Abstract
Objectives
Most dentists maintain awkward and restricted postures for prolonged periods that stress the body while providing direct patient care. Information about working posture must be analysed in a more systematic manner to provide a deeper understanding of the relationship between working posture and work-related musculoskeletal disorders (MSD). Therefore, the present study aimed to clarify the effects of different lines of vision during tooth preparation, such as the direct and the mirror view technique, on-body tilt (angle), muscle activity, and sitting balance, which may correlate with the reduction or prevention of MSD.
Methods
A mannequin head with a maxillary right first molar embedded in a model was attached to the dental chair headrest. Two different techniques for tooth preparation were selected: direct view and mirror view. Muscle activity, body tilt (angle), and sitting balance were analysed as independent parameters.
Results
Different tooth preparation techniques had a distinct influence on body tilt (angle), muscle activity, and sitting balance. The direct view technique resulted in significantly larger values for all parameters, except for the activity of the spinal column erector muscles than the mirror view technique.
Conclusion
Based on these results, the direct view technique for tooth preparation, which is used by most dentists in practice, imposes a burden on the lower back, shoulders, and neck of the dentist.
Key words: Dental practice, Education, Posture, Muscle activity, Sitting balance
Introduction
Dental treatment involves procedures performed with a high degree of precision in a relatively restricted space. Specifically, (i) the oral cavity offers a narrow, limited space for instrumentation, (ii) treatment is possible from 1 direction, and (iii) a high level of accuracy is required. Most dentists experience considerable loads on the muscles of the neck, shoulders, and lower back while providing treatment. Combined with a flexed cervical spine, dentists may encounter high precision work demands and sustained static loading of the back, neck, and shoulders.1
In general, working posture is related to musculoskeletal health and musculoskeletal disorders (MSD). According to an epidemiological study by Gallagher,2 work performed in unusual and restricted postures is associated with significantly higher rates of musculoskeletal complaints than work that does not require these postures. The relationship between working posture and MSD is supported by overexertion, differential fatigue, and cumulative load theories to explain musculoskeletal injuries.3 Bertolaccini et al4 investigated the effects of posture on the activity of the superior trapezius and longissimus muscles. Sitting with the trunk leaning forward at 45° resulted in a significant increase in the activity of both muscles. For many years, lower back pain has been the leading cause of absence from work and the leading indication for medical rehabilitation.5
Dental professionals are susceptible to MSDs that result from incorrect posture at work.1,6, 7, 8, 9, 10 According to Pope-Ford1 dental work-related MSDs are caused by overexertion, awkward postures, and repetitive motions. Improper postures adopted by dentists during work cause discomfort and disorders of the musculoskeletal system and the peripheral nervous system.8 Musculoskeletal problems represent a significant burden for dental professionals.9 Poor posture and inappropriate ergonomics may result in a wide variety of MSDs.7 Thus, dentists should focus on improving posture. A relationship exists between prolonged, static (motionless) muscle contractions and muscle ischemia or necrosis. Weak postural muscles of the trunk and shoulder may lead to poor operator posture. As muscles adapt by lengthening or shortening to accommodate these postures, muscle imbalances may occur, leading to structural damage and pain.10 Musculoskeletal problems have become a significant issue for both dentists and dental hygienists.9
Several studies have examined the relationship between MSDs and the posture of dental professionals while providing care. The working posture of dentists and dental hygienists was assessed using work sampling and video techniques and postural data of the neck, shoulders, and lower back were recorded. Dentists and dental hygienists spent at least half of their time working with their necks flexed at an angle of at least 60°, and their trunks were flexed at an angle of at least 30°.11 Pope-Ford1 used a motion tracking system to quantify posture variations during 4 specific dental procedures (cavity preparation, tooth extraction, mirror check, and the application and removal of dental dam clamps) in a simulation laboratory. The data provide a biomechanical evaluation of abnormal lumbar ranges of motion believed to be associated with an increased risk of lower back pain (LBP). When tasks were performed in the seated and standing postures, lateral flexion and axial rotation ranges of motion limits for the risk of injury were consistently exceeded, providing insights into the causes and prevention of work-related MSD.1
Dental treatment includes various procedures, such as tooth extraction, root canal treatment, fillings, and periodontal therapy. Tooth preparation involves the reduction of enamel and dentin to an accuracy of ≤0.1 mm. Most dentists prepare teeth using direct vision and are forced to adopt abnormal postures that twist the upper part of the body. Thus, the direct view technique imposes a burden on the cervical and lumbar vertebrae, resulting in work-related MSDs.1,6, 7, 8, 9, 10, 11 In contrast, the mirror view technique represented by proprioceptive derivation (pd) concept12 allows the dentist to view the working field from the 10:00 to the 12:30 position and maintain an upright posture. To date, the relationship between postures adopted by dentists for different lines of vision and MSDs has not been elucidated.
