Abstract
Objective
To monitor wound healing following surgical extraction of wisdom teeth using the novel Inflammatory Proliferative Remodeling (IPR) Scale.
Methods
A prospective study design was used. Participants included 94 otherwise healthy adult patients undergoing surgical extraction of a wisdom tooth at a tertiary medical centre from June 2018 to June 2019. The IPR Scale was completed by two resident surgeons in oral and maxillofacial surgery at three time points after the procedure, corresponding to the three phases of wound healing. Mean subscale and total scores were calculated. Patients graded their preoperative anxiety, intraoperative pain, and pain during follow-up on a 10 cm visual analog scale, and the findings were correlated with the IPR Scale scores.
Results
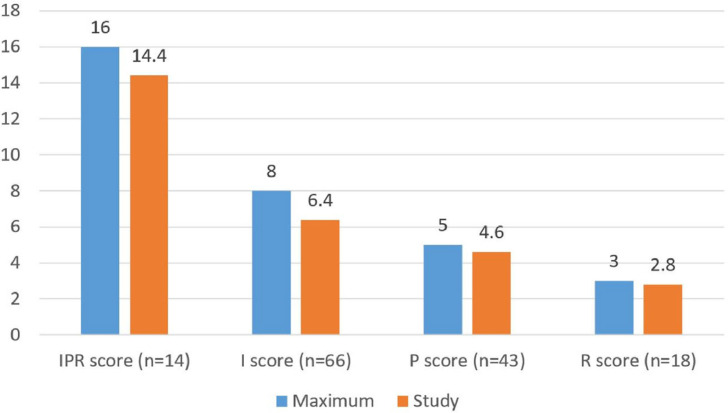
Mean IPR total score (range 0–16) was excellent (14.43 ± 1.45). Mean scores by healing phase were as follows: inflammatory 6.35 ± 1.34 (range 0–8); proliferation, 4.56 ± 0.8 (range 0–5); remodeling, 2.83 ± 0.51 (range 0–3). There was a positive correlation between mean preoperative anxiety level (5.9 ± 3.6) and intraoperative pain perception (2.4 ± 2.4; P = 0.65) and a negative correlation between mean preoperative anxiety level and IPR Scale scores for each healing phase. Two cases were complicated by abscesses which resolved with treatment.
Conclusion
The IPR Scale is a promising tool for the effective evaluation of the wound healing process following wisdom tooth extractions. Relaxation methods and behavioural adaptation might help to lower patient anxiety and thereby improve oral wound healing.
Key words: Inflammatory Proliferative Remodeling Scale, Surgical extraction, Wound healing scale
Introduction
The healing response is an essential phylogenetically primitive defence mechanism.1 Injuries of any kind initiate a complex series of proximate and often overlapping biological events directed toward restoring tissue integrity.1 All tissues follow an essentially identical pattern consisting of three main phases: inflammatory, proliferation, and remodeling. The specific characteristics of each phase, however, may differ by tissue type.1 Disturbed wound healing may be due to the surgical procedure itself or the type of wound and has many clinical manifestations. The informed surgeon is able to identify early signs and symptoms of complications in the soft tissue and perform timely interventions to ensure a good outcome and favourable progression of wound repair. Therefore, wound healing scales may be useful in this setting.1,2
Nevertheless, wound healing scales are infrequently used in oral surgery and have been investigated mainly in split-mouth studies of patients after tooth extraction. A recent review described eight wound healing scales designed for oral and maxillofacial surgery.3 The most often cited was Landry's Healing Index2,4 which measures five clinical outcome parameters: tissue colour, bleeding on palpation, presence of granulation tissue, incision margin (epithelialisation and connective tissue exposure), and suppuration. Scores range from 0 (poor healing) to 5 (excellent healing).2,4 Other scales included: the Early Wound Healing Index (EHI),5,6 which divides the quality of healing into five levels according to flap closure, presence of fibrin, and partial or complete necrosis of the interproximal tissue; the visual analogue scale (VAS) Cosmesis Scale2,7,8; Wound Evaluation Scale (WES)2,7; and Three-Score VAS Categorical Scale.8 However, in none of them did the outcome parameters correlate with the wound healing phases, including Landry's Index which has undergone several modifications for this purpose,9, 10, 11, 12 and in none was the ideal oral wound healing process defined.
