “Adequate” being considered as 2 or more times a day Toothbrushing timing was categorised as “Adequate” vs “Inadequate,” with “Adequate” being considered as responding both “Morning after breakfast” and “Evening and no eating/drinking after brushing.”
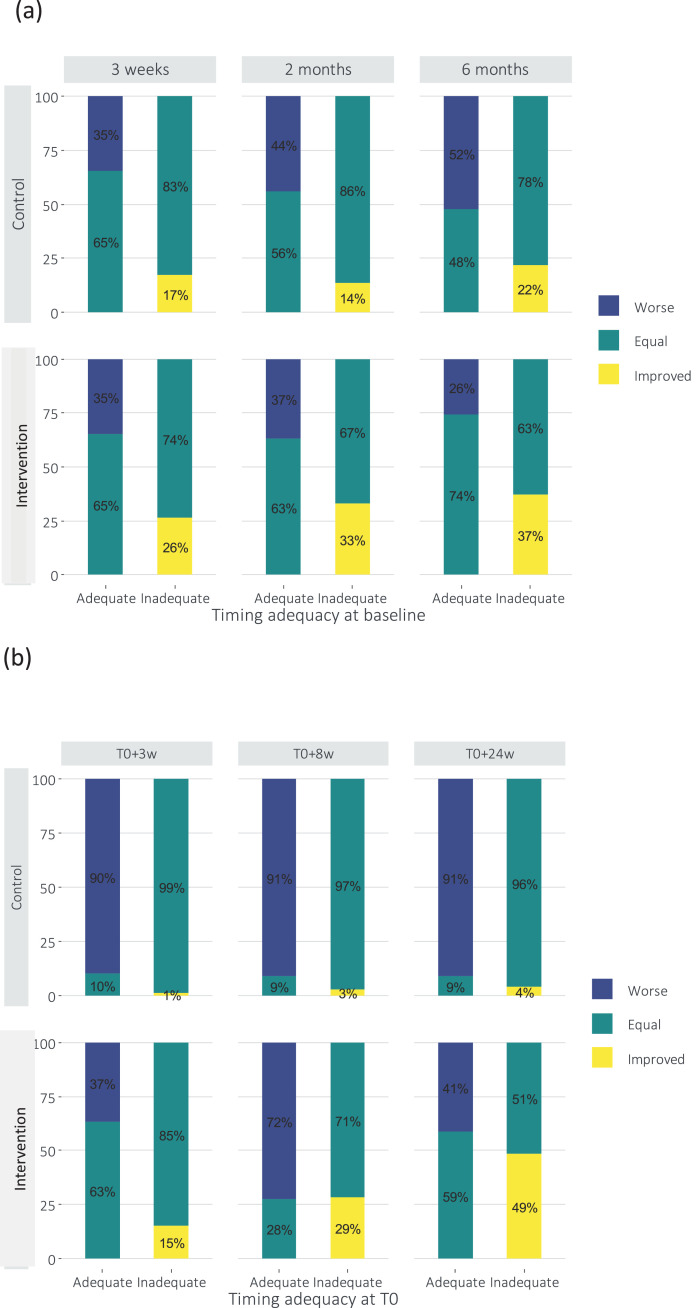
The effect of the intervention was analysed, comparing the effect on each timepoint against baseline, with changes from adequate to inadequate categorised as “worse,” no change categorised as “equal,” and changes from inadequate to adequate categorised as “improved.”
For the primary and additional endpoints, estimates of the crude effect of the intervention on outcome variables were categorised into binary responses and sequentially adjusted for children and school characteristics at baseline, including child's grade, age, and gender, child's opinion on the importance of everyday brushing, use of fluoride toothpaste, and location of the school.
The effect of the intervention was analysed based on a conditional logistic approach for each of the 3 evaluation timepoints: T0 + 3w (T0 + 21), T0 + 8w (T1) and T0 + 24w (T2) and reported as odds ratio (OR) with 95% CI.
Ethics
This study was conducted in accordance with the Declaration of Helsinki. Ethical approval was received from the Nigerian State Universal Basic Education Board and the Health Research Ethics Commission at the Faculty of Dental Teaching, Trisakti University, Indonesia. All parents or legal carers of the participating children signed an informed consent form.
Results
Randomisation and data set
All 2021 children from Indonesia (n = 914 control, 1107 intervention) provided data for all timepoints. Of the 1947 children from Nigeria, children without the baseline assessment or without assessment at T0 + 21, T1, and T2 were excluded. Such exclusions were more prominent within the intervention group (n = 593 [139 and 454, respectively]; 57.5%) in comparison to the control group (n = 264 [67 and 197, respectively]; 28.9%). Finally, 4 schools, all from the control group (n = 344 children), were excluded based on problems related with data registers at all evaluation timepoints. A total of 750 children remained following exclusions. In the control group, 311 provided baseline data, and 290, 277, and 287 provided data at Weeks 3, 8, and 24, respectively. In the intervention group, 439 children provided baseline data, and 395, 406, and 355 provided data at Weeks 3, 8, and 24, respectively.