Most dentists maintain awkward and restricted postures for prolonged periods during tooth preparation, thus placing considerable loads on the body. However, sufficient countermeasures are not implemented to relieve the awkward posture. In patients with a typical MSD, LBP is a symptom rather than a disease. Similar to other symptoms, such as headache and dizziness, LBP can have several underlying causes. Approximately 90% of LBP cases are nonspecific.13 Thus, popular strategies to prevent LBP or MSD are based on limiting exposure to risk factors. A previous study has described workplace interventions aimed to reduce the excessive loading of the spine.14 A significant increase in the prevalence of MSD-related pain was observed among the group who worked using the direct vision technique.15 Hence, studies that evaluate the effects of different lines of vision on posture and MSD during tooth preparation are urgently needed. Goniometers, inclinometers, photographic techniques, electrogoniometers, and video recording systems are used to measure working postures. Information about working posture must be collected and analysed in a more systematic manner to provide a deeper understanding of the relationship between working posture and work-related MSD.3
The present study aimed to clarify the effects of different lines of vision during tooth preparation, such as the direct and the mirror view technique, on-body tilt (angle), muscle activity, and sitting balance, which may correlate with the occurrence, reduction, or prevention of MSD.
Materials and methods
Maxillary right first molar embedded in a model (A2-94[cross] ma16, Nissin Dental Products Inc.) mounted to a mannequin head (Simple mannequin III, Nissin Dental Products Inc.) was attached to dental units or patient chairs and used for tooth preparation. Two techniques for tooth preparation were selected: direct view and mirror view. Two dental units or patient chairs in a simulation laboratory were used. Signo G50 (J. Morita Mfg. Corp.) was used in the direct view technique and Spaceline EMCIA III UP (J. Morita Mfg. Corp.) in the mirror view technique.12
Ten male dentists who routinely treat patients using the mirror view technique of pd concept were selected (average age: 34.9 ± 5.4 years) (Table 1). Two types of tooth preparation were chosen to be prone to tilting by direct view technique: an occlusal surface cavity and the distal axial surface of an abutting tooth. Each procedure was performed thrice using each technique in a random sequence. TF-22 (Mani Inc.) was used for the occlusal surface cavity, and TR-13 (Mani Inc.) was used to prepare the axial surface of the abutting tooth in each preparation. In the direct view technique, the movement of the doctor's chair was not constrained. In the mirror view, the chair movements ranged from the 10:00 to the 12:30 position.