To counter this problem, the Inflammatory Proliferative Remodeling (IPR) Wound Healing Scale (Table 1)3 was developed to assist surgeons in monitoring postoperative oral mucosal wound healing. The scale is divided into three subscales corresponding to the three phases of wound healing, and each is rated at the appropriate time point during follow-up,3 yielding three subscale scores and a total score. The outcome parameters of the subscales depend on the biological events that occur during that specific phase.
-
•
The inflammatory phase (days 3–5 postoperatively) is characterised by vasoconstriction of the injured vasculature with aggregation of circulating platelets that adhere to each other to form a fibrin plug. This results in haemostasis which sets the stage for provisional matrix foramtion.1 Once haemostasis is secured, vascular permeability is increased, allowing blood plasma and other cellular mediators of healing to pass through the vessel walls by diapedesis. The corresponding clinical manifestations include swelling, redness, heat, and pain.
-
•
The proliferative phase (14 days postoperatively) is characterised by the formation of pink granulation tissue containing inflammatory cells and by collagen secretion. The corresponding clinical manifestations include re-epithelialisation, pink tissue colour and scar formation.1,3 Dysregulation of this phase may cause excess collagen and scar contracture.
-
•
The aim of the remodeling phase (6 weeks postoperatively) is to balance matrix degradation (removal of weaker type II N-collagen) with matrix formation (replacement with stronger type I collagen). Homeostasis of the collagen fibres and the extracellular matrix of the scar is regulated by serine proteases and matrix metalloproteases. The corresponding clinical manifestations are normal tissue colour and scar formation.1,3 Any disruption of this orderly balance can lead to excess or inadequate matrix degradation and result in either a keloid scar or wound dehiscence.
Table 1.
Characteristics, timing, and scoring of the IPR Wound Healing Scale
| T/Phase | Score |
|||
|---|---|---|---|---|
| Parameter | Score 0 | Score 1 | Total score | |
| Inflammatory T: 3–5 days | Bleeding, spontaneously or on palpation | Yes | No | /8 |
| Granulation tissue | Yes | No | ||
| Haematoma | Yes | No | ||
| Tissue colour | Redder or whiter than opposite side tissue | Like the opposite side tissue | ||
| Incision margins | Incomplete flap closure/fibrin clot/partial necrosis/complete necrosis | Complete flap closure/fine fibrin line | ||
| Suppuration | Yes | No | ||
| Edema VAS (1–10) | VAS 6–10 | VAS 1–5 | ||
| Pain VAS (1–10) | VAS 6–10 | VAS 1–5 | ||
| Proliferative T: 14 days | Re-epithelialisation | Partial | Complete | /5 |
| Tissue colour | Redder or whiter than opposite side tissue | Like the opposite side tissue | ||
| Scar | Scar wider than 2 mm/contour irregularity | No scar/scar less wide than 2 mm/contour regularity | ||
| Suppuration | Yes | No | ||
| Pain VAS (1–10) | VAS 6–10 | VAS 1–5 | ||
| Remodeling T: 6 weeks | Scar | Scar wider than 2 mm/contour irregularity | No scar/scar less wide than 2 mm/contour regularity | /3 |
| Tissue colour | Redder or whiter than opposite side tissue | Like the opposite side tissue | ||
| Pain VAS (1–10) | VAS 6–10 | VAS 1–5 | ||
| Total process | /16 | |||
As part of the IPR Scale evaluation, patients rate their level of anxiety before the procedure and level of pain during the procedure and follow-up on a VAS.