Children's baseline demographics
Baseline demographics of children were unbalanced for some characteristics across both groups in Indonesia (N = 2021) and Nigeria (N = 750) (Table 1). In Indonesia, significantly more children in the intervention group reported understanding the importance of oral health (P < .05), and they were significantly older than those in the control group (P < .05). Significantly more children in the control group were from urban schools (P < .05) and reported awareness of adequate frequency of toothbrushing than those in the intervention group (P < .05).
Table 1.
Childrens' baseline demographics by assigned group.
| Indonesia |
Nigeria |
|||
|---|---|---|---|---|
| Control 914 N (%)* |
Intervention 1107 N (%)* |
Control 311 N (%)* |
Intervention 439 N (%)* |
|
| Age | ||||
| Median (P25, P75) | 9 (7, 10) | 10 (9, 10)† | 8.0 (7.0-10.0) | 9.0 (8.0-10.0) |
| Gender | ||||
| Male | 449 (49.1) | 559 (50.5) | 161 (51.8) | 212 (48.8) |
| Female | 465(50.9) | 548 (49.5) | 143 (46.0) | 222 (51.2) |
| Schools | ||||
| Rural | 553 (60.5) | 746 (67.4)† | 166 (53.4) | 271 (61.7)† |
| Urban | 361 (39.5) | 361 (32.6) | 145 (46.6) | 168 (38.3) |
| Toothbrushing frequency | ||||
| Inadequate | 303 (33.3) | 330 (29.9) | 220 (71.0) | 347 (79.2)† |
| Adequate | 608 (66,7) | 775 (70.1) | 90 (29.0) | 91 (20.8) |
| Toothbrushing timing | ||||
| Inadequate | 592 (65.1) | 707 (64.3) | 297 (96.4) | 417 (95.6) |
| Adequate | 318 (34.9) | 393 (35.7) | 11 (3.6) | 19 (4.4) |
| Importance of oral health | ||||
| Important | 832 (91.0) | 1042 (94.2)† | 306 (98.7) | 431 (98.2) |
| Not important | 17 (1.9) | 22 (2.0) | 2 (0.6) | 4 (0.9) |
| Do not know | 65 (7.1) | 42 (3.8) | 2 (0.6) | 4 (0.9) |
| Awareness of adequate frequency of toothbrushing (if consider oral health important) | ||||
| Inadequate | 79 (9.5) | 137 (13.4)† | 155 (51.0) | 97 (22.6)† |
| Adequate | 753 (90.5) | 886 (86.6) | 149 (49.0) | 332 (77.4) |
| Fluoride toothpaste | ||||
| Use | 761 (83,3) | 939 (84.8) | 272 (88.0) | 245 (55.9)† |
| Do not use | 91 (10.0) | 80 (7.2) | 16 (5.2) | 39 (8.9) |
| Not sure | 62 (6.8) | 88 (7.9) | 21 (6.8) | 154 (35.2) |
P25 = 25th percentile; P75 = 75th percentile.
Wilcoxon test for continuous variable; χ2 test for all other variables.
Percentage of nonmissing responses within the study group.
P < .05.
In Nigeria, significantly fewer children in the intervention group used fluoride toothpaste and had adequate frequency of toothbrushing (P < .05). As in Indonesia, significantly more children in the control group were from urban schools (P < .05). Significantly more children reported awareness of adequate frequency of toothbrushing in the intervention group than in the control group (P < .05). Children in Nigeria had lower reported rates of adequate frequency of toothbrushing (<30%) than children in Indonesia (>70%).