Table 1.
Characteristics of dentists.
| No. | Age (year) | Height (cm) | Body weight (kg) | Length of clinical experience (years) | Major field of dentistry |
|---|---|---|---|---|---|
| 1 | 34 | 174 | 62 | 9 | general dentistry |
| 2 | 30 | 175 | 80 | 6 | general dentistry |
| 3 | 33 | 173 | 87 | 8 | restorative dentistry |
| 4 | 36 | 166 | 66 | 12 | prosthetics |
| 5 | 27 | 172 | 62 | 3 | general dentistry |
| 6 | 30 | 163 | 52 | 6 | general dentistry |
| 7 | 35 | 183 | 83 | 11 | restorative dentistry |
| 8 | 40 | 168 | 74 | 15 | restorative dentistry |
| 9 | 37 | 174 | 68 | 13 | general dentistry |
| 10 | 47 | 168 | 84 | 21 | prosthetics |
| Mean | 34.9 | 171.6 | 71.8 | 10.4 | |
| SD | 5.4 | 5.4 | 11.0 | 4.9 |
SD, standard deviation.
Muscle activity, body tilt (angle), and sitting balance were analysed as independent parameters.
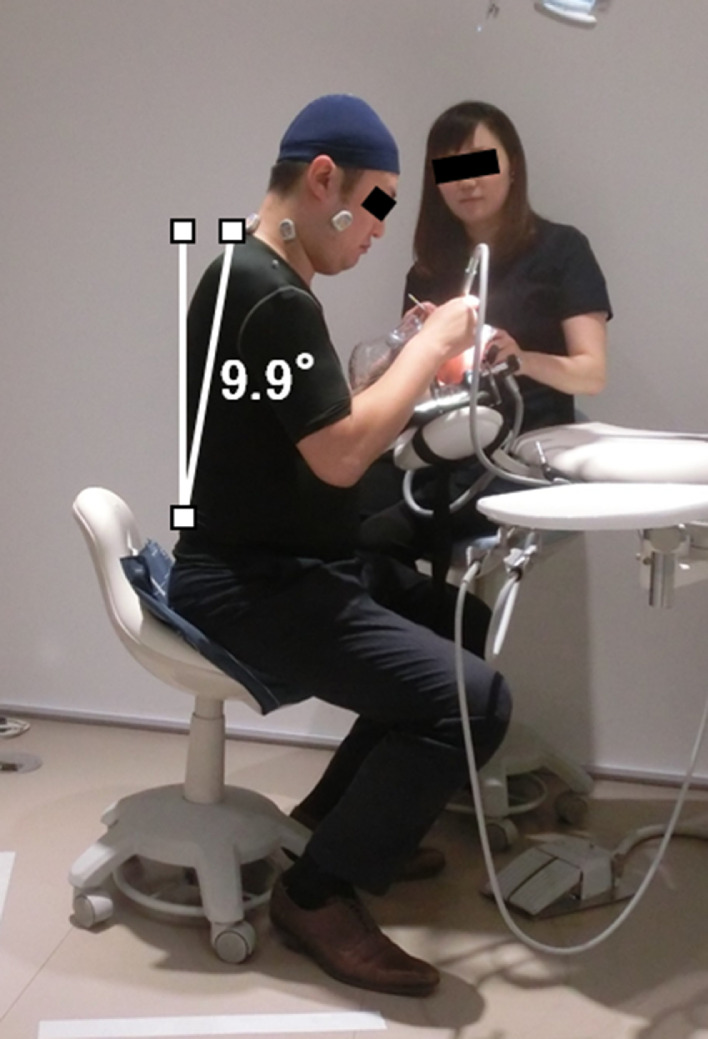
Videos were recorded using a digital hi-vision video camera (HC-V520M, Panasonic Corporation) from the lateral side of the subject and analysed for body tilt (angle). Four markers were placed on the parietal, the seventh cervical vertebra, the first lumbar vertebra, and floor surface to measure the angle between the parietal and the seventh cervical vertebra and the seventh cervical vertebra and the first lumbar vertebra. During the video recording, a vertical line to the floor was established and placed in the image as a standard for the angle. The electromyograms were synchronised with digital video images. In the synchronous display provided by the Pixel Runner (Tellusimage), trigger signals were inputted into the WEB-7000 and light signals into the video image, both by direct current, to synchronise them. An analysis package (Angle) in the video analysis software DARTFISH 9 (Dartfish Japan Co., Ltd.) was used to analyse the angle (Figure 1). In this case, a larger value indicated a larger inclination.
Fig. 1.
A representative measurement obtained with the mirror view technique during tooth preparation.