Surgical extractions are defined by the American Dental Association as ‘surgical removal of an erupted tooth requiring elevation of a mucoperiosteal flap and removal of bone and/or section of tooth'.13 Tooth extraction is one of the most common procedures in dentistry in general and oral surgery in particular.13 Surgical extraction may be necessary in cases of tooth impaction in bone and/or soft tissue, tooth decay below the bone level, insufficient remaining clinical crown, tooth or root fracture, presence of periapical lesions or disease, and other conditions according to the discretion of the practitioner.13
Surgical extraction of impacted wisdom teeth involves ostectomy and surgical injury to the soft tissue, leading to pain and edema as part of the normal inflammatory response.14 Potential complications include bleeding, infection, nerve damage, and jaw fracture.15 The risks are influenced by background factors such as patient age, gender, and health status, according to the American Society of Anesthesiologists,16 in addition to clinical factors such as bone density, tooth position, degree of impaction, and surgeon experience.17
The aim of this study was to monitor the postoperative wound healing process following surgical wisdom tooth extraction using the IPR Scale.
Methods
Patients and setting
A prospective study was performed in the Department of Oral and Maxillofacial Surgery of a tertiary medical centre in Israel from June 2018 to June 2019. The protocol was approved by the institutional Helsinki Committee (approval number 0431-18-RMC). Participants included otherwise healthy consecutive patients aged 18 years or more who were diagnosed with a partial bony impacted wisdom tooth based on panoramic X-rays and underwent surgical extraction. Exclusion criteria were diabetes mellitus, smoking habit (cigarettes or other materials), and steroid intake. All eligible patients who agreed to participate in the study signed an informed consent form. Demographic and clinical data were obtained at enrolment.
Extraction procedure
Extractions were performed by a resident in oral and maxillofacial surgery. Local anaesthesia of the inferior alveolar, lingual, and buccal nerves was induced by infiltration of 2–3 capsules of lidocaine hydrochloride 2% and epinephrine at a ratio of 1:100,000. The surgeon evaluated patient pain perception prior to the start of the procedure by tapping the tongue, lower lip, chin, and gums around the relevant tooth. A triangular partial Neumann flap was raised to gain access to the tooth.18 Closure was performed by buccal flap advancement, and the entire surgical area was covered due to flap mobilisation. Suturing was performed with 3–0 catgut sutures.
After the extraction, patients were prescribed amoxycillin (Moxypen®) 500 mg three times/day for 7 days or, for those sensitive to penicillin, clindamycin 300 mg three times/day for 7 days. Additionally, patients were instructed to rinse with chlorhexidine 0.2% mouth rinse two times/day for 10 days, and in the event of acute pain, to take an analgesic (dipyrone 500 mg or paracetamol 500 mg) three times/day for up to 7 days.
Wound healing evaluation
At the time of surgery, two second-year residents in oral and maxillofacial medicine asked each patient to describe their preoperative anxiety level (registered before anaesthesia was induced) and intraoperative pain level (registered after anaesthesia was induced) by marking the appropriate place along a 10 cm line drawn on a sheet of paper.
During follow-up, the IPR Scale was used to monitor the wound healing process. Patients were requested to present at the clinic at 3–5 days, 14 days, and 6 weeks after the extraction day, corresponding to the three phases of wound healing (inflammatory, proliferative, and remodeling, respectively; Table 1). At each visit, the surgeon used the appropriate subscale to evaluate the wound. Each clinical manifestation was scored 0 or 1, yielding three subscale scores ranging from 0–8, 0–5, and 0–3, accordingly. The surgeon also took a clinical photo of the wound with a smartphone camera and submitted it for evaluation by two experts in oral and maxillofacial surgery (Fig. 1, Fig. 2, Fig. 3, Fig. 4). During the visits, patients again rated their pain level on the VAS. At the end of follow-up, the total score of the IPR Scale was calculated (0–16), where 0–4 indicated poor healing, 5–10 acceptable healing, and 11–16 excellent healing3 (Table 1). The subscale scores were given different weights in the calculation of the total score commensurate with their importance to the healing process. The inflammatory phase was considered the most important because inflammation can endanger the subsequent series of biologic events leading to early wound healing.1 The remodeling phase carried the least weight because it can continue for several years and basically involves maintenance of stability.1,3
Fig. 1.

Clinical appearance after impacted tooth extraction, inflammatory phase (first follow-up visit).
Fig. 2.