Crude effect of BDN programme on oral health knowledge and behaviour
Oral health knowledge
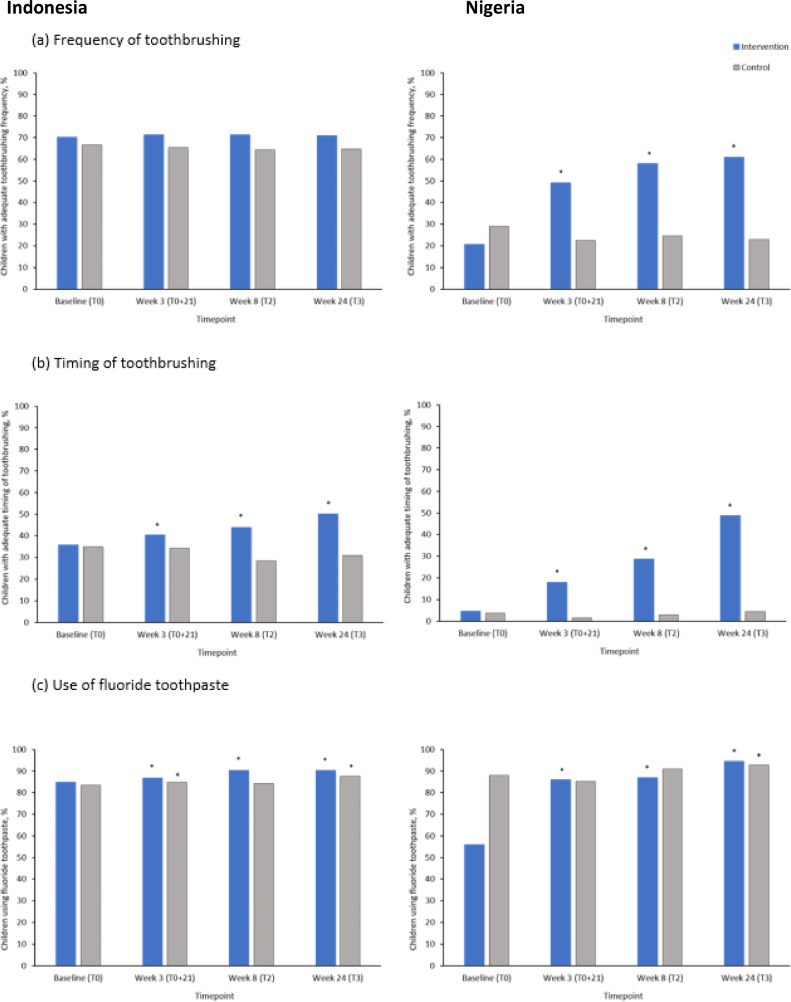
The proportion of children who considered everyday brushing as important remained high throughout the study for all groups in both Indonesia and Nigeria (>90%), and there was no significant difference from baseline at any timepoints or between groups, apart from a significant decrease in children from Indonesia in the control group at Week 24 (P < .05) (Tables 2 and 3). Children from the intervention group in Indonesia demonstrated a significant increased awareness of the importance of adequate toothbrushing frequency compared with the control group (P < .05) (Tables 2 and 3). A greater proportion of children from both countries reported using fluoride toothpaste at all study timepoints compared with baseline in both the intervention and control groups (P < .05) (Tables 2 and 3, Figure 1).
Table 2.
Crude data from Indonesia.
| Intervention |
Control |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| T0 | T0 + 21 | T1 | T2 | T0 | T0 + 21 | T1 | T2 | ||
| Behaviour | Frequency | 70.1 | 71.3 | 71.2 | 70.8 | 66.7 | 65.3 | 64.3 | 64.8 |
| Timing | 35.7 | 40.2* | 43.9* | 50.5* | 34.9 | 34.2 | 28.3† | 30.9† | |
| Knowledge | Everyday | 94.2 | 94.9 | 94.9 | 94.9 | 91.0 | 91.7 | 90.3 | 83.5† |
| Awareness | 86.6 | 88.1* | 89.7* | 94.3* | 90.5 | 90.3 | 88.8 | 89.7 | |
| Fluoride | 84.8 | 88.8* | 90.3* | 90.2* | 83.3 | 85.4† | 84.2 | 87.6* | |
,†Statistically significant difference in proportions relative to intervention and control baseline (P value < .05 from McNemar's test).
Table 3.
Crude data from Nigeria.
| Intervention |
Control |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| T0 | T0 + 21 | T1 | T2 | T0 | T0 + 21 | T1 | T2 | ||
| Behaviour | Frequency | 20.8 | 49.1* | 58.1* | 61.1* | 29.0 | 22.4 | 24.5 | 23.0 |
| Timing | 4.4 | 17.8† | 28.6† | 48.7† | 3.4 | 1.4 | 2.9 | 4.2 | |
| Knowledge | Everyday | 98.2 | 99.0 | 99.5 | 99.4 | 98.7 | 98.6 | 96.8 | 98.6 |
| Awareness | 77.4 | 93.2* | 90.8* | 88.7* | 49.0 | 63.3† | 57.4† | 67.5† | |
| Fluoride | 55.9 | 85.8* | 86.9* | 94.4* | 88.0 | 85.2† | 91.0 | 92.7† | |
,†Statistically significant difference in proportions relative to intervention and control baseline (P value < .05 from McNemar's test).
Fig. 1.
Effect of Brush Day & Night programme or control on knowledge/behaviour and toothbrushing habits in school children from Indonesia and Nigeria at Weeks 3, 8, and 24 compared with baseline (FAS).
*Statistically significant improvement from baseline (P value < .05 from McNemar's test).
BDN = Brush Day & Night; FAS = full analysis set.