Electromyographic (EMG) measurements of the superior trapezius and the spinal column erector muscles, which have a significant correlation with increased cervical flexion and activity levels related to MSD,4 were collected bilaterally using the multichannel telemetry system WEB-7000 (Nihon Kohden). This system primarily consists of an EMG (ZB-150H), EMG transmitters (cordless telemetry electrodes), BIO Repeater (ZB-700H), receiver antenna (ZR-700H), receiver, and personal computer. The electrodes for the upper trapezius were placed at 50% on the line from the acromion to the spine on the C7 vertebra, and the electrodes of the spinal column erector muscles were placed 2 finger-widths lateral to the spinous process of L1. The lower cutoff frequency was 30 Hz, the higher cutoff frequency was 5 kHz, and the sampling frequency was 10 kHz. Data collected from 3 stable 10-second periods of muscle activity during each trial were analysed, and integrated values were compared.
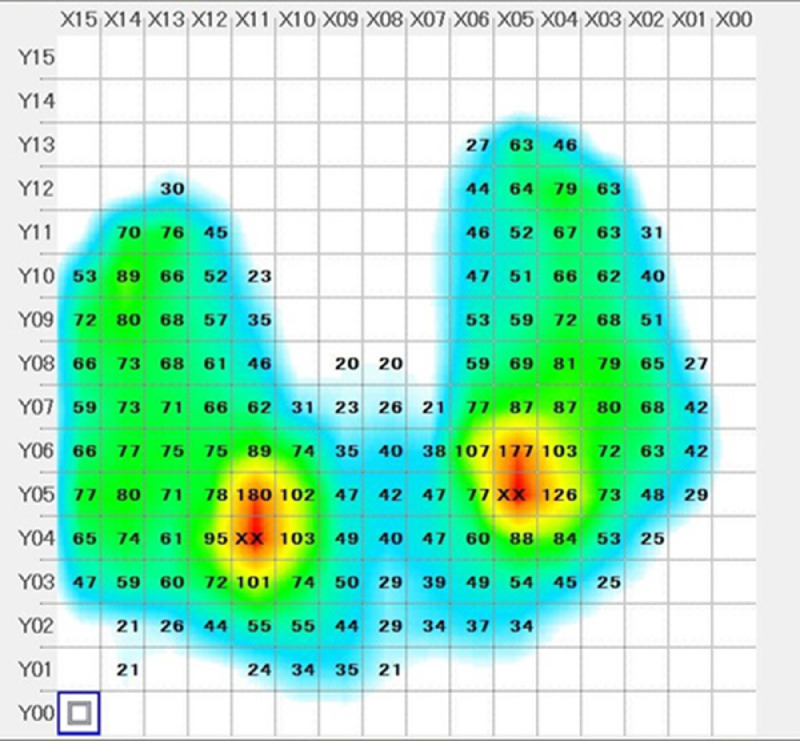
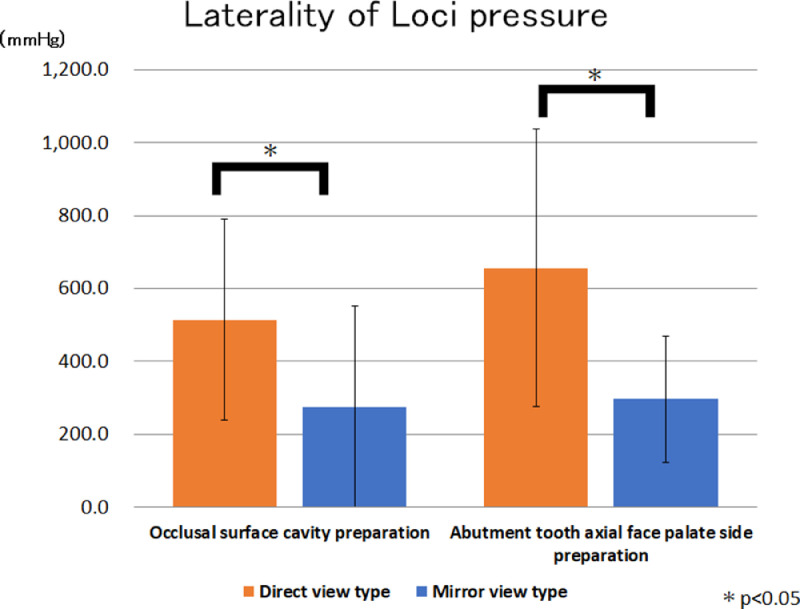
The laterality of pressure at each locus was measured and analysed using SR Softvision (Sumitomo Riko Co., Ltd.).16 The sensor sheet was divided into 16 sections, and the pressure value was obtained for each square. The measurable range was 20-200 mm Hg. We compared the sum of the pressure values for the 8 squares located around the highest part of the right and left seat pressures (Figure 2).
Fig. 2.
Pressure at each locus was measured and analysed using a sensor sheet (SR Softvision).
Data were analysed using Excel statistics (Microsoft Japan) statistical software with the Kolmogorov-Smirnov test for the analysis of normality and the Mann-Whitney U-test for body tilt, masseter muscle activity, and laterality of pressure at each locus. A P value <.05 was considered significant.
The study protocol, which was approved by the Tokyo Dental College Ethics Committee (Approval No. 763), was explained in detail to all participating dentists before the commencement of the experiment, and written consent was obtained from each participant. The study adhered to the tenets of the Declaration of Helsinki on the ethical treatment of human subjects.
Results
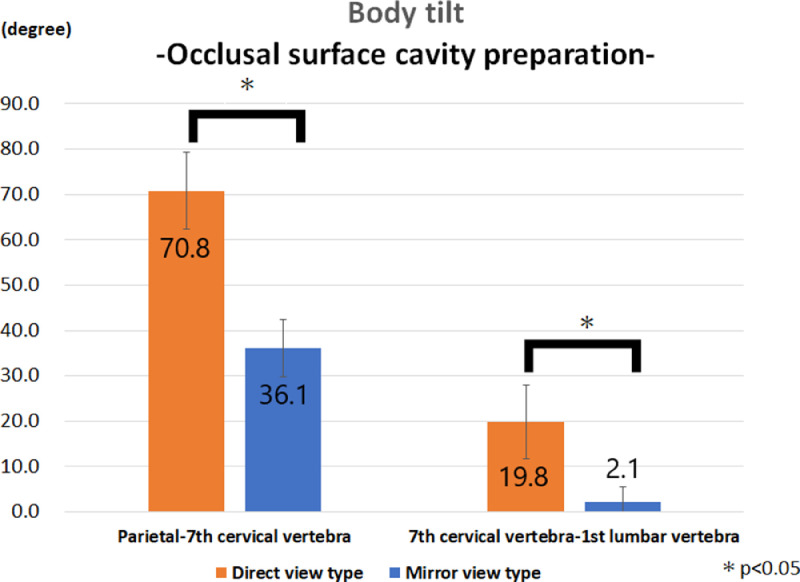
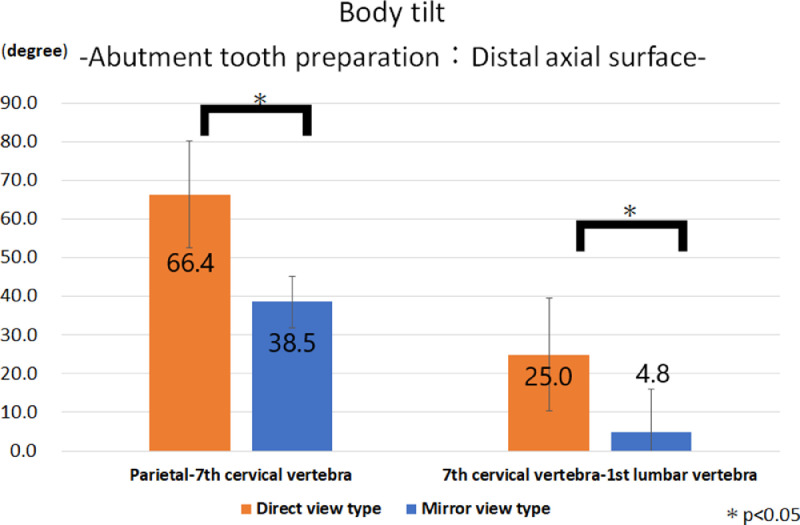
The body tilt and statistical analysis are shown in Fig. 3, Fig. 4. The use of the direct view technique to prepare the occlusal cavity and the distal surface of the abutting tooth produced a larger value for angles of the parietal to the seventh cervical vertebra (direct view: 70.1, 66.5, mirror view: 36.5, 38.5) and the seventh cervical vertebra to the first lumbar vertebra (direct view: 19.9, 25.0, mirror view: 2.5, 5.0), with significant differences between the direct view and the mirror view techniques. The direct view technique required the dentist to tilt the head more than 65° while preparing the occlusal cavity and the distal surface of the abutting tooth.