Clinical appearance after impacted tooth extraction, inflammatory phase (first follow-up visit).
Fig. 3.

Clinical appearance after impacted tooth extraction, proliferative phase (second follow-up visit).
Fig. 4.

Clinical appearance after impacted tooth extraction, proliferative phase (second follow-up visit).
Statistical analysis
Statistical analysis was conducted using SAS software, version 9.4 (SAS Institute Inc., Cary, NC, USA). Continuous variables are presented as means and standard deviations, and categorical variables as numbers and percent. Student t-test was used to compare continuous variables between groups and Fisher exact test or chi-square test, as appropriate, was used for categorical variables. Two-sided P values < 0.05 were considered statistically significant.
Results
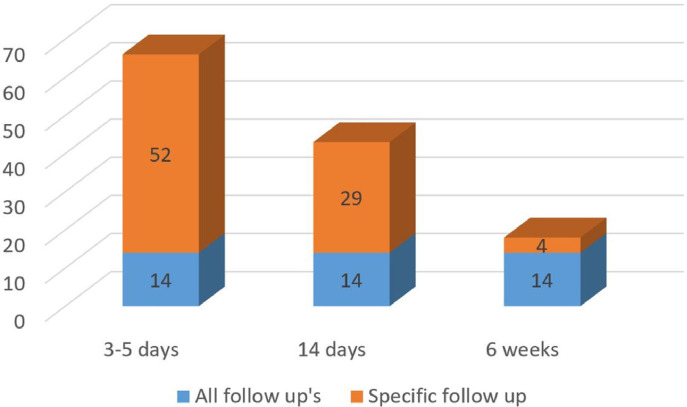
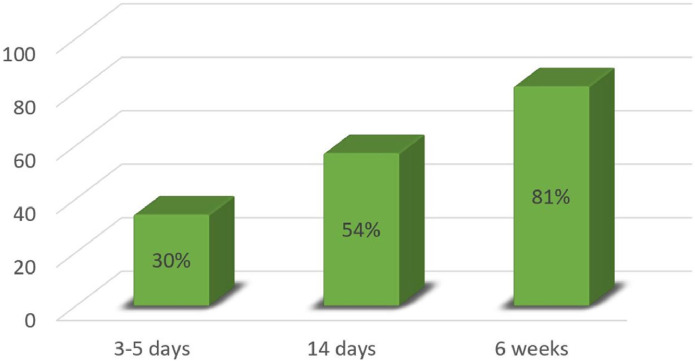
The study group included 94 patients (42 male 52 female) of mean age 45.5 ± 20.6 years (range 18–87). The mean operative time was 21.6 ± 13.4 minutes (median, 20 minutes; Table 2). Sixty-six patients attended the first follow-up visit, 43 the second, and 18 the third (Figure 5); the corresponding dropout rates were 30%, 54%, and 81% (Figure 6).
Table 2.
Self-reported VAS scores for preoperative anxiety, intraoperative pain and procedure timing in 94 patients undergoing tooth extraction
| Parameter | No | Mean | SD | Median | Range |
|---|---|---|---|---|---|
| Anxiety VAS | 88 | 5.9 | 3.6 | 6 | 1–10 |
| Pain VAS | 90 | 2.4 | 2.4 | 1 | 1–10 |
| Timing (minute) | 83 | 21.6 | 13.4 | 20 | 10–60 |
IPR, Inflammatory Proliferative Remodeling; VAS, visual analogue scale.
Fig. 5.
Fourteen of the 94 patients attended all three follow-up visits (orange). Of the remaining patients, 52/80 attended the first, 29/80 the second and 4/80 the third (blue).
Fig. 6.
Dropout rates according to the wound healing phases.
The mean VAS score was 5.9 ± 3.6 for preoperative anxiety and 2.4 ± 2.4 for intraoperative pain (Table 2). There was a positive correlation between preoperative anxiety and intraoperative pain (P = 0.65).