Oral health behaviour
In Indonesia, the proportion of children with adequate frequency of toothbrushing was high in both intervention and control groups at baseline and did not change across the study duration (Table 2 and Figure 1). In Nigeria, the proportion of children with adequate frequency of toothbrushing in the intervention group increased significantly across all timepoints, compared with baseline (P < .05) (20.8% [T0], 49.1% [T0 + 21], 58.1% [T1], 61.1% [T2]) (Table 3 and Figure 1). This was not observed for children in the control group. The proportion of children with adequate timing of toothbrushing significantly increased from baseline at all timepoints in the intervention groups in both Indonesia and Nigeria (P < .05) (Tables 2 and 3, Figure 1). In children with inadequate timing of toothbrushing at baseline, significantly greater improvements were seen at all timepoints in both countries in the intervention group compared with the control group (P < .05) (Figure 2).
Fig. 2.
Change in the adequacy of timing of toothbrushing according to the baseline status in (a) Indonesia and (b) Nigeria.
Effect of BDN programme on oral health knowledge and behaviour adjusted for children and school characteristics at baseline
Oral health knowledge
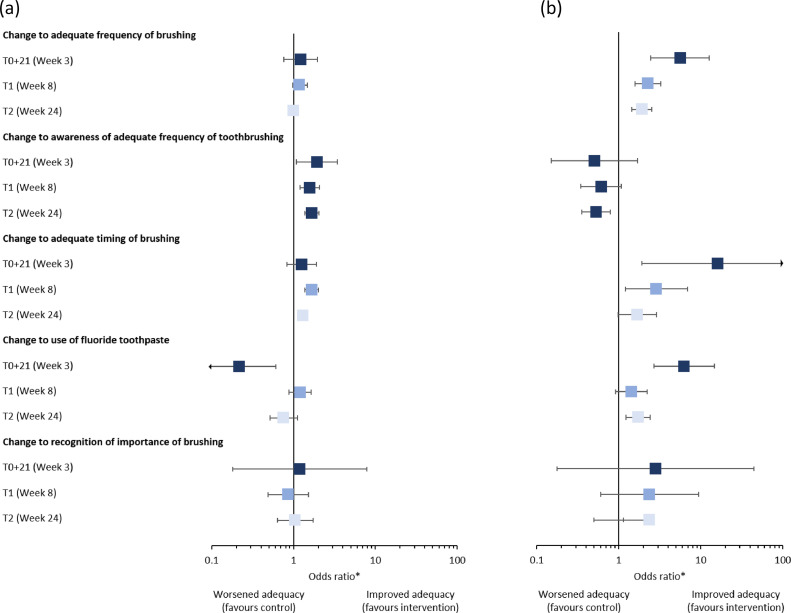
When adjusted for child and school characteristics, there were no significant differences in children's opinion on the importance of everyday brushing in the intervention and control groups in both Indonesia and Nigeria (Tables 4 and 5, Figure 3).
Table 4.
Effect of the intervention on Indonesia children's knowledge and behaviour.
| T0 + 3w |
T0 + 8w |
T0 + 24w |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| N | OR | 95% CI | N | OR | 95% CI | n | OR | 95% CI | |
| Change to adequate frequency of brushing | |||||||||
| Crude effect of the intervention | 1997 | 1.352 | 0.905-2.018 | 2001 | 1.197 | 0.992-1.445 | 2005 | 1.076 | 0.951-1.217 |
| Adjusted effect*†‡§ | 1997 | 1.217 | 0.757-1.958 | 2001 | 1.171 | 0.983-1.468 | 2005 | 1.002 | 0.871-1.153 |
| Change to adequate timing of brushing | |||||||||
| Crude effect of the intervention | 1996 | 1.482 | 1.046-2.101 | 1999 | 1.684 | 1.416-2.001 | 2000 | 1.498 | 1.344-1.670 |
| Adjusted effect *†‡§ | 1996 | 1.257 | 0.833-1.894 | 1999 | 1.663 | 1.377-2.010 | 2000 | 1.296 | 1.137-1.476 |
| Change to recognition of everyday brushing as important | |||||||||
| Crude effect of the intervention | 2014 | 1.222 | 0.404-3.702 | 2014 | 1.366 | 0.913-2.044 | 2016 | 1.974 | 1.468-2.652 |
| Adjusted effect *†‡§ | 2014 | 1.183 | 0.180-7.795 | 2014 | 0.860 | 0.488-1.515 | 2016 | 1.044 | 0.632-1.725 |
| Change to being aware of adequate frequency of toothbrushing | |||||||||
| Crude effect of the intervention | 1826 | 1.921 | 1.079-3.419 | 1800 | 1.575 | 1.195-2.075 | 1751 | 1.666 | 1.364-2.036 |
| Adjusted effect*†‡§ | 1826 | 1.672 | 0.677-4.129 | 1800 | 1.741 | 1.232-2.461 | 1751 | 1.607 | 1.277-2.022 |
| Change to fluoride toothpaste | |||||||||
| Crude effect of the intervention | 2010 | 0.847 | 0.473-1.516 | 2015 | 1.266 | 0.989-1.622 | 2014 | 1.106 | 0.902-1.357 |
| Adjusted effect *†‡§ | 2010 | 0.216 | 0.077-0.605 | 2015 | 1.203 | 0.885-1.634 | 2014 | 0.759 | 0.514-1.122 |
CI = confidence intervals; n = number of children; OR = odds ratio.