Fig. 3.
During occlusal cavity preparation, the direct view technique produced a larger body tilt at the angles of the parietal to the seventh cervical vertebra and the seventh cervical vertebra to the first lumbar.
Fig. 4.
During the preparation of the distal surface of the abutting tooth, the direct view technique produced a larger body tilt at the angles of the parietal to the seventh cervical vertebra and the seventh cervical vertebra to the first lumbar vertebra.
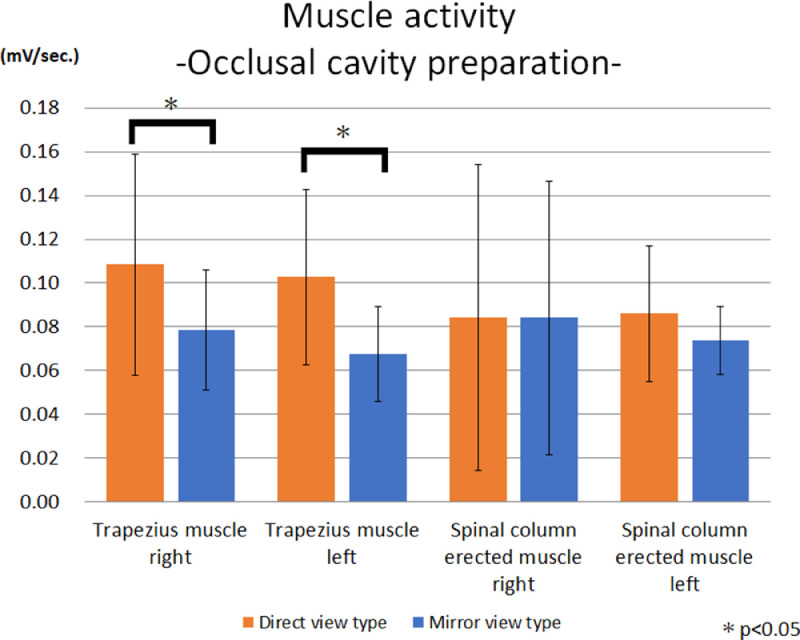
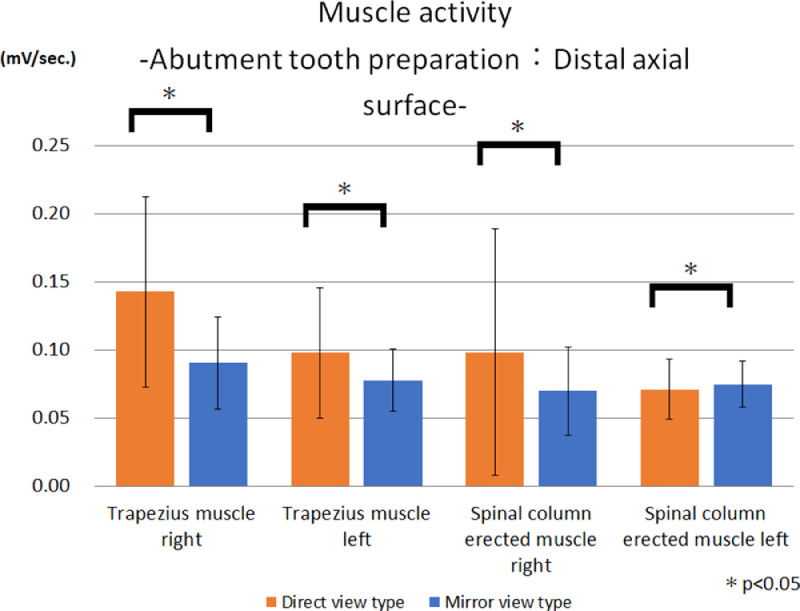
The muscle activities and statistical analyses are shown in Fig. 5, Fig. 6. The use of the direct view technique to prepare the occlusal cavity resulted in significantly larger values for the right and left trapezius muscles than the mirror view technique. Moreover, the left spinal column standing muscle showed greater activity. Dentists using the direct view technique to prepare the distal surface of the abutting tooth showed significantly larger values for the activities of the right and left trapezius muscles and the spinal column erector muscles than those using the mirror view technique.
Fig. 5.
During occlusal cavity preparation, the direct view technique resulted in significantly greater activities of the right and left trapezius muscles than the mirror view technique. Furthermore, the left spinal column erector muscle showed increased activity.
Fig. 6.