The mean total wound healing score on the IPR Scale was 14.43 ± 1.45, which is considered excellent. The mean wound healing scores for the three subscales (phases) were as follows: inflammatory phase, 6.35 ± 1.34; proliferative phase, 4.56 ± 0.8; and remodeling phase, 2.83 ± 0.51 (Figure 7). There was a negative correlation between the mean preoperative anxiety score on the VAS and the IPR Scale scores at each healing phase (inflammatory phase: r = —0.12, P = 0.34; proliferative phase: r = —0.02, P = 0.86; remodeling phase: r = —0.13, P = 0.64).
Fig. 7.
Patient wound-healing scores on the IPR Scale. IPR, Inflammatory Proliferative Remodeling; I, Inflammatory; P, Proliferative; R, Remodeling.
The effect of patient sex and age on IPR Scale scores, for both the subscales and the total, and on patient anxiety and pain was investigated. The results are shown in Table 3. Comparison by sex yielded a significant between-group difference in the inflammatory phase, with female patients having a lower wound healing score than male patients (4.56 ± 0.97 vs. 6.18 ± 1.33, P = 0.003 with the t-test and P = 0.02 with the Wilcoxon signed rank sum test). To evaluate the effect of age, the study group was divided into two groups: 18–25 and 26–87 years. There were no significant between-group differences in any of the subscale scores or the total score.
Table 3.
Effect of sex and age on scores of the IPR Scale in 94 patients undergoing tooth extraction
| Characteristic | Total score | Wound healing phase |
||
|---|---|---|---|---|
| Inflammatory | Proliferation | Remodeling | ||
| Patient sex | ||||
| Male | 9.39 ± 5.15 | 6.88 ± 0.97 | 4.56 ± 0.89 | 2.9 ± 0.32 |
| Female | 8.68 ± 4.15 | 5.88 ± 1.7 | 4.56 ± 0.75 | 2.75 ± 0.71 |
| Patient age | ||||
| 18–25 years | 10.0 ± 4.84 | 6.18 ± 1.62 | 4.67 ± 0.71 | 2.83 ± 0.41 |
| 26–87 years | 8.73 ± 4.55 | 6.28 ± 1.62 | 4.53 ± 0.83 | 2.83 ± 0.58 |
Two cases were complicated at the first follow-up (inflammatory phase) by the formation of an abscess requiring surgical drainage and a second course of antibiotics. Both resolved, and the patients showed proper healing at the subsequent follow-up visit (proliferative phase).
Discussion
Several studies have used indexes or scales to evaluate the wound healing process after extractions.2,5,10 The IPR Scale solves many of the problems of prior wound healing scales, including the lack of a standardised definition of ideal wound healing, failure to distinguish among the different phases of the wound healing process, and lack of correlation between the wound healing parameters applied and the wound healing phases.3 The scale is intended to help surgeons decide if and when to intervene in the healing process, according to the specific phase – inflammatory, proliferative, or remodeling.
As part of our evaluation, patients rated their anxiety and pain at different time points. The findings confirmed that oral surgery provokes high levels of anxiety before the procedure and this may affect pain perception during the procedure.
Eli et al.19 reported similar results in a study of 60 patients undergoing implant insertion wherein there was a significant relationship between state anxiety and pain perception at all time points evaluated: immediately before surgery, immediately after surgery, and four weeks postoperatively.
In our study, a negative correlation was found between VAS anxiety scores and IPR Scale scores, indicating that the more anxious the patient before the extraction, the lower the IPR Scale scores in all three phases. This finding supports the direct influence of anxiety on oral wound healing following extraction. It is well recognised that psychological stress can activate the hypothalamic-pituitary-adrenal and the sympathetic-adrenal-medullary axes, leading to enhanced glucocorticoid and catecholamine production, which can in turn directly affect several components of the healing process. Significant evidence from animal and human studies indicates that physiological stress responses can specifically impair the inflammatory phase.20 Of 193 healthy students who underwent a surgical procedure resulting in a 3.5 mm wound on the hard palate, those reporting high levels of depressive symptoms were almost 3.6 times more likely to be classified as slow healers than low dysphoric students.21 Greater clinician awareness of the association between psychological factors and wound healing might lead to more patient referrals for instruction in relaxation methods and behavioural adaptation, making the process easier for both patient and surgeon.