Children's grade.
Children's sex.
Children's opinion on the importance of everyday brushing (at baseline), usage of fluoride toothpaste (at baseline), and feeling of pain in the mouth while eating (at baseline).
School location (rural vs urban).
Table 5.
Effect of the intervention on Nigerian children's knowledge and behaviour.
|
T0 + 3w |
T0 + 8w |
T0 + 24w |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| n | OR | 95% CI | N | OR | 95% CI | n | OR | 95% CI | |
| Change to adequate frequency of brushing | |||||||||
| Crude effect of the intervention | 672 | 8.774 | 4.363-17.640 | 672 | 2.634 | 1.957-3.545 | 634 | 2.453 | 1.943-3.097 |
| Adjusted effect*‡§‖ | 5.593 | 2.466-12.685 | 2.265 | 1.582-3.244 | 1.922 | 1.452-2.544 | |||
| Change to adequate timing of brushing | |||||||||
| Crude effect of the intervention | 676 | 24.429 | 5.320-112.174 | 676 | 3.477 | 1.982-6.100 | 635 | 2.766 | 1.890-4.049 |
| Adjusted effect*¶‖ | 16.125 | 1.923-135.192 | 2.888 | 1.206-6.913 | 1.681 | 0.983-2.875 | |||
| Change to recognition everyday brushing important | |||||||||
| Crude effect of the intervention | 681 | 4.000 | 0.500-31.980 | 678 | 3.240 | 1.166-9.003 | 639 | 1.817 | 0.826-4.000 |
| Adjusted effect†‖ | 2.806 | 0.176-44.750 | 2.381 | 0.599-9.462 | 2.383 | 0.497-1.144 | |||
| Change to being aware of adequate frequency of toothbrushing | |||||||||
| Crude effect of the intervention | 640 | 1.139 | 0.542-2.394 | 636 | 1.091 | 0.779-1.530 | 604 | 0.777 | 0.607-0.993 |
| Adjusted effect†§¶‖ | 0.505 | 0.150-1.705 | 0.608 | 0.344-1.076 | 0.529 | 0.356-0.785 | |||
| Change to fluoride toothpaste | |||||||||
| Crude effect of the intervention | 679 | 8.810 | 4.330-17.925 | 675 | 1.821 | 1.245-2.662 | 636 | 1.925 | 1.459-2.539 |
| Adjusted effect*†¶‖ | 6.272 | 2.692-14.610 | 1.428 | 0.914-2.230 | 1.730 | 1.234-2.425 | |||
CI = confidence interval; n, number of children (control/intervention); OR = odds ratio.
Children's grade.
Children's age.
Children's adequacy of brushing timing at baseline.
Children's usage of flour toothpaste at baseline.
Children's adequacy of brushing frequency at baseline.
School location (rural vs urban).
Fig. 3.
Effect of Brush Day & Night programme on knowledge/behaviour and toothbrushing habits in school children from (a) Indonesia and (b) Nigeria at Weeks 3, 8, and 24 compared with control (FAS).
*Adjusted for child's age, grade, baseline behavioural characteristics, and school location.
BDN = Brush Day & Night; FAS = full analysis set.
In Indonesia, children in the intervention group had a 60% (95% CI 28%-100%) higher probability of being more aware of the adequate frequency of toothbrushing after 24 weeks compared with the control group (Table 4, Figure 3). In the Nigeria intervention group, the opposite was observed: Children demonstrated a 47% higher probability (21.5%-64%) of not being aware of the adequate frequency of toothbrushing compared with the control group (Table 5, Figure 3).
In Nigeria, there was a significant 73% (23%-142%) greater probability of children reporting using fluoride toothpaste in the intervention group compared with the control group at Week 24 (Table 5 and Figure 3). There was no significant difference between children from Indonesia in the intervention and control groups at any timepoint for this outcome (Table 4, Figure 3).
Oral health behaviour
Children in the intervention group from Nigeria had a 92% (95% CI 45%-154%) greater probability of presenting adequate frequency of brushing at 24 weeks compared with the control group (Table 5, Figure 3).
In Indonesia, children in the intervention group had a 30% greater probability (14%-48%) of presenting adequate timing of brushing compared with the control group (Table 4, Figure 3). In Nigeria, at Week 8, children in the intervention group had a 189% (21%-581%) greater probability of presenting adequate timing of brushing compared with the control group (Table 5, Figure 3).