During the preparation of the distal surface of the abutting tooth, the direct view technique produced significantly greater activities in the right and left trapezius muscles and the spinal column erector muscles.
The sitting balance and statistical analyses are shown in Figure 7. The use of the direct view technique to prepare the occlusal cavity and the distal surface of the abutting tooth produced a significantly larger value than that of the mirror view technique.
Fig. 7.
During the preparation of the occlusal cavity and the distal surface of the abutting tooth, the direct view technique produced significantly larger pressures at each locus than the mirror view technique.
Discussion
This is the first study to investigate the effects of different lines of vision during tooth preparation on body posture by systematically analysing several quantitative data points. Based on the results, the direct view technique resulted in significantly larger values for body tilt, muscle activities, and sitting balance, except for the activities of the spinal column erector muscles during occlusal cavity preparation, than the use of the mirror view technique. The direct view technique, which is used by most dentists in daily practice while treating patients, imposes a burden on the lower back, shoulders, and neck. These results are consistent with the outcomes reported in related studies investigating the correlation between the posture of dental professionals and MSDs. Pain was significantly more prevalent among the group who worked using direct vision.15 In addition, a peculiar working posture causes MSD.1,6, 7, 8, 9, 10
The results obtained in the present study have an interesting correlation with the hypothesis proposed by Carter.17 The theory suggested that the human head constitutes about 8% of the total body weight. The average weight is 14 pounds in men and 11 pounds in women. Therefore, the head is the main culprit in torque generation because it relates to the operator position. Operators are required to lean or tilt forward to achieve a direct line of vision into the oral cavity. For every second that the bowling ball head is positioned at a 45° forward lean or tilt originating from the cervical area of your neck, 6.56 foot-pounds of torque must be resisted to prevent the face from crashing into the chest.17 The present study reported a tilt of >65% when the dentist used the direct view technique. Furthermore, inclined and increased torso weight may also increase the load on the lower back.
The activities of the trapezius and spinal column erector muscles substantially increased to support the increased weight of the head and the torso. Moreover, continuous unusual posture configurations and muscle activities may lead to the development of MSDs. Vieira and Kuma3 explained the relationship between unusual postures and MSDs in their study. Prolonged, repeated, awkward, constrained, and asymmetric postures can overload tissues by exceeding their thresholds of tolerable stress, causing injury because of overexertion or imbalance.18 The maintenance of prolonged static posture compresses the veins and capillaries inside the muscles, causing microlesions due to the absence of tissue oxygenation and nutrition.19 An unusual posture primarily leads to injuries affecting muscles, tendons, and ligaments. Nerve injury is secondary to compression or ischemia. Bones and cartilage in joints are affected by handling loads and strains accumulated over several years.18 According to Marklin and Cherney,11 flexed and abducted joint posture requires higher muscle forces to maintain these static postures because of the mechanical disadvantage of the muscles relative to the joints. The high muscle forces then produce high compression loads on the joint. The posture assumed by dentists and dental hygienists requires sizeable muscle forces and, concomitantly, high compression loads on the joint.
Several research surveys and literature reviews have evaluated the relationship between the prevalence of musculoskeletal pain or MSDs and dental practices.20, 21, 22, 23, 24 A study that used a self-reported questionnaire to examine work-related MSDs observed a high percentage (75%) of reported pain in dental students.21 A self-administered online questionnaire study20 revealed that 85% of the participants had experienced some work-related pain in the dental profession. Another study performed with the self-administered Nordic musculoskeletal evaluation chart in a young generation showed a 70% incidence of back pain among dentists, with lower back pain predominating in 48% of the cases. Most subjects (91%) had mild-to-moderate levels of pain severity, and approximately 10% had severe lower back pain. The majority of dentists (57%) only treated 1-3 patients per day.22 A cross-sectional survey using random cluster sampling indicated that approximately 90% of dentists reported MSD pain. Moreover, lower back pain was the most commonly reported symptom (about 68%).25 Data were collected from dentists and dental nurses using the Baseline Risk Identification of Ergonomic Factors (BRIEF) survey, and interviews with structured questionnaires indicated that most workers frequently complained of pain in a combination of 3 sites (neck, shoulders, and back).23 Moreover, dental hygienists in Australia have high rates of neck and shoulder disorders based on self-reported and physician-diagnosed neck and shoulder pain.24 Furthermore, a review by Hayes et al9 reported that the prevalence of general musculoskeletal pain ranged from 64% to 93%. The back (36.3%-60.1%) and the neck (19.8%-85%) were the most prevalent regions for pain in dentists, and the hands and the wrists were most frequently affected in dental hygienists (60%-69.5%).