We found no effect of patient age on the wound healing process. However, comparison by sex revealed that female patients had significantly lower wound healing scores than male patients. These results are in line with the study of Engeland et al.22 who evaluated 212 patients 7 days after sustaining a 3.5-mm circular wound on the oral hard palate. They found that the mucosal wound healing process was slower in women than men (P = 0.008) regardless of age, suggesting that sex hormones play a role in oral mucosal wound healing, favouring men.
In the present study, there was a considerable dropout rate at the second and third follow-up visits. To our knowledge, there are no studies of tooth extraction in which follow-up was extended to 6 weeks. Given the good results on the PRI Scale, we assumed that the dropout rates were high later into follow-up because healing had already largely occurred, and the patients felt no need to attend subsequent clinic visits. Telecommunication technologies offer an increasingly popular solution for high follow-up attrition rates, and they may be adapted for use in wound healing to appropriately monitor outcomes according to relevant scales.23 Systematic reviews have shown that patients find the use of interactive videos acceptable in diverse medical contexts.24 The advantages include increased accessibility of specialist expertise, less need for travel, reduced waiting times,24 and cost- and time-saving for both patients and the healthcare system. In cases of surgical wounds, videos allow for direct visualisation by the clinician which is essential for diagnosis, treatment, and follow-up.
Future studies are needed to test the IPR Scale for wider applications in oral mucosal surgery so that clinicians will be able to identify wound healing patterns and specific modifiers that may promote or inhibit the healing process following surgical procedures.
Funding
No funding was procured for this work.
Conflict of interest
The authors declare that there are no conflicts of interest.
REFERENCES
- 1.Miloro M, Ghali GE, Larsen P, et al. 3rd ed. 2012. Peterson's Principles of Oral and Maxillofacial Surgery. Montpelier, VTPMPHUSA. [Google Scholar]
- 2.Pippi R. Post-surgical clinical monitoring of soft tissue wound healing in periodontal and implant surgery. Int J Med Sci. 2017;14:721–728. doi: 10.7150/ijms.19727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamzani Y, Chaushu G. Evaluation of early wound healing scales/indexes in oral surgery: a literature review. Clin Implant Dent Relat Res. 2018;20:1030–1035. doi: 10.1111/cid.12680. [DOI] [PubMed] [Google Scholar]
- 4.Yelamali T, Saikrishna D. Role of platelet rich fibrin and platelet rich plasma in wound healing of extracted third molar sockets: a comparative study. J Maxillofac Oral Surg. 2015;14:410–416. doi: 10.1007/s12663-014-0638-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Farina R, Simonelli A, Rizzi A, et al. Early postoperative healing following buccal single flap approach to access intraosseous periodontal defects. Clin Oral Invest. 2013;17:1573–1583. doi: 10.1007/s00784-012-0838-6. [DOI] [PubMed] [Google Scholar]
- 6.Wachtel H, Schenk G, Bohm S, et al. Microsurgical access flap and enamel matrix derivative for the treatment of periodontal intrabony defects: a controlled clinical study. J Clin Periodontol. 2003;30:496–504. doi: 10.1034/j.1600-051x.2003.00013.x. [DOI] [PubMed] [Google Scholar]
- 7.Quinn JV, Wells G. An assessment of clinical wound evaluation scales. Acad Emerg Med. 1998;5:583–586. doi: 10.1111/j.1553-2712.1998.tb02465.x. [DOI] [PubMed] [Google Scholar]
- 8.Quinn JV, Drzewiecki AE, Stiell IG, et al. Appearance scales to measure cosmetic outcomes of healed lacerations. Acad J Emerg Med. 1995;13:229–231. doi: 10.1016/0735-6757(95)90100-0. [DOI] [PubMed] [Google Scholar]