Discussion
The BDN programme is a behavioural change intervention targeting children of primary school age.11 The programme promotes, repeats, and reinforces good toothbrushing and oral hygiene behaviours over a 21-day engaging programme to encourage the habit of brushing day and night, with previous demonstrated efficacy in several countries.15 However, additional evidence would confirm the effectiveness of the programme in improving children's oral health knowledge and behaviour. To this end, this study aimed to assess change in oral health knowledge and behaviour in a randomised cluster sample and compare the effect of the programme with a control group of children.
Indonesia and Nigeria were selected for this study as the BDN programme has previously been implemented in both countries, ensuring the programme is run as effectively as possible on 2 different continents.15 It also provides results from countries with different relevant baseline characteristics.
Crude analysis of the data demonstrated that there were improvements, overall, in oral health knowledge in both cohorts from the 2 countries, achieving significance in the intervention group in Indonesia and also in the control group in Nigeria. The stated use of fluoride toothpaste improved at all timepoints in both groups from both cohorts from the 2 countries compared with baseline, with slightly greater improvements in children in the intervention groups. The proportion of children who considered everyday brushing as important remained high throughout the study period.
In the Nigerian cohort, being in the intervention group was associated with greater improvements in oral health behaviour (frequency and timing of toothbrushing) than participation in the control group. In Indonesia cohort, only the timing of toothbrushing improved significantly in the intervention group when compared with the control. The frequency of toothbrushing would not be expected to show differences as the initial values were already high in both groups.
When analysing the crude effect of the programme, it can be verified that, compared with the previous study,15 the results of the intervention group show similar improvements throughout the 24 weeks. This is observed in both cohorts from the 2 countries. In the previous study of the effectiveness of the BDN programme, 25% more children brushed their teeth twice a day after 6 to 12 months, compared with a 40% increase at 24 weeks in this study. An analysis adjusted for children and school characteristics at baseline was also employed in the initial study and, therefore, supports the crude analysis employed in our study.
Other studies in both developing and developed countries that employed unadjusted analysis support our findings. In a study by Vangipuram et al in children aged 12-15 years in Bangalore, the effectiveness of a peer (school)-led- versus a dentist-led oral health education programme was analysed over 6 months. Results indicated that both programmes were effective in improving oral health knowledge, attitude, behaviour, and clinical outcomes.17 Studies have also concluded that classroom-based training provides significant improvements in oral health knowledge and behaviour, increasing the use of fluoride toothpaste and a twice-daily toothbrushing habit.18, 19, 20, 21, 22 Further, several investigations have confirmed that schools are ideal locations for toothbrushing interventions in children because they offer long-term opportunities, with repeated exposures, to develop healthy behaviours15,23, 24, 25 and improve oral health outcomes.6,26 It has also been reported that children need visual stimuli to promote learning of brushing techniques.6,27
Although the improvements in oral health knowledge and behaviour revealed by the crude analysis of this study reflect results from the initial study of 10 countries by Melo et al,15 there were some significant differences in baseline characteristics between the intervention and control groups in both countries. For this reason, a multivariate analysis was carried out, sequentially adjusting for children and school characteristics at baseline, including child's grade, age, and gender, child's opinion on the importance of everyday brushing, use of fluoride toothpaste, and location of the school.
When data were adjusted, children in the intervention group in Indonesia still demonstrated an increase in their awareness of adequate toothbrushing frequency. Likewise, increases in toothbrushing frequency seen in the crude analysis were also observed after adjustment. However, the adjusted data revealed that fluoride use increased in Nigerian children, an effect not seen in the crude data. Furthermore, adjustment of data revealed that improvements in adequate timing of brushing seen across all timepoints in the crude data are restricted to the 8-week timepoint in Nigerian children and to both the 8- and 24-week timepoint in Indonesian children. Taken together, it can be concluded that the 21-day BDN programme improved oral health knowledge and behaviour across both cohorts from the 2 countries.
After completion of the BDN programme, the improvements in timing of toothbrushing, importance of everyday brushing, stated use of fluoride toothpaste, and awareness of adequate toothbrushing timing (only for Indonesia cohort) remained high after 6 months, suggesting that the programme reinforces knowledge and encourages lasting behavioural change and improved oral hygiene.
These results demonstrate that reinforcement and repetition of messages and procedures are important to the sustainability of healthy behaviours like toothbrushing, at least for 24 weeks.15,24 It may therefore be appropriate to run the BDN programme biannually, timed to coincide with the beginning of the school year and repeated prior to the end of the school year before the summer holidays.