As mentioned, the prevalence of work-related MSDs among dental professionals is high, sometimes or in some cases affecting their daily activities and even forcing them to change their work setting.20 The maintenance of unusual and restricted postures during treatment is strongly associated with MSDs. Therefore, the risk factors related to MSDs among dentists and dental professionals should be minimised or eliminated. The roles of ergonomics, counselling, proper techniques of patient handling, and other processes should be emphasised to ensure that dental professionals can work efficiently.20
First, pain was significantly prevalent in dentists using direct vision.15 The results of the present study indicate that dentists using the direct vision technique adopt awkward postures. Therefore, the mirror view technique should be considered for dental treatment. Dentists should also recognise proper equipment usage to improve working posture,26 neutralise nonergonomic behaviours, and reduce risks.27The use of a mouth mirror and loupes helps to reduce torque by decreasing the degree of forward lean or tilt.17 Dental professionals should select appropriate dental furniture or dental devices that promote proper body posture by reducing the magnitude and duration of deviated joint postures, which, in theory, would decrease the risk of MSDs.11 However, a current study22 also revealed that although 63% of the subjects were aware of the advantages of using assistive tools, only 40% used them. The rate of MSDs could be reduced by promoting awareness of the value of available assistive devices. A hospital and an educational institution should support the use of workstations and dental tools with ergonomic designs to fit the individual and task.23
Second, the patient (and many dentists and hygienists) should be well-informed over the entire course of his or her illness and should be encouraged to adopt a healthy lifestyle that includes regular physical exercise.5 Thoracic spine mobilisation added to a stabilisation exercise increases the muscular strength of patients with chronic lower back pain.28 Functional training for dentistry should include an exercise prescription for dental health care personnel.29
Furthermore, we should focus on identifying the risk factors affecting work-related MSDs, such as age, sex, dental specialty, work environment, number of contact hours with patients, and a history of severe MSD.20,21,25,30
Although this study produced important findings, it has limitations that must be noted. First, the participants were relatively young. Second, only male subjects were included. Moreover, the patient's perceived discomfort was not assessed, which may contribute to our understanding of the correlation between objective measurements and subjective perceptions. Future studies should include a sample of both genders with a wider age group and a discomfort scale, such as a visual analogue scale, should be used.
Conclusions
The use of different tooth preparation techniques, namely, the direct or mirror view technique, influenced the body tilt (angle), muscle activity, and sitting balance. The direct view technique resulted in significantly larger values for body tilt, muscle activities, and sitting balance than the mirror view technique, except for the activities of the spinal column erector muscles in occlusal cavity preparations. Based on these results, the direct view technique, which is used by most dentists in practice while treating patients, imposes a burden on the lower back, shoulders, and neck during tooth preparation procedures.
Acknowledgments
Acknowledgements
The authors would like to thank all study participants for their kind cooperation with this study. In particular, the subjects were acknowledged for their willing participation in this study.
Conflicts of interest
This study was funded by J. MORITA MFG. CORP., Osaka, Japan.
References
- 1.Pope-Ford R. A quantitative assessment of low back pain in dentistry. Procedia Manufactur. 2015;3:4761–4768. [Google Scholar]
- 2.Gallagher S. Physical limitations and musculoskeletal complaints associated with work in unusual or restricted postures: a literature review. J Saf Res. 2005;36(1):51–61. doi: 10.1016/j.jsr.2004.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Vieira ER, Kumar S. Working postures: a literature review. J Occup Rehab. 2004;14(2):143–159. doi: 10.1023/b:joor.0000018330.46029.05. [DOI] [PubMed] [Google Scholar]
- 4.Bertolaccini Gda S, Nakajima RK, Filho IF, Paschoarelli LC, Medola FO. The influence of seat height, trunk inclination and hip posture on the activity of the superior trapezius and longissimus. J Phys Ther Sci. 2016;28(5):1602–1606. doi: 10.1589/jpts.28.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chenot JF, Greitemann B, Kladny B, Petzke F, Pfingsten M, Schorr SG. Non-specific low back pain. Dtsch Arztebl Int. 2017;114(51-52):883–890. doi: 10.3238/arztebl.2017.0883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayes MJ, Smith DR, Cockrell D. Prevalence and correlates of musculoskeletal disorders among Australian dental hygiene students. Int J Dent Hyg. 2009;7(3):176–181. doi: 10.1111/j.1601-5037.2009.00370.x. [DOI] [PubMed] [Google Scholar]