- 9.Pippi R, Santoro M, Cafolla A. The effectiveness of a new method using an extra-alveolar hemostatic agent after dental extractions in older patients on oral anticoagulation treatment: an intrapatient study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120:15–21. doi: 10.1016/j.oooo.2015.02.482. [DOI] [PubMed] [Google Scholar]
- 10.Panneerselvam E, Balasubramanian S, Raja VBK, et al. Plain lignocaine' vs 'lignocaine with vasoconstrictor'—comparative evaluation of pain during administration and post-extraction wound healing by a double blinded randomized controlled clinical trial. Acta Odontol Scand. 2016;74:374–379. doi: 10.3109/00016357.2016.1160148. [DOI] [PubMed] [Google Scholar]
- 11.Mozzati M, Gallesio G, Di Romana S, et al. Efficacy of plasmarich growth factor in the healing of post extraction sockets in patients affected by insulin-dependent diabetes mellitus. J Oral Maxillofac Surg. 2014;72:456–462. doi: 10.1016/j.joms.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Marenzi G, Riccitiello F, Tia M, et al. Influence of leukocyte-and platelet-rich fibrin (L-PRF) in the healing of simple post extraction sockets: a split-mouth study. Biomed Res Int. 2015 2015 doi: 10.1155/2015/369273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Surgical Extraction of Erupted Teeth and Retained Roots. Dental Coverage Guideline. Minnetonka, MN: United HealthCare Services; 2018, publication no. DCG005.04,1–2.
- 14.Balamurugan R, Zachariah T. Comparison of primary and secondary closure with a buccal mucosal-advancement flap on postoperative course after mandibular impacted third molar surgery. Oral Maxillofac Surg. 2020;24:37–43. doi: 10.1007/s10006-019-00814-w. [DOI] [PubMed] [Google Scholar]
- 15.Manor Y, Abir R, Manor A, et al. Are different imaging methods affecting the treatment decision of extractions of mandibular third molars? Dento Maxillofac Radiol. 2017;46 doi: 10.1259/dmfr.20160233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jerjes W, Swinson B, Moles DR, et al. Permanent sensory nerve impairment following third molar surgery: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:e1–e7. doi: 10.1016/j.tripleo.2006.01.016. [DOI] [PubMed] [Google Scholar]
- 17.Baensch F, Kriwalsky MS, Kleffmann W, et al. Third molar complications in the elderly – a matched-pairs analysis. J Oral Maxillofac Surg. 2017;75:680–686. doi: 10.1016/j.joms.2016.11.021. [DOI] [PubMed] [Google Scholar]
- 18.Izquierdo Gómez K, González Navarro B, Ortiz G, et al. The importance of flap design in third molar surgery: a systematic review. Biomed J Sci Tech Res. 2018;11:8798–8803. BJSTR. MS.ID.002164. [Google Scholar]
- 19.Eli I, Schwartz-Arad D, Baht R, et al. Effect of anxiety on the experience of pain in implant insertion. Clin Oral Implants Res. 2003;14:115–118. doi: 10.1034/j.1600-0501.2003.140115.x. [DOI] [PubMed] [Google Scholar]
- 20.Gouin J-P, Kiecolt-Glaser JK. The impact of psychological stress on wound healing: methods and mechanisms. Immunol Allergy Clin North Am. 2011;31:81–93. doi: 10.1016/j.iac.2010.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bosch JA, Engeland CG, Cacioppo JT, et al. Depressive symptoms predict mucosal wound healing. Psychosom Med. 2007;69:597–605. doi: 10.1097/PSY.0b013e318148c682. [DOI] [PubMed] [Google Scholar]
- 22.Engeland CG, Bosch JA, Cacioppo JT, et al. Mucosal wound healing – the roles of age and sex. Arch Surg. 2006;141:1193–1197. doi: 10.1001/archsurg.141.12.1193. [DOI] [PubMed] [Google Scholar]
- 23.Perednia DA, Allen A. Telemedicine technology and clinical applications. JAMA. 1995;273:483–488. [PubMed] [Google Scholar]
- 24.Mair F, Whitten P. Systematic review of studies of patient satisfaction with telemedicine. BMJ. 2000;320:1517–1520. doi: 10.1136/bmj.320.7248.1517. [DOI] [PMC free article] [PubMed] [Google Scholar]