A strength of this study is that it was carried out in children aged 8-10 years (median from both countries and groups), which is close to the 7- to 9-year age range in which the BDN programme has been previously demonstrated to be most effective.15 It was also carried out in Indonesia and Nigeria, 2 countries that have prior experience of the BDN programme. The age range and location therefore ensure that the intervention is run as efficiently and effectively as possible, whilst the control group allows for comparison other than to baseline values.
A weakness of the study is that the exclusions from the Nigerian study limit the usefulness of comparisons between countries due to the differences in sample size and compromise the integrity of the randomised and controlled nature of the study in Nigeria due to uneven dropout rates. However, the Nigerian cohort data are still valid because they can be compared to a control group. Although the crude analysis revealed certain improvements in both oral health knowledge and behaviour over the 24-week period, it also revealed similar improvements in both intervention and control groups in other knowledge and behaviour outcomes. These improvements may be explained by the fact that the control group received a toothpaste and toothbrush at the beginning of the programme, which may itself be a motivating intervention. However, it should be noted that, from an ethical point of view, it would not be acceptable to deny children the toothbrush and toothpaste. In addition, the control group may also have been influenced by being observed clinically and being required to answer questionnaires periodically, which can condition the responses. This effect would also be expected in the intervention group. It could therefore be concluded that the appropriateness of the control group may have been compromised. It may also have been more appropriate to carry out the questionnaire without conditioning children through being observed clinically and being required to answer questionnaires periodically.
Conclusion
With the BDN programme, Indonesian children showed a 30% greater probability of presenting adequate timing of brushing and a 60% greater probability of being aware of the adequate frequency of toothbrushing after 24 weeks. Nigerian children showed a 92% greater probability of presenting adequate frequency of brushing and a 73% greater probability of using fluoride toothpaste at 24 weeks. These results were observed after both crude and adjusted analysis, with the exception of improvement in fluoride toothpaste use, which was observed after adjusted analysis. The BDN programme is effective at improving children's oral health knowledge and behaviour over a 21-day programme, with results lasting at least 6 months, compared with a control population.
Conflict of interest
P.M., C.F. and S.T. report no conflicts of interest regarding the work under consideration for publication, no relevant financial activities outside the submitted work, and no patents or copyrights. S.M. is employed by Unilever Oral Care.
Acknowledgments
Acknowledgements
The authors would like to thank the following study leads: Dr Tri Erri Astoeti, National Liaison Officer Indonesian Dental Association, and Dr Olabode Adeyemi Ijarogbe, President, Nigerian Dental Association. They also thank Dr Sofia Correia, University of Porto, for her contribution to the data analysis. Medical writing assistance in the form of preparation and revision of the manuscript was provided by Lee Kempster at MediTech Media, under the authors’ conceptual direction and based on feedback from the authors.
Funding
This article is published as part of a supplement sponsored by Unilever. Medical writing assistance, in the form of preparation and revision of the manuscript, as well as support of the conduct of the research, was supported financially by Unilever.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.identj.2021.01.014.
Appendix. Supplementary materials
Referencess
- 1.Glick M, Williams DM, Kleinman DV, Vujicic M, Watt RG, Weyant RJ. A new definition for oral health developed by the FDI World Dental Federation opens the door to a universal definition of oral health. Int Dent J. 2016;66(6):322–324. doi: 10.1111/idj.12294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.GBD DALYs, Hale Collaborators Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1859–1922. doi: 10.1016/S0140-6736(18)32335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gilchrist F, Marshman Z, Deery C, Rodd HD. The impact of dental caries on children and young people: what they have to say? Int J Paediatr Dent. 2015;25(5):327–338. doi: 10.1111/ipd.12186. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Sugars and dental caries factsheet. Available from: https://www.who.int/news-room/fact-sheets/detail/sugars-and-dental-caries. Accessed 3 November 2020.
- 5.Illinois Department of Public Health. Illinois Department of Public Health promotes oral health during National Children's Dental Health Month. Available from:http://www.idph.state.il.us/public/press14/2.21.14_National_Childrens_Dental_Health_Month.htm. Accessed 3 November 2020.
- 6.Calderon SJ, Mallory C. A systematic review of oral health behavior research in American adolescents. J Sch Nurs. 2014;30(6):396–403. doi: 10.1177/1059840514544034. [DOI] [PubMed] [Google Scholar]
- 7.Jackson SL, Vann WF, Jr., Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children's school attendance and performance. Am J Public Health. 2011;101(10):1900–1906. doi: 10.2105/AJPH.2010.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kwan SY, Petersen PE, Pine CM, Borutta A. Health-promoting schools: an opportunity for oral health promotion. Bull World Health Organ. 2005;83(9):677–685. [PMC free article] [PubMed] [Google Scholar]
- 9.Curnow M, Burnside G, Pine C. IADR; San Francisco, CA: 2017. Sustained dental health benefits for adults from childhood toothbrushing intervention. Abstract 0549. [Google Scholar]
- 10.dos Santos AP, Nadanovsky P, de Oliveira BH. A systematic review and meta-analysis of the effects of fluoride toothpastes on the prevention of dental caries in the primary dentition of preschool children. Community Dent Oral Epidemiol. 2013;41(1):1–12. doi: 10.1111/j.1600-0528.2012.00708.x. [DOI] [PubMed] [Google Scholar]
- 11.FDI World Dental Federation. Brush Day & Night 12 Years of Improving Oral Health Worldwide. Available from: https://www.fdiworlddental.org/sites/default/files/media/resources/fdi-bdn_12_years_oral_health.pdf. Accessed 3 November 2020.