- 7.Vakili L, Halabchi F, Mansournia MA, Khami MR, Irandoost S, Alizadeh Z. Prevalence of common postural disorders among academic dental staff. Asian J Sports Med. 2016;7(2):e29631. doi: 10.5812/asjsm.29631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Szymanska J. Disorders of the musculoskeletal system among dentists from the aspect of ergonomics and prophylaxis. Ann Agric Environ Med. 2002;9(2):169–173. [PubMed] [Google Scholar]
- 9.Hayes M, Cockrell D, Smith DR. A systematic review of musculoskeletal disorders among dental professionals. Int J Dent Hyg. 2009;7(3):159–165. doi: 10.1111/j.1601-5037.2009.00395.x. [DOI] [PubMed] [Google Scholar]
- 10.Valachi B, Valachi K. Mechanisms leading to musculoskeletal disorders in dentistry. J Am Dent Assoc. 2003;134(10):1344–1350. doi: 10.14219/jada.archive.2003.0048. [DOI] [PubMed] [Google Scholar]
- 11.Marklin RW, Cherney K. Working postures of dentists and dental hygienists. J Calif Dent Assoc. 2005;33(2):133–136. [PubMed] [Google Scholar]
- 12.Montakarn C. Differences in dentists’ working postures when adopting proprioceptive derivation vs. conventional concept. Int J Occup Saf Ergon. 2005;11(4):441–449. doi: 10.1080/10803548.2005.11076662. [DOI] [PubMed] [Google Scholar]
- 13.Koes BW, van Tulder MW, Thomas S. Diagnosis and treatment of low back pain. BMJ. 2006;332(7555):1430–1434. doi: 10.1136/bmj.332.7555.1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maher C, Underwood M, Buchbinder R. Non-specific low back pain. Lancet. 2017;389(10070):736–747. doi: 10.1016/S0140-6736(16)30970-9. [DOI] [PubMed] [Google Scholar]
- 15.Hayes MJ, Smith DR, Taylor JA. Musculoskeletal disorders and symptom severity among Australian dental hygienists. BMC Res Notes. 2013;6:250. doi: 10.1186/1756-0500-6-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yanagiseko Y, Kawasima S, Kozaki K, Itoh J, Sejimo T, Tanaka H. Truncus training of a Quadriplegic cerebral palsied patient (Use of JOBA and SR softvision). Scientific truncus training using Horse-riding simulator and plane pressure measurement device. J Jpn Soc Para Sports Sci. 2017;(26):74–77. [Google Scholar]
- 17.Carter J. The inevitability of neck and back pain. DentistryIQ. 2006 https://www.dentistryiq.com/dental-hygiene/career-development/article/16348337/the-inevitability-of-neck-and-back-pain Available from. Accessed November 2018. [Google Scholar]
- 18.Kumar S. Theories of musculoskeletal injury causation. Ergonomics. 2001;44(1):17–47. doi: 10.1080/00140130120716. [DOI] [PubMed] [Google Scholar]
- 19.Kumar S. A conceptual model of overexertion [correction of oxerexertion], safety, and risk of injury in occupational settings. Hum Factors. 1994;36(2):197–209. doi: 10.1177/001872089403600202. [DOI] [PubMed] [Google Scholar]
- 20.Alghadir A, Zafar H, Iqbal ZA. Work-related musculoskeletal disorders among dental professionals in Saudi Arabia. J Phys Ther Sci. 2015;27(4):1107–1112. doi: 10.1589/jpts.27.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Carvalho MV, Soriano EP, de Franca Caldas A, Jr., Campello RI, de Miranda HF, Cavalcanti FI. Work-related musculoskeletal disorders among Brazilian dental students. J Dent Educ. 2009;73(5):624–630. [PubMed] [Google Scholar]
- 22.Gaowgzeh RA, Chevidikunnan MF, Al SA, El-Gendy S, Karrouf G, Al SS. Prevalence of and risk factors for low back pain among dentists. J Phys Ther Sci. 2015;27(9):2803–2806. doi: 10.1589/jpts.27.2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chaiklieng S, Suggaravetsiri P. Ergonomics risk and neck shoulder back pain among dental professionals. Procedia Manufact. 2015;3:4900–4905. [Google Scholar]
- 24.Morse T, Bruneau H, Michalak-Turcotte C, et al. Musculoskeletal disorders of the neck and shoulder in dental hygienists and dental hygiene students. J Dent Hyg. 2007;81(1):10. [PubMed] [Google Scholar]
- 25.Al-Mohrej OA, AlShaalan NS, Al-Bani WM, Masuadi EM, Almodaimegh HS. Prevalence of musculoskeletal pain of the neck, upper extremities and lower back among dental practitioners working in Riyadh, Saudi Arabia: a cross-sectional study. BMJ Open. 2016;6(6) doi: 10.1136/bmjopen-2016-011100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ayatollahi J, Ayatollahi F, Ardekani AM, et al. Occupational hazards to dental staff. Dent Res J. 2012;9(1):2–7. doi: 10.4103/1735-3327.92919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rafeemanesh E, Jafari Z, Kashani FO, Rahimpour F. A study on job postures and musculoskeletal illnesses in dentists. Int J Occup Med Environ Health. 2013;26(4):615–620. doi: 10.2478/s13382-013-0133-z. [DOI] [PubMed] [Google Scholar]
- 28.Yang S-R, Kim K, Park S-J. The effect of thoracic spine mobilization and stabilization exercise on the muscular strength and flexibility of the trunk of chronic low back pain patients. J Phys Ther Sci. 2015;27(12):3851–3854. doi: 10.1589/jpts.27.3851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones AC, Forsythe S. Functional training for dentistry: an exercise prescription for dental health care personnel. J Calif Dent Assoc. 2005;33(2):137–145. [PubMed] [Google Scholar]
- 30.Hodacova L, Sustova Z, Cermakova E, Kapitan M, Smejkalova J. Self-reported risk factors related to the most frequent musculoskeletal complaints among Czech dentists. Industrial Health. 2015;53(1):48–55. doi: 10.2486/indhealth.2013-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]