- 12.Melo P, Malone S, Rao A, Fine C. A 21-day school-based toothbrushing intervention in children aged 6 to 9 years in Indonesia and Nigeria: protocol for a two-arm superiority randomized controlled trial. JMIR Res Protoc. 2020;9(2):e14156. doi: 10.2196/14156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization (WHO). Local action: creating health promoting schools. 2000. Report No: 1727-2335. Available from:https://apps.who.int/iris/handle/10665/66576. Accessed 3 November 2020.
- 14.Cooper AM, O'Malley LA, Elison SN, et al. Primary school-based behavioural interventions for preventing caries. Cochrane Database Syst Rev. 2013;(5) doi: 10.1002/14651858.CD009378.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Melo P, Fine C, Malone S, Frencken JE, Horn V. The effectiveness of the Brush Day and Night programme in improving children's toothbrushing knowledge and behaviour. Int Dent J. 2018;68(Suppl 1):7–16. doi: 10.1111/idj.12410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Melo P, Fine C, Malone S, Taylor S. Impact of the brush day & night programme on wellbeing, plaque and dental caries in children. Int Dent J. 2021;71(Suppl 1) doi: 10.1016/j.identj.2021.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vangipuram S, Jha A, Raju R, Bashyam M. Effectiveness of peer group and conventional method (Dentist) of oral health education programme among 12-15 year old school children - a randomized controlled trial. J Clin Diagn Res. 2016;10(5) doi: 10.7860/JCDR/2016/17725.7844. ZC125-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Esan A, Folayan MO, Egbetade GO, Oyedele TA. Effect of a school-based oral health education programme on use of recommended oral self-care for reducing the risk of caries by children in Nigeria. Int J Paediatr Dent. 2015;25(4):282–290. doi: 10.1111/ipd.12143. [DOI] [PubMed] [Google Scholar]
- 19.Joybell C, Krishnan R, SK V. Comparison of two brushing methods- fone's vs modified bass method in visually impaired children using the audio tactile performance (ATP) technique. J Clin Diagn Res. 2015;9(3) doi: 10.7860/JCDR/2015/11307.5651. ZC19-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCauley HB, Davis LB, Frazier TM. Effect on oral cleanliness produced by dental health instruction and brushing the teeth in the classroom. J School Health. 1955;25:250–254. [Google Scholar]
- 21.Patil SP, Patil PB, Kashetty MV. Effectiveness of different tooth brushing techniques on the removal of dental plaque in 6-8 year old children of Gulbarga. J Int Soc Prev Community Dent. 2014;4(2):113–116. doi: 10.4103/2231-0762.138305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ceyhan D, Akdik C, Kirzioglu Z. An educational programme designed for the evaluation of effectiveness of two tooth brushing techniques in preschool children. Eur J Paediatr Dent. 2018;19(3):181–186. doi: 10.23804/ejpd.2018.19.03.3. [DOI] [PubMed] [Google Scholar]
- 23.Tolvanen M, Lahti S, Hausen H. Changes in toothbrushing frequency in relation to changes in oral health-related knowledge and attitudes among children - a longitudinal study. Eur J Oral Sci. 2010;118(3):284–289. doi: 10.1111/j.1600-0722.2010.00737.x. [DOI] [PubMed] [Google Scholar]
- 24.Brukiene V, Aleksejuniene J. Theory-based oral health education in adolescents. Stomatologija. 2010;12(1):3–9. [PubMed] [Google Scholar]
- 25.Flanders RA. Effectiveness of dental health educational programs in schools. J Am Dent Assoc. 1987;114(2):239–242. doi: 10.14219/jada.archive.1987.0033. [DOI] [PubMed] [Google Scholar]
- 26.Biesbrock AR, Walters PA, Bartizek RD. Short-term impact of a national dental education program on children's oral health and knowledge. J Clin Den. 2004;15(4):93–97. [PubMed] [Google Scholar]
- 27.Hebbal M, Ankola AV. Development of a new technique (ATP) for training visually impaired children in oral hygiene maintenance. Eur Arch Paediatr Dent. 2012;13(5):244–247. doi: 10.1007/BF03262878. